
Emergency Medicine Through Leadership, Research, and Mentorship
An interview with Lewis S. Nelson, MD


Emergency Medicine Through Leadership, Research, and Mentorship
An interview with Lewis S. Nelson, MD

Exploring the R38 Mechanism: A Research Training Opportunity for Medical Residents

Ali S. Raja, MD, DBA, MPH SAEM President Massachusetts General Hospital
Harvard Medical School
Board Liaison to:
• Bylaws Committee
• Telehealth Interest Group
• Wilderness Medicine Interest Group

Pooja Agrawal, MD, MPH
Member at Large
Yale Department of Emergency Medicine
Board Liaison to:
• Ethics Committee
• Research Committee
• Academy for Diversity and Inclusion in Emergency Medicine (ADIEM)
• Informatics, Data Science, and Artificial Intelligence Interest Group
• Research Directors Interest Group
• Sex and Gender in Emergency Medicine Interest Group
• Tactical and Law Enforcement Interest Group
• Guidelines for Reasonable and Appropriate Care in the Emergency Department (GRACE)

Nicholas M. Mohr, MD, MS
Member at Large University of Iowa Carver College of Medicine
Board Liaison to:
• Equity and Inclusion Committee
• Program Committee
• Simulation Academy
• Disaster Medicine Interest Group
• Evidence-Based Healthcare & Implementation Interest Group
• Transmissible Infectious Diseases
Interest Group
• Advanced Research Methodology Evaluation and Design (ARMED)

Michelle D. Lall, MD, MHS SAEM President-Elect Emory University
Board Liaison to:
• RAMS Board
• Nominating Committee
• Committee of Academy Leaders (COAL)
• Academy of Geriatric Emergency Medicine
• Educational Research Interest Group
• Operations Interest Group

Jeffrey P. Druck, MD
Member at Large University of Utah School of Medicine
Board Liaison to:
• Awards Committee
• Clerkship Directors in Emergency Medicine
• Academic Emergency Medicine Pharmacists Interest Group
• Toxicology/Addiction Medicine Interest Group
• Certificate in Academic Emergency Medicine Administration (CAEMA)

Ava Pierce, MD
Member at Large UT Southwestern Medical Center, Dallas
Board Liaison to:
• Education Committee
• Workforce Committee
• Academy of Women in Academic Emergency Medicine
• Behavioral and Psychological Interest Group
• Oncologic Emergencies Interest Group
• ARMED MedEd

Jody A. Vogel, MD, MSc, MSW SAEM Secretary-Treasurer Stanford University
Board Liaison to: • Global Emergency Medicine Academy • Finance Committee • Airway Interest Group
• Social Emergency Medicine and Population Health Interest Group

Julianna J. Jung, MD, MEd
Member at Large
Johns Hopkins University School of Medicine
Board Liaison to:
• 2025 Consensus Conference Committee
• Fellowship Approval Committee
• Grants Committee
• Academy of Administrators in Academic Emergency Medicine (AAAEM)
• Clinical Researchers United Exchange (CRUX) Interest Group
• Palliative Medicine Interest Group
• Emerging Leader Development Program (eLEAD)

Lewis S. Nelson, MD, MBA Chair Member
Rutgers New Jersey Medical School
Board Liaison to:
• Consultation Services Committee
• Quality and Patient Safety Interest Group
• Vice Chairs Interest Group
• Chair Development Program

Daniel N. Jourdan, MD
Resident Member Henry Ford Hospital
Board Liaison to:
• Wellness Committee
• Climate Change and Health Interest Group
• Innovation Interest Group
• Neurologic Emergency Medicine Interest Group

Wendy C.
MD SAEM Immediate Past President UCLA Department of Emergency Medicine
David Geffen School of Medicine at UCLA

Ryan LaFollette, MD
Member at Large University of Cincinnati
Board Liaison to:
• ED Administration and Clinical Operations Committee
• Faculty Development Committee
• Membership Committee
• Academy of Emergency Ultrasound (AEUS)
• Critical Care Interest Group
• Emergency Medical Services Interest Group
• Pediatric Emergency Medicine Interest Group

to:
• SAEM Executive Committee
• Association of Academic Chairs of Emergency Medicine (AACEM)
• RAMS Board
• SAEM Foundation

in



Harvard Medical School/Massachusetts General Hospital 2024-2025 President, SAEM
As I reflect on our incredible progress in 2024, I want to express my heartfelt gratitude to all SAEM members and staff for their unwavering commitment to academic emergency medicine. Your dedication has propelled SAEM to new heights, making this year one of transformational growth and visionary leadership. Together, we’ve continued to break records, innovate, and shape the future of our specialty. Let’s take a moment to celebrate the many accomplishments of 2024.
In 2024, SAEM achieved a historic milestone with 9,200 members — a nearly 34% increase over the past five years. This remarkable growth reflects the strength of our community and our ability to bring together diverse professionals at all career stages.
SAEM24, held this past May in Phoenix, was our largest and most successful annual meeting to date. It featured the highest number of submissions ever for didactics, abstracts, innovations, and clinical images. With over 3,900 attendees—a record—this event showcased groundbreaking research, innovative educational content, and dynamic networking opportunities. Key highlights included our largest-ever SonoGames competition, which attracted a record 105 residency programs, as well as new workshops focused on addressing critical issues in emergency medicine.
The SAEM Foundation achieved remarkable milestones in 2024, awarding $1 million in grants—its largest funding
SAEM members, your extraordinary efforts made 2024 a banner year for our Society! Your dedication, engagement, and active participation have driven SAEM’s continued growth and success, shattering records across the board, including:
Highest membership numbers in SAEM’s history.
Record-breaking attendance at the SAEM24 annual meeting.
Unprecedented submissions for abstracts, didactics, workshops, innovations, and clinical images for SAEM24. Most committee interest forms ever submitted.
Record-setting award nominations.
We are incredibly grateful for all you’ve contributed to these remarkable achievements. As we step into the new year, let’s build on this momentum together.

total ever—to support 30 researchers and educators in academic emergency medicine.
In May 2024, SAEMF received a transformative $1 million commitment from SAEM, significantly enhancing resources for advancing emergency medicine research. This major donation coincided with a 58% surge in grant applications, underscoring the growing demand for research funding in the field.
Additionally, SAEM raised a record $104,015 for emergency medicine through this year’s Academy, Committee, and Interest Group Challenge and introduced two groundbreaking RAMS funding opportunities: the Ali and Danielle Raja RAMS Medical Student Research Grant and the David E. Wilcox, MD, FACEP Scholarship.
These initiatives are important steps forward in supporting research and career development for future leaders in emergency medicine.
SAEM’s journals continue to thrive thanks to the dedicated efforts of their editorial boards, reviewers, and authors.
Both journals experienced an increase in submissions in 2024, with Academic Emergency Medicine (AEM) showing a notable 27% growth. AEM remains a leading journal in the field, retaining its position as one of the largest peerreviewed publications in emergency medicine.
Academic Emergency Medicine Education and Training (AEM E&T), which received its first Impact Factor™ in 2023, continues to grow steadily, with a consistent rise in submissions.
Addressing a critical gap in nonopioid use disorder treatment, SAEM published the fourth Guideline for Reasonable and Appropriate Care in the Emergency Department (GRACE) series, SAEM GRACE-4: Alcohol Use Disorder and Cannabinoid Hyperemesis Syndrome Management in the Emergency Department
In 2024, SAEM expanded its efforts to promote diversity, equity, and inclusion (DEI) through several impactful initiatives and resources. Among these, the SAEM Board of Directors issued a strong statement in April opposing the EDUCATE Act. The statement emphasized that the proposed bill disregards the essential role of DEI initiatives in advancing health equity and improving patient outcomes.
Other 2024 SAEM community-developed DEI initiatives included:
• Expanded Diversity, Equity, and Inclusion Curriculum: Four new chapters were added:
- Ableism
- Intersectionality
- Identity-First Language
- Dealing with Racist or Bigoted Patients and Colleagues
• SAEM24 Consensus Conference: The conference, themed “Creating a Diverse and Sustainable Emergency Medicine Investigator Pathway,” focused on establishing a robust and diverse pipeline of federally funded clinicianscientists in emergency medicine.
• SAEM EM Mentorship and Pathway Program Directory: A comprehensive guide designed to help address health disparities, strengthen the emergency medicine pipeline, and cultivate the next generation of diverse professionals.
• DEI Glossary of Terms: A resource aimed at fostering inclusive dialogue and a deeper understanding of key DEI concepts.
• Leadership, Engagement, and Academic Pathway (LEAP): A program designed to support and encourage academic careers in emergency medicine.
continued on Page 6
• SAEM DEI Resource Library: A free online platform featuring articles, books, videos, and other educational materials on DEI topics such as the history of discrimination, patient care disparities, and faculty diversity.
Through these initiatives, SAEM reinforced its dedication to fostering a more equitable and inclusive emergency medicine community.
In 2024, 400 members authored more than 170 SAEM Pulse articles, contributing to a 46% growth in submissions from the previous year. To accommodate this growth, SAEM Pulse implemented several changes in 2024:
• A clear publication mission statement to guide future content.
• Updated SAEM Pulse Submission Instructions and Writer Guidelines, aligning with best practices and streamlining the submission process.
• An automated submission form to replace the previous email system, simplifying submissions, reducing errors, and speeding up turnaround times.
In 2024, SAEM’s academies, committees, and interest groups reaffirmed their dedication as leaders and innovators in emergency medicine (EM) education and research, contributing prolifically to the field. These included over 50 webinars, a record 170 SAEM Pulse articles, as well as curricula, didactics, abstracts, toolkits, podcasts, and more. This community-generated content brings diverse perspectives and insights, enriching the collective knowledge base and providing valuable resources for continuous learning and professional development.
Participation and engagement within SAEM saw remarkable growth in 2024, highlighted by a nearly 20% increase in committee sign-ups. SAEM also launched a new tier system for interest groups, complete with a checklist to guide groups aspiring to achieve Academy status. To further strengthen community connectivity, the transition to the HigherLogic Thrive platform enhanced the user experience with features such as a centralized social feed, streamlined navigation, and improved resource accessibility.
Here is a selection of the newest and noteworthy educational highlights from SAEM’s community groups:
• Comprehensive Fall Risk Assessment and Prevention Literature
• Boarding and Crowding Toolkit
• Roadmap to Emergency Medicine Research Funding
• Social Emergency Medicine Integrated Network for Advancing Research (SEMINAR)
• Securing Your First Faculty Position: A Guide for Residents and Fellows
• Roadmap to Emergency Medicine Research Funding
• Emergency Medicine Interest Group (EMIG) Guide: Curriculum & Handbook
• Biostats Made Simple, Sessions 1-6
In partnership with the NIH Office of Emergency Care Research and the National Institute of Neurological Disorders and Stroke, the Neuro-EM Scholars National K12 Program was launched in 2024 to recruit, mentor, and train early-career EM faculty in neurological disorder research. The program also emphasizes diversity and encourages participation from underrepresented backgrounds. SAEM’s strategic approach and partnerships in this initiative represent a pivotal moment for progress and innovation in EM research.
Thank you for being part of this extraordinary journey. I’m incredibly proud of all we achieved together in 2024. From record-breaking growth to innovative programs and research funding, SAEM remains at the forefront of academic emergency medicine. I encourage you to explore the many resources available to you as a member and stay engaged as we continue to shape the future of our specialty. Here’s to an even brighter 2025!
ABOUT DR. RAJA : Ali Raja, MD, DBA, MPH, is a professor of emergency medicine at Harvard Medical School and the deputy chair of the department of emergency medicine at Massachusetts General Hospital.
We’re immensely grateful for your contributions in 2024 and invite you to continue this exciting journey with us as we enter the new year! Here are ways for you to make an impact on the future of SAEM:
• Renew your membership: SAEM offers a range of membership benefits tailored to every stage of your career. Renew your membership today and make the most of what SAEM has to offer!
• Attend SAEM25: Join us May 13-16, 2025, in Philadelphia for top-tier educational content, networking, and career development in academic EM. Register today!
• Run for a leadership position in 2025: Consider nominating yourself for a society-wide elected office.
• Submit your work: Share your research and insights through publications like AEM or AEMET, Pulse, or by submitting your work for the SAEM annual meeting
• Attend a regional meeting: Participate in an SAEM Regional Meeting to share your research, receive/provide mentorship, and network with others in your area.

Washington University in Saint Louis
2024-2025 RAMS Board President
It’s hard to believe we’re already halfway through the academic year! So much has happened in the past few months: for our resident members, the 2024 fellowship match results have been announced and for our medical students, interviews for the 2025-2026 residency match season are drawing to a close. In my own program, I’ve had the opportunity to meet and interview many medical students who are emergency medicine-bound. I have been consistently impressed by the incoming class of emergency physicians I have met on the interview trail. They are diverse, accomplished, and enthusiastic about our specialty. The future of our field is bright.
The Resident and Medical Student (RAMS) board continues its work for you. In our ongoing efforts to increase membership engagement, we are actively seeking more opportunities for RAMS involvement within SAEM’s committees and academies. If you haven’t already, I highly recommend joining an academy or interest group to engage in the subspecialty work that most interests you and to connect with faculty mentors who are national leaders in their fields. As part of your SAEM membership, RAMS members can join an academy or interest group at any time for free. For those of you already involved in committee, academy, and/or interest group work, let us help you promote your opportunities for RAMS participation!
The RAMS board has exciting plans for the coming months. We will soon finalize our strategic plan for 20252027, setting our agenda to develop RAMS into leaders in academic emergency medicine. Additionally, we will host several webinars focused on professional development, including topics such as creating your residency rank list, transitioning from medical school to residency financially, and navigating the evolving landscape of medical technology in the clinical setting. If you can’t attend a webinar when it’s live, all past webinars are available on the SAEM website
Finally, RAMS board elections for 2025-2026 will open on January 27. As chair of the nominating committee this year, I’ve enjoyed reviewing the candidate packets for the upcoming election cycle. We have an outstanding slate of candidates, and I’m excited to see who will serve on the RAMS board next year. Be sure to check your email and SAEM account so your election ballot can be counted!
SAEM 25 in Philadelphia is just a few short months away. I look forward to seeing you all there!
ABOUT DR. CLOESSNER: Emily “Ly” Anne Cloessner, MD, MSPH, is a current PGY-4 and chief resident at Washington University in Saint Louis.
“The incoming class of emergency physicians is diverse, accomplished, and enthusiastic about our specialty. The future of our field is bright.”
Lewis S. Nelson, MD, is a professor and chair of the Department of Emergency Medicine at Rutgers New Jersey Medical School in Newark, New Jersey, and chief of the Division of Medical Toxicology at University Hospital. In January 2025, he will assume the role of dean at the Charles E. Schmidt College of Medicine at Florida Atlantic University.
Board-certified in emergency medicine, medical toxicology, and addiction medicine, Dr. Nelson has built a distinguished career in academic leadership and clinical expertise. Prior to his tenure at Rutgers, he served as vice chair for academic affairs and director of the medical toxicology fellowship at New York University School of Medicine.
Dr. Nelson’s leadership extends to several national organizations. He has served as a director of the American Board of Emergency Medicine (ABEM), president of the American College of Medical Toxicology (ACMT), chair of the Medical Toxicology Subboard, and president of the Association of Academic Chairs in Emergency Medicine (AACEM). Additionally, he has contributed to the Accreditation Council for Continuing Medical Education (ACCME) and currently holds the position of chair on the board of the Society for Academic Emergency Medicine (SAEM).
An influential academic, Dr. Nelson is an editor of Goldfrank’s Toxicologic Emergencies and serves on the editorial boards of Annals of Emergency Medicine and the Journal of Medical Toxicology. His research focuses on the medical and social consequences of substance use, particularly opioid overdose, alcohol withdrawal, and alternative pain relief strategies. His work has significantly shaped health policy on substance use, clinical care across healthcare settings, and education for learners at all levels.
Dr. Nelson has received numerous honors, including the American College of Emergency Physicians (ACEP) Award for Outstanding Contribution in Research (2023), NJMS Faculty of the Year (2018), and the ACMT Career Achievement Award (2018). He has also been a long-standing consultant to the Centers for Disease Control and Prevention (CDC), the Department of Health and Human Services (DHS), and the Food and Drug Administration (FDA).
A graduate of the State University of New York Health Science Center at Brooklyn (Downstate), Dr. Nelson completed his emergency medicine residency at Mount Sinai School of Medicine and a fellowship in medical toxicology at New York University School of Medicine. He also holds an MBA from Brandeis University.
Dr. Nelson’s career is defined by his dedication to advancing emergency medicine, medical toxicology, and public health through leadership, research, and service to the academic emergency medicine community.



What inspired you to join SAEM, and what aspects of the organization’s mission resonate most with you?
As a career academic clinician, SAEM’s focus on the role of education, research, and faculty development in improving patient outcomes represent what I value most.
As a current SAEM board member, what do you value most about the organization’s role in advancing emergency medicine education and research?
I most value SAEM’s focus on our members’ career interests and needs by providing platforms, such as committees and interest groups, to grow and engage with colleagues and leaders. I also highly appreciate the SAEM’s extensive collaboration within and outside the organization to tackle issues critical to the advancement of our specialty, such as faculty development and emergency department (ED) boarding.
What unique expertise or insights do you bring to the board, and how do you plan to contribute to addressing the challenges facing both our specialty and the organization?
I am the inaugural “chair member,” which represents an ex officio role for the past president of the Association of Academic Chairs in Emergency Medicine (AACEM). I bring
my perspectives as a long-standing chair who has other organizational leadership roles to (hopefully) enhance SAEM’s role as a member-centered, externally facing service organization.
What do you hope to achieve during your term on the board, and how do you see these contributions advancing SAEM’s strategic goals?
SAEM is a strong, member centered organization with diverse goals, nearly all of which reflect those of an academic chair. I am most interested on improving the pipeline of faculty with research skills, which is also a focus of AACEM, and on addressing faculty career satisfaction and longevity.
In your opinion, what role does SAEM play in shaping the future of emergency medicine, and how can the organization expand or strengthen that role?
By providing opportunities for communicating with likeminded colleagues, SAEM plays a key role in promoting critical thinking about our concerns and strategic thinking about solutions. The annual meetings, the online
“The emergency department, which serves as the face of the health care system to every community, is the first touch point for many patients with a substance use disorder.”
continued from Page 9
communities, and the active committee structure provides fertile ground on which to grow collaboration that set the trajectory for the future.
Are there specific SAEM programs or initiatives that have had a significant impact on your professional growth or practice?
SAEM’s focus on professional development has been highly instrumental in my career development, particularly in the second half of my career. Participation in the Chair Development Program (CDP) and my deep involvement with the affiliated AACEM have provided learning, skill-building, and networking opportunities that are hard to find anywhere else.
What emerging trends or challenges do you foresee in managing substance-related emergencies, and how can emergency medicine educators better prepare clinicians to address these issues?
No communities have been immune to the grasp of the substance use crisis. The ED, which serves as the face of the health care system to every community, is the first touch point for many patients with a substance use disorder. This optimally positions us with the opportunity to engage these patients in a consideration of the personal and social consequences of their disease and to provide support for them to seek treatment. In addition, the funding environment from federal agencies interested in investing in low barrier ED programs is favorable for clinicians championing ED based care. Unlike most other diseases, in which a plethora of systems and clinicians exist to manage their disorder, the substance-using population is marginalized and disconnected, lacks adequate access and funding for care, and is challenging to study due to structural issues, such as poor follow up.
Your research addresses critical topics like opioid management and medication safety. How can emergency medicine academicians translate these research findings into real-world practice while maintaining patientcentered care?
As a specialty we have stepped up and made incredible progress in identifying patients with or at risk for substance-use related consequence and engaged

Dr. Nelson explaining the uses and toxicity of the mayapple plant.
them in both short term and longitudinal treatment. For example, we have metered our opioid prescribing, distributed or prescribed naloxone, and created navigator programs to get our patients the care that they need to recover. All of these are evidence-based strategies that make sense. Burgeoning within the specialty is a focus on other substances, particularly alcohol and stimulants. We have clearly taken ownership of this societal concern and made great strides to address it.
Looking ahead, what areas of medical toxicology or emergency medicine research hold the greatest potential to transform the field?
One of the best parts about both specialties is that there are an endless number of research opportunities that can transform both the specialty and healthcare. Academic emergency physicians and medical toxicologists are

involved in basic science, clinical and translational, epidemiological, health services, and many other important venues. Substance use research reaches beyond opioids, and is increasingly focused on alcohol and alcohol withdrawal, stimulants, novel psychoactive substances, cannabis, and those less acutely consequential, such as nicotine. Well initiated, evidence-informed care in the ED for patients with common poisonings such as acetaminophen, carbon monoxide, or snakebite will pay dividends in improving healthcare outcomes.
You’ve held leadership roles in organizations like the American College of Medical Toxicology, AACEM, and SAEM. What lessons have you learned about leading change in academic emergency medicine?
As John Donne famously said, “No man is an Island,” and that is increasingly true of success in academic health care. Without a team, collaboration, communication, and trust, we will never optimize progress. Helping those to whom I am accountable identify and act on their interests is an important part of academic leadership.
What strategies have you found most effective for fostering collaboration and innovation among faculty, residents, and students?
Providing both opportunity and support that allow people to succeed (and occasionally fail, which is ok) has proven to be a successful approach. We choose academic healthcare because we enjoy making positive change in things about which we are passionate. Research and scholarship are daunting without the right infrastructure, which is a departmental expectation to support. This includes making mentorship connections, vetting research ideas, thinking through methodological strategies, allocating statistical and informatics effort, and providing operational support. Mentorship is key in academic medicine. What role does mentorship play in your vision for emergency medicine, and how do organizations like SAEM support these efforts? Mentorship is a skill that is honed through interpersonal engagement and academic collaboration. SAEM provides an environment to foster growth of these skills both through its formal educational activities and opportunities for relationship building.
Please complete the following three sentences:
1. In high school, I was voted most likely to thrive in settings of controlled chaos.
2. A song you’ll find me singing in the shower is (Have you heard me sing? I hum a repertoire of Beatles music.)
3. A quote I live by is “It’s all relative.”
Who would play you in the movie of your life and what would that movie be called?
Neil Patrick Harris in “Doogie Becomes a Dean.”
If you could invite three people, past or present, to your dream dinner party, who would be on the list?
1. Larry David, comedian, actor, writer and television producer.
2. Serena Williams, former professional tennis player, widely regarded as one of the greatest of all time
3. Stephen Dubner, journalist, podcaster, radio host and author of the popular “Freakonomics” book series
What is your guiltiest pleasure (book, movie, music, show, food, etc.)?
Twice a day ice cream (even when not on vacation).
You have a full day without any obligations — how do you spend it?
Being outside, doing anything, perhaps getting in a run or catching up on work (particularly during a thunderstorm!).
What tops your bucket list?
Wine tasting in Tuscany with my family. What's one thing few people know about you?
My ringtone is “Frolic “(the “Curb your Enthusiasm” theme song).
By Danielle Haussner, MD; Catrina Cropano, MD; Michael Redlener, MD; Samuel E Sondheim, MD, MBA; Amos J. Shemesh, MD; and
Mark Hanna, MD, on behalf of the SAEM Disaster Medicine Interest Group and the SAEM Administration and Operations Committee
Ensuring Emergency Department Preparedness During Downtime
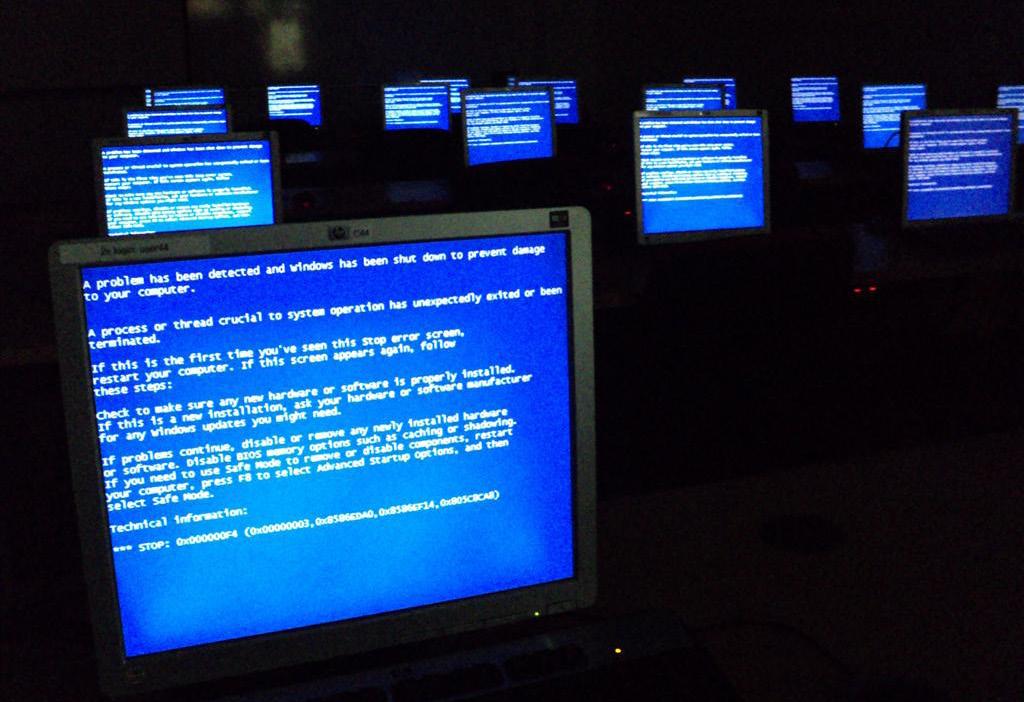
As health care continues to undergo rapid digital transformation and increasingly relies on technology to function, cyber disruptions have emerged as a significant threat to hospitals. These attacks can compromise protected health information, disable electronic medical records (EMRs), disrupt medical devices such as pumps,
monitors, and ventilators, and hinder essential communication systems, including internet and phone networks. Downtime, defined as the failure or unavailability of technological systems, can severely disrupt workflows, impact patient outcomes, and lead to substantial financial burdens.
Emergency departments (EDs) are especially vulnerable because they provide 24/7 urgent and emergent
care to undifferentiated patients. Preparing for unplanned and prolonged downtime is essential. Cyber disruptions are no longer hypothetical but inevitable, as demonstrated by recent high-profile incidents. A ransomware attack disabled Staten Island’s Richmond University Medical Center’s EMR for three weeks, while a 2024 attack on Ascension left its EMR inoperable for six weeks.

“With 386 health care cyberattacks reported this year to date, the need for robust downtime procedures in emergency departments is more critical than ever.”
Real world casualties of unplanned downtime events include canceled surgical procedures, rerouted emergency medical services (EMS) patients, and inaccessible medication terminals. Beyond operational impacts, unplanned downtime carries devastating financial risks. A single data breach in health care costs an average of $11 million, encompassing system recovery, data restoration, and legal liabilities. The U.S. Department of Health and Human Services Office for Civil Rights imposes substantial penalties for violations of the Health Insurance Portability and Accountability Act (HIPAA). For instance, the Change Healthcare cyberattack caused significant disruptions, with 74% of affected hospitals reporting impacts
on patient care and 94% reporting financial losses. Among hospitals hit by ransomware attacks, 53% reported increased mortality rates, and 54% were unable to provide full patient services.
With 386 health care cyberattacks reported this year to date, the need for robust downtime procedures in emergency departments (EDs) is more critical than ever. This article outlines key strategies for ED operations leadership to address these challenges and maintain care delivery during such disruptions, drawing on experiences from NewYorkPresbyterian and Mount Sinai Health Systems in New York City.
Addressing Planned vs. Unplanned Downtime
EDs are adept at managing planned EMR downtimes, which are typically scheduled during overnight hours when patient volumes are lower. These planned interruptions allow for strategies such as minimizing patient movement, placing bulk orders before the shutdown, coordinating communication among multidisciplinary teams, and completing documentation once systems are restored. However, while effective for scheduled events, these strategies are insufficient for unplanned or prolonged downtimes, exposing a significant gap in preparedness. As the frontline of health care, EDs must be equipped to maintain operations during
continued on Page 15
Figure 1. Downtime checklist for clinical administrator.

continued from Page 13
unforeseen disruptions. Notably, in 2023, the average duration of unplanned downtimes caused by ransomware attacks was 18.7 days.
For unplanned downtime events, procedures should be initiated at the 20-minute mark. A clinical administrator, such as a physician or nursing leader, should lead a huddle to update staff, activate downtime processes, and escalate the issue to departmental and hospital leadership. Using a checklist-based framework, such as the Team Strategies and Tools to Enhance Performance and Patient Safety (TeamSTEPPS) model, ensures essential actions are taken to sustain care delivery effectively. For reference, see Figure 1, which provides an example checklist from Mount Sinai Morningside and Mount Sinai West.
A downtime cart (Image 1), equipped with preassembled patient charts and standardized documentation, is essential. These materials should include forms for lab orders, medications, imaging, nursing actions, provider notes, progress notes, and consent forms. Checklist-style order forms ideally list commonly ordered items with standard dosing, frequency, delivery methods, etc. to reduce ordering errors and to improve efficiency. Specialized binders for codes and notifications like cardiac arrest, trauma, stroke, and sepsis should also be prepared. Provider notes should align with 2023 evaluation and management (E/M) coding updates to facilitate streamlined documentation and billing.
To track patient movements during downtime, a rolling whiteboard with room numbers, and dry-erase markers can help maintain real-time changes in patient movements. For transparency, patients should be informed of the downtime and its potential impact by a dedicated patient notification team, ideally involving nursing leadership and patient services.
Pharmacy and nursing staff should manage the automated medication dispensing system (e.g., Pyxis) in override mode, manually verifying each medication issued to ensure accuracy. ED providers should have access to the imaging system (e.g., PACS) to review available images, with radiologists either present in the clinical space for formal interpretations or providing reliable communication for all reads. Critical radiology and laboratory results must be reliably and promptly communicated to providers via telephone. On-call directories should be regularly updated to facilitate easy access to consultants or admitting teams, with clearly defined escalation paths and backup contacts available. Overhead announcements should be used for codes and notifications to ensure timely team coordination and response.
A readily available library of preprinted discharge instructions for common chief complaints should be accessible for distribution to patients at discharge. Providers should also be supplied with prescription sheets that comply with state regulations for issuing discharge medications. After patient disposition, all charts should be finalized and submitted to the medical records team for proper processing.
Downtimes can be challenging for ED providers, staff, and patients, but proactive planning and welldesigned strategies can minimize their impact and ensure continuity of care until systems are restored. Key steps include implementing structured huddles, utilizing checklists, providing intuitive prebuilt materials, establishing clear workflows and communication channels, and coordinating protocols across ancillary and consult services. Each site should customize downtime protocols to meet its specific structure and operational needs.
A formal downtime committee with representatives from multiple sites fosters collaboration, standardization, and the exchange of best practices. Regularly conducting and refining
downtime drills further strengthens preparedness. By adopting these strategies, EDs can cultivate a culture of readiness and continue to deliver high-quality emergency care, even during the most disruptive events.

