INNOVATIONS
WHOLE PERSON HEALTH







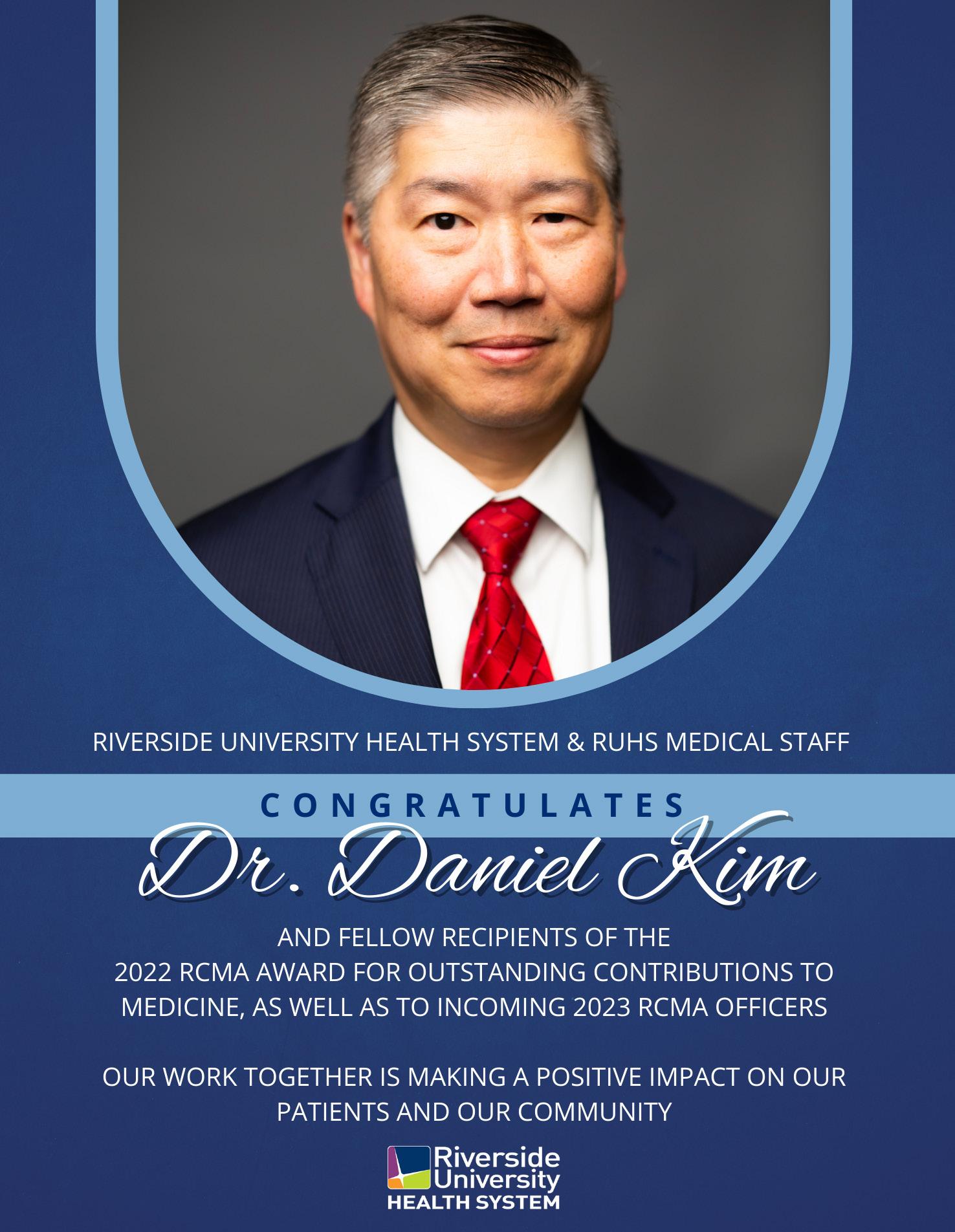
 GEOFFREY LEUNG MD, M.Ed
GEOFFREY LEUNG MD, M.Ed
 RIVERSIDE COUNTY HEALTH OFFICER DEPARTMENT OF PUBLIC HEALTH
RIVERSIDE COUNTY HEALTH OFFICER DEPARTMENT OF PUBLIC HEALTH
Our theme for this issue of the RUHS Innovations Magazine is “the whole person.” We are excited about this edition because we believe it speaks to our philosophy and approach to health. In the following pages, we highlight some of our integrated specialty services that cover the gamut of head to toe physical health needs, including dental, ophthalmologic (eye), pulmonary (lung), gastrointestinal (digestive tract), podiatric (foot), and women’s health services. We explore some of the ways in which RUHS supports non-medical whole person needs, such as food, transportation, and interpretation services. And we discover some of the ways in which RUHS Behavioral Health is pioneering integrated whole person programs to improve treat-
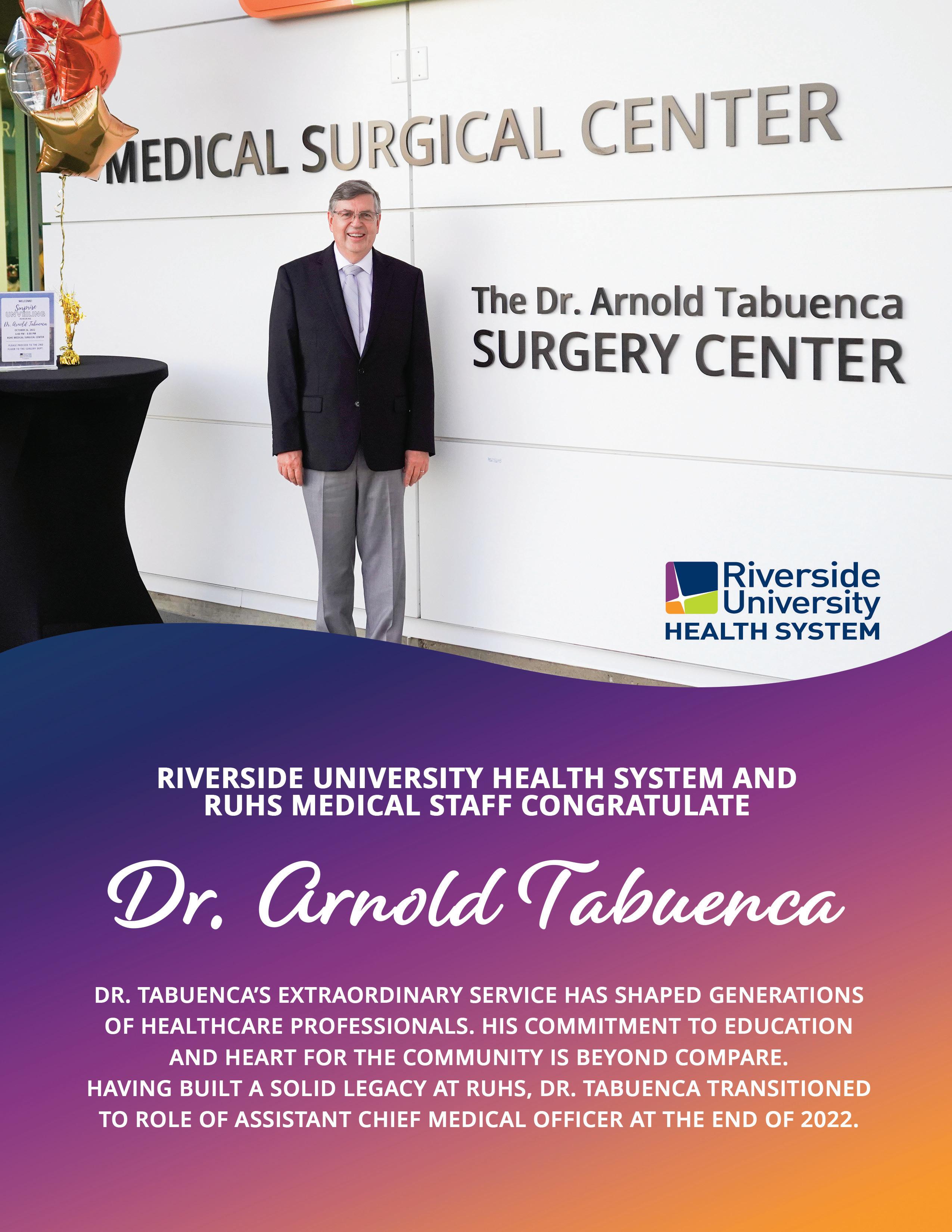
ment, recovery, and prevention of behavioral health and substance use conditions. Importantly, this edition spotlights RUHS’s Whole Person Health Score, which was recently published in the New England Journal of Medicine Catalyst (August 2022) and recognized in a CDC (Centers for Disease Control and Prevention) “Science in Brief” (November 2022) as an innovative tool to measure holistic health and underlying social determinants of health. Finally, this edition provides Dr. Arnold Tabuenca, a beloved RUHS leader who has embodied this “whole person” approach, an opportunity to reflect upon his many years as Chief Medical Officer. We hope you enjoy this edition of the Innovations Magazine focusing on RUHS’s approach to “the whole per-
Scan the QR Code to read
The New England Journal of Medicine:

