
17 minute read
Preparing for a Pandemic
from CHF Summer 2020
by MediaEdge
PREPARING FOR
A PANDEMIC Se preparer à une pandémie
Advertisement
By/Par Rebecca Burns
It was the second week of March when things started to change. Schools across the country shuttered their doors to students and employers sent staff home to work. As city streets became eerily quiet amid shelter-in-place orders, hospitals country-wide were abuzz with the hustle and bustle of staff preparing for an influx of COVID-19 patients.
In Quebec, the facilities management team at McGill University Health Centre (MUHC) was readying to go into overdrive. MUHC is a bilingual academic health network spread over four hospitals. The centre — one of the largest and most modern in North America — provides tertiary and quaternary care to the immediate population of Montreal and Quebec as a whole, supporting seven clinical missions and offering more than 70 specialty health services.
In the beginning, facilities management’s primary task was to convert patient rooms from neutral or positive pressure to negative pressure. The first requests were, predictably, to switch over the rooms on the intensive care units. At MUHC’s Glen site, things ramped up quickly — an entire wing was converted in less than a week.
MUHC’s emergency measures coordination centre (CCMU), a decision-making body comprised of infection control and clinical and administrative leadership, was responsible for establishing facilities management’s priorities. Working with the Ministry of Health, they assessed the province’s ever-evolving needs and how best to share the workload across the network.
Next, facilities management received requests to convert L es choses ont commencé à changer dans la deuxième semaine de mars. Dans tout le pays, les écoles ont fermé leurs portes aux élèves et les employeurs ont envoyé leurs employés travailler à partir de la maison. Alors que les rues des villes devenaient étrangement silencieuses en raison des directives de confinement, les hôpitaux de tout le pays étaient bousculés par l’agitation du personnel qui se préparait à un afflux de patients infectés par la COVID-19.
Au Québec, l’équipe de gestion des installations du Centre universitaire de santé McGill (CUSM) s’apprêtait à passer en vitesse supérieure. Le CUSM est un réseau universitaire de santé bilingue réparti dans quatre hôpitaux. Le centre, l’un des plus grands et des plus modernes en Amérique du Nord, fournit des soins tertiaires et quaternaires à la population de Montréal et de l’ensemble du Québec. Il soutient sept missions cliniques et offre plus de 70 services de santé spécialisés.
Au début, la tâche principale de la gestion des installations a consisté à convertir les chambres des patients d’une pression neutre ou positive à la pression négative. Les premières demandes ont été, comme on pouvait s’y attendre, de transformer les chambres des unités de soins intensifs. Au site Glen du CUSM, les choses se sont accélérées : on a transformé une aile entière en moins d’une semaine.
Le Centre de coordination des mesures d’urgence (CCMU) du CUSM, un organe décisionnel composé de responsables du contrôle des infections et de membres des directions clinique et administrative, a été chargé d’établir les priorités dans la gestion
regular inpatient rooms to negative pressure. These were designated for COVID-19 patients who were sick enough to be hospitalized but not in need of a ventilator. Ultimately, MUHC needed many more of these than ICU rooms; however, that reality didn’t reveal itself until several weeks into COVID-19’s arrival in Montreal.
Despite being a world-class facility, it was not simple to convert spaces at the Glen site. While some modifications were achievable by modulating exhaust and supply dampers, other solutions involved installing plastic barriers with zipper openings and portable high efficiency particular air (HEPA) filtration units. In all cases, room conversions required finetuning of dampers or fans, as well as manual measuring to ensure appropriate room conditions were met (like differential pressure and exhaust f low rate) since the necessary instrumentation was not already in place.
During these unprecedented times, priority has been given to form over function. Because of the time sensitive nature of requests, sometimes, while achieving the desired environmental conditions, solutions have had a less than ideal effect on the users. In certain cases, clinicians still have to open zippers or roll-up plastic when they need to reach patients. In order to minimize these inconveniences, each modification is carefully planned in collaboration and coordination with facilities management and the affected clinical teams, including nurses and doctors on the affected floors.
The older infrastructure of MUHC’s Montreal General Hospital (MGH), Lachine Hospital and Montreal Neurological Institute and Hospital required a different type of intervention. In most instances, to convert a room to negative pressure, the team had to remove a window to exhaust a portable HEPA filtration unit to the outside. Some windows had been in place, untouched, for several decades. Despite the extra labour, MGH’s facilities management team managed to convert 23 ICU rooms to negative pressure in a week and a half, taking a whole floor to 26 COVID-19-ready rooms from just three.
