Academic Career Guide



 By Brian J. Zink, MD, Sr. Associate Chair of Education and Faculty Development, University of Michigan, Ann Arbor, MI.
By Brian J. Zink, MD, Sr. Associate Chair of Education and Faculty Development, University of Michigan, Ann Arbor, MI.
In 1961 four general practitioners, led by James Mills, Jr, MD gave up their private practices and established a contract with Alexandria Hospital to become the first full-time emergency physicians in the U�S� Their Alexandria Plan model met some opposition but was soon a huge success, with patients and community physicians rallying around the four mavericks The Alexandria Plan garnered a great deal of attention from the world of medicine, the public, the media, and many physicians who wished to replicate the Alexandria Plan in their own hospitals� Within five years a number of Alexandria-type groups had sprung up across the country
By the end of the decade, emergency physicians began to organize The first steps were taken in Michigan in 1968 where John Wiegenstein, MD, a general practitioner who was working in an Alexandria Plan-like group in Lansing, sought to bring emergency physician colleagues together to develop and deliver educational programs to cover their knowledge and procedural gaps Wiegenstein collected eight physicians in Lansing in August 1968, and they boldly
called themselves the American College of Emergency Physicians (ACEP)� A few months later, a national meeting was held in Virginia that attracted about 40 physicians, and the collected physicians decided to join the Michigan ACEP group and create a national ACEP organization, with John Wiegenstein elected as the first President ACEP grew exponentially in its first 5 years The first national educational meeting, called the “Scientific Assembly,” was held in 1969 in Denver, CO�
The academic development of emergency medicine (EM) lagged about a decade behind the initial clinical practice In the academic world the three established pillars for success were advanced clinical care, education, and research Emergency medicine was becoming credible in the clinical arena as a new form of practice by the late 1960’s and had a growing national specialty organization in ACEP� However, it had no accredited residency training programs or any significant foothold in medical schools or academic medicine Research by emergency physicians in the fledgling field was also non-existent�

Most early emergency physicians did not have full training for the diverse practice that they encountered in emergency departments (EDs) The need for additional education was recognized by the early leaders of emergency medicine, and the earliest attempts to address this were from ACEP continuing medical education programs At Massachusetts General Hospital (MGH), a fellowship in emergency medicine was offered out of the internal medicine department in the late 1960’s It consisted of two weeks of didactic and procedure sessions, and work in the MGH ED The early emergency physicians who completed the program were thus able to say that they had “done a fellowship in emergency medicine at the MGH!”
The first institution to embark on residency training in emergency medicine was the University of Cincinnati, where a young internist named Herbert Flessa was assigned to manage the emergency room at Cincinnati General Hospital Flessa needed to put more bodies in the busy ED where no one else really wanted to work, and decided to apply for a residency training program� He applied to the American Medical Association in 1969 and was approved to start a 2 year residency in 1970� The test case for this new residency was Bruce Janiak, MD, a Cincinnati medical student with a developing interest in emergency medicine Janiak played a big role in developing his own residency curriculum and became the first emergency medicine resident� His training was largely unsupervised in the emergency department (ED), and consisted mainly of various rotations on other services where he did consults and managed patients in the ED Janiak, was successful, and the residency took off with 5 members in the next class

Other emergency medicine residencies quickly sprung up at Medical College of Pennsylvania, led by David Wagner, MD, a pediatric surgeon, and at the Los Angeles County + University of Southern California Medical Center where Gail Anderson, MD, an obstetrician/gynecologist negotiated to form the first academic department of emergency medicine in 1971 Other early residencies were founded by anesthesiologist Donald Thomas, MD, at University of Louisville, and by surgeon Peter Rosen, MD, at the University of Chicago� Rosen became a prominent mentor and developer of early academic leaders at Chicago, and later at Denver General Hospital� By 1975, over 30 new emergency medicine (EM) residencies had been born Most of these were in the American Midwest, and were usually not at the most prestigious medical schools or teaching hospitals The traditional academic powerhouses in medicine would be reluctant to accept the new EM practices for 2 more decades
The early EM residents had no certifying board in emergency medicine, and therefore lacked that level of distinction in the house of medicine� Despite this, they were highly employable in a wide-open job market Many EM residency graduates could go directly from training to lucrative positions as medical directors of hospital ED’s� Importantly, some of them stayed at their training hospitals and became the first true academic emergency physician faculty members�

As the early residencies were forming, a parallel process of academic development was happening in some university hospitals and medical centers� It was common in these teaching hospitals for junior academic surgeons to be assigned to oversee the ED The academic EDs were typically staffed by residents from various services, with minimal attending physician supervision The origins of the first academic organization in emergency medicine, the University Association for Emergency Medical Services (UA/EMS), can be traced to initial meetings of a few surgeons in 1968 and a charter meeting in 1970 at the University of Alabama in Birmingham where 138 participants came, representing 96 of the 119 U�S� and Canadian medical schools� An organizational caucus was held later in 1970, and surgeon Charles Frey, MD of the University of Michigan was elected the first UA/EMS President By 1972, UA/EMS had leased management services from the early ACEP organization, but was not closely linked to ACEP in terms of mission or ideology
From 1970-1975 UA/EMS was dominated by surgeons who worked at institutions that did not have EM residency programs The group was not initially supportive of the development of EM residencies, or of EM as a new medical specialty� Eventually, three surgeons who had started residencies, David Wagner at Medical College of Pennsylvania, Ronald Krome at Detroit Receiving Hospital, and Peter Rosen at University of Chicago became UA/EMS members and began to change the dynamic in the organization to be less surgical and more EM oriented When Wagner became President of UA/EMS in 1976, one of the first things he did was change the name to the University Association of Emergency Medicine This was a symbolic shift that moved the organization toward supporting EM residency training, academic departments of EM, and specialty status The legacy of the early surgeons in UA/EMS and later UAEM was that they drew attention to emergency care as an area of medicine that had been neglected, and stimulated academic centers to at least acknowledge the growing patient volume and lack of an organized approach to caring for this diverse group of patients�
The academic development of emergency medicine would not have continued if EM had not become established as the newest medical specialty by the AMA and the American Board of Medical Specialties (ABEM)�

Opposition to EM as a specialty from existing boards and specialties was intense For example, a landmark 1973 meeting hosted by the American Medical Association (AMA) in Chicago, the Conference on Education of the Physician in Emergency Medicine, drew together all the major stakeholders in medical specialties, government, and hospitals and had contentious debates on the value of EM residency training, who should teach EM, and the need for a specialty of emergency medicine� The “Blue Book” proceedings of this meeting eventually did endorse residency training and movement toward a specialty, but a strong opposition still existed
For many of the more maverick early EM residency graduates, the creation of a specialty board was not a high priority� However, the more senior leaders who had established emergency medicine believed the field could succeed only if it had specialty status� The process was complex and difficult The first step was to incorporate as a non-approved board� Thus, the American Board of Emergency Medicine (ABEM) was established in 1976 out of ACEP and UAEM Next the early leaders had to prepare a certifying examination, and then apply to the American Medical Association (AMA) and American Board of Medical Specialties (ABMS) in a 12 step approval process� The ABEM leadership team consisted of pioneers like James Mills, Jr, John Wiegenstein, and R R Hannas, as clinical practitioners, along with Peter Rosen, Gail Anderson, David Wagner, George Podgorny, and Ron Krome, who were more academically oriented After a year of toil and negotiations, the EM leaders felt that they would be successful in the ABMS delegation vote for ABEM approval� They were very wrong, as ABMS voted down ABEM 100 to 5
Some of the opposition to EM as a specialty came from academic leaders in other fields who were concerned about competition for training on ED patients, a fear that medical students would choose emergency medicine over the established disciplines, and loss of revenue as the academic pie would be proportionately smaller with a new member in the mix Eighteen months of intense, politically charged negotiations ensued where the EM leaders compromised by allowing other specialties to have seats on the ABEM board in return for their support Finally, in September of 1979, the ABMS approved ABEM as a “modified conjoint board,” and emergency medicine became the 23rd US medical
specialty� The jubilation of the founders of the field was mixed with the realization that a true specialty now needed to emerge, with a strong academic and practice base, a new certifying exam, a residency review process, and active participation in the house of medicine
Another academic organization, The Society for Teachers of Emergency Medicine (STEM) was created out of ACEP in 1975 as a “paper organization” to gain access to the Council of Academic Societies (CAS) in the American Association of Medical Colleges (AAMC) STEM was initially led by Robert Dailey, MD, who was a wellknown West Coast residency leader, and Peter Rosen, MD STEM was primarily engaged in issues relating to residency and medical student education� Many early academicians were members of both UAEM and STEM�
The early academic leaders of UAEM and STEM, as well as those who were promoting specialty development, realized that conducting research was an important part of becoming a credible academic field in the world of medicine� None of the founders of the field had any background or expertise in research, but at a few of the early academic residency sites, faculty members began to conduct research in emergency medicine� Blaine White, at Detroit Receiving Hospital and James Niemann, at the University of California at Los Angeles Harbor Medical Center were doing animal and cellular research in resuscitation In Cincinnati, William Barsan, Steven Dronen, Edward Otten, James Roberts, and Michelle Biros were doing hemorrhagic shock, resuscitation, and toxicology research� In Pittsburgh, where the famous resuscitation research laboratory of anesthesiologist Peter Safar was based, emergency physicians Ronald Stewart, Norman Abramson, Donald Yealy created a hot bed of airway, cardiac and brain resuscitation and emergency medical services research� One of the first EM researchers to gain national attention with publications in major medical journals was Gabor Kelen, MD from Johns Hopkins University� Kelen was in the midst of a burgeoning HIV epidemic in Baltimore, and did landmark work on HIV recognition and testing in ED patients� This early group of EM researchers attracted residents to their work, and eventually established fellowships to formally train emergency physicians in research theory and methods By conducting and publishing quality research and eventually competing successfully for federal research grants, emergency medicine gained desperately needed credibility in the world of academic medicine at a time when many were skeptical of the scholarly basis for the new field
Academic emergency medicine evolved rapidly across the US in the 1980’s� The number of residencies mushroomed, and medical schools increasingly formed clerkships or electives in emergency
medicine� Emergency medicine was the first field to mandate 24 hour attending physician supervision of residents� Emergency physicians began to develop as administrative leaders in medical schools, hospitals, and national medical organizations
By 1989, ABEM had enough of a foothold in the house of medicine to be officially approved as a primary board by ABMS Also in 1989, UAEM and STEM merged to form the Society for Academic Emergency Medicine (SAEM), which became the leading academic organization for the specialty
The 21st century has been a time of tremendous growth in academic EM� In 1970 there were no EM residencies – now there are over 230, with over 2,400 positions offered in the match each year� In 1970 there were no academic departments of emergency medicine, now there are at least 85 EM has become a popular career choice for US senior medical students� Only internal medicine and pediatrics match more US seniors than emergency medicine (www�nrmp�org)�
Education was the driver for academic development in EM The innovations of EM in bedside teaching, new learning methods, and national engagement in medical education have been considerable� More recently, academic emergency physicians have played an increasing role in medical student education through EM clerkships or electives, and more generally in curriculum development, and positions in the dean’s office For post-residency education, more and more fellowships are available for EM residency graduates
The research realm has also blossomed for EM in the past decade� EM investigators are increasingly receiving National Institutes of Health (NIH) or major foundation funding in resuscitation, acute cardiac care, shock, neurological emergencies, and injury prevention� Emergency physicians lead large NIH-funded network trials in stroke and shock� In 2012 the NIH created the Office of Emergency Care Research to promote, foster and coordinate emergency medicine research, and named researcher Jeremy Brown as the first Director�
In less than half a century, emergency medicine has progressed from being a novel medical practice by largely untrained physicians, to become a cutting edge, academic medical specialty with challenging, innovative educational programs and innovative research� The persistence and determination of the early academic leaders to create a strong foundation for emergency medicine in the academic world has paved the way for future academic emergency physicians to be more effective teachers and investigators� The end result will be a level of high quality emergency care that will benefit patients worldwide

Emergency physicians, regardless of their practice environments, provide essential patient care at the front lines of our nation’s healthcare safety net For the purposes of this discussion, we will define the field of “academic” emergency medicine as a faculty position within a residency-training program dedicated toward the pursuit of education, research, and/or administration relating to resident learners and their patients� Conversely, “privatepractice”, commonly referred to as “community” emergency medicine, can be described as a career dedicated to the art and practice of emergency medicine outside of the residency-learning environment� Hybrid environments also exist mostly consisting of hospital sites where residents complete their rotations away from their primary teaching institution� Emergency physicians practicing in a hybrid environment will have interactions and teaching opportunities with residents though they often are not responsible for meeting scholarly requirements set forth by the primary academic institution
Upon completion of emergency medicine training, residents must make a difficult choice to enter either academic or community practice Much of this decision will ultimately depend on which aspects of the practice environments align most closely with a resident’s values and career aspirations A 2008 study demonstrated that emergency physicians who assumed leadership roles in their day-to-day practice or in organized medicine were twice as likely to report high career satisfaction as those who did not assume a leadership role (‘08 Career Satisfaction) Other associations with higher career satisfaction included: those who found their work exciting and personally rewarding, job security, fair compensation, involvement with clinical teaching, consulting, or having political involvement� Conversely, not enough time for personal life, lack of control over working conditions, lack of excitement at work, lack of job security, and lack of personal reward were all cited as reasons for low career satisfaction (‘08 Career Satisfaction)� Fortunately, both academic and private practice settings each offer unique advantages for longterm career satisfaction�
One of the major advantages for the academic physician involves the opportunity to educate residents, medical students, as well as fellow colleagues and coworkers� Academic emergency physicians also have the opportunity to travel, lecture, contribute scholarly work, perform research, and serve as training mentors for future generations of emergency physicians� Academic emergency physicians will often have scholarly requirements in addition to their clinical duties� Previously, an academic physician may have worked in an environment where he or she would have to “publish or perish” on a traditional clinical-research track� However, many institutions have created additional pathways for promotion in academic medicine in addition to the traditional clinical researcher route� A hybrid “clinical educator” promotion track, for example,
may be tailored toward a career in academic medicine with greater emphasis on medical education rather than research but this track also typically has requirements for continued scholarly activity� More recently, institutions have adopted a new purely “clinical” track that allows for advancement by mainly working clinical shifts and providing high quality bedside teaching Doctors in this latter track will have less protected time but also less scholarly requirements� Keep in mind that each academic institution has its own nomenclature and definitions for promotion tracks and it is worthwhile to gather this information from the Department Chair
Emergency physicians in private practice, on the other hand, often have a majority of their time dedicated to clinical practice� Depending on the specific practice or group, salary also tends to be relatively higher in the private practice setting compared to the academic environment� Fringe benefits vary widely amongst both academic and private practice groups The time that a private-practice physician spends non-clinically also differs from that of the academic physician with most of the time away from work available for personal activities Outside of group meetings, many community doctors are able to maintain a strong amount of flexibility with their time� However, there are certainly options for involvement outside of clinical shifts and each private group will offer various opportunities for greater investment within the group� Depending on the political structure of the group, individual physicians will be invited or encouraged to be involved outside the clinical areas in varying degrees� Potential areas of service can include administrative duties such as quality assurance, patient safety, ED operations, and providing ongoing education for the group Other important factors to consider when joining a private practice include: medical malpractice and tail coverage, physician turnover, available specialists on call, and the collegiality of the emergency department with hospitalists and medical staff�
One of the major advantages for the academic physician involves the opportunity to educate residents, medical students, as well as fellow colleagues and coworkers.
Emergency physicians in private practice, on the other hand, often have a majority of their time dedicated to clinical practice.
From a medical student perspective, it may be too early to consider an academic versus community career, however the emergency medicine-bound medical student will have a few considerations to make in choosing their residency in preparation for a future career� For instance, choosing to train in an institution with a university affiliation may afford the resident more opportunity to be involved with the training of medical students and increased access to university libraries, research librarians, and other educational facilities� Generally, training in an academic institution will give the resident greater exposure to academic faculty of all ranks and potentially greater opportunity for academic mentorship Alternatively, a community-based residency may be a better reflection of the post-residency private practice environment� All emergency medicine residencies will have variable degrees of opportunities to perform scholarly activity and seek mentorship� Another consideration in choosing residency is the 3 year versus 4 year path A resident completing a 3-year residency will have the advantage of finishing early and priming themselves for an earlier fellowship and better salary in the first year post-residency� However, the 3-year graduate may have difficulty securing an academic position at a 4-year institution in the first year out of residency given that they will be at the same postgraduate level of a fourth-year resident
Residency training is critical in the decision of whether to pursue a career in academics versus community It is important to work in as many clinical environments as possible during residency training to get a sense of the differences� If your residency curriculum does not include a broad range of training sites, consider electives and moonlighting as ways to gain experience and insight into academic versus community settings, urban versus suburban versus rural settings, and hybrid EDs� Residency is also an opportunity to seek out mentors and obtain advice from your faculty� Senior residents and alumni are often underutilized resources Residents will often change their minds multiple times between academics and community during residency so it’s prudent to keep doors open by maintaining good relationships with faculty, maintaining networks, and positioning yourself with academic pursuits
There are advantages and disadvantages to going straight into an academic job versus a community job The advantages for immediately embarking on an academic career include an earlier start on research, education or administrative pursuits and a more expedited path toward promotion You also start the transition from resident to faculty sooner and stay in a

known environment for those training at an academic program Disadvantages include lower reimbursement, more obligations and expectations outside of clinical shifts, and a lack of exposure beyond one’s own academic institution
The advantages of going into a community position straight out of residency include the opportunity to consolidate your training and “sharpen your teeth” as an emergency physician without the safety net of faculty and co-residents� The reimbursement is often higher and there is greater flexibility in schedule Disadvantages include increased expectations for patient throughput and less discussion regarding cases�
When choosing whether to pursue an academic or community position coming out of residency, keep in mind that most emergency physicians change jobs within the first 3 years of practice It is increasingly more common to switch between academics and
community practice� Making the transition from an academic to a community job is likely more feasible Making the transition from a community job into academics could potentially be more challenging due to the limited number of available academic positions and the significant amount of networking required for obtaining an academic position If you decide to pursue a community ED position but are not ready to completely rule out academics in the future, picking up per diem shifts in an academic department can help you extend the window of opportunity to transition from community to academics
Ultimately, the decision between academics and community is a very personal decision that must take into account many professional and personal factors� Picking a career that will provide you personal and professional satisfaction, opportunity for growth, joy in work, sense of camaraderie, and work-life balance will lead to the greatest chance of job satisfaction and longevity�
The SAEM Graduate Medical Education Committee would like to thank Eric Wei, MD, MBA and Allison Luu, MD for their help in editing this section.
References:
1 http://littlewhitecoats blogspot com/2011/01/academics-vs-community-practice html
2011 (Orman, Rodgers, Weingart)
2 http://www kevinmd com/blog/2013/05/emergency-physicians-burning html
3� Sanders AB, Fulginiti JV, Witzke DB, Bangs KA� Characteristics Influencing Career Decisions of Academic and Nonacademic Emergency Physicians� Ann Emerg Med� 1994 Jan;23(1):81-7� PubMed PMID: 8273964�
 By Jonathan E. Davis, MD, Professor & Academic Chairman, Department of Emergency Medicine, MedStar Georgetown University Hospital and MedStar Washington Hospital Center, Georgetown University School of Medicine, Washington, DC and Joanne L. Oakes, MD, Associate Professor of Emergency Medicine; Assistant Dean, Educational Programs; Distinguished Teaching Professor, The University of Texas Health Science Center at Houston, Houston, TX.
By Jonathan E. Davis, MD, Professor & Academic Chairman, Department of Emergency Medicine, MedStar Georgetown University Hospital and MedStar Washington Hospital Center, Georgetown University School of Medicine, Washington, DC and Joanne L. Oakes, MD, Associate Professor of Emergency Medicine; Assistant Dean, Educational Programs; Distinguished Teaching Professor, The University of Texas Health Science Center at Houston, Houston, TX.
Introduction
There are many reasons why an emergency physician (EP) may choose an academic career pathway: teaching, intellectual stimulation, a desire to contribute to residency education and the greater body of knowledge of emergency medicine (EM), and many others Some physicians enter residency with the intent to pursue an academic career, while others decide to pursue an academic track later during residency, fellowship training, or after years of community practice This chapter will discuss several key considerations in choosing academics and how to plan your residency training if you may be interested in pursuing an academic career�
One strategy to ensure that all potential EM career options remain open is to strive to become a “totipotent” EP during the course of residency training, with excellence in both clinical EM and in scholarship� Scholarship involves the creation or dissemination of knowledge through teaching, writing, integration, application, or discovery Residency is the time to lay the initial foundation in each of these areas – a foundation that will grow and mature with opportunities and experience over time
When, if ever, is it too late to choose academics? The short answer: it is never too late! However, the development and refinement of the essential skill set for success in academics during the course of residency training will prepare you if you decide to pursue academics at any point during your career� Not all academic EPs chose an academic career pathway immediately following training It is possible to successfully shift from community practice to academics, although making this transition a success may become more challenging with advancing time due the necessity of growth and refinement of the core skill set required for a success on an academic career track�



The requisite skills for success in academics can be readily achieved during a 3 or 4 year residency� The goal is to begin building one’s academic skill set during residency, regardless of program format Academic employers want motivated, interested, and highly productive faculty members� Experiences during residency that may further academic skills include dedicated teaching, research or writing projects with sound mentorship, or electives in niche areas of interest, such as ultrasonography, international EM, Emergency Medical Services (EMS), disaster medicine, or critical care� To view a complete list of residency programs, including location and length, search in the SAEM Residency Directory A 4 year format may provide additional time for advancing academic skills through added elective time or tracks focusing on areas of interest Fellowship training following a 3 year format may also provide unique opportunities for academic skill development and refinement within a particular focus area�
It may be difficult for a new graduate of a 3 year training program to obtain a first-year faculty position at a 4 year program This becomes less of an issue following completion of one year in practice (or a year of fellowship training) for 3 year residency graduates� In addition, the majority of training programs (and hence the preponderance of academic faculty positions) are in the PGY1-3 format (Of 240 total programs, 72% are PGY 1-3 format) based on current information available on the Emergency Medicine Residents’ Association (EMRA) website�
With the wide array of skills needed for success in academics, it may seem daunting to obtain any (let alone all) of them during residency training� It is important, however, to remember that exposure takes precedence over mastery during residency� Trying to “do it all” may be counterproductive, leading to premature burnout and career dissatisfaction Familiarity with the academic process is paramount� Most academic faculty members have particular areas of interest and expertise, ie their “niche,”
where they focus efforts Gain exposure to many skills, with a focus on particular skills of greatest interest to you
A mentor is “a wise or trusted counselor or teacher,” which in EM might be an upper level resident or a faculty member A good mentor is one who is willing to share knowledge from prior experiences with leadership, administration, research, and clinical teaching, and who is willing to direct mentees to additional resources for learning� Start first within your residency program� Who
Residency is the time to acquire the requisite academic skill set, which includes clinical, teaching, research, writing, administrative, and “people” skills
1. Clinical Skills – The most important aspect of emergency practice remains excellence in patient care� Superior clinical skills in history taking, physical examination, risk stratification, use of evidence based medicine, and cohesive, efficient clinical decision making should be acquired and refined during residency training
2. Teaching Skills – Scholarship involves the creation or dissemination of knowledge� Teaching is one form of dissemination Clinical (or bedside) teaching skills are learned primarily through the supervision and mentoring of junior residents, interns and medical students Ask for feedback from mentors, peers, and your students� Many residencies offer a “how to teach” curriculum to upper level residents� Teaching tutorials are available online, and the American College of Emergency Physicians (ACEP) offers a teaching fellowship for EM physicians� Didactic teaching skills are equally crucial for academic success� The adage “practice makes perfect” rings especially true for didactic presentation skills� The more experience and comfort you gain with teaching in small and large groups early in your career will serve you well in the future
3. Research Skills – Discovery through research (whether clinical, educational, or bench) is another essential academic skill� It is most important to be involved with the discovery process� Knowledge of the fundamentals of study design, institutional review board (IRB) processes, data collection/analysis, as well as experience with bringing-it-all-together as a manuscript or abstract are foundational research skills Whether this involves a single small-scale project or an in-depth experimentation in the laboratory is variable, and remains highly individualized� See SAEM’s Advanced Research Methodology Evaluation and Design (ARMED) course to learn the fundamental knowledge and skills to design a high quality research project� and grant proposal�
4. Writing Skills – Expressing oneself in prose is essential for effective synthesis and dissemination of knowledge� The more experience you can gain with this process during the course of training, the better prepared you will be for future academic success� Writing skills are necessary for abstracts, manuscripts, IRB and grant applications, curriculum development, lectures, policies – in short, everything academics! Writing skills may also be developed and refined by authoring review articles, textbook chapters, or by serving as an editor SAEM features a Grant Writing Workshop at their Annual Meeting each year Seek out writing opportunities during residency, and ask for feedback from mentors
5. Administrative Skills – An exceptional way to gain administrative experience is to get involved with committee work, whether at the local (residency program and hospital), regional, or national level In addition, working towards and achieving committee leadership positions is a great way to further refine your organizational, writing, task completion, leadership, speaking, and networking skills� Leadership positions within the residency, such as chief resident duties, also provide additional administrative experience with tasks such as scheduling, budgeting, finances, conflict resolution, counseling, and advocacy�
6. “People” Skills – Although all of the aforementioned skills are essential for a career in academics, it is difficult (if not impossible) to effectively utilize any of them without effective “people” skills� You must learn to manage, lead, and communicate with others in your different roles, and employ high emotional intelligence in all of your interactions� You must learn to give and receive feedback, work in teams, and develop active listening skills Mentors are a great resource in this regard – many people skills are learned and refined through role modeling Seek feedback from faculty members you respect and admire Take the time to network with other clinicians, educators, and academicians in a variety of settings� This may stimulate ideas or allow for collaboration on future projects�
are the leaders? Who are the great communicators or teachers? Who are the productive researchers? Who presents nationally and publishes? Who will give useful, constructive feedback for your career journey? Participation in local, regional, or national EM organizations, such as SAEM, RAMS, AAEM, RSA, ACEP, and EMRA, also provide countless opportunities for mentorship through presentations, forums, networking, and collaboration�
The decision to pursue a chief residency position can be challenging, as the duties and responsibilities will vary from program to program The “pros” of any chief position are numerous – you will gain valuable administrative experience with residency issues, from remediation and discipline to policy making and quality improvement� You will have opportunities to use and improve teaching, communication, and writing skills� Opportunities for publications or work on projects with faculty members may be available� The chief is viewed as a leader among his or her peers, a resident advocate, and a problem solver�
The “cons” of a chief year include questions of time and “the hassle factor ” The first question to answer is, “Will this be worth my time?” Some chief positions are funded as an additional year after graduation, with the chief functioning as a junior faculty member in addition to performing administrative duties, sometimes combined into an administrative fellowship� Other chief positions are incorporated into the final year of residency, combining the rigors of senior year with additional leadership demands The senior-as-chief role may create tensions among peers within the same level of training, and may add significant time demands to training, along with requiring strong organizational skills “The hassle factor” for you as chief is the knowledge that you are often the first person to hear from faculty, residents, program directors, and off-service programs when problems arise� Some view this as troubling, while others view this as invaluable growth experience
Overall, the learning and leadership opportunities offered through participation as a chief resident are vast A good place to develop the skills and strategies needed to succeed as a chief resident as well as gain mentoring is through the Chief Resident Forum offered each year at the SAEM Annual Meeting There may be some heartache with all the hard work, but most former chief residents walk away from the experience with great insight into the rewards and rigors of residency leadership and life in academics�
Obtaining a graduate degree in public health, epidemiology, education, research, business, or law (to name a few) may be advantageous to one’s academic EM career as it creates a focus for future work, whether for teaching, research, funding or writing� You will
have expertise in one particular area, have time to pursue your thesis or project(s), and gain invaluable opportunities for lifelong mentorship and collaboration with experts outside of EM� As an expert, you may be called upon to participate in local, state, or national policy making, committees, or teaching� An additional degree is also considered an advantage in the competitive academic job market�
The disadvantages of pursuing a graduate degree include time and money Does the pursuit of the degree require that you leave EM for a significant period of time? Is there adequate protected time to achieve your goals? Will the time away from potential income be repaid through job satisfaction later? Will you be able to use your degree in your EM work?
The decision to pursue a graduate degree will ultimately be determined by an individual’s career goals and interests� While not for everyone, those who choose to pursue a graduate degree to complement a career in EM often find they have gained unique skills to enhance career satisfaction in the academic EM world
Academic departments want enthusiastic, productive, well rounded faculty members who will contribute to the department’s overall mission When considering an academic job, focus on the institution’s work environment� Are faculty members using their abilities to the fullest? What career paths are possible at the institution? How much support is there for innovative ideas both within the department and institution? Is startup funding available for new projects? How are the faculty rewarded for their efforts? What is the promotion structure like? What is the turnover rate? What is the mission of the department? What are your opportunities for ongoing professional development? Comparing the institution’s values with your goals is essential to find a position that is a good fit� Advising and mentoring are essential – ask your trusted mentors for their thoughts and feedback�
The foundations of success in academics are excellence in both clinical EM and in scholarship Residency training is the time to pursue these skills, which can be refined with time and experience The requisite academic skill set includes clinical, teaching, research, writing, administrative, and “people” skills� Focus on skills of particular interest to you while gaining exposure to the entire academic skill set� This approach will prepare you for future success should you choose to pursue an academic career pathway�
Making a decision about life after residency can be a daunting task For those who are considering a career in academic emergency medicine, the question of whether to pursue fellowship training or seek a faculty position straight out of residency has likely crossed your mind You may be wondering: Do I need to complete a fellowship to be competitive for a faculty position? What benefits are there to doing a fellowship? What are the downsides? This chapter aims to answer some of these questions and identify how a fellowship can jumpstart your career
First and foremost, a fellowship is a training opportunity� Emergency medicine is fortunate to offer a wide range of fellowships� This type of training will provide you with additional knowledge and skills in a specific area of expertise

that may be clinically related (pediatrics, toxicology) or not (research, education) You will spend a great deal of time developing skills in a specific area of study� Additionally many fellowships offer advanced degree opportunities to give you additional competencies and help deepen your understanding� View a complete list of fellowship programs, where they are located, type of fellowship, and length of program in the SAEM Fellowship Directory� This expertise will allow you stand out against your peers as a leader in a given field of your choosing and better equip you to handle responsibilities of the job you assume after training
Fellowship is an opportunity to pursue advanced training in an area that you enjoy and are passionate about� In doing so, you begin to carve out a specific niche for yourself This not only allows you to steer your career towards content that you care about, but also is a way to make yourself indispensable to prospective employers because not everyone will possess the expertise that you do� Check out the RAMS Roadmaps to get an idea of some possible areas of interest
Additionally, by creating this niche, you will likely gain some control over how you spend your work hours, which can be very empowering By being able to focus your efforts on an area of interest and having some influence over your work activities, you will likely achieve a greater degree of job satisfaction�
Academic physicians often have multiple competing responsibilities including clinical, administrative, and teaching duties Protected time to pursue one’s professional interests is highly valued but not always easy to come by This may be particularly true for new faculty members who have yet to demonstrate a justification for protected time� However, it is this
time that is needed in order to be productive in scholarship, which is essential for promotion and career advancement in academic medicine� Very rarely is this precious commodity of time ever handed out as freely as it is during fellowship and it can be particularly valuable to jumpstart scholarly projects before the promotion and tenure clock starts ticking
Another benefit to completing a fellowship is the dedicated mentorship that comes along with it� You have close contact with an expert in your field of interest who is directly responsible for your knowledge acquisition and career progression� The value of this cannot be overestimated Mentorship has been shown to increase career preparedness, productivity, and likelihood of promotion� Mentors provide motivation, collaboration, guidance and critical appraisal of your work They can make your path to career advancement much more efficient by helping you avoid common mistakes and providing you with professional opportunities you might not otherwise have had� Having a good mentor is like having a roadmap to success Without one, you may at times find yourself lost trying to navigate through uncharted territory and may struggle to accomplish your career goals
By having protected time under direct guidance of an expert you will be able to increase your scholarly output� This serves as a type of currency in academic medicine and you will want to have as much of it as possible� It is a means by which your work can be disseminated to others further demonstrating your capabilities to prospective employers� Additionally, projects that you began in fellowship can be continued or built upon afterwards, allowing you to hit the ground running when you take your first faculty position�
Fellowship is an opportunity to pursue advanced training in an area that you enjoy and are passionate about.
Another benefit to completing a fellowship is the dedicated mentorship that comes along with it.
Fellowship also provides an avenue for networking with people who share your professional interests� This networking allows for the communication of ideas and opportunities It also may ignite collaborative efforts on scholarly projects which can increase their impact� Eventually you may find yourself becoming part of a community that disseminates information and supports one another in their professional pursuits, a highly desirable entity
By choosing to pursue additional training after residency, you may also increase your competitiveness for faculty positions As academic emergency medicine becomes more competitive, department leadership are seeking candidates who are already well prepared to handle job tasks It is essential that candidates be able to demonstrate their proposed value to the department and fellowship is one way to do so Having a fellowship and/or advanced degree provides a form of validation of the skill set you have attained and that little bit of

“alphabet soup” may increase your marketability and help you land a job in a competitive market�
Imagine you are a chair seeking to hire a new faculty member for the education arm of your department You have two intelligent candidates both with outstanding academic records� Candidate A is graduating residency at the end of the year, has been involved in teaching activities and is the middle author on a peer reviewed research publication Candidate B is completing a fellowship in education and a Master’s degree in education at the end of the year, was involved in teaching activities during residency, functioned in the role of assistant clerkship director during fellowship, and is the primary author on 3 education research manuscripts Which candidate would you select?
There are some departments that require new faculty to be fellowship trained, and it is not difficult to imagine why� While this trend may not be widespread currently, it is something we are likely to see more of in the future as the job market becomes increasingly competitive�
Fellowship training is not without costs and these costs are primarily in the form of time and lost potential income You will be spending an additional year or two in training and while you will likely be making more money than you did as a resident you will not be making what you would as a full time faculty member or community emergency medicine physician� Your schedule and the amount of hours will also vary depending on what fellowship you decide to do You may be required to take call� Because you will be in a training program with certain requirements you will also not have as much control over your professional life as you would have, had you not decided to pursue advanced training These are important issues to reflect on and discuss with your family as deciding to do a fellowship affects more than just you as an individual I believe that the benefits of completing a fellowship far outweigh the costs, but this is a decision everyone must make for themselves


There are a lot of good reasons to do a fellowship and I’ve highlighted a few of them above� There are also bad reasons to do a fellowship and these are also important to consider�

Don’t do a fellowship because you don’t know what you want to do after residency Fellowship is not a good placeholder for your professional life� Remember you will be sacrificing time and money to pursue this additional training so you’ll want to be sure that it is an area that you are truly interested in If you are unsure about where you want your career to go, it is better to do some self-reflection, discuss with mentors, speak with experts in the areas you are considering, or try small projects or experiences during residency to get real life exposure rather than commit to a fellowship�
Don’t do a fellowship because you think it will guarantee you an academic job in your desired location� There are no guarantees in life, plain and simple Landing a job is more about the qualities you have and the skills you possess� Now a fellowship may give you additional training, degrees, etc , but you will need to demonstrate what you can do with this education� Fellowship training is not a golden ticket to your dream job
Finally, don’t do a fellowship because you are afraid to make that jump from trainee to provider This is a difficult bridge to cross, but we all must cross it� Again, doing a fellowship does not come without sacrifices so it is not something to pursue just to delay the next step in your career If you do so, you might end up spending a year of two of your life focused on something you are not really interested in, learning information that may not be applicable to your future career
In summary, fellowship training can be an expedient way to gain expertise in an area that you are passionate about, receive protected time and dedicated mentorship to increase your scholarly productivity before you are burdened with other competing job tasks, and meet like-minded people who can become a supportive community and source of collaborators for future professional endeavors� While not without sacrifices, fellowship can be the perfect jumpstart to a satisfying career for the right individual�
Preparing for a career in Academic Emergency Medicine requires introspection and setting personal goals

Traditionally, an academic career encompasses participation in research, didactic teaching, clinical and bedside instruction, leadership, mentoring, and scholarly projects It involves medical student, resident and peer education It may involve development of continuing medical education for physicians, nursing staff, and prehospital care providers� It also may involve the community at large, or the hospital system and physicians from other specialties� Academic physicians may participate in many of these areas, or they may focus their energy on one particular area
Success in academics requires time, and keeping an open mind
It is important to have goals and priorities, but often, unplanned opportunities arise and lead to a new area of focus� An academic career can occur in a university-
based system, or in a non-university-based system It is ideal to develop some type of long-range career goal� It is important to envision how this career may evolve over the next ten or twenty years What seems ideal or enjoyable in the short term may not be sustainable over time It is pivotal to reflect on how one’s career may change over time� The beauty of an academic career is that it is extremely flexible, with new opportunities arising, and the ability to modify goals and objectives
The main hurdles for the resident training for a career in academics are lack of time due to the demand of the clinical load, and fatigue� Depending upon the training setting, there may not be much opportunity to learn the skills of teaching, administration, research, publishing, communication, and the building of relationships through networking� Identification of a mentor is critical and can help in providing a framework to gain these experiences, both during residency and beyond� It is helpful if the mentor’s career interests are similar to the resident’s In this way, the resident may learn by instruction by the mentor, as well as by modeling, because the mentor will lead by example� A mentor can guide a resident toward research projects, writing projects, teaching, and involvement in academic societies that will improve the chances that the resident will succeed in an academic environment� Over time, this relationship allows the individual to develop his or her own mentoring style as well
Most academic institutions expect a considerable amount of teaching from faculty members� The ideal time to begin to acquire these skills is in medical school and residency, as many institutions do not provide formal training in teaching� Clinical teaching can be
very challenging in the field of emergency medicine, as there are constant clinical pressures, as well as learners with varying levels of experience in the Emergency Department The challenge is to provide outstanding care while providing instruction and meeting the learners’ needs These skills are best acquired over time, and can be modified with experience� While outside the scope of this discussion, there is a body of literature available discussing concepts of adult learning and effective teaching principles� Motivated instructors will review this body of literature in order to become efficient and effective clinical educators� There are also courses available in this realm, such as the American Association of Medical College (AAMC) courses on faculty development opportunities in education at the national meeting that is open to medical school and teaching faculty� The Society for Academic Emergency Medicine (SAEM) has many resources in this area, such as the “Clinical Teaching Educational Boot Camp: Be the Best Teacher” at the SAEM Annual Meeting each year� The American College of Emergency Physicians (ACEP) has a Teaching Fellowship program for two weeks during each year� The Council of Residency Directors (CORD) offers many sessions at the yearly Academic Assembly that are devoted to education� Residents can begin by assuming a leadership role with medical students, and later junior residents in the Emergency Department setting� This could range from helping a medical student tailor an effective presentation to a faculty member, to interpretation of laboratory values or x-rays, and further to assisting with procedures performed by junior residents� Other opportunities lie in volunteering to be a clinical skills instructor for medical students or being a medical student advisor or mentor It is important for an educator to reflect on teaching methods and focus on their role as the role of the learner changes

Setting expectations for the learner and giving effective feedback, as well as learning how to assess performance are essential skills that can be acquired during residency�
Residency is also the ideal time to improve lecture and presentation skills, which are very important to the academic physician Although most educators agree that the lecture format is not the most effective means of transmitting principles, it is still the most common method of teaching in academic emergency medicine� Computer skills are essential, as most lectures are now given on computerized programs given in a slide format, often with embedded videos and clips� Skill in performing internet searches, medical database searches, and basic statistical procedures is essential in preparing these presentations� Speaking skill and style can be honed during lectures to small groups of residents and attendings during residency This experience is excellent training for academic presentations later in a career, whether it be at national meetings, guest lectures, or lectures within the institution In addition, it provides an opportunity to work on writing and effective communication skills Gaining experience leading small group sessions and workshops with learner participation, including methods such as the “flipped classroom” are essential to the academic physician to keep learners engaged�
Effective communication skills are mandatory for the successful academician Even if these skills do not come naturally, it is possible to cultivate them by associating with other successful academicians Individuals who associate with successful educators and researchers are likely to become successful themselves� These relationships teach the learner about the informal network that supports productivity, and they provide insight into the inner workings of professional organizations� This allows one to identify who are the most productive individuals, and how their behavior leads them to success It is ideal to begin this process in residency by beginning to participate in academic tasks�
These tasks may be as simple as planning residency programs such as lecture series, in-training exam review, journal club, or by serving on residency committees� Serving as chief resident is excellent in terms of administrative preparation, and offers the opportunity to acquire skills in developing personal relationships and effective communication While formal professionalism training is not available in many residencies, these skills can be learned by modeling and identification of suitable mentors
Wise use of social media and awareness of free online medical education (FOAM) resources is essential for the academician, as learners will be using these resources whether they are assigned or not� SAEM has an extensive library of FOAMed Resources including websites, blogs, podcasts, videos Another good reference is SAEM Online Academic Resources (SOAR) which is a site that hosts a variety of online educational resources Including past presentations, a library of downlaodable curriculum, and other online resources� Social media and FOAMed have transformed the availability of medical information for both the general public as well as physicians, and is available anytime to anyone with a computer or handheld device Professionalism in social media is of the utmost importance for physicians having access to and using it Online learning tools are powerful and are continuing to be developed and their roles are expanding rapidly� The academician must keep up to date and use these resources wisely, as well as weigh sources carefully as much of the content may be unedited�
Administrative training during residency is useful in understanding how economic, political, societal, consumer and organizational pressures affect academic medical centers� Understanding these pressures, as well as the formal structure of relationships between academic medical centers, academic departments, the medical school, the university, and the hospital, lends
Identification of a mentor is critical and can help in providing a framework to gain these experiences, both during residency and beyond. It is helpful if the mentor’s career interests are similar to the resident’s. In this way, the resident may learn by instruction by the mentor, as well as by modeling, because the mentor will lead by example.
insight into how to be an effective academician� This understanding is essential for those individuals wishing to pursue careers focused in administration, such as medical director or department chairperson�
Reading and writing skills are essential to the academic physician, whether they be primarily involved in clinical teaching, didactics, research, or administration Some of these skills are acquired through review of the current medical literature� Evidence based medicine courses can help with both the reading of the literature, as well as critical assessment, which can improve the resident’s own writing skills Promotion in academia often depends upon quality publications, whether it be bench or clinical research, or educational literature and research� Critical reading and writing skills are best learned at the residency level or better yet, earlier�
For those physicians interested in research, developing research skills during residency can be very helpful� This is another area in which identifying a mentor involved in research is critical A research project during residency is a wonderful way to gain experience with the Institutional Review Board process It provides experience in understanding the difficulties of developing, implementing, analyzing, and preparing a research project It forces some study of statistical methodology and data analysis� It provides an opportunity to work on reading and writing skills� It also provides an opportunity for an oral presentation or poster presentation both locally and at a national meeting level, where speaking skills can be practiced It also provides an opportunity to become proficient with computer media� The exposure to Emergency Medicine academicians through research presentations during residency is unparalleled� The Resident and Medical Student (RAMS) Research Committee through SAEM is a great vehicle to gain experience in research and presenting it� SAEM also has the Advanced Research Methodology Evaluation and Design (ARMED) course targeted toward junior faculty in order to jump start their research career
Fellowship training is another way for residents to spend more time preparing for a career in academic emergency medicine Fellowships in emergency medicine are available in the following areas such as: Toxicology, International Medicine, Research, Education, Administration, Emergency Medical Services (EMS), Pediatric Emergency Medicine, Sports Medicine, Injury Prevention, Ultrasound, as well as programs that
involve degrees in public health and epidemiology� More information regarding fellowship programs and what they offer can be found in the SAEM Fellowship Directory� Many of these fellowships (Toxicology, Hyperbaric Medicine, Sports Medicine, Pediatric Emergency Medicine, EMS, Pain Medicine, Hospice and Palliative Medicine, and Critical Care) lead to board certification by the American Board of Emergency Medicine� The advantages of fellowship training are the opportunity for continued socialization to the world of academia, more time to forge relationships and focus on an intense period of study in an area of interest, and developing expertise with a less rigorous clinical load than that of full-time faculty� A fellowship also allows for preparation as an academic mentor to others as one’s own career matures� Fellowship graduates may be more sought after in the job market due to development of an area of expertise, as well as demonstration of the ability to draw funding during fellowship as a marker for the future A drawback of fellowship training includes drawing a salary that is less than that of a full time faculty member, and the total time spent during training is extended by doing a fellowship
When a candidate pursues a career in academic medicine, it is important to tailor the curriculum vitae appropriately to highlight those experiences that demonstrate an ability to succeed in the academic environment Again, academic advising and mentoring is essential� Interviews should ideally be scheduled in the first half of the final year of residency, as most positions start July 1st, and some positions may be highly sought after� This also allows for several different interviews and travel, as well as second visits if necessary� One important factor to consider is the academic work environment Are faculty members using their abilities to the fullest? What career paths are possible at the institution? How much support is there for innovative and new ideas? Is startup funding available for new projects? How are the faculty rewarded for their efforts? What is the promotion structure like? What is the turnover rate? What is the mission of the department? Comparing how these values measure with those of the candidate are pivotal to finding a position that is a good fit for the candidate� Ideally, the time to prepare for an academic career is as early as possible Keeping an open mind and jumping on opportunities to teach, to do research, to get administrative experience, and to learn to be an excellent communicator are helpful in beginning to acquire the academic skill set�
Creating a healthy career in medicine is becoming more and more challenging� Specifically, the unique demands of emergency medicine (EM) require a strategic approach� There have been a growing number of studies addressing burnout and resilience, which include a focus on time management, navigating between professional and personal responsibilities, recognition of the risks of burnout, development of strategies to foster resilience, and establishment of ongoing mentorship 1 In this chapter, the topics above will be discussed with the goal of assisting you in developing your own approach and strategies for wellness in your life�

Wellness is a broad term that has a vast array of meaning for each person In that context, stop and take a moment to consider the question: What does wellness mean to you?
There are several definitions of wellness on a global and national scale The World Health Organization defines wellness as a state of complete physical, mental and social well-being, and not merely the absence of disease or infirmity 2 The National Wellness Institute defines wellness as a conscious, self-directed and evolving process of achieving full potential This definition of wellness can be divided into 6 dimensions: occupational, physical, social, intellectual, spiritual and emotional 3 Wellness is not static but rather a continuum, and at times “being well” may be the middle ground and at other times, it might be euphoria For any individual, particularly an EM physician, your definition of wellness and the things that keep you well will vary as you go through different stages of both your personal and professional life� Remember, long-term wellness isn’t just the absence of unhealthy feelings, burnout or impairment, but it is the active involvement in things that rejuvenate and revitalize you�
Wellness in emergency medicine is achievable, but there are many challenges to maintaining a sense of wellness during your career as an EM physician� The nature of EM inherently challenges our wellness As EM physicians, we witness tragedy such as unexpected death, violence, and are exposed to a variety of complicated illnesses and disease processes that are frequently undifferentiated when first encountered� There are other stressors that are key for EM physicians and include: minimal capacity to appropriately eat during busy shifts, isolation from social support due to scheduling constraints, briefness of relationships with ED patients, and difficult or challenging interactions with ED colleagues, physicians from other specialties, patients, and their families
Prolonged shift work is frequently cited as a cause of sleep disorders From a circadian perspective, it is optimal for shift start times never to be rotated� Although when shift start times are rotating, the circadian clockwise rotation of days to evenings to overnights is preferred� When possible, working a single night shift is ideal so that you never reset your circadian rhythm and remain in a diurnal orientation� There are different sleep techniques that are employed by shift workers that can facilitate proper sleep hygiene Split sleep is a method that involves sleeping 3-4 hours immediately before a night shift and then 3-4 hours following the shift� With this technique, at least part of each sleep episode is during the normal circadian time when sleep is expected 4 Anchor sleep is important for night shift workers� With this technique on your nights off, you would stay awake until 3-4am and then sleep until 10-11am so that you can maintain your nocturnal orientation and still have time during the day to socialize 5 A quiet and dark place for daytime sleeping is a necessity, and you should consider your daytime sleeping as protected time
If achieving wellness is uniquely challenging, how do some EM physicians successfully navigate their careers with apparent ease and have a fulfilling long-term experience in EM? In the remainder of the chapter, we will discuss strategies to achieve long-term career satisfaction, which positively impacts wellness�
There are several ways to navigate personal and professional responsibilities that would positively impact one’s wellness and well-being� The strategies listed below are applicable across the 6 dimensions of wellness previously mentioned�
There are several definitions of wellness on a global and national scale. The World Health Organization defines wellness as a state of complete physical, mental and social well-being, and not merely the absence of disease or infirmity.
Wellness in emergency medicine is achievable, but there are many challenges to maintaining a sense of wellness during your career as an EM physician. The nature of EM inherently challenges our wellness.
• Create a plan to find and fulfill your mission. What is your mission? Give yourself a moment to reflect on this question You may have several missions in a variety of contexts that are part of your personal, relational, professional and academic life Establishing a central mission or sense of purpose in your life will help keep you centered despite the challenges you might be facing in the current moment Strive to articulate a long-term vision, which will help you construct a roadmap to fulfill your mission Purposefully charting your accomplishments, sacrifices and progress towards these goals will continuously give life to your fulfillment of your mission
• Connect with your colleagues. The importance of relationships with your colleagues substantiates and validates similar and shared experiences at work and at home When you know your ED colleagues as people and not just fellow physicians, a common bond is created� Without this personal relationship, our goals and purposes are sometimes lost, and we may feel as if we are in isolation� The emotional stress that we are

exposed to on a daily basis can seem overwhelming� For example, sharing our thoughts after a bad case or mass disaster by conversing and debriefing with those around us can help us preserve our sense of well-being
• Enjoy what you do. Maybe you are not able to do this all the time, however try to reflect upon the work you do and remember your knowledge and experience can change lives It is important to enjoy both the practice of EM and your work environment Smile and laugh when appropriate to help alleviate the stress and anxiety that is a part of the emergency department
• Physical well-being. The literature supports that physical activity is critical for career success and personal well-being� Physical activity can be as intense as a high frequency exercise routine or leisurely such as walking and stretching� Any physical activity will improve your quality of life� It is important to establish a routine that you can maintain This time for physical activity should be calendared into your schedule so that you “always have time for it ” Adequate and high
quality sleep coupled with regular physical activity is known to improve quality of sleep and overall sleep hygiene A diet that is well balanced, nourishing, and includes adequate hydration is also important�
• Immediate family. Creating and maintaining a healthy relationship with your immediate family is crucial� This is where time management skills are critical We are not always available for important events and holidays because of the demands of an EM schedule� Therefore, it is important to be present and fully engaged when you are home� Give your family your undivided and uninterrupted attention when you are spending time with them - unplug and put the smartphone, tablet, and laptop away� Prioritize your clinical schedule and request off important life events (birthdays, anniversaries, graduations, etc�)�
• Keep in touch with extended family and friends. They are often a voice of reason, perspective, and support� If you don’t feel comfortable talking to a friend or family member, consider using a professional therapist particularly if you are having feelings of depression or burnout
Time management is a unique skill set that is challenging to obtain given the demands of our specialty� EM physicians encounter challenges in the workplace including high acuity patient encounters and intense work schedules that include nights, weekends and holidays� Strategic ways to maximize personal time is a deliberate exercise
• Make plans and take time for yourself and your family. A proactive approach is required to include activities that are critical to you and your family� Plan activities that you enjoy These might be simple things such as putting your children to bed, watching TV with your significant other or going to the movies with a friend� On a larger scale, you may also enjoy activities like attending a live show or concert, taking a weekend getaway, or travelling abroad No one will advocate that you take time for yourself and your family except you! This time should be a priority so protect it and schedule it Physicians are masters of delayed gratification, and it is difficult to be an excellent medical professional without taking time for yourself