Editor's Pick of 2022!
RIVERSIDE UNIVERSITY MEDICAL CENTER ON BEING FEATURED IN THE NEW ENGLAND JOURNAL OF MEDICINE: EDITOR’S PICKS OF 2022!

Anthony Firek, MD, MS
Bijan Sasaninia
Diep Tran, MPH, MA
Geoffrey Leung, MD, EdM
Dhruv Khurana, MS, MA, PhD
Mahbuba Khan, MD

In 2022, I was tasked with being the Program Coordinator for the Whole Person Health Score (WPHS) project at Riverside University Health System (RUHS). The California Department of Health Care Services had initiated a multi-year program that requires health systems to improve health outcomes and quality of life of residents and offer a broad service delivery system. In response to the new state requirements, my department was uniquely created to support the implementation and expansion of the WPHS throughout Riverside County. The goal was to teach our health system to think about overall health in a new way and create a pathway for our care teams to address complexities for our vulner-
able patient populations. The Whole Person Health Score is an innovative holistic health measurement tool that was developed at RUHS over six years ago and is based on a 28-question assessment that measures six different areas of health.

The goal of the tool is to capture the elements in a person’s life that make the biggest impact in regards to life-expectancy and well-being. The assessment produces a color-coded letter score in each area of health that both the provider and patients can easily understand. The Whole Person Health Score is designed to track change over time and supports strategic care coordination by simplifying and pri-

oritizing areas of greatest need for the patient. Ultimately, the WPHS is designed to empower patients to make improvements towards their health.
This project requires a lot of attention to detail to be effective. For example, in this role, it was necessary to develop processes and workflows that enabled care coordination throughout different departments. I’ve also developed and managed workgroups for more than 15 different WPHS projects and have also helped to establish program goals and priorities, coordinated with our research team, and developed informational materials to educate care teams on how to best utilize the WPHS tool in order to have a holistic approach to care.
The work to create the Whole Person Health Score was really led and inspired by patients. In fact, patients helped with determining the wording, the placement, and significance of questions used in the assessment. The unusual and ultimate six-letter display of the Whole Person Health Score was based on feedback from patients, who stated that letters were easier to understand than numbers.
When I first joined the WPHS workgroup in 2017, I was a volunteer health coach that had helped pilot the assessment among patients. My role as a health coach was to provide supplemental health education and motivational support to assist patients to self-manage their chronic medical conditions. In piloting the assessment, we would ask them what they thought each question meant, if the questions were important to understanding their health, and if the color-coded score accurately described their perception of their overall health.
The most compelling experience was when we were asking patients about whether we should include a question about “The Purpose of Life.” This question incited a deeper dialogue with patients, and I was humbled by how compelling patients were in telling their story, discussing significant events that led to how they acquired their chronic conditions, where they were at with their health, and what motivated them to move forward. I feel that going through the WPHS with patients provides a therapeutic interaction that give patients a moment to reflect on what really matters in life.
There were times where I would find some patients that were in significant distress. However, finding the appropriate resources was initially challenging and not always straightforward. At that time, I
started to capture patient stories and the barriers that were presented (with the patient’s permission), and I would present them as patient case studies to leadership to bring awareness of the complexity of needs identified with the WPHS and how their unmet needs impacted their self-management of care. The stories challenged the workgroup to think through feasible solutions to assist the patient and possible pathways where we could improve care delivery. My work to advocate for patients led me to being asked to join the RUHS Team as a full-time staff member. My work now focuses on exploring how WPHS impacts our patients, advocating for use of the WPHS within RUHS, training care teams on the WPHS, and helping care teams realize the value and benefit of learning of the whole person approach to care in their scope of work.
What I am excited about is that Riverside County has initiated an Integrated Service Delivery program to improve accessibility of county-wide services. As part of this effort, Riverside County Departments (starting with those related to Health and Human Services) will collaborate to utilize tools like the WPHS to engage with county residents, identify health disparities, and inform strategic planning on how to allocate health and social resource and interventions for our population and improve service delivery overall. This initiative gives me hope that the patient stories I presented to the RUHS leadership years ago has had a positive impact and that countless people dedicated to the wellbeing of our community are working together to find robust and effective solutions for complex health and social problems, especially for those residents who may be in times of critical need.
In the future, I am looking forward to increasing numbers of care teams at RUHS that will find value in adopting the WPHS as a meaningful metric that can help them better engage and collaborate with their patients and promote conversations on how everyone has the potential to achieve a long and healthy life. I look forward to seeing how the Whole Person Health Score can help to further transform the way in which our health system delivers care to all of our residents, including those in greatest need. I envision a future where people throughout Riverside County and beyond can be informed on what actions can be taken to improve their position in life and strive towards a path of self-improvement.

Riverside University Health System - Language and Cultural Services has helped serve our LEP community for over 15 years. Through continued commitment, prioritization, and long-term planning they have paced their efforts devoting resources toward providing high-quality language access services to RUHS patients and communities. The department has changed throughout the years, but the one thing that remains constant is our mission and purpose.
Cary Stueland Administrative Services Manager I and Gabriela Vargas Administrative Services Analyst II, share a conversation to provide an insight into what RUHS - Language and Cultural Services is all about.
Cary: What types of services are offered through Language and Cultural Services?
Gabriela: RUHS offers patients and families with Limited English Proficiency (LEP) free access to a medical interpreter at no cost to them. Our services are provided by a team of professional medical interpreters via in-person, telephonic, and virtual means in over 250 languages. Virtual and telephonic language access services are available 24/7, 365 days a year. In-person medical interpreters are available during business hours and some locations also have extended availability. Video Relay Services are also available upon request.
Cary: Which languages are available through your services?
Gabriela: At RUHS Medical Center, we currently provide in-person interpretation in ASL, Spanish, and Mandarin/ Chinese. At the RUHS Medical Center, Arlington Campus, Moreno Valley Community Health Center, and Corona Community Health Center, we provide in-person Spanish interpretation.
Telephonic and virtual interpreting is available in over 250 different languages at all locations 24/7, 365 days per year.
Cary: How many medical interpreters does RUHS have onsite?
Gabriela: Our team consists of 20 medical interpreters, 18 Spanish, 1 Chinese/Mandarin, and 1 ASL and Spanish.
Cary: How many interpreted encounters would you say are performed within 12 months?
I hope you are ready to be amazed. Looking at the 12 months from July 2021 to June 2022, Language and Cultural Services interpreted 38,746 in-person encounters and facilitated another 134,520 via telephonic and virtual means. More astounding, telephonic and virtual call volume also totaled 1,671,473 minutes within these 12 months.
Cary: What is the difference between Interpretation and Translation?
Gabriela: Interpretation is rendering a spoken or signed message into another spoken or signed language while preserving the context and meaning of the source language content. Translation is the process of converting written words or text from one language into another language. This must be done with accuracy, cultural sensitivity, and literacy level maintaining the same meaning as the original document.
Cary: Are there translation resources for RUHS?
Gabriela: Yes, we have a team of 5 translators, 4 Spanish, and 1 Chinese/Mandarin that work diligently on translation projects for different programs and departments at RUHS.
Cary: How many translation projects has this team completed?
Gabriela: In the 12 months from July 2021 to June 2022, the translation team completed 205 translation projects. The complexity of these projects ranges from low to high and some take longer to complete than others. There are many factors to consider such as the word count of the original document, the document format, the number of pages, not to mention the source language, and our thorough review process. We have translated medical records from foreign countries, patient education materials, consents, hospital communications, marketing materials, and much more.
Cary: What is something new that is happening with Language and Cultural Services?
Gabriela: I am proud to share some initiatives we are currently working on. We are always looking for ways to improve our services and ensure that we provide the best possible care for our patients. We provide continuous support to sustain the success of these initiatives and are continuously monitoring and making assessments to adjust for evolving needs at RUHS.
One of our latest initiatives would allow us to extend in-person language access services for patients that are admitted to the emergency room at RUHS Medical Center during the night shifts. This would amplify our in-person services to patients and families that visit RUHS after normal business hours. This is still in the development stages, but we are hopeful that it will be up and running in the near future.
Another project we have been working on for the past year and a half is introducing additional technological resources into departments and locations that experience high LEP volume. Virtual interpretation services are now accessible through a mobile