As time marched on, one ICU floor per hospital was deemed insufficient to support the potential influx of COVID-19 patients. The CCMU directed facilities management to begin work on des installations. En collaboration avec le ministère de la Santé, il a évalué les besoins en constante évolution de la province et la meilleure façon de répartir la charge de travail au sein du réseau.
Ensuite, la direction des installations a reçu des demandes de transformation de chambres d’hospitalisation ordinaires en chambres à pression négative. Celles-ci étaient destinées aux patients COVID-19 qui étaient suffisamment malades pour être hospitalisés, mais qui n’avaient pas besoin d’un ventilateur. Au final, le CUSM a eu besoin de beaucoup plus de ce type de chambres que de chambres en soins intensifs, mais cette réalité ne s’est révélée que plusieurs semaines après l’arrivée de la COVID-19 à Montréal.
Bien que le site Glen soit une installation de classe mondiale, la transformation de ses espaces n’a pas été facile. Si certaines modifications ont pu être apportées en modulant les volets d’évacuation et d’alimentation, on a aussi eu recours à d’autres solutions, comme l’installation de barrières en plastique avec des ouvertures à fermeture éclair et d’unités portatives de filtration d’air à haute efficacité (HEPA). Dans tous les cas, la transformation des chambres a nécessité un réglage précis des volets ou des aérateurs, ainsi que la prise manuelle de mesures pour s’assurer que chaque chambre remplissait les conditions appropriées (comme la pression différentielle et le débit d’expulsion), puisque l’instrumentation nécessaire n’était pas encore en place.
En ces temps sans précédent, la priorité a été donnée à la forme plutôt qu’à la fonction. En raison du caractère urgent des demandes, il est arrivé que, tout en permettant d’atteindre les conditions environnementales souhaitées, les solutions n’aient pas eu un effet idéal sur les utilisateurs. Dans certains cas, les cliniciens doivent encore ouvrir une fermeture éclair ou rouler du plastique pour atteindre un patient. Afin de réduire ces inconvénients au minimum, chaque modification est soigneusement planifiée en collaboration et en coordination avec la gestion des installations et les équipes cliniques concernées, y compris les infirmières et les médecins des étages concernés.
L’ancienne infrastructure de l’Hôpital général de Montréal (HGM) du CUSM, de l’Hôpital de Lachine et de l’Institut et hôpital neurologique de Montréal réclamait un autre type d’intervention. Dans la plupart des cas, pour transformer une


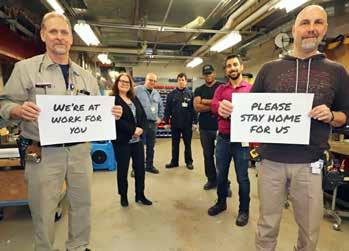
t TOP TO BOTTOM: Desks with Plexiglas walls were set up in front entrances for safety reasons. Montreal General Hospital facilities staff share a message to help ‘flatten the curve.’

converting other patient units to negative pressure isolation rooms. This caused cascades of patients to be relocated to other units. In every case, a feasibility study had to be done to ensure the new space could support all necessary care activities, including ventilation, medical gasses and electrical capacity. Before patients could be transferred to the new area, day-to-day equipment had to be installed, too, which included everything from call bells to macerators and even new curtains.
Simultaneously, facilities management was responsible for a flurry of other tasks aimed at reducing the risk of transmission within the four hospitals. Teams were busy removing half of all tables and chairs, as well as any magazine and pamphlet displays from public areas; and installing hundreds of additional hand sanitizer stations, hands-free sinks and Plexiglas walls in entrances, reception areas and around food service cashier stations. They also helped set up signage to encourage physical distancing, including reminders about MUHC’s new elevator, stair and water fountain etiquette.
In concert, permanent and temporary partitions or separating walls made of drywall, Plexiglas and even curtains were installed in various clinical areas, including dialysis and emergency department waiting rooms. Teams also installed windows in more than 50 patient room doors at MGH and the Glen site so medical staff could observe patients without entering the room in full personal protective equipment. On top of that, facilities management managed the installation of three COVID-19 screening tents and a resuscitation tent for non-COVID patients outside MGH’s trauma/ambulance bay. pièce en pression négative, l’équipe a dû enlever une fenêtre pour évacuer l’air d’une unité portative de filtration HEPA. Certaines de ces fenêtres étaient en place, intactes, depuis des dizaines d’années. Malgré le surcroît de travail, l’équipe de gestion des installations de l’HGM a réussi à transformer 23 chambres en soins intensifs en une semaine et demie, faisant passer un étage entier de trois à 26 chambres prêtes pour la COVID-19.