• Be realistic. There is not enough time in the day to do everything you would like to do and still get adequate sleep� A daily schedule only works if it is realistic and maintainable so avoid over-burdening your schedule� Consider scheduling additional “work” time into your shifts� Schedule an 8 hour shift as 10 hours� Complete documentation while “at work”, answer email, and work on other academic requirements� Try to get home ontime instead of late�
• Invest in a time management tool. There are countless print and electronic time management resources available� Research what’s available, and choose and master the ONE method that is best for you and your family Multiple lists can organize professional and personal goals� Daily, weekly, monthly, and longer term lists can be helpful Set goals for yourself and your family to ensure balance over time Revisit these lists periodically to add, subtract, and modify goals�
There are many definitions of burnout, but the most comprehensive one is a “syndrome of emotional exhaustion, depersonalization, and a sense of low personal accomplishment that leads to ineffectiveness at work 6” Burnout is common and affects between 30-65% of EM residents and faculty at any given time� Burnout may present with frank changes in personality or as subtle changes that only the most intimate friends/ partners may notice� Burnout must be watched for with vigilance, as this will insidiously affect your life choices and long-term career� Manifestations of physician burnout include:
• Loss of interest in work
• Feelings of fear, avoidance, isolation, anger, and, ultimately, loathing for work
• Fatigue, exhaustion, inability to concentrate, anxiety, insomnia, irritability
• Increased use of alcohol and drugs
• Headache, back or neck pain, gastrointestinal distress, malaise
• Anxiety, divorce, broken relationships, and disillusionment7
The problem with burnout is that the people experiencing it are often too disconnected to recognize their symptoms Therefore, friends, families, and colleagues are often the first to notice burnout If you are being asked about burnout, you should heed the warning, and start talking to those that may be a resource for you� There are multiple resources available for you to use to identify burnout in either yourself or a colleague and to help you The critical first step is the recognition and ownership of these feelings of burnout 8, 9 There are resources available on the SAEM website that have been put together by the SAEM Wellness Committee�
The value of prioritizing your personal care cannot be overemphasized. Accept that you can’t do it all everyday and prioritize being present for the task at hand and outsource things that you can. Get involved in departmental, hospital, or national committees or projects that provide a sense of personal accomplishment and expand your sense of belonging and community.
Alcohol and drug dependence is a special concern� Anyone suspected of substance abuse should be immediately reported to their superiors so that an intervention can be made to prevent harm to self or others
Psychiatric illness is another special consideration Psychiatric illness often presents early in one’s career given the typical age of onset of psychiatric illness� Fatigue, physical, mental, and emotional stress may accelerate the disease processes of depression, anxiety, and other psychiatric disorders
A special note to the female Emergency Physician: there are unique stressors that apply directly to your gender� Without a doubt, patients will bluntly and subtly consider you different; at times considering you to be a nurse or using familiar statements such as “honey or sweetie,” and not “Dr� X”� Staff will often times have different expectations of you than of your male colleagues� Motherhood, in particular, is a difficult role to balance with professional duties� Things that may help negotiate this challenge include: finding a mentor who has had similar experiences, setting realistic expectations for yourself, learning to set limits, and not feeling guilty when you say no to requests� The Academy of Women in Academic Emergency Medicine (AWAEM) and The American Association of Women Emergency Physicians (AAWEP) are great resources for the female Emergency Physician Both these organizations have a philosophy of mentoring women through each phase of their career�
The alternate to burnout is resilience� Resilience is the capacity to respond to stress in a healthy way such that goals are achieved at minimal psychological
and physical cost; resilient individuals “bounce back” after challenges while also growing stronger 10 It is critical to develop strategies to foster resilience by taking care of yourself and those around you� Medical education enculturates us in self-sacrificing behavior so it is important to recognize that you must take care of yourself first The value of prioritizing your personal care cannot be overemphasized� Accept that you can’t do it all everyday and prioritize being present for the task at hand and outsource things that you can Get involved in departmental, hospital, or national committees or projects that provide a sense of personal accomplishment and expand your sense of belonging and community� Make connections with people senior to you with similar interests, however, never take on new responsibilities if you are feeling stressed or if you are busy building your academic foundation In addition to having a mentor, be a mentor� Sharing your experiences, collaborating on research or writing projects, and helping others to find their own true interests can be very career-affirming and is often recognized in the academic promotions process
Emergency medicine brings great career satisfaction but has a unique set of challenges that can lead to increased stress� It is paramount to be able to recognize burnout and foster personal resilience� Preserving and navigating personal and professional responsibilities, utilizing time management strategies, actively engaging with a mentor, and taking a proactive approach to your wellness will help ensure a long and healthy career in emergency medicine�
References:
1 Taylor, C, Taylor, J, and J Stoller The Influence of Mentorship and Role Modeling on Developing Physician-Leaders: Views of Aspiring and Established Physician Leaders Journal of General Internal Medicine October 2009 24:10; 1130-1134
2 World Health Organization Preamble to the Constitution of the World Health Organization as adopted by the International Health Conference, New York, June 19-22, 1946; signed on 22 July 1946 by the representatives of 61 States (Official Records of the World Health Organization, no 2, p 100) and entered into force on 7 April 1948
3 Hettler, Bill The Six-Dimensions of Wellness The National Wellness Institute www nationalwellness org
4 Thomas, Harold Circadian Rhythms and Shift Work ACEP Policy Statement Emergency Physician Shift Work 2003
5� Minors, DS and JM Waterhouse� Does ‘anchor sleep’ entrain circadian rhythms? Evidence from constant routine studies� Journal of Physiology 1983 December; 345:451-467
6� Maslach C, Schaufeli WB, and MP Leiter� Job burnout� Annual Review of Psychology� 2001; 52: 397-422�
7 Birnbaum A and M Haughey Can you be an EM resident and still experience “Wellness?” SAEM Newsletter of the Society for Academic Emergency Medicine, November- December 2004
8 Maslach C, Jackson S and M Keiter Maslach Burnout Inventory Manual 3rd ed Palo Alto, Ca: Consulting Psychologist Press; 1996
9 Bintliff, Kaplan, Meredith Wellness Book for Emergency Physicians ACEP 2004
10 Epstein RM, Krasner MS Physician resilience: what it means, why it matters and how to promote it Academic Medicine 2013; 88:301-303
11 Nobay, F, Donnelly, A Creating a Healthy Career – Time Management, Wellness and Mentoring SAEM Academic Career Guide Chapter 6 2006
Clinical educators provide the foundation of medical education in the academic setting� Throughout medical school and Emergency Medicine residency training, educators take on many forms and come in all shapes and sizes Some most heavily contribute through research while others find their niches through fellowship training and contribute to the educational milieu in more specific ways (think ultrasound, EMS, toxicology, etc)� Many of these physicians gravitate to academic centers where they will continue to pursue their academic interests Other physicians, like ourselves, elected to make clinical education in addition to clinical practice our main focus�
Clinical educators work in emergency departments where active, formal learning is occurring Clinical educators are expected to devote time educating through direct interaction with the learners while seeing patients in the

clinical setting� Learners typically include medical students and residents This interaction involves observation of the learner in the clinical environment and providing feedback� However, education is also provided by acting as a role model and demonstrating how to practice as an effective Emergency Medicine physician Clinical education is at the foundation of medical education�
Being a clinical educator is often in association with an Emergency Medicine residency program, however, you may work in a hospital where learners come from other departments (Internal Medicine, Family Medicine, Pediatrics, OB/Gyn, etc) to obtain emergency department experience

In these settings, the clinical educator makes a significant impact by teaching learners at the bedside Residents and students look to attending physicians to guide their management of patients in the emergency department

Of course, clinical education may conjure up the image of teaching in a university setting However, we obtained our first jobs as clinical educators, not at large university hospitals, but rather at community settings with academic affiliations with an emergency medicine residency Residents rotated in the departments where I worked and my interest in teaching led me to pursue the role of a clinical educator�
Clinical responsibility will vary depending upon what other interest or endeavors you participate in As a clinical educator in an academic environment, you may be expected to work more clinical hours than those physicians who dedicate their time to other, nonclinical endeavors such as research or administration/operations Alternatively, you may work at other sites where resident coverage is not as robust, meaning that you will be seeing a higher percentage of patients independently�
One of the sites that I experienced as a clinical instructor was a very high volume, urban ED� There was a resident or two available every shift However, that resident was split among two attendings As a result, 60-70% of the volume in that environment was consistently seen independently by attending physicians�
A clinical educator position does not mean all the shifts you work will include resident coverage� Whereas researchers, residency program leadership, and administrators devote their non-clinical education time to their niches, those who function as

Clinical educators provide the foundation of medical education in the academic setting.
clinical educators also contribute by seeing patients independently in the clinical arena� As clinical educators, there are many positions where a significant percentage of your shifts are without residents entirely� I routinely have worked at various community emergency departments without residents�

However, this in and of itself provides opportunities to become a better teacher by maintaining one’s own clinical skills and efficiency You may often hear of Emergency Medicine attendings who work almost exclusively with residents and lament about the amount of time that has passed since they last intubated a patient or placed a central line as these are procedures that often go to residents to further their education experience Clinical educators who don’t work all shifts with residents can more easily maintain these skills� Further, clinical educators consistently maintain the flow of the departments when residents aren’t present�
Ultimately, I feel this makes me more effective teaching the skills that I continue to practice and readily maintain Residents I interact with are typically aware of these responsibilities which does provide a sort of credibility� While routinely managing teams of residents in fully staffed academic departments certainly has its own challenges, sometimes unrecognized by the residents, I am routinely asked by learners how practice changes in the “real world�” Having additional experience, often practicing in different environments, lends to me an experience that I am able to pass on to resident and medical student learners� This is, in essence, an important part of being an effective role model
In the positions I have held, I have learned selfmotivation and dedication to teaching must be primary drivers to succeed as clinical educators As a clinical educator, you must actively seek out opportunities to teach This goes beyond simply listening to residents and students present cases while you adjust their plans accordingly� It is important to constantly probe for depth of knowledge
Questions that may have obvious answers to you may reveal a knowledge gap on the part of the resident or student that requires filling�
However, engaging learners in the department may often be difficult secondary to the multiple competing interests that attendings face on every shift In addition to direct patient care there are multiple interruptions that often lead to less time for teaching It is important to be prepared to overcome these competing interests� Having canned talks with teaching for common complaints ready is an example of how one might increase efficiency of teaching� Sometimes, teaching and feedback may have to be saved for the end of the shift Regardless it must occur as a commitment to teaching is paramount to being an effective clinical educator� It is important to respect the effort that the learner is providing by rewarding them with a dedicated, concerted effort to be an educator
Typically, demands of your non-clinical time are not as great as a clinical educator as those experienced by physicians who engage in research, administration/ operations roles, residency leadership This does have
the advantage of making the maintenance of work-life balance easier to attain However, there is no shortage of opportunities to participate and be of value as a clinical educator�
You may be asked or expected to participate in didactic education in the form of attending weekly residency conferences and/or creating and giving lectures� Participating in procedure labs, simulation session, and journal clubs provide other important opportunities to remain involved as a clinical instructor and demonstrate the degree of investment that you are willing to make�
Being a clinical educator in an academic setting also provides additional resources to explore other non-clinical opportunities I have immersed myself in department leadership and quality improvement positions that were born of an interest to remain involved with teaching as a clinical instructor in academic settings�
Obtaining a position as a clinical instructor was made easier by early demonstration of a desire to remain engaged in active teaching Enthusiasm for being a clinical instructor often become apparent to you in residency or early in your career� This is often reflected in the formal feedback you receive from medical students and resident physicians� This feedback, in the form of evaluations and citations/awards for efforts made towards clinical instruction were instrumental in my gaining employment opportunities that involved resident and student teaching If you enjoy teaching in the clinical arena and the evaluations that you receive from students and residents demonstrates an appreciation for your efforts, these are good indications that the role of the clinical instructor may be appropriate for you
Many Emergency Medicine physicians can recall the attendings physician who seemed less than enthusiastic about teaching during shift and more interested in having residents write notes, place orders, and call consultants for them� Whether or not this is actually the case, this perception often leads to losing the privilege of working with learners However, it highlights the importance of remaining engaged and conversely, physicians who demonstrate a joy and a knack for teaching often have the opportunity to acquire more shifts where active learners participate�
For me, enjoying teaching led to my learning to incorporate it into my everyday practice in the emergency department Finding, or rather creating, time to teach when the department is busy is a skill that will require effort to develop Preparing canned talks, actively searching for teaching points, or making
the effort to circle back around after a shift is over to teach are examples of the efforts that typically are noticed and appreciated by learners and make you a much more effective clinical educator� I routinely email residents and students to provide post shift follow up and highlight teaching points and areas to improve� Reviewing charts for proper documentation also provides an avenue for feedback and further education�
Be a proactive educator and your learners respond with their own enthusiasm and, very importantly, display the improvement you hoped to achieve with them
After years of remaining immersed in the educational environments that are medical school and residency, I found myself truly enjoying the role of teacher� Specifically, I enjoyed the opportunity to teach at the bedside
Good clinical educators have an enthusiasm for teaching and are approachable, communicative, and are actively supportive� These are the traits that we identify among our own most valued clinical educators from the times we were students and residents� These are the traits I strive to emulate as an educator
Teaching medical students and junior residents how to approach emergency medicine complaints, perform procedures, and navigate through a busy department brings a sense of satisfaction that rivals that which I receive when providing patient care The understanding that I may positively impact future patient care by being an effective teacher is particularly rewarding
However, I was not interested in more formal roles in education Program and curriculum development, while extremely important, were simply not an interest� I also knew that research and additional fellowship training were not the paths I desired to take�
What I did want was the ability to work primarily clinically but with the opportunity to continue to teach future practitioners of Emergency Medicine This role could be of particular interest to Emergency Medicine physicians who are recently graduated and would like to continue to broaden their clinical experience However, it also allows for those who are further along in their careers to test the waters of academic Emergency Medicine
Being a clinical instructor was also beneficial in maintaining my own clinical education Continued teaching is joined with continued learning� Working in an environment where active learning is routine has pushed me to keep pace not only with our colleagues but with the residents who are learning the constantly evolving specialty of Emergency Medicine
 By Gillian Schmitz, MD, Associate Professor, University of Texas School of Medicine, San Antonio, TX and Cherri Hobgood, MD, Professor and Chair, Department of Emergency Medicine, Indiana University School of Medicine, Indianapolis, IN.
By Gillian Schmitz, MD, Associate Professor, University of Texas School of Medicine, San Antonio, TX and Cherri Hobgood, MD, Professor and Chair, Department of Emergency Medicine, Indiana University School of Medicine, Indianapolis, IN.
Updated November 2015 by Kevin King, MD, Director, Medical Student Education & Hector Caraballo, MD, Associate Director, Medical Student Education, Department of Emergency Medicine, University of Texas Health Science Center San Antonio.
When many emergency physicians think of a career in academics, teaching emergency medicine residents is what first comes to mind Yet, medical student education has been a part of the emergency medicine academic landscape for years Historically, clerkship directors have had a relatively limited role of shepherding EM-interested students through elective MS4 clerkships and the subsequent interview process� But today, as medical schools integrate emergency medicine into their curricula and the number of mandatory EM clerkships continue to expand, academic
emergency physicians have a myriad of opportunities to impact undergraduate medical student education (UME) at multiple levels� Some examples of activities available to medical student educators include:
• Classroom and bedside teaching during both the pre-clinical and clinical phases of UME
• Development of UME curriculum
• Mentorship of students in both pre-clinical and clinical years
• Education (UME) related research
• Technical and procedural didactics
• Faculty advisor to student interest groups in EM
In 1995 the Macy Foundation published, “The Role of Emergency Medicine in the Future of American Medical Care�” This report illustrated the surprisingly poor training US medical students receive in the fundamentals of emergency care and life support� At that time, less than 20% of US medical schools had required courses in emergency medicine in their curricula� To correct this deficiency, the report recommended all applicants for medical licensure have specific training in emergency care during medical school Further, the report recommended that competency in emergency care should be assessed during the United States Medical Licensing Examination (USLME) Although faculty members from many different
medical specialties could contribute to basic instruction in emergency medical care, physicians certified in emergency medicine were recommended by the Macy Foundation report as best qualified to be teachers of emergency medicine
As of 2011, fifty-two percent of medical schools require an emergency medicine clerkship� A standardized curriculum exists for both third and fourth year medical students The new curriculum incorporates the most current Liaison Committee on Medical Education (LCME) requirements and discusses additional aspects of the educational model such as feedback, evaluation, and implementation� Furthermore, in 2014, the American Association of Medical Colleges (AAMC) published the Core Entrustable Professional Activities for Entering Residency (CEPAER) outlining newly established proficiency requirements of a graduating medical student� Of interest, EPA #10: “Recognize a patient requiring urgent or emergent care and initiate evaluation and management,” will likely result in a large expansion of emergency medicine content into all four years of medical education curricula
Over the past several years, US medical schools have migrated away from the classic, discipline-based curriculum (i�e�: anatomy, microbiology, pathology, pharmacology) and toward a “problem-based” curriculum that covers all the classic topics, but in a system and problem-based method� Students now have education modules regarding the cardiac system with the anatomy, physiology, pathology, etc� all integrated into that module Theoretically this allows students to more easily integrate the requisite knowledge from
Over the past several years, US medical schools have migrated away from the classic, discipline-based curriculum (i.e.: anatomy, microbiology, pathology, pharmacology) and toward a “problem-based” curriculum that covers all the classic topics, but in a system and problem-based method.
As our specialty is involved in virtually all areas of a hospital-based practice, emergency physicians can participate in the development and instruction of a large number of education programs in the pre-clinical years.
each discipline into a cognitive structure that supports medical practice� At many institutions, this phase is also shortened to 18 months, permitting more clinical experience�
At some institutions, practicing physicians are requested to teach during the clinical integration portions of the education modules Often, these are case-based sessions in which clinicians help students learn to apply their newly-found knowledge in a clinical scenario With EM’s broad-based and dynamic clinical practice, we are particularly suited to provide this instruction
Beside didactic instruction, emergency physicians can also participate in longitudinal preceptorships, history and physical examination courses, and become involved in other educational courses such as bedside ultrasound, disaster preparedness, resource utilization, and many other topics� As our specialty is involved in virtually all areas of a hospital-based practice, emergency physicians can participate in the development and instruction of a large number of education programs in the pre-clinical
years� Medical schools are constantly searching for interested faculty and many opportunities are available to the willing emergency medicine faculty

Ideally, all medical students should participate in a mandatory emergency medicine clerkship during their clinical years However, here again, US medical schools are re-designing the clinical years of medical school No longer is there a “third year” were the students complete all their core requirements in one continuous block� Rather, at many institutions, students are given 18 months or so to complete 12 months of “core” clerkships and permitted to interspace elective courses at their discretion� This permits students to explore their career options earlier in their education
Typically, an emergency medicine required or “core” clerkship is completed during the latter part of their clinical education (classically during the fourth year)� The thinking goes that, as emergency medicine is a specialty predicated on a broad knowledge of all medical
specialties, it is best taught after the student has acquired that broad exposure to several medical fields As a consequence, most medical schools that require an emergency medicine clerkship do so in the latter portion of the clinical education (during the fourth year)� However, there is a growing number of medical schools that integrate emergency medicine into the early part of the clinical curriculum (the third year)
Regardless of the timing of the emergency medicine experience, students are exposed not only to the clinical practice of emergency medicine, but are taught the principles of recognizing acutely ill or unstable patients and the initial steps to assess and stabilize them Furthermore, emergency medicine is unique in US medicine� As opposed to many other fields, emergency physicians spend virtually their entire careers evaluating undifferentiated patients with complex medical problems� Thus, emergency medicine is an excellent laboratory in which students can practice and refine their clinical skills including history, physical exam, and medical decision-making
As medical schools pivot to address the AAMC’s new CEPEAR requirements, emergency medicine is uniquely suited to address many of these areas, especially the aforementioned EPA #10� When emergency medicine faculty are involved in the education of undergraduate students, opportunities abound both for the department and the faculty members Faculty can become involved in medical student education operations such as curriculum committee or student promotions committee, potentially influencing the design of the overall medical school curriculum Often, for interested faculty, these activities can lead to leadership positions within the medical school For the academic departments, becoming an integral part of the student curriculum can help increase parity between emergency medicine and the other, “classic” fields such as internal medicine or surgery Additionally, as students gain exposure to EM, many subsequently choose to pursue emergency medicine, improving the quality of emergency medicine residency candidates
The Emergency Medicine Clerkship Director (CD) is the course director for one or more medical student clerkships At some



Thus, emergency medicine is an excellent laboratory in which students can practice and refine their clinical skills including history, physical exam, and medical decision-making.
institutions, the CD will also have one or more assistants� The CD is responsible for the design and implementation of the emergency medicine clerkship they run� Duties include curriculum development, faculty training, evaluation of both students and faculty, course improvement, and ensuring compliance of all education activities with medical school and regulatory agency rules and regulations� Organizations such as SAEM offers specialized groups such as the Clerkship Directors in Emergency Medicine (CDEM) specific to clerkship directors as well as training�
As previously mentioned, emergency medicine is relatively new to the medical school curriculum landscape This provides an opportunity for emergency medicine educators to implement unique, novel techniques to teach students Not only can EM educators teach new content, they can also develop novel approaches to medical education� Examples of such innovation include the use of asynchronous learning tools, the use of ultrasound at the bedside, and the use of simulation to practice delivering bad news to patients and their families Additionally, clerkships in wilderness medicine, bedside ultrasound, toxicology, international medicine, and EMS are popping up at some schools to address student interest in the full breadth of EM�
Regardless of the course, Clerkship Directors will gain experience in educational design, leadership, organizational skills, and learner assessment�

Student interest groups in emergency medicine are common fixtures in the pre-clinical years at many medical schools The purpose of these student-led organizations is to provide opportunities for preclinical students to gain exposure to what an emergency medicine career is like� Many groups invite speakers, arrange procedure labs and provide information to their membership regarding the practice of emergency medicine� Most medical schools require that any sanctioned medical school group have a faculty mentor or preceptor� Generally, the mentor provides advice to the student leadership of the group and assists as needed to obtain resources from the medical school (at our institution, a faculty signature is required to reserve a room, for instance) Involvement in a student interest group is a good opportunity for a faculty member to gain their first experiences working with students�
As emergency medicine becomes a more prominent part of undergraduate medical education, the opportunities for education research will undoubtedly grow� Currently, the Clerkship Directors in Emergency Medicine (CDEM) and the Society for Academic Emergency Medicine (SAEM) actively promotes the creation and publication of such research both in journals, such as the Academic Emergency Medicine (AEM) and Academic Emergency Medicine Education and Training (AEM E&T) and the research forums at the SAEM conference in the spring Additionally, SAEM offers the Advanced Research Methodology Evaluation and Design (ARMED) course It covers everything you need to know to start a research project�
The process of selecting a career specialty can start at any point in medical school� Most medical schools assign advisors to students upon matriculation These advisors are oriented toward the students’ global academic development but cannot always provide specialty specific advice, especially if the student chooses a specialty other than their mentor’s�
It is critically important that emergency medicine educators be available for students seeking specialty career advice In a study by Blumstein et al, 38% of emergency medicine residency applicants surveyed reported receiving information only in an informal manner from an emergency physician and 57% received negative information from non-emergency physicians regarding EM
Emergency medicine has become an increasingly popular career choice for medical students over the past several years� As a consequence, the application
process has become more competitive and complex� Students will require high-quality guidance on their career choice� Faculty who choose to undertake this task will be rewarded with a rich and longitudinal mentor relationship with motivated medical students While the specifics of how to advise students is outside the scope of this document, advisors will find themselves helping students discern their fitness for EM, generating application strategies, providing reassurance and celebrating successes A mentor is more than just a role model; he or she has an active role in the future and career development of a student A number of studies have consistently demonstrated that individuals with supportive mentors have greater job satisfaction and greater productivity A mentor can, in fact, be the primary influence on career selection� This is especially true for women and underrepresented minorities in academic medicine, although there is a paucity of available mentors� Faculty can find more information on how to be an effective EM mentor through CDEM, both at their conference and their website
Many opportunities exist to help you build an academic career focused on teaching medical students To view a complete list of open clerkship programs including location, electives offered, where to apply, positions per rotation, institution setting and more see the SAEM Clerkship Directory� The rewards of an academic career are deeply personal and bountiful If you enjoy teaching and seek the daily challenge of creating an environment where education is of paramount importance, then a career in teaching medical students may be for you� You will contribute to the betterment of your students, the institution, and the specialty�
1 Bowles LT, Sirica CM (eds) The Role of Emergency Medicine in the Future of American Medical Care New York: Josiah macy Jr Foundation, 1995
2 Manthey, D et al, Task Force on National Fourth Year Medical Student Emergency Medicine Curriculum Guide Report of the Task Force on National Fourth Year Medical Student Emergency Medicine Curriculum Guide Ann Emerg Med 2006
3 Core Entrustable Professional Activities for Entering Residency, Curriculum Developers Guide Available at www aamc org
4 Lawrence LL, Counselman FL, Gluckman W, Guidelines for Undergraduate Education in Emergency Medicine ACEP Online www ACEP org
5� Tews MC, Hamilton GC� Integrating Emergency Medicine Principles and Experience Throughout the Medical School Curriculum: Why and How Acad Emerg Med 2011;18;(10)1072-80 PMID: 21996073
5� Binder LS, DeBehnke DJ� The Importance of Being Earnest----and Student-centered� Acad Emerg Med� 1998:5 (1)103�
6 Blumstein HA, Cone DC Medical Student Career Advice related to Emergency Medicine Acad Emerg Med 1988; 5(1): 69-72
7 Paice E, Hears S, Moss F How Important are Role Models in Making Good Doctors? BMJ 2002;325:707-710
8 Jackson VA, Palepu A, Szalacha L, Caswell C, Carr PL, Inui T Having the Right Chemistry: A Qualitative Study of Mentoring in Academic Medicine Acad Med 2003;78:328-34
9 Garmel GM Mentoring Medical Students in Academic Emergency Medicine Acad Emerg Med 2004; 11:1351-1357
From the day you start as an emergency medicine (EM) residency program director (PD) you will be working arduously and putting in long hours every week towards getting the job done� It is very likely that in your EM residency PD position you will be working harder and putting in more hours than any of your previous jobs in medicine, including EM residency� Why do that? Think about the answer to this question carefully before pursuing and then accepting an offer to become an EM residency PD
As an EM PD you will probably receive a higher salary than the position you were in prior to becoming a PD� In addition, because the Accreditation Council of Graduate Medical Education (ACGME) Residency Review Committee in EM (RRC-EM) limits the annual scheduled clinical hours for an EM PD to a maximum of 960 per year, as an EM PD you will very likely be working less annual clinical hours than what you had been assigned in your position prior to

becoming an EM PD� You may receive an individual office with more square footage than the administrative space allocated to you in the past and as an EM PD you now have what many in medical academia might consider a prestigious title and academic advancement Sounds good, right? In many ways it may be, but compensation, no matter how attractive, a large individual office, no matter how private and spacious, a prestigious title, no matter how impressive, and advancement on the academic ladder are, in my view, insufficient by themselves for long-term fulfillment in the role of EM PD� For that, I believe a vision for being an EM PD is needed
Becoming an EM PD affords one with an opportunity to truly have a say in how emergency medical care is delivered and who will provide emergency medical care in the future An EM PD is intimately involved with the selection process for EM residents who will carry on our values as physicians and who will represent us individually, as EM physicians, and collectively, as the specialty of EM, in the world� An EM PD is accountable for training the next generation of EM physicians and preparing them to evaluate and treat the unplanned and unanticipated acutely ill and injured of all ages but to also address and solve health care problems from local to global including those that have yet to arise�
There are many perspectives utilized in trying to define the term vision� For this chapter vision will be defined as having the following characteristics: future based, seeing the possibility for something to emerge, not predicted by past performance or history, not defined or determined by current circumstances, and invented or created in language� In this model a vision stays in existence only through continuous communication, both verbal and non-verbal, and through actions and behaviors
consistent with the vision� Additional parameters for a powerful vision include: it is highly inclusive, it connects actions to purpose, it excites you, and when spoken leaves others with the possibility of participation in and contribution to something bigger than the individual
Here are examples of vision statements I have created to inspire and motivate me throughout the twenty plus years I have served as an EM PD:
To enhance well-being and have each and every person leave with an experience of having been valued.
To provide dignity, compassion, and enhance the wellbeing of each and every person.
To build emergency medicine residency programs and train residents to go beyond the didactic and experiential thirty-six month curriculum that comprises traditional emergency medicine residency training to teach foundational principles of critical thinking and model timeless values and ideals which graduates can draw upon to inform their medical practice for the entirety of their career in emergency medicine as well as rely on throughout their lives.
As an EM PD and Department of EM Chair the following vision statement I created has always served to motivate and inspire me:
To build a Department of Emergency Medicine that serves as a model of excellence for what is possible for people: a safe haven where training the next generation takes place in an environment of scholarly inquiry with a commitment to well-being and where the highest quality patient-centered emergency medical care is delivered with timeliness, operational efficiency, dignity,
Becoming an EM PD affords one with an opportunity to truly have a say in how emergency medical care is delivered and who will provide emergency medical care in the future.
An EM PD is accountable for training the next generation of EM physicians and preparing them to evaluate and treat the unplanned and unanticipated acutely ill and injured of all ages but to also address and solve health care problems from local to global including those that have yet to arise.
compassion, and a driving commitment to honor the human spirit, to celebrate diversity, and to combine the latest of science and technology with an ever present awareness of the value of the human touch as a power for healing.
So is all the hard work and time required to be an EM PD worth it? I think so� As has been said by many PDs, it is the best job in the world What is the magnitude of the impact an EM PD can make by educating and training the next generation of EM specialists? Working a full-time clinical schedule in an Emergency Department an attending in EM can evaluate and treat 3,000 – 3,500 patients per year Over a twenty-five to thirty year clinical career that equates to 75,000 to 95,000 patients whose lives have been touched through the provision of emergency medical care If an EM PD graduates ten EM residents per year who each go on to work full-time clinical schedules over a career of twenty-five to thirty years, those graduates can evaluate and treat 750,000 to 950,000 patients� Over a twenty-year career as an EM PD that number increases to 15,000,000 – 19,000,000 patients whose lives have been touched through the
provision of emergency medical care, a very powerful demonstration of the power of leverage and ripple effect�
No need to reinvent the wheel The responsibilities and accountabilities associated with the position of EM residency PD are well delineated in the 2016 ACGME RRCEM program requirements:

There must be a single program director with authority and accountability for the operation of the program. The sponsoring institution’s GMEC must approve a change in program director. The program director must submit this change to the ACGME via the ADS. The program director should continue in his or her position for a length of time adequate to maintain continuity of leadership and program stability.
Qualifications of the program director must include: requisite specialty expertise and documented
educational and administrative experience acceptable to the Review Committee, current certification in the specialty by the American Board of Emergency Medicine, or specialty qualifications that are acceptable to the Review Committee, current medical licensure and appropriate medical staff appointment; and at least three years’ experience as a core faculty member in an ACGME-accredited emergency medicine program.
The program director must administer and maintain an educational environment conducive to educating the residents in each of the ACGME competency areas. The program director must: oversee and ensure the quality of didactic and clinical education in all sites that participate in the program.
The program director must be clinically active in emergency medicine. The program director must not work more than 20 hours per week clinically, on average, or 960 clinical hours per year.

The program director must: approve a local director at each participating site who is accountable for resident education, approve the selection of program faculty as appropriate, evaluate program faculty, approve the continued participation of program faculty based on evaluation, monitor resident supervision at all participating sites, prepare and submit all information required and requested by the ACGME. This includes but is not limited to the program application forms and annual program updates to the ADS, and ensure that the information submitted is accurate and complete.
The program director must: ensure compliance with grievance and due process procedures as set forth in the Institutional Requirements and Emergency Medicine implemented by the sponsoring institution, provide verification of residency education for all residents, including those who leave the program prior to completion, implement policies and procedures consistent with the institutional and program
requirements for resident duty hours and the working environment, including moonlighting and, to that end, must distribute these policies and procedures to the residents and faculty, monitor resident duty hours, according to sponsoring institutional policies, with a frequency sufficient to ensure compliance with ACGME requirements, adjust schedules as necessary to mitigate excessive service demands and/or fatigue; and if applicable, monitor the demands of at-home call and adjust schedules as necessary to mitigate excessive service demands and/or fatigue, monitor the need for and ensure the provision of back up support systems when patient care responsibilities are unusually difficult or prolonged.
The program director must: comply with the sponsoring institution’s written policies and procedures, including those specified in the Institutional Requirements, for selection, evaluation and promotion of residents, disciplinary action, and supervision of residents, be familiar with and comply with ACGME and Review Committee policies and procedures as outlined in the ACGME Manual of Policies and Procedures
The program director must obtain review and approval of the sponsoring institution’s GMEC/DIO before submitting information or requests to the ACGME, including all applications for ACGME accreditation of new programs, changes in resident complement, major changes in program structure or length of Emergency Medicine training, progress reports requested by the Review Committee, requests for increases or any change to resident duty hours, voluntary withdrawals of ACGMEaccredited programs, requests for appeal of an adverse action; and, appeal presentations to a Board of Appeal or
the ACGME. The program director must obtain DIO review and co-signature on all program application forms, as well as any correspondence or document submitted to the ACGME that addresses, program citations, and/ or request for changes in the program that would have significant impact, including financial, on the program or institution.1
If all the above sounds like a lot to keep track of and accomplish that is because it is! An EM PD is a job you can’t get done by yourself� A high-performing team is necessary to accomplish all the accountabilities of an EM PD and deliver all the outcomes that are expected of an EM PD which segues to some of the skill sets and prerequisites for the successful fulfillment of the job of an EM PD: outstanding leadership, high emotional quotient (EQ), exceptional communication skills, conflict resolution, and relationship bridge-building abilities Your leadership team should include your EM program coordinator, chief residents, and assistant/associate PDs� Nurturing, empowering, inspiring, as well as holding your leadership team, both individually and collectively, accountable for the success of the program and achieving all the expected program outcomes is a key part of your job as an EM PD
Over the course of three to four years of EM residency training innumerable unforeseen day to day concerns, complaints, and upsets will occur and be brought to the EM PD for adjudication and resolution Fortunately most of these issues are not serious� However, many have the potential to require significant time to resolve� Unanticipated stresses affecting EM residents will likely occur over the course of one’s tenure as an EM PD� Some may involve unsatisfactory performance in academics,
While there are a number of academic roles and positions that can forward one’s mission to become an EM PD, the one that is closest to that trajectory is assistant/associate PD (APD). This is a job that will provide a broad range of responsibilities and accountabilities that equip one with the prerequisite experiences that facilitate a smooth transition to EM PD.
clinical care, or professionalism/communication while others may be of tragic proportion and could involve loss or death of a loved one, serious to fatal physical illness, clinical depression, or even suicide� It is essential to fully understand and embrace this key role of an EM PD�
There are many career pathways to becoming an EM PD During the first one to three years after EM residency graduation the journey starts with passing your written and oral boards and becoming an excellent, well-respected clinician and bedside teacher, the bedrock on which all successful leadership positions are built in EM Develop an academic niche in an area which can serve as a foundation for didactic and simulation lab teaching in the program and becoming known for a particular expertise Volunteer to participate in areas of the residency program such as interview season, new EM resident orientation, and practice/mock oral board exam sessions Ask to become a member of the Clinical Competency Committee or the Program Evaluation Committee Get involved with clinical operations, quality, and/or projects designed to improve the patient experience Develop a reputation as a problem solver, a “yes” person with a can-do positive, optimistic attitude� Take on and resolve an issue that matters to the program and department and about which people complain but has no owner� Seek out and find a mentor who has achieved what you are striving to accomplish With today’s technology and ability to communicate over the internet a mentor does not always have to be in your Department of Emergency Medicine� In addition, you can receive mentoring from more than one person as well as persons with expertise and experience in a wide range of medical, scientific, and healthcare related disciplines
If an academic role offered to you in your department during the initial years following residency graduation does not appear to be immediately relevant to your envisioned career path towards an EM PD consider that the role you take on and handle may well open important doors to your future and that the value of an opportunity, especially when presented in the early years of your career development, is not always apparent at the time it is presented to you Contribute without expectation of a quid pro quo Generosity works� The results of a project that initially does not
appear germane to your plans to becoming an EM PD may segue into opportunities for publication, invited speaking, and teaching at a regional to national level that ultimately have a very positive impact on moving closer to your career goals
While there are a number of academic roles and positions that can forward one’s mission to become an EM PD, the one that is closest to that trajectory is assistant/associate PD (APD) This is a job that will provide a broad range of responsibilities and accountabilities that equip one with the prerequisite experiences that facilitate a smooth transition to EM PD� Being in this role for three to four years while not mandatory is a great asset to have prior to becoming an EM PD� An EM PD will often stay in that position for a minimum of five years In some Departments the EM PD may stay in that position for ten to twenty years If the latter is the case in the department where you are working as a core residency faculty and APD, be willing to move to create opportunity to become an EM PD within a time frame that is consistent with your career goals and aspirations As you develop professionally your greatest future career opportunities may not be in your current department or even geographically where you envisioned living� This career reality will require careful consideration and discussion with family, significant others, loved ones, and friends
Without a clear vision and purpose for taking on the position, without the right preparation and understanding of the demands of the position, without the requisite emotional intelligence, positive, optimistic attitude and leadership skills, and without the right supportive and empowered team both at work and at home, the job of EM PD can quickly become overwhelming, frustrating, exhausting, and lead to a journey down the road to burnout� However, armed with all prerequisites, being an EM PD can be and has been said by many to be the greatest job in the world� After having been blessed with the opportunity to serve as an EM PD for over twenty years I am of the opinion that being an EM PD is, indeed, the greatest job in the world� I wholeheartedly recommend it to you It is worth what it takes and I encourage you to pursue it with gusto�
 By Willard W. Sharp MD, PhD Assistant Professor, Section of Emergency Medicine University of Chicago.
By Willard W. Sharp MD, PhD Assistant Professor, Section of Emergency Medicine University of Chicago.
Congratulations! If you are reading this chapter, chances are that you have decided to pursue the difficult but rewarding challenge of being a physician scientist� Physician scientists not only deliver clinical care and carry out teaching responsibilities, but also pursue scientific studies to create innovation in the practice of medicine These advances can be in the form of educational, clinical, translational, or basic science discoveries� While innovation is an essential aspect of medical care, it is costly and requires investment in the form of time, effort, and supplies� Unfortunately, funding for research does not come directly from clinical revenue and investigators must continuously search for sources of funding� The most significant and prestigious source of funding for health related research is the National Institutes of Heath (NIH) NIH grants provide significant funding enabling protected time from clinical and teaching duties, in addition to funding time for collaborating investigators, research assistants, technical staff, supplies, and even administrative costs for the participating institutions However, funding from the
NIH is very competitive and writing NIH grants can be time consuming� Alternatively, there are other public agencies and private foundations that fund research� Many of these organizations have disease specific or training level specific grants� The American College of Emergency Medicine Physicians (ACEP) and the Society for Academic Emergency Medicine (SAEM) are good starting points to begin a search for funding opportunities In addition, many universities and hospitals have internal grants and funding opportunities that investigators should search for� Regardless of the funding source, nearly allpotential funding organizations will require an application outlining the purpose and scope of the proposed studies� Thus, the ability to write high quality grant applications is as important of a skill to be mastered by the physician scientist as the designing of experiments and publishing manuscripts�
In today’s political and economic environment, competition is fierce for funding and success does not come easy even for veteran researchers Excellent grant writing skills and persistence in effort are essential tools for survival� Even simple misspellings or grammatical errors can be enough to irritate grant reviewers resulting in rejection of the most promising of grants� While, it is true that a well-written grant will not overcome the deficiencies of a poor hypothesis or experimental design, well-designed grants can be killed by poor grantsmanship� Although, grants will vary in topic and scope, successful grants have certain fundamental characteristics In this chapter, these characteristics will be reviewed in the context of the three phases of grant writing: preparation, writing/assembly, and post-editing/submission An overview of the process is shown in Table 1�
Formulate a hypothesis and specific aims
Approximate a budget
Identify a funding agency and application dates



Seek advice/collaborators
Writing Phase
Follow funding agency format
Specific Aims
Preliminary data
Schematics/Figures
Pre-Submission Phase
Final editing/review
Letters from collaborators/mentors
Post Submission
Planning for resubmission
Have a plan B
Laying the foundations for a grant proposal can take considerable amounts of time so it is always best to start as early as possible before an identified submission deadline� During the preparation phase the following four tasks will need to be completed; 1) Formulate a hypothesis and specific aims, 2) identify a funding agency, 3) approximate a budget, 4) seek advice/ collaboration Although these tasks are performed simultaneously, for organizational purposes, they will be reviewed here sequentially
The first task is to formulate a hypothesis as well as several specific aims designed to test the hypothesis During this step, the entire grant’s scope and complexity will be formulated As ideas are formulated, essential questions to ask are: What is already known about this topic? Is the topic worth studying? How will the study change current practice if successful? What knowledge gaps will the study fill? Are innovative techniques or strategies needed to answer the problem? At the NIH, grants are judged by five criteria: (Significance, Innovation, Approach, Investigator, and Institution)� Three of these five criteria (Significance, Innovation, and Approach) are formulated at this stage of the grant writing process� Clearly, these are daunting tasks and will require significant investments of time by the investigator� A good way to get the process started is
by performing a thorough literature review to ensure that the study being constructed is unique Grants that ask clinically relevant questions and that have the opportunity to change clinical practice in a meaningful manner are likely to garner the most attention from reviewers�
The second task is to identify a funding agency� Identifying an appropriate funding agency will be determined by the topic of the grant, the amount of funding required, and the length of funding required� As indicated earlier, the NIH typically provides the greatest amount of funding for the longest periods of time� A standard modular NIH R01 grant for independent investigators currently has a budget of $250,000 a year for direct costs, in addition to covering indirect costs based on the institution’s negotiated rate, and typically covers a 4 to 5 year period� A non-modular R01 can cover even greater direct costs, but require a more detailed budget justification To determine whether the NIH has ever funded a grant on the topic being proposed, the NIH reporter web tool can perform a search of all current and past funded grants by topic (projectreporter�nih� gov)� NIH program officers are another good sources of information and are often willing to discuss new grant ideas particularly with junior investigators� Prospective applicants to the NIH are encouraged to seek out NIH program officers in the field of their proposed study to discuss a possible grant submission early in the process�

Current standard deadlines for new RO1 series grants are in February, June, and October of each year, although specific funding notices can have deadlines throughout the year Because of the lengthy grant application, review, and funding cycles, it can be 8-10 months from the time a grant is submitted to actual funding This again reinforces the concept of the need for starting early� In addition to the NIH, there are numerous other public and private agencies that fund research Many of these organizations have variable deadlines for grant submissions Again, the ACEP and SAEM websites are a good starting point for searching for EM related grants and funding organizations�
The third task is to determine an approximate budget for the grant� This is important to do early, as it will determine the funding agency and complexity of the grant� Questions to be addressed at this stage are how much of your time/salary/effort will be on the grant? Will other individuals be on the grant and if so what will be the amount of their salary and percent effort? How many months or years will funding be needed? If the investigator or an employee’s entire salary is not on this particular grant, what percentage of their effort (salary) will be dedicated to the proposal and what will the other
funding sources be? It is often good to contact your department’s or institution’s grants administration to see if they can help you draft a preliminary budget once you have an idea of how much time you will need to devote to the project, the number of other investigators/ assistants needed, and the amount of equipment/ supplies required The length (months/years) of the grant is another important budget consideration� Often the length of the grant is related to the number of specific aims� Each specific aim should be thought of in terms of how many scientific publications it will produce Many investigators consider each aim to produce between one to two manuscripts� Thus, if a grant proposal has three specific aims, it can be expected to produce between three and six manuscripts� The time course for these studies must then be budgeted accordingly
The fourth and final task of the preparation phase is to identify potential collaborators or colleagues who might be able to help with the proposed studies� Research does not occur in isolation, and today in order to be successful, one will need to find innovative ways of collaborating For example, there may be more sophisticated strategies to test the proposed

hypothesis that the investigator is incapable of doing alone Identifying a colleague(s) who can help with performing or training in these strategies can make the proposal stronger and more likely to get funded� In addition, colleagues in the field of interest may have experience with applying for certain grants and may be able to offer advice and tips on how to organize a grant proposal� Finally, it must always be remembered that funding organizations are not only funding the research proposal, they are also making a choice to fund a particular investigator� By establishing a network of colleagues and collaborators, an investigator is communicating her niche of expertise to the scientific community and establishing herself as a leader in their field Funding organizations may know of an investigator through their scientific network and this in itself will be important in the funding process
In summary, the preparation phase of grant writing is the most important phase It is also the most time consuming and intellectually challenging part of the process Hastily and well-prepared grants both stand out to reviewers, each with opposite effects Taking time to construct an excellent hypothesis and specific aims, identifying the appropriate funding agency, formulating a preliminary budget, and assembling a network of supportive colleagues will go a long way to ensuring a grant proposal has the highest chances of success before the writing process even begins�
Once the four tasks of the preparation phase have begun, actual writing of the grant can be initiated For practical instructions on how to write a grant, SAEM has a series of Grant Writing Webinars� Each year SAEM offers a Grant Writing Workshop at the SAEM Annual
Meeting as well� This phase may take several weeks to several months once the hypothesis and specific aims have been finalized� Every funding organization has its own formatting and submission instructions, so it is important to obtain these at the beginning of the writing process� A funding organization’s instructions should be followed explicitly, as many organizations will automatically reject proposals that are not entirely compliant� For many organizations, the first page often consists of a “specific aims” page composed of a short introduction, the hypothesis, and the specific aims of the proposal This page should also state something about why the investigator is ideally and uniquely positioned to answer the question being proposed� Many grant reviewers decide how interested they are in a grant proposal and how closely they will read the rest of the application while reading the specific aims page The importance of this first page cannot be overemphasized� It provides the reviewer a “first impression” of the proposal and the investigator Grants are often “killed” or “funded” by reviewers at this early point in the application
Following the specific aims page, the rest of the grant application is used to elaborate in detail on the problem being studied, the ideas proposed on the specific aims page, and the merits of the investigator and the environment they are in The research strategy section of an NIH grant typically is divided into three sections: background and significance, innovation, and approach These sections may be developed to a maximum of 12 pages (total) with 0�5 margins� Arial 11-point font is the suggested font of choice Some grant agencies, such as the NIH, also require preliminary data demonstrating that the proposed hypothesis has merit and that the investigator has the ability to carry out the proposed
By establishing a network of colleagues and collaborators, an investigator is communicating her niche of expertise to the scientific community and establishing herself as a leader in their field. Funding organizations may know of an investigator through their scientific network and this in itself will be important in the funding process.
studies� In some instances, preliminary data may take a year to collect, while in others, it may only take a few months� Ironically, preliminary data in the form of published manuscripts is ideal� This is because published data is peer reviewed and demonstrates to the reviewers that the data is highly promising and the investigator has ability to carry out meritorious research� Thus, it behooves the investigator to have published some papers on the topic of interest prior to grant submission and to include relevant data from these publications in the proposal� It should however be noted that not all NIH or private foundation grants require preliminary data� This is particularly true for career development and “high risk/high reward” grants classifications
Diagrams or cartoons of the hypothesis and demonstrating how each specific aim tests the hypothesis are very helpful to grant reviewers and are encouraged Alternatively, figures or tables demonstrating the experimental design can be used� Figures and tables facilitate rapid understanding of what the proposal is about and go a long way in facilitating the reviewer’s understanding of the proposal If there is room on the specific aims page, some investigators find it helpful to include a schematic�
The writing phase can be summarized as the period in which the hypothesis and specific aims are elaborated on and formatted according to the grant agencies guidelines� Figures and preliminary data will go a long way to helping the reviewers to understand the proposal�
Once a draft of the grant has been written, the post editing/submission phase of the grant writing process begins� During this stage comprehensive review of the grant occurs along with finalization of supplemental documentation being supplied with the grant It will be important to have colleagues and friends look over the grant carefully The grant will need not only to be edited for content and ideas, but for clarity, grammar, and spelling as well� Having individuals both in and outside your field of research review your proposal is often helpful� Colleagues in your field can help with technical or theoretical concerns while colleagues outside your field can help insure that the concepts being communicated are sufficiently explained and that technical jargon is kept at a minimum Having even a family member review the proposal for readability in addition to grammatical and spelling errors can be quite helpful However, beware of superficial commentary as “it looks good” or “it’s fine ” Comments characterized by vague generalities
and lacking specific commentary often indicate that the proposal was only read at a superficial level and that the investigator should continue to seek out opinions� Remember, it is always better to get critical or even harsh advice from colleagues that result in a successful grant application than to get pleasantries from colleagues resulting in a rejected grant proposal
Funding organizations often require varying amounts of supplementation materials These materials can consist of CVs (or formatted biosketches), letters of support/recommendation, finalized budgets, and institutional animal care and use committee (IACUC) and/or institutional review board (IRB) documentation� Be sure to leave at least several weeks to work with your institutional representatives to submit the grant� Details regarding budget, animal or human patient approval, and formatting regulations often take longer than one thinks and should not be rushed in the days prior to final submission
Following the submission of the grant, there will be an immediate and well-deserved sense of relief� However, in the weeks following submission, work will need to begin in earnest on the initial aims In the competitive world of grant funding, it should be assumed that the funding agency will want a revised application or that the proposal will need to be submitted to a different funding organization for funding Continuing to work on the grant will not only allow one to address potential concerns of the reviewers, it will also generate more preliminary data for a revised version of the grant� It will also allow for a “plan B” if the funding organization rejects the proposal It should always be remembered that funding agencies have their particular interests and focus and that competition for funding is fierce Thus, if a grant is rejected, it does not necessarily mean that it was poorly designed or written� Resiliency and tenacity are absolutely essential characteristics for the physician scientist� Grants that are funded are often the result of many failed attempts
In summary, grant writing is a necessary part of the academic endeavor of the physician scientist and requires a skill set similar to the other skills of an emergency medicine physician Proper planning in advance, careful writing and organizational skills, and collaboration with others all increase the chances of writing a successful grant These characteristics, along with a mindset of persistence and resiliency, are required for the successful physician scientist

