









Follow and interact with us on Twitter: @HealthBusiness_











Follow and interact with us on Twitter: @HealthBusiness_

With NHS pressures regularly in the headlines, many were surprised that former health secretary, current chancellor Jeremy Hunt did not announce any major funding packages for the NHS in his spring budget.
Meanwhile, Health Education England has joined NHS Digital and officially merged with NHS England, creating one single organisation to run the NHS. The new organisation will eventually be smaller than its three former branches.
This issue of Health Business magazine investigates how technology can be used to cut waiting times, reduce health inequalities and improve learning resources.
We look out how agencies can be used to help with staffing pressures and how apprenticeships are benefitting an NHS trust in Kent.
This year marks 75 years of the NHS, with large celebration planned both inside and outside of the NHS. There are many ways to join in the celebration and Health Business will be getting involved too. Look out for the next issue of HB which will be an NHS 75th anniversary special.
Polly Jones, editor
To register for your FREE Digital Subscription of Health Business magazine, go to www.healthbusinessuk.net/digital-subscription or contact Public Sector Information, 226 High Road, Loughton, Essex IG10 1ET. Tel: 020 8532 0055 www.healthbusinessuk.net
PUBLISHED BY PUBLIC SECTOR INFORMATION LIMITED
226 High Rd, Loughton, Essex IG10 1ET. Tel: 020 8532 0055 Web: www.psi-media.co.uk
EDITOR Polly Jones PRODUCTION MANAGER/DESIGNER Dan Kanolik PRODUCTION DESIGNER Jo Golding PRODUCTION CONTROL Deimante Gecionyte
ADMINISTRATION Enkelejda Lleshaj WEBSITE PRODUCTION Freya Courtney ADVERTISEMENT SALES Lauren McGowan, Azad Miah, Maziar Movassagh
PUBLISHER Damian Emmins GROUP PUBLISHER Karen Hopps
© 2023 Public Sector Information Limited. No part of this publication can be reproduced, stored in a retrieval system or transmitted in any form or by any other means (electronic, mechanical, photocopying, recording or otherwise) without the prior written permission of the publisher. Whilst every care has been taken to ensure the accuracy of the editorial content the publisher cannot be held responsible for errors or omissions. The views expressed are not necessarily those of the publisher.ISSN 1478-7687
Health Business is a member of the Independent Press Standards Organisation (which regulates the UK’s magazine and newspaper industry). We abide by the Editors’ Code of Practice and are committed to upholding the highest standards of journalism. If you think that we have not met those standards and want to make a complaint please contact Polly Jones or Angela Pisanu on 0208 532 0055. If we are unable to resolve your complaint, or if you would like more information about IPSO or the Editors’ Code, contact IPSO on 0300 123 2220 or visit www.ipso.co.uk









07 News
Health Education England merges with NHS England; NHS public satisfaction at record low; and Virtual wards treat 100,000 in a year
Marie Loizides, associate director of performance analytics at Barking, Havering, and Redbridge University Hospitals NHS Trust explains how switching to digital referrals has slashed patient waiting times

A recent report by Public Policy Projects has said that ICSs need to use digital innovation in order to reduce health inequalities. HB picks out some key points from the report
A new 3D anatomy teaching tool has been launched which will feature the most expansive skin tone library ever available in global health education. Health Business spoke to some of those involved in the project
Chris Dimitriadis, chief global strategy officer at ISACA (Information Systems Audit and Control Association) on how public sector organisations can protect themselves from cyber threats

Following his appearance at the Digital Health Rewired conference in March, Professor Ben Goldacre explains why information governance is not enough when it comes to protecting privacy

Stockport NHS Foundation Trust’s Green Plan has been officially ratified at the trust’s most recent board meeting

NHS Providers recently published a report entitled: “No more sticking plasters: repairing and transforming the NHS estate”. HB investigates
We are more aware of infection control than ever before. Covid, flu, mpox, though below their peak, are still around and we can’t get complacent. Here are some top tips for infection control in your building