Dr. Haussner is an assistant attending physician in the department of emergency medicine at NewYorkPresbyterian Weill Cornell Medicine and a fellow in healthcare leadership and management. She can be reached at dbm9003@med.cornell.edu

Dr. Cropano is an assistant professor in the department of emergency medicine at the Icahn School of Medicine at Mount Sinai and serves as the medical director for the Mount Sinai Beth Israel emergency department and as associate medical director for the Mount Sinai West emergency department. She can be reached at catrina. cropano@mountsinai.org


Dr. Redlener is an associate professor in the department of emergency medicine at the Icahn School of Medicine at Mount Sinai and serves as the medical director for the Mount Sinai West emergency department. He can be reached at michael. redlener@mountsinai.org
Dr. Sondheim is an assistant professor in the department of emergency medicine at the Icahn School of Medicine at Mount Sinai and serves as the assistant medical director for the Mount Sinai Morningside emergency department. He can be reached at samuel.sondheim@mountsinai.org

Mark Hanna, MD, is an assistant professor in the department of emergency medicine (in pediatrics) at the Vagelos College of Physicians and Surgeons at Columbia and the director of disaster preparedness for NYP-West. He can be reached at mh4401@cumc.columbia.edu

Dr. Shemesh is an assistant professor in the department of emergency medicine at NewYork-Presbyterian Weill Cornell Medicine and serves as the director of clinical and faculty affairs. He can be reached at ajs9039@med.cornell.edu

By K. Robert Thompson III, MD, MBA and James Summers, MD, on behalf of the SAEM Administration and Operations Committee
The University of Cincinnati Department of Emergency Medicine is home to the nation’s first emergency medicine residency and provides emergency care at two hospitals in the UC Health System. The University of Cincinnati Medical Center (UCMC) is a tertiary referral center, a Level-1 Trauma Center, and the safety-net hospital for Southwest Ohio, handling an annual volume of 65,000 patient encounters. West Chester Hospital (WCH), a suburban community hospital and Level-3 Trauma Center, manages an annual volume of 43,000 patient encounters.
To address growing patient volume and waiting times, the UC
Department of Emergency Medicine implemented various initiatives, with mixed success. Ultimately, "Triage Protocols" were established at both UCMC and WCH. These protocols allow nursing staff to collect designated diagnostics (e.g., labs, electrocardiograms, X-rays) based on the chief complaint. However, as post-pandemic boarding burdens increased, the department faced higher-acuity patients in the waiting room and a rising number of patients leaving without being seen (LWBS), often without the ability to address concerning results.
In August 2022, the Provider in Triage (PIT) model was launched at
UCMC. The primary goal was patient safety, particularly addressing significantly abnormal lab values and conducting more targeted evaluations of waiting room patients. Several operational changes were required to implement this project. First, the 12-bed fast-track pod was converted into a standard acuity pod. Two large rooms were then transformed into vertical care areas with three loungers separated by curtains to treat lower-acuity patients. Attending staffing was adjusted to cover these new care areas, enabling the redeployment of Advanced Practice Providers (APPs) from the fast-track area to PIT, where

“The value of having more patients seen by a provider, even if they leave before treatment completion, cannot be overstated. This process has allowed the identification of patients with time-sensitive conditions that may have been missed with traditional triage methods.”
they performed medical screening exams (MSEs) for patients awaiting beds. Efforts were made to preserve resident education by limiting nontime-sensitive imaging during initial evaluations.
The following year, the emergency department (ED) partially opened a new, state-of-the-art facility. This phased opening allowed for early adjustments to address anticipated boarding challenges. The design incorporated triage rooms, workspaces, and internal waiting areas to support a 24/7 Provider in Triage (PIT) model.
While awaiting the completion of the full facility, specifically the fasttrack pod, the department trialed a hybrid PIT staffing model. This model combined advanced practice providers (APPs) and faculty members to try to optimize patient flow through the PIT process. Faculty were tasked with conducting medical screening exams (MSEs) alongside APPs and managing fast-track patients with residents. However, were pulled in too many directions for the hybrid model to function effectively within the interim fast-track space.
When the fast-track pod became
operational during the final phase of the ED opening, the department transitioned to a PIT model fully staffed by APPs, with double coverage scheduled from 10 a.m. to 1 a.m. The redesigned space enabled staff to efficiently screen patients, administer therapeutics, facilitate patient movement, and discharge patients without occupying an ED room. Additionally, the PIT process empowered APPs to utilize resuscitation bays for patients needing a room immediately and
“The Provider in Triage process empowered advanced bays for patients needing a room immediately and ensured were appropriately prioritized, significantly advancing

continued from Page 17
ensure those requiring the next available room were appropriately prioritized. This approach significantly advanced the department's mission of enhancing patient safety and care efficiency.
In November 2022, WCH initiated a similar PIT model aimed at improving the safety of patients waiting in the lobby. The existing triage space was adapted to allow providers to perform MSEs and initiate work-ups more efficiently, prioritizing the sickest patients and those with time-sensitive conditions.
Compared to UCMC, WCH experiences a lower burden of boarding; thus, one challenge at WCH was creating a dynamic PIT model that could be activated during periods of boarding and deactivated when boarding was less prevalent. This approach ensured that resources were allocated appropriately to areas of greatest need.
To accomplish this, activation criteria were established, including a composite of the number of patients in the lobby and the number of patients “to be admitted.” When activation criteria were met, the PIT team was assembled. The PIT team and their responsibilities are as follows:
• Triage Nurse: Conducts triage questions, takes vitals, and orders protocol labs and electrocardiograms based on the complaint.
• Medic (when available): Starts IVs and collects protocol labs.
• Provider (usually an APP): Performs
MSEs, orders additional labs or imaging, and administers preapproved therapeutics.
• PIT Nurse: Collects labs, administers medications, coordinates patient movement through the triage process, and cleans PIT rooms between patients.
• Lead Nurse: Pulls patients into PIT rooms, collects additional labs as needed, repeats vital signs on lobby patients every two hours, discharges patients from triage as appropriate, and rooms patients in ED beds once available.
When activation criteria are met, two patient rooms near the front of the ED are repurposed as PIT rooms. In these rooms, the PIT provider can perform MSEs, order additional diagnostics and therapeutics, and identify patients who need a room immediately or who may be suitable for discharge once their work-up is complete. A second triage area and a family consult room are designated as "discharge rooms," where attending physicians can evaluate low-risk patients from the lobby who have completed their workups and decide whether to discharge them or order additional diagnostics.
If a patient leaves before an MSE, they are classified as Left Without Being Seen (LWBS). If the patient leaves after an MSE but before being roomed, they are classified as Left Before Treatment Complete (LBTC). The combined total of LWBS and LBTC patients is referred to as the Walkout Rate.
When the PIT model was implemented in August 2022, the LWBS/Walkout rate was 10% at both UCMC and WCH, with the goal of reducing it to 3%. As of November 2024, UCMC's LWBS rate has
advanced practice providers to utilize resuscitation
those requiring the next available room
dropped to 3.92%, and WCH’s rate has improved to 2.9%. Walkout rates have been more difficult to change, with UCMC showing stable rates that are trending downward and WCH improving to 4%. As part of the safety mission, both UCMC and WCH review the cases of all LBTC patients, call back any patients with critical or significantly abnormal results, and document the discussion. At UCMC, LBTC cases from the previous 24 hours are reviewed by the Medical Direction Team, while WCH uses the morning shift APP to conduct this review. Between August 2022 and November 2024, follow-up calls were made to 518 patients from the UCMC and 133 patients from WCH. These patients had critical or significantly abnormal test results that might otherwise have gone unaddressed. The value of having more patients seen by a provider, even if they leave before treatment completion, cannot be overstated. This process has allowed the identification of patients with time-sensitive conditions that may have been missed with traditional triage methods. Additionally, patients who see a provider in triage not only tend to wait longer in the lobby before walking out but are more likely to complete their visits. While efforts to optimize the PIT process continue, its impact on improving patient safety, morbidity, and mortality is a crucial to the mission of providing timely and appropriate care to all patients presenting to the emergency departments.


Dr. Thompson is an associate professor of emergency medicine at the University of Cincinnati and serves as the medical director at the University of Cincinnati Medical Center.
Dr. Summers is an assistant professor of emergency medicine at the University of Cincinnati and serves as the associate medical director at the University of Cincinnati West Chester Hospital.

By Nathan Sandalow, MD; Cole Ettingoff, MPH; Dana Im MD, MPhil, MPP; and Michael Wilson, MD, PhD on behalf of the SAEM Behavioral and Psychological Interest Group
An educator is working with a medical student during his first clinical shift when a call comes over the radio: “We’re coming to you with a 15-year-old male… self-inflicted gunshot wound… bradycardic, hypotensive.” On arrival, brain matter is visible from a wound near the ear. As a dedicated educator, you demonstrate how to assess for brain death and pupil reactivity. The student asks clinical questions and shows great interest. Later, you notice the student staring at the spot where the teen was pronounced dead. Emotionally, he turns to you
and asks, “What do I do now? How am I going to sleep tonight?” How would you respond?
Clinicians expect to face difficult moments and are responsible not only for their own emotional wellbeing but also for the well-being of their patients. As educators, there is an added responsibility to help learners process their reactions to stressful events. Students, many of whom have never experienced traumatic scenarios, are particularly vulnerable. The reactions of those around them can significantly impact how they incorporate the experience and shape their approach
to future trauma. Educators have the opportunity — and the responsibility — to intervene early, setting students on a path toward resilience in a highstress career.
Students are aware that they are being evaluated and may modify their reactions to impress their evaluators. Therefore, it is essential to remain sensitive to subtle signs of distress. This article reviews strategies for addressing these issues.
While students may anticipate witnessing disturbing events, it is crucial to acknowledge this
“Students are at high risk of psychological distress and are least well-trained for coping with these stressors.”
possibility during orientation.
Reassuring students that long-term psychological effects are unlikely can help prepare them. Good educators adjust their level of supervision based on students’ technical abilities, but similar sensitivity should be applied to students' life experiences. This ensures they feel comfortable sharing when an event causes distress. Trauma-informed care recognizes that each person may be affected by different exposures. Educators should avoid appearing judgmental if a seemingly benign event triggers strong feelings in a student.
Orientation materials should include information on self-care, such as encouraging physical exercise and proper sleep hygiene, especially for overnight shifts. Students should be reminded that cold, dark environments should be arranged after overnight shifts to help facilitate rest. Proactive self-care practices — such as sleep hygiene, diet, and exercise — are essential for recovery.
Point-of-Care Strategies
Most trauma survivors experience good psychological recovery. The primary way that attendings can help students is by taking care of their own emotional needs while remaining present for those around them. A wide range of normal reactions exist, and none are inherently inappropriate. A study of student experiences with death found that while students often believe crying is unacceptable, they appreciate the opportunity to share a tear with attendings (Pessagno et al). Grounding techniques, such as box-breathing, should be taught and demonstrated for students. If students become extremely distressed and unable to continue, offer them a break from clinical duties. Students are rarely critical to the team and should

be allowed time for self-care when possible. A brief walk, preferably outdoors, can help.
Humor can strengthen camaraderie and ease tensions, but it must be used sensitively. What may be acceptable among colleagues could offend patients, families, or others outside the group (Watson). Students, undergoing the process of initiation, may struggle to distinguish between appropriate and offensive humor. They may also laugh to ingratiate themselves with others, even if they are uncomfortable. To avoid inappropriate humor, it is best to refrain from making jokes. However, humor is a natural human response
to tragic events; after all, we are humans before we are clinicians. Jokes that mock or poke fun of others are never acceptable, and overuse of humor may indicate poor emotional processing, even if individual jokes seem appropriate.
A sense of helplessness is a significant risk factor for posttraumatic stress disorder (PTSD). Students, being the least trained members of the team, are at the highest risk (d’Ettorre et al). Giving students specific tasks, such as practicing relevant procedures or

from Page 21
learning an algorithm, will help them find meaning in the event and incorporate it productively. Highlighting the importance of simple tasks, such as assisting with equipment or applying pressure to a wound, can help mitigate feelings of helplessness.
Schools should refer traumatized students to counseling and peer groups when necessary. Social isolation is a known risk factor for adverse outcomes. Clinical rotations can feel isolating compared to preclinical years, so incorporating time for students to socialize and discuss cases — even if not specifically about psychological trauma — can be therapeutic.
Psychological first aid (PFA) encourages minimal disruption to usual routines. Students experiencing traumatic events should be encouraged to continue hobbies and exercise, though this may be difficult due to the demands of emergency medicine (EM). Absence policies should reflect this reality, allowing for recovery time following traumatic events. A brief period for self-care should include connecting with friends and family, as well as rest and relaxation.
Simulation can help prepare students for challenging events without direct patient risk. However, using simulation to expose students to death is not recommended, as it can cause unnecessary distress without providing substantial benefit. Ethical arguments against creating distress in students are strong, especially for those not pursuing a career in direct patient care.
Universal psychological debriefing has been studied and found to be potentially harmful. The proposed mechanism is that such counseling can overly consolidate a mildly
disturbing memory, increasing the risk of PTSD. Psychological debriefing should not be confused with debriefing to improve team performance, which should include directing distressed participants to available resources. According to the World Health Organization, psychological debriefing should be replaced by PFA, which specifically cautions against forcing individuals to talk about their feelings if they do not wish to.
Emergency personnel are at higher risk for alcohol and drug abuse, and tragic events can trigger substance use. Students may also be inclined to use drugs or alcohol but may not disclose this to their evaluators. While alcohol and benzodiazepines can temporarily blunt emotions, they prevent proper emotional processing. Students should be cautioned against relying on these substances as coping mechanisms.
Medications for PTSD Prevention
Some promising evidence suggests that controlled use of steroids, selective serotonin reuptake inhibitors (SSRIs), intranasal oxytocin, and betablockers could help prevent PTSD in high-risk individuals (Frijling et al). While these medications are not yet approved for clinical use, there may be a future role for psychological "postexposure prophylaxis" in individuals exposed to traumatic events.
Stressful events are a natural part of emergency medicine, and students are particularly vulnerable to psychological distress. As clinicians and educators, it is our role to guide students through these challenges, promoting long-term career longevity and emotional resilience. Orientation materials should introduce students to self-care strategies, and educators should help students find meaningful ways to contribute to the team while remaining sensitive to their emotional needs. After a traumatic event, students should be encouraged to maintain their routines, with adjustments to their clinical schedules if necessary. Social connections should be promoted, while isolation
and numbing behaviors should be discouraged.
To answer the student's question: “While it’s natural for you to have difficulty sleeping tonight, it is unlikely that you will experience long-term psychological effects. If you can find meaning in this case, it may become an opportunity for emotional and professional growth. I suggest you read about suicide prevention or brain injury to prepare for future cases. You could also contribute by writing an article for SAEM Pulse on strategies for dealing with stressful events. Do not perseverate. If you find it difficult to take your mind off the event, try taking a walk outdoors, playing a game with friends, or exercising. Let’s check in soon to see how you are doing. If you are still having trouble, I can refer you for counseling.” (Note: No students were harmed in the writing of this paper.)

Dr. Sandalow is an associate professor of emergency medicine at Chicago Medical School and an attending physician at Advocate South Suburban Hospital. His professional focus is on innovations in medical student education and curricular development.

Cole Ettingoff is a medical student with an interest in all aspects of emergency medicine, EMS, and public health. He is vice president of the American Association of Public Health Physicians and particularly interested in the unique role emergency medicine plays in the broader healthcare system.


Dr. Im is an attending emergency physician at Mass General Brigham and Harvard Medical School, where she leads quality and safety initiatives across the MGB Emergency Medicine System as the MGB enterprise emergency medicine director of quality and safety.
Dr. Wilson is an associate professor in the departments of emergency medicine and psychiatry at the University of Arkansas and serves as the emergency department lead for neurological emergencies, psychiatric emergencies, and substance use disorders.

By Andrew Melendez, DO and Salil Phadnis, MD
As the academic year progresses, fellows across the country may find themselves balancing the excitement of starting their wellearned fellowships with the realities of navigating the job market as future attending physicians. This can be particularly challenging for those in one-year fellowships, where the timeline is short and intersects with other obligations like written board exams. To guide fellows through this process, Dr. Anna Bona from Indiana University School of Medicine and Dr. Annemarie Cardell from Emory University recently shared their insights during a Simulation Academy Early Career
Subcommittee session. Their discussion highlighted a significant gap in graduate medical education: while many residency programs offer a "life after residency" component in their curriculum, the nuances of seeking employment after fellowship are often left to mentorship and trialand-error experiences.
The panelists focused on four key topics, which are outlined below.
A crucial first step in this process is self-reflection on career aspirations. Fellows should consider asking themselves:
• What proportion of my time do I want to allocate to simulation vs. clinical practice?
• Is there a particular group of learners I want to work with?
• Is interprofessional simulation a priority for me?
• Do I want to focus on quality and safety initiatives?
• Am I interested in collaborations, such as EMS education partnerships?
• Do I anticipate my simulation career following an administrative path (e.g., simulation center director) or a medical education path (e.g.,
“The transition from fellowship to a faculty position is an exciting yet challenging culmination of years of dedicated training.”
graduate medical education core faculty)?
• Is simulation research a key interest, and do I anticipate needing support with funding and grant writing?
Discussing the answers to these questions with a fellowship mentor can help fellows narrow down a list of institutions to target.
Early engagement with key personnel such as simulation directors, residency program directors, and department chairs is highly recommended. Fellows should reach out to mentors from their residency and fellowship programs to connect with faculty at institutions of interest. Keep your curriculum vitae (CV) updated throughout your fellowship year so it is readily available for a "warm introduction." These connections and the conversations that follow can clarify expectations for prospective faculty positions, uncover unanticipated opportunities, and potentially even lead to interviews before positions are publicly posted.
Fellows should not underestimate the freedom of choosing their own location post-fellowship. This is an opportunity to take newly developed skills to the place that best aligns with personal and professional goals. Unlike previous moves dictated by medical school acceptances and the Electronic Residency Application Service (ERAS) algorithm, fellows now have control over their location.
Considerations for fellows include:
• The moderate benefit of remaining at their current institution or returning to their residency training site, as the familiar environment may ease the transition to a faculty role.

• Personal and family preferences, especially after years of limited choices during training.
• Regional variations in job offerings and compensation.
Gaining an understanding of regional norms for compensation and benefits during the negotiation phase is new for most fellows. It is rare to accept a job offer without negotiating in some way. Fellows can ask local mentors and seek connections with junior faculty in the target city to clarify local norms. This knowledge helps ensure fellows are not undervalued. City-specific advice is often shared by mentors from a fellow’s residency or fellowship program who have experience helping trainees negotiate contracts.
The transition from fellowship to faculty position is an exciting yet challenging culmination of years of dedicated training. Although the process may seem overwhelming, taking time to reflect on career goals, seeking mentorship, and making meaningful connections can lead to
valuable opportunities. Choosing a location that aligns with both personal and professional priorities adds another layer of fulfillment. Finally, embracing the negotiation process allows fellows to start their new roles with confidence and clarity. With preparation and mentorship, fellows can turn this pivotal moment into the foundation for a successful career.

Dr. Melendez is a medical simulation fellow at Yale Center for Healthcare Simulation and an instructor of emergency medicine at Yale School of Medicine. He earned his medical degree from Touro University California and completed his residency in emergency medicine at the University of Connecticut.

Dr. Phadnis is a medical simulation fellow at Indiana University. He earned his medical degree at the University of South Florida Morsani College of Medicine and completed his residency in emergency medicine at Florida Atlantic University Schmidt College of Medicine. X: @salphadnis

By Matthew C. Johnson, MD and Luke Duncan, MD
The placement of central venous catheters (CVCs) has significantly advanced over the past few decades with the development of ultrasound guidance and the Seldinger technique. A common indication for CVC placement is poor intravenous (IV) access in hypovolemic or vasodilated patients requiring volume resuscitation, vasoactive medications, or venous access. Studies have linked the diameter of the internal jugular vein to central venous pressure, demonstrating that during episodes
“Research has shown that passive leg raises can increase the diameter of the internal jugular vein, potentially facilitating successful cannulation.”
of vasodilation or hypovolemia, the internal jugular vein often becomes small and easily compressible, which
can make cannulation challenging. To enhance vessel size and improve success rates, patients are typically
positioned in the Trendelenburg position.
Research has shown that passive leg raises can increase the diameter of the internal jugular vein. It follows that an increased vessel size may facilitate cannulation; however, this technique has not been widely explored as an adjunct for placing internal jugular CVCs.
In the case covered in this article, an 85-year-old man with septic shock caused by a perforated sigmoid colon was profoundly hypovolemic and required crystalloid resuscitation and dual vasopressors. Ultrasound revealed that his internal jugular vessels were completely collapsible. Initial attempts to place the catheter were unsuccessful due to vessel collapse. The Trendelenburg position did not adequately dilate the internal jugular vein, as shown in Image 1. However, using a passive leg raise, significant dilation of the internal jugular vein was observed, enabling successful cannulation (Image 2).
Although the leg raise in this case was performed manually, using a hospital bed to elevate the legs could achieve similar results. This technique may prove useful in assisting with CVC placement in patients experiencing hypovolemic or vasodilatory shock with compressible vasculature. Further consideration and study of this approach may be warranted.



Dr. Johnson is a surgical critical care fellow in the Department of Emergency Medicine at Albany Medical Center.
Dr. Duncan is an associate professor of emergency medicine and surgical critical care. He is the assistant program director of the resuscitation and emergency critical care fellowship, medical director of extracorporeal life support services, and division chief of critical care in the Department of Emergency Medicine.


By Corlin Jewell, MD; Dana Loke, MD; Stephannie Acha-Morfaw, MD; and Abraham Alseryani
Early clinical exposure to emergency medicine is uncommon for medical students, who often focus on research during the summer of their first year. These research opportunities frequently lack mentorship and hands-on clinical experience. To address this gap, the University of Wisconsin* developed the Emergency Medicine Summer Immersion Program. This initiative provides rising second-year medical students with practical experience and a comprehensive understanding of emergency medicine. The program offers insights into the operations of emergency departments and prehospital agencies, with an emphasis on recruiting students from
disadvantaged backgrounds who are interested in serving historically marginalized communities.
A significant lack of representation persists among emergency medicine physicians from underrepresented groups. In 2020, only 28% of clinically active emergency medicine physicians identified as women, 9.2% as Hispanic or Latino, 4.9% as Black or African American, and 0.1% as American Indian or Alaska Native Additionally, a 2022 study of 37,485 medical students revealed that 17% identified as underrepresented in medicine (URiM), and among these, 23.9% were from low-income backgrounds.
The definition of URiM has expanded to include individuals who contribute diverse intellectual and cultural perspectives due to life experiences such as overcoming adversity, financial hardship, or being first-generation college students. Programs like the Summer Immersion Program aim to address these barriers by fostering mentorship, building community, and providing support. These efforts can enhance graduate medical education (GME) placement and contribute to a more diverse emergency medicine workforce.
The program’s inaugural participant, Abraham Alseryani, joined the immersion from May to June 2024.

“This environment provided me with a profound understanding of modern emergency medicine and the critical role of emergency department providers.”
A first-generation college graduate and medical student with a multicultural background spanning Mexico to Jordan, Alseryani exemplifies the program’s mission. Reflecting on his experience, he shared:
“The majority of patients I encountered had complex, highacuity medical issues. Some faced acute crises complicated by chronic conditions, while others sought care in the emergency department due to a lack of alternative options. This environment provided me with a profound understanding of modern emergency medicine and the critical role of emergency department providers.
“The program included handson clinical skill sessions where I learned suturing techniques and the basics of point-of-care cardiac ultrasounds. I also assisted with fracture reductions and casting under the guidance of orthopedics residents and learned to work closely with consultants. These practical skills will be invaluable as
I develop my professional identity as a physician.
“However, the highlight was shadowing various emergency medicine physicians. Observing different approaches to handling difficult situations and delivering bad news offered insights that cannot be taught in a classroom. Despite their varying personalities and methods, all the physicians shared a commitment to treating every patient regardless of socioeconomic status — a principle deeply resonant with me, given my own experiences with inadequate health care access. This dedication has strengthened my resolve to pursue emergency medicine.
“Overall, the program was an invaluable learning opportunity that deepened my passion for the field. I strongly recommend it to students considering emergency medicine. It provides a clear understanding of the specialty and the chance to engage with a community of dedicated healthcare professionals.”

Alseryani aspires to become an emergency medicine physician serving underserved populations. Hopefully, the Summer Immersion Program will continue to attract students like him, enhancing the diversity of the emergency medicine workforce and inspiring future leaders in the field.
*The Emergency Department at the University of Wisconsin-Madison, a Level 1 trauma center, serves adults, pediatric patients, and as a regional burn center. In 2023, it treated more than 70,000 patients.

Dr. Jewell is director of the Medical Student Education Fellowship, partner in longitudinal teacher coaching, and an assistant professor of emergency medicine at the University of Wisconsin School of Medicine and Public Health. She leads the medical student clerkship team for emergency medicine.

Dr. Loke is assistant director of medical student education, quality lead for the Veterans Hospital Emergency Department, and resident education partner in longitudinal teacher coaching. She is also an assistant professor of emergency medicine at the University of Wisconsin School of Medicine and Public Health.

Dr. Acha-Morfaw is assistant director of medical student education, chair of the Equity, Diversity, and Inclusion Committee in the Department of Emergency Medicine, and assistant block leader for acute care at the University of Wisconsin School of Medicine and Public Health. She is also an assistant professor of emergency medicine.

By Jason Rotoli, MD; Luke M. Johnson MD; Richard W. Sapp, MD; and Wendy C. Coates, MD, on behalf of the SAEM Academy for Diversity and Inclusion in Emergency Medicine Accommodations Committee
In the fast-paced environment of the emergency department (ED), effective communication with patients is essential to deliver equitable care. With nearly 1 in 4 Americans having a disability, health care providers must accommodate a wide range of abilities and communication needs. The Americans with Disabilities Act (Titles II and III) requires institutions to provide necessary accommodations for individuals with disabilities.
While some patients may use augmentative and alternative communication (AAC) devices, others may need additional accommodations for full communication access. Similar to foreign language interpretation, relying on family members or companions for communication should be avoided unless they are specifically trained for this purpose, as doing so may unintentionally alter critical information. In emergencies, however, any available means of communication may be necessary.
This article highlights several applications that can enhance communication between emergency providers and patients requiring accommodations. Although many of these tools may be compliant with the Health Insurance Portability and Accountability Act (HIPAA), it is recommended that all communication applications be used on HIPAA-compliant devices to protect patient privacy. The following examples are designed and/or endorsed by individuals with disabilities.
The DHH community encompasses a wide range of identities and communication preferences. For instance, some individuals use American Sign Language (ASL) and identify as culturally Deaf, while others identify as deaf or hard of hearing (HoH) and may rely on a combination of spoken language, written language,
BigText*
Live Transcribe*
Voice4u TTS
lip reading, or sign language. Given these varied preferences, no single communication method works for everyone, and emergency providers should familiarize themselves with multiple options.
For patients who use ASL, a qualified in-person ASL interpreter is generally preferred. When unavailable, virtual
remote interpreting (VRI) may be an alternative, though it has limitations such as reliance on internet speed, screen clarity, and positioning challenges. For those who prefer spoken or written language, several applications can facilitate communication, the following table provides some viable options.
Live Transcription — Turns spoken words into written text on your device with good contrast and the ability to change the size of your font.
Live Transcription —Turns spoken words into written text on your device with the ability to change the size of your font. Apple
Live Transcription — Reads what you type in your choice of naturalsounding voices. The app can read words from a photograph with optical character recognition (ORC) technology. Apple
* Denotes a free application
“Critical materials such as hospital forms, medical records, and discharge instructions are rarely provided in accessible electronic formats that enable the use of adaptive voiceover software.”
Approximately 10% of noninstitutionalized U.S. adults report a speech, language, or voice disability. These individuals face significant health care disparities, including lower access to technology that could address communication barriers. Experts
Voice4u
Proloquo2Go
estimate that 5 million Americans could benefit from AAC to enhance communication.
AAC tools, including picture communication boards, speechgenerating devices, and app-based technologies, can bridge these
gaps. They are particularly useful for individuals with intellectual disabilities (e.g., Down syndrome, Fragile X syndrome), neurodevelopmental disabilities (e.g., autism spectrum disorder), and motor disabilities (e.g., cerebral palsy).
Picture/symbol-based technology to generate verbal communication. Android; Apple
Picture/symbol-based technology to generate verbal communication. Apple
Speak For Yourself * Picture/symbol-based technology to generate verbal communication. Apple
Leeloo*
Picture/symbol-based technology to generate verbal communication with text-to-speech voice capability. Android; Apple
* Denotes a free application continued on Page 33

continued from Page 31
Navigating the health care system can be particularly challenging for individuals who are blind or have low vision due to numerous provider and institutional barriers. Many health
care providers lack the necessary training and awareness to effectively support patients with visual needs. As a result, patients' ability to read and interpret written documents is often overestimated, and appropriate accommodations are frequently overlooked. Critical materials such as hospital forms, medical records,
Voice Dream Reader
and discharge instructions are rarely provided in accessible electronic formats that enable the use of adaptive voiceover software. The table below outlines readily available textto-speech technologies that can assist in making these written materials accessible to patients with visual needs.
Text-to-speech application with screen reader and continuous text highlighting. Apple
Siri* Integrated iPhone text-to-speech application and screen reader technology. Apple
TalkBack* Integrated android text-to-speech application and screen reader technology. Android
Seeing AI*
Speech-to-text and screen reader technology. Apple
* Denotes a free application
Ensuring communication accessibility not only improves bidirectional information exchange, but also fosters inclusion, promotes patient autonomy, and empowers individuals with disabilities. By incorporating these applications into their practice, emergency medicine providers can take meaningful steps toward delivering equitable health care to all patients.
Disclaimer: The applications mentioned in this article are not officially endorsed by the Society for Academic Emergency Medicine (SAEM). The opinions expressed are those of the authors and do not necessarily reflect the views of the SAEM Academy for Diversity and Inclusion in Emergency Medicine (ADIEM) as a whole. This list is not intended to be comprehensive or exhaustive. Furthermore, the authors have no financial affiliations with any of the recommended applications.
“Approximately 10% of noninstitutionalized U.S. adults report a speech, language, or voice disability, yet 5 million Americans could benefit from augmentative and alternative communication (AAC) tools to enhance communication.”