application on iPads. We have delivered over 150 new iPads equipped with the application throughout RUHS Medical Center, Arlington Campus, and Community Health Centers. Currently, we are in the process of incorporating more throughout other locations. In addition to delivering the equipment, we provide training to staff ensuring an optimal end-user experience.
Cary: In the time that you’ve been a part of Language and Cultural Services, how has the program changed for the better?
Gabriela: I onboarded with RUHS - Language and Cultural Services in April of 2021. I am constantly saying that I feel so proud to be a part of this team because our services are evolving alongside the healthcare system. One example is, we are a department that makes data-driven and evidence-based decisions. We closely monitor the performance of our program. We are continually measuring and analyzing data to improve the quality of care that we provide our LEP community. The data we collect also plays a big part in determining the department’s future direction and our overall organization. We have been able to use data to address the needs of RUHS departments and locations. Some of the data analyzed include language mix, interpreter utilization by department/ location, encounter types, translation requests, and more. This data supports decisions we make regards to workflows, budgets, and staffing needs.
Cary: How are Language and Cultural Services connected to other programs? How does this benefit the patient?
Gabriela: Language Access Services are important and play a significant role to provide holistic care for patients. Language and Cultural Services works collaboratively with all RUHS programs to facilitate communication. We provide departments and other programs access to professional medical interpreters ensuring that patients have full and equal access to all services provided by RUHS. Healthcare and communication are two critical areas that must work together to deliver the best possible care for patients. We connect to other programs by serving our purpose.
In my experience, I have learned that when patients are provided language access, they have a golden opportunity to become engaged in their healthcare. Once a patient understands their condition(s), care plan(s), and healthcare, they make behavioral
changes. They become more compliant taking initiative and ownership, making necessary adjustments to their lifestyle fully knowing they have a chance to improve their quality of life.
Cary: Is there someone in your department who serves as a role model or a great example of the program’s ideals?
Gabriela: If I am, to be honest, all our medical interpreters serve as role models. Medical interpreters are often the unsung heroes of the healthcare world. People don’t realize what they endure when they interpret encounters in the first-person role. It is amazing to me how they can immediately go from encounter to encounter and mentally adjust in between. Sometimes they have less than five minutes in between and depending on the types of encounters some of them are tough. Just to give you an idea, we have had medical interpreters perform more than 300 in-person encounters in one month. Our team is a great example of what it means to be a professional medical interpreter, the hard work it entails, and the professionalism needed to fulfill the needs of the LEP community. They are truly inspirational.
Cary: What tech or platforms help improve patient care and/or improve patient outcomes?

Gabriela: The application in the iPads used to access a virtual interpreter has added value to patient
care and outcomes in the sense that the service is mobile and innovative all at once. This makes it possible to provide our services as needed. It’s great technology and is very easy to use. This benefits patient outcomes in many ways. When a patient comprehends their responsibilities, they make informed decisions about their health. Which in turn, also plays a big part in shortening hospital length of stay and reducing hospital readmission rates.
Cary: What are you looking forward to in the future?
Gabriela: Healthcare evolution has taught me to be a visionary advocating for growth and change when necessary. In the future, I look forward to the possibility of incorporating community outreach into our services. Promoting and raising awareness of our language access services is powerful. We can encourage the LEP community to seek healthcare for their conditions, whether chronic or acute. The more we reach out to the community, the more population health has the potential to improve. We want our communities to feel supported in knowing that we do everything we can to reduce healthcare disparities. We provide them with equal access to all our healthcare programs, and we want them to know RUHS provides language access services at no cost to them when they are visiting any of our facilities.
 HARA
HARA
Dentistry can resolve many of the common oral health problems patients face. Modern materials and techniques are evidenced based and provide long lasting functional and cosmetic results. Why then, when we have these capabilities, do people still struggle with dental problems? Although people may want to go forward with treatment, barriers exist preventing them from doing so. These barriers come in many shapes and sizes, and only by applying a tailored solution that takes into consideration the whole patient can we overcome them. Where some offices may view patients as a collection of dental problems, our department is taking a holistic approach that strives to understand our patients, and doing so help them better navigate the
issues that are keeping them more completely from optimal health. In this article, I’m going to focus on three of the biggest barriers that our patients face and how our team is helping to remove them.
Socioeconomic barriers are perhaps the easiest to recognize. Modern dentistry is incredibly advanced but often has a price tag that many find out of reach. Fortunately for our patients, the Federally Qualified Health Center (FQHC) model has largely removed finances from the equation, because all treatment rendered at the clinic is completely covered by Medi-Cal or for a nominal fee based on income. Despite this huge benefit, indirect costs associated with care still make dental treatment too expensive

for some. For example, not all patients have paid time off, so missing work means losing income, and taking time off work now becomes an expense. With this in mind, we strive to accommodate work and childcare schedules. We also make a deliberate effort to help patients group their dental visits with their other appointments, so they miss less work and can complete treatment in as few visits as possible, minimizing these indirect costs. Additionally, those with socioeconomic barriers are often forced to choose between access to care and quality. I am extremely proud that the dental techniques and materials used in our clinics are exhaustively researched and are of equal and often better quality than those found in private dental practices. All of our clinics utilize state of the art equipment with institutional levels of infection control and quality assurance. We are truly removing this barrier, improving access to care without sacrificing quality or the patient experience.
clinics are generally located close to public transportation. In general, our patients face a lot less resistance when establishing care at our office. It isn’t unusual for an individual who hasn’t seen a doctor in years to quickly find themselves with a new primary care provider and dentist all in the same day.
Finally, even if patients can access care, other barriers could prevent them from achieving optimal treatment outcomes. Research is linking systemic health to oral health and emerging evidence suggests that treating oral health conditions may even improve chronic problems elsewhere in the body. Perhaps the best example of this connection is gum disease. According to the CDC, 47.2% of adults aged 30 and older and 70.1% of adults 65 years and older have some form of gum disease. Left untreated, this chronic condition can affect or worsen the body’s ability to manage other inflammatory conditions like cardiovascular disease, rheumatoid arthritis and type 2 diabetes. If our treatment takes a one-sided approach, we diminish our ability to overcome this last barrier. This is why our team makes it a priority to educate patients on these connections with the end goal of helping them to improve both their oral health and their systemic health. However, even patients without dental problems benefit from our holistic care messaging. Because of our shared electronic health record (EHR) we can help track their blood pressure, stress the importance of taking prescribed medications and help remind patients of necessary vaccinations. By engaging with patients as part of a collective healthcare team, we help patients achieve optimal outcomes.
Our patients also face numerous logistical barriers. Navigating the healthcare field in a second language, arranging reliable transportation, and locating an in-network clinic can take weeks. However, because dentistry is one part of a common facility (with our colleagues in primary care, pharmacy and behavioral health right down the hall) our patients only wage this war once. We also utilize the same electronic health record—Epic—allowing us view and share information with the other healthcare teams. So, when a patient comes into the dental clinic often, we are building on an existing relationship. We already know their primary care providers, their medications, and their current health issues, so patients don’t have to start from scratch when they see us. Most of our staff is bilingual and we have interpretation services readily available. Our
Treating the whole person is essential to developing long lasting relationships with patients. At our clinics where dentistry is integrated into the healthcare team, patients benefit from our holistic approach to healthcare at a level they may not be able to find elsewhere.