The Security Event (TSE), the UK’s no.1 award-winning commercial, enterprise and domestic security event returns to the NEC Birmingham on 25-27 April 2023. This year’s event is set to bring even more exclusive products and launches of the latest security products and solutions from some of the biggest and best names in the security industry
The NHS must embrace the agency workforce. During this staffing crisis, recruitment agencies and temps are playing a crucial role in keeping wards open and the wheels of the NHS turning, writes Yerin Seo, senior campaigns advisor at the Recruitment and Employment Confederation
With health sector vacancies at a record high, one NHS trust in Kent is battling back by offering more than 300 fully-paid apprenticeships, from nursing to administrators
Designed with infection control in mind, Vepps Hygen is fully HBN 00-10 Part C compliant. A rigid and stable system, Vepps Hygen is impervious to water and easy to clean and maintain. Its seamless design, manufactured from one piece of Solid Grade Laminate (SGL), has flush-fitting hinges and lockable access doors that minimise dirt traps. It’s a simple, easy-click wall system with concealed fixing channels for a quick yet sturdy, longlasting installation. From basins and WCs to scrub-up troughs and showers, we’re proud to now offer more than 120 variations as well as multi-panel units to choose from when writing your healthcare specifications.
Get in touch for advice and guidance on specifying Vepps Hygen for your healthcare project.


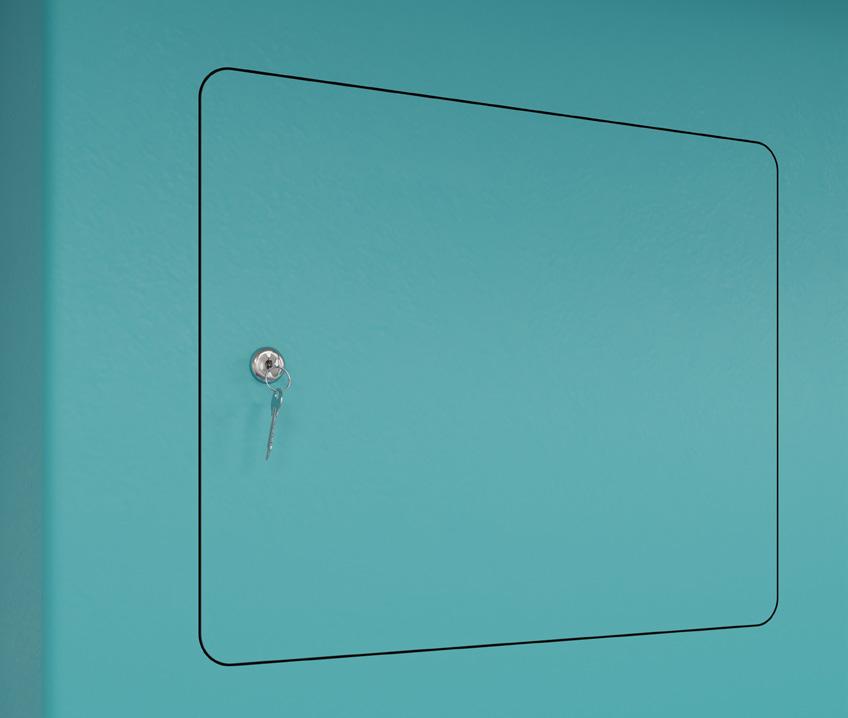

 Ross Houghton, Healthcare Business Development Manager ross.houghton@venesta.co.uk
Ross Houghton, Healthcare Business Development Manager ross.houghton@venesta.co.uk




role in improving the quality of health and care services and growing the number of staff working in the NHS over the last decade.
The transfer will see NHS England take over responsibility for all activities previously undertaken by Health Education England, including planning, recruiting, educating and training the health workforce, and ensuring it has the right numbers, skills, values and behaviours in place to support the delivery of excellent healthcare to patients and the public.
“Our colleagues from Health Education England bring a wealth of experience, knowledge and expertise, which will be invaluable in our aim to help the NHS improve the health and care of the people it serves.”
Dr Navina Evans, chief workforce, training and education officer at NHS England, said: “I want to thank every single one of my former Health Education England colleagues and partners for their contribution.
NHS England and Health Education England have legally merged, creating a new single organisation to lead the NHS in England.
The news follows the merger of NHS Digital and NHS England on 1 February. Now, the NHS’s people, skills, digital, data and technology expertise have been brought together into one national organisation to deliver high-quality services for everyone in England.