Dr. Rotoli is an attending emergency physician and associate professor of emergency medicine at the University of Rochester Medical Center. He is the associate emergency medicine residency program director and directs the Deaf Health Pathways humanities elective at the University of Rochester School of Medicine and Dentistry. His research focuses on health disparities among marginalized populations, particularly Deaf American Sign Language users. He is fluent in ASL and works with Partners in Deaf Health, a nonprofit organization promoting awareness of the health care needs of culturally Deaf individuals.



Dr. Sapp is a fourth-year resident in the Harvard Affiliated Emergency Medicine Residency who is passionate about improving health care for individuals with disabilities through medical education and research on health care disparities.
Dr. Coates is an education scientist who advocates for improved access and quality of care for individuals with disabilities. She is the immediate past president for the Society for Academic Emergency Medicine.
Dr. Johnson is an emergency physician on the medical staffs at Geneva General Hospital and Soldiers and Sailors Memorial Hospital.

By Stefanie Sebok-Syer, PhD; Jean Reyes, MBA, MSN, RN; Andrew Stromberg, MD; Cathy Castillo; Julie Craven; Natasha Humphries, MBA; Brent Portman; Ting Pun, PhD; and Saumya Sao
Emergency Medicine (EM) physicians specialize in providing care for unscheduled and undifferentiated patients of all ages. The emergency department (ED) is often seen as the U.S. health care system’s safety net — “the one place in the U.S. health care system where care is guaranteed, and for some patients, emergency care is the only medical treatment they receive.” Central to this role of advocating for patients,
is understanding the needs of communities and society. Patient and Family Advisory Councils (PFACs) offer an effective way to gather input directly from the sources, i.e., patients, families, and caregivers.
PFACs are groups of patients and family members who meet regularly — typically monthly — to integrate the voices of patients, their loved ones, and caregivers, into hospital operations in ways that inform and
improve patient care. Established in the 1980’s, PFACs traditionally focus on health care policy, design, and implementation aspects. However, there may be missed opportunities in leveraging PFACs to support EM education and research.
An example of how supporting and embracing PFACs can lead to strong and sustained partnerships comes from Stanford Health Care (SHC) in Palo Alto, California. In 2016, SHC established an
“Patient and Family Advisory Councils offer an effective way to gather input directly from the sources, i.e., patients, families, and caregivers.”
Emergency Department (ED) PFAC aimed at providing insights and feedback to improve the ED patient experience. In the past year, the SHC ED PFAC worked to make the MyHealth app more user-friendly, helping patients access protected health information, communicate with their health care team, and schedule appointments.
In addition to the more conventional work of a PFAC, such as providing feedback on a new Hospital-at-Home Program, the ED PFAC has also supported EM education initiatives and advanced research projects. For example, the ED PFAC supported the refinement of EM’s specialtywide entrustable professional activities (EPAs). Involving the ED PFAC in this process allowed educators to more precisely define the competencies needed for resident physicians. Their feedback helped clarify language to ensure that competencies were clearly communicated to faculty, allied health professionals, and patients. For example, the EPA “Manage patients in the face of clinical or diagnostic uncertainty” was revised, based on patient feedback, to “Manage clinical or diagnostic uncertainty when caring for patients,” emphasizing the collaborative nature of the physician-patient relationship.
From a research perspective, the SHC ED PFAC has played a key role in supporting the 2023 Society for Academic Emergency Medicine’s Consensus Conference on Precision Emergency Medicine
Members of the SHC ED PFAC regularly contribute to EM research in several ways: 1) reviewing grants for the Patient-Centered Outcomes Research Institute (PCORI), 2) assisting with recruiting participants for data collection, 3) volunteering to participate in studies when eligible, and 4) sharing research findings with the broader ED patient community. This year, the ED PFAC developed its own research agenda and is collaborating with Stanford University researchers and SHC staff to design and conduct studies on topics patients and families identify as important. For example, they are exploring issues such as diversity, equity, and inclusion in clinical operations data, as well as examining geriatric patients’ views on virtual medical visits.
A recent and significant milestone for the SHC ED PFAC was the creation of the monthly Orchid Award, an initiative aimed at recognizing ED physicians, allied health professionals, and staff for exceptional patient-centered care. This award acknowledges the hard work and dedication of ED staff, emphasizing that patients and families notice the efforts made to provide the best care possible.
As demonstrated through the examples from the SHC ED PFAC, involving patients in the process and allowing them to contribute to advancing academic Emergency Medicine through education and research strengthens our ability to fulfill the mission of emergency care


Dr. Sebok-Syer is an assistant professor in the department of emergency medicine at Stanford University and an EM faculty representative on the Stanford Health Care emergency department patient and family advisory council.
Jean Reyes is an emergency services nurse manager at Stanford Health Care and the nursing representative on the Stanford Health Care emergency department patient and family advisory council. She has been recognized as a leader in elevating patient care standards for organizational efficiency and amplifying patient and family voices in ED decision-making processes.

Dr. Stromberg is a clinical instructor in the department of emergency medicine at Stanford University and an EM faculty representative on the Stanford Health Care emergency department patient and family advisory council. He is currently in the health care administration fellowship at Stanford and holds an MBA from UC Berkeley Haas.

Cathy Castillo is chair of the Stanford Health Care emergency department patient and family advisory council and a founding member. She has been a caregiver for relatives with myelodysplastic syndrome, stroke, traumatic brain injury, Asperger syndrome, and joint replacement, among other conditions.




Julie Craven is a founding member of the Stanford Health Care emergency department patient and family advisory council. She is a patient, caregiver, liver transplant recipient, and cancer survivor.
Natasha Humphries is a member of the Stanford Health Care emergency department patient and family advisory council, both as a caregiver and patient of Stanford Health Care. She lives in Silicon Valley and has worked for Fortune 100 companies in global business operations.
Brent Portman is a member of both the Stanford Health Care emergency department patient and family advisory council and the SHC disabilities PFAC. He is a Stanford Health Care patient and routinely advocates for initiatives that optimize patient care.
Dr. Pun is a member of the Stanford Health Care emergency department patient and family advisory council and a Patient-Centered Outcomes Research Institute (PCORI) ambassador. He is also a member of the West Health Collaborative for Telehealth and Aging and the Center of Excellence for Telehealth and Aging.

Saumya Sao is a first-year medical student at Stanford School of Medicine.

By Matthew Tews, DO; Navdeep Sekhon, MD; and Doug Franzen, MD, on behalf of the SAEM Clerkship Directors in Emergency Medicine academy
Albert Einstein once said, “Education is not the learning of facts, but the training of the mind to think.”
Medical education is increasingly overwhelmed by an expanding body of facts that grow exponentially over time. While knowledge is essential, the core skill in medicine lies in the ability to think critically about patient care. Emergency medicine (EM) teaches learners how to approach the undifferentiated ill or injured patient, ruling out and managing lifeand limb-threatening emergencies. This foundational skill should be taught to all learners during an EM clerkship, though it represents only the tip of the iceberg for what EM offers in terms of learning and skill development.
The role of EM in medical education is broad, and the structure of the EM clerkship in undergraduate medical education (UME) has evolved significantly over the past few decades. EM clerkships now include a variety of formats, such as the traditional four-week, fourth-year clerkship; third-year clerkships, including integrated selectives and two-week rotations; longitudinal clerkships; and even accelerated clinical curricula, where EM can be integrated at various points. Alongside these structural curricular changes, new curricula and innovative resources have emerged, along with updated competencies, Entrustable Professional Activities, and revisions to core EM educational blueprints
Despite these changes, EM educators have worked diligently to define the educational experience for medical students. They have also created valuable resources for EM clerkship directors and students, especially through the Clerkship Directors in Emergency Medicine (CDEM). Founded in 2008 with the mission of serving as the voice for UME, CDEM became the first academy of the Society for Academic Emergency Medicine (SAEM). Today, CDEM is a community of educators committed to enhancing medical student education within EM and providing resources to standardize the EM clerkship experience across institutions.
As in all areas of the specialty, the development of EM clerkship education builds upon the work of those who came before. Significant contributions have been made to reach the current position, with multiple curricula and educational resources created by CDEM members and implemented in EM clerkships (see Table 1). This body of work has evolved over time, and since 2020, the CDEM curricula and assessments have been managed by the CDEM Curriculum and Assessment Committee (CDEM CAC) to ensure resources remain current and relevant. These materials are available on the SAEM CDEM Curriculum website
With the curricular shifts and updated resources available to learners, there is a growing desire to standardize the curriculum and align assessments with a single core framework for EM clerkships. In response, the CDEM CAC initiated a review to update the EM clerkship curriculum, with approval from the CDEM Executive Committee. In January 2024, a call went out to CDEM members via the SAEM community listserv, and a working group of 17 members from diverse institutions convened to determine the next steps for curricular revisions.
The working group’s focus is to create a single, standardized curriculum outlining the core knowledge, skills, and attitudes required for all students completing a four-week EM rotation. This curriculum will be applicable regardless of the timing within a student’s academic program, the specialty resources available at the institution’s emergency department,
“The goal is to answer the question: What core body of Emergency Medicine knowledge and skills should every graduating medical student possess, regardless of their future specialty?.”
the location of the clerkship, or the student’s intended specialty. In other words, the goal is to answer the question: What core body of emergency medicine knowledge and skills should every graduating medical student possess, regardless of their future specialty?
Over the coming months, the working group will engage with the EM community through surveys, presentations, and discussions at EM conferences. The process will culminate in a virtual consensus conference in Fall 2025, following broad input from EM educators, residents, and students. The final curriculum is expected to be available in early Spring 2026, with plans for ongoing curriculum and assessment management through CDEM.
With this project, CDEM continues its mission to serve as the voice of EM undergraduate medical education. The goal is to provide an updated, standardized four-week core curriculum for every medical student completing an EM clerkship. This curriculum will be linked to highquality content, mapped to existing or new assessments, and include
recommendations for utilizing existing curricula and resources. Additionally, CDEM will provide implementation materials and ongoing support through the CDEM CAC.
This effort builds upon the tremendous work of those who have contributed to the field, and it will continue to grow and evolve through the contributions of current and future CDEM members

Dr. Tews is a professor in the Department of Emergency Medicine at Indiana University School of Medicine and serves as associate dean and campus director for IUSM-West Lafayette. He completed medical school at Des Moines University College of Osteopathic Medicine and his residency at Michigan State University. An active member of CDEM for over 15 years, Dr. Tews has contributed to numerous curricular and assessment initiatives and currently leads the CDEM Curriculum Update Working Group.

Dr. Sekhon is an associate professor and clerkship director at the Baylor College of Medicine's Henry J. N. Taub Department of Emergency Medicine. He completed medical school at the University of California, San Diego, and his residency at East Carolina University. Dr. Sekhon is currently a member-at-large on the CDEM Executive Committee and serves as chair of the Curriculum and Assessment Committee.

Dr. Franzen is an associate professor in the Department of Emergency Medicine at the University of Washington and serves as associate residency director and director of student programs for UW Emergency Medicine. He completed medical school at the University of Michigan and residency at Virginia Commonwealth University Medical Center.

By Cecilia Schowe, PharmD, MS, BCPS and Iram Nasreen, PharmD, on behalf of the SAEM Education Committee and SAEM RAMS


Emergency medicine pharmacists (EMPs) play an essential role in patient care in the fast-paced environment of the emergency department (ED), improving outcomes through effective medication management, patient safety, and teamwork.
This article highlights the daily responsibilities and contributions of two dedicated EMPs: Josh Senn, PharmD, BCPS, BCEMP, at UofL Health in Louisville, Kentucky and Giles Slocum, PharmD, BCCCP, BCEMP, at Rush University Medical Center in Chicago.
The path to becoming an EMP can vary. Dr. Senn earned his Doctor of Pharmacy (PharmD) from Belmont University and completed a postgraduate year one (PGY1) residency
at Norton Healthcare. After five years helping establish an emergency medicine pharmacy program at a community hospital, he joined UofL Health, where he now practices as an EMP and directs the PGY2 EMP Residency Program. Dr. Senn also serves as a faculty member at the University of Louisville School of Medicine.
Dr. Slocum took a slightly different path to emergency medicine pharmacy. After earning a Bachelor of Science in Biology and working as a pharmacy technician for
“Engaging with the SAEM community has opened doors for mentorship, collaboration, and education, shaping my career in ways I never imagined.”
three years, Dr. Slocum earned his PharmD from the University of Iowa. He completed a PGY1 residency at Swedish American and a PGY2 in emergency medicine pharmacy at the University of Rochester. He currently practices at Rush University Medical Center, directs the PGY2 EMP Residency Program, and is an assistant professor at Rush University.
Practice Environment
Dr. Senn works in a Level 1 trauma center and comprehensive stroke and burn center within an academic medical center that sees 65,000 patients annually. His health system, which includes eight hospitals, provides emergency medicine pharmacy services at five of them. Dr. Slocum practices at an academic medical center that serves 75,000 patients annually. His hospital specializes in complex bleeding disorders and disaster preparedness to address the challenges of a major city with frequent mass gatherings. It is also a designated hemophilia treatment center, comprehensive stroke center, and chest pain center.
Medication Management
Effective medication management is central to the responsibilities of EMPs. Dr. Senn ensures medication safety through prospective order verification, managing clinical alerts, and assisting with event reporting and debriefing. He also educates nursing staff and precepts the nurse residency program, allowing new nurses to shadow the EMP. To ensure medication availability, Dr. Senn oversees automated dispensing cabinet (ADC) inventory, minimizes procurement from central pharmacy, and ensures that frequently used medications are readily accessible. PGY2 emergency medicine residents support this effort through a project aimed at optimizing ADC inventory.
Dr. Slocum focuses on optimizing medication builds in the EPIC system, enhancing order sets, and monitoring Pyxis stock. He prevents errors through prospective drug reviews, closed-loop communication, and minimizing verbal orders. Although his contributions are difficult to quantify, Dr. Slocum emphasizes the importance of preventing errors and saving “soft dollars.” He collaborates with pharmacy information technology and Pyxis teams to adjust stock levels, monitor trends, and prioritize critical medications, while also working with procurement teams to manage drug shortages and ensure continuity of care.
Both Dr. Senn and Dr. Slocum are integral to emergency response situations, where timely and accurate medication management is crucial. Dr. Senn is heavily involved in trauma and code resuscitations, where he provides medication recommendations, prepares critical medications such as thrombolytics for acute ischemic strokes, and coordinates the ordering and dosing of clotting factor products like prothrombin complex concentrate (PCC). He also responds to code blues hospital-wide during certain shifts and collaborates with the poison control center for therapy recommendations in toxicological emergencies. His expertise is often called upon in critical situations, answering drug information questions and working closely with attending physicians and residents to make therapeutic decisions.
Dr. Slocum similarly plays a key role in high-stakes situations like resuscitations, rapid sequence intubations, and neurologic emergencies. He ensures the timely and accurate management
of medications during code blues, strokes, and trauma cases, confirming doses, routes, and techniques while providing guidance on drug compatibility and contraindications. Dr. Slocum frequently acts as an extra set of hands, priming lines, setting up pumps, and using closed-loop communication to prevent errors. Every medication is carefully labeled with the drug name, concentration, and patient-specific dose to ensure accuracy. He also ensures that medications are dispensed, charged, and documented correctly, supporting continuity of care. To stay prepared, Dr. Slocum stays current on protocols, participates in simulations, and debriefs after critical events, ensuring that he remains calm and focused in the most critical moments of patient care.
Both Dr. Senn and Dr. Slocum ensure continuity of care after ED discharge. Dr. Senn leads a discharge culture callback program under a collaborative practice agreement, where he has the authority to modify, discontinue, or initiate therapies. He also coordinates discharge kits and counseling for medications such as doxycycline, naloxone, and post-exposure prophylaxis. Similarly, Dr. Slocum oversees the ED culture follow-up process, ensuring that patients receive appropriate postdischarge care and education. Their efforts provide a critical safety net for identifying and addressing any outstanding treatment needs.
Both Dr. Senn and Dr. Slocum are dedicated to educating pharmacy professionals and healthcare teams. Dr. Senn precepts students and
continued on Page 41

from Page 39
residents, supervises pharmacy technicians, and oversees ED pharmacy operations. He regularly lectures emergency medicine medical residents and provides educational resources for nursing staff through MEDucations, which cover key emergency medicine topics.
Dr. Slocum is also heavily involved in mentorship, working with PGY1 and PGY2 pharmacy residents and contributing to medical residents’ education. He leads nursing education initiatives, participates in multidisciplinary meetings, and provides patient discharge counseling. Dr. Slocum views education as a key aspect of fostering collaboration and improving patient outcomes, both within the ED and across the healthcare system.
Both Dr. Senn and Dr. Slocum are integral members of their respective interdisciplinary teams, ensuring continuous support for nearly every aspect of patient care. Dr. Senn provides clinical pharmacy coverage 22 out of 24 hours a day, always ready to assist with medication preparation for procedures like rapid sequence intubation, managing medication for status patients, coordinating with families for anticoagulation information, and even applying C-collars for trauma patients. His approachable demeanor and diverse skill set make him a trusted and invaluable teammate.
Dr. Slocum maintains a constant, reliable presence in the ED, creating a dedicated space for easy access by the team. His availability during both routine and high-pressure moments reinforces his role as a trusted resource. His positive attitude and focus on patient-centered care further strengthen this trust, as does his commitment to improving processes, such as optimizing Pyxis workflows and reviewing order sets, which streamline practice for nurses and providers. Dr. Slocum also values honesty and humility, readily admitting
when he doesn’t have an answer, then quickly finding and sharing the necessary information, reinforcing his reliability and dedication to patient care.
Beyond their work in the ED, Dr. Senn and Dr. Slocum contribute to hospitalwide initiatives. Dr. Senn is involved in key committees, including those focused on sepsis, stroke, mass casualty, opioid stewardship, and Pharmacy and Therapeutics (P&T). He supports emergency medicine pharmacy resident research and quality improvement initiatives and helps with stroke and thrombolytic therapy competencies for pharmacy and nursing staff.
Dr. Slocum plays a key role in shaping hospital protocols, particularly in areas that intersect with infectious diseases, critical care, and solid organ transplant. He supports resident research and contributes to national emergency medicine studies through the Emergency Medicine PHARMacotherapy Research Network (EMPHARM-NET). Nationally, Dr. Senn coordinates continuing education programming for state and national organizations, while Dr. Slocum is an active member of the American College of Clinical Pharmacy (ACCP) and the American Society of HealthSystem Pharmacists (ASHP), serving in previous leadership roles and shaping initiatives that empower EM pharmacists to provide evidencebased care.
Despite the significant contributions of EMPs to patient outcomes and safety, expanding the role remains challenging. Dr. Senn faces difficulty justifying the need for full-time EMP coverage based on cost-savings metrics, particularly when clinical leadership does not fully appreciate the value of EMPs. This lack of recognition often hinders efforts to secure additional personnel and expand services.
Dr. Slocum highlights the growing pharmacist shortage, worsened by
declining enrollment in pharmacy schools. To address this, he emphasizes the importance of recruiting and retaining talent by demonstrating the tangible value of emergency medicine pharmacy and creating sustainable work environments. Another challenge is balancing the broad scope of responsibilities in the fast-paced ED, where pharmacists must maintain expertise in both direct patient care and operational roles to ensure safety and efficiency. Staying current on new medications, understanding their effects, and critically reviewing the expanding body of medical literature are also essential for maintaining evidence-based practice.
Emergency medicine pharmacists are critical members of the health care team, optimizing patient care through their expertise in medication management, safety, and collaboration. As the role continues to evolve, staying connected with the wider health care community will be essential for further advancing the profession. To expand the impact of EMPs, it is crucial to advocate for their contributions, demonstrate their value, and build strong relationships across the health care system. To get involved and expand your impact, consider joining the SAEM Academic Emergency Medicine Pharmacists (AEMP) interest group for valuable networking, education, and professional development opportunities.


Dr. Schowe is a PGY2 emergency medicine pharmacy resident at UofL Health in Louisville, Kentucky. She is an active member of SAEM RAMS and the SAEM AEMP interest group.
X: @cecilia_pharm
Dr. Nasreen is a PGY2 emergency medicine pharmacy resident at Rush University Medical Center in Chicago, Illinois. She is an active member of SAEM RAMS and the SAEM AEMP interest group.
X: @iramnasreen

By Jeremy Simon, MD
Let’s consider a few case vignettes.
1. A 65-year-old male, otherwise healthy and alert, presents to your emergency department (ED) with a forehead laceration sustained from a trip and fall. The bleeding is controlled, but the laceration requires sutures.
2. A 65-year-old male, known to your department for frequent visits due to intoxication, presents to your ED in an obtunded state, likely from alcohol, with a forehead laceration from a witnessed trip and fall. The head CT is normal, the bleeding is controlled, but the laceration requires sutures.
3. A 65-year-old male, known to your department for frequent visits due to intoxication, presents to your ED in an obtunded state, likely from alcohol, with a forehead laceration from a witnessed trip and fall. The head CT is normal, but the laceration is bleeding heavily, with a small pool of blood collecting on the CT table.
Do you need consent before suturing these lacerations? The general (though not entirely accurate) answer is yes. It is illegal to touch someone or perform a procedure, such as inserting a needle or making an incision, without their consent. This is true in the ED just as it is on the street. However, the specific
type of consent required can vary depending on the circumstances.
However, to provide a more specific answer to the cases above, several key concepts must be clarified. Not all consent is the same. The most familiar form of consent is explicit consent, where a patient grants permission to a provider to perform a particular intervention. This permission is usually formalized through a signed consent form. Medical ethics dictates that such consent is valid only if the patient fully understands the risks and benefits involved, meaning that informed consent is required. (This article will not discuss the specifics of obtaining
“It is illegal to touch someone or perform a procedure, such as inserting a needle or making an incision, without their consent.”
consent.) Explicit consent is required for high-risk procedures, surgeries with significant downsides (such as an amputation), or interventions that involve risks, benefits, or processes not immediately obvious (such as certain low-risk surgeries).
Another form of consent is implicit consent. When a patient is told that a nurse needs to draw blood and they extend their arm, they are implicitly indicating their agreement to the procedure, even though they have not formally stated their consent. This type of consent is appropriate for lowrisk, well-understood procedures, such as venipuncture and intramuscular or subcutaneous injections. It is important to note that these interventions are often considered covered by a blanket consent-totreatment form that many EDs have patients sign during registration. While these forms may lead to the assumption of consent, they do not, in and of themselves, authorize the provider to proceed with a procedure like venipuncture.
The final form of consent is presumed consent. In this case, consent is presumed because it is generally expected that most people in similar situations would agree to the intervention. Presumed consent is used in situations where it is impossible to obtain consent directly, often in urgent circumstances. This form of consent applies to many resuscitations and traumatic events, explaining why much emergent care is provided without explicit consent. For example, in the case of a posttraumatic tension pneumothorax, a chest tube is placed without waiting for informed consent because of the urgency of the situation. Similarly, if a patient is in ventricular tachycardia (v-tach) arrest, defibrillation will

proceed without waiting for consent, based on the presumption that most individuals would want their heart restarted in such a situation. However, it’s important to note that an inability to obtain consent is not enough to justify presumed consent. There must also be an urgency to act. Otherwise, the patient's mental status must be evaluated or a surrogate decisionmaker must be contacted.
With these concepts in mind, let’s revisit the cases to provide more specific answers.
In the first case, where an alert patient presents with a minor laceration, explicit consent is required. However, unless your institution’s policy dictates otherwise, it doesn’t need to be formalized through documented informed consent. If the patient understands the situation and does not object, implied consent can be assumed. Suturing is a low risk, widely understood procedure that most people expect when they present with a laceration.
In the second case, with the intoxicated patient who cannot provide consent due to their altered mental status, explicit consent is still needed. However, because the patient
is unable to consent, implied consent cannot be assumed. There is no urgency in this case. We know when the laceration occurred, and we have at least 12, if not 24 hours, to suture it. There is sufficient time to wait for the patient to regain alertness before proceeding with suturing.
The third case is different. Here, the patient is bleeding heavily from the wound, which can happen with forehead and scalp lacerations. Immediate intervention is required, as delay could result in hemorrhagic shock or even exsanguination. In this situation, presumed consent can be applied, based on the assumption that most patients, if they were alert, would agree to suturing to stop the bleeding. Given the emergent nature of the situation, this is a reasonable action under the principle of presumed consent.

Dr.
Simon is a professor of emergency medicine at Columbia University and a faculty associate at the Columbia Center for Clinical Medical Ethics.

By Lucas Oliveira J. e Silva, MD, PhD, on behalf of the SAEM Academy for Geriatric Emergency Medicine
In May 2024, unprecedented flooding in Porto Alegre, Brazil, exposed the vulnerabilities of older adults during natural disasters. As water levels surged past historical records, older residents faced disproportionate risks, highlighting the urgent need for disaster preparedness strategies tailored to their unique needs. The catastrophe displaced thousands and revealed gaps in emergency response systems, particularly in addressing the challenges faced by older adults.
Evacuating elderly residents proved to be one of the most difficult tasks during the crisis. Many were hesitant to leave their
homes, either due to emotional attachment or unawareness of the imminent danger. Others were too frail or medically dependent to be moved easily. In neighborhoods like Cavalhada, rescue teams faced heartbreaking delays navigating flooded streets to reach isolated seniors. This tragedy underscores the importance of creating community-focused evacuation plans that prioritize the mobility and safety of older adults. Simple interventions, such as preregistering seniors for assistance and establishing localized evacuation drills, could significantly improve outcomes in future disasters.
The health care system bore the brunt of the disaster, with emergency department (ED) visits mirroring the ebb and flow of the floodwaters. Initially, access to care declined as infrastructure collapsed and transportation networks failed. Many, especially seniors, delayed seeking care due to physical or logistical barriers. However, as conditions stabilized, EDs experienced a surge in patients, including elderly individuals with untreated injuries, exacerbated chronic illnesses, and mental health concerns. This “tsunami effect” of delayed medical crises is well-documented in disaster medicine but presents unique

“This tragedy underscores the importance of creating community-focused evacuation plans that prioritize the mobility and safety of older adults.”
challenges for older adults, who often have multiple comorbidities and limited resilience.
Months later, the impact on seniors remains evident. Many lost their homes, medications, and essential medical devices, leaving them vulnerable to deteriorating health. Without personal belongings or medical records, their care became more complex, further straining an already overwhelmed health care system. Additionally, the psychological toll of displacement and loss has been profound, with social isolation — an important risk factor for geriatric health decline — exacerbated as displaced seniors struggled to reconnect with their communities. Efforts to provide ongoing support, such as mobile medical units, mental
health services, and social outreach programs, have been crucial but often insufficient.
The flood also highlighted the role of health care professionals in disaster response. Emergency physicians were at the forefront, adapting quickly to the evolving crisis. They managed not only acute injuries but also the longterm consequences of displacement on chronic diseases, such as diabetes and hypertension, which worsened due to the interruption of routine care. This experience underscored the importance of disaster training and preparation for health care providers, particularly in areas prone to natural disasters.
This flood demonstrated that, in times of disaster, older adults are often the most affected but least
prepared. Proactive measures, such as community-driven risk assessments, preemptive evacuation planning, and robust social support networks, are essential to protecting this vulnerable population in future emergencies. Policymakers and community leaders must collaborate to create systems that address the unique challenges of aging populations during crises, ensuring that no one is left behind.

Silva is an adjunct professor of emergency medicine in the department of emergency medicine at Hospital de Clínicas de Porto Alegre, Universidade Federal do Rio Grande do Sul, Porto Alegre, RS, Brazil.