The teams previously known as Whole Person Care (WPC) and Health Homes Program (HHP) are now known as CalAIM Enhanced Care Management (ECM). They’re now comprised of a group of care managers within all community health clinics as well as the main campus. Each team has:
• An RN care manager
• A Behavioral Health Specialist (BHS) care manager
• A Care Coordinator (CC)
• Two Community Health Workers (CHW)
The goal of this group is to provide care management to high risk, complex needs patients, with the intention of helping them improve their health and reduce the impact of chronic disease. Each member of the ECM team is trained in motivational interviewing and employs this training when they set goals. Since the goals are set with the patient, the patient is more likely to be engaged in reaching them.
The team receives a list of high need patients from Inland Empire Health Plan (IEHP). IEHP uses two social determinants of health (SDOH) risk screens, (the John Hopkins ACG screen and the Healthy People Index (HPI) screen). Patients are rated as high, medium and low risk for utilization of resources, including unnecessary emergency department usage, and inpatient utilization. Depending on the level of risk, the ECM team contacts enrolled patients between one and two times per month and often, more frequently.
To start care, ECM team members complete an initial screening to determine eligibility for enrollment. They also complete a Whole Person Health Score (WPHS) screen and a CHA. ECM team members have relationships with, and access to, many community and County services and make referrals to resources through Connect IE and other methods. The team also ensures that these referrals are provided or, they problem solve with patients/clients to
assist with barriers.
An ECM team can enroll up to a total of 250 patients into care. There are targets set for enrollment per team member, as well as, per team. The entire RUHS ECM team also has targets for achievement in the following areas:
• Creating/implementing/updating a care plan on a monthly basis (or more frequently depending on risk stratification).
• BP documentation
• BP achievement
• PHQ9 documentation

• PHQ9 improvement
• A1C documentation
• A1C improvement
• Completion of a CHA
The ECM team enrolls clients who are screened and referred by the RNs in the Probation Department also as transition out of incarceration is one of the enrollment criteria. There have been almost 17,000 probationers screened. In data analysis on outcomes, there was a 65% reduction in reincarceration. There are many success stories from this group. Here is one example of someone who was helped by this team:
SITUATION:
-Client had multiple medical problems, including congestive heart failure, hypertension, atrial fibrillation and, recent hospitalization for pneumonia requiring a thoracentesis. He was told that his heart was working at 10% from meth-induced cardiomyopathy. He was wearing an external life vest defibrillator and reported feeling recent shocks. He said the doctor gave him 6 weeks to live.
-Other diagnoses included were depression and anxiety. Client and longtime/supportive girlfriend were homeless, which made charging
his defibrillator difficult.
-Client was not interested in going to a shelter due to crowds and the possibility of being separated from girlfriend.
SUCCESS:
-WPC Outreach Team met with client and obtained information that the client was a Veteran. Client was placed in brand new Veteran housing within a month of screening.
-His health improved drastically. His heart function increased to 40% and he no longer needs the external defibrillator. He also married his girlfriend.
The Enhanced Care Management team can assist the highest risk members of the community with their training and knowledge of available resources. The populations who may qualify for ECM enrollment are as follows:
Has one of the following:
• Lacks a fixed, regular, and adequate nighttime residence
• Has a primary residence that is a public or private place not designed for, or ordinarily used for habitation
• Lives in a shelter
• Is exiting an institution to homelessness
• Will imminently lose housing in the next 30 days
• Is an unaccompanied youth or member of a family with children and youth who are defined as homeless under other Federal statues
• Is fleeing domestic violence
And has one of the following:
• Complex physical health need*
• Complex behavioral health need*
• Complex developmental health need*
*with inability to successfully self-manage, for whom coordination of services would likely result in improved health outcomes and decreased utilization of high-cost services
Has one of the following:
• 5 or more emergency room visits in the last 6 months
• 3 or more unplanned hospital* and/or short-term skilled nursing facility stays in the last 6 months
*unplanned hospital stays exclude voluntary surgeries and deliveries
Has all of the following:
• A DSM diagnosis of substance-related and addictive disorder (excl. tobacco use)
• One or more complex SDOH risk factors*
And one of the following:
• At high risk for institutionalization, overdose, and or suicide
• Use of hospital, ER, or urgent/crisis care for sole source of care
• Two or more ED visits or two or more hospitalizations due to SMI or SUD in the last 12 months
*e.g., lack of access to basic needs, inability to work or engage in the community, former foster youth, recent law enforcement contact related to mental health or substance use.
Has all of the following:
• A DSM diagnosis of mental disorder (or one is suspected)
• Experiences personal distress, disability or dys function in social/work/personal life, or at risk of loss of function related to social/work/personal life
• One or more complex SDOH risk factors*
And one of the following:
• At high risk for institutionalization, overdose, and/or suicide
• Use of hospital, ER, or urgent/crisis care for sole source of care
• Two or more ED visits or two or more hospital izations due to SMI or SUD in the last 12 months
*e.g., lack of access to basic needs, inability to work or engage in the community, former foster youth, recent law enforcement contact related to mental health or substance use.
• Is an individual transitioning from incarceration in the last 12 months
And has at least one of the following:
• Chronic mental illness
• Substance Use Disorder (SUD)
• Chronic disease (e.g., hepatitis C, diabetes)
• Intellectual or developmental disability
• Traumatic brain injury
• HIV or pregnancy
DIVISION CHIEF PULMONARY AND CRITICAL CARE MEDICINE
For several years, Riverside University Health System (RUHS) – Medical Center has been part of a national movement to work to reduce the incidence of delirium in the Intensive Care Unit (ICU), to support more positive outcomes for the patient. Known as the ICU Liberation Bundle (A-F), these methods were developed with the goal of guiding healthcare workers to ways that can limit, or eliminate delirium, which is common during hospitalization. There are three major subtypes of delirium: hyperactive, hypoactive, and the most common type, which is a mixed form of both hyperactive and hypoactive delirium. In a general sense, delirium is a disturbance of consciousness or acute change in cognition, as well as a reduced ability to focus or shift attention.
“What we know is that about 50 to 80% of all patients who are hospitalized in an ICU will develop some form of delirium. We also know that if a patient develops delirium, there’s a likelihood of increased mortality, upwards of 10%,” said Dr. Walter Klein, Division Chief of Pulmonary and Critical Care Medicine at Riverside University Health System. Dr. Klein noted that in prior years, common practice was to use various medications to treat delirium, such as antipsychotic medications or different sedatives, but none of these seemed to reverse delirium within the ICU. With that in mind, the best treatment appears to be prevention.