Éventuellement, on a jugé qu’il ne suffisait pas d’avoir un étage d’unité des soins intensifs par hôpital pour accueillir l’afflux potentiel de patients COVID-19. Le CCMU a demandé à la direction des installations de commencer la transformation d’autres unités de patients en chambres d’isolement à pression négative. Cela a entraîné une cascade de déplacements de patients vers d’autres unités. Dans tous les cas, il a fallu réaliser une étude de faisabilité pour s’assurer que le nouvel espace pourrait accueillir toutes les activités de soins nécessaires, y compris la ventilation, les gaz médicaux et la capacité électrique. Avant que les patients puissent être transférés dans la nouvelle zone, il a fallu également installer des équipements de base, comme des sonnettes d’appel, des broyeurs et même des rideaux.
Simultanément, la direction des installations était chargée d’une foule d’autres tâches visant à réduire le risque de transmission au sein des quatre hôpitaux. Les équipes ont dû retirer la moitié des tables et des chaises, ainsi que tous les présentoirs de magazines et de brochures des aires publiques, puis installer des centaines de postes de désinfection des mains, d’éviers sans contact et de murs en plexiglas dans les entrées, les aires de réception et autour des caisses des services de restauration. En outre, elles ont contribué à la mise en place d’une signalétique encourageant la distanciation, notamment en rappelant les nouvelles règles concernant les ascenseurs, les escaliers et les fontaines.
On a installé dans diverses zones cliniques des cloisons permanentes et temporaires ou des murs de séparation en placoplâtre, en plexiglas et même en rideaux, notamment dans les salles de dialyse et d’attente des services d’urgence. Les équipes ont également installé des fenêtres dans plus de 50 portes de chambres de patients à l’HGM et au site Glen, pour permettre au personnel médical d’observer les patients sans devoir pénétrer dans la chambre avec un équipement de protection individuelle complet. De plus, la direction des installations a géré l’installation de trois tentes de dépistage de la COVID-19 et d’une tente de réanimation pour les patients non infectés par la COVID, le tout à l’extérieur de la zone trauma/ambulance de l’HGM.
Dans une deuxième vague de demandes du CCMU, on a confié à la direction des installations la transformation en pression négative de diverses salles afin de répondre à tous les besoins potentiels des patients COVID-19 attendus. Parmi les espaces ainsi convertis (à l’aide d’un système d’aide à l’étanchéité en pression négative placé devant les portes des salles à pression
In a second wave of requests from the CCMU, facilities management was asked to switch over various procedure rooms to negative pressure in order to attend to all potential needs of incoming COVID-19 patients. Operating rooms, dentistry suites and interventional imaging were among those converted by introducing a negative pressure seal assist system in front of the doors of the positive pressure procedure rooms.
With the introduction of various procedure rooms, how to safely transport a COVID-19 patient through the hospital soon became a preoccupation. Following clinical directives established by the CCMU, MUHC identified specific elevators at each hospital for COVID-19 patient transport. In order to reduce the risk of contamination and minimize downtime for cleaning, facilities management installed portable HEPA filtration units inside each elevator.
After several months of working long days, evenings and weekends, facilities management has helped MUHC attain a certain level of operation. However, things continue to evolve. As the province plans for a slow ramp up to more regular day-to-day volumes and operations, establishing clear hot and cold patient zones is becoming increasingly important. It remains to be seen what the future holds for COVID-19 and MUHC, but what is clear is many of these ‘temporary’ modifications will likely become permanent.
Rebecca Burns is responsible for the environmental dossier within the technical services directorate at McGill University Health Centre (MUHC). This article was written in collaboration with Steven Yamamoto, associate director of technical services at MUHC, and Justin Ciampini and Mohamed Merheb, facility managers at MUHC’s Glen site and Montreal General Hospital, respectively.
positive), mentionnons des salles d’opération, de dentisterie et d’imagerie interventionnelle.