By Xochitl Olivares, MSHA and Arthi Kozhumam, MScGH
Global Health Fellowships are diverse and vary across institutions, offering opportunities in areas such as disaster medicine, policy, medical education, and more. This variation makes it essential to research several programs to find one that aligns with your passions. It is important to remember that the goal of global health is not to "save" a community but learn and to exchange knowledge and skills in a culturally sensitive manner.
Most programs participate in a match system similar to residency. Applications can generally be submitted through the SAEM Global EM Fellowship portal. In addition to submitting an application, most
programs also require a letter of interest and a curriculum vitae (CV) sent directly to the fellowship director. Each program has its own specific requirements and deadlines, but clinical competence, research experience, an understanding of collaborative work, and humility will strengthen your application.
Dr. Jane Yee, medical director of the Emergency Medicine (EM) Global


Health Fellowship at the University of Utah, was interviewed about the program. Dr. Alex Gallaer, a current chief resident and incoming global health fellow at the University of Utah, also shared his perspective on his interest in the fellowship. Both emphasized the importance of being honest about the origin of one's interest in global health and longterm career goals, whether focused locally or globally.
EM Global Health Fellowship at the University of Utah
According to Dr. Gallaer, emergency medicine (EM) global health fellowships are “very heterogeneous,” with programs offering unique opportunities and varying lengths
“Global health is not to 'save' a community but learn and exchange knowledge and skills in a culturally sensitive manner.”
of time abroad. Utah’s global health fellowship emphasizes teaching EM education and skills while also contributing to the development of sustainable systems to improve health care abroad. Both Dr. Yee and Dr. Gallaer agree that the skills learned abroad are highly transferable to working with residents at home.
While Utah’s global health fellows work on projects in locations such as Peru, India, and the Indian Health Service, the main focus is on delivering EM education in Vietnam. This partnership, which began in 2013 with Cho Ray Hospital and University Medical Center in Ho Chi Minh City, has transitioned from telelectures and in-person conferences to a more formal diploma program, with several classes of graduates. The ultimate goal is to develop a sustainable emergency medicine residency program with the support of local leaders.
Before fieldwork begins, usually for a few weeks in September, the Utah team prepares their teaching curriculum, educates partners about expectations, and coordinates with nominated physicians. On-site, fellows teach through prepared lesson plans and workshops at the national EM/critical care conference. After returning to Salt Lake City, fellows continue teaching online and may travel back as needed later in the year.
Dr. Yee encourages applicants to clearly articulate their interest in global health and recognize that their work will contribute to a larger goal or mission. “You should go into global health to refine your career goals and apply them to different contexts,” she advises. Dr. Gallaer agrees, stressing that applicants should seek programs that allow them the space to explore

Ho Chi Minh City operating bay for emergency room traumas
and develop their interests. He also highlights that having a desire to teach, both locally and internationally, is a valuable trait for a successful fellowship experience.
Both Dr. Yee and Dr. Gallaer emphasize the importance of humility. Global health work can be humbling due to differences in time, space, and cultural practices between the fieldwork site and the fellow’s home base. They recommend that applicants carefully consider the feasibility and ethics of their ideas, seek local input, and demonstrate a willingness to learn. Additionally, they remind applicants that "global health can be local too," especially when addressing domestic health disparities.
While global work is possible without a fellowship, the global EM fellowship is designed for EM physicians who want to integrate global health into their long-term career goals. These fellowships provide invaluable training in international emergency care, creating culturally sensitive, sustainable initiatives, and developing transferable skills in emergency medicine.


Xochitl Olivares is a fourth-year medical student at Universidad Autónoma de Guadalajara. She plans to apply for emergency medicine in the 2026 match. She previously earned a master's in health care administration from Texas Tech University Health Sciences Center and a degree in anthropology from Texas Tech University.

Arthi Kozhumam is a third-year Medical Scientist Training Program (MSTP) student at Northwestern University Feinberg School of Medicine, Chicago.

By Humphry Chisambiro, MD, and Randall Ellis, MD, MPH, MBA, on behalf of the SAEM Global Emergency Medicine Academy
Emergency services are crucial for treating patients with serious but potentially reversible conditions. This care spans from transportation to the hospital to inpatient care for those in critical states. A health system’s readiness to respond to emergencies is a crucial indicator of its effectiveness. Emergency care involves the simultaneous stabilization, diagnosis, and treatment of undifferentiated patients. Key components of this care include:
• Recognizing emergencies and critical illnesses through a triage system, monitoring, and early warning scores.
• Stabilizing the patient with lifesaving essential and emergency care.
• Diagnosing emergency and critical conditions through appropriate evaluation, testing, and reassessment.
• Treating emergency and critical illnesses based on differential and definitive diagnoses.
• Determining the appropriate location for ongoing care, which may involve referral to a higher level of care, admission to a shortstay unit, surgery, an inpatient ward, a High Dependency Unit, Intensive Care Unit, or discharge to community-level care.
Malawi, a landlocked country in sub-Saharan Africa, is experiencing a rise in conditions that require emergency services. Road traffic collisions have become a major
concern, with particularly high mortality rates among pedestrians and bicyclists. The overall mortality incidence from road traffic injuries in Malawi is estimated at between 23.5 to 29.8 per 100,000 personyears based on data from 2020. Additionally, from 2010 to 2020, an average of 180,000 to 225,000 disability-adjusted life years (DALYs) were lost annually in a population averaging 1,364 million.
Noncommunicable diseases (NCDs) also contribute significantly to Malawi’s emergency disease burden. NCDs are now the second leading cause of adult deaths after HIV/AIDS, and account for 16% of all deaths (17% in males and 14% in

“Noncommunicable diseases are now the second leading cause of adult deaths in Malawi, accounting for 16% of all deaths, and hypertension prevalence stands at a notably high 32.9%.”
females). Hypertension prevalence among adults in Malawi is notably high at 32.9%, surpassing rates observed in many other countries in the region. Furthermore, the prevalence of ischemic heart disease and stroke stands at 6.5%, with rates of 4.4% in men and 8.4% in women
Malawi is also prone to natural disasters, particularly flooding. The most recent disaster, Cyclone Freddy, resulted in over 1,000 deaths and more than 2,000 injuries. The high number of casualties was partly due to households built on hillsides and in mudslide-prone areas
Malawi has a three-tier health care system comprising primary, secondary, and tertiary levels. The Ministry of Health assigns clinical staff to various facility types as follows:
Primary
- Village health posts
- Outreach clinics
- Health centers
- Community hospitals
Secondary - District hospitals
Tertiary - Central hospitals
The first point of contact for a patient in Malawi is typically through government health centers, Christian Health Association of Malawi (CHAM) facilities, or private clinics. In the case of an emergency, guardians or well-wishers need to arrange private transport to the nearest health facility. Ambulances are available but are primarily used for interfacility transfers. The absence of a
- Health surveillance assistants (now disease control surveillance assistants)
- Medical assistants, clinical officers, and nursing officers
- Medical officers, clinical officers, and nursing officers
- Medical specialists, medical officers, clinical officers, and nursing officers
nationwide ambulance service means that in the event of an accident, injury, or trauma, bystanders must provide initial first aid and transport the patient to the nearest health facility.
The level of support and care patients receive depends on the facility they visit, often constrained
continued on Page 51
“By creating professional organizations that prioritize data locally tailored interventions, Malawi can strengthen its emergency reduce morbidity and mortality from the increasing burden

collection, research, and emergency care system and of emergency conditions.”
continued from Page 49
by the availability of equipment and resources. Lower-level care, such as that provided by health surveillance assistants, is typically inadequate due to limited clinical training and lack of resources. A 2020 survey found that, despite the expertise available in higher-level care, necessary resources are often lacking. Another study showed that the absence of standardized protocols for emergency and critical care in these facilities impedes service delivery.
In 2015, the World Bank supported an experimental Emergency Medical Services (EMS) pilot program in Malawi. This initiative aimed to improve emergency patient transport, particularly along the M1 road, a major highway running through the northern and southern regions. The pilot project focused on enhancing emergency response capabilities and reducing mortality rates from road accidents in the targeted area. An impact evaluation of the EMS pilot has not yet been published.
Efforts to improve emergency medicine in Malawi have been ongoing. Kamuzu University of Health Sciences introduced an emergency medicine specialist training program in 2021, which is the only such program in the country. The four-year Master of Medicine (MMED) program currently has four Malawian registrars enrolled. The program recruits new registrars annually, but the number of applicants has decreased due to a lack of available scholarships.
The MMED curriculum includes clinical training, such as Advanced Cardiac Life Support and Basic Life Support, as well as research and teaching activities with undergraduate students. The goal is to train specialists who will provide, teach, and monitor emergency care delivery in Malawi, thus improving the emergency care landscape. Currently, there are four emergency medicine specialists in Malawi, with three serving on the Kamuzu University of Health Sciences faculty to train and supervise postgraduate students.
Additionally, using the World Health Organization’s (WHO) Basic Emergency Care guidelines, some districts have conducted training sessions for nurses, clinical officers, and other health workers. These sessions aim to enhance the capacity for emergency care delivery by providing these health care providers with the basic knowledge needed to initiate essential interventions when patients present at their facilities.
Malawi has seen an increase in health care budgetary allocation, rising from 36.2% in the 2022/23 budget to 41.4% in the 2024/25 budget. However, these funds are primarily directed toward disease programs such as malaria, HIV/AIDS, and tuberculosis, rather than towards a comprehensive emergency system. Improving the emergency care systems could potentially improve the outcomes of these disease programs, as they would share staff and resources.
In 2021, the Ministry of Health, with support from nongovernmental stakeholders, released Emergency & Critical Care Strategy: Framework for Implementing Emergency & Critical Care Services in Malawi 2021-2031. This comprehensive strategy outlines the goals and actions required to implement and improve emergency and critical care services in Malawi. Capacity building for health care staff in emergency care is identified as a critical goal to ensure high standards of patient care. Resource mobilization through advocacy for parliamentary budget allocations or nongovernmental organizations
is also emphasized as essential for advancing this goal.
One potential initiative is to establish a professional organization dedicated to advocating for various aspects of emergency medicine in Malawi. Developing a robust emergency medical service in a resource-limited setting such as Malawi requires careful planning and consideration of available resources. Interventions must be tailored to local constraints while ensuring that patient outcomes are not compromised. These interventions should be thoroughly researched and standardized to maintain high-quality care.
Data collection and research play a critical role in addressing health care challenges in low-income countries. Research can inform the development and refinement of improvised interventions and provide essential insights into the burden of emergency conditions. This data is necessary to guide the effective allocation of resources — whether human, financial, or material — ensuring that limited resources are used in the most effective manner.
By creating professional organizations that prioritize data collection, research, and locally tailored interventions, Malawi can strengthen its emergency care system. These efforts can help reduce morbidity and mortality from the increasing burden of emergency conditions.


Dr. Chisambiro is a third-year emergency medicine resident at Kamuzu University of Health Sciences in Malawi. He currently practices at Queen Elizabeth Central Hospital in Blantyre, located in southern Malawi.
Dr. Ellis is associate director of emergency medicine programs with Seed Global Health and a part-time lecturer at Mbarara University of Science and Technology in Uganda.

By Kyle Bernard, MD, MHSM; Rohit Mukherjee; Arwen Declan, MD, PhD; Brian Milman, MD; and Donald Wright, MD, MHS
on behalf of the SAEM Informatics, Data Science, and Artificial Intelligence Interest Group
An Introduction to Epic Cosmos for Research
For decades, and particularly since the Health Information Technology for Economic and Clinical Health Act (HITECH) of 2009, health systems have invested heavily in Electronic Health Records (EHRs). Digitized health records offer easier data access with associated opportunities for quality improvement and research initiatives. Health systems can share data and collaborate on such initiatives, however, data sharing is often hampered by regulatory, privacy, and technological
barriers. These challenges can be addressed with collaborative, systematic approaches that develop databases shared across systems. This article focuses on the Cosmos database and its applications in research.
What is Cosmos?
Cosmos is a vendor-mediated database created and managed by Epic Systems in Verona, Wisconsin. It relies on the voluntary submission of patient information from Epic customers. Currently, the database contains over 275 million patients, 13.5 billion encounters, 35,000
clinics, and 1,500 hospitals. The Cosmos database is described well in a 2021 overview article
Participation in Cosmos requires organizations to follow Epic’s Cosmos guidelines and organize their data using a standardized framework, known as a data ontology. Once standardized, deidentified patient information is sent to Epic servers.
Organizations joining Cosmos submit their historical data upon enrollment and continue to upload new data regularly. This process uses Epic’s CareEverywhere (CE)

“Cosmos contains over 275 million patients, 13.5 billion encounters, and data from 35,000 clinics and 1,500 hospitals, making it a powerful resource for population-level analyses.”
infrastructure as a vendor-specific health information exchange (HIE) to share data across health systems. Patient records are matched across systems using unique CE identifiers as de-identified tokens, creating a unified record for each patient. Epic regularly monitors the data for completeness and accuracy.
How Does Cosmos Protect Individual Privacy?
Cosmos is designed for populationlevel analyses and is classified as a limited database under the Health Insurance Portability and Accountability Act (HIPAA). To maintain de-identification, the system prevents results based on fewer than 10 individuals. Local institutional
review board (IRB) policies should be followed, with many IRBs categorizing Cosmos research as not involving human subjects. Some IRBs provide blanket approval for Cosmos-based research.
Cosmos contains a vast array of discrete, or structured, data points per patient. It excludes unstructured data, such as free text, and nonstandardized variables like the HEART score. The database includes information from inpatient, outpatient, and emergency department visits, including lab values, medications, diagnoses, imaging rates, procedure codes, vital signs, and social determinants of health. Emergency
department metrics, such as length of stay and time to provider, are also available.
As the largest EHR vendor in the United States, Epic’s Cosmos database is broadly representative of the U.S. population. However, it only includes patients who receive care at Epic customer sites, potentially introducing market-related biases. At present, the database also includes two non-U.S. Epic customers.
Cosmos supports various retrospective study designs, including
continued on Page 55
“Researchers can explore epidemiological populations, leveraging Cosmos' massive external validity and detect true effects

cohort, cross-sectional, and casecontrol methodologies. Researchers can explore epidemiological questions across large populations with relative ease. Previous studies using publicly available “big data” datasets like Surveillance, Epidemiology, and End Results (SEER), National Health and Nutrition Examination Survey (NHANES), The Cancer Genome Atlas (TCGA), and Medical Information Mart for Intensive Care (MIMIC), demonstrate the potential of such retrospective designs. Such retrospective designs can inform clinical risk algorithms, support clinical decision making, and compare the effectiveness of interventions.
Cosmos has also been utilized to assess the effectiveness of the vaccine JYNEOS for Monkeypox and to examine links between SARS-CoV-2 infection and Type 1 Diabetes
Data mining can be used to discover patterns, trends, and insights from large datasets such as Cosmos by leveraging statistical, mathematical, and computational techniques. The massive population available in Cosmos can support studies’ statistical power. The associated large sample sizes also increase the likelihood of detecting true effects of interventions, diversifying populations by demographics to improve external validity, controlling for confounding factors, capturing longitudinal data over time using temporal queries, and employing natural language processing and machine learning models to stratify data and perform comprehensive analysis to reflect real world settings.
Cosmos, like any research tool, has limitations. Population bias may arise from Epic’s market penetration, which is strongest in urban and academic settings. For example, data from the Veterans Administration is not included, and rural healthcare centers may be underrepresented due to lower EHR adoption rates.
The database’s regular updates can introduce inconsistencies in query results. Cosmos typically updates every few weeks and patient populations may change with each update, thus, data queries run before and after a data update may reflect different populations with different statistical descriptions. Researchers may need to adjust reporting strategies or focus on proportional analyses.
Additionally, local resources may affect a researcher’s ability to use Cosmos to address complex questions or perform advanced analyses. Investigations that cannot be answered using Cosmos’ typical web-based query interface will require the analytical toolset and SQL familiarity; if an institution cannot provide these personnel, then its researchers may be unable to address these more complex questions.
Using Cosmos requires researchers to grapple with the typical challenges of using large data sets, such as dimensional heterogeneity, irregularity, and scarcity. The CE identifier, while generally reliable as a HIPAAcompliant token for matching patients across databases, it is not flawless and may lead to duplicate records for some patients.
and sequential logic, and the interface includes graphing functions and spreadsheet exports. Cosmos also offers an analytical toolset for more advanced statistical modeling. Access to the analytical toolset requires additional training, and optimal use may require familiarity with writing SQL queries; R and Python access are also included.
Researchers interested in using Cosmos should confirm their organization’s membership on the Cosmos website. Membership is typically managed by information technology services or the chief medical information officer’s team. Additional training resources are available on Epic’s UserWeb. Collaborative efforts with local clinical informatics teams can further enhance research outcomes



Dr. Bernard is an assistant professor of emergency medicine and provider informaticist at the Medical College of Wisconsin.
Rohit Mukherjee is a medical student at Rutgers Robert Wood Johnson Medical School and a Fulbright scholar.
Dr. Declan is the assistant research director at Prisma Health Upstate and a clinical assistant professor at the University of South Carolina School of Medicine - Greenville and Clemson University.

Dr. Milman is an assistant professor and residency research director in the Department of Emergency Medicine at UT Southwestern.
Dr. Wright is a fellow in the Yale-New Haven HospitalVeterans Administration Clinical Informatics Fellowship and an instructor in the Department of Emergency Medicine at the Yale School of Medicine. epidemiological questions across large massive sample size to improve effects of interventions.”
Clinicians at organizations participating in Cosmos can access the database through a web portal after completing data use agreements and organization-specific Epic training. The user interface is nearly identical to Epic’s SlicerDicer application and allows users to create queries using advanced logic without programming experience. Queries can include basic statistics, trends,


By Wan-Tsu Wendy Chang, MD; Hannah Mishkin, MD, MS; Neha Raukar, MD, MS; Laura Walker, MD, MBA; Wendy Sun, MD, and Lindsay MacConaghy, MD, on behalf of the SAEM Academy of Women in Academic Emergency Medicine Leadership Committee
The holiday season often highlights the challenges of balancing personal and professional responsibilities. Whether observing religious, cultural, or personal traditions — or simply managing a busier schedule — this time of year can bring significant stress. From juggling packed schedules and managing finances to maintaining wellness while meeting professional obligations, these pressures can linger into the new year.
A poll by the American Psychological Association, underscores this stress, citing financial strain, time management, and interpersonal demands as
common factors. To help address these challenges, this article (part of a series on AI in Academic Emergency Medicine) explores how large language models (LLMs) can support work-life balance — not only during hectic seasons, but yearround.
One of the simplest ways to integrate LLMs into daily life is by using them to refine search results and organize tasks. Unlike traditional search engines that rely on keyword matching, LLMs excel at interpreting context and conversational queries, delivering more relevant and
personalized results.
To maximize the benefits of LLMs, it’s essential to provide clear instructions in prompts. For example:
• Define the desired output.
• Specify the level of expertise the AI should assume.
• Identify the intended audience.
• Break down complex prompts into manageable steps.
• Outline the preferred format, such as bullet points or tables.
Here are practical ways LLMs can streamline personal time and set the foundation for a more balanced and productive year.
Organizing Schedules and Events
• Post-Holiday Recovery Planning: Use LLMs to balance professional shifts with personal obligations to transition smoothly into the new year.
Example prompt: “Help me organize a weekly schedule with 12-hour shifts, family dinner planning, and one selfcare day.”
Meal Planning and Grocery Lists
• Healthy Start to the Year: Use LLMs to develop meal plans focused on nutrition and convenience.
Example prompt: “Create a healthy meal plan and grocery list for busy professionals that includes high-protein options and minimal prep time.”
Managing Stress and Wellness
• Building New Habits: Use LLMs to design mindfulness practices or fitness routines for the new year.
Example prompt: “Create a weekly plan for relaxation techniques, including mindfulness and 20-minute daily exercise routines.”
Setting and Achieving New Year’s Resolutions
• Goal Planning: Use LLMs to set realistic goals and break them into actionable steps for professional and personal growth.
Example prompt: “Help me create a year-long plan to achieve my New Year’s resolution of professional growth. Suggest monthly educational activities, conferences, or skills to focus on.”
Gift-Giving Assistance
• Thoughtful Appreciation: Use LLMs to generate meaningful gift ideas for colleagues and loved ones.
Example prompt: “What are some meaningful gifts to show appreciation for my team?”
Travel Coordination
• Winter Travel Planning: Use LLMs to plan itineraries for travel or conferences.
Example prompt: “Help me plan a threeday itinerary for a medical conference and include leisure activities.”
Streamlining Tasks
• Delegating and Prioritizing: Use LLMs to set goals and break down larger tasks into manageable pieces.
“Large language models are valuable tools not only during the holiday season but throughout the year, offering support to balance work, wellness, and personal life.”
Example prompt: “Help me prioritize my monthly to-do list for January, including work deadlines and personal goals.”
Budget Management
• Financial Reset: Use LLMs to create a budget to recover from seasonal expenses and prepare for the year ahead.
Example prompt: “Create a budget plan for January that prioritizes savings and essential expenses.”
• Maintaining Connections: Use LLMs to draft thoughtful messages to colleagues and friends reflecting on the past year and future goals.
Example prompt: “Write a professional yet warm new year email for my team.”
Large language models are valuable tools not only during the holiday season but throughout the year. For emergency medicine physicians, these AI-powered “virtual assistants” can alleviate the pressures of professional and personal responsibilities. By integrating LLMs into everyday routines, it’s possible to reclaim time, reduce stress, and focus on what matters most.
As the new year unfolds, consider experimenting with LLMs to help plan schedules, manage finances, and streamline daily tasks. These tools offer a practical way to create balance and make life easier for busy physicians.
This article was reviewed and edited with the assistance of ChatGPT, an AI-powered writing tool, to enhance clarity, flow, and organization.






Dr. Chang is an associate professor of emergency medicine at the University of Maryland. Her professional focus is on medical education and the management of neurologic emergencies.
Dr. Raukar is an associate professor and vice chair for academic advancement and faculty development at Mayo Clinic Rochester.
Dr. Walker is an assistant professor of emergency medicine at Mayo Clinic. She is a leader in emergency medicine and hospital operations, with a focus on health systems, equity, and quality improvement.
Dr. Mishkin is the emergency medicine residency program director at Reading Hospital, Tower Health, in West Reading, Pennsylvania.
Dr. MacConaghy is an assistant professor of emergency medicine at Geisinger Commonwealth School of Medicine and assistant residency program director at Guthrie Robert Packer Hospital in Sayre, Pennsylvania.
Dr. Sun is an assistant medical director of the York Street Campus Emergency Department at Yale – New Haven Health, an administration fellow, and an instructor of emergency medicine at the Yale School of Medicine.

By Jeremy Brown, MD
The National Institutes of Health (NIH) supports a variety of grant mechanisms, including the well-known R01 grant for independent researchers, the K23 mentored grant for junior clinical investigators, and P01 grants that fund multidisciplinary, long-term research programs. However, some grant mechanisms are less widely recognized, such as the R38, which will be discussed in this column.
The NIH comprises 27 Institutes and Centers, each with its own approach to supporting research. Some grant mechanisms are available across all Institutes, while others are supported by only a few. If you are interested in applying for a
grant, contact the relevant Institute and speak to a program officer, who can explain the application process.
Like the K awards, the R38 supports research training and career development, but with a distinct focus. The R38 is an institutional program that offers mentored research during medical residency. Typically, it is awarded to universities, enabling residents to pursue research training that aligns with the mission of the funding NIH Institute. For example, the National Heart, Lung, and Blood Institute (NHLBI) supports a program at the Medical College of Wisconsin, offering two years of dedicated, protected research time for internal medicine residents who wish to become physician-scientists. The
NHLBI also supports an R38 at the University of Iowa’s Department of Internal Medicine. This one-year program supports internal medicine and pediatric residents who want a more short-term immersion in research.
Additionally, the National Institute of Allergy and Infectious Diseases (NIAID) supports The Ohio State University’s Research in Residency Physician Scientist Initiative. This recently funded initiative provides two years of research training in immune-mediated disease, infectious disease, and immunotherapeutics, targeting resident investigators from the Departments of Medicine, Neurology, Pathology, Surgery, and Plastic Surgery.

“The R38 is an institutional program that offers mentored research during medical residency.”
Where does this leave the emergency medicine (EM) community? While current R38 programs may not specifically include emergency medicine residencies, some, like the Stanford Integrated Cardiovascular-Pulmonary Residency Research Training Program, are open to residents from any specialty. EM residents who are interested should inquire at their university to determine whether the program could support them. While scheduling time for research training may be challenging, EM
residency directors may be willing to accommodate residents who have an opportunity to join an R38 program.
Departments of Emergency Medicine should also consider developing and applying for an R38 program. Such a program could target residents from both emergency medicine and other specialties, potentially enhancing the department’s prestige and fostering the next generation of talented, passionate clinical emergency care investigators.

Dr. Brown is the director of the Office of Emergency Care Research (OECR) where he leads efforts to coordinate emergency care research funding opportunities across NIH. Additionally, Jeremy is the primary contact for the NINDS Exploratory and Efficacy FOAs and serves as NIH's representative in government-wide efforts to improve emergency care throughout the country. He is also the medical officer for the SIREN emergency care research network which is supported by both NINDS and NHLBI. Email: Jeremy.brown@nih.gov

By Meta Carroll, MD, on behalf of the SAEM Pediatric Interest Group
Case Scenario
A 12-year-old boy collapses while playing basketball with his friends after school. His 13-year-old friend initiates CPR, and paramedics arrive to find an apneic, unresponsive child in ventricular fibrillation. After successful defibrillation, return of spontaneous circulation occurs, and the child is transported to a community hospital. In the emergency department (ED), the child remains lethargic with sonorous respirations and is intubated. The parents report that the child has Catecholaminergic Polymorphic Ventricular Tachycardia
(CPVT) and had been off his antiarrhythmic medication for months due to the family losing health insurance. A critical care transport team from a tertiary children’s hospital is contacted. Ventricular ectopy is noted on the monitor, and lidocaine is started prior to transport. At the children’s hospital’s cardiac intensive care unit, the child undergoes therapeutic hypothermia. Within 24 hours, he is awake and alert, later undergoing sympathectomy and the insertion of an implantable cardiac defibrillator. The cardiology and social work teams proceed with family
education and discharge planning. Approximately two weeks after the cardiac arrest, the child is fully recovered and ready to return home.
This case highlights the “chain of survival” that leads to an optimal outcome after out-of-hospital arrest. This unbroken chain includes bystander CPR, prehospital provider interventions, ED readiness for resuscitation and post-arrest care, pediatric critical care transport, and definitive care at a tertiary pediatric center.
Now, let’s focus on one vital link in this chain: the community hospital

“More children’s lives are saved in emergency departments ready for ill or injured pediatric patients, with high pediatric readiness reducing in-hospital mortality by up to 76%.”
emergency department. In hospitals with limited pediatric resources, what are the key elements needed for an ED team to be adequately prepared to handle pediatric emergencies?
Each year, approximately 30 million children visit emergency departments, with 80% or more presenting at general hospitals. In 2001, guidelines for optimizing pediatric care in the ED were published by a team representing the American Academy of Pediatrics (AAP) and the American College of Emergency Physicians (ACEP). However, a 2003 study found that only 6% of surveyed EDs had all the recommended pediatric equipment and supplies. A national
steering committee aimed to address these gaps in pediatric care. The first step was the creation of a webbased assessment tool to measure adherence to the pediatric readiness guidelines. The Emergency Medical Services for Children Innovation and Improvement Center (EIIC) is home to the National Pediatric Readiness Project (NPRP), tasked with improving outcomes for children with illness or injury presenting to any emergency department in the United States. The NPRP provides a pediatric readiness toolkit, checklist, and clinical care guidelines, among other resources. A summary of the pediatric readiness checklist is provided in the table.
The assessment tool calculates a weighted Pediatric Readiness Score (wPRS), which ranges from
1 to 100. A score of 100 indicates that an ED meets the recommended guidelines, including having a pediatric champion, staff competencies, a quality improvement program, and pediatric-specific equipment, supplies, medications, policies, protocols, and clinical care guidelines. This score serves as the starting point for any ED leader striving to improve pediatric readiness.
Pediatric readiness scores matter because EDs that are well-prepared for pediatric patients save more children’s lives. In a retrospective study of 983 emergency departments
continued on Page 63

across 11 states, the highest-scoring EDs (wPRS of 88-100) had a 76% lower in-hospital mortality rate for medical conditions compared to the lowest-scoring EDs (wPRS of 0-58). The difference was also significant for traumatic injuries, with a 60% lower inhospital mortality rate in high-scoring EDs. A cross-sectional analysis that examined geographic accessibility to EDs with high pediatric readiness found that while most children could reach an ED within 30 minutes, only half could access one at or above the 90th percentile for pediatric readiness. Although EDs may be geographically close to home, many children may not have access to pediatric-ready EDs, highlighting the need for continued commitment to improving pediatric readiness.
For the patient in this case, several factors in the ED contributed to a positive outcome. These included skilled staff, immediate access to the necessary equipment, medications, and supplies, well-established practice guidelines, effective team communication, and quick access to a tertiary pediatric hospital. After receiving a report from paramedics, ED nurses placed monitors, provided oxygen, obtained vital signs, and established intravenous access. The pediatric emergency physician performed rapid sequence intubation, assisted by a respiratory therapist, with a radiology technician standing by for a bedside x-ray. Pharmacy staff prepared a lidocaine bolus and infusion. Access to a tertiary pediatric hospital was facilitated with a single phone call, mobilizing a pediatric critical care transport team and enabling direct communication with a pediatric cardiologist. The transfer plan and ongoing critical care were discussed with the parents, emphasizing family-centered communication.
After the child’s departure, the work of pediatric readiness continued. The ED team debriefed, restocked
Pediatric Emergency Care Coordinator
Competency of Nurses and Providers
Quality Improvement
ED Policies, Procedures, Protocols
Disaster Preparedness
Clinical Care Guidelines
Interfacility Transfers
Improving Patient Safety
Physician, nurse, or advanced practice provider who serves as “pediatric champion” to manage/oversee processes listed below.
Maintenance of skills and knowledge of pediatric assessment and care for medical and traumatic conditions, medication and equipment usage, critical procedures, disaster readiness, team communication, family-centered care, and more.
Pediatric-specific indicators for data analysis, system improvements, and monitoring of individual and/or team performance.
Pediatric-specific guides for triage, sedation/analgesia, immunization status, consent, social issues, behavioral health issues, restraint, death of a child, DNR orders, caretaker education, discharge planning, and more.
Plan that addresses pediatric-specific needs in a disaster or mass-casualty incident, including drills, medications, equipment, supplies, family reunification, and more.
Evidenced-based guidelines and pathways that provide medical decision-making support contemporaneous to patient care.
Interfacility transfer agreements and guidelines, with criteria for transfer, communication, and process specifics, all prioritizing family-centered care.
Attention to the prevention of error and harm to children in specific areas (e.g. use of kilograms, complete set of vitals, medication dosing, and safety event reporting).
ED Support Services Guidelines for services often required in the care of pediatric patients (e.g. radiology, laboratory medicine, language interpretation, social services, others).
Medications
Equipment and Supplies
High-volume ED supplies
Adapted from the
Analgesics, anesthetics, anticonvulsants, antidotes, antipyretics, antiemetics, antihypertensives, antimicrobials, antipsychotics, sedatives, vasopressors, vaccines, bronchodilators, and neuromuscular blockers.
General equipment (e.g. infant scale, pediatric defibrillator pads) and specialty equipment for vascular access, monitoring, respiratory support, fracture management, pediatric procedural trays/kits, and more.
For EDs with >10K pediatric visits/year: video laryngoscopy, central venous catheters, chest tubes, inotropes, lumbar puncture trays, noninvasive ventilation, and tracheostomy tubes.
Readiness Project checklist.
Adapted from the National Pediatric Readiness Project checklist
all supplies in the resuscitation room, and conducted a quality and process review. The team planned future simulated cases to maintain their skills. Feedback from the transport team helped the ED staff learn about the child’s clinical course and recovery, reinforcing their commitment to pediatric readiness.
The ED clinical setting requires emergency physicians to maintain a comprehensive skill set, which includes managing pediatric respiratory, gastrointestinal, cardiac, infectious, endocrinologic, oncologic, surgical, and trauma-related emergencies. Highest priority is given to procedural skills necessary
for managing pediatric airway compromise, respiratory failure, and circulatory collapse. This expertise goes beyond pediatric advanced life support certification, allowing emergency physicians to provide highquality care for pediatric patients in every clinical encounter.