Dr. Klein is supportive of the ICU Liberation Bundle, stating that “a move towards this [bundle] is a huge step towards holistic, patient-centered care. We’re no longer treating a diagnosis; we’re treating the patient.” What is the ICU Liberation Bundle? In short, it’s a series of steps, labeled A through F, that correspond to individual elements that have shown to assist patients in avoiding de-
lirium during their hospital visit.
• A Element: Assess, Prevent, and Manage Pain
• B Element: Both Spontaneous Awakening Trials (SATs) and Spontaneous Breathing Trials (SBTs)
• C Element: Choice of Analgesia and Sedation
• D Element: Delirium: Assess, Prevent, and Manage
• E Element: Early Mobility and Exercise
• F Element: Family Engagement and Empowerment
These six elements are implemented with a goal of controlling pain and minimizing sedation, both of which are clearly associated with an increased risk of developing delirium in the ICU. Additionally, the healthcare team will perform a paired spontaneous awakening, where the sedation is removed and a spontaneous breathing trial is done. When combined with mobilization and family engagement, these techniques have impressive results.
According to the Society of Critical Care Medicine’s (SCCM) website*, these changes can make a huge impact on the outcome of a patient’s visit to the ICU. “By fostering a holistic approach to treating patients and improving ICU team communication, the ICU Liberation Bundle has been proven in multiple studies involving more than 20,000 patients to:
• Decrease the likelihood of hospital death within seven days by 68%
• Reduce delirium and coma days by 25% to 50%
• Reduce physical restraint use by more than 60%
• Cut ICU readmissions in half
• Reduce discharges to nursing and rehabilitation facilities by 40%
At Riverside University Health System, the results have been positive, with multiple disciplines stepping in early in the patient’s care, even if the patient is on mechanical ventilation. Dr. Klein says that “we are getting physical therapy, occupational therapy and speech therapy involved, doing cognitive therapy and mobilizing patients early in their treatment.” The team approach is an exciting aspect, because everyone has the ability to participate in this bundle, from the physician team to the bedside nurses and therapists.
When Dr. Klein and the RUHS team began implementing this bundle in 2015, there was a lot of education and training, that is continuing today as they onboard new team members. Rolling out this program was a positive thing, overall. He noted that the arrival of the COVID-19 pandemic has provided some challenges for many reasons, one of which being the lack of engagement of family and friends, which has been limited by ongoing visitor restrictions. Additionally, the pan-
demic has led to an influx of temporary healthcare workers (often referred to as ‘travelers’), so there’s a learning curve for those members of the team, and it also generates the need for constant training of new staff.

As the healthcare community continues to rebuild from the pandemic, the goal is to get engagement from across all disciplines to provide holistic treatments to every patient. “Ultimately, I feel that this is the reason why all of us went into medicine, to focus on patient-centered care,” said Dr. Klein, and he believes that this approach offers opportunity to positive interactions between different care teams, stating “I think this is something that will grow with time and allow for collaboration across disciplines, which is one of the most exciting things for me.”
*https://www.sccm.org/Clinical-Resources/ICULiberation-Home/ABCDEF-Bundles
In a rural corner of rural Mississippi in the 1960s, a physician pioneer named Dr. Jack Geiger opened one of the first community health centers in the nation. After meeting with the people in the local community, he identified high rates of severe malnutrition in the children and young adults. He came up with a radical idea: to prescribe them food. Dr. Geiger wrote out prescriptions for food to be used at local grocery stores; he asked the grocers to send the bill to his clinic pharmacy.
The federal agency that funded the health center (the Office of Economic Opportunity, later part of the Department of Health and Human Services) sent an official to stop Dr. Geiger and remind him that the allocated money could only be used for “medical” purposes and a pharmacy can only dispense medications. Dr. Geiger famously replied: “Well, the last time that I looked in my textbooks, the specific therapy for malnutrition was food.” Through his intervention and advocacy, Dr. Geiger and his team effectively ended malnutrition in the county they served. He built a prolific career based on championing the principles of social medicine: that a physician’s duty is to treat the whole person, beyond the four walls of the clinic, through community health action and advocacy.
It was this same idea that led to the development of the “Food is Medicine” program at RUHS Moreno Valley Community Health Center. Our initial plan was to implement a food prescription (Food Rx) model and


partner with local farmer’s markets and grocery stores to connect our patients with low-cost fresh produce. But after the COVID-19 pandemic shut down many of those in-person opportunities, we listened to the needs of our patient community and pivoted to planning for direct food distribution from within our clinic space.
We began with a community needs assessment using the “Hunger Vital Signs,” a two-item validated screening tool for food insecurity. In the first months of the pandemic, over one-third of our clinic patients screened positive for food insecurity. This data reinforced the stories we heard from our patients: those people living in lower-income communities were at greatest risk of health disparities as a result of the COVID-19 pandemic. But these problems were not due to the virus alone; they were the consequences of generations of structural inequities and policies that created food deserts and lack of access to adequate nutrition.
In late 2021, our “Food is Medicine” program catapulted from idea to implementation through collaboration with RUHS Public Health. The CalFresh Healthy Living team, led by Valerie Comeaux, identified a community partner in Feeding America Riverside San Bernardino (FARSB) to deliver food boxes each month to our community health center. These food boxes contain shelf-stable goods such as beans, grains, pasta, milk, canned fruits and vegetables, and other nutrition support for our patients. Furthermore, Valerie and
the RUHS Public Health team coordinated nutrition education classes to help patients and their families incorporate the contents of the food boxes into their healthy lifestyles.