Maintenant qu’on disposait de ces types de salles, il fallait cette fois concevoir un protocole de transport des patients COVID-19 à travers l’hôpital. En suivant les directives cliniques établies par le CCMU, le CUSM a identifié, dans chaque hôpital, certains ascenseurs pour le transport de ces patients. Afin de réduire le risque de contamination et les temps d’arrêt pour le nettoyage, la direction des installations a mis en place des unités portatives de filtration HEPA dans chaque ascenseur.
Après plusieurs mois de longues journées (et soirées et fins de semaine) de travail, la direction des installations a permis au CUSM d’atteindre un certain niveau de fonctionnement. Or, les choses continuent d’évoluer. Le gouvernement provincial prévoyant un retour très graduel aux activités et aux volumes normaux, il devient de plus en plus important d’établir des zones chaudes et froides bien claires. Il reste à voir ce que l’avenir réserve à la COVID-19 et au CUSM, mais on sait d’ores et déjà que nombre de ces modifications ‘temporaires’ risquent de devenir permanentes.
Rebecca Burns est responsable du dossier environnemental au sein de la direction des services techniques du Centre universitaire de santé McGill (CUSM). Cet article a été rédigé en collaboration avec Steven Yamamoto, directeur adjoint des services techniques du CUSM, et Justin Ciampini et Mohamed Merheb, gestionnaires des installations du site Glen et de l’Hôpital général de Montréal (respectivement) du CUSM.


What’s your outbreak protocol?
Communicable diseases cause a significant burden on society 1 and the widespread outbreak of COVID-19 has brought a harsh reality for both healthcare and non-healthcare facilities alike. This respiratory disease, caused by a coronavirus, SARS-CoV-2, is a reminder of the importance of infection prevention efforts and the need for continued vigilance. 2
In the current COVID-19 pandemic, there have been numerous incidents of infection outbreaks at different types of non-healthcare facilities, such as large warehouses, food plants, meat manufacturing plants, grocery stores, etc. 3
As public facilities and business open in a phased manner after the unprecedented lockdown and closure due to COVID-19, it is imperative that cleaning, disinfection and infection prevention and control measures are undertaken and adhered to in order to prevent additional outbreaks. 2
Educate.
COVID-19 has also highlighted the importance of infection control and prevention education for facility managers, custodians and professional cleaners to ensure facilities/businesses are cleaned and disinfected properly to help prevent the spread of illness causing germs and protect human health. 4,5
Everything from hand hygiene to wearing masks to personal protective equipment, to choosing the correct product for each cleaning job, to knowing the proper process to implement, and execute environmental disinfection, all play a vital role in helping prevent the spread of communicable infections. 4
Be “healthcare clean”. “Healthcare clean”, an approach to cleaning that aims to reduce or eliminate microbial contamination of all hard surfaces and non-critical equipment within the healthcare environment, may also be applied to non-healthcare settings, such as schools, offices, retail, hospitality, warehouses, fitness facilities, grocery stores, shopping centres, etc. 6
Similar to practices implemented during normal flu seasons, it is important to ensure routine cleaning is being done when trying to stop the spread of mass communicable infections such as COVID-19. 7
Surveys show that nearly all employees (86%) agree that disinfecting hard surfaces is one of the best ways to prevent germ transmission, and employers should make available and provide hand sanitizers and disinfecting wipes at employee workstations. 8
Plan to prevent.
Toronto Public Health has issued a COVID-19 factsheet for non-healthcare workplaces that recommends frequent cleaning and disinfecting of common areas and high-touch surfaces such as door handles, counters, cabinet doors, elevator buttons, light switches, faucets, toilet handles, hand rails, touch screen surfaces and keypads. Common areas should have soap, hand sanitizer and disinfectant. 9
In addition, the Ontario Ministry of Labour, Training and Skills Development, has issued comprehensive guidelines for various sectors of industry to help protect workers, customers and the general public from COVID-19: 4,10
• Adherence to infection prevention and control (IPAC) protocols; • Hand hygiene, including the use of alcohol-based hand rub and hand washing; • Assessment of the risk of infection transmission and the appropriate use of personal protective equipment, including correct selection, safe application, removal and disposal; • Disinfect all frequently touched surfaces daily including desks, cubbies, cafeteria tables, restroom stalls/stall doors, door handles, keyboards/mice, pencil sharpeners and sink fixtures; • Disinfect after routine cleaning is complete; • Remove any visible soil from the surface with a detergent-based cleaner before applying a disinfectant; • Disinfect surfaces from “clean” areas, such as classrooms, to “dirty” areas, such as restrooms, to minimize crosscontamination; • When disinfecting, ensure surfaces remain visibly wet for the contact time specified on the product label.