A busy emergency department (ED) is one of the most complicated operational environments that exists� It is a place where critical interplay exists among physicians, nurses, and acutely ill patients, often under significant time constraints and often involving other medical services in the hospital in real time and at unusual hours To further complicate this picture, add into this mix the Emergency Medical Service system, law enforcement, and occasionally the news media, as well as the heavy-handed legal requirements of providing care to further complicate the picture� Last but not least, add the challenge of being adequately compensated for our work� Who would want to be responsible for all of this?
As the ED, we are the “buffer” if you will, that smoothes out to the extent possible the unscheduled occurrence of acute illness and injury as it enters the medical system We provide initial interventions so that individuals are transitioned safely to the next step, whether it be a procedure, in-hospital treatment, or discharge and treatment
Michael A. Peterson, MD, FAAEM, Professor of Medicine, The Geffen School of Medicine at UCLA, Vice Chair and Chief of Operations, Department of Emergency Medicine, Harbor-UCLA Medical Center, Torrance, CA.at home� Because of the unpredictable nature of our business and its association with acutely ill individuals, the ED tends to be a problem-generating engine for the hospital, often with patient complaints and bad outcomes Other times we merely act as a problem “pass-through” portal, as complicated patients with predictably poor outcomes and complex social issues enter the hospital through the ED� We are, in essence, the hospital’s other front door� This type of environment is one of the challenges that appeals to those of us who gravitate toward ED administration�
Now, add onto all of that the additional complications that exist in an academic center, including supervising and teaching physicians in training from all specialties, along with their mandated curricula and work rules� There is also the challenge of the oft under resourced academic hospital If the hospital is a government institution there is likely a dearth of capitalist incentives driving improvement in the system Indeed, financial pressures may be at odds with the system efficiency� (What happens in a system where the more productive you are, the more money you lose?) There are also government hiring and work regulations limiting managerial flexibility, as well as advocacy groups such as labor unions who may weigh heavily on system operational decisions�
It makes sense to start with why one might opt to be a medical director at all, whether it be in a community hospital or an academic center� Many of the duties and challenges of the medical director are the same regardless of the type of hospital� Medical directors
ensure that the working environment is properly equipped and staffed, and champion processes that optimize the primary product of the ED: safe and timely emergency care� The tasks are numerous, including hiring, scheduling, billing and finance, patient satisfaction, quality improvement, accreditation surveys and regulatory investigations, peer review, policy and process, public relations, equipment identification and acquisition, budgeting, and contract development and management In a bigger operation, these tasks are often shared among several individuals, with the director as the “lead ”
This kind of work tends to attract individuals for several reasons: prestige, money, fewer evening/night/ weekend hours (although in some cases it may be more) or the enjoyment of administrative work Many directors are “fix it” people We enjoy identifying problems and crafting solutions, and having the satisfaction of seeing the improvements our “fixes” create We often work collaboratively within the department, hospital, or even at the corporate or multi-hospital group level Collaborative work can be socially stimulating and provide a sense of connection to the hospital or corporation that patient care alone does not It can also improve one’s own experience in providing care in the ED by breaking down barriers between the emergency physician and medical staff (especially helpful when you call for those 3 a�m� admissions)� Over time, one develops a skill set of creating productive and lasting change; a skill set that is unfortunately often underappreciated� One of the best skills to develop is the ability to foresee the future with regards to operations� Specifically, knowing what attempts at change will likely succeed and which will fail, as well as seeing the potential for problems that haven’t yet
As the ED, we are the “buffer”, if you will, that smoothes out to the extent possible the unscheduled occurrence of acute illness and injury as it enters the medical system.
Collaborative work can be socially stimulating and provide a sense of connection to the hospital or corporation that patient care alone does not.
occurred, and steering the organization away from these hazards I also like developing a vision for the future of the ED from a medical practice standpoint� As a clinician, we impact the lives of individual patients as we treat them As a medical director, I can see my actions impact hundreds if not thousands of patients each year, as well as the physicians, nurses, and ancillary staff that care for them�

Examples of projects I’ve been involved in recently: 1) Being an active participant in the building of a new ED with a vision to make the facility a visually, as well as physically, healing place� We ensured the department was equipped with cutting-edge technology and a myriad of tools to ensure that physicians have the best resources available for their patients� We configured the new ED to function in the next big disaster, and for the evolution of the delivery of medical care that we predict will happen;
2) Building new operational processes through analyzing, modifying, and adopting the best practices seen at other institutions� One example is the creation of a rapid screening area; 3) Developing electronic warning systems and procedures for the ED and hospital for overcrowding; 4) Developing a financial program to incentivize physicians; a program that rewards both the physicians and the department budget� These are but a few of the ever-changing and creative opportunities that we don’t get with patient care alone�
The truly rare bird however is the academic medical director Many perceive this position as having all of the downsides of directorship without the financial advantages found in a community directorship position Why be an academic medical director? I think the answer is found in what one of my mentors explained as the difference between an “academician” and a “clinician who teaches�” The latter is primarily a physician who also likes to teach, the former is a teacher who also happens to be a physician This is no different for the academic medical director� We are teachers who also like administrative work If you are not sure if you are a teacher first, I suggest that you not initially seek out an academic directorship, but rather sample academia in general to see if it fits Otherwise you will be subject to all the disadvantages of administrative work without the balance of enjoying academic life, and will also likely make less money than a community ED director�
On the other hand, if you get great satisfaction from the educational process, and seek the life of an administrator, this job may be right for you Many advantages await you, including an often constant demand for your skill set in the academic setting� In addition, you get the intellectual stimulation as well as the personal satisfaction of working with learners and guiding them on their journeys, and if you are truly lucky, mentoring them in areas beyond medicine� The choice became obvious to me after working as a director in a
non-academic teaching hospital, then as a director at an academic training program, interspersed with work as a clinician in several private practice positions� With time it became clear what brought me the most satisfaction, making it easier to confidently choose a career path Sampling everything before deciding isn’t absolutely necessary, but the structure of our specialty makes it easy to do so if you choose�

What is the life of an academic medical director like? I work 40 to 50 hours a week, mainly because I work for the government (some academic directors work more, but likely make more money as well)


I also get a reasonable amount of time off and have a great deal of flexibility with my schedule� Forty to 50 hours a week is more than most pure clinical emergency physicians work, but only about one-third to one-half of my hours are clinical� Clinical hours in our crowded, high acuity public emergency department tend to be my most intense and fatiguing hours, although they are exciting and satisfying� The rest of my schedule and work focus is mostly dictated by me, save for a few standing meetings and the occasional deadline for a work product� This controllable pace in the office is a welcome contrast to the chaos of the ED I often find myself glad to get back to one of these activities after a stretch of doing the other, which provides a nice balance�
My administrative time is filled with many meetings Some are scheduled and some are impromptu, be they within our department, among hospital departments, meetings with hospital leadership, or occasionally at the multi-hospital level� Recently the chief medical officer of the hospital system invited me to investigate applying concepts of a department program I developed to the entire hospital system, giving me the opportunity to meet and collaborate with physicians from across the system This is an opportunity that could impact hundreds of physicians at a time�
I spend a considerable amount of time collaborating with my team, running the various parts of our ED, troubleshooting, designing fixes, and implementing them� We use a lot of data in deciding where the problems are and monitoring fixes, so data analysis skills are helpful (or at a minimum understanding how to use a spreadsheet)� I’m working with administrators and physicians from outside our ED to improve how the different medical services interface over patient care, including agreements on division of work� Communication with clinicians is a key aspect, and I’m involved in new ways of making administrative information available to clinicians when they need it, including collaborating with another physician on using a smart phone technology for this process�
Communication with clinicians is a key aspect, and I’m involved in new ways of making administrative information available to clinicians when they need it, including collaborating with another physician on using a smart phone technology for this process.
I am also involved with patient billing, and oversee the distribution of payments under an incentive plan for physicians� These and a myriad of short and longterm projects are always on my desk� Time management becomes a key skill for any administrator so that priorities can be kept and deadlines are met�
On top of all of this, we academic directors are primarily teachers� I spend a considerable amount of time preparing for teaching both in the ED and in formal didactic sessions� As the lead director, I’m responsible for most of the practice management educational curriculum, including job searching, contracts, negotiating skills, billing and coding, and personal finance Last but not least, academicians are responsible for the advancement of knowledge in emergency medicine (and like all academicians, the advancement of our academic rank) Writing and publishing may be a key part of your academic job, although this varies greatly by program Rarely I’m involved in actual research, but more typically I write book chapters and other monographs� I used to have a distaste for writing, but as I did more of it and saw how it also helped me in other areas of my job,
I began to enjoy it� Although you may not be required to do much publishing, you will most likely be involved in a significant amount of teaching�
Last but not least is leadership As we acquire experience, it is our obligation to help others who are in need of our expertise Leadership is one way to meet this obligation, and there are numerous opportunities I serve on the national committee that affects the practices and lives of thousands of emergency physicians, and it is a wonderful opportunity to give back to the specialty�
If you are still in training, seek out resources in your department to get a taste of the position� Talk to your clinical director about his or her job, and take advantage of any elective that may be available to you in ED administration� Volunteer on a project that is underway, or even design your own under the tutelage of the director and carry it out� Remember though that

the advantages of being a director may not be obvious during an elective, because most of the benefits are long-term (developing relationships in the hospital and the satisfaction from a successfully designed and implemented project) or just not visible (better hours, better control over your time�)
If you’re out of training, consider an assistant director position in order to learn from a more experienced director Taking on a full director position without experience is possible, but there is a steep learning curve Educational opportunities such as the American College of Emergency Physicians Director’s Academy can prepare you for the challenges of the position� A valuable reference is the textbook “Emergency Department Management” (see “Suggested Reading” at the end of this section ) It is an excellent guide on all the various aspects of the administrative skill set, laid out by experienced ED administrators�
1� Create the best position you can� I was curious early on in my career when I noticed a fair number of job advertisements for directors of EDs� I wondered why physicians already working in those EDs didn’t want to assume the director position The simple fact is that being made the director of an ED is not always a “promotion ” The position often comes with a host of tasks that the rank-and-file emergency physician wants nothing to do with� As I’ve moved through several director positions, I’ve realized that the key element in determining whether the job is an outstanding one or more of a drudge is understanding the full scope of your job and what each task entails� For more experienced candidates, this may mean ensuring certain undesired tasks (a common one is creating the clinical schedule) are delegated to others Early in your career you will have less ability to negotiate significant boundaries around your responsibilities, but it doesn’t mean you shouldn’t make an effort
2� Dress the part� It has been said that we dress for others, not ourselves Nowhere is this more true than in administration� When you dress professionally it sends a message to those you work with: that you are serious about your job, respect those you are meeting and working with, and are successful�
3� Develop a reputation as a problem solver, not a problem generator
4� Make yourself valuable to the department and the hospital This often requires a commitment to communication and making sure others know what you’ve accomplished
5� If you don’t have good people skills, work on them� If you can’t communicate with others in a way that facilitates rather than inhibits the collaborative process, you won’t be successful over the long term
6� Understand nursing administrative culture; they are often more regimented and can be less flexible Understand how this affects the nursing staff, both frontline clinical staff and nursing leadership� Earn their trust and engage them with a collaborative approach�
7� Value real-time communication� E-mail or texting can be very efficient when used correctly, but they have limits I’ve noticed that junior administrative staff may undervalue person-to-person communication and what it can accomplish A phone call, or in the right circumstances, an in-person meeting is absolutely necessary to efficiently and entirely complete a task� In addition, it helps to build relationships and shows commitment to the collaborative process�
Lastly, being an academic medical director doesn’t have to absorb your whole career� You always have the option of developing yourself in another direction in academia if operations does not suit you, or if you just need a break I spent many years as an ultrasound director between stints in operations Both moving into and out of this position were welcome changes at the time!
So, if you are a teacher (or think you might be), and see an exciting challenge in working in a collaborative environment to influence the setting in which other emergency physicians exist, then an academic medical directorship might be the career path for you�
Suggested Reading:
Strauss and Mayer’s Emergency Department Management� Strauss RW, Mayer TA (Eds�)� 1st ed� McGraw-Hill, 2014�
 By Donna Carden, MD, Professor, Department of Emergency Medicine, College of Medicine, University of Florida, Gainesville, FL.
By Donna Carden, MD, Professor, Department of Emergency Medicine, College of Medicine, University of Florida, Gainesville, FL.
The majority of advances in patient care, graduate medical education and healthcare delivery emerge from academic medical centers through biomedical, educational and health services research�1,2 For emergency physicians, an academic career provides opportunities to make new scientific discoveries that influence patient care in novel and substantive ways, to educate and train the next generation of providers, and to improve the overall healthcare delivery system�1 As such, an academic career is a creative, collaborative, problem-solving exercise that provides the opportunity to contribute to the greater good 1,3 Although potentially delightful and immensely rewarding, an academic career is time-consuming and requires skills and expertise not acquired through traditional medical school and residency training 4-8 Laying the foundation for a successful academic career rarely happens by serendipity but rather, requires thoughtful planning and a solid foundation that begins in the early attending years�
Laying the foundation of a successful academic career begins before taking the first faculty position and is predicated on several key elements relevant to a career in research, education or clinical operations� These elements involve a partnership between the faculty member and the prospective department and institutional leadership

Faculty Responsibility: The first responsibility of the new faculty member seriously committed to tackling an academic career is to define their own academic interest or focus� In academic emergency medicine, the focus might take the form of physician-scientist, clinician-educator, or clinician-educator-administrator and may be based on the faculty member’s unique skills, experience, prior training or simple curiosity Although it is preferable to identify an academic focus during residency training, it is not a fatal career flaw to leave the focus ill-defined at the first job interview However, new faculty should determine how committed the prospective department chair is to assisting junior faculty identify and nurture their career focus prior to taking the job Because academic practice plans for protected time and non-clinical salary support reflect the mission and vision of the department and institution, it is imperative that the early-stage faculty member inquire in detail about the practice plan when applying for and interviewing at a prospective institution�9 If the department and institution are unable to provide protected time and salary support or additional training and educational opportunities for junior faculty intent on becoming experts in their area of interest, it will be difficult to succeed in an increasingly competitive academic environment�4,9


The most important thing about a goal is having one The early-stage attending should establish approximately two annual goals that when woven together and successfully executed over five-ten years, become benchmarks on the path to a successful academic career (Table 1) This is a daunting but achievable task that requires assistance from mentors�
Because academic practice plans for protected time and non-clinical salary support reflect the mission and vision of the department and institution, it is imperative that the early-stage faculty member inquire in detail about the practice plan when applying for and interviewing at a prospective institution.
Time-Frame
1� Establish focus
2� Establish and articulate 1-, 5-, and 10 year goals
3� Identify mentors
4� Follow-through on commitments
5 Establish expertise
6� Publish
1� Define department/institutional priorities
2� Articulate expectations and benchmarks for faculty success
3� Provide protected time
4 Identify training and educational opportunities
5� Help set realistic, high-yield annual goals
6� Provide dedicated workspace
7� Provide administrative infrastructure
8� Facilitate mentorship
9� Support promotion and tenure
A successful academic career is a collaborative apprenticeship that requires strong mentorship 4,9 A mentee’s academic track-record begins to be established by training or even publishing with a mentor recognized for specific expertise The junior faculty member should seek out content, methodologic, career, and personal mentors 10 Not only should mentors outside the home institution be considered, but the ideal content and methodologic mentors may come from disciplines outside emergency medicine In fact, by strengthening translational and multifaceted research programs, interdisciplinary research collaborations can positively impact the likelihood of future research funding and thus, a successful long-term academic career�5
Another key element and faculty responsibility on the path to a successful academic career is commitment� Establishing a reputation as someone who completes assigned tasks may seem such common sense as to be unworthy of articulation However, follow-through on commitments is a nuanced faculty responsibility that can dictate career success� In other words, commitments should be carefully considered and chosen wisely
Becoming recognized as one who completes tasks on-time and produces an outstanding work product establishes trust and respect by the department chair, collaborators and mentors� However, junior faculty may be asked to take on high burden: low yield assignments that are detours rather than benchmarks on the career path� Establishing approximately two annual goals that facilitate longer-term career growth in collaboration with the department chair can ensure the early-stage faculty member’s time is spent effectively Aligning clinical, educational, research and administrative tasks can amplify early career productivity� Thus, committee work at the department, institutional, local, regional and national level are administrative tasks that should be aligned with faculty member’s focus and taken on early in the academic career Again, discussing annual goals and administrative tasks with the department chair and trusted mentors can ensure annual accomplishments become benchmarks on a successful career path rather than disjointed tasks that distract and exhaust the early-stage faculty Finally, commitment also means persistence and sustained effort despite inevitable false starts, blind leads, rejected papers and unfunded grant proposals
Although a rewarding academic emergency medicine career can be achieved without additional fellowship, certificate or graduate-degree training, success at the highest levels increasingly requires such expertise 4-8 Becoming an expert in a focused area requires earlystage faculty study and attending conferences on their chosen subject matter However, passive participation is insufficient to achieve real academic success� The successful academic emergency physician must move from passive learner to active scholar by innovating, writing, teaching, and speaking about their focus area The physician-scientist might consider formal research training, including a Master’s in Public Health (MPH), Master of Science in Clinical Epidemiology (MSCE) or Doctorate (PhD) degree� The clinical-educator should consider studying educational theory or obtaining an MPH or Master’s of Education (MEd) The clinicaleducator-administrator might consider a Master’s of Business Administration (MBA) Not all departments and institutions have the ability to support early-stage faculty, even those with exceptional aptitude and

commitment in such educational endeavors Thus, it is incumbent on the faculty member to inquire about additional training opportunities at the initial job interview and prior to taking the first faculty position
Scholarship is critical at all stages of an academic career, including the early post-training years Speaking at state and national conferences helps establish the faculty member’s reputation but the academic trackrecord is solidified by the publication record� Publishing with a mentor recognized for specific expertise demonstrates to outside review committees and funding agencies the faculty member’s capacity for similar expertise Scholarship describing increasingly focused scientific discoveries, educational innovations or health services research is expected as the career advances� However, the early-stage faculty member can focus on case reports and case series as well as systematic reviews to solidify their own knowledge and expertise in their focus area and to begin to formulate a scholarly track-record�
Department Responsibility: Nurturing exceptionally committed and capable junior faculty into successful academicians does not happen by chance� Great academic advancements are rarely achieved in 15-minute intervals between patients, on weekends or after grueling clinical shifts�1,3 Excellent research requires undisturbed time and space to fully develop, test, and hone an idea�3 Thus, junior faculty with demonstrated aptitude and commitment to an academic career require protected time from some clinical, teaching and administrative duties� It is the clinical revenue practice plan that provides salary support and thus, protected time, for nonclinical activities� The practice plan is often based on a clinical ‘tax’ that supports nonclinical activity, a base salary with annual merit awards for clinical or scholarly activity or some hybrid of the two�9 It is incumbent upon the department chair, in collaboration with institutional leadership, to distribute clinical revenues such that the department’s clinical, research, and educational missions are leveraged and maximized
Faculty require department support other than protected time in the early stages of their academic career and much of this support is provided by the department chair The training and educational opportunities available to faculty meeting well-defined benchmarks should be clearly articulated by the chair The department chair also plays a critical role in assisting early-stage faculty set realistic annual goals that are benchmarks on the academic career path Early-stage faculty also require dedicated workspace and an infrastructure of administrative and technical
support�4 The chair may also be in a unique position to facilitate connections between junior faculty and potential mentors at the home institution and on the broader national stage� Finally, the department chair must understand the institutional rules and culture of promotion and tenure and ensure early-stage faculty are on-track for institutional recognition as well as career advancement� In brief, the department and institutional commitment to the young faculty member’s career advancement is rivaled only by the faculty member’s commitment to their own academic trackrecord Building an academic career is a long-term partnership between faculty member and department and institutional leadership that begins in the early attending years
One of the key components of a successful academic career is obtaining funding to support research and educational activities 11 It is also well-recognized that the inability to obtain outside funding can stunt or derail academic growth� Well-funded and experienced mentors can help junior faculty identify and successfully compete for extramural funding� Department leadership also has a key role here by providing faculty with opportunities to attend grant-writing workshops or by providing seed funding for pilot or preliminary data� Despite the wellrecognized importance of obtaining research funding, the early-stage faculty member may benefit most from the very act of writing the grant proposal� Turning lofty ideas into a logical, succinct, well-written proposal is
Department Responsibility: Nurturing exceptionally committed and capable junior faculty into successful academicians does not happen by chance. Great academic advancements are rarely achieved in 15-minute intervals between patients, on weekends or after grueling clinical shifts.
likely to shed light on untestable hypotheses, gaps in logic, inadequate methods, uncertain outcomes or questionable significance� Allowing sufficient time for review and revision by mentors and colleagues requires self-discipline These lessons are invaluable to the early-stage faculty member, regardless of the ultimate funding decision
Laying the foundation of a successful academic career begins during or immediately after residency or fellowship training, escalates rapidly in post-training years 2-5, and often extends through post-training year 10�1 Dwindling national research support and clinical reimbursement are challenges on this long and arduous path to academic success�1,12 While the level of National Institutes of Health funding available is out of the control of the individual investigator, there are other factors that influence the academic career path of promising academicians that are under the proximal control of the faculty member, department and institution�
Key challenges that can derail an academic career include insufficient time to fully develop and test research ideas, unstable funding, lack of
committed mentors, competition with better-trained scientists, burdensome regulatory compliance, and insufficient support from the home institution�1 Many of these obstacles can be minimized by strategic planning by the faculty member and department and institutional leadership� Both faculty member and department leadership must recognize the importance of dedicated time and work space, and the special training and expertise required to become a successful academician Department or institutional administrative infrastructure can allow junior faculty to be mentored through challenges including regulatory compliance; leaving more time to focus on grant and manuscript writing� Institutional support in the form of bridge funding, on-site collaborations and mentorship also contribute to academic career success 1 The successful academic career requires similar time, effort and dedication as clinical training� Success is rarely achieved as a part-time activity or by chance Understanding and embracing the rigors of an academic career path and searching out departments and institutions that provide opportunities for career advancement lay the foundation of an academic career
References:
1 Tong CW, Ahmad T, Brittain EL, et al Challenges Facing Early Academic Cardiologists Journal of the American College of Cardiology Jun 3 2014;63(21):2199-2208
2 Nabel EG, Braunwald E A Tale of Coronary Artery Disease and Myocardial Infarction The New England Journal of Medicine Jan 5 2012;366(1):54-63
3 Justice AC Leaky pipes, Faustian Dilemmas, and a Room of One’s Own: Can We Build a More Flexible Pipeline to Academic Success? Annals of Internal Medicine Dec 1 2009;151(11):818-819
4 Perry JJ, Snider CE, Artz JD, et al CAEP 2014 Academic Symposium: “How to make research succeed in your emergency department: How to develop and train career researchers in emergency medicine” Cjem May 2015;17(3):334-343
5 Kaji AH, Lewis RJ, Beavers-May T, et al Summary of NIH Medical-Surgical Emergency Research Roundtable held on April 30 to May 1, 2009 Annals of emergency medicine Nov 2010;56(5):522-537
6 Ling LJ Proceedings of the Future of Emergency Medicine Research Conference, Part I: Executive Summary Academic Emergency Medicine : Official Journal of the Society for Academic Emergency Medicine Feb 1998;5(2):147-151
7 LaMantia J, Deiorio NM, Yarris LM Executive summary: Education research in emergency medicine-opportunities, challenges, and strategies for success Academic Emergency Medicine : Official Journal of the Society for Academic Emergency Medicine Dec 2012;19(12):1319-1322
8 LaMantia J, Hamstra SJ, Martin DR, et al Faculty development in medical education research Academic Emergency Medicine : Official Journal of the Society for Academic Emergency Medicine Dec 2012;19(12):1462-1467
9� Bagai A, Udell JA� Academic Practice Plans for Early Career Clinician Investigators: The Fourth Pillar of Success� Journal of the American College of Cardiology Oct 20 2015;66(16):1839-1841
10� Lynne Richardson M, FACEP� Building a Career in Academic Emergency Medicine� 2014�
11� Chitnis PR� Grants: A key ingredient for a successful academic career� Faseb J� Apr 2007;21(5):A95-A95�
12 NIH Table #206 Competing Applications, Awards, Success Rate and Total Funding by Application Type, NIH Institution/Center and Activity Code Fiscal Years*2003-2012 Office of Statistical Analysis and Reporting; 2013

