Interventional Radiology
Uterine Fibroid Embolisation: the Past, the Present, and the Future The past Uterine fibroids are estimated to be present in up to 75 per cent of women, and cause symptoms in up to 35 per cent. Patients with small fibroids or with mild symptoms may be suitable for conservative treatment options. For women with large fibroids or who have failed conservative treatment, a more definitive approach is needed [1]. Fibroid embolisation (UFE) was first described in 1974 by interventional radiologist Jean-Jacques Merland. It became a mainstream treatment option following a landmark paper in The Lancet in 1995, followed on by the REST and EMMY trials in the early 2000s [1]. High-level evidence now shows us that fibroid embolisation performed by interventional radiologists (IRs), provides women with similar improvement in quality of life at up to 10 years after embolisation compared with traditional surgical treatments, including hysterectomy and myomectomy [1]. In 2006, the Medical Services Advisory Committee (MSAC) compared the efficacy, cost, and safety of UFE. They recommend public funding of embolisation (MBS item 35410), however placed a condition that referrals should come from a gynaecologist in order for Medicare to provide the rebate [2].
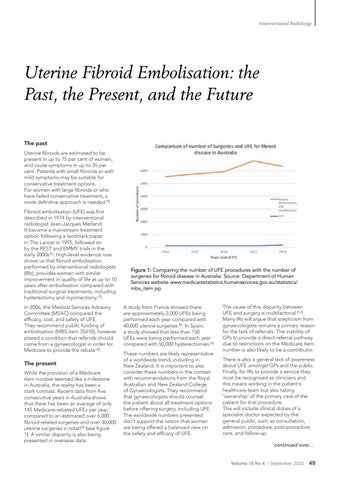
The present While the provision of a Medicare item number seemed like a milestone in Australia, the reality has been a stark contrast. Recent data from five consecutive years in Australia shows that there has been an average of only 145 Medicare-rebated UFEs per year, compared to an estimated over 6,000 fibroid-related surgeries and over 30,000 uterine surgeries in total![1] (see figure 1). A similar disparity is also being presented in overseas data.
Figure 1: Comparing the number of UFE procedures with the number of surgeries for fibroid disease in Australia. Source: Department of Human Services website www.medicarestatistics.humanservices.gov.au/statistics/ mbs_item.jsp A study from France showed there are approximately 2,000 UFEs being performed each year compared with 40,000 uterine surgeries [3]. In Spain, a study showed that less than 150 UFEs were being performed each year compared with 50,000 hysterectomies [3]. These numbers are likely representative of a worldwide trend, including in New Zealand. It is important to also consider these numbers in the context with recommendations from the Royal Australian and New Zealand College of Gynaecologists. They recommend that gynaecologists should counsel the patient about all treatment options before offering surgery, including UFE. The worldwide numbers presented don't support the notion that women are being offered a balanced view on the safety and efficacy of UFE.
The cause of this disparity between UFE and surgery is multifactorial [1,3]. Many IRs will argue that scepticism from gynaecologists remains a primary reason for the lack of referrals. The inability of GPs to provide a direct referral pathway due to restrictions on the Medicare item number is also likely to be a contributor. There is also a general lack of awareness about UFE amongst GPs and the public. Finally, for IRs to provide a service they must be recognised as clinicians and this means working in the patient's healthcare team but also taking 'ownership' of the primary care of the patient for that procedure. This will include clinical duties of a specialist doctor expected by the general public, such as consultation, admission, procedure, post-procedure care, and follow-up. continued over... Volume 16 No 4 I September 2020
49