This month marks the one-year anniversary of the “Food is Medicine” program at Moreno Valley Community Health Center. At the start of this journey, we were discouraged at the overwhelming volume of patients who initially screened positive for food insecurity in our clinic. Through the steady implementation of our program since last November, our community impact increased from a handful of brochures and referrals to over one-thousand food boxes distributed into the community.
I am deeply inspired by the entire team that supported this critical intervention, including our patients, community partners, clinic staff, and program volunteers. The “Food is Medicine” program truly reflects the whole-person approach to care championed throughout the RUHS network.
We further improve upon our existing program by listening to our partners at each stage of implementation. Based on the collective feedback of our patients and staff, we plan to expand the “Food is Medicine” program into our entire network of community health centers in the coming year. Our next steps include incorporating a delivery service (through a partnership with DoorDash) for patients with limited transportation options. In addition, we are coordinating with a community garden at UC Riverside to bring fresh produce to our patients who screen positive for food in-
security.
Each of these innovations is buoyed by the expertise of the RUHS Public Health team; their perspective helps us find collaborative solutions that are community-based, practical, and sustainable for the future. We plan to utilize the resources of our RUHS Population Health teams to match these important nutrition interventions with health outcomes for chronic disease management.
The significant health disparities highlighted by the COVID-19 pandemic were the catalyst for implementing the “Food is Medicine” program. There are still major structural and policy changes necessary to improve access to healthy foods for the communities we serve. But with the momentum from this last year in addressing food insecurity, I am confident that our team will continue using the whole-person perspective to bend the arc towards health justice for our patients and their families.
In the last two months, the RUHS Family Medicine Residency Program interviewed over one-hundred fourthyear medical students for one of twelve internship positions for the next academic year. At the end of each interview, the students ask a series of questions that tend to blend together over time. But the question that I love is when a student asks why I choose to work at RUHS for the last eight years. The answer is simple: because everyone I work with believes deeply in our mission of treating both the patient and community, using the whole-person principles of social medicine.
 STEVE SERRAO MD, MPH, PhD
STEVE SERRAO MD, MPH, PhD
RACHEL CARSON PHYSICIAN ASSISTANT
BREANNA REYES-GARCIA PHYSICIAN ASSISTANT
Dr. Steve Serrao:Many gastroenterology disease conditions can be traced to lifestyle and whole person care. The impact of years and decades of insult to the body by unhealthy food choices, alcohol and smoking are cumulative and can result in terminal disease. Furthermore, we are recognizing the importance and impact of the brain gut axis in patients with inflammatory bowel disease and even among healthy patients. Our Gastroenterology team has put together a collection of conditions that are overlooked and are silently impacting our patients.
Dr.
Wichit Srikureja:How often do you think about your pancreas? Interestingly, the pancreas is crucial to your health and survival, as it is responsible for two of the most important basic functions of life. First, the pancreas secretes digestive enzymes so our gastrointestinal (GI) track can break down and absorb nutrients (vitamins, minerals, fats, and glucose to name a few) from our diet. Second, once the GI tract absorbs these nutrients. The pancreas is then critical in empowering cells to use the nutrients. For example, the pancreas secretes insulin which enables cells to utilize the glucose they require to work and survive. Without insulin, a person would starve to death no matter how much they ate. With such critical roles to play, it only makes sense to take care of our pancreas.
Pancreatic diseases range from an inflammation called pancreatitis to pancreatic cancer. In the case of some patients with pancreatitis, the inflammation of their pancreas never goes away and is called chronic pancreatitis, a life disrupting and painful condition. Currently, pancreatic cancer is the fourth leading cause of death in our country.
Often, the first time a person learns they have pancreatic cancer is when they visit a doctor because of unexplained stomach pain, jaundice (yellowing of skin and the whites of the eyes), and unintentional weight loss.
For too many, their cancer is already in an advanced stage. Although there are no guarantees, there are certain things known to reduce the risk of pancreatic cancer and pancreatic diseases. First, if you are a smoker, quit. Smoking is an avoidable risk factor for pancreatic cancer. Second, stop drinking alcohol. Heavy alcohol is linked to pancreatic cancer. It is also known that heavy alcohol use can lead to acute and chronic pancreatitis. Chronic inflammation increases pancreatic cancer risks. Third, maintain a healthy weight.
Fourth, eat a healthy diet because it is known to reduce the risk of pancreatic cancer. A diet low in sugar, low in processed and red meats, high in whole grains, fruits and vegetables contributes to the overall health of the pancreas. Let’s keep our pancreas happy as it continues to work in the background to make life happen for all of us.
Dr. Pejman Solaimani:
Non-alcohol fatty liver disease (NAFLD) is defined as accumulation of fat in liver cells. NAFLD is the most common liver disorder in western countries and is mainly related to western diet and lifestyle resulting in central obesity, high cholesterol, and diabetes.
Recent advances in healthcare have resulted in significant progress in treatment and eradication of hepatitis C, however, preventing and or reversing NAFLD continues to be challenging in western societies. Most of us believe that if we don’t drink alco-
hol, our liver will be fine. Although avoiding excessive alcohol intake can prevent liver damage, other factors such as a healthy diet, regular exercise and other healthy lifestyle modifications are crucial to maintain a healthy liver. Unfortunately, NAFLD can result in inflammation, fibrosis and in most severe cases, cirrhosis. Cirrhosis is an end stage liver disease and is associated with several complications. It increases risk of confusion, ascites, GI bleeding and liver cancer, among many other complications. I can speak for my gastroenterologist colleagues that most of our most challenging cases are when cirrhotic patients present with variceal bleeding requiring emergent upper endoscopy. Although most cases are addressed successfully, there are situations that patients don’t make it because they waited too long.
It is time that we educate our patients on NAFLD risks and the importance of healthy lifestyle modifications. A multidisciplinary approach is critical getting primary care providers, dieticians, and specialists such as endocrinology together would take us in the right direction to minimize the NAFLD risk factors such as obesity, diabetes, and high cholesterol.
Dr. Manish Shrestha:
Inflammatory bowel disease (IBD), comprising ulcerative colitis (UC) and Crohn’s disease (CD), is a chronic inflammatory disorder of the gastrointestinal tract. UC involves the colon, whereas CD can affect any part of the luminal gastrointestinal tract. It is estimated that approximately 3 million US adults have IBD and arises from an uncontrolled immune mediated inflammatory response to intestinal bacteria and their products in genetically predisposed individuals. Its clinical course is highly heterogenous, with symptoms ranging from mild to disabling and severity ranging from mild to severe disease. Although a predominantly intestinal disease, IBD can affect other organ systems, such as joints, eyes, skin, liver, lung, and pancreas. Early diagnosis and prompt treatment are of utmost importance to improve outcomes and maximize well-being. The management of IBD is rapidly evolving. IBD patients are more likely to suffer from depression, anxiety, fatigue, sleep disturbance and social dissatisfaction than the general population. Despite increased risk for infections, bone disease, and certain malignancies, IBD patients are not receiving preventative care services at the same rate as the general population. In addition to treatment approach directed at healing inflammation, a more
comprehensive, holistic approach to IBD care that address the physical, psychological, and social well-being of patients living with IBD realizes the best outcomes for our patients.

Rachel Carson and Breanne Reyes Garcia: It’s no secret that there is a huge brain-gut connection. We notice it throughout our lives; butterflies in our stomach when we see a romantic interest, nausea when we must get in front of a crowd to speak, however, we are reluctant to accept that connection when the symptoms become problematic such as they do with Irritable Bowel Syndrome (IBS), not to be confused with Inflammatory Bowel Disorder (IBD). Mental health is so stigmatized that we are often unwilling to admit the toll it takes on our physical bodies. Patients are often taken aback when they receive a diagnosis of IBS, they feel as though they are being told that their symptoms aren’t real; there must be something else wrong to explain the abdominal pain, the unexpected and unpleasant changes in bowel habits.
The symptoms of IBS for many are triggered by stress/anxiety, and it’s a vicious cycle because those symptoms trigger more stress/anxiety. It truly begins to affect people’s day-to-day lives, having to schedule their whole day around fear of what symptoms might crop up. It’s important to take time with these patients and provide them with reassurance and resources that can help them overcome these symptoms, such as providing them with a referral to a Nutritionist to help them follow a low FODMAP diet (a diet low in sugars that may cause intestinal distress), telling them about IBS guided apps such as Nerva, and making sure they are setup with Behavioral Health. Most patients end up being appreciative and overall see symptom improvement when the time is taken to provide them with support they need.
 JENNIFER STEWART RDN, MBA PUBLIC HEALTH PROGRAM DIRECTOR
JENNIFER STEWART RDN, MBA PUBLIC HEALTH PROGRAM DIRECTOR
-Hippocrates, Father of Modern Medicine


“Eat food. Not too much. Mostly plants.”
Are you eating enough fresh produce? The 20202025 Dietary Guidelines for Americans recommend 1.5 - 2 cup equivalents of fruits and 2 - 3 cup equivalents of vegetables daily. A healthy diet supports immune function and also helps to prevent obesity, type 2 diabetes, cardiovascular diseases, and some cancers. Centers for Disease Control (CDC) used the most recent 2019 Behavioral Risk Factor Surveillance system (BRFSS) data to estimate intake. However, only a small amount of people consume enough produce, with the survey finding that overall, only 12.3% of adults met fruit recommendations and 10.0% met vegetable recommendations.
With this guidance in mind, Riverside University Health System- Medical Center and other sites throughout Riverside County have paired up with the Women, Infants and Children (WIC) supplemental nutrition program to offer the ability to use WIC Fruit and Vegetable benefits and summertime WIC Farmers Market checks.
Those receiving CalFresh benefits can also shop at
farmers markets that accept EBT, and as an added benefit, their dollar buys twice as much at markets participating in the Market Match program. Senior Farmers Market Nutrition Program coupons are also offered seasonally.
Going to a local farmers market in Riverside County is a convenient and uplifting experience. You see the proud faces of the farmers who have put their hearts into growing foods to nourish the community. They rise early on the morning of the markets to bring the freshest produce to sell. They get to meet new people weekly, see their regulars, and let them sample fruits and vegetables – possibly for the first time.
Eating local produce has so many benefits to the residents of our county. Fresh produce picked in the morning provides the fresh, ripe items to sell; there are not days needed to transport the produce to sell it and it benefits the local economy by supporting our local agriculture.
“Let food be thy medicine and medicine be thy food.”
- Michael Pollan, AuthorFarmersMarketatRiversideUniversityHealthSystem-MedicalCenter. PhotobyCameronCramer
RUHS Nutrition and Health Promotion Branch’s WIC and CalFresh Healthy Living Grant staff are proud to support the farmers markets. The WIC program provides both the seasonal (June to September) $28 farmers market checks and monthly $25 - $49 fruit and vegetable benefits per participant to purchase produce, and these benefits are being utilized by local families. For example, in 2021, from June to September 6,700 WIC families used 17,169 WIC seasonal checks to purchase produce at the markets, adding $120,183 to the local farmers economy. This does not take into account the monthly WIC fruit and vegetable benefits or the Market Match dollars.
Additionally, WIC health educators are stationed at farmers markets throughout the county during the summer market hours and can utilize the technology of the web-based WIC WISE program to allow WIC participants to be certified to pick up the checks and receive nutrition information regarding