The advancement from Assistant to Associate professor within the medical school is a leap much greater than you probably can anticipate So, if this is your goal as an academic emergency physician, you must start the process now Most departments will assign you an initial rank of Clinical Instructor or Assistant Professor After this, the promotion/tenure (P/T) process is individual to each institution� It usually is about 7-8 years and the process itself from beginning to end can take up to 18 months or more This variability should encourage each faculty member to become familiar with their institution’s by-laws, learn about the promotion process, and understand what constitutes scholarly activity within their academic environment� Our training rarely or incompletely prepares us for the specifics of career advancement in the academic arena As the complexities and variability of our jobs increase, even the most talented amongst us need guidance and careful attention to career development� We are all
unique in our interests and will require a well-thoughtout career plan The process should have measurable goals, frequent re-assessment, and effective mentoring� Discipline will be a key predictor for success as our time is limited and demands are constantly increasing The objectives for this chapter will be to:
1� Define, in general, the requirements of an institution’s Promotion and Tenure Committee
2 Become knowledgeable about what documentation you will need
3� Identify areas of interest and career focus
4� Organize a portfolio for achievements, certifications, letters, evaluations, contacts, etc that can be used for supporting documentation
5� Define a networking system with other faculty who have advanced to the Associate Professor level and establish supportive relationships
6� Recognize the importance of volunteering and becoming involved in both regional and national organizations that represent our specialty
The P/T committee is made up of faculty members who have already achieved promotion and may be tenured These individuals are charged by the institution with the task of insuring that all faculty who are promoted have achieved expertise in an academic area, demonstrated their effectiveness in teaching, fulfilled clinical service requirements, and contributed in a meaningful way to the mission of the institution�
To get started, you will first need a letter from the sponsoring Department Chair which clearly identifies the promotion to Associate Professor and professional category� Each institution will have different names or titles for these specific categories They may be defined as medical educator, investigator, clinician investigator, clinician scholar etc� or they may be simply defined as a clinical track or a traditional track Make sure you know in which category you’re applying� As an example, a Research-Educator track is intended for individuals who may have a doctoral rank in both basic science and clinical departments with a major career commitment to basic science or clinical research that is likely to result in funding by peer-review granting agencies� The second track, identified as the Clinician-Educator track, is intended primarily for clinical faculty and represents a scholarly academic track of equal stature/status as
the Research-Educator track� Both research and service activities are required
Most academic medical centers have goals that require mastery in three areas: patient care, education and research This “triple threat” was obtainable in the past but has been increasing difficult for individual faculty to contribute to all three� Faculty members may need to focus their efforts in one or two of these academic arenas� For the most part, most faculty focus on patient care and research or patient care and education One of the issues facing faculty who wish to be promoted is that the Promotion and Tenure Committees tend to value patient care and research over the latter 1-4 A report from Johns Hopkins found that the chances of having a higher academic rank were 85% lower for academic clinicians and 69% lower for teacher-clinicians than for research faculty�1 Faculty who spend more than 50% of their time caring for patients were more likely to be on a non-tenured track and showed slower career progression than those who spent less than 50% of their time caring for patients 2 In addition, time to promotion was significantly shorter for those who spent 80% of their time in research than those whom spent 30% or less� It has been reported that rates of promotion were slower, even with defined criteria and tracks within the clinician-educator faculty This delayed promotion may be related to longer periods of time required for identification and development of expertise in either clinical or educational areas�4 Some institutions have yet to define standards for early advancement for faculty in the above track
Required documentation for the Promotions and Tenure Committee will include, but may not be limited to, the following:
1� Detailed and comprehensive letter of recommendation from the Department Chairperson� The letter should include a qualitative and quantitative assessment of your clinical, teaching, research and administrative contributions to the School of Medicine, its affiliated institutions and any other local, state, national or international activities�
2� Curricula Vitae, including Bibliography (the bibliography must include complete title, bibliographic citation, and date)� Manuscripts in preparation are not allowed�
To get started, you will first need a letter from the sponsoring Department Chair which clearly identifies the promotion to Associate Professor and professional category.
3 Summary of Teaching Responsibilities indicating evidence of teaching quality and teaching quantity�
4� Summary of clinical responsibilities�

5� List of at least six outside authorities of the same rank to which you are applying, four internal (your University faculty) authorities and usually eight students or residents that you have had contact with during your career The Promotions Committee will decide whom they contact for letters of recommendation from a list you may provide The recommender is often someone you have never worked with clinically but may have collaborated with on a project Copies of your most significant manuscripts (original research papers are most important to the Committee, book chapters less so) Manuscripts in press must have an editorial acceptance letter�
Keeping track of all scholarly and administrative activity will be invaluable Develop a portfolio to document every lecture, all teaching/lecture evaluations, awards, CME certificates, special training, Press-Ganey reports, medical student and resident evaluations, and all publications and on-going projects� In light of the ACGME Core Competencies and the more recent Milestones Project many faculty have developed innovative ways to evaluate and measure these six competencies Working with the Residency Program Director and Core leadership faculty and assessing their needs for innovative approaches to the advancement of residents may prove invaluable� Keeping in contact with former residents and faculty as well as current faculty that can attest to both your teaching excellence and academic success will be paramount in the promotion process These residents and faculty should span your entire time at the institution and include several “senior” faculty (faculty with academic rank of Associate Professor or Professor)
Keeping track of everything you do as a faculty member will be a key to your successful rise up the promotion ladder Areas involving teaching can include
lectures, CME, bedside teaching evaluations, curricula development, awards and new innovations in teaching� These become even more important as we begin to measure outcomes in the general competencies As an example, if you participated in an educational activity such as a simulation session or a large animal lab teaching procedures, it would be important to have a letter or email from the director of the educational activity Keep all this documentation in a portfolio We all do more teaching and spend more time than we will remember over the course of our academic careers and leaving this documentation to memory will render its scope incomplete�
Mentoring is recognized as a crucial component of professional development in the field of academic medicine� For junior faculty hoping to progress from Assistant to Associate professor, establishing relationships as both a mentee and mentor are critical Those whom participate in a formal mentoring program as a mentee have self-reported perceptions of improved career development, as well as improved knowledge, skills, and attitude in professional development and scholarship (Fleming 2015; Kashiwagi 2013)
Additionally, participation as a mentor to junior faculty and learners in your department is viewed by others as a significant positive contribution Mentoring can include medical student advising and mentoring junior faculty and senior residents Get involved with your school’s Emergency Medicine interest group Many medical students, interested in Emergency Medicine, are looking for faculty knowledgeable about the application process and other Emergency Medicine programs� Most medical school Deans holds a lot of stock in educating and advising medical students and your participation becomes noticed� Being a member of the medical school admissions committee will help you become acquainted with other faculty within the medical school including both those in the basic sciences as well as clinical faculty Building these bridges and developing relationships with others not only in Emergency Medicine will ultimately be a bonus
Administration can be a large part of any core faculty’s time but may be important in contributions to the Department and relationships formed with other faculty within the University� Volunteering for medical school committees such as admissions (as mentioned above), graduate medical education, resident education, and residency leadership committees are all areas where your leadership skills can be developed Assistant, Associate or Program Director positions can aid your advancement within the administrative arena If your research interest is in an area that is tied to the hospital’s administrative mission, this can work to your advantage It is important to gain recognition in your community in which your work�
Appropriate scholarship has traditionally been evidenced by publications of original research in peer reviewed journals� Large-scale blinded randomized controlled prospective clinical trials are often most revered in clinical research and by the promotions committee� Research focus in a particular area is highly desirable and increases the potential for external grant support and promotion� Many institutions will only award tenure to those who can demonstrate ability to obtain funding through outside grants Recently, the definition of scholarship has been expanded to include published curricula, syllabi, web based publications and other multimedia materials that have been used for teaching Peer-reviewed publications, case reports, book chapters, and case-review articles all contribute to scholarly productivity� Participation in editorial services for specialty journals in Emergency Medicine is always of value�
In conclusion, the faculty member who wishes promotion to the Associate level needs to obtain a mentor and develop a plan, generally formulated in conjunction with his/her Chair, to determine what will be expected prior to being recommended for promotion to the Associate Professor level� As
mentioned, this plan may involve a specific window of time This is especially true in institutions whose by-laws demand that all faculty members be tenured� This clock is usually set between seven to nine years� This means that the faculty member must complete all of the requirements for promotion within that time period or leave the faculty To avoid this concern, academically oriented Emergency Physicians should understand the consequence of accepting a tenure track appointment The advantage of this system is that pressure is placed on the department to ensure promotion and the department chair not only becomes expert in helping faculty accomplish the tasks that are necessary, but also is closely involved in monitoring progress The faculty member may feel a great deal of pressure to engage in research, obtain grants, and publish in peer-reviewed journals Many faculty members, with the support of their chair, choose the non-tenure track position� Non-tenure track positions don’t usually dictate specific time frames for promotion� However, the chair may not monitor or encourage faculty performance leading to promotion as carefully as she/he would monitor tenure track faculty Additionally, the faculty member may not feel the same amount of pressure to be promoted and so may not work as hard in the scholarly arena�
Attaining promotion to the level of Associate Professor requires careful and thoughtful planning the moment you take a position and engage in an academic career track� Participating in activities that allows a faculty member to demonstrate teaching excellence and a focus of scholarly activity is essential� Clinical excellence is a requirement unless one is solely in the Research Track and has no clinical requirements Documentation of accomplishments that demonstrate to the institution the faculty’s value and their scholarly achievements are mandatory� The rewards of achievement are well worth the effort for they attest to recognition by the academic community that a faculty member has been successful in adding to the value of that community and helping fulfill the institution’s mission of teaching, research, and service�
References:
1 Thomas, PA, Diener-West M, Canto MI, Martin DR, Post WS, Shrieff MB “Results of An Academic Promotion and Career Survey of Faculty at the Johns Hopkins University School of Medicine” Acad Med 2004; 79258-264
2 Buckley LM, Sanders K, Shih M, Hampton CL, “Attitudes of Clinical Faculty About Career Progress, Career Success and Recognition and Commitment to Academic Medicine: Results of a Survey” Arch Int Medicine 2000; 160:2625-2629
3 Levinson W, Rubenstein A “Mission Critical-Integrating Clinician-Educators into Academic Medical Centers” N Eng J Med 1999; 341:840-843
4� Kelly WN, Stross JK, “Faculty Tracks and Academic Success” Ann Int Med 1992; 116:654-659�
5� Sheffield JV, Wipf JE, Buchwald D, “Work Activities of Clinician-Educators” J Gen Intern Med 1998;13;406-9�
6 Kashiwagi DT, Prathibha V, Cook DA, “Mentoring Programs for Physicians in Academic Medicine: A Systematic Review” Acad Med 2013; 88:1029-1037�
7 Fleming GM, Simmons JH, Xu M, Gesell SB, Brown R, Cutrer WB, Gigante J, Cooper WO, “A facilitated peer mentoring program for junior faculty to promote professional development and peer networking” 2015; 90(6):819-826
 By John E. Prescott, MD, Chief Academic Officer, Association of American Medical Colleges, Washington, DC
By John E. Prescott, MD, Chief Academic Officer, Association of American Medical Colleges, Washington, DC
Introduction
No one enters Emergency Medicine with the goal of being a dean� Yet over the past twenty years, more and more academic Emergency Physicians are being presented with the opportunity of contributing to academic medicine through this unique pathway� Who ends up being a dean? What’s it like? When does one have to make this career choice? How does one become a dean? And finally, why would an Emergency Physician choose this career pathway? This chapter will answer these questions and offer some additional insight into the “life of a dean ”
The organizational structure of most medical schools is dependent on the leadership provided by departmental chairs, center directors and deans (assistant and associate)� Chairs lead discreet departments that correlate with specific academic disciplines Center directors often lead multi-disciplinary or interdisciplinary functional units� Academic deans usually coordinate and lead traditional mission-based activities such as research,
education, and clinical service as well as other key organizational units such as faculty affairs, student affairs, and diversity

Perhaps it’s my many years living in Washington, DC that have influenced my thinking, yet I have found it useful to describe the governance of medical schools by drawing parallels to the leadership that exists at state and federal levels� The role of the chair parallels that of governors; each has operational responsibility for a defined organizational unit� Center directors are like cabinet secretaries and often have direct influence over large entities with a specific focus Assistant/associate deans closely parallel senators in that they have little direct operational control of an organization, yet they possess great power in influencing and directing actions across the country/school�
As of February 2016, there were six Emergency Physicians leading medical schools as dean In this capacity, they serve as the chief academic officer for their institutions and are responsible for ensuring the success of a large, highly complex, and constantly evolving academic enterprise� Most school deans have
previously served as chairs of academic departments and/or served as associate deans�
All of us wrestle with questions about our career paths, and I truly believe we often end up in our roles through a combination of motivation, opportunity, fate, preparation, and perseverance� Never in my wildest dreams as a medical student did I see myself as a leader in academic medicine, yet somehow it happened� Later in my career, the thought of serving as associate dean never crossed my mind as I became founding departmental chair� As dean I tried to anticipate what surprises I would encounter next in my career, and today I’m still seeking answers�
Over time, I’ve come to better understand myself� I have always enjoyed leading and have consistently looked for opportunities to serve others EM was still in its infancy when I completed my residency training, and there was a great push for graduates to assume leadership in EDs and to develop academic departments� Just as others have unique clinical, educational, and research abilities, I had a skill set that helped to enable
individuals to organize and develop strategies to move our new Emergency Department forward
Individuals who want to serve as an assistant/ associate dean are likewise seeking a way of contributing more to their institution Sometimes, they have been asked to fill an open position as an interim and have found the experience challenging and fulfilling� And for others, this is a natural next step in their career progression within a given mission� Many individuals serve their school in this capacity for years and both the school and dean are content with this arrangement For others, the position is one that will eventually lead to even greater responsibility within the institution Still others, once they have tried the administrative aspects of academic medicine, are certain they want to return to their prior careers
If you want to serve as a medical school dean, you must carefully assess your desire, motivation and strengths You must know your “comfort zone” – what is it that you like to do? What are your strengths? What are your weaknesses? Will your ego get in the way? Do you have the required skill set?
If you are seeking control and power by becoming a dean, choose another career path� Deans have more influence than direct control and chairs and university presidents quickly discern which deans serve the institution and which deans serve themselves
Seek mentorship and advice from those who currently hold the position within your academic institution and from the outside� Find out what it is that keeps them going and what it is that has allowed them to succeed� Also, speak with those who have decided not
to become a dean� There are many chairs in EM who have consciously made the decision not to move into the dean’s office – why is that so? A good friend of mine once reminded me that just because I could do a particular job didn’t mean that that job was right for me
Understand what your family wants to do and is prepared to do – pursuing a deanship is truly a family decision and will affect each and every member If moving is out of the question – that factor must enter into all of your decision-making You become a very public figure not only within the university setting but within your state and even nationally�
Serving as dean was one of the most challenging yet fulfilling jobs I’ve ever had� Like the practice of EM, being a dean is a constant challenge with new twists and turns every day No matter how carefully you plan a day or a week, there are always unexpected challenges and opportunities that keep the job fresh and invigorating As is the ED, there are systems and protocols to assist you to be more effective and efficient but sometimes they are simply overwhelmed by circumstances Being dean is not for the faint-hearted – it is no gentle canoe trip across a calm lake Rather, it is white-water rafting at its most challenging – even with the best skills you are going to get wet� The key is to stay safe, remain in the boat, and enjoy the ride
As dean, you are expected to set the vision for the school, be a good steward of resources – facilities, personnel, and money, and you have to recruit, retain, and develop the very best talent that you can Everything you do as dean falls into these categories�
If you want to serve as a medical school dean, you must carefully assess your desire, motivation and strengths. You must know your “comfort zone.” What is it that you like to do? What are your strengths? What are your weaknesses? Will your ego get in the way? Do you have the required skill set?
Consistent, sincere, and clear communication throughout the institution is key to your success The most important skills for the dean include the ability to listen, make fair and objective decisions with incomplete information, set high expectations for performance and to be available for guidance and mentoring – not at all unlike the skills of your average Emergency Physician
By default, by the time issues rise to your attention as dean, they have been unsuccessfully addressed at other levels Simple “black and white” questions give way to many “gray” concerns and a strong set of personal and institutional values, based on your school’s mission, is needed to center you and your decisions These values also assist you in working with all of the big egos that present to your office, often seeking resources that benefit only a few individuals or a particular section/ department� As dean, you must remind others of their responsibility to work for the betterment of the institution� Your perspective must cross disciplines and missions and you must have the vision and willpower to know when and how to get the best out of individuals and how to give them someone and something to believe in
To be successful, you must be good at delegating and have good people surrounding you that you can trust� Like the physician in charge during a mass casualty incident, the dean loses effectiveness if he/she is providing direct care� The dean must be the one leading, directing, and inspiring others
Personnel issues take up more time than imagined and physicians are not usually adept at dealing with them Most of us have received little formal training in evaluating, mentoring and counseling individuals, but it is absolutely essential that you possess these skills as dean You must be able to draw out the best in
individuals as well as how to hold them accountable for their actions and decisions Look for opportunities to enhance these skills�
As dean, you must get comfortable with the fact that your work is never done and the demands of the position can have serious consequences on your family� The “shift” never ends and if your schedule is left unchecked, it will consume you and all of your personal time� Time off and away from the office and university/school events must be rigorously enforced to ensure your long-term survival and happiness with the position� Being dean is like being in a marathon – so think in terms of running a marathon that never ends All Emergency Physicians have “burned the candle at both ends” for a short time, when you’ve had to assist others due to unexpected staffing shortages or a family emergency� However for the dean, this practice will lead to marked inefficiency and lessened effectiveness Long-term success as dean depends on maintaining your health despite an overloaded schedule full of unhealthy breakfasts, lunches, dinners, and social functions
First, there must be a strong personal desire, and that desire must be built around an understanding of the job – the prerequisites, the commitment, the challenges, and the expectations� Others must believe in you and you must have the confidence that you can do the job
Get experience at leading – most deans have been department chairs and this experience has given them knowledge of personnel issues, operations, academic issues like promotion and tenure, faculty development, and departmental/school finances�
If you are particularly strong in one of the three traditional missions – maintain that strength but
First, there must be a strong personal desire, and that desire must be built around an understanding of the job – the prerequisites, the commitment, the challenges, and the expectations. Others must believe in you and you must have the confidence that you can do the job.
To be successful, you must be good at delegating and have good people surrounding you that you can trust.
seek ways to enhance your knowledge of the other missions� My own experience was that I had a great deal of knowledge of our clinical mission and certainly knew the finances of the school� I had to plot out how to get additional information regarding research and education
My formal preparation began while being chair and really took off as an associate dean and CEO of the faculty practice plan My life experiences in college, medical school, the Army, and as a new faculty member also presented me with a host of leadership opportunities Learn from past mistakes and gain a reputation for listening, approaching difficult issues with an open mind, and for achieving clarity in assigning responsibility�
Once you’ve chosen this career path, learn everything you can about it and become known in your field Prospective deans need to make their name outside of EM, and they have to be able to demonstrate an appreciation of all the missions of the school or academic enterprise�
Seek additional responsibilities by speaking with your chair and dean� Letting them know of your interest can pay off in a major way when a new opening occurs or opportunity develops� They can also assist you in identifying programs that will help enhance your skills�
Test the waters The AAMC’s Council of Deans has a yearlong fellowship program for those interested in becoming dean� For women, the Executive Leadership in Academic Medicine (ELAM) program offers an outstanding curriculum� Update your CV and keep it current - opportunity has an uncanny ability to strike at unusual times
Attend non-EM focused academic meetings and head to the AAMC’s annual meeting to make national contacts and gain a broader perspective Alternatively, serve on a national committee� The exposure is good for you as an individual and for your department and school
An individual once recommended to me that I should expand my thought processes beyond medical journals and a weekly newsmagazine� I subscribed to FORTUNE

and the Harvard Business Review and soon found myself adopting innovative ways to address problems
The six Emergency Physicians who served as deans of their medical schools have approached this question with different solutions All face similar demands on their time and all have dramatically curtailed their clinical, teaching, and research activities due to the administrative demands of the job� But each has maintained some contact with their specialty – whether it be the occasional shift in the ED, teaching students or residents, or maintaining their scholarly activity
During the five years immediately preceding my becoming the dean, I served as clinical associate dean and as the President/CEO of our faculty practice plan As I accepted my new responsibilities, I simultaneously stepped down as chair and subsequently there was a gradual decline in my active participation within the academic department� This was difficult for me because I enjoyed my time in the ED with the residents, and as an Emergency Medicine faculty member, I took great pride in literally knowing the names of all of the house staff in every specialty But because of my new responsibilities, I had to cut back my clinical and educational tasks and soon had a difficult time knowing even the names of the EM residents I remember asking myself, “Was I ready for this?” – and honestly my answer was “Yes and no ”
Well-meaning individuals often ask, “Do you miss being a doctor?” My answer is that I’m still a practicing physician but with a different set of patients and priorities I’ll certainly never stop thinking like a physician and hope that I never stop thinking like an Emergency Physician
Can I still recognize a sick patient from across the room? Absolutely� Do I hesitate to act when I see a patient in an emergent situation? Never But if I’m honest with myself and ask if should I be mentoring and guiding the rising generations of EM residents in the ED, the answer is clearly no - my skill set has changed� This does bother me to a degree but times have changed, and I have accepted that I do remind myself that one new benefit is that I’m often given the opportunity to teach across all specialties and across generations of physicians
Finally, as dean, those occasional shifts were good for me and there were some unanticipated benefits to working in the ED� I found out first-hand about key issues – problems with consultants, patient flow, and I learned about new treatments, etc And when you are dean, there is nothing quite like calling a consultant and asking them to see a patient in the ED Delays almost never occur and the EM residents and staff love to see that�
Academic medicine is undergoing profound changes and the role of the dean is constantly evolving� While all medical schools seek to educate physicians prepared to meet the health needs of our nation, they vary in the degree to which they emphasize research, clinical care, and community outreach Resources, organizational complexity, and the school’s position within healthcare delivery systems will be unique factors facing every dean As institutional leaders, deans must be prepared for ongoing change and challenges
What does one do after being a dean? Sometimes deans are asked to take on additional leadership responsibilities within their university or health system Others move to on to assume openings at a national level in academic medicine, the government, or within healthcare Some return to the faculty to return to clinical care or to pick up on projects and/or research that was placed on hold�
Dean’s jobs can end rather unexpectedly, usually as a result of a change in leadership at the university or health system level� Individuals should not define themselves by their job or its title but rather by those all-important individual characteristics that make them unique In reality, this is easier said than done The vast majority of former deans find new roles that draw on their leadership experience�
I absolutely believe that my decision to enter Emergency Medicine prepared me well for my role as dean, and I wouldn’t trade any of the experiences I have had in the 30+ years since I left my residency program� Nor would I trade the opportunity I had to serve as dean� It was a uniquely fulfilling experience that allowed me to provide service to others at the highest level, even as it prepared me for new challenges and undertakings Thus, I look eagerly forward to other Emergency Physicians joining the ranks of the Council of Deans�
 By James Hoekstra, MD, Vice President for Network Clinical Affairs, Professor of Emergency Medicine, Wake Forest Baptist Health, Winston-Salem, NC.
By James Hoekstra, MD, Vice President for Network Clinical Affairs, Professor of Emergency Medicine, Wake Forest Baptist Health, Winston-Salem, NC.
Academic Emergency Medicine continues to grow and mature, from its infancy in the 1970s to its present stature as an established force in academic medicine� This growth is evident in the growing number of training programs, faculty, and academic departments It’s also evident in the quality of our residency recruits and the growth of our clinical programs� At the same time, the quality of research and scholarly productivity in academic EM is steadily improving With the growth of any medical specialty, there are strengths, weaknesses, opportunities and threats to our continued success� How we navigate the academic and clinical minefields in the next few decades may well determine whether or not we meet our potential� Healthcare in the U�S� is undergoing remarkable changes, with the advent of the Accountable Care Act, the move to value, and the financial pressures on healthcare and health systems These market forces will continue to pressure emergency medicine, as it solidifies its niche in the healthcare ecosystem