Dr. Carroll is a clinical assistant professor at Northwestern University Feinberg School of Medicine and a distinguished clinician at Ann & Robert H. Lurie Children's Hospital of Chicago. She also contributes to education, quality improvement, and clinical service at Northwestern Medicine Central DuPage Hospital.

By Hayley Gartner, PharmD, on behalf of the SAEM Academic Emergency Medicine Pharmacists Interest Group
Psilocybin and psilocin are psychoactive compounds found in certain mushrooms, such as Psilocybe cubensis, commonly known as “magic mushrooms” or “shrooms.” These compounds primarily affect serotonin receptors (e.g., 5-HT2A), producing dose-dependent hallucinogenic, dissociative, and euphoric effects similar to those of lysergic acid diethylamide (LSD). Psilocybin and psilocin are classified as Schedule I substances under the Controlled Substances Act of 1970, severely limiting their use and research. However, in recent years, several states (e.g., Oregon) and cities (e.g., Denver, Seattle, Detroit, Minneapolis) have decriminalized psilocybin. Products advertised to contain psilocybin have also become more widely available, sold in forms such as chocolates, gummies, and pre-rolled cones, despite federal restrictions. These products are often sold with minimal regulation in various retail settings, including smoke shops, gas stations, and online stores.
In the past few years, U.S. poison centers have reported a notable increase in exposures to psilocybincontaining products. While psilocybin was traditionally used in religious ceremonies, cultural rituals, and the
occasional Grateful Dead concert, it has recently gained attention in psychiatry as a potential therapeutic agent for conditions such as treatment-resistant depression, anxiety, smoking cessation, and substance use disorder. The rise in exposures may reflect this growing public interest in psilocybin’s potential therapeutic effects, with some individuals seeking selftreatment. However, due to its Schedule I status, clinical data on the safety and efficacy of psilocybin for these conditions remains limited.
Another concern is the variability and lack of transparency in commercially available psilocybin
“Psilocybin and psilocin are psychoactive compounds found in certain mushrooms that primarily affect serotonin receptors, producing hallucinogenic, dissociative, and euphoric effects.”
products. Some products claim to contain psilocybin or “proprietary blends” of psychoactive mushrooms, but ingredient analysis has found that many contain none. Instead, these products may include unregulated substances such as kavalactones, muscimol, and acetylpsilocin. While these substances can produce effects similar to psilocybin, they also carry unique risks. For instance, kavalactones may cause hepatotoxicity, while muscimol, found in Amanita mushrooms, can lead to central nervous system (CNS) depression, seizures, and respiratory complications. Recently, the Centers for Disease Control and Prevention (CDC) and the Food and Drug Administration (FDA) issued a recall for Diamond Shruumz™ brand products, including chocolates, cones, and gummies, after reports of severe adverse effects such as CNS depression, seizures, and respiratory failure. Despite the recall, similar products remain on the market, and previously purchased Diamond Shruumz™ items still pose risks.
Recognizing psilocybin intoxication can be challenging, particularly when the exposure involves a retail product with unknown or contaminated ingredients. Standard toxicology screens do not detect psilocybin or psilocin, so health care providers must rely on clinical presentation and history. The peak effects of psilocybin typically occur 1 to 3 hours after consumption. Common symptoms include mydriasis (seen in more than 90% of cases), confusion, nausea, vomiting, tachycardia, hypertension, euphoria, perceptual distortions, and agitation, which can result in either a “good trip” or a “bad trip.” Minor cases, characterized by gastrointestinal
discomfort or mild CNS depression, are generally managed with supportive care. However, more severe symptoms, such as hallucinations or agitation, may benefit from a lowstimulation environment, such as a dimly lit room with calm, reassuring interactions to reduce distress.
Severe agitation or seizures should be managed with benzodiazepines as the first-line treatment. If seizures persist, escalation to barbiturates or propofol may be necessary. Seizures are more likely to occur with contaminated retail products than with psilocybin-containing mushrooms. In cases of hyperthermia, rapid cooling measures are essential. Pharmacologic treatments, such as risperidone, which has a high affinity for antagonism at 5-HT2A receptors, have been suggested to attenuate symptoms of psilocybin intoxication, though this remains theoretical rather than evidence-based.
Emergency clinicians should stay informed about psilocybin intoxication and the use of commercially available products, as increased accessibility and growing public interest in psilocybin use are likely to lead to more presentations in emergency departments. Despite the recall of certain psilocybin-mimicking products, others remain available, some of which may cause severe and potentially life-threatening effects. Additionally, since the full range of adverse effects is not yet well understood, individuals who have previously purchased psilocybin-like products may still be at risk.
Given the complex clinical presentation and range of possible adverse effects, emergency medicine providers should be prepared for a spectrum of scenarios involving

natural psilocybin and psilocybinmimicking retail products.
Understanding appropriate management strategies — from supportive care in mild cases to pharmacologic intervention in more severe cases — is crucial in addressing this rising trend. Poison centers are available 24/7 at 1-800222-1222 to provide expert guidance on managing psilocybin exposures.
For a comprehensive overview on the identification, symptoms, and treatment of various neurotoxic mushrooms, see the Wilderness Medicine article on page 110 To submit future "Ask the Pharmacist" questions, please use this link.

Dr. Gartner is a clinical toxicology and emergency medicine fellow at the University of Florida Health Jacksonville and the Florida/USVI Poison Information Center Jacksonville. X: @hayleygartner

By Yuliya Pecheny DO, MEd and James Blum, MD, MPP, on behalf of the SAEM Education Committee
When individuals shop at a grocery store, visit a website, or engage in other consumer activities, they generally have a clear idea of the costs involved. They manage their spending accordingly. However, this concept does not always apply to health care, particularly in the emergency department (ED). In many cases, neither patients nor physicians have a clear understanding of the potential costs of an emergency visit, including the prices of labs or imaging that may be ordered. This lack of transparency limits informed decision-making for both parties. Patients struggle to
assess the urgency of their medical condition and consider alternatives such as urgent care or primary care clinics. Emergency medicine providers face challenges in determining whether certain tests or treatments might reduce the overall cost for patients. For instance, could ordering a point-of-care test (POCT) for troponin rather than a lab test lower the total bill? If hospitals provided a standard “menu” of average ED service costs, based on billing data, would it help inform patients, or might it discourage them from seeking necessary care?
With the growing volume of ED visits and rising health care costs, physicians must become more
aware of the financial burden patients face. If health care remains a business, physicians should advocate for better transparency to prevent surprise medical bills and support efforts to make costs more accessible and understandable for patients.
A common question is the average cost of an ED visit. Unfortunately, costs vary widely by state, ranging from the $600s to thousands of dollars. According to the Health Care Cost Institute, the average cost of an ED visit without insurance in 2021 was $2,909. This figure includes triage fees, facility fees, professional

“This lack of transparency limits informed decision-making for both parties. Patients struggle to assess the urgency of their medical condition and consider alternatives such as urgent care or primary care clinics.”
fees, and supplies. The complexity of health care pricing arises from the lack of a “standard” cost and from numerous factors that affect pricing. These include Medicare rates, negotiated insurance rates, individual deductibles, and co-payments. Billing is also based on Current Procedural Terminology (CPT) codes, which reflect symptoms, treatments, and interventions. CPT codes allow for price comparisons across hospitals but obtaining an itemized bill — necessary to make these comparisons — often requires extra time and is sent after the visit, making it less helpful for upfront cost estimation.
Uninsured patients often face additional financial challenges, as they are charged at a premium due to lack of coverage.
Unlike other types of medical care, there is no single payer for ED visits. Medicaid, a federally funded, stateadministered program for low-income and disabled individuals, is currently the largest payer. Private insurance companies, which individuals purchase through their employers, or the Health Insurance Marketplace
established by the Affordable Care Act (ACA), are the second-largest group of payers. Medicare, the federally funded program for individuals over 65, is third. The final group consists of uninsured patients who pay for their visits out of pocket or have uncompensated care. There are also several other smaller groups who have their care paid for through a combination of these options or other programs.
For insured individuals, the amount paid for an ED visit depends on
continued on Page 69
“Medical schools health economics has the same

the specifics of their insurance plan and is divided into direct and indirect costs. The largest indirect cost is the premium, which patients pay regardless of the amount of medical care used. Insurance plans may also include cost-sharing measures, requiring patients to pay part of the cost of their care through co-payments, deductibles, or coinsurance.
In addition to insurance-related costs, patients may be billed directly for services not covered by their insurance. This is known as “balance billing” and has gained attention in recent media and through federal legislation such as the No Surprises Act. This act seeks to protect patients from balance billing when receiving emergency care at an out-of-network facility or when receiving out-ofnetwork services at an in-network facility. The act aims to remove patients from disputes over these charges, requiring physicians and insurance companies to settle directly. Organizations such as the American College of Emergency Physicians (ACEP) are advocating for fair treatment of emergency providers under this legislation.
The advocacy surrounding the No Surprises Act, while complex, emphasizes the need for physicians to understand the economics and public policies that influence how they
are paid. This knowledge is crucial because it affects both patient care and physicians' livelihoods. High health care costs are a financial burden for many Americans, often leading them to avoid care due to concerns about the costs. This results in patients presenting to the emergency department with advanced complications of conditions that could have been treated earlier, at a lower cost. Understanding how patients pay for medical care can help develop solutions at both the clinical and policy levels. Additionally, it’s important to recognize that the services patients pay for include the care provided by emergency physicians. While patients should not be overcharged or burdened, it is also vital that physicians are fairly compensated for their expertise, rather than allowing insurance companies to profit disproportionately.
Medical schools should standardize the education offered on health economics and public policy to ensure that every student has the same basic understanding of how the medical system interacts with the rest of society. In addition, emergency medicine residencies should make sure to provide similar education to residents as part of their didactic plan. While the ACGME currently requires “considerations of value, equity, cost awareness, delivery and payment” to be incorporated into emergency medicine resident education, this should be more specifically refined so that residents all receive similar education and as physicians have a shared understanding of how patients
schools should standardize the education offered on economics and public policy to ensure that every student same basic understanding of how the medical system interacts with the rest of society.”
pay for care and how they as providers will be compensated.
Given the importance of understanding how emergency care is financed, education on health policy and economics should be integrated into medical school and residency education. While many medical schools include some form of health economics, the quality and consistency of this education varies. Medical schools should standardize their approach to health economics and public policy to ensure all students gain a basic understanding of how health care systems interact with society. Similarly, emergency medicine residencies should ensure that similar education is provided. Although the Accreditation Council for Graduate Medical Education (ACGME) requires that resident education include "consideration of value, equity, cost awareness, delivery, and payment," the curriculum should be more precisely structured to ensure that all residents are educated about the economics of emergency care. This includes understanding how patients pay for care and how providers are compensated for their services.
Understanding the complexities of health care payment in the U.S. is a challenging task, but it is crucial for emergency physicians and residents to advocate for a system that better serves patients while fairly compensating those providing emergency care.


Dr. Pecheny is the assistant program director of the medical education and technology fellowship at Prisma Health in Greenville, South Carolina. She is also an assistant professor at the University of South Carolina School of Medicine Greenville.
Dr. Blum is a fourth-year emergency medicine resident at Boston Medical Center.
He graduated from the Icahn School of Medicine and Harvard Kennedy School. Prior to medical school, he worked on Capitol Hill.

By Halle Fitzgerald, MD, and Diana Yan, MD, MEd, on behalf of the SAEM Simulation Academy
This article is adapted from SAEM Simulation Academy Mentor Hour hosted on July 16, 2024. Panelist included four former and current presidents of the SAEM Simulation Academy.
Introduction
Simulation is a rapidly growing field within medical training, particularly in emergency medicine. It has proven to be as effective as, if not more effective than, traditional teaching strategies for health care providers.
Simulation leverages a variety of technologies and methodologies, enabling trainees to work through realistic scenarios and learn from
mistakes in a safe, controlled environment. It integrates essential competencies such as patient care, interpersonal skills, communication, professionalism, practice-based learning, debriefing, leadership, research, and education
Looking ahead, health care systems are likely to adopt simulation-based learning as a standard component of training, much like the airline industry, nuclear power plants, and the military. For the field of simulation to continue its expansion, it is essential to support simulation specialists in advancing their own careers. Insights from a
panel of former and current SAEM Simulation Academy presidents reveal five key strategies for professional growth in this dynamic field.
Participate in conferences and events to discover new opportunities for professional growth. Assess the landscape in your field to identify ways to enhance your skills, strengthen your training, and connect with key individuals who can support your goals. Determine the pathways to achieve your objectives, whether that involves pursuing further
training, joining a committee, or stepping into an open role.
If you take on a new position, proactively identify and mentor someone to fill your current role, ensuring a smooth transition and fostering growth for others. Additionally, recruit junior colleagues to assist with responsibilities and learn to delegate tasks to create mutually beneficial opportunities for advancement.
Key #2: Embrace Opportunities
When relevant opportunities arise, say “yes” — even if you’re unsure whether the role is the right fit or you don’t fully understand what it entails. Don’t let self-doubt hold you back from advancing your career. Step outside your comfort zone by volunteering for roles that may feel unfamiliar or challenging.
Even if a position doesn’t turn out to be the best fit, approach it as a learning experience. Give it time— perhaps a few years—to gain valuable skills, connections, and insights. The experience you gain may unexpectedly benefit your long-term career goals.
Key #3: Discover your Niche Research what areas already exist in your field and identify gaps where new opportunities may lie. Ask informed questions to gain a deeper
panel discussions, or other platforms that play to your abilities.
Key #4: Increase Your Visibility and Impact
Make yourself indispensable by showcasing your work to as many people as possible. The more individuals who engage with and learn from simulation, the more essential and sustainable it becomes, making it easier to grow.
Identify opportunities to integrate simulation into existing spaces and processes. This could involve joining committees like the root cause analysis (RCA) group, learning new protocols, or leveraging challenges — such as power outages or disaster scenarios — as opportunities to demonstrate simulation’s value as part of the solution.
Additionally, invite leaders and decision-makers to observe and participate in simulation activities firsthand. Seeing the work in action can reinforce its importance and foster continued support.
Key #5: Market and Self-Promote
In the field of simulation, education doesn’t always have a clear, tangible return on investment, which can make it harder to market. To overcome this, it’s important to frame your work in a way that tells a compelling story.
technologies. Marketing your efforts effectively means showcasing these broader, impactful elements.
Finally, don’t shy away from selfpromotion. Writing an article about the innovative work happening in your simulation center, or highlighting your accomplishments, can help further the mission and keep simulation alive. Successful individuals often submit their own nominations for awards — be bold and take similar initiatives to spotlight your work and contributions to the field. It's not selfish — it's essential to gain visibility and help your work thrive.


Dr. Fitzgerald is a third-year emergency medicine resident at Mount Sinai Morningside/West.
Dr. Yan is an assistant professor of emergency medicine, pediatrics, and medical education at Icahn School of Medicine at Mount Sinai.


By Jody A. Vogel, MD, MSc, MSW and Nicholas Mohr, MD, MS
On October 8, 2024, the Agency for Healthcare Research and Quality (AHRQ) hosted the “Summit to Address Emergency Department Boarding” (i.e. the Summit) at the U.S. Department of Health and Human Services Headquarters in Washington, D.C. The Summit was organized by AHRQ to bring together national leaders to discuss the impact and potential solutions for hospital boarding in U.S. emergency departments, and the Society for Academic Emergency Medicine (SAEM) had representatives there to talk about the impact of boarding in academic medicine.
This Summit was the culmination of years of advocacy by emergency medicine, public health, and patient advocacy organizations. In 2022, SAEM co-sponsored a letter to
“Boarding worsens patient outcomes, and it has taken a significant toll on the emergency care workforce.”
the White House that argued that emergency department boarding is a U.S. public health crisis that leads to preventable patient harm, physician burnout, and staffing shortages. In 2023, 44 members of Congress signed a call to action to Dr. Xavier Becerra, secretary of the U.S. Department of Health and Human Services, to advocate for the
development of a task force to lead a federal response to the boarding crisis. This Summit was the first step of the federal response to that request.
At the Summit, Dr. Robert Otto Valdez, Director of the Agency for
continued on Page 75




“This community is not a bunch of emergency physicians pounding their fists on the table... but a matrixed number of incentives and structural changes that can get us to a place where we have a health system that we can be proud of." – Dr. Brendan Carr
SPECIAL REPORT
continued from Page 72
Healthcare Research and Quality, kicked off the one-day meeting by telling the story of a U.S. health care delivery system that was broken. He described the goal of the meeting as bringing together experts from diverse backgrounds to propose policy solutions to improve functioning and capacity in U.S. emergency departments. He also introduced attendees from multiple federal agencies, patient representatives, hospital administrators, representatives from other specialty organizations, and emergency medicine professional organizations representing physicians, nurses, trainees, and academic medical centers.
During the meeting, an artist captured the high points of the discussion in real time (Figure 1). Several of the themes that emerged from the discussion included:
• Those who study emergency department boarding widely agree that boarding is caused by bottlenecks in hospital throughput. It is not an emergency department problem—it is a hospital problem, and low-acuity emergency
department patients are not the cause.
• Boarding is not being uniformly measured or tracked, which makes describing the problem and its public health impacts difficult.
• Boarding worsens patient outcomes, and it has taken a significant toll on the emergency care workforce. Boarding also disproportionately affects patients who are already marginalized.
• One of the primary drivers of emergency department boarding is hospital and physician reimbursement strategy. If hospitals are financially incentivized to prioritize certain types of patient problems and healthcare services, boarding in emergency departments will persist. Solutions to improve care for boarding patients in the emergency department and improve utilization of inpatient beds add value, but reimbursement policy is driving the reality of boarding.
• Solutions will require collaboration between policymakers, payers, and the healthcare delivery system.
Attendees participated in five breakout sessions to propose solutions in the following areas: system-wide financial and regulatory enhancements, real-time regional
“Solutions will require collaboration between policymakers, payers, and the healthcare delivery system.”
health system data, measurement and metrics; workforce development, supportive technology, and workforce safety; rural solutions; and behavioral health connections.
Dr. Brendan Carr, emergency physician and chief executive officer of Mount Sinai Health System, led a discussion of many of the themes during his “Conversation with the CEO.”
“This community is not a bunch of emergency physicians pounding their fists on the table,” he said. “These are folks that can see the failed social policy and the chinks in the armor of the healthcare system and can help you find not a magical silver bullet, but a matrixed number of incentives and structural changes that can get us to a place where we have a health system that we can be proud of.”
SAEM will continue to participate in discussions with partners at AHRQ and other collaborators in addressing the emergency department boarding crisis.


Dr. Vogel is an associate professor of emergency medicine and the inaugural vice chair for academic affairs in the department of emergency medicine at Stanford University. She is secretary-treasurer for SAEM.
Dr. Mohr is a professor of emergency medicine, anesthesia critical care, and epidemiology at the University of Iowa Carver College of Medicine. He is the vice chair for research in the department of emergency medicine and a member-at-large on the SAEM Board of Directors.

By Robert W. Seabury, PharmD and Ana Bienvenida, PharmD
The Patient Case
A 42-year-old female was found unresponsive, surrounded by several empty acetaminophen bottles. Naloxone was administered without effect, and she was emergency intubated for airway protection. Post-intubation vital signs were within normal limits, and an arterial blood gas (ABG) revealed a pH of 7.1, a PaCO2 of 27 mmHg, and a PaO2 of 400 mmHg. Laboratory results showed an acetaminophen concentration of 926 mcg/mL, an anion gap of 24 mmol/L, a CO2 of 13 mmol/L, a serum creatinine
(SCr) of 1.9 mg/dL, a lactate of 4.5 mmol/L, alanine aminotransferase (ALT) of 120 units/L, and aspartate aminotransferase (AST) of 141 units/L. N-acetylcysteine (NAC) 150 mg/kg was administered as a one-hour infusion, followed by a 250 mg/kg infusion over 21 hours. Fomepizole 15 mg/kg was given intravenously once, then 10 mg/kg every 12 hours. Despite appropriate antidotal therapy, her clinical status worsened, necessitating multiple vasopressors. Repeat laboratory values showed an acetaminophen concentration of 902 mcg/mL, an
anion gap of 36 mmol/L, a CO2 of 7 mmol/L, an SCr of 2.9 mg/dL, a lactate of 11.3 mmol/L, ALT of 215 units/L, and AST of 223 units/L.
High-Risk Acetaminophen
Poisoning
High-risk acetaminophen poisonings, also known as massive acetaminophen poisonings, are typically defined as acetaminophen ingestions of at least 30 g or acetaminophen concentrations that are at least double the treatment line on the Rumack-Matthew nomogram. Though rare, high-risk poisonings

“High-risk acetaminophen poisonings can present with metabolic acidosis, elevated lactate, and altered mental status within hours of ingestion, potentially leading to death within the first 24 hours.”
differ from other acetaminophen ingestions. Most acetaminophen poisonings have an insidious onset, often presenting with nonspecific symptoms within the first 24 hours. Hepatic injury develops 24 to 36 hours after overdose and peaks at 72 to 120 hours. These poisonings can progress to fulminant hepatic failure, multisystem organ dysfunction, and death. Conversely, high-risk acetaminophen poisonings may present within hours of ingestion with metabolic acidosis, elevated lactate, and altered mental status, and they can be fatal within the first 24 hours. Notably, significant hepatotoxicity may not be present initially.
Mechanisms explaining the early metabolic and lactic acidosis in some high-risk acetaminophen poisonings include NAPQI-induced uncoupling of oxidative phosphorylation and direct acetaminophen-induced mitochondrial toxicity.
NAC is the primary antidote for acetaminophen toxicity and is most effective when started within the first eight hours of acute ingestion. Its effectiveness, however, appears to depend on acetaminophen concentration. Some evidence suggests patients with higher acetaminophen concentrations
may be at an increased risk of treatment failure despite early NAC administration. Theoretical explanations for treatment failure include potential underdosing of NAC, suggesting that higher NAC doses may be required for more severe overdoses. A common higher-dose NAC regimen involves an initial 150 mg/kg infusion over 15 to 60 minutes, followed by a 250 mg/kg infusion over 16 hours. Table 1 compares this higher-dose regimen to the standard intravenous regimen. However, evidence evaluating this protocol is
Traditional 3-dose regimen ("'Prescott Protocol"')
regimen
1 - 150 mg/kg 15-60 minutes Bolus over 15-60 minutes Provides 300 mg/kg in the first 21 hours
2 - 50 mg/kg 4 hours 12.5 mg/kg/hr 3 - 100 mg/kg 16 hours
Table 1. Traditional vs. Higher Dose Intravenous (IV) N-Acetylcysteine (NAC) Dosing Regimen
Fomepizole administered within 6 hours of starting HD?
No need for fomepizole dose at start of HD
Last dose fomepizole administered less than 0.5 hours at end of HD?
Last dose fomepizole administered between 1-3 hours prior to the end of HD?
Last dose fomepizole administered greater than 3 hours prior to end of HD?
continued from Page 77
Administer fomepizole dose at start of HD
Do not administer fomepizole after HD
Administer half-dose fomepizole after HD
Administer full dose fom epizole after HD
limited, and available retrospective data indicate no clear difference or at most, a modest benefit. A consensus statement currently supports the idea that increased NAC doses may be necessary for high-risk acetaminophen poisonings, with consultation from a toxicologist or poison control center recommended.
Fomepizole has recently been proposed as a potential adjunct for treating high-risk acetaminophen overdoses, particularly in combination with NAC. It inhibits the enzyme responsible for converting acetaminophen to its toxic metabolite and also interferes with an enzymatic pathway thought to induce mitochondrial oxidative stress. Fomepizole is administered as a 15 mg/kg intravenous dose once, followed by 10 mg/kg every 12 hours for 48 hours, and subsequently 15 mg/kg intravenously every 12 hours. Though most evidence is based on animal studies or case series/case reports combined with NAC, clinical data on fomepizole’s efficacy in high-risk acetaminophen overdoses is limited. A consensus statement indicates that current evidence does not support a standardized recommendation for its use in acetaminophen poisonings.
Extracorporeal treatments (ECTRs) accelerate the elimination of both endogenous and exogenous toxins through processes like
1 Acetaminophen concentration > 1000 mcg/mL and NAC is NOT administered 1D
2 Altered mental status, metabolic acidosis, elevated lactate
Acetaminophen concentration > 700 mcg/mL & NAC is NOT administered 1D
3 Altered mental status, metabolic acidosis, elevated lactate
Acetaminophen concentration > 900 mcg/mL & NAC IS administered 1D
GRADE system. LOE = Level of evidence. 1D = strong recommendation, very low level of evidence
diffusion, convection, adsorption, and centrifugation. Acetaminophen, with its low molecular weight (151 kDa), small volume of distribution (< 1 L/kg), and low protein-binding (10–30%), is particularly suited for extracorporeal elimination. ECTRs are typically not necessary for most acetaminophen poisonings; however, they may offer benefits in severe, high-risk overdoses by correcting existing acidosis and mitigating mitochondrial dysfunction through removal of acetaminophen. The threshold for initiating ECTR in high-risk acetaminophen poisoning remains unclear. Available evidence largely derives from case reports involving very high acetaminophen concentrations.
The Extracorporeal Treatments in Poisoning (EXTRIP) working group, consisting of content experts in poisonings and/or extracorporeal treatments from specialties including nephrology, toxicology, emergency medicine, pediatrics, and critical care, provides recommendations on extracorporeal elimination in poisoned patients. Table 2 summarizes EXTRIP recommendations for ECTRs in acetaminophen poisonings, which align with recent consensus statement guidelines
EXTRIP recommends intermittent hemodialysis (IHD) as the preferred ECTR for acetaminophen poisonings; other options, such as intermittent hemoperfusion, continuous renal replacement therapy (CRRT), and exchange transfusion in neonates, are alternatives if IHD is unavailable. EXTRIP also advises continuing ECTR until there is sustained clinical improvement.
Both NAC and fomepizole are
dialyzable, requiring dosing adjustments during IHD and CRRT. While NAC is up to 25% removed by CRRT and up to 50% by IHD, EXTRIP recommends increasing NAC doses to compensate for these losses. Specifically, NAC infusion rates should be raised by one-third during CRRT and doubled during IHD. Fomepizole should be administered every four hours during IHD, and some patients may need additional doses before and/or after IHD (Figure 1). During CRRT, fomepizole should be administered every 8 hours.
EXTRIP recommendations serve as a valuable resource for clinicians involved in toxicology, particularly in guiding the use of ECTRs for certain toxicities. The guidelines cover over 20 different poisonings and include indications for extracorporeal treatments, situations where ECTRs are not recommended, the preferred types of treatment, and cessation criteria.
Though extracorporeal treatments are rarely indicated for acetaminophen poisonings, they may be appropriate for certain high-risk overdoses — particularly those with markedly elevated acetaminophen concentrations and severe symptoms such as metabolic acidosis, elevated lactate, and altered mental status. EXTRIP provides guidelines on the use of ECTRs for high-risk acetaminophen poisoning. In such cases, ECTRs should be combined with NAC and possibly fomepizole. Higher NAC doses may be necessary, and both NAC and fomepizole require dosing adjustments during IHD and CRRT. Clinicians should consider consulting a local toxicologist or poison control
center (1-800-222-1222) when planning to use high-dose NAC, fomepizole, or ECTRs for high-risk acetaminophen toxicity.
Given the patient’s rapid deterioration and continued elevated acetaminophen concentration (greater than 900 mcg/mL), the toxicology service recommended renal replacement therapy. Continuous venovenous hemodiafiltration (CVVHDF) was initiated, with NAC and fomepizole doses increased to 16.6 mg/kg/h and 10 mg/kg every 8 hours, respectively. After 32 hours of CVVHDF, her metabolic acidosis resolved, her vasopressors were titrated off, her mental status improved, and acetaminophen concentration dropped from 902 to 53 mcg/mL. ALT and AST levels peaked at 300 and 388 units/mL, respectively. NAC and fomepizole were discontinued after 24 hours once ALT, AST, and acetaminophen levels normalized. The patient was extubated and discharged to the psychiatry service in normal health


Dr. Seabury is an emergency department pharmacist at Upstate University Hospital in Syracuse, New York.
Dr. Bienvenida is an emergency medicine clinical pharmacist at Legacy Emanuel Medical Center in Portland, Oregon. X: @BienvenidaAna

By Hayley Gartner, PharmD and Allyson Greenberg, PharmD, on behalf of the SAEM Toxicology and Addiction Medicine Interest Group and the SAEM Academic Emergency Medicine Pharmacists Interest Group
Background
Toxic alcohols are organic compounds containing one or more hydroxyl groups and are not intended for human consumption. The most clinically relevant toxic alcohols are methanol, ethylene glycol, and isopropanol. Methanol is commonly found in products such as windshield washer fluid, cooking fuel, and carburetor cleaner, and may also be present in illicit moonshine. Ethylene glycol serves as a reagent in industrial settings and is the primary ingredient in antifreeze. Isopropanol is used in disinfectants and as a solvent in both industrial and
laboratory environments. Ingestion is the primary route of exposure for all three toxic alcohols. While inhalation exposure is possible with more volatile alcohols like methanol and isopropanol, it rarely leads to toxicity. In some cases, chronic dermal exposure can also lead to toxic effects.
Toxic alcohols can cause intoxication but generally are not directly toxic, except for isopropanol. The toxic effects of methanol and ethylene glycol arise primarily from their organic acid metabolites. Alcohol
dehydrogenase (ADH) and aldehyde dehydrogenase (ALDH) are the key enzymes involved in metabolizing these substances. ADH initiates the oxidation of toxic alcohols, producing aldehydes (except for acetone from isopropanol). These aldehydes are then further oxidized by ALDH to yield toxic carboxylic acid metabolites: methanol is converted to formic acid, and ethylene glycol is metabolized to oxalic and glycolic acids. ADH plays a crucial role in the formation of these toxic metabolites. Additionally, lactic acidosis may occur due to the effects of methanol and ethylene glycol metabolites.