the best use of the produce. Having the staff on site increases redemption of the coupons which in turn puts more produce on the tables of families with young children.
CalFresh Healthy Living Staff provide extra coordination promoting the Market Match at the farmers market. Using this program, families can further extend their purchasing power and receive a matching amount of money to spend, up to $10 per visit, when using their monthly WIC benefits, WIC farmers markets coupons or CalFresh EBT. Participants can use this Market Match benefit monthly.
If your goal is to incorporate more fresh produce into your regular diet, consider making a visit to a local farmers market part of your weekly routine. Shopping at farmers markets is a great way to support local farmers, and get the freshest possible fruits and vegetables on your table. To learn more, please visit: rivhero.com and marketmatch.org.
The Podiatric Surgery Team at Riverside University Health System is offering comprehensive services that are nothing short of life-changing. After a discussion with Dr. Joseph Park, it’s clear that providing care for patients’ foot issues has come a long way over the past few decades. “What we have at RUHS is this system where we provide care for all patients with foot and ankle problems. That ranges from people with diabetic foot exams, all the way up to complex deformity and reconstruction.”
The podiatric surgery staff works in collaboration with multiple departments to help patients manage the challenges with their feet and basically everything below the knee. Providing the best care often involves a multidisciplinary approach, so while the podiatric team works primary on the foot and surrounding areas, internal medicine doctors help the patient to manage their diabetes, and vascular surgeons help improve blood flow to help things heal. Understanding that what they do is often tied to other areas of a person’s health, as well as their overall care plan, is an important and exciting part of what the podiatric surgery team does every day.
A large focus of the podiatric surgery team is helping those who haven’t been able to get the care they need. According to Dr. Park, “They’re just unable to find the time to go to the doctor’s office because they need to provide for their families. In doing that, they often neglect themselves, and by the time they see us, it’s in an emergent situation and we’re dealing with a limb salvage or life-saving situation.” While preventative care would be ideal, in cases where that wasn’t possible, RUHS’s podiatry staff can handle amputations, as well as complex surgeries to help people save their limbs, which is critical for quality of life.
“Mobility is life. If people don’t have the ability to ambulate independently, that decreases quality of
life and longevity of life as well. People’s expected lifespan is dramatically decreased if they get an amputation,” notes Dr. Park. The podiatry team also works with patients after they are discharged, understanding that care doesn’t stop when the patient leaves the hospital. To ensure that patients are getting the proper home care, whether it’s a complex wound or a situation that requires a home health nurse visit, they coordinate that, as well as physical therapy to help them learn how to put weight back on their foot.
One thing about podiatry is very clear: there is a seemingly endless amount of challenges, as well as treatments. Dr. Park commented that while “infection and diabetes are a lot of what we do, but we also see people who have painful musculoskeletal deformities, like a bunion. We also see complexities such as a club foot that wasn’t treated properly when they were a child, and now they’re an adult and their foot is literally turned sideways. We can help them with everything, from the sports medicine side of things, all the way up to surgery.” Dr. Park believes that the variety of the day-to-day is the reason why most people pursue this field; they are rewarded with involvement in the full spectrum of patient care.
Dr. Park also noted that RUHS’s team is truly exceptional, in that all four of the attendings (Dr. Adrienne Estes, Dr. Rebecca Moellmer, Dr. Kelly Parks, and Dr. Park himself) are fellowship-trained, which is extremely rare in the podiatric world, as typically only 5 to 10% of this specialty have fellowship training. All four are also faculty at the Western University of Health Sciences College of Podiatric Medicine. Another example of the unique qualifications that the RUHS team has, is that Dr. Estes specializes in Charcot reconstruction. Dr. Park says that “many times a patient will come in for a second or third opinion, because they’ve been told that amputation
is the only option. Sometimes, it is. But sometimes, we can help these patients and after multiple surgeries, and many months of care, they’re walking! Many times, we are able to save the foot!”

Admittedly, podiatric surgery has come a long way in the last few decades. Dr. Park observed that “in the last ten years or so, podiatric medicine and surgery is becoming more integrated with mainstream medicine. Most of our patients are very medically complex, so we’re working with diabetes, kidney disease, heart disease and everything in between!”
It’s clear that the podiatric surgery team has taken so many steps (pun intended) to elevate the quality of care that they provide to RUHS’s patients and they’re not finished yet. The team is expanding their services to include a limb salvage program, led by Dr. Molkara, and are also aiming to launch a residency program within the next few years. Dr. Park is looking forward to the future and said that “the team we have at RUHS is a unique group of individuals who are able to provide high level care. It is extremely rare to have this level of training in the podiatric world. It’s very exciting.”