The volume of patients accessing emergency departments throughout the country has continued to grow at an inexorable pace� According to the National Hospital Ambulatory Care Survey, ED volumes have increased nationally at about 1 5% per year, to a total of 136 million visits in 2012, or 44 visits for every 100 persons� Of these visits, approximately 84% take place in large cities, and 17% are in teaching hospitals� The latter statistic illustrates the crucial role of academic emergency departments in the provision of emergency care in the US
The demographic trends in the US population predict continued growth in ED utilization over time as well As the population ages, the need for ED utilization also grows� In the last decade, the percentage utilization of the ED by persons over 65 years old has increased to 15%� Patients over 65 are more acutely ill, have more co-morbid conditions, and require the use of more technology and diagnostics which are only available in an ED These factors result in an almost 40% ED admission rate for elderly patients�
The increasing utilization of diagnostic technology and access to specialists are also tightly linked to increased ED utilization� The rapid accessibility of MRI, CT, nuclear imaging, etc, is only available in the ED setting� As long as EDs retain the relatively exclusive access to real-time, after-hours diagnostic and therapeutic technology, ED utilization will continue to grow� Academic emergency departments are usually on the cutting edge with diagnostic and therapeutic applications, and are therefore better equipped with diagnostic technology than their community counterparts, leading to a disproportionate share of the technology-driven growth of academic emergency services� Similarly, the continued specialization of medicine favors the growth of emergency medicine� Patients with specific complaints related to their specific illnesses, when given a choice, prefer access to specialists for their treatment� This preference for specialization favors the continued growth of academic emergency departments, where access to specialists of all types is more possible�


The volume of patients accessing emergency departments throughout the country has continued to grow at an inexorable pace.




























Since the first EM residency program was initiated in 1970, there has been steady growth in the number and quality of EM teaching programs� At present, there are over 230 EM residency programs, with over 2400 residency slots available each year through the match� The positions in the EM match are being filled by higher and higher quality candidates There was a 99 6% fill rate in the 2015 NRMP match, with 79% filled by US graduates�


In the scholarly arena, research in emergency medicine continues to flourish� In the 1980s, it was rare for an emergency physician to be federally funded through the NIH or CDC� At present, there are over 70 NIH funded investigators in EM, with over $39M in annual support� The NIH has created an Office for Emergency Care Research, which will work with EM to grow funding opportunities for acute illness and injury trials It also funded a K-12 fellowship training program for emergency
medicine career development� Finally, the acute illness and injury research consortiums like NETT, CPCCRN, ROC, etc� continue to grow� Emergency physicians are also taking advantage of grant opportunities through PCORI, which funds research on patient-centered outcomes in acute illness� Given that clinical care is our strength, and access to patients with acute illness is greater in the ED than anywhere else, EM funding for clinical research should continue to grow�
Internal or foundation funding sources such as the SAEM Research Fund and Emergency Medicine Foundation (EMF) also provide training grants and mentorship opportunities for emergency physicians who are interested in developing their academic skills These grants provide funding for career development of emergency physicians, regardless of disease state or topic-specific funding restrictions Their success is well documented, and their funds should continue to grow�
We are in the midst of unprecedented change in medicine� The U�S� healthcare system is too expensive, and is growing at an unsustainable rate The Accountable Care Act and subsequent Medicare and Medicaid changes have resulted in declining reimbursement, uncompensated care mandates, quality penalties, and complicated over-regulation� These forces have placed enormous financial pressures on health systems, forcing them to look for alternative methods of containing cost and increasing revenue The result has been a “move to value” which strives for the triple aim of increased quality, decreased cost, and increased patient satisfaction Medicare, Medicaid, and managed care payers are moving to more aggressive quality incentives, gain-share and risk-based payer contracts, and a return to the days of capitation The
move to value has placed a target on emergency medicine and emergency departments, which are seen as high cost centers ED utilization reduction is a common strategy in value based payment systems, from Medicare Shared Savings Programs to Medicaid Advantage to managed care capitation� This will be our challenge in the next decade, to not only justify the cost of emergency care, but to work with our primary care colleagues and ACO leadership to reduce readmissions, decrease avoidable admissions, and improve communication and transitions of care from the ED to the outpatient setting� Emergency medicine needs to take a lead in reducing costs for the patients under our care, while maintaining quality and patient satisfaction�
One such cost reduction opportunity is observational medicine� The diagnostic technologies that are brought to bear on our patients often require an extended length of stay, beyond the traditional ED stay� Serial

examinations, serial blood testing, MRIs, CTs, and nuclear medicine studies all add to the ED length of stay; making it difficult to balance the need for speed in ED throughput with the need to justify medical necessity for hospital admissions Observation units, run by emergency physicians, with the ED as a gatekeeper, provide such a clinical service Chest pain, asthma, CHF, syncope, TIA’s, intoxications, abdominal pain, gastroenteritis, etc� can all be easily managed in a short stay, intensive diagnostic or therapeutic setting, avoiding admission or readmission scenarios�
Another example of cost reduction in EM is the provision of multidisciplinary care in the ED to reduce admissions for patients who are socially challenged or medically complex� Working with social work, care coordination, pastoral care, or home health to place patients in hospice, nursing homes, or other alternative settings of care reduces hospital admissions and reduces costs, while increasing patient satisfaction Access to an observation unit is extremely helpful in these patients, given that their lengths of stay can be prolonged
Although EM has classically been centered on acute care, the move to value has resulted in some ED’s actually providing preventive care� Preventive care measures include smoking cessation education, alcoholism screening, HIV screening, immunizations, hypertension screening and referral, adult pneumococcal immunizations, referral of children without primary care physicians to a continuing source of care, identification and counseling of geriatric patients at risk of falls,
Pap tests in women having a pelvic exam in the ED, counseling for smoke detector use, routine social service screening, depression screening, domestic violence screening, safe firearm storage counseling, motorcycle helmet use counseling, and youth violence counseling programs are also possible and have been instituted� In so doing, EDs become a provider of public health, reducing adverse outcomes and cost for a population under care�
Emergency physicians should take leadership positions in their local ACOs, clinically integrated networks, and hospital quality committees� We must do our part to increase quality and reduce cost while meeting our quality benchmarks, improving ED throughput, and increasing patient satisfaction�
In general, anything that threatens emergency medicine’s ability to provide care for patients in the ED is a threat to academic emergency medicine� This includes both financial threats as well as direct competition from other specialties ED boarding of admitted patients is a huge threat� Declining reimbursement is a huge financial threat Competition for our patients by primary care centers, after hours urgent care centers, or other hospital systems is a threat� Whereas these threats are real, they are also quite obvious to all participants, and probably don’t require much discussion� There are a few threats to academic emergency medicine that are “sleepers” however, which we must guard against�
First, we must maintain our focus on the provision of emergency care, any time, any disease, regardless of our patient’s payer status or social acceptability. When we stray from these principles, we will stray from our most important duty, which is to our patients.
First, we must maintain our focus on the provision of emergency care, any time, any disease, regardless of our patient’s payer status or social acceptability� When we stray from these principles, we will stray from our most important duty, which is to our patients Maintaining this high ground will forever give us credibility with our peers and our patients Academic medical centers and academic EDs provide the foremost examples of these principles in action�
Second, we must continue to search for new opportunities to expand or redefine our clinical niche, while we respond to the changing forces in healthcare� Many of the opportunities will be provided out of the clinical needs of our patients and the clinical needs of the health system� Failure to seize new opportunities for filling clinical needs for our patients is a shortsighted strategy what will lead to unmet potential for our specialty� Failing to respond to the rapid development of “value based care” with new and different care models and strategies to reduce cost and increase quality will result in marginalization of our specialty as a “high cost” center
Third, in the research arena, we must apply our clinical strengths to research in clinically relevant acute illness� Our strength is access to the patient with acute illness, at a time when diagnostics or therapies which can have the most effect, are most efficacious� We must search for collaborations with other specialties which can enhance our care, at the same time that we can help them have access to acutely injured and ill patients Emergency medicine was not created in a specialty vacuum, but to enhance the care of patients
in all specialties� Research involving these therapies should either involve or be initiated by academic EM physicians in academic ED’s� Emergency physicians should look for collaborative relationships with other specialties which are “win-win” for both specialties
Finally, on the academic side, we must take advantage of our educational strengths� We provide a unique educational opportunity for students and residents to treat acutely ill and undifferentiated patient populations� We also provide some of the best bedside teaching of any specialty, in a setting where the most diagnostic and therapeutic interventions can be utilized acutely� This educational niche cannot be under-estimated in its worth to academic medicine
It is difficult to find an area of academic emergency medicine that is not growing� Clinical care, research, and education in emergency medicine continue to flourish The clinical need continues to grow and redefine itself, the research on acute illness continues to mature, and the education of today’s brightest physicians predicts a bright future for our specialty� Academic emergency physicians with vision and leadership will continue to lead this growth, and define the future of our specialty�
References:
1 National Hospital Ambulatory Medical Care Survey: Available at: http://www cdc gov/nchs/data/ahcd/nhamcs_emergency/2011_ed_web_ tables pdf Accessed on October 20, 2015
2 National Residency Match Program Accessed on October 20, 2015
3 Blue Ridge Institute for Medical Research NIH Funding to US Medical Schools Accessed on October 20, 2015
4� National Institutes of Health Office of Emergency Care Research, accessed at http://www�nigms�nih�gov/about/overview/OECR/Pages/ default�aspx, on October 20, 2015
Hospital administration is a dynamic environment directly influenced by patient outcomes, compliance standards, financial analyses, and staff expectations Hospital administrators provide strategic management of these areas and are held accountable for the organization’s success� Effective hospital administrators often wear many “hats” and work collaboratively with internal and external stakeholders who frequently have differing interests Successful hospital administrators are comfortable making difficult, but sometimes unpopular, decisions to ensure high-quality patient care and hospital sustainability�1
The role of physicians in hospital administration has drastically increased since the passage of the 2009 Affordable Care Act (ACA), which established the mandate for greater alignment among physicians, healthcare systems, and insurance payers Traditionally, administrators with business or policy backgrounds have led hospitals Since the

passage of the ACA, many high-performing hospitals have realized the value of recruiting physician-leaders to serve in key administrative positions�2 Due to their professional training and clinical expertise, physicianleaders have an increased ability to identify hospitalwide opportunities for improvement and develop new interventions to create high-quality, efficient care delivery systems� Physician-leaders are also able to engage hospital medical staff and physician medical groups with greater ease due to understanding the challenges of clinical practice�
Emergency physicians are rapidly increasing in hospital administration as executives and medical directors As emergency physicians, we have worked alongside each medical and surgical specialty and possess insight into each specialty’s key challenges and interests We also understand the concept and importance of interdisciplinary, coordinated care involving physicians, nurses and support staff Finally, our day-to-day clinical encounters as emergency physicians prepare us to be nimble and decisive in difficult situations
Historically, hospital administrators have been personified as “suits” and non-clinical leaders that prevent physicians from doing what is best for their patients due to financial or political influences�3 These sentiments have been especially strong in academic medical centers� However, the increase in physician executives, especially from academic backgrounds, is steadily changing this perception of hospital leaders Hospital administration allows physicians to establish organizational vision, culture, and values to create an environment dedicated to providing the best patient experience and clinical outcomes� Physician administrators also have the ability to design and implement clinical processes and programs that directly impact the delivery of high-quality care to numerous patient populations� Lastly, administration allows physician leaders to make scholarly contributions to medical education, implementation research, and quality improvement by identifying care delivery challenges and solving them through the use of clinical and analytical skills�
There is no defined pathway to become a physician administrator� However, the following are several steps to consider on the journey to become an administrator
• Step 1: Prepare Yourself for a Role in Administration.
There are several educational opportunities available to prepare for a career in hospital administration Administration requires skills in several areas, such as population health management, finance, strategic planning, policy, and leadership� These skills are often not taught in medical school or residency Hence, many physician-leaders engage in formal education programs to obtain a master-level degree in Business Administration, Public Health, or Public Administration with an emphasis in Healthcare Management� SAEM offers a certificate in Academic Emergency Medicine Administration (CAEMA) There are also several emergency medicine administration fellowships throughout the country that prepare physicians for emergency department (ED) or hospital administration career (see SAEM Fellowship Directory)� Many emergency medicine medical groups also have administration fellowships that focus on leadership development and group management
Regardless of the amount of education one may receive, most of the training and preparation to be an effective administrator takes place on the job� Each organization is unique and has its own culture The most important first step when beginning in a new administrative position is to meet with each of the key leaders of the organization to clearly understand the strategic goals and objectives and how you can apply your expertise to add value to the organization
• Step 2: Get Involved in Your Own Department.
The best experiential step toward becoming a hospital administrator is to take on a leadership role in your own emergency department (ED)� Your ED is your home base� Make sure that you have developed into a successful change agent before you venture to other parts of the hospital or healthcare system� First, identify lowhanging fruit or problems that are widespread but are easy to fix� These problems or issues may be projects, such as improving hand-off communication among residents or attendings using a standardized format
The best experiential step toward becoming a hospital administrator is to take on a leadership role in your own emergency department (ED).
or implementing evidence-based clinical pathways to improve patient outcomes Regardless of the issue, achieve some easy wins and work towards more complex issues within your department that require more substantial process improvements Second, focus on building genuine rapport, trust, and camaraderie among your peers and supervisors You will need the support of your department and your department’s leadership during your professional development and future administrative endeavors Finally, volunteer for appropriate departmental committees and leadership positions
• Step 3: Get Involved with Hospital Committees and Lead.

As you improve the internal challenges within your department, begin to identify multi-specialty issues that impact patient care� In the age of electronic health record systems, clinical practice and patient outcome data are at your fingertips� Reach out to your medical and surgical colleagues to develop task forces to improve underperforming clinical processes that involve the participation of multiple specialties, such as Trauma or Stroke care Next, develop data-driven, ED-based
interventions that carry over to other departments of the hospital When you orchestrate multidisciplinary interventions, it is important to be objective and serve as an ambassador for the patient� Think of the patient’s overall care and not simply his or her acute care in the emergency department� Finally, get involved with other non-direct patient care committees, such as hospital readmission, physician wellness, or credentialing committees� Building relationships with other physicianleaders and administrators in the hospital is key to developing into a strong hospital leader�
• Step 4: Engage Nursing Leadership.
Nurses are the backbone of all hospitals and healthcare organizations� They are responsible for executing the clinical care that contributes to desired patient outcomes, which enable hospitals to develop into high-performing institutions As a physician administrator, it is important to understand nursing practices, concerns, and limitations to achieve greater alignment between all clinicians Engaging and working collaboratively with nursing leadership are critical steps toward becoming a successful physician-leader
•
Executive leaders are people too! Most CEOs, CMOs, and other executive leaders enjoy speaking to physicians that are interested in pursuing leadership roles Arrange meetings with these executive leaders and ask them how they navigated to their current positions� In addition, ask for advice and “lessons learned” to inform your own professional journey Executive leaders spend each day listening to others’ challenges and fixing system-level issues Therefore, offer your assistance to the executive Simple, genuine phrases, such as “Please let me know if I can ever be of assistance to you” or “Please contact me if you have a problem that you think I can help to fix” are gestures to inform the executive that you are willing to help and are open to new opportunities The executive will be grateful and likely accept your offer� Be prepared to assist the executive and ensure the assigned task is completed successfully�
There is no algorithm or validated pathway to become a hospital administrator� In fact, many administrators progress through their careers due to serendipitous opportunities� Often, you will hear leaders state stories such as the following: “I led a project and presented it at a conference The next week I received a phone call from an executive who recruited me to this hospital ” Do not be afraid to take on new projects or accept a new position that is offered to you, even if you feel under-qualified� Often others see your talents and strengths with more clarity than you see your own� In the words of Thomas Jefferson, “With great risk comes great reward ”
Failure is always a possibility However, failure is one of the greatest teachers� Your steps after a failure or disappointment determine your tenacity as a leader Some concepts to keep in mind as a physician-leader are to do the following:
• Keep the patient at the center of all decisions�
• Focus on patient clinical outcomes and experience to target opportunities for improvement
• Build strong, collaborative relationships with internal and external interest groups�
• Identify your strategic objectives and goals and monitor them frequently
• Learn from other leaders what to do and what not to do�
• Form a team with people that are highly skilled in your areas of weakness A leader is only as good as her team�
• Develop your own leadership core values�
My professional core values are SAVE:
S: Service—to patients, team members, organization, and community� My professional motto is, “What can I do to help you?”
A: Acknowledgement—of others’ contributions and value
V: Vision—to lead successful initiatives and the organization
E: Excellence—continuous commitment to achieving a standard of excellence in all matters of the organization
Physician administrators are essential to creating top performing hospitals and health systems that provide patient-centered, high-quality care� A career in administration allows emergency physicians, in particular, to have a great influence over direct patient care for thousands of patients, while still engaging in intellectually stimulating activities that extend beyond the ED� Being an administrator is not for everyone� However, if you are a visionary leader who enjoys a dynamic environment that requires collaborative teamwork, strategic planning, and problem resolution, then administration may be an ideal career choice for you�
References:
1 Elliot, Victoria “Hospitals’ New Physician Leaders: Doctors Wear Multiple Hats” Oct 2015 Nov 2015
2 Hayes, Chris, Vandad Yousefi, Tamara Wallington, and Amir Ginzburg “Case Study of Physician Leaders in Quality and Patient Safety, and the Development of the Leadership Network ” Healthcare Quarterly (2010): 68-73
3 Fairchild, David G , Evan M Benjamin, David R Gifford, and Stephen J Huot “Physician Leadership: Enhancing the Career Development of Academic Physician Administrators and Leaders ” Academic Medicine 79 3 (2004): 214-218
 By Jeffrey Ricks, MD
By Jeffrey Ricks, MD
For many, the mental model, or framework for our understanding, of Military Emergency Medicine is strongly influenced by popular media and, as such, falls short of reality Television series such as the widely successful “M*A*S*H” (1972-1983) and the less successful “Combat Hospital” (2011), illustrate the difficulties of caring for injured and ill people in combat environments Movies such as “Pearl Harbor” (2001) show glimpses into the chaos that ensues from coordinated tactical assaults and the resultant mass casualty events While it is undeniably true that all military nurses look like Ben Affleck or Kate Beckinsale, and all military physicians look like Jennifer Garner or Josh Hartnett, these are fictional portrayals that focus more on the emotional dilemmas that face military medical personnel than the practice of medicine in the military� Ironically even the non-fictional docuseries “Inside Combat Rescue”, which shows scenes from inside a NATO hospital in Afghanistan during 2012, is an unrealistic representation of military emergency medicine That hardened-building containing a hospital in a combat zone with advanced
imaging capabilities, numerous emergency physicians, nurses, corpsmen and surgeons available to respond at all hours of every day is not reproduced anywhere else in military medicine Rather, emergency medicine in the military is the practice of medicine in limited resource environments