Ethylene glycol
Methanol
Isopropanol
Inebriation, acute kidney injury, visual disturbances, pulmonary dysfunction, abdominal pain, coma, occasionally Parkinsonian symptoms
Inebriation, abdominal pain, decreased vision with blindness, Parkinson-like features (rare)
Inebriation, depressed sensorium, abdominal pain
Table 1. Summary of Key Clinical & Laboratory Findings
Clinical Presentation and Diagnostic Testing
Toxic alcohols initially induce central nervous system (CNS) depression, which can progress to multi-organ dysfunction. Methanol exposure can lead to visual disturbances and retinal injury. Symptoms typically occur within 6 to 24 hours but may be delayed up to 72 to 96 hours with ethanol co-ingestion. Neurologic complications can develop days to weeks after exposure. Ethylene glycol metabolizes into oxalate crystals, which deposit in the lungs, heart, and kidneys, leading to significant organ dysfunction. Neurologic impairment typically emerges within the first 12
Increased osmolal gap and high anion gap metabolic acidosis, calcium oxalate crystalluria dihydrate (early) and monohydrate (late), hypocalcemia, lactate gap (discrepancy between findings from a point of care analyzer and laboratory test)
Increased osmolal gap and high anion gap metabolic acidosis, increased formate, lactic acidosis with cellular hypoxia, spurious increase in serum creatinine concentration
Increased osmolal gap, acetonemia, ketonuria
“Toxic alcohols initially induce central nervous system depression, progressing to multi-organ dysfunction.”
hours, followed by cardiac and pulmonary complications 12 to 24 hours later, and acute kidney injury between 48 to 72 hours post-exposure. Concurrent organ dysfunction is possible. Ethanol co-ingestion may delay clinical manifestations due to competitive antagonism at alcohol dehydrogenase enzymes.

Isopropanol causes CNS depression, with possible respiratory compromise, cardiovascular collapse, acute pancreatitis, hypotension, and lactic acidosis. Clinically significant serum levels begin above 50 mg/dL, with deep coma observed at concentrations above 150 mg/dL. Acetone, a metabolite, can falsely elevate serum creatinine levels due to interference with laboratory assays. Multiple concentrations may be needed to guide
treatment, including the cessation of hemodialysis.
Methanol and ethylene glycol exposures pose serious health risks, primarily due to their toxic metabolites. Treatment focuses on preventing metabolism, correcting metabolic acidosis, and eliminating the toxins and their metabolites.
The preferred antidotal treatment is fomepizole, which is indicated if the serum methanol or ethylene glycol concentration exceeds 20 mg/dL or if there’s strong suspicion of exposure accompanied by an osmolal gap greater than 10 mOsm/ kg or unexplained metabolic acidosis. Ethanol remains an option when access to fomepizole is limited. Methanol and ethylene glycol concentrations often do not return in a clinically relevant period. Therefore, if there is a high clinical suspicion of toxicity, the patient should be treated with fomepizole or ethanol. Both ethanol and fomepizole inhibit alcohol dehydrogenase, the enzyme that
continued on Page 82
Fomepizole
Ethanol
Folic Acid
Folinic acid (Leucovorin)
Pyridoxine (Vitamin B6)
Thiamine (Vitamin B1)
Competitive inhibitor of ADH, prevents formation of toxic metabolites
Competitive inhibitor of ADH, prevents formation of toxic metabolites
Metabolism of formic acid (formate) to carbon dioxide and water
Active form of folic acid bypassing first pass metabolism
15 mg/kg IVPB
10 mg/kg IVPB every 12 hours x 4 doses (48 hours), then 15 mg/kg every 12 hours (increase in dose is necessary, as fomepizole induces its own metabolism)
Co-factors: Methanol toxicity
50 mg IV
50 mg iV
50 mg every 4-6 hours x 24-48 hours
Administer folic acid maintenance regimen following first dose of folinic acid
Co-factors: Ethylene Glycol toxicity
Cofactor to convert glyoxylate to glycine
Aid conversion of glyoxylate to alphahydroxy-beta-ketoadipate
Table 2. Summary of Antidotal & Adjunctive Therapies
*Administer all three cofactors if ingested substance is unknown
100 mg IV
100 mg IV
Dose adjust for patients requiring hemodialysis (HD); patients require
Concentrations of at least 100 mg/dL should prevent metabolism of toxic alcohols to organic acid
In HD, administer 1 dose prior to and another at completion of HD
Use as initial dose in critically ill patient, metabolic acidosis
50 mg IV every 6 hours x 24-48 hours Glycine is non-toxic
100 mg IV every 8 hours x 24-48 hours
**Magnesium should be replete on an as needed basis, as it is present in ethylene glycol’s metabolism
TOXICOLOGY
continued from Page 81
metabolizes methanol and ethylene glycol into their toxic metabolites. Ethanol was used historically before the development of fomepizole and has several drawbacks, including the need for constant monitoring and the potential for CNS depression, which may require intensive care. A serum ethanol level of 100 mg/dL is typically maintained for efficacy. While fomepizole is preferred due to its safety profile and minimal monitoring requirements, it may be unavailable or costly in some regions, where ethanol (either IV or oral) can be used as an alternative.
Hemodialysis may also be indicated for these patients. Hemodialysis rapidly removes methanol, ethylene glycol, and their toxic metabolites. Specific indications (Table 3) are outlined
Alpha-hydroxy-betaketoadipate is non-toxic
“Methanol and ethylene glycol poisoning are lifethreatening and require prompt diagnosis and treatment to reduce mortality, while isopropanol poses a lower fatality risk.”
by the Extracorporeal Treatments in Poisoning (EXTRIP) workgroup.
Adjunctive therapies including folic acid, pyridoxine, and/or thiamine are recommended to facilitate the conversion of ethylene glycol and methanol into less toxic metabolites. Intravenous bicarbonate can also be used to manage metabolic acidosis and increase the ionization and excretion of formate, a toxic methanol metabolite that can damage the optic nerve.
Isopropanol exposure management differs from ethylene glycol and methanol exposures, in that supportive care is usually sufficient. However, hemodialysis may be necessary if serum isopropanol concentration reaches 500 mg/dL or higher, or if the patient presents with hypotension or lactic acidosis. Alcohol dehydrogenase inhibitors are not recommended, as they slow the elimination of isopropanol.
PLASMA EG CONCENTRATION
• Fomepizole used: Suggested if EG concentration >310mg/dL
• Ethanol used: Recommended if EG concentration >310mg/dL; suggested if EG concentration 124–310mg/dL
• No antidote available: Recommended if EG concentration >62mg/dL
OSMOL GAP when there is evidence of EG exposure
• Fomepizole used: Suggested if osmol gap >50
• Ethanol used: Recommended if osmol gap >50; suggested if osmol gap is 20–50
• No antidote available: Recommend if osmol gap >10
PLASMA GLYCOLATE CONCENTRATION
• Recommended if glycolate concentration >12 mmol/L
• Suggested if glycolate concentration 8–12mmol/L
ANION GAP when evidence of EG exposure
• Recommended if anion gap >27mmol/L
• Suggested if anion gap 23–27mmol/L
CLINICAL INDICATIONS
• Coma: recommended
• Seizures: recommended
• Kidney Impairment:
o In patients with CKD (eGFR <45mL/min/1.73m2): suggested
o Patients with AKI (KDIGO stage 2 or 3): recommended
• Coma
• Seizures
• New vision deficits
• Blood pH ≤7.15
• Persistent metabolic acidosis despite adequate supportive measures and antidotes
• Serum anion gap >24 mmol/L
• Serum methanol concentration >700 mg/L in context of fomepizole therapy
• Serum methanol concentration >600 mg/L in context of ethanol treatment
• Serum methanol concentration >500 mg/L in absence of ADH blocker
• In absence of methanol concentration, osmol gap may be informative
• In context of impaired kidney function
Table 3. Extracorporeal Treatments in Poisoning Workgroup (EXTRIP) Indications for Hemodialysis in Methanol and Ethylene Glycol Toxicity
The Bottom Line
Methanol and ethylene glycol poisoning are life-threatening and require prompt diagnosis and treatment to reduce mortality, while isopropanol poses a lower fatality risk. Diagnosis can be challenging since typical signs, such as high
anion gap metabolic acidosis and increased osmolal gap, may not always be present. High-pressure liquid chromatography is ideal for confirmation, but it is often inaccessible, highlighting the need for rapid diagnostic tools. Treatment generally includes alcohol
1. Initial Presentation: Toxic alcohol poisoning may first appear as inebriation. However, toxicity typically occurs later as the alcohol is metabolized into organic acid anions, leading to metabolic acidosis and organ damage
2. Delayed Onset of Toxicity: Because the toxic effects are due to metabolized byproducts, there is often a delay between ingestion and the appearance of clinical symptoms
3. Diagnostic Indicators: Before serum toxic alcohol levels are available, the serum anion gap and osmolal gap help guide treatment but do not rule out toxicity, especially if patient history is concerning
4. Treatment: Therapy includes inhibiting alcohol dehydrogenase (ADH) with fomepizole or ethanol. Adjunctive therapies may include bicarbonate, along with folic or folinic acid, pyridoxine, and thiamine
5. Definitive Therapy with Hemodialysis: For critically ill patients, hemodialysis is the most effective treatment. It clears both the alcohol and its toxic byproducts while helping to correct metabolic acidosis and electrolyte disturbances
dehydrogenase inhibitors and hemodialysis, although availability and protocols may differ.
Poison centers are available 24/7 at 1-800-222-1222 to offer expert guidance on managing toxic alcohol exposures. It is advisable to consult a local toxicologist to determine the most effective treatment. Regularly connecting with your local poison center can help ensure that your institution’s protocols align with the latest research and best practices.


Dr. Gartner is a clinical toxicology and emergency medicine fellow at the University of Florida Health Jacksonville and Florida/USVI Poison Information Center Jacksonville. X @hayleygartner
Dr. Greenberg is a clinical pharmacy specialist in emergency medicine at the University of Chicago Medicine.

By Tori Ehrhardt, MD
Introduction
Provisional data released this year by the Centers for Disease Control and Prevention (CDC) National Center for Health Statistics indicate a decline in opioid overdose deaths from 2023 to 2024. While this trend may offer cautious optimism, it is essential to interpret these figures within the proper context. Opioid overdose remains a leading cause of death in the U.S., and barriers to primary care frequently lead individuals with opioid use disorder (OUD) to seek care in the emergency department (ED). These visits may be the result of opioid overdose, substance use-related complications such as
withdrawal, or unrelated medical or psychiatric concerns. In all cases, it is critical to assess the nature of the patient’s substance use and, when indicated, provide appropriate management.
In the ED, the first priority is to rule out any immediate life-threatening conditions. For patients presenting with acute opioid overdose and respiratory depression, naloxone, a mu-opioid receptor antagonist, should be administered. Following naloxone, patients should be monitored and stabilized medically before considering long-term treatment.
When patients present with opioid withdrawal, management approaches differ. Some may have received naloxone and become symptomatic, while others may present at varying stages of withdrawal hours to days after their last opioid use. Symptomatic management of withdrawal symptoms often involves adjunct medications (see Table 1).
Long-term management options for OUD in the ED setting include methadone, buprenorphine, and naltrexone. These medications should be available for ED clinicians to initiate in patients who meet the DSM-5 criteria for opioid use disorder (OUD). The criteria
“In all cases, it is critical to assess the nature of the patient’s substance use and, when indicated, provide appropriate management.”
Abdominal cramping
encompass impaired control of substance use, physical dependence, social or interpersonal impairment, and high-risk use. In cases where OUD criteria are not met, medications for OUD (MOUD) are not indicated.
One of the major challenges in ED management of OUD is ensuring access to outpatient treatment. Resource availability varies across health care systems, with some offering robust bridge programs that provide outpatient counseling and medication access, while others have limited options. Knowing local resources and available referral options is key to ensuring proper follow-up for patients after acute ED treatment.
Several medications are used to treat OUD, including naltrexone, buprenorphine, and methadone. Naltrexone, a mu-opioid receptor antagonist, can be prescribed by any licensed practitioner. Buprenorphine, a partial agonist, can be prescribed by any practitioner with a DEA license allowing the prescription of Schedule III substances. Following the Consolidated Appropriations Act of 2023, practitioners no longer need a DATA-waiver (X-waiver) to prescribe buprenorphine. This legislation also lifted limitations on the number of
patients a provider can prescribe buprenorphine to, facilitating broader access.
Regarding methadone prescribing in the ED, legislation allows for the “dispensation of narcotic drugs to relieve acute withdrawal symptoms from opioid use disorder (OUD).” This is known as the “Three-Day Rule.” Under this rule, practitioners are permitted to provide a threeday supply of narcotic medications for initiating maintenance or detoxification treatment for OUD, in accordance with relevant state, federal, or local laws. This provision bypasses the typical restriction that methadone can only be prescribed by Opioid Treatment Programs (OTPs) or by practitioners with special permission from the Drug Enforcement Administration (DEA).
In practice, this allows ED physicians to prescribe methadone, which can act as a bridge to ongoing treatment or facilitate access to follow-up care — both of which have been shown to improve patient retention in treatment.
However, clinicians should be mindful of key considerations when prescribing medications for opioid use disorder in the ED, as these decisions can have important implications for patient care.
mg q8h
mg q6h
When choosing the most appropriate medication for a patient, several factors must be considered, particularly the time elapsed since the patient’s last opioid use and available outpatient follow-up options. For naltrexone, the required gap between opioid use and initiation of treatment is recommended to be at least 7-10 days or up to 14 days for patients on long-acting opioids like methadone. This makes naltrexone challenging to start in the ED setting and may not be the optimal choice for most patients.
Buprenorphine, a partial agonist at the mu opioid receptor, requires a shorter gap since the patient’s last opioid use, but the duration varies based on the substance and usage frequency. Different dosing strategies exist, and clinicians should follow current guidelines while discussing options with the patient. For longacting formulations, a short-acting oral “test dose” is typically given first to avoid precipitated withdrawal before administering the injection.
Short courses of methadone can be given in the ED, either as an initial dose or a continuation of treatment, with dosing based on local

Buprenorphine Formulations –partial agonism at opioid receptor
Buprenorphine-Naloxone
Buprenorphine
Methadone Formationsfull agonism at opioid receptor
Methadone
Naltrexone Formations- full antagonism at opioid receptor
or
Table 2. FDA- Approved Medications for Opioid Use Disorder
*General guidelines for chronic therapy as provided in SAMHSA Treatment Improvement Protocol for MOUD; refer to full document for further considerations to determine therapy for an individual patient
**Weekly and monthly formulations of extended-release buprenorphine are available
continued from Page 85
regulations, patient characteristics such as age and pregnancy, and potential concurrent opioid use.
In all cases, it is essential to ensure that the medication chosen can be continued after discharge, particularly for shorter-acting medications. Understanding outpatient follow-up options will guide the selection of the most appropriate MOUD for each patient.
When initiating MOUD, the primary concern with buprenorphine is the risk of precipitating withdrawal, which can be painful and affect future medication adherence. It’s crucial to assess the severity of a patient’s withdrawal before administering medication that could worsen symptoms. The Clinical Opioid Withdrawal Scale (COWS) helps categorize withdrawal severity and guide management, but it should be considered along with the patient’s last opioid use and any history of precipitated withdrawal. Since synthetic opioids vary in their effects, it’s difficult to predict how a substance will interact, making dosing decisions challenging. Traditional starting doses range from 2-4 mg, but higher
“Opioid use disorder remains a prevalent and complex issue for many ED patients. While management is challenging, the strategies outlined above, combined with empathetic and non-judgmental care, are essential for improving patient outcomes and providing pathways for long-term recovery.”
doses (8 mg or more) are sometimes used. If precipitated withdrawal occurs, additional buprenorphine and adjunct medications with various dosing strategies may be needed. ED clinicians can also seek help from addiction medicine or toxicology services for complex cases.
Opioid use disorder remains a prevalent and complex issue for many ED patients. While management is challenging, the strategies outlined above, combined with empathetic and non-judgmental care, are essential for improving patient outcomes
and providing pathways for longterm recovery. By embracing these treatment protocols, ED clinicians can play a critical role in managing opioid use disorder and helping patients achieve healthier lives.

Dr.
Ehrhardt is a first-year toxicology fellow at Emory University school of medicine.

By Aymane Rouchdy
As Match 2025 approaches, congratulations are in order — both for you, and by extension, for all of us. Reaching this milestone is no small feat. We’ve devoted years to studying textbooks, tackling clinical challenges, and envisioning the kind of doctors we aspire to become. Now, as we finalize our rank lists with Match Day just around the corner, a mix of emotions — excitement, hope, fear, and, most prominently, uncertainty — feels both familiar and overwhelming.
Uncertainty is an inherent part of this process and confronting it can be one of the most challenging aspects. But what if we reframed it? Instead of allowing uncertainty
to consume us, what if we viewed it as an opportunity for growth and reflection?
To address uncertainty, we must first identify the emotions it stirs:
• Fear: Will I match? Will I thrive in the program I end up in? Fear often leads us to question our value, whispering that we might not belong.
• Anxiety: Anxiety thrives in the spaces we can’t control. It feeds on “what ifs” and the endless secondguessing about what we might have said or done differently.
• Frustration: When reality doesn’t align with our expectations — such as receiving fewer interviews than
anticipated — frustration can set in. The process may feel opaque or overwhelming.
• Self-despair: This is the heaviest of all, the nagging voice that suggests, “I’m not enough.” Rejection feels deeply personal, even though it is often influenced by factors beyond our control.
Confronting the Emotions
Each of these emotions is valid, and each has a way forward. Here are some strategies to address them:
• Facing Fear: Fear loses its power when we name it. Ask yourself, what exactly am I afraid of? Challenge those fears with facts. Most applicants successfully match, and those who don’t often
“Uncertainty is an inherent part of this process, but instead of allowing it to consume us, we can view it as an opportunity for growth and reflection.”

find fulfilling pathways through the Supplemental Offer and Acceptance Program (SOAP) or alternative routes. While uncertainty is real, it is not a final judgment.
• Managing Anxiety: Anxiety thrives on the uncontrollable. Counter it by focusing on what you can control — completing your rank list, maintaining routines, and grounding yourself in the present. (Self-care idea: Take a 45-60 minute nature walk at least three times a week, with your favorite warm drink and playlist or podcast.)
• Reframing Frustration: Frustration can be reframed as growth. Every setback teaches adaptability — a critical skill in emergency medicine. Reflect on the challenges you have overcome to get here and the resilience you’ve built.
• Overcoming Self-despair: Alain de Botton of The School of Life explains, “We are not always humiliated by failing at things; we are humiliated only if we first invest our pride
and sense of worth in a given achievement, and then do not reach it.” This resonates deeply. Our worth is not tied to Match results; it’s shaped by the patients we’ve cared for, the mentors who’ve guided us, and the grit it took to get us here.
Although we cannot eliminate uncertainty, we can navigate it with intention. Consider these approaches:
• Find Stillness: Spend time alone in a quiet place, focusing inward on your dreams, hopes, prayers, and aspirations. Pause and reconnect with why we’re here in the first place.
• Redefine Success: True fulfillment comes from living a life aligned with our values. Whether we match at our top choice or discover an unexpected path, this process is about building a meaningful life and career aligned with our values.
• Practice Gratitude: Gratitude shifts focus from what’s missing to
what’s abundant. Reflect on the mentors who have supported you, the patients who have trusted you, and the personal growth you have achieved.
• Lean on Your Support Network: Talk with a trusted mentor, classmate, or loved one. Share your fears and hopes. We’re not alone in this process. Sometimes talking can lighten the emotional burden.
• Focus on the Process: There’s a quiet power in letting go of the outcome and finding pride in the effort. We have done the work; now we trust the process to unfold as it should.
Match Day isn’t the end of the journey; it’s the start of another chapter. The skills we are developing now — resilience, adaptability, the ability to move forward in the face of uncertainty — will be just as critical in the emergency department as our clinical knowledge.
As we move through these next few months, remember that we belong here. Match Day does not define us. We’ve already proven we have what it takes to thrive in emergency medicine.
Here’s to Match 2025 and to embracing the unknown, one step at a time.

Aymane Rouchdy is a fourthyear medical student at Ross University School of Medicine with a strong interest in emergency medicine. He supports fellow medical students by sharing insights on navigating the challenges of medical school and the residency application process. X: @aymaner25

By Jose Miguel Juarez, MD, MS
Introduction
Bedside ultrasound evaluation of the aorta is a critical skill for emergency medicine (EM) physicians, allowing for the rapid identification of acute aortic syndromes, such as aortic dissection. This diagnostic capability is essential for managing both stable and critically ill patients.
Abdominal aortic ultrasound evaluation in the emergency department (ED) is well-established, extensively studied, included in the American College of Physicians (ACEP) Emergency Ultrasound Guidelines, and incorporated into emergency medicine residency
ultrasound curricula. However, pointof-care evaluation of the thoracic aorta in the emergency department remains less defined, studied, and practiced clinically. Challenges in thoracic aortic imaging, such as interference from the sternum, ribs, and lungs, can make obtaining intrathoracic views difficult, though achievable.
Although various ultrasound views of the thoracic aorta are described in current emergency medicine literature, a systematic approach has yet to be presented. This article introduces a basic bedside ultrasound protocol, the BETA Exam, for evaluating the thoracic aorta in
the emergency department when acute aortic syndrome is suspected.
Timely recognition of acute aortic syndromes, including dissections and intramural hematomas, is essential in emergency settings to optimize patient outcomes. The primary sonographic feature of an acute aortic dissection is a mobile, hyperechoic, well-defined intraluminal dissection flap that creates a false lumen. For an acute intramural hematoma, the key sonographic feature is a thickened aortic wall with mixed echogenicity and a crescentic or circumferential appearance.
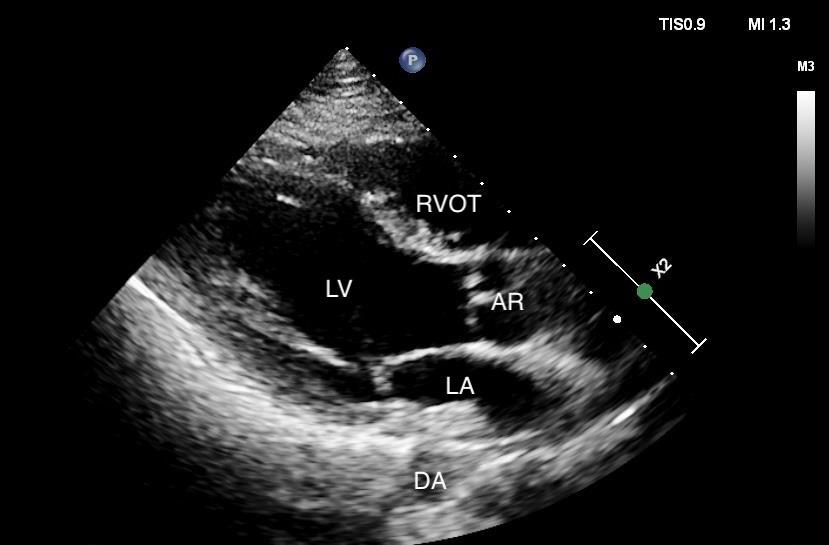

“A dilated or aneurysmal aortic root is often the first observed sonographic indicator of a dissection.”
Aortic Root
The aortic root can be assessed using the standard parasternal long axis (PLAX) cardiac view (Figure 1). A normal aortic diameter at the level of the sinuses of Valsalva is less than 4.5 cm, measured using the “leading edge to leading edge” method during diastole, when the aortic valve is closed. A dilated or aneurysmal aortic root is often the first observed sonographic indicator of a dissection. However, false-positive interpretations can result from this limited view, as the hyperechoic aortic valve cusps can mimic a dissection flap when closed.
Evaluation of the proximal ascending aorta using a “high” PLAX view has been described in cardiology literature. This view is obtained by moving the probe up one rib space from the standard PLAX window and rocking medially (Figure 2). Additionally, a right parasternal view
can be used for further assessment. This sagittal view is obtained by placing the probe in the second or third right parasternal intercostal space with the marker oriented cephalad (Figure 3). Positioning the patient in the right lateral decubitus position may optimize this view.
The aortic arch can be evaluated using the suprasternal notch view (Figure 4). This view is obtained by placing the phased-array probe in the suprasternal notch area with the marker oriented toward the patient’s left jaw. It provides visualization of the aortic arch and branching arteries, including the brachiocephalic artery, left common carotid artery, and left subclavian artery. Identifying a dissection flap in any of the branching arteries is clinically significant and often warrants further evaluation with computed tomography (CT) angiography of the neck and head.
Transverse views of the descending aorta are routinely obtained with
standard PLAX and apical fourchamber views. Ensuring adequate depth to include the entire aorta is important to avoid missing acute pathology. A long axis view of the descending aorta can be obtained using the following techniques:
1. From the PLAX view, rotate the probe 45 degrees clockwise, stopping before reaching the parasternal short axis view (Figure 5).
2. From the A4C view, rotate counterclockwise approximately 60 degrees, as if transitioning to an apical two-chamber view.
Fine probe adjustments, such as rocking or fanning, may be required to optimize these views.
BETA Protocol
The thoracic aorta can be systematically evaluated using the following sequence:



“Timely recognition of acute aortic syndromes, including dissections and intramural hematomas, is essential in emergency settings to optimize patient outcomes.”
ULTRASOUND
continued from Page 91
1. Aortic root: Begin with the standard PLAX view.
2. Ascending aorta: Use the high PLAX and right parasternal views.
3. Aortic arch: Evaluate the arch with the suprasternal notch view.
4. Descending aorta: Visualize the descending aorta using modified PLAX and A4C views.
Limitations
The anatomical course of the thoracic aorta and surrounding structures allows only segmented evaluation through transthoracic views. Common blind spots include the distal

Figure 5. Left parasternal view of the sagittal descending thoracic aorta. LV = left ventricle, RV = right ventricle, PDA = proximal descending thoracic aorta, DDA = distal descending thoracic aorta
ascending aorta and proximal aortic arch.
Conclusion
Bedside cardiac ultrasound in the emergency department traditionally evaluates conditions such as heart failure, right heart strain, pericardial effusion, and valvulopathies. Incorporating the BETA protocol enables emergency physicians to evaluate acute thoracic aortic syndromes. While point-of-care ultrasound cannot replace computed tomography angiography for comprehensive assessment, it is invaluable for critically ill patients who cannot be transported to a scanner. The emergence of transesophageal echocardiography (TEE) in the ED offers additional opportunities for
bedside evaluation but is limited to intubated, sedated, and critically ill patients. The BETA protocol, in contrast, can be applied to a broader range of patients, providing emergency physicians with a valuable diagnostic tool and practical, systematic approach to evaluating for acute aortic syndromes at the bedside

Dr. Juarez is a clinical assistant professor of emergency medicine and ultrasound faculty at NYU Grossman School of Medicine. He is also an emergency medicine attending at the Ronald O. Perelman Department of Emergency Medicine at

By Josue Reyes, DO
Point-of-care ultrasound (POCUS) has become an indispensable diagnostic tool in emergency medicine. As a resident, I quickly appreciated the rapid diagnostic approach that POCUS offers. However, during my dedicated ultrasound rotation, I learned it is much more than just a diagnostic tool; it also has therapeutic value. This is especially true for obstetric ultrasound, which provides critical insights into the rapid assessment of pregnant patients.
In the fast-paced environment of the emergency room, time is often a critical factor. Obstetric ultrasound allows for quick, noninvasive evaluation of maternal and fetal well-being, offering real-time visual information that aids clinical decision-making and improves patient outcomes. However, its value extends far beyond the clinical realm when you consider its impact on the patient experience.
Emergency room visits often occur during some of the most stressful moments in a person’s life. As expert clinicians, it is not only our role to evaluate emergent etiologies but to also provide reassurance
and emotional support when possible. For pregnant patients facing the stress of uncertainty, the ability to visualize their fetus and observe its well-being can provide immediate reassurance and reduce anxiety. Real-time images not only de-escalate tense situations but also offer patients a clearer understanding of their condition.
Building rapport with patients in the emergency setting is always challenging due to time constraints, but obstetric ultrasound offers a unique opportunity to connect with them and establish a relationship. By explaining the images on the screen, discussing next steps, and preparing patients for anticipated

“Obstetric ultrasound allows for quick, noninvasive evaluation of maternal and fetal well-being, offering real-time visual information that aids clinical decision-making and improves patient outcomes.”
wait times, you can reassure them that their concerns are heard and respected. In these moments, I see firsthand how obstetric ultrasound not only enhances medical care but also helps alleviate fears, offers emotional reassurance, reduces anxiety, and builds trust in a very short time.
As physicians, our primary focus is always patient well-being. However, in the high-stress environment of the emergency room—managing life-anddeath situations and making critical decisions—we can sometimes lose sight of this goal. Performing obstetric ultrasounds offers an unexpected source of joy, connection, and mental wellness for both patients and physicians.
These moments of connection highlight the human side of our work, allowing us to share in the hope and joy of expectant parents, even
amidst the chaos of an emergency room. They remind us that health care goes beyond treating illness— it’s also about celebrating life. In a setting where negative outcomes can sometimes overshadow victories, such meaningful experiences help maintain our sense of purpose and the profound impact we have on patients' lives.
As a physician and the proud father of two beautiful children, I understand firsthand the anxiety that can accompany pregnancy, especially in the context of emergency care. During my own experiences, awaiting ultrasound appointments provided both reassurance and comfort. Seeing our child with our own eyes on the screen reassured us in ways that words alone could not. There is something deeply calming about seeing a child’s movements or hearing
their heartbeat. For us it offered a sense of security, relief, and hope. As emergency room physicians, we are uniquely positioned to offer this same sense of comfort to our pregnant patients, making a meaningful difference not only in their clinical care but in their emotional well-being. If you have not experienced this firsthand, take the opportunity with your next expectant patient to perform an obstetric ultrasound. Pay attention to their expressions as they see their baby on the screen and share in the joy of that meaningful moment.


