4 minute read
Unloading in a Paediatric Population: A Panel Discussion
ensured open communication, keeping the group informed and efficient. The framework for all animal testing and clinical testing must be agreed upon by the group. Honest bidirectional feedback and criticism help to stress test concepts and produce the best ideas. The FDA is considered a third partner in this team, providing key insight on how to propel mechanical support devices into the clinic.
Impella’s unique position within the patient’s circulation, specifically within the heart, provides local, regional and systemic circulatory feedback. Future directions include the use of non-intuitive advanced metrics to assist support timing and elucidating mechanical support device-to-device interactions, such as Impella with extracorporeal membrane oxygenation.
Advertisement
Industry and academic collaboration are the hallmarks of great medical interventions, including antibiotics, genomics and medical devices. The amalgamation of academic ideas and industrial engineering enables innovation from bench to bedside.
Dr Vivian Dimas is Medical Director of the Adult Congenital Heart Disease Program at Medical City Dallas in the Heart and Spine Hospital. Panel attendees included Dr Sebastian Tume, Assistant Professor of Pediatric Critical Care at Baylor College of Medicine and Director of Cardiac ICU at Texas Children’s Hospital; Dr Iki Adachi, Associate Professor of Congenital Heart Surgery at Baylor College of Medicine and Co-Director of the Mechanical Circulatory Support Program at Texas Children’s Hospital; Dr Brian Morray, Pediatric Interventional Cardiologist and Associate Professor of Pediatrics at the University of Washington School of Medicine at Seattle Children’s Hospital; Dr Athar Qureshi, Professor of Pediatrics at Baylor College of Medicine and Medical Director of the Catheter Lab at Texas Children’s Hospital; Dr Christina J Vanderpluym, Co-director of the Stroke and Cerebral Vascular Center and Medical Director of Cardiac Antithrombosis Management and Monitoring Program at Boston Children’s Hospital, as well as Assistant Professor of Pediatrics at Harvard Medical School; and Dr Ryan Davies, Associate Professor of Cardiovascular Thoracic Surgery at UT Southwestern and Surgical Director for Heart Transplantation and Mechanical Circulatory Support at Children’s Hospital Dallas.
The aetiology of paediatric acute cardiogenic shock (CS) varies more than that in adults, and may include coronary artery disease, myocarditis, congenital heart disease, cardiomyopathy, diastolic heart failure and systolic heart failure. Unlike in adults, ischaemic coronary artery disease is not a common CS aetiology in children. Paediatric CS patients often possess a single ventricle, or have undergone a Fontan procedure or biventricular repair. Treatment options are limited by smaller patient size, reduced ventricular dimensions and lack of mechanical support devices approved for use in children. Percutaneous circulatory support options, such as balloon pumps, may enable haemodynamic support for adults, but are often more harmful in children.
Left ventricular (LV) unloading is necessary to decrease ventricular size and pressure in paediatric CS patients. The standard LV unloading approach at many centres is static balloon atrial dilation of the septum, balloon atrial septostomy, stenting the atrial septum or left atrial venting with extracorporeal membrane oxygenation (ECMO) support. ECMO is often used due to ease of access and rapid oxygenation of the blood; however, lack of optimal coronary reperfusion compromises long-term patient recovery. After ECMO placement, immediate echocardiogram imaging to assess canula position and ventricular ejection status can help determine whether additional LV unloading is required. The panellists recommend additional haemodynamic support modalities, such as the Impella transvalvular pump, to achieve LV unloading. The panellists discussed specific patients, in which the Impella 5.5, used in combination with ECMO, improved recovery in ischaemic CS patients by decreasing LV end-diastolic pressure. The Impella device provides greater ease of placement, acute decompression and a bridge to weaning the patient off ECMO, reducing ECMO-associated morbidity. Discussion also focused on the utilisation of LV unloading, followed by right ventricular support prior to resorting to ECMO in paediatric CS patients. Dr Adachi and Dr Morray further discussed using Impella-mediated LV unloading for singleventricle paediatric CS patients with failed Fontan circulation, as it decreases central venous pressure, improves cardiac output and increases survival.
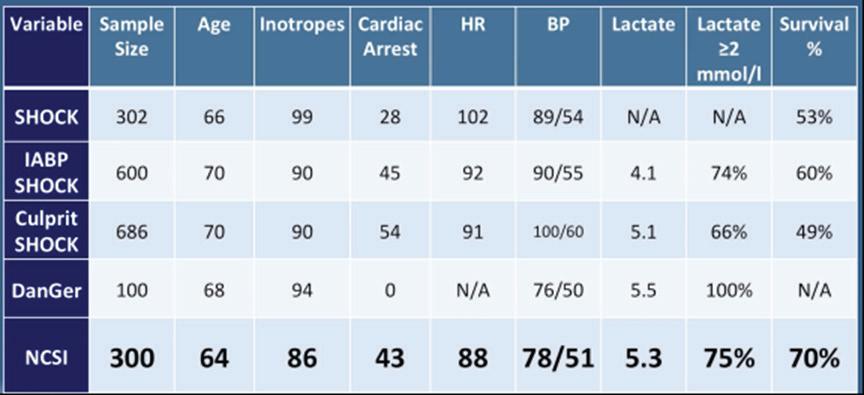
A multidisciplinary approach to assess paediatric CS patients ensures selection of the least invasive and most effective surgical techniques and LV unloading method. Determination of CS aetiology by monitoring the (lack of) response to therapies, biventricular dysfunction, chronicity of heart failure and lactate levels can assist with appropriate device selection. Vascular access techniques, such as hybrid access and trans-cable access, together with reduced sheath and catheter size, can decrease surgical complications. Timing of placement and removal of mechanical support devices should be optimised. Physician collaboration with industry partners is critical to driving development of paediatric-specific mechanical unloading devices.
Moderated by Vivian Dimas, MD1 Presented by Sebastian Tume, MD,2,3 Iki Adachi, MD,2 Brian Morray, MD,4 Athar Qureshi, MD,2,3 Christina J VanderPluym, MD5 and Ryan Davies, MD6
1. Medical City Children’s Hospital/Medical City Heart and Spine Hospital, Dallas, TX, US; 2. Baylor College of Medicine, Houston, TX, US; 3. Texas Children’s Hospital, Houston, TX, US; 4. University of Washington School of Medicine Seattle, WA, US; 5. Harvard Medical School, Boston, MA, US; 6. UT Southwestern Dallas, TX, US