CloroxPro™ can help.
The rapidly evolving situation with COVID-19 has triggered Public Health Agency of Canada’s (PHAC) Emerging Pathogen Policy*. This policy permits manufacturers of disinfectants to make efficacy claims for its disinfectants against the emerging viral pathogen if: • The disinfectant has a Broad Spectrum Virucidal efficacy claim, meaning that it has a claim against anyone of the following four viruses approved by Health Canada: Poliovirus type 1, Chat strain (ATCC VR-1562) or Human adenovirus type 5 (ATCC VR-5) or Bovine parvovirus (ATCC VR-767) or Canine parvovirus (ATCC VR-2017) • Or, carry a specific claim against a specific coronavirus, such as MERS-CoV, SARS-CoV or human coronavirus strain 229E • Or, carry a specific claim against non-enveloped viruses of the picornaviridae, caliciviridae, astroviridae, reoviridae, or papillomaviridae families The following CloroxPro™ products are on Health Canada’s list of hard-surface disinfectants with evidence against COVID-19: • Clorox Total T360® Disinfectant Cleaner, DIN 02460769 • Clorox® Germicidal Bleach, DIN 02459108 • Clorox® Disinfecting Wipes, DIN 02492636 • Clorox® Clean-Up® Disinfecting Bleach Cleaner, DIN 02494019 • Clorox Healthcare® Germicidal Disinfecting Cleaner, DIN 02469278 • Clorox Healthcare® Bleach Germicidal Wipes, DIN 02465671 • Clorox Healthcare® Fuzion™ Cleaner Disinfectant, DIN 02459744 • Clorox Healthcare® Hydrogen Peroxide Cleaner Disinfectant,
DIN 02403528 • Clorox Healthcare® Hydrogen Peroxide Cleaner Disinfectant
Wipes, DIN 02406225 • Clorox Healthcare® VersaSure™ Alcohol-Free Cleaner
Disinfectant Wipes, DIN 02473151
* https://www.canada.ca/en/health-canada/services/drugs-health-products/disinfectants/covid-19/list.html References: 1. Diener A & Dugas J. Inequality-related economic burden of communicable diseases in Canada. Can Commun Dis Rep Suppl 2016;42:S1-S7. 2. Ontario Agency for Health Protection and Promotion (Public Health Ontario), Provincial Infectious Diseases Advisory Committee. Best practices for prevention, surveillance and infection control management of novel respiratory infections in all health care settings. 1 st revision. Toronto, ON: Queen’s Printer for Ontario; 2020. 3. These are the Calgary-area workplaces hit hardest by COVID-19 outbreaks. https://www.cbc.ca/news/canada/calgary/covid-list-workplace-outbreaksahs-calgary-asfd-1.5564639. Accessed May 11, 2020. 4. Resources to prevent COVID-19 in the workplace. May 8, 2020. https://www.ontario.ca/page/resources-prevent-covid-19-workplace. Accessed May 10, 2020. 5. COVID-19 Standard Operating Procedure – Disinfection of Touchpoints. https://www.ccohs.ca/images/products/pandemiccovid19/pdf/std-op-proc-disinfection.pdf. Accessed May 10, 2020. 6. Gauthier J. “Hospital clean” versus “construction clean” – is there a difference? Can J Infect Control 2004;19(3):150-2. 7. Cold and Flu Season. https://www.wsps.ca/Information-Resources/Topics/Cold-and-Flu-Season.aspx. Accessed May 10, 2020. 8. Clorox Professional Products Company Survey. May 2015. 9. Toronto Public Health Covid-19 Fact Sheet. https://www.toronto.ca/wp-content/uploads/2020/02/8d59-Fact-Sheet_NovelCoronavirus.pdf. Accessed May 10, 2020. 10. Ontario Agency for Health Protection and Promotion (Public Health Ontario), Provincial Infectious Diseases Advisory Committee. Best practices for environmental cleaning for prevention and control of infections in all health care settings. 3 rd ed. Toronto, ON: Queen’s Printer for Ontario; 2018.