By Jackie Jian, DO
As ultrasound technology becomes more common in emergency medicine practice and residency training, there is often hesitation to take the next step in performing advanced sonographic assessments for patients. One challenging aspect for both trainees and faculty is evaluating waveforms produced by spectral Doppler or M-mode.
M-mode
M-mode technology involves the ultrasound machine sending and receiving data along a single scan line, displaying the data with the x-axis representing time and the y-axis representing distance. This technique is most useful for assessing the movement of rapidly moving structures, such as inferior vena cava (IVC) respiratory variation or the fast movement of cardiac valves opening and closing.
“Spectral Doppler provides a quantitative measure of blood flow through either pulsed wave Doppler or continuous wave Doppler.”
Doppler ultrasound relies on the frequency shift between the transmitted and received Doppler signals when targeting a moving object. For example, blood moving toward the ultrasound probe produces a higher reflected frequency, while blood moving away from the probe generates a lower frequency. This difference allows the machine to display both flow direction and velocity. Spectral Doppler provides a quantitative
measure of blood flow through either pulsed wave Doppler (PWD) or continuous wave Doppler (CWD).
Pulsed wave Doppler sends a short burst of sound and listens for echoes at specific intervals, enabling the machine to sample data from a specific point on the screen. However, PWD has limitations in measuring high-speed velocities, where aliasing occurs, leading to inaccurate results. Continuous wave Doppler sends and receives signals constantly, allowing for
measurements of high velocities but without the ability to focus on a specific point in the flow. Both PWD and CWD generate waveforms that help assess a patient's physiology and potential pathology.
At the SAEM Sonogames last year, a test was conducted to assess resident learners' ability to interpret waveforms. Below is a "cheat sheet" for emergency department (ED) physicians on common waveforms to recognize:
To assess respiratory variation in the IVC, obtain a long-axis view of the IVC and place the M-mode line over its anterior and posterior walls. This will plot the variation (if any) in the IVC with respiration.
• The first image shows normal respiratory variation.
• The second image demonstrates coaptation of the vessel walls, indicating dehydration.
• The third image shows a plethoric IVC with no respiratory variation.
EPSS provides a surrogate measure of left ventricular ejection fracture. In the parasternal long-axis view, place the M-mode line through the septum and the tip of the anterior mitral leaflet. The machine will capture the mitral valve's rapid opening during diastole and systole. The distance between the E-point (the first wave) and the septum can determine normal versus abnormal ejection fraction.
• A measurement over 14 mm is abnormal, while a measurement less than 7 mm is normal.
• The first image shows a normal ejection fraction, and the second shows an abnormal measurement.
For suspected tricuspid regurgitation, place the CWD line over the regurgitant jet in an apical fourchamber view and assess the
“Multiphasic arterial waveforms are normal and indicate healthy arterial flow, while deviations could suggest stenosis.”

Waveform Cheat Sheet
pressure gradient.
To assess for aortic stenosis, place the CWD line through the aortic outflow tract in the apical fivechamber view. The peak velocity can be used to grade the severity of the stenosis, with a velocity greater than 4 m/s indicating severe stenosis.
The first image shows a multiphasic (or triphasic) arterial waveform, which is considered normal. This waveform has three phases:
1. High forward flow during systole (the contraction phase of the heart),
2. A brief reversal of flow during early diastole (the relaxation phase of the heart), which causes the waveform to cross the baseline,
3. Forward flow in late diastole, resulting from the reflection of blood from the closed aortic valve.
A monophasic arterial waveform, shown in the second image, lacks these three distinct phases and may suggest the presence of stenosis, or
narrowing, in the blood vessel.
The first image in this series demonstrates grade 1 diastolic dysfunction, characterized by an E/A reversal. Normal diastolic function displays a larger E-wave reflecting early diastole and a smaller A-wave indicating atrial contraction.
• The second image shows an assessment using tissue Doppler, with the TWD gate placed on the mitral annulus in an apical fourchamber view.
• In normal function, the e' wave should be larger than the a' wave, with any reversal signifying diastolic dysfunction.
ABOUT THE AUTHOR

Dr.
Jian is the ultrasound director at Guthrie Clinic Robert Packer Hospital Emergency Medicine Residency.

By Katren Tyler, MD; Bryn Mumma, MD; Jeff Druck, MD; Al’ai Alvarez, MD; Neha P. Raukar, MD, MS; Michelle D. Lall, MD, MHS; Marla C. Doehring, MD; Reuben Johnson, MD, Nick Ashenburg, MD; Simiao Li-Sauerwine, MD MSCR; Andrew Wong, MD, MBA; and Amanda J. Deutsch, MD on behalf of the SAEM Wellness Committee
While the holidays for this year are behind us, it is not too early start planning for future holidays. For emergency physicians, holidays often mean more than just celebrations; they bring shifts in the emergency department (ED) while balancing family and social commitments. This perennial challenge in academic emergency medicine (EM) departments requires careful attention to equity and faculty well-being. Departments must navigate the intricate balance of professional responsibilities, personal priorities, and cultural values to create schedules that meet the diverse needs of their teams.
Most academic EM departments rely on holiday rotation systems to manage coverage. These systems divide holidays into blocks and rotate faculty assignments annually to distribute the burden. Typical holiday shifts include winter holidays such as Thanksgiving, Christmas, and New Year’s, as well as summer holidays like Memorial Day, Labor Day, and the Fourth of July. Protected periods range from 1–7 days, with most departments protecting four days around a holiday. Some schedules include additional days for travel and family time.
It is common for departments to require faculty to work two holiday blocks per season. "Faculty" refers to fellows and staff physicians scheduled as emergency department (ED) attendings.
Strengths of holiday rotation systems include:
• Predictability: Faculty know in advance which holiday blocks they will cover, allowing for long-term planning.
• Flexibility: Shift swaps and trades are common, offering room for individual preferences.
• Shared Responsibility: Most EM professionals understand that
working holidays is a necessary part of the job.
However, challenges remain, such as perceptions of inequity, inflexibility for extended travel, and dissatisfaction with how shifts are distributed.
Universal Challenges
Despite differences between departments, many EM teams report recurring issues with holiday scheduling:
• Uneven Workload Distribution: Pairing certain holidays (e.g., grouping Thanksgiving and New Year’s) creates an imbalance, with some faculty working more holiday shifts than others. Short, protected periods exacerbate this, especially when shifts are assigned during the holiday week outside of protected time.
• Limited Time for Travel: Short protected periods, often just one or two days, make it difficult for faculty to travel or spend time with family.
• Non-Essential Services: Some departments reduce lower-acuity services, such as urgent care or fasttrack, even when patient volumes are low.
• Diversity of Needs: Faculty have varying personal, cultural, and religious preferences, which makes a one-size-fits-all scheduling system inadequate.
• Lack of Transparency: Without clear guidelines, faculty may perceive holiday scheduling as arbitrary or unfair. Transparency is needed for shift requirements, expectations for nocturnists, part-time staff, fellows, and consultants (e.g., toxicology or addiction medicine). It should also clarify how seniority and non-compliance with availability requirements are handled.
Actionable Solutions for Academic Emergency Departments
Addressing the importance of holidays to most faculty, especially those with family obligations, the following strategies can help mitigate scheduling challenges:
1. Reevaluate Holiday Groupings

Challenge: Grouping major holidays leads to disproportionate burdens on some faculty.
Solutions:
• Decouple Major Winter Holidays: Assign Thanksgiving, Christmas, and New Year’s independently to balance the load.
• Balance Across the Year: Pair winter holidays with summer holidays (e.g., Memorial Day, July 4th, Labor Day) to distribute the workload more evenly.
• Weighted Scheduling: Assign faculty one "heavy" holiday, one "light" holiday, and one free period during the winter season.
2. Incorporate Faculty Preferences Challenge: Current systems often overlook individual values and priorities.
Solutions:
• Preference Ranking: Let faculty rank their preferred and least preferred holidays to help guide scheduling decisions.
• Survey Availability: Collect data on preferred travel dates to accommodate extended trips.
• Consistent Block Lengths: Standardize holiday block durations or match shorter blocks with other significant dates throughout the year.
• Pre-Scheduling Trades: Allow block swaps before finalizing the
schedule to better align with faculty preferences.
3. Offer Incentives for Holiday Shifts Challenge: Holiday coverage is challenging for many faculty.
Solutions:
• Financial Incentives: Offer bonuses or other financial rewards for holiday coverage.
• Non-Monetary Rewards: Provide additional vacation days, preferential scheduling for future rotations, or departmental recognition.
4. Expand Protected Break Periods Challenge: Short, protected periods around holidays limit travel and family time.
Solutions:
• Extend Protected Time: Increase the protected period to 2–5 days around major holidays.
• Trade for Future Flexibility: Allow faculty to work multiple holidays in one year in exchange for extended time off in another.
• Holiday Buyout: Allow faculty to exchange less desirable shifts (e.g., weekends or overnights) for full holiday weeks off.
5. Increase Transparency Challenge: Faculty may feel excluded from the scheduling process.
on Page 101

Solutions:
• Publish Guidelines: Share clear criteria for holiday assignments, especially for specific roles (e.g., nocturnists, part-time faculty, fellows).
• Visualize Assignments: Publish a holiday shift schedule that clearly displays assignments for all faculty and makes comparisons straightforward.
• Create a Scheduling Committee: Include representatives from various career stages (junior, mid-career, and senior faculty) to ensure diverse input.
6. Recognize Diverse Holidays Challenge: Traditional winter holiday schedules overlook cultural and religious holidays outside the majority.
Solutions:
• Expand Protected Dates: Include cultural holidays (e.g., Ashura, Diwali, Hanukkah, Lunar New Year) in the schedule for consideration.
• Substitution Options: Allow faculty to exchange traditional holidays for those aligned with their beliefs, practices, or traditions.
7. Leverage Data for Optimization Challenge: Schedules may not reflect actual staffing needs or faculty preferences without data-driven insights.
Solutions:
• Analyze Patterns: Use data analytics to identify trends in patient volume and faculty availability.
• Predictive Modeling: Anticipate staffing needs to optimize coverage while minimizing strain.
8. Reassess Staffing Needs Challenge: Departments continue with the standard schedule on holidays, even when patient volumes are low.
Solutions:
• Analyze Historical Volumes: Review patient volume data to identify lowdemand services that can be scaled back.
• Focus on Core Services: Prioritize essential emergency services, reducing coverage for lower-acuity areas.
9. Account for School Vacations
Challenge: Faculty with school-age children struggle to align holiday shifts with school vacations.
Solutions:
• Scheduling with School Calendars: Adjust the holiday calendar and shifts to accommodate common school vacation periods and allow for greater flexibility for parents.
• Flexible Non-Clinical Work: Allow remote or flexible scheduling for nonclinical tasks during school breaks.
10. Pilot and Refine Changes
Challenge: Systemic changes may involve risks or unknown outcomes.
Solutions:
• Test Strategies: Pilot new scheduling approaches during a single holiday season or with a small group of faculty.
• Collect Feedback: Gather faculty input on satisfaction and outcomes to refine processes before a full rollout.
A Framework for Success
Holiday scheduling in academic EM departments reflects broader challenges in managing diverse, highperforming teams. However, these challenges also present opportunities for improvement and innovation.
Key principles for success include:
• Equity: Ensure that no group bears an unfair burden.
• Flexibility: Adapt to the varied needs and preferences of faculty.
• Transparency: Maintain clear, consistent communication regarding the scheduling process.
• Inclusivity: Recognize and respect the cultural and personal values of all team members.
With thoughtful planning and a commitment to collaboration, academic EM departments can develop holiday schedules that support faculty well-being, foster equity, and maintain the highest standards of patient care. By addressing both systemic and individual needs, holiday scheduling can transform from a perennial pain point to a reflection of shared values and priorities







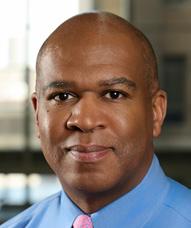




Dr. Tyler is a clinical professor of emergency medicine at the University of California, Davis.
Dr. Mumma is a clinical professor of emergency medicine at the University of California, Davis.
Dr. Druck is a professor of emergency medicine at the University of Utah, Department of Emergency Medicine.
Dr. Alvarez is a clinical associate professor at Stanford University.
Dr. Raukar is an associate professor of emergency medicine at Mayo Clinic.
Dr. Lall is a professor of emergency medicine at Emory University School of Medicine.
Dr. Doehring is an associate professor of clinical emergency medicine at Indiana University School of Medicine.
Dr. Johnson is an associate professor of emergency medicine at Washington University School of Medicine.
Dr. Ashenburg is an assistant professor of emergency medicine at Stanford University.
Dr. Li-Sauerwine is an associate professor of emergency medicine at The Ohio State University.
Dr. Wong is a clinical professor of emergency medicine at the University of California, Davis.
Dr. Deutsch is a clinical assistant professor of emergency medicine at Thomas Jefferson University.

By Luis Miranda, MD, MS; Vytas Karalius, MD; Amanda J. Deutsch, MD; and Christine R Stehman, MD on behalf of the SAEM Wellness Committee Subcommittee on Trainee Well-Being
The following story is not fictional. It is based on actual incidents which likely mirror experiences shared by many in the emergency medicine community.
Imagine this: during the first hour of her first-ever emergency department (ED) shift, a resident excitedly picks up her first patient. She is “The Doctor.” With her stethoscope around her neck, she walks into the room, only to find the patient unresponsive to her greeting and introduction. The nurse informs her this is a new development. Reaching for the patient’s neck, the resident feels for a pulse—nothing. The nurse immediately starts compressions as the resident runs to get the attending physician.
The team works together to stabilize the patient. The attending instructs the resident to call the medical intensive care unit (MICU) fellow. As the resident makes the
call, her mind blanks. What follows is one of the most difficult patient presentations she has ever given. She stumbles through the details, explaining that the patient is now stabilized, intubated, and on pressors.
The fellow asks, “Okay, can you tell me about the patient’s medical history?”
The resident replies, “Sorry, when I got to the room, she was unresponsive and pulseless.”
The fellow responds, “Why don’t you read a little about the patient and call me when you’re prepared?”
Recognizing the panic on the resident’s face, the attending takes the phone and completes the patient’s admission to the unit.
Later, the resident asks the attending why the fellow was rude, despite knowing she was an intern presenting her first patient. The
attending explains, “You have to understand that many services dislike when the ED calls because it means more work for them. Think about it: how would you feel if the same person called you every day asking you to take on additional tasks?”
Lacking an understanding of research on workplace incivility, the resident concludes that inpatient services mistreat emergency physicians because ED calls are seen as "extra work." Determined to counter any consultant objections, she adopts a mindset of turning each interaction into a challenge to "win"— either by compelling consultants to "come down and physically see the patient" or by refuting their refusals and workarounds.
Sometime later, she encounters another difficult situation. While presenting a post-operative patient with acute abdominal pain
and lactic acidosis, a consultant’s senior interrupts her, questioning her assessment. “Do a better job presenting and managing the patient,” he says. “Don’t call just because we did the surgery and the patient is in pain.”
When the consultant arrives, the resident confronts him: “There’s no reason to talk to me like that. Remember, while you’re upstairs at a computer looking at a screen, I’m looking at the patient.”
The consultant’s response catches her off guard: “I’m sorry if I made you feel that way. That wasn’t my intention. We’re always happy to see the patient.”
Reflecting later, the resident feels uneasy about her approach. While her aggressive stance may have succeeded in compelling the consultant to see the patient, it undermined the foundation for a professional relationship. It was their first meeting, and she realizes she knew nothing about the consultant’s challenges or how his day was going. This experience prompts her to shift her perspective, recognizing the consultant’s inherent worth and the value of showing respect and empathy in similar interactions.
A later incident deepens her understanding. While working a community ED shift, she calls urology to request a catheter change. The urologist responds with dismissive texts, calling the consult unnecessary, unprofessional, and “a waste of time.” He asks to speak with her attending. After a discussion with the attending, the resident receives an apologetic message from the urologist. He admits to once being in her shoes and acknowledges his unprofessional behavior. This recognition gives the resident pause. While the urologist had been rude, her equally harsh tone and attitude had only escalated the conflict. She realizes the importance of handling such situations with grace rather than treating them as battles to win.
Armed with this new perspective, the resident adopts a different approach in future interactions. During a heated call with an interventional radiology
(IR) attending, she responds calmly: “I’m sorry you feel that way, but please remember you were once in my shoes, and I’m just following instructions.” After a moment, the attending apologizes for yelling, explaining he was under stress from a difficult case.
Not all interactions, however, are fraught with rudeness. Once, the resident called a fellow at 4 a.m., bracing for pushback. Instead, the fellow was supportive and kind. When the resident expressed surprise, the fellow responded, “I’m sorry you’ve had to deal with rudeness. While I can’t speak for others, remember they may have a lot on their plate. Please don’t take their behavior personally.”
Anderson and Pearson in examined the idea of workplace incivility in the late 1990s and found it wasn’t widespread enough to warrant regular investigation. Fast-forward to today, where incivility has become commonplace in and out of medicine. A medical culture once defined by collaboration has shifted due to competition, malpractice concerns, and the pressure to excel. These factors have normalized disrespect among colleagues. According to a scoping review by Abate and Greenburg, “incivility and mistreatment across the medical education continuum is persistent, pervasive, and often inadequately reported and addressed.”
Beyond its prevalence, incivility is contagious. Reflecting on her first shift, the resident wonders if she unintentionally perpetuated the cycle of rudeness she experienced. She concludes that breaking the cycle requires pausing to respond thoughtfully while reminding everyone of their shared goal: delivering the best patient care. Such reminders often lead to apologies and self-reflection, fostering a more collaborative environment.
In today’s divided world, creating a supportive workplace is more important than ever, especially as many physicians face burnout. Mistreatment — whether from patients, visitors, or colleagues — degrades patient care, teamwork,
communication, and physician wellbeing. Studies, including one by Lu, et al. of over 8,000 emergency medicine residents, underscore the need to address and mitigate these internal dynamics to safeguard physician well-being and promote a healthier work environment. Solutions will likely emerge from systemic and organizational efforts, such as implementing and enforcing zerotolerance policies.
While organizational policies, such as implementing and enforcing zero-tolerance policies, play a critical role, individuals also have a part to play. Reflecting on her experiences, the resident learns that humility and empathy can foster understanding and strengthen professional relationships. Acknowledging the humanity and vulnerabilities of others strengthens the shared commitment to patient care. By working together, we can reclaim a culture of respect for each other, and collaboration, keeping the focus on healing and improving lives — both those of our patients and our colleagues.




Dr. Miranda is an emergency medicine resident at Thomas Jefferson University. X: @luisemmd
Dr. Karalius is an assistant program director at Stanford Emergency Medicine.
Dr. Deutsch is the SAEM Wellness Committee chair and director of well-being at Thomas Jefferson University. X: @amandajdeutsch
Dr. Stehman is the director of wellness education at the University of Illinois College of Medicine-Peoria/OSF Healthcare.

By Maia Winkel, MD; Jeffrey Druck, MD; Monisha Dilip MD, MBA; Maria Moreira, MD; Kyra Reed, MD; Saadia Akhtar, MD; Cindy Bitter, MD, MPH; Al’ai Alvarez, MD; Amanda Deutsch, MD; Nicholas Ashenburg, MD; Stephanie Balint; Cristina Sanchez, MS; and Rupinder Sekhon, MD, MBA, on behalf of the SAEM Wellness Committee
The culture of emergency medicine has long been defined by resilience, quick decision-making, and unwavering dedication. However, this emphasis on non-stop productivity is taking a toll on emergency medicine physicians, with many reporting burnout, fatigue, and moral distress. The demanding nature of the job often overshadow the importance of self-care, contributing to a professional environment that views rest as a luxury rather than a necessity. As Dr. James O’Shea and his colleagues observed in a 2020 article, this cultural expectation, particularly the habit of “pushing through” shifts, may prevent
physicians from engaging in crucial self-care practices, including taking adequate breaks.
This article examines how the culture of emergency medicine can be reshaped to better prioritize wellness, fair scheduling, and practical support for all staff members. Drawing on discussions from the SAEM Wellness Committee and insights from fellow physicians, we explore ways to foster a healthier, more balanced approach to emergency care.
The Challenge of Wellness in Emergency Medicine Emergency physicians are frequently
caught between their dedication to patient care and their own well-being. This tension is especially evident in the discrepancy in staff workflows. While nurses have mandated breaks, physicians often go entire shifts without time for rest, hydration, or nourishment. As Al’ai Alvarez, MD, points out, this disparity strains team collaboration, as different roles receive varying levels of support for self-care. While breaks for nurses are meant to prevent burnout and maintain patient safety, similar policies have not been uniformly extended to physicians, who feel compelled to “push through” their shifts.

“Research also shows that increased fatigue is correlated with a greater number of adverse events, further underscoring the need to mitigate physician fatigue.”
Logistical barriers, such as single coverage shifts where there is no other physician to take over patient care, can exacerbate this issue. However, successful pilot programs at local, national, and international levels demonstrate that these barriers are not insurmountable. A 2022 meta-analysis revealed that taking breaks at work are associated with greater energy, stronger engagement, and improved task performance. As the literature supports the value of breaks, how can practice align with the research? Instituting policies that ensure physicians take breaks, similar to the California Nurse Association’s mandated breaks for nurses in California, could help alleviate burnout, improve mood, and foster a more supportive environment. Research also shows that increased fatigue is correlated with a greater number of adverse events, further underscoring the need to mitigate physician fatigue. Until such policies are developed, attending physicians can set an example for residents by modeling self-care, including breaks, to establish a new norm of valuing rest as integral to professional resilience.
Rupinder Sekhon, MD, MBA, has introduced a “mid-shift check-in” at her hospital, where residents are encouraged to pause, reflect, and attend to their well-being. At the start of each shift, the attending physician and resident set a shared goal, with the attending also sharing their own shift goal, modeling the behavior, reinforcing self-care practices, and demonstrating the importance of balancing achievable professional goals with personal well-being. This mid-shift check-in offers residents the opportunity to assess progress toward the goal while taking time for basic needs — eating, hydrating, or using the restroom. Such simple practices reduce fatigue and stress, support overall well-being, and signal to residents prioritizing their health is not only acceptable, but essential to sustaining their performance.
Kyra Reed, MD, focuses on a particularly sensitive subject –lactation on shift – by regularly checking in on lactating trainees to ensure they maintain their pumping schedules. One practical strategy
she employs is offering to hold a colleague or trainee’s phone during breaks, which helps offload the cognitive burden of taking time for oneself and provides a model for others.
This approach raises a key question: how can emergency departments cultivate a consistent culture of wellness? Small suggestions, such as saying “Why don’t you grab a snack?” instead of “Take a break,” can shift perceptions and increase the likelihood that residents and attending physicians will take short respites during long shifts. Additionally, providing healthy snacks in break areas can support those without the time or resources to prepare meals. These small adjustments can reinforce the value of wellness as part of the workday and integrate an atmosphere of well-being into the context of shift work.
Equity extends beyond break policies
continued on Page 107

continued from Page 105
to include holiday and religious observance scheduling. Cindy Bitter, MD, MPH, noted that some physicians have their religious holidays respected in scheduling, while others do not, leading to feelings of marginalization. Ensuring consistent respect for diverse cultural and religious observances in scheduling can foster a more inclusive environment, where all practitioners feel respected and supported.
Balancing night shifts across different age groups is another ongoing challenge. While age discrimination concerns hinder efforts to protect older physicians from the health risks of night shifts, Stephanie Balint, a medical student, emphasized the importance of finding accommodations for older practitioners while maintaining fair coverage. Specialized roles like nocturnist positions could offer a potential solution, offering a pathway for those who prefer night shifts and highlighting the need for flexible scheduling that supports diverse practitioners.
Flexible scheduling policies, including provisions for pregnant residents to avoid night shifts during their first and third trimesters, also help promote wellness. Evidence links night shift work to negative health outcomes, such as menstrual disturbances, endometriosis, infertility or time to pregnancy, and higher rates of miscarriage in female physicians.
The physical work environment plays a critical role in supporting wellness. Cindy Bitter, MD, MPH, discussed her hospital’s attempt to create a “healing garden,” though the space lacked the qualities needed for true relaxation. By contrast, Al’ai Alvarez, MD, shared how his hospital’s rooftop garden, overlooking mountains, has become an important resource for staff to de-stress. This contrast illustrates the importance and impact of thoughtfully designed wellness spaces on staff mental health.
Saadia Akhtar, MD, noted that dedicated break rooms for residents are often repurposed into administrative workspaces. This shift highlights a need to prioritize wellness spaces in hospitals, where staff can recharge between cases. In highstress environments like emergency medicine, thoughtfully designed wellness areas can be a vital resource for mental and physical recuperation, offering the restorative benefits needed to help health care providers recharge between cases.
Leadership plays a significant role in normalizing wellness practices. As Amanda Deutsch, MD, pointed out, when leaders visibly prioritize selfcare, it sends a strong message to their teams. By modeling behaviors such as taking breaks and balancing work with personal needs, leaders shape a culture where well-being is as integral to professional identity as patient care.
The ongoing discussions within the SAEM Wellness Committee reflect a broader movement within health care to create work environments that respects, supports, and prioritizes the well-being of practitioners. Surveys examining shift practices, holiday coverage, and the potential for mandated breaks could illuminate current gaps and guide the creation of fairer, more sustainable policies.
Ultimately, transforming the culture of emergency medicine to prioritize wellness, equity, and inclusivity is not merely a matter of comfort — it is essential to attracting and retaining skilled practitioners and maintaining high standards of patient care. Through continued dialogue, creative problem-solving, and commitment to improvement, emergency medicine can evolve to reflect the values and meet the needs of those who dedicate their lives to it.
Wellness is achievable within our professional culture if we prioritize self-care and each do our part to advocate for supportive practices within our teams













Dr. Winkel is the Emergency Medicine Physician Wellness Fellow and a clinical instructor at Stanford University.
Dr. Druck is a professor of emergency medicine at the University of Utah, Department of Emergency Medicine.
Dr. Dilip is an assistant professor of emergency medicine and the assistant director of quality at Columbia University Medical Center.
Dr. Moreira is a professor of emergency medicine at the University of Colorado, medical director of continuing education and simulation, and director of professional development and well-being for the Denver Health ED.
Dr. Reed is an assistant professor of both clinical emergency medicine and clinical pediatrics and the emergency medicine residency assistant program director at Indiana University.
Dr. Akhtar is a professor of emergency medicine and medical education, as well as senior associate dean for trainee well-being and resilience in graduate medical education at Mount Sinai’s Icahn School of Medicine.
Dr. Bitter is an associate professor of emergency medicine and the director of resident research and a wellness co-champion at Saint Louis University.
Dr. Alvarez is an associate professor of emergency medicine and the director of well-being at Stanford University.
Dr. Deutsch is a clinical assistant professor and the director of well-being for the department of emergency medicine at Thomas Jefferson University.
Dr. Ashenburg is an assistant professor of emergency medicine at Stanford University.
Stephanie Balint is a fourth-year medical student at Quinnipiac University with a diverse background in emergency medicine.
Sanchez is a fourth-year medical student at Florida State University.
Dr. Sekhon is a professor of emergency medicine at the Beth Israel Deaconess Medical Center.