The scope of emergency medicine in the military is not isolated to the combat environment and is fully represented across the range of military operations, because the military has a role in times of war as well as times of peace and conflicts other than war� Operations other than war include humanitarian assistance, disaster relief, civil support, peacebuilding, peacemaking, nation assistance, and antiterrorism� Emergency medicine has a role in all of these operations in both hospital and non-hospital environments� Military treatment facilities (MTF’s) are hospitals that exist to care for military personnel, their dependents and retirees back home at all times� These MTF’s include large tertiary care academic centers as well as community hospitals
Hospitals in the military also exist forward and are not limited to brick and mortar walls� Emergency medicine has a presence in forward deployed hospitals on board ships and on land, during combat as well as non-combat operations� Some of these hospitals are “confined” by plywood, if one is lucky, or more typically by tents� Emergency medicine has a presence in non-hospital environments providing pre-hospital care of injuries and illnesses in support of diving and submarine operations undersea, ground operations on land, and flight operations in the air Some military emergency physicians are also astronauts in the National Aeronautics and Space Administration All these hospital and non-hospital environments are limited by the availability of resources whether that is location, personnel, equipment, supplies, or time The preparation for a career in military emergency medicine begins in medical school as the motivated student learns not only how to manage the patient with unlimited resources but also how to diagnose and treat in austere limited resource environments
The essence of emergency medicine in and out of the military is the practice of medicine despite limited resources Even large civilian tertiary care centers have limitations� Most often these are facility limitations such as inpatient or emergency department beds, staff to care for patients, and availability of diagnostic equipment If these were truly unlimited resource environments, patients would not have to wait hours or days to be seen in an emergency department, and boarding patients would be merely science fiction nightmares akin to zombies The ability to care for the undifferentiated sick and injured patient is the cornerstone of emergency medicine and requires the mastery of clinical decision making with limited information� However, the extent of the limitations seen in military medicine is rarely discussed and even less frequently experienced in most training programs� With the notable exception of training programs that incorporate wilderness and international medicine discussions, residents are rarely challenged to consider how to diagnose and treat conditions with only basic laboratory capabilities, rudimentary plain film radiography without computed tomography, and a limited medication arsenal The importance of history and physical exam become evident in these environments� In addition, the emergency physician must have a well-practiced and robust playbook to call upon when the only light comes from your headlamp and the generator failure precludes the use of ultrasound and video laryngoscopy assistance with procedures� Trainees who will be practicing in more significantly limited resource environments should be afforded opportunities to better prepare them for the challenges of their future career
Preparing the trainee to excel in their military emergency medicine career requires an honest appraisal of the strengths and weakness of the individual and opportunities that the program can provide� Whether a fellow, resident, or student, the individual must possess the capacity and motivation to learn� They should actively seek out learning opportunities to help them perform in austere conditions� Mentoring, guided discussions, and on-the-spot clinical teaching moments are all great opportunities to improve the trainee’s interview, physical exam skills, and clinical decision making Experienced faculty should encourage the individual to consider diagnostic and management strategies in a variety of hypothetical, limited resource environments The trainee, when safe and appropriate, should be encouraged to try alternative procedural approaches and by doing so increase their comfort and capability� Supplementary training opportunities such as additional critical care and inpatient trauma rotations, electives with exposure to austere environments and emergency medical services, plus participation in disaster planning and mass casualty drills can provide valuable experiences and increase the capability of the trainee� Many organizations, such as SAEM, have uniformed services interest groups and reduced rates for military members�
Military physicians operating in both the pre-hospital and forward deployed hospital environments must be capable of providing care for critically injured and ill patients for an uncertain time prior to evacuation for definitive care� In addition, emergency physicians in these situations may be called upon to first assist in craniotomies, thoracotomies, laparotomies, fasciotomies, and other surgical procedures Recognizing limited
Preparing the trainee to excel in their military emergency medicine career requires an honest appraisal of the strengths and weakness of the individual and opportunities that the program can provide. Whether a fellow, resident, or student, the individual must possess the capacity and motivation to learn.
monitoring, diagnostic, and treatment capabilities, the successful emergency physician needs to know management goals beyond the initial resuscitation to include inpatient care for 72 hours or more before evacuation may be possible Training programs that are plagued by boarded patients actually provide good exposure and learning opportunities for emergency medicine trainees� If one’s training program is blessed with the infrequent boarder, the trainee may benefit from additional critical care rotations Those individuals with additional inpatient trauma and operative exposure will be more capable of assisting in forward deployed environments, when performing rare procedures, and improve outcomes for patients� For example, a peri-mortem caesarian section should not be the first time one performs a midline laparotomy incision; this skill should be learned on a less critical patient� The goal is not a demonstrated competency on long-term inpatient care or all surgical procedures, but rather a reasonable familiarization and capability to perform when needed�
Understanding the principles of pre-hospital care is vital for all emergency physicians, but differences exist between the civilian and military models Beginning with nomenclature, the civilian sector categorizes trauma centers based on capability with the highest level assigned the Roman numeral I, and facilities with less capability distinguished by higher numbers (II through V) Conversely, the military model is a tiered system that classifies discrete levels of care based on capability by assigning Arabic numeral distinctions with a Level 1 asset having the fewest resources and a Level 5 having the most� The intent of both models is the rapid transport of the patient from point of injury to the nearest regional facility with the most capability� However, because of the remote location of military assets around the globe, the patient often moves stepwise from point injury through all necessary levels taking days to weeks to reach the comprehensive Level 5, tertiary care center back in the States� Evacuating patients between levels of care may utilize ground, air and seafaring platforms Emergency medicine training programs that maximize learning opportunities in wilderness medicine, emergency medical services, and international medicine can provide clinical exposure to limited resource environments and improve the care delivered by future military emergency physicians
Some key components of military emergency medicine are difficult to simulate, in general, and
are rarely seen, thankfully, in the civilian setting� Mechanisms of injury in combat, and from terrorist attacks, include high velocity projectiles and high explosives in addition to all the common causes of non-battle injuries Historical reviews of casualties injured by these mechanisms reveal a high incidence of potentially salvageable injuries that have changed the treatment priorities when caring for these patients� Exsanguination from massive extremity hemorrhage is so rapid and frequent that during the initial evaluation and resuscitation, tourniquet application to stop extremity exsanguination occurs first The primary survey should begin with an assessment for extremity hemorrhage, and a tourniquet should be applied to the proximal limb immediately if necessary Integrating this principle is easy as the trauma algorithm is simply expanded to begin with “X” for exsanguination before moving onto “A” for airway� Additionally, mass casualty events and disasters are rare but not military-unique phenomena Trainees should be encouraged to participate in disaster and mass casualty training at the facility and regional level Additional coursework in chemical, biologic, radiologic and nuclear incident management would aid in the preparation for a career in the military
Emergency medicine trainees interested in a career in the military would benefit from integrating these experiences into their curricula� Furthermore, they are synergistic with emergency medicine training goals and help individuals meet the required objectives for advancement�
In addition to operational experiences, military emergency medicine has career opportunities in administration, academics, and research� Available fellowships include Pediatrics, Toxicology, Ultrasound, and Emergency Medical Services, as well as training in hyperbaric and aerospace medicine
Compensation and promotion in the military is based on time in service, performance, and successfully reaching career milestones� Information on base salary, housing allowance, and bonuses is readily available on-line and by talking to recruiters from the respective services: Army, Navy�

In every “Sponsoring Institution”, the ACGME designation for hospitals that host residency or fellowship programs, a single individual is responsible for the graduate medical education (GME) training programs� Some Sponsoring Institutions host only one training program with a dozen residents and others host dozens of programs with hundreds of residents� Because the size and scope of the Sponsoring Institutions varies so widely, the role of the DIO varies widely too In very small institutions, the DIO may also be the program director of the institution’s only program� In some institutions, the DIO role stands alone or is an embedded function for individuals called Chief Academic Officers, Directors of Medical Education, Vice-President of Academic Affairs, and Assistant/Associate Deans for Graduate Medical Education
This chapter discusses the role of the DIO and discusses the scope of other titled roles in which the DIO role is embedded� The chapter also describes the career pathway to the penultimate Graduate Medical Education administrative position in most institutions
The ACGME DIO is a relatively new position, becoming a requirement in 1998 for institutions wishing to receive ACGME accreditation for GME Specifically, the ACGME requires institutions to identify a “DIO: The individual who, in collaboration with a Graduate Medical Education Committee (GMEC), must have authority and responsibility for the oversight and administration of each of the Sponsoring Institution’s ACGME accredited programs, as well as for ensuring compliance with the ACGME Institutional, Common, and specialty/subspecialtyspecific Program Requirements”� Prior to 1998, many institutions had an individual in charge of graduate medical education with titles such as director, vice president, chief, or associate dean that served that role�
The DIO role was originally created to make certain that a single individual could be held accountable for the ACGME accredited programs In its early iteration, the role was largely transactional� The DIO was the approver of program complement changes, manager of the mid-cycle internal review, developer of policies and procedures and was peripherally involved in the accreditation process for specific programs Program accreditation was seen as a program director responsibility� While the DIO assisted in document preparation, the role of the DIO in the accreditation survey was confined to a brief interaction with the site surveyor and was largely focused on institutional issues The DIO position has significantly evolved since first articulated in 1998 particularly because of the evolution of the ACGME Next Accreditation System (NAS) The Annual Program Evaluation and Annual Institutional Report are more important than ever as the ACGME has moved from periodic accreditation cycles to continuous accreditation with periodic site visits� The DIO now must make certain that each program is meeting the accreditation requirements; focused on resident performance outcomes, and adherent to the myriad of institutional requirements, regulatory mandates, and compliance imperatives� The NAS and the Clinical Learning Environment Review (CLER) has made certain
that the DIO has an unambiguous leadership role with direct reporting to the Chief Executive of the Sponsoring Institution and that the GME infrastructure is coordinated with, and facilitates, the institution’s quality, patient safety, and process improvement initiatives� These changes in ACGME’s expectations for institutional oversight and integration have elevated the role of the DIO to that of a senior administrator in many institutions�
The primary role and responsibilities of DIOs involve oversight and administration of residency and fellowship programs� Reisenberg and colleagues published an 11-item DIO responsibilities score (DIORS) rating that included items such as GME oversight, institutional contact for ACGME and other GME organizations, and GMEC involvement� The DIO is accountable for the institution’s CLER visit� CLER visits typically occur every 18-24 months and involve specific institutional educational review in the domains of quality, patient safety, supervision, fatigue management, transitions of care, and professionalism The DIO leads residency program internal reviews, provides GME budget oversight, and manages discipline and residency director performance� Most DIOs are in the latter half of their career and have been involved in GME for the majority of their professional life Many have had previous leadership or management experience, often as residency program directors (PDs) DIOs are often but not always physicians�
Clinical competence, medical knowledge, and teaching skills are assumed skills of a DIO� The DIO position is primarily an administrative leadership position As such, additional leadership and management competencies such as professionalism, communication skills, financial management, and human resources knowledge are essential� DIOs often gain specific competencies in policy development, visa knowledge, and legal issues involving educational agreements�
Ensuring compliance (institutional, program, individual) is a heavily weighted function for the DIO position For many clinician educators, the amount of teaching and patient care decreases as one becomes a DIO and the transition to a compliance focus can
The DIO now must make certain that each program is meeting the accreditation requirements; focused on resident performance outcomes, and adherent to the myriad of institutional requirements, regulatory mandates, and compliance imperatives.
present a challenge� A comment from a DIO in the Riesenberg article referenced below states “I used to be a facilitator and coordinator Now, I am an auditor and enforcer” exemplifies this� GME funding sources are stressed Federal GME funds come to hospital and cost and revenue streams are often in different budgets within an institution� This can to lack of a shared vision and narrative of the strategic value of GME within different parts of the same institution� The DIO position is a relatively new one and one not as known as other traditional positions Authority, accountability, responsibility and resources definition and clarity are often an evolving narrative with lines of authority in GME less clear than in areas such as Undergraduate Medical Education Much of GME leadership and management comes through indirect persuasion and influence rather than direct lines of authority� The heavy administrative load makes it a challenge for DIOs to publish many first author peer-reviewed publications, the currency of many medical school promotion processes�
As more national discussion involves health care and health professions education as a public good, the DIO position provides an outstanding opportunity to design the ideal clinical learning environment of the future� Changing priorities in health care and health professions education is moving emphasis from individual exceptionalism to team based care, from rescue care to population health, and from a narrow focus on medical knowledge to a focus on broader competencies such a systems based practice, practice based learning, interpersonal communication skills, and professionalism� DIOs are often on executive managements teams with other operational leaders and have a unique opportunity to bridge the link between academics and clinical operations Emergency physicians have a unique skill sets and set of experiences to thrive in this environment�
While the DIO role is described in general terms by the ACGME, the DIO role is often embedded in other larger positions such as Vice President for Academic Affairs, Chief Academic Officer, Associate Dean for Graduate Medical Educations and others� Like the DIO position, these positions vary widely among institutions When the DIO role is part of a larger position, additional responsibilities may be assigned for Simulation Training, Library Services, Student Affairs, Research, and may be further integrated with internal learner functions such as Organization and Staff Development The skill sets required for the additional task overlap considerably with the DIO role and assuming them brings a level of integration to the DIO role that facilitates rather than complicates execution of DIO function� In addition, larger roles, particularly when titled similar to other administrative position, places the DIO position in the “C-Suite” and is often more elevated in the organizational structure than a stand-alone DIO role
Like every senior career position, a charted path is more likely to yield success after years of career investment; such is true for the DIO/CAO position Emergency Physicians, particularly prior Program Directors, often have the skill set needed to effectively function as the DIO Several key touchstones build the requisite skills and competencies:
1� Serve as a Program Director and develop a highly level of familiarity with accreditation requirements and program management
2 Manage the EM residency program budget and understand the basics of hospital finance, budget

3 Become involved in the hospital GME functions and serve on the Graduate Medical Education Committee to develop a broad understanding of how various programs implement and execute accreditation requirements�
4� Develop effective in managing interdepartmental discussions that require compromise, detailed project analysis, and complex implementation�
5� Understand the basics of Graduate Medical Education financing and the challenges to managing hospital GME funding�
6� Garner experience in strategic planning, strategic thinking, principled negotiation, consensus building, and complex problem solving
For individuals interested in developing DIO competencies further, the ACGME usually has a DIO “boot camp” as a pre-day to their annual meeting The Association of American Medical Colleges Group on Residency Affairs (AAMC-GRA) has a leadership course for DIOs Ultimately, the key to a DIOs success is their ability to identify and implement best practices in creating a clinical learning environment to provide outstanding patient care and professional education�
Table 1 Characteristics, Roles, and Responsibilities of the Designated Institutional Official (DIO) Position in Graduate Medical Education� Riesenberg, Lee; Rosenbaum, Paula; Stick, Sheldon, Academic Medicine 81(1):8-16, January 2006�
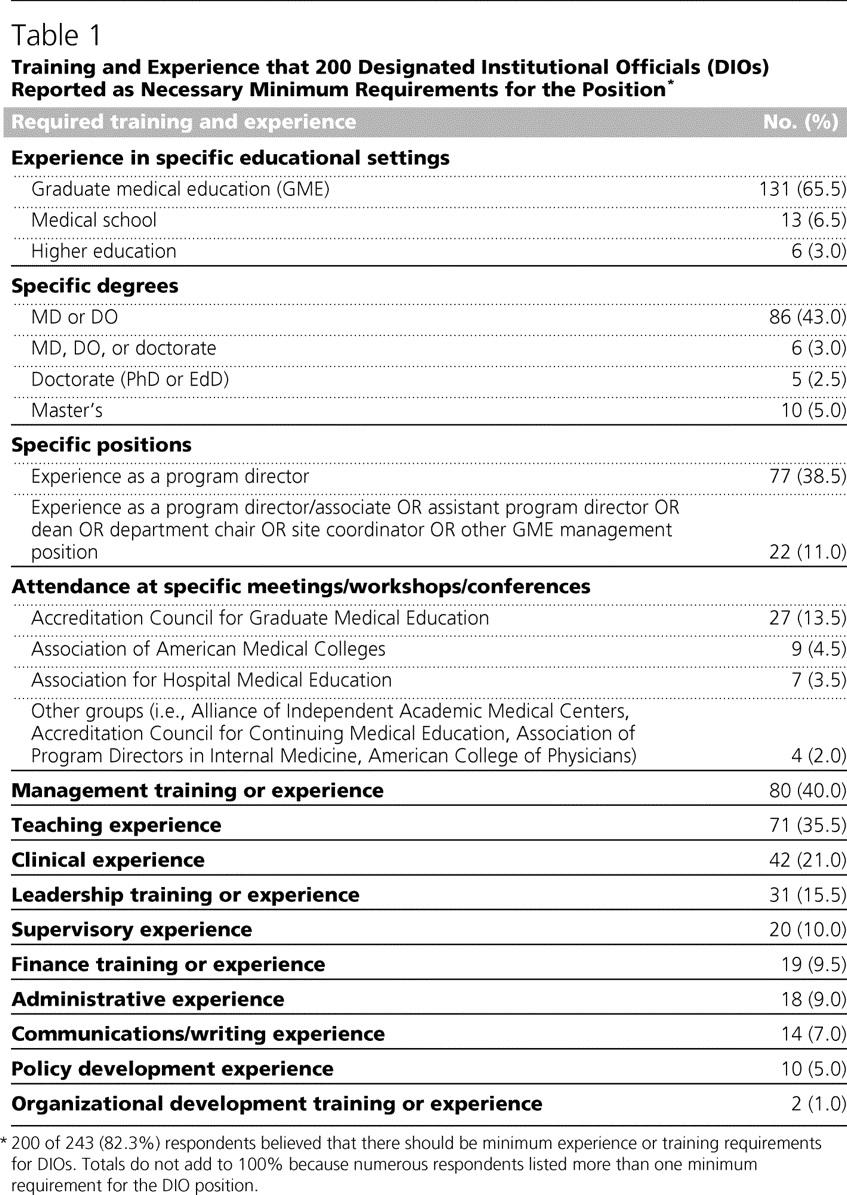
Table 2 Competencies, Essential Training, and Resources Viewed by Designated Institutional Officials as Important to the Position in Graduate Medical Education� Riesenberg, Lee; Rosenbaum, Paula; Stick, Sheldon, Academic Medicine 81(5):426-431, May 2006 DOI: 10�1097/01�ACM�0000222279�28824�f5
Recommended Reference Readings:
1 Riesenberg et al Characteristics, Roles, and Responsibilities of the Designated Institutional Official (DIO) Position in Graduate Medical Education� Acad Med 2006; 81:8-16�

2 Bellini et al Beyond Must: Supporting the Evolving Role of the Designated Institutional Official JGME 2010 147-150�
3 Riesenberg et al Competencies, Essential training, and Resources Viewed by Designated Institutional Officials as Important to the Position in Graduate Medical Education� Acad Med 2006; 81:426-431�
4� Nelson� The Designated Institutional Official: One DIO’s Perspective� Acad Med 2006; 81:17-19�
Are you interested in getting an advanced degree besides an MD/DO? If so, there are several questions to explore before you make a decision What advanced degrees are available to me? Why would I need an advanced degree? Who should get advanced degrees? When is a good time to get one? Where should you get it? How much work and expense does it take? Is it worth it (will I get a return on investment)? Although medical education in the United States does address scientific research, introductory health economics, epidemiology, and statistics, no single topic is covered in great detail� (1) These topics are not necessarily explored in depth during residency or fellowship training so it has become more common for clinicians to pursue advanced degrees as an adjunct to our medical training This chapter will address these questions and offer some guidance

Advanced degree-seekers have several choices, and Hall et al� summarized these succinctly� (1) The Doctor of Philosophy (Ph D ), Master’s of Public Health (MPH), and Master’s of Business Administration (MBA) are popular degrees currently� The table illustrates advanced degrees and their implications (Table) Each advanced degree is awarded through a graduate school and has unique features� With the emerging interest in health care administration and education, we are seeing several new options on the graduate degree landscape� Common features include a combination of classroom work, either synchronous or asynchronous, leading to course credits, and a dissertation under close mentorship Some programs, such as a Ph�D, are combined with medical degree programs, while others can be obtained before or after We recommend reviewing U�S� News & World Report for the school’s ranking, visiting their website or reading course catalogs for class descriptions, and speaking with recent graduates before applying



Physicians complete medical school and are given an MD or DO, which are terminal degrees� An additional degree should not be a goal in itself but a means to achieve future goals in your clinical and/ or academic career� Your career goal may be to pursue scholarship in bench or clinical research, disease prevention, global health, or seek an educational role in the residency program or medical school You may desire to be the director of a department or an administrator of a hospital You may find a passion in the health policy or medico- legal issues in the healthcare An advanced degree will give you a tool to enhance your skillset�
Perry et al� reported that the positive contributors for a clinical researcher included research training to include an advanced degree (2) A Master’s Degree in Science will help you to build skill in statistics, critical review of scientific literature, and manuscript writing skills, which are essential to building your research career A Master’s Degree in Public Health (MPH) is similar except the course is less stringently focused on clinical research; instead it requires students to perform field work People who completed an MPH are more likely to be generalist clinicians, have more peer reviewed publications, and receive more NIH funding than those without degrees (3) A Master’s of Business Administration (MBA) is an ideal degree to be a department director who oversees finances and operations in conjunction with non-physician administrators It often is required or highly desirable
People who completed an MPH are more likely to be generalist clinicians, have more peer reviewed publications, and receive more NIH funding than those without degrees.
MBA Administrator, medical director pathway Many programs are not necessarily healthcare oriented�
MHA Administrator, medical director
Contrast to MBA, the degree gives topics more specific to health care administration
MHPE, MME, MEd Faculty at medical school Choice of programs and tuition
MPH Epidemiologist, Clinical scientist Less stringent than MS, requires a field study
MS Clinician scientist
JD Medical legal expert
PhD* Clinical and basic scientist
for many potential physician executives as part of the application process� Juris Doctor (JD) is a professional degree, similar to medical school, in that students spend about 3-4 years of didactics and course works, and need to pass a bar exam to practice in the court�
The data of Perry et al suggests that early stage investigations are more likely to be funded if researchers have proper research training and an advanced degree� (2) Burkhardt et al� surveyed American Board of Emergency Medicine (ABEM) examinees and reported that an interest in science and a record of peer review publications were associated with an interest in an academic career (4) Thus, it is likely beneficial for residents, fellows, and junior faculty who are interested in academic careers to pursue advanced degrees, as most degrees require structured training that leads to scholarship and peer review publications
Recently, we have started to see high-quality studies from community practice, such as Kaiser Permanente, and since there are several hybrid models available, where students have the option of splitting their clinical time between academics and community practice, it is not paradoxical to seek these types of degrees even if students are not committed to academic practice
Other potential candidates would be those who are assuming a progressive role as a medical director in their institutions� Administrators are required to have knowledge of hospital finances and quality improvement, which an MBA or an MHA can offer� The presence of a physician administrator is always valued
Somewhat more research and mathematically oriented than MPH
Requires at least 3 years of course works and pass a bar exam
It may take substantial time to obtain degree
feasibility.
as he can provide unique expertise from both a clinical and administrative perspective� These degrees can enhance leadership skills for clinicians, and those who are interested can take advantage of coursework so as to launch a relevant project in the department and improve efficiency, quality of care, and revenue
If you intend to pursue a role as an education expert at the medical school or graduate school, you may find a Master’s in Health Profession Education (MHPE), Master’s in Medical Education (MME) or Master’s in Education (MEd) suitable for your goals Recently, expertise in medical education has gained popularity, as there are more fellowship programs targeted at medical education or simulation among EM training programs in the US� It is clearly advantageous for an academician to have an advanced degree when you are working with a full-time non-clinician education specialist� This would be an ideal degree if you have a passion for education, and we have started to see several peer-reviewed publications (many of which are becoming PubMed-indexed titles), so you would be likely to advance your career via educational impact and promotion�
Everyone has a different timeline to pursue a degree� If someone already has the right skill set for a career goal, he or she will not be in need of an advanced degree� If someone is needing additional skills and has support from their department leadership and family, they are well-situated to pursue a degree� Most degrees require substantial time, which will slow down some aspects of your life� A study from the Harvard School of Public Health showed that its graduates were more likely to be
funded by NIH if they were enrolled before the age of 40, and generalist had their course works published (5) Thus, pursuing a degree would be appropriate if you are preparing for a scholarly productive career�
Generally speaking, course work required for graduate degree is more labor intensive than undergraduate courses� Most courses offer 3 credits per semester, which requires you to spend 3 hours in class or online, and you will spend about 9 hours reviewing related articles and homework assignments, resulting in a total of 12 hours per week, per course, or spend between 1 and 2 hours per day� It would be advisable to set up a weekly calendar to coordinate your study schedule, and try your best to get around your work and family to fit the schedule�
It is recommended to pursue an advanced degree when you are at the stage of 1) fellowship, 2) junior faculty, 3) before or after medical school, or 4) a later stage of EM residency� It is also possible to acquire an advanced degree if you are advancing your career, and your institution supports you pursuing an executive MBA or its equivalent� Departmental support is essential, as the program requires a lot of time and tuition expenses, which can be negotiated�
This has become an interesting question, as students now have the option to pursue an advanced degree in a brick and mortar classroom setting or online Several online master’s degree programs are available, and they can be useful if a student cannot find the right program nearby� Most academic institutions have graduate schools, and many courses are available online The important point is that online learning requires organization and self-discipline� Students need to schedule their coursework around their work and family obligations� On the other hand, busy executives are taking many MBA courses online and go to campus only for specific courses
If your goal is simply to master the content, you may not benefit from a classroom setting, but it may have an added benefit if you need to expand your network through classroom interaction, which is vitally important If you are affiliated with an academic institution, your department may pay your tuition, or you may qualify for a tuition reduction, and training grants may be available�
Even if you do not have protected time, and graduate schools do not approve your admission, there is a strategy You can always start with the certificate program where you can take about half of the required course and advance to the full degree work�
Many physicians choose to seek an advanced degree to gain the skills to engage in research at higher levels or to enhance leadership or business skills� (1) We also have seen many pioneers in Emergency Medicine who succeeded in their field without an additional degree In the end, the real or perceived benefits of pursuing an advanced degree beyond traditional medical education has to be weighed against time, intellectual, and emotional investment required to achieve such a training (1) By pursuing a degree, you will spend 2-4 years of your career studying further, and likely spending between 20,000 to 50,000 dollars for tuition In return, you may have a powerful tool to launch a successful academic or administrative career� The risk benefit analysis is a very personal one as no two situations are alike�
If you have the right skill-set to advance or enjoy your career, getting an advanced degree may not be necessary� But if you are aspiring to a new skill or to advance your expertise and a niche, pursuing an advanced degree might be right for you If you are interested in pursuing these options, I would recommend that you discuss your interest with your mentors early and chart an appropriate course�
Acknowledgements:
We greatly appreciate the advice and sharing unique aspects from Christopher Bennett, MD, MA and Joseph Wood, MD, JD
References
1 Hall JF Advanced Degrees in Academic Colorectal Surgery Clin Colon Rectal Surg 2013;26(4):250-3
2 Perry JJ, Snider CE, Artz JD, Stiell IG, Shaeri S, McLeod S, et al CAEP 2014 Academic Symposium: “How to Make Research succeed in Your Emergency Department: How to Develop and Train Career Researchers in Emergency Medicine” CJEM 2015;17(3):334-43
3 Krousel-Wood M, He J, Booth M, Chen CS, Rice J, Kahn MJ, et al Formal Public Health Education and Career Outcomes of Medical School Graduates PLoS One 2012;7(6):e39020
4 Burkhardt JC S-CR, Santen S Resident Values in A Rational Decision-making Model: An Interest in Academics in Emergency Medicine Internal and Emergency Medicine 2016:1-5
5� Goldhamer ME, Cohen AP, Bates DW, Cook EF, Davis RB, Singer DE, et al� Protecting an Endangered species: Training Physicians to Conduct Clinical Research Acad Med 2009;84(4):439-45