 VIKRAM KUMAR MD, MBA CHIEF HEALTH INFORMATION OFFICER
VIKRAM KUMAR MD, MBA CHIEF HEALTH INFORMATION OFFICER
To emphasize the evolving digital/human interactivity, this article was completely generated by ChatGPT,anAIlanguagemodeldevelopedbyOpenAI,withminoredits(italicized)madebytheauthor. The images used were generated by DALL-E, an AI imagegenerationmodeldevelopedbyOpenAI.The authorhasreviewedthearticleforaccuracy.
The digital presence as it applies to healthcare refers to the collection and use of electronic data and information related to an individual’s health and wellbeing. This can include a wide range of data, such as personal health information, medical, behavioral,andsocial history, lab results, and medication records, which are stored in electronic health records (EHRs) or other digital systems.
The digital presence of individuals can have a significant impact on their holistic healthcare experience and wellbeing , as it allows healthcare and other providers to access and share important information about their health in a secure and efficient manner. This can improve the continuity of care, reduce the risk of errors, and provide valuable data for research purposes.
The current state of digital health is rapidly evolving and growing. The widespread adoption of technology in healthcare has created new opportunities for improving patient outcomes, reducing costs, and enhancing the overall delivery of care. Digital health includes a wide range of technologies such as electronic health records (EHRs), telemedicine, mobile health apps, wearable devices, and artificial intelligence. These technologies are being used to improve patient engagement, streamline clinical workflows, and drive more personalized and effective treatment plans. Despite the rapid growth, there are still challenges in digital health, including data privacy and security, interoperability, and regulatory barriers.
The future state of digital health is expected to be characterized by more advanced technologies, more seamless integration, and more widespread adoption. Predictive analytics and artificial intelligence are expected to play a larger role in clinical decision making and personalized medicine. Remote monitoring and telemedicine are expected to become more widespread, enabling more convenient and accessible care for patients. The use of wearables and mobile health apps is also expected to increase, allowing patients to take a more active role in managing their own health.
There is also expected to be a greater emphasis on data privacy and security, as well as on developing common standards and protocols for data exchange. Additionally, there will likely be a greater impetus on integrating digital health with traditional healthcare systems, creating a more comprehensive and seamless healthcare experience for patients.
In short, the future state of digital health is expected to be more advanced, more convenient, and more focused on empowering patients to take control of their own health.
The term “whole person health score” is a broad and general concept that refers to an evaluation of an individual’s overall health and well-being. It typically takes into account a wide range of physical, mental, and social factors that contribute to a person’s health, such as exercise habits, nutrition, stress levels, and access to healthcare services. The main purpose of a whole person health score is to provide individuals with a more holistic and comprehensive understanding of their health and well-being. By considering multiple factors, rather than just one or two, whole person health scores can provide a more accurate picture of a person’s overall health status and help identify areas for improvement. However, the accuracy and usefulness of a whole person health score will depend on the methods used to calculate the score and the sources of data used.
The exact definition and methodology of a whole person health score can vary depending on the organization or system using it. Some whole person health scores may use self-reported data, such as surveys or questionnaires, to determine an individual’s score. Others may use biometric data, such as blood pressure or body mass index (BMI), or electronic health records to create a more comprehensive evaluation of a person’s health.
Riverside University Health System’s (RUHS) Whole PERSON Health Score (WPHS) is a health assessment tool that helps individuals understand their overall health status. The score considers multiple aspects of a person’s health, including physical health, mental health, and social well-being, to give a comprehensive view of their health. The WPHS is designed to help individuals identify areas of their health that may need improvement and to provide them with information and resources to support their health journey. The score is generated based
on information collected through a health assessment questionnaire and can be used as a baseline for tracking progress over time. The WPHS is a component of RUHS’s broader mission to provide comprehensive, patient-centered care and improve the health of the communities it serves.
6.Chronic Disease Management: Digital health technologies can improve the management of chronic diseases by providing access to real-time data, facilitating communication between patients and providers, and enabling more proactive and effective care.
7.Patient Engagement: Digital health technologies can improve patient engagement by providing access to educational resources, health tracking tools, and personalized care plans, enabling patients to take a more active role in managing their own health.
Digital health has the potential to improve whole person health by empowering patients and healthcare providers to address physical, mental, and social health needs more effectively. Some of the ways digital health can achieve this include:
1.Personalized Medicine: Digital health technologies can help providers deliver more personalized care by providing access to a wealth of patient data, including genetics, lifestyle, and health history.
2.Mental Health Support: Digital health technologies can provide access to mental health resources and support, such as online therapy, support groups, and self-care tools, helping to address the growing need for mental health services.
3.Collecting and sharing patient data: Digital health tools can collect and store patient data, such as medical history, lifestyle habits, and health outcomes, allowing providers to have a more holistic picture of the patient’s health.
4.Enhancing communication and collaboration: Digital health tools can help providers communicate and collaborate more effectively, enabling them to share information and work together to provide more coordinated and holistic care.
5.Supporting remote monitoring and telemedicine: Digital health tools can enable remote monitoring of patients and telemedicine consultations, making it easier for patients to receive care from their homes and reducing the need for in-person visits.
8.Health Literacy: Digital health technologies can improve health literacy by providing access to accurate, trustworthy health information, enabling patients to make informed decisions about their health and overall wellbeing.
Additionally, Artificial intelligence (AI) has the potential to help create tailored holistic care plans for patients and care givers by analyzing vast amounts of patient data and making predictions about their holistic health needs including:
1.Predictive Analytics: AI algorithms can analyze large datasets of patient data, such as medical and other records, demographic information, and lab results, to identify patterns and predict future health and life outcomes. This information can be used to create tailored care plans that address specific needs and risk factors.
2.Clinical Decision Support: AI algorithms can provide real-time decision support to healthcare providers, helping them make informed treatment decisions based on the latest medical knowledge and evidence considering the patient andfamily’spreferences.
3.Personalized Medicine: AI can help healthcare providers deliver more personalized care by using patient-specific data to identify individual risk factors, predict disease progression, and recommend treatments tailored to each patient’s unique needs.
4.Symptom Monitoring: AI algorithms can analyze data from electronic health records and patient-generated data, such as symptoms reported through mobile apps, to detect changes in wellbeing and identify potential issues.
By analyzing vast amounts of patient data and making predictions about health needs, AI has the potential to help providers create more effective and efficient care plans for patients.
There are several gaps in the adoption of digital health technologies that can limit their widespread use and impact on patient outcomes. Some of the main gaps include:
1.Cost: The cost of digital health technologies, including hardware and software, can be a barrier for both patients and providers.
2.Interoperability: Digital health technologies often lack standardization and interoperability, making it difficult for providers to seamlessly integrate these tools into their workflows and exchange data between systems.
3.Data privacy and security: The handling of sensitive patient data is a major concern, and there are gaps in the implementation of robust data privacy and security protocols that can limit the adoption of digital health technologies.
4.Regulation: The regulatory environment for digital health is complex and can create barriers for the adoption of new technologies. Regulations need to be updated to keep pace with the rapidly changing digital health landscape.
5.Provider adoption: Healthcare providers may be resistant to change and may not fully embrace digital health technologies, which can limit their uptake and impact.
6.Patient adoption: Patients may not be familiar with digital health technologies and may not trust them, or they may have limited access to devices or internet connectivity, which can limit their ability to use these tools.
Addressing these gaps in the adoption of digital health technologies is essential for realizing their full potential and creating a more efficient and effective healthcare system. This can involve investments in infrastructure, standardization and interoperability, data privacy and security, regulatory reform, provider education and engagement, and patient education and engagement.
There are disparities in digital health due to unequal access and utilization of digital health technologies and services across different populations. These disparities can result in unequal health outcomes and a wider health inequity gap. Some of the main drivers of disparities in digital health include:
1.Socioeconomic status: Lower-income and marginalized populations often have limited access to digital health technologies and services due to financial constraints.
2.Education: Individuals with lower levels of education may have limited digital literacy and may not be able to effectively use digital health tools and fully understand privacy and security.
3.Geography: Rural areas often have limited access to high-speed internet and digital health services, making it more difficult for residents to access and utilize these technologies.
4.Age: Older individuals may not be as familiar with technology and may have limited access to digital devices, making it harder for them to use digital health services.
5.Race and ethnicity: Minority populations may have limited access to digital health technologies due to systemic and institutional barriers, including discrimination and lack of cultural competency in digital health services.
Addressing these disparities in digital health is important for creating a more equitable and accessible healthcare system. This can involve improving access to digital health technologies and services, increasing digital literacy, and addressing systemic and institutional barriers that limit access for marginalized populations.
Overall, digital health can play an important role in supporting holistic care by facilitating the collection and sharing of patient data, enhancing communication and collaboration among healthcare providers, and supporting personalized and proactive care. However, it is important to carefully consider the privacy and security implications of this presence and ensure that individuals have control over their digital presence, including the ability to access and manage their health information.

Edward Bacho, MD EDITOR-IN-CHIEF
Nicole Orr PRODUCTION MANAGER
Ester Parada Bonilla DESIGN DIRECTOR
Lesley Anne Bellows COPY EDITOR AND WRITER
Cameron Cramer PHOTOGRAPHY
ARTICLE CONTRIBUTORS:
Bijan Sasaninia
Breanna Reyes-Garcia
Cary Stueland
Gabriela Vargas
Geoffrey Leung, MD, M.Ed
Jennifer Stewart, RDN, MBA

Joseph Park, DPM, FACFAS
Judi Nightingale, DrPH, RN
Lesley Anne Bellows
Manish Shrestha, MD, MBBS

Moazzum Bajwa, MD, MPH
Pejman Solaimani, MD
Peter Hara, DMD
Rachel Carson
Steve Serrao, MD, MPH, PhD
Vikram Kumar, MD, MBA
Walter Klein, MD, FCCP
Wichit Srikureja, MD
INNOVATIONS WORKGROUP:

Adriana Rosato, MD
Edward Bacho, MD
Frank Flowers Jr., MD
Geoffrey Leung, MD, M.Ed
Mahbuba Khan, MD
Matthew Chang, MD
Michael Mesisca, DO
Nicole Orr
Raul Coimbra, MD, Ph.D., FACS
Ronald Johnson, MD
Shunling Tsang, MD, MPH
Vikram Kumar, MD, MBA