By Negin Ceraolo, MD, MS and Kevin Watkins, MD
Hunting-related injuries are becoming more common due to the growing popularity of hunting. For wilderness medicine providers, understanding the types of injuries that can occur is essential. However, data on the epidemiology of these injuries is limited. Although many assume hunting injuries are primarily related to gunshot wounds, falls actually account for a larger proportion.
Falls contribute to 50 percent of hunting-related injuries, with treestand falls being the most
common. A treestand is a platform used by hunters to elevate themselves in trees for better visibility and concealment. These platforms are typically positioned 19 to 20 feet above the ground and can become slippery, particularly in wet or icy conditions. Falls from treestands often lead to severe injuries. A recent study found that 59 percent of fall victims experienced spinal fractures, 47 percent suffered lower extremity fractures, 18 percent sustained upper extremity fractures, and 18 percent had closed head injuries. Surgery was required in 81 percent of fall-related cases, and 8.2
percent of victims had permanent neurological deficits.
Treestand-related injuries can include suspension trauma, also known as harness hang syndrome. This condition can occur within 5 to 30 minutes of hanging in a harness and results from blood pooling in the legs, potentially leading to hypovolemic shock. Complications such as rhabdomyolysis and renal failure may develop with prolonged suspension. Management in wilderness settings involves quickly releasing the suspension, laying the individual flat, administering
“Fifty percent of hunting injuries result from falls, with treestand incidents being the most common cause.”
intravenous fluids if available, and considering calcium for potential hyperkalemia.
Injuries involving firearms are another significant category. These can result from firearm misfires, weapon malfunctions, or shooting incidents. Improper handling of firearms poses risks not only to hunters but also to their companions. According to a recent study, gunshot wounds account for 29 percent of hunting injuries, with 58 percent of these being self-inflicted. Common causes of gunshot wounds include:
• Victims unintentionally stepping into the line of fire.
• Shooters mistaking victims for game.
• Shooting during rapid movements when tracking game.
Preventing firearm accidents is crucial, but in the event of such injuries, evacuation and trauma management following established guidelines are essential. Wilderness medicine providers may find a tourniquet invaluable, and the MARCH mnemonic (massive hemorrhage, airway, respiration, circulation, head injury, and hypothermia) serves as a useful framework for prioritizing treatment.
Arrow-related injuries also occur, often caused by falling on arrows or accidentally triggering crossbows. Management involves stabilizing the injury by clipping the arrow shaft to about four inches from the skin and ensuring the arrow remains stabilized during transport. Removal should only occur in an operating room to prevent further harm.
Hunters can reduce the risk of injuries

Oak Hill Trailhead-Photo captured by Negin Ceraolo
by following these guidelines:
• Select sturdy, rough-barked trees, such as oak trees, for climbing.
• Avoid carrying equipment with both hands while climbing.
• Keep firearms unloaded and broadheads covered during climbs.
• Use a harness or climbing belt at all times.
• Replace weak or worn lumber on treestands.
• Avoid putting weight solely on a single branch. Secure hands and feet before reaching for new holds.
• Clear logs and upturned branches from areas beneath treestands.
• Follow the manufacturer’s instructions when installing commercial treestands.
• Wear non-skid footwear to prevent slipping in wet or icy conditions.
• Ensure firearms are clean and loaded with the correct ammunition; inspect arrows for defects.
• Wear bright orange clothing to enhance visibility and avoid accidental shootings.
• Carry a whistle, flashlight, cell phone, and first aid kit while hunting. As hunting grows in popularity across the United States, it is vital to recognize the associated risks and injuries. This awareness can guide effective management for injured patients and help hunters take necessary precautions to improve safety.


Dr. Ceraolo is an emergency medicine resident at Cleveland Clinic Akron. She is active on X: @neginkh74
Dr. Watkins is core faculty at Cleveland Clinic Akron General and an assistant professor of emergency medicine at Northeast Ohio Medical University. He serves as division head of wilderness medicine and teaches through the track and elective, the local wilderness life support in the medical professional program, and the Cuyahoga Valley Wilderness Medicine Conference. He is a member of SAEM’s Wilderness Medicine Interest Group.

By Kailee M. Pollock, PharmD and Kevin Watkins, MD, on behalf of the SAEM Wilderness Medicine Interest Group
Of the thousands of mushroom species that exist, only about 100 are toxic to humans. Although rare, mushroom toxicity can occur due to improper identification, harvesting, storage, or preparation. This review focuses on neurotoxic mushrooms, highlighting the symptoms, identification, and treatment approaches.
While symptoms often overlap, recognizing distinct presentations is essential for guiding identification and appropriate treatment. In general, Poison Control should be involved and treatment modality of these toxidromes is largely guided by symptoms. Charcoal
may be considered if presentation is within an hour of ingestion and the patient is without significant risk for aspiration. Intravenous fluids, electrolyte replacement, and antiemetics are commonly used treatments. For agitation, patients may need benzodiazepines, and intubation may be required in severe cases, although respiratory failure is uncommon. Atropine is frequently recommended for muscarinic ingestions but should be reserved for more severe cases of bronchorrhea or bradycardia. Some neurotoxic mushrooms also contain isoxazole toxins, which can worsen encephalopathy when treated with atropine.

Inocybe spp. (Fiber Heads)
Inocybe species are a large genus of mushrooms found in temperate and tropical areas of the Northern Hemisphere. These small mushrooms typically have brown, conical caps that appear
fibrous with a prominent central umbo (protuberance). They are often misidentified as edible mushrooms, leading to poisoning. The main toxin, muscarine, modulates parasympathetic receptors that affect muscles, glands, the heart, pupils, and the central nervous system (CNS). Symptoms may present 20-30 minutes after ingestion and last for several hours.

Clitocybe spp. (Funnel Caps)
Clitocybe species, often found in lawns and wood chips from summer to fall, have whitish tan to gray caps that may turn upwards to form a funnel shape with maturity. The gills run down the stalk. Toxicity is similar to that of Inocybe mushrooms.

Amanita muscaria (Fly Agaric)
Found throughout the temperate and boreal regions of the United States, particularly on the forest floor in the fall. Amanita muscaria has a distinctive, white-spotted red cap with white gills underneath, although there are variations in cap color. The stalk is white and brittle with a bulb-like base. Despite common belief, it contains only small amounts of muscarine. The primary toxicity often arises from isoxazole compounds, such as muscimol and ibotenic acid.

Amanita pantherina (Panther Cap)
This mushroom has a white-spotted brown cap and free gills and grows on the forest floor in the fall. It is sometimes ingested intentionally for its hallucinogenic effects. The toxins in Amanita pantherina include muscimol, a gamma-aminobutyric acid (GABAA) receptor agonist, and ibotenic acid, a N-methyl-D-aspartate (NMDA) receptor antagonist. Symptoms include dizziness, sedation, nausea, weightlessness, ataxia, dysphoria, visual and colored hallucinations, space disorientation, agitation, fasciculations, seizures, and coma. Onset of toxidrome can appear within a couple of hours and last up to 12 hours, although hospitalizations and fatalities are rare.
Psilocybin
Psilocybin and Psilocin
Psilocybin and psilocin, the active compounds in certain hallucinogenic mushrooms, primarily affect serotonin receptors, leading to hallucinations. Symptoms include visual and auditory hallucinations, ataxia, paranoid delusions, disorientation, agitation, anxiety, increased empathy, mystical experiences, and derealization. Additional signs include tachycardia, dilated pupils, and dysuria. Patients may later become lethargic. Severe reactions can lead to seizures and respiratory failure.
For an in-depth examination on psilocybin and psilocin exposure, see the “Ask the Pharmacist” article on page 64

Psilocybe spp. Wikimedia. Accessed 2024.
Psilocybe spp. (Magic Mushrooms)
The entire mushroom contains psychoactive compounds, with the highest concentration found in the cap. Potency varies depending on the specific species, but the genus as a whole shares similar morphological characteristics. These mushrooms grow throughout much of the U.S. and can be difficult to identify as they are often mistaken for other "little brown mushrooms." Psilocybe mushrooms are small, yellow-brown fungi with hygrophanous (waterabsorbing) caps, and their spore prints range from purple to brown in color. When bruised, they may exhibit a characteristic blue staining reaction. While their psychoactive effects typically cause hallucinations, the potential for lethal ingestion is extremely low. Lethal outcomes usually result from misidentification, rather than acute toxicity.

Panaeolus cyanescens. Wikimedia. Accessed 2024.
Panaeolus cyanescens (Blue Meanie)
Found in wood substrate in parts of the U.S, including Alabama, California, Hawaii, Florida, Kentucky, Louisiana, Mississippi, North Carolina, Tennessee, and Texas, Panaeolus cyanescens has a cap and long stripe that is brown when immature and becomes off-white or gray with greenish-blue bruising. The gills are continued on Page 113

continued from Page 111
mottled with purple-black spores and show an adnexed attachment. It is known for being one of the most potent recreational psilocybin mushrooms in North American, and it is widely pursued for recreational use in areas of natural growth.
Gymnopilus spp.
Many members of the Gymnopilus spp. contain psilocybin. Typically found growing in clusters on wood chips in pine and coniferous forests, these mushrooms have a rusty-red cap and spore prints. Their stems are orange-brown, and they lack rings. The gills are adnate and yellowish with rusty-red coloring toward the center. The smell is fruity but the bitter taste often deters consumption.
Pannaeolina spp.
These small mushrooms are commonly found in lawns and contain psilocybin. They have a brown, hemispherical cap with sootblack gills, which are attached to a cylindrical brown stem. The spore print is jet black. They grow on compost piles and fertilized lawns and grow throughout the U.S., particularly in California where they are the most common psilocybin mushroom.

Pluteus spp.
Found in eastern North America on wood, these mushrooms have hemispherical caps that range from brown to gray with darkened centers. Their gills are crowded and pinkish, and the stipes are white, occasionally with some other coloration. When bruised, they exhibit a blue staining reaction.

This small, white mushroom has a thin flesh that becomes yellow as it ages. It resembles oyster mushrooms, but unlike the oyster mushroom, it has no stalk. It grows on conifer wood in the Pacific Northwest during the fall. Previously considered edible, it is now known to cause fatal encephalopathies in individuals with end-stage renal disease. Symptoms can appear up to 31 days after consumption and include dysarthria, ataxia, paralysis, seizures, and myoclonus. The toxin has yet to be definitively identified.

distress, followed by ataxia, blurry vision, and purple urine, as well as occasional liver or renal abnormalities. Symptoms appear 4-6 hours or more after ingestion.

Morchella spp. Wikimedia. Accessed 2024.
Morchella spp. (Morel Mushrooms)
Found in groups in wooded areas in North America from March to June, morels are conical, honeycombshaped mushrooms with vertical ridges and hollow white stems. Although typically safe to consume, these mushrooms must be properly cooked. This species contains hydrazine which is eventually metabolized to N-methylhydrazine subsequently depleting GABA. Raw or undercooked morels contain hydrazine toxins, which cause cerebellar syndrome, including ataxia, dizziness, tremors, dysarthria, nystagmus, and disorientation. Cooking destroys the toxin, making the mushrooms safe for consumption.
This fan-shaped mushroom, with a brownish-orange cap, grows on dead wood of deciduous trees. It has a sweet odor and taste and contains polyprotic acid. Potassium hydroxide (KOH) can be used for identification as fruit bodies will stain bright violet if a drop is applied. The toxin can cause “neurotoxic delayed syndrome” that presents with gastrointestinal


Dr. Watkins is core faculty at Cleveland Clinic Akron General, where he serves as director of wilderness medicine and is ultrasound faculty. He is also vice chair of the SAEM Wilderness Medicine Interest Group and a WLS-MP instructor. Dr. Pollock is an MS3 at Ohio Heritage College of Osteopathic Medicine and a clinical pharmacist at Cleveland Clinic Akron General. She is also involved in the research committee for the Wilderness Medical Society and a WLS-MP instructor.
Each year at SAEM’s Annual Meeting, Annual Alliance donors are invited to the SAEMF Donors’ Coffee & Networking Session where they learn first-hand about the important role they play in readying tomorrow’s emergency medicine researchers and educators. During SAEM24, Dr. Di Coneybeare, who received the 2023 SAEMF Education Project Grant, shared:
“As part of my own professional identity, I feel that this grant has been transformative. Of all the things I consider myself to be, an educator, a clinician, a Fellowship Director – I had never really considered researcher to be a part of that equation. But now, since working on this project together, it has really inspired a list of possible future publications, as well as subsequent grants – the most ambitious of which is potentially applying to HRSA for their burnout and resiliency studies. Thank you all for your generosity. This grant has turned out to be the gateway to a lifetime career of research.”
— Di Coneybeare, MD, MHPE Columbia University Vagelos College of Physicians and Surgeons

When you become a 2025 Annual Alliance donor, you not only contribute to advancements in emergency care but also unlock exclusive benefits that express our deepest thanks for your commitment. Some of the benefits most valued by Annual Alliance members are those they receive at the SAEM Annual Meeting, such as:
• Recognition on the prestigious Digital Donor Display
• Exclusive invitation to SAEMF’s Coffee and Networking Event
• VIP Lounge Access
• Sedan transportation from the airport
who are passionate about improving emergency care. As a member of the Annual Alliance, you will be a part of an esteemed network of leaders in emergency medicine who strive to advance emergency medicine! Donate Now!
• Recognition varies by donor level. A gift of any amount will lead to donor recognition.
Submit Your Academy Award Nominations!
Each year SAEM’s academies present awards in recognition of excellence and achievement in their respective fields of interest. For details and qualifications, visit our academy award webpages and nominate yourself or a colleague you admire for one of these honors. The deadline for nominations is February 7, 2025. Note: to be eligible for an award, a nominee must be a member of the presenting academy. Join an academy for free at any time during the year.
A Warm Welcome to Our New Members!
We’re delighted to welcome our newest members to the SAEM family. Below are those who’ve recently joined our community. Welcome!
• Military Members
• Faculty Members
• Medical Student Members
• Administrative Associates
• YP1 Members
• YP2 Members
• Administrative Members
• Pharm Student Members
• Pharm Resident Members
• Excellence Award Winners
• Fellow Members
• Pharmacist Members
• Resident Members
Announcing Two Exciting Opportunities for Aspiring EM Editors!
Applications are currently being accepted for resident and fellow editor positions for SAEM’s two peer-reviewed journals. This is a unique opportunity for mentorship and hands-on experience in peer review, editing, and the journal publishing process.
• AEM Resident Editor: Apply by Monday, February 3, 2025
• AEM E&T Fellow Editor: Apply by Monday, February 17, 2025
Don’t Miss These SAEMF Funding Opportunities!
Emergency Medical Foundation (EMF)Society for Academic Emergency Medicine Foundation (SAEMF) Medical Student Research Grant in Memory of Dr. Amy H. Kaji — Up to $5,000. This grant offers up to four medical students early exposure to emergency medicine (EM) research, along with skill-building and networking opportunities through the EMF-SAEMF Grantee Workshop. Apply by 5 p.m. CT, January 10, 2025.
SAEMF Emergency Medicine Interest Group Grant (EMIG) — $500 grants that support emergency medicine interest groups (EMIGs) in advancing medical student education, fostering innovative educational
methodologies in undergraduate education, and enhance EMIG-led activities. Apply by 5 p.m. CT, January 31, 2025.
GEMSSTAR for Emergency Medicine Supplemental Funding Program — $25,000 The National Institute on Aging Grant for Early Medical/Surgical Specialists’ Transition to Aging Research (GEMSSTAR) is funded through an NIA R03 small research project grant. Investigators may include a Professional Development Plan (PDP) alongside the R03, supported by non-R03 funds. To support emergency medicine GEMSSTAR applicants in their PDP, SAEMF and EMF jointly established the GEMSSTAR for Emergency Medicine Supplemental Funding Program, with a separate application process from the NIA R03. Apply by 5 p.m. CT, February 15, 2025.
Early bird registration is open for SAEM25, to be held May 13-16, 2025, in Philadelphia, Penn. SAEM25 promises a robust educational lineup, with in-depth workshops, enriching didactic sessions, pioneering research, focused forums, and more. The meeting is a hub for mentorship, networking, and collaboration, bringing together EM professionals at all career stages to form connections that shape their personal and professional paths. Join us for the academic EM event of the year! Discover more and register today!
Now Open: SAEM25 Housing, and Childcare. These fill fast, so act now!
The SAEM Residency & Fellowship Fair provides a streamlined, cost-effective recruitment opportunity, reaching hundreds of potential candidates in a single event, saving you valuable time and resources. The fair encourages interactive discussions for candidates to ask questions, gain program insights, and make informed decisions, helping you assess their suitability more clearly. Learn more and register your program today!
Round up your crew and get in on the friendly competition by signing up for these SAEM25 team activities:
• Simulation Academy SimWars — the ultimate national simulation competition just for EM residents.
• SonoGames® — a competitive, games-based educational event focused on pointof-care ultrasound.
• Dodgeball — emergency medicine residency teams from all over the battle it out in this classic playground game with a grownup twist.
• SAEM RAMS Hunt — residency teams engage in patient care challenges related to sex, gender, and diversity at local landmarks, concluding with a networking event featuring complimentary food and drinks.

Susan Hoffert, MD, has been named the first woman to receive emeritus status in the Indiana University School of Medicine Department of Emergency Medicine. Since joining the faculty in 2001, Dr. Hoffert has had an exemplary 23-year career in pediatric emergency medicine. Over the past two decades, she has provided critical care to tens of thousands of children and mentored more than a thousand medical students, residents, and fellows in the field of pediatric medicine.

Ron Stewart, MD, a founding member and first president of the National Association of EMS Physicians (NAEMSP) has passed away.
Dr. Stewart’s groundbreaking work in emergency medicine and paramedicine has had a lasting global impact. After earning his medical degree from Dalhousie University, Dr. Stewart advanced paramedicine in California as Los Angeles County’s first paramedic director. He later founded the Center for Emergency Medicine at the University of Pittsburgh, revolutionizing paramedic training. As health minister in Nova Scotia, he transformed the province’s emergency medical services.
Dr. Stewart’s legacy includes significant contributions to education and research, including a $1.3 million donation to Dalhousie Medical Research Foundation. He received numerous honors, including the James O. Page Award and the Companion of the Order of Canada.

David Hancock, PhD, instructor of gerontology in emergency medicine at Weill Cornell Medicine, has received a K01 grant for $644,319 over five years to support his research, "The EM-AD: A Novel Measure of Elder Mistreatment Among Dementia Family Caregivers". This funding will advance Dr. Hancock's work on elder mistreatment in caregiving settings, a critical issue affecting both patients and families. His research aims to improve the understanding and identification of mistreatment, offering valuable insights to the fields of emergency medicine and gerontology.

Hal J. Minnigan, MD, PhD, retired this fall from his position as assistant professor of clinical emergency medicine in the Indiana University School of Medicine Department of Emergency Medicine, after more than 20 years. Throughout his career, Dr. Minnigan has been an influential figure in both the Wishard Memorial Hospital and Sidney & Lois Eskenazi Hospital emergency departments. His commitment to providing residents with a well-rounded education and his steadfast advocacy for the resources that patients deserve have left an indelible mark on the institutions he served.

Eugenia South, MD, MSHP, Ralph Muller Presidential Associate Professor at the Perelman School of Medicine and associate vice president of health justice at the University of Pennsylvania Health System. Dr. South was recognized for her leadership in developing and testing interventions to dismantle structural racism and prevent firearm injury in Black neighborhoods. As faculty director of the Center for Health Justice at the University of Pennsylvania, she has made transformative contributions to advancing health through the lens of racial, environmental, and economic justice.

Gregory L. Henry, MD, a respected educator, leader in emergency medicine, and past president of ACEP, has passed. His career spanned decades of mentorship, teaching, and advocacy. Dr. Henry’s passion for patient safety and risk management, along with his storytelling ability, made him a memorable speaker and teacher.
Dr. Henry served as ACEP president (1995-96) and held multiple leadership roles, including as a Board member and chair of the Long Range Policy Committee. He received ACEP’s John G. Wiegenstein Leadership Award in 1998 for his outstanding contributions.
He was a clinical professor at the University of Michigan and chief of emergency medicine at Oakwood Hospital. Author of several books and articles, Dr. Henry also served as a consultant and speaker on health policy and risk management. He was active in numerous medical organizations throughout his career. Dr. Henry was a longtime member of our SAEM community.
President: Becky McGowan, MBA
Board Liaison: Julianna J. Jung, MD
The Academy of Administrators in Academic Emergency Medicine (AAAEM) supports professionals managing the administrative and business functions of academic emergency medicine departments, including patient care, education, research, and residency program administration.
• The Academy of Administrators in Academic Emergency Medicine (AAAEM) Benchmark Committee is collecting data for the FY24 academic year to support its annual benchmark surveys. These surveys evaluate the clinical, education, and research missions of academic emergency medicine departments and divisions. For questions or assistance with submitting your organization’s data, contact Alyssa Tyransky at alyssa.tyransky@osumc. edu. Preliminary results from the FY24 data collection will be available at the AAAEM booth during SAEM25 in Philadelphia this May. Stop by to learn more about the surveys and AAAEM.
President: Katie Hunold Buck, MD
Board Liaison: Michelle D. Lall, MD, MHS
The Academy for Geriatric Emergency Medicine (AGEM) focuses on improving emergency care for older patients. It advances research, education, and faculty development, serving as a unified voice for professionals in geriatric emergency medicine and addressing related challenges.
• Save the date for the next AGEM webinar, “Career Longevity in Academic Emergency Medicine,” on March 6, 2025, at 6 p.m. CT. In partnership with AWAEM, this engaging session features a panel of late-career academic emergency medicine physicians sharing their personal journeys, strategies for avoiding burnout, and practical tips for building a fulfilling, enduring career in this challenging field.
• Do you know someone who has made significant contributions to geriatric emergency medicine? Nominate yourself or a colleague for an Academy of Geriatric Emergency Medicine (AGEM) award! Nominations are open for the Gerson-Sanders Award, Academic Career Achievement Award, Education Career Achievement Award, Mentorship Award, and Early Career Achievement Award. Details are available here. Please note: except for the GersonSanders Award, nominees must be AGEM members (membership is free!).
• Attention medical students, residents, and fellows! The Academy of Geriatric Emergency Medicine (AGEM) offers an AGEM Geriatric EM Away Rotation Scholarship (for medical students and residents) and Annual Meeting Scholarships (for medical students, residents, and fellows). Applicants must be AGEM members (membership is free!). For details, including application information and deadlines, visit our webpage.
Chair: Alyssa Valentyne, MD
Board Liaison: Daniel N Jourdan, MD, NRP
The Climate Change and Health Interest Group at SAEM tackles the intersection of climate change and public health, focusing on research, education, and advocacy. It promotes sustainable practices and policies to mitigate climate-related health impacts through a multidisciplinary approach.
• The remaining meetings for our interest group are scheduled for January 9 and March 27 at 12 p.m. CT via Zoom, with an in-person meeting at SAEM25 in Philadelphia, May 2025. All are welcome to attend!
• The SAEM Climate Change and Health Interest Group has been actively developing climate health curricula. Members have submitted SAEM didactic proposals, and the group is working on American Board of Emergency Medicine certification modules focused on climate-related diseases.
Chairs: Samuel Sondheim, MD, MBA and Marta Rowh, MD, PhD, MPH
Board Liaison: Nicholas M. Mohr, MD, MS
The Disaster Medicine Interest Group advances the science and practice of disaster medicine by supporting research, publishing findings, and providing expert guidance on disaster preparedness and response. The group focuses on improving Mass Casualty Incident (MCI) readiness and addressing challenges in emergency department response amid high boarding volumes.
The SAEM Disaster Medicine Interest Group (DMIG) proudly recognizes members who recently contributed to disaster response efforts:
• Charles B. Kemmler, MD, PhD, FACEP, FAAEM (University of Pennsylvania): Deployed to Hurricanes Helene and Milton.
• Nicholas E. Kman, MD, FACEP (OSU Wexner Medical Center): Deployed to Hurricanes Helene and Milton for 21 days.
• Shira A. Schlesinger, MD, MPH, FACEP, FAEMS (Harbor-UCLA Medical Center): Deployed to Hurricane Milton.
• Douglas Char, MD (Washington University): Deployed to Hurricanes Debby, Helene, and Milton. Thank you for your service and dedication!
Chair: Jennifer Mitzman, MD
Board Liaison: Ryan LaFollette, MD
The Pediatric Emergency Medicine Interest Group aims to enhance pediatric emergency care by advancing science and education. Its mission focuses on improving care through training, education, and fostering collaboration between general and pediatric emergency medicine specialists.
• The SAEM Pediatric Emergency Medicine Interest Group meets on the third Wednesday of each month at 2 p.m. CT and will hold an in-person meeting at SAEM25 in Phildelphia, May 2025 .
• Award nominations will soon open for the Nate Kuppermann Mentor in Research Award, the Marianne Gausche-Hill Mentor in Education Award, and the 2025 Rising Star Award (for those less than seven years out from training). Nominations are due by March 1, 2025. Details will be shared via the community listserv. Nominees must be active SAEM members.
Chairs: Rebecca Barron, MD; Ynhi Thomas, MD
Board Liaison: Pooja Agrawal, MD, MPH
The Sex and Gender in Emergency Medicine Interest Group aims to highlight the impact of patient sex and gender on emergency care. Its mission is to integrate these concepts into emergency medicine education and research, raising awareness and improving care delivery.
This past year, particularly during the SAEM annual meeting, was an active and productive time for the SGEM Interest Group.
• RAMS Hunt: For the third consecutive year, Dr. Jeannette Wolfe led the RAMS Hunt, a scavenger hunt cosponsored by ADIEM, AWAEM, the SAEM SGEM Interest
Group, and RAMS. Teams of three residents completed sex- and gender-related challenges at Phoenix landmarks before gathering at a local restaurant to connect with residents and faculty, including SGEM experts. Prizes were awarded for best time, team name, and T-shirt.
• Pre-Meeting Workshop: Dr. Ynhi Thomas, co-led the workshop Breaking Through the Glass Ceiling: Networking Best Practices for Women in Emergency Medicine. Focused on advancing women in academic emergency medicine, the session covered networking, mentorship, and the impact of sex, gender, race, and ethnicity on career progression. Participants engaged in presentations, group activities, and discussions aimed at fostering career development and leadership.
• Gender-Based Violence Didactic: Dr. Rebecca Barron moderated Future Directions in Gender-Based Violence Research, co-sponsored by ADIEM, AWAEM, and the SAEM Social Emergency Medicine and Population Health Interest Group. The expert panel discussed sexual assault, intimate partner violence, immigrant and refugee health, traumainformed care, and cultural considerations in research.
• Race, Ethnicity, Sex & Gender Data Didactic: Former SGEM chair Dr. Angela Jarman participated in Best Practices for Collecting and Reporting Race, Ethnicity, Sex & Gender Data, cosponsored by ADIEM and the SAEM Research Committee. Dr. Jarman presented on best practices for collecting sex and gender data and joined a panel discussion to guide participants in developing effective data collection strategies.
Wilderness Medicine
Chair: Joshua Timpe, MD
Board Liaison: Ali S. Raja, MD, DBA, MPH
The Wilderness Medicine Interest Group at SAEM brings together emergency physicians to address the challenges of medicine in wilderness and austere environments. It fosters research, education, and collaboration on topics like outdoor injuries and environmental emergencies, enhancing skills for resource-limited settings.
• Throughout the year, the Wilderness Medicine Interest Group will post questions across all major social media platforms. Follow along on your preferred platform, stay sharp, showcase your knowledge, and post your response! A prize will be announced at SAEM25.

POST YOUR OPEN JOBS IN FRONT OF OUR QUALIFIED CANDIDATES!
Accepting ads for our “Now Hiring” section!
Deadline for the next issue of SAEM Pulse is February 1.
For specs and pricing, visit the SAEM Pulse advertising webpage.

Leverage our many diverse sponsorship options to maximize your presence, build brand awareness, and connect with emergency medicine leaders both in and beyond the conference.
Hosting a 50-minute symposia is a great way to showcase your expertise, and drive business growth through valuable connections and exposure, and share your company’s latest products and services with engaged thought leaders.

13-16,


About Us: Penn State Health is a multi-hospital health system serving patients and communities across central Pennsylvania. We are the only medical facility in Pennsylvania to be accredited as a Level I pediatric trauma center and Level I adult trauma center. The system includes Penn State Health Milton S. Hershey Medical Center, Penn State Health Children’s Hospital and Penn State Cancer Institute based in Hershey, Pa.; Penn State Health Hampden Medical Center in Enola, Pa.; Penn State Health Holy Spirit Medical Center in Camp Hill, Pa.; Penn State Health Lancaster Medical Center in Lancaster, Pa.; Penn State Health St. Joseph Medical Center in Reading, Pa.; Pennsylvania Psychiatric Institute, a specialty provider of inpatient and outpatient behavioral health services, in Harrisburg, Pa.; and 2,450+ physicians and direct care providers at 225 outpatient practices. Additionally, the system jointly operates various healthcare providers, including Penn State Health Rehabilitation Hospital, Hershey Outpatient Surgery Center and Hershey Endoscopy Center.
We foster a collaborative environment rich with diversity, share a passion for patient care, and have a space for those who share our spark of innovative research interests. Our health system is expanding and we have opportunities in both academic hospital as well community hospital settings.

Benefit highlights include:
• Competitive salary with sign-on bonus
• Comprehensive benefits and retirement package
• Relocation assistance & CME allowance
• Attractive neighborhoods in scenic central Pennsylvania



May 13-16, 2025 | Philadelphia Marriott Downtown