Health Education England was the body responsible for the education and training of the health workforce and has played a critical

It is expected that, by the end of 2023/24, the new organisation will be between 30-40 per cent smaller than the current combined size of NHS England, Health Education England and NHS Digital.
NHS England’s chief executive, Amanda Pritchard, said: “Today marks a major milestone as we come together as one single organisation. This puts workforce, data, digital and technology at the heart of our plans to transform the NHS, enabling better, more joined-up decision-making at system, regional and national levels, and more effective and efficient use of our resources.
Chancellor Jeremy Hunt has unveiled his budget, with no major announcements for the NHS.

Hunt claimed that this was a budget for growth and that long-term, sustainable and healthy growth pays for the NHS.
The budget included plans to make the UK a more exciting place to invest and speed up access for NHS patients to get new drugs.
On NHS pensions, the budget includes changes that will stop over 80 per cent of NHS doctors from receiving a tax charge. Pensions annual tax-free allowance will increase from £40,000 to £60,000 and the Lifetime Allowance will be abolished.
Hunt also said that the NHS workforce plan that was promised in the Autumn Statement will be published shortly.
Hunt also claimed that: “High inflation is the root cause of the strikes we have seen in recent months.”
READ MORE
“There remains so much to do, so now is the time to build on the achievements of Health Education England, NHS Digital and NHS England. Bringing together the three organisations allows us to align service, workforce, and financial planning and delivery. A united approach to improving service, embedding new technology and ensuring the workforce has the skills and numbers to deliver improvements is a huge opportunity for the NHS, one we intend to take together.”
The British Social Attitudes survey has revealed that public satisfaction with the NHS has reached the lowest level ever recorded.
Only 29 per cent of people said they were satisfied with the NHS in 2022 – seven percentage points lower than last year.
In 2010, satisfaction was at 70 per cent.
51 per cent of respondents were dissatisfied with the NHS, which is the highest proportion since the survey began.
The main reason people gave for being dissatisfied with the NHS was waiting times for GP and hospital appointments (69 per cent), this was followed by staff shortages (55 per cent) and a view that the government does not spend enough money on the NHS (50 per cent).
Those who were satisfied with the NHS cited that NHS care is free at the point of use (74 per cent), the quality of NHS care (55 per cent) and that it has a good range of services and treatments available (49 per cent).
Responding to the results, an NHS spokesperson said: “While this survey reflects the public’s perceptions of the significant pressure on our services, it is clear the overwhelming majority still very firmly value the fundamental principles of the NHS – which is welcome as we head towards the NHS’ 75th birthday.

“Importantly, even with more people accessing our services than ever before, it also shows strong satisfaction with the range of services and the quality of care patients receive, which is a testament to our hardworking, dedicated staff working across all corners of the NHS.
“However, there is no doubt that the NHS has been under sustained pressure in recent months which has impacted the experiences of patients – at the time this survey was carried out, staff had just treated more people with Covid-19 in hospital over the summer than the past two combined, GPs were delivering millions more appointments each month compared to before the pandemic, and it was the busiest October ever for A&E attendances and the most serious ambulance call-outs.
“The NHS is taking significant steps to further improve patient experience, including our recently-launched blueprint to recover urgent and emergency care alongside continuing to slash the long waits for elective treatment which inevitably built up during the pandemic, and we are working on new plans to boost primary care for patients as well as publishing a long-term workforce strategy shortly.”




Available in hard copy or app format: The
New product for 2023: Co-ParentPad for LGBTQ+ non-birthing parents


Follow us on:

@dadpaduk
For more information on DadPad: www.thedadpad.co.uk

The government has unveiled a new strategy intended to protect the NHS from cyber attacks.
The Cyber Security Strategy for Health and Adult Social Care lists five ways to build cyber resilience in health and care by 2030.
The intention is to ensure that services are better protected from cyber threats, securing sensitive information and ensure patients are able to continue to access care.
The strategy includes five ways to minimise the risk of cyber attacks and other cyber security issues, and to improve response and recovery following any incidents across health and social care systems. The five pillars include: identifying the areas of the sector where disruption would cause the greatest harm to patients, such as through sensitive
information being leaked or critical services being unable to function; uniting the sector so it can take advantage of its scale and benefit from national resources and expertise, enabling faster responses and minimising disruption and building on the current culture to ensure leaders are engaged and the cyber workforce is grown and recognised, and relevant cyber basics training is offered to the general workforce. The other two pillars are embedding security into the framework of emerging technology to better protect it against cyber threat and supporting every health and care organisation to minimise the impact and recovery time of a cyber incident.
A full implementation plan is set to be published in the summer.
Health minister Lord Markham said: “We’re harnessing the power of technology to deliver better, safer care to people across the country – but at the same time it’s crucial we’re also bolstering the defences of our health and care services.
“This new strategy will be instrumental to ensure every organisation in health and adult social care is set up to meet the challenges of the future.
“This is an important step to ensure we’re building an NHS which is sustainable and fit for the future, with patients at the centre.”
READ MORE
NHS England has launched a consultation on plans to create a single source of healthcare data in England to improve the quality of care for patients.
The consultation is part of the Acute Data Alignment Programme (ADAPt).
The plans would mean that NHS-funded and private healthcare activity data would be available in one place for the first time, in an attempt to provide a more comprehensive insight into the quality of treatment and care across both the NHS and private healthcare settings.
The consultation comes after the Paterson Inquiry, which recommended bringing data on all consultant activity together in the same place. The inquiry followed the conviction of breast cancer surgeon Ian Paterson for performing harmful and unnecessary surgery on
patients across both NHS and private settings.
Pilots have shown that private providers are able to submit admitted patient care data directly to the NHS and that this has a number of benefits, in particular where data on private hospital activity can be linked to information on NHS-funded care. This can provide insights such as the number of emergency readmissions following discharge from a private provider.
The consultation will run until 20 April 2023.
James Austin, director of data strategy and policy at NHS England, said: “NHS data already plays an important role in how we provide high quality patient care and monitor safety reporting systems across the NHS.
“This vision of a single repository of healthcare information, combining NHS and private healthcare, will help provide better insights and lead to improved care and
treatment for all patients across both the NHS and private healthcare sectors.
“Working jointly on the ADAPt programme has enabled us to see the benefits of how this might work. We’d now like to invite healthcare professionals, patient groups and individuals to share their views by responding to the consultation.”
READ MORE



NHS Shared Business Services (NHSSBS) has formally announced the second iteration of its framework agreement, Technology Enabled Care Services 2.

The framework is designed to respond to the need within the NHS and social care sector to free up beds, reduce the backlog of appointments, speed up patient discharge, and reduce the burden on the stretched social care sector.
The framework has been designed with contributions from NHS England (NHSE) Transformation Directorate, local authorities, national technology enabled care (TEC) policy makers like TEC Cymru, as well as industry bodies including the TSA (TEC Services Association).
The announcement comes at a time in which the NHS is grappling with longer
hospital waiting times, hospitals being fuller than pre-pandemic and a discharge crisis.
Virtual wards feature as a key part of the recovery plan. There is a plan to scale up capacity from a current 7,000 virtual ward beds to 10,000 this autumn ready for the winter.
The new framework enables GP Practices, hospitals, health centres and emergency services to procure remote clinical monitoring, intelligent activity monitoring, patient controlled personalised healthcare records and virtual ward solutions which can support health and care professionals to deliver effective and efficient clinical care for patients.
Adam Nickerson, Head of CategoryDigital & IT Procurement Frameworks, at
NHS SBS commented: “The coronavirus pandemic added to waiting lists and the knock-on effects of a lack of beds in the NHS and social care sector. As such, NHSE is looking to deploy virtual ward beds to scale up capacity from 7,000 to 10,000 this autumn, ready for next winter.
“As part of this ambition, ICSs are expected to deliver virtual ward capacity equivalent to 40-50 virtual ward beds per 100,000 people by December 2023, with virtual ward services developed across ICSs and provider collaboratives, rather than individual institutions. In so doing, improving health and integrated care across the health and care system.
READ MORE




What sets us apart from our competition is our dedication and commitment to quality; our innovative quality assurance methodologies provide complete transparency for our clientsproject work can be monitored and checked digitally from any smartphone, tablet, laptop or desktop. Our expert fire stoppers are highly trained and provided with ongoing CPD opportunities such as internal e-learning courses in order to keep knowledge and practice updated according to building regulations and manufacturer specifications.

Taking the #Revolutionforquality to Antarctica!
Click here to read more



The #Revolutionforquality is going global!

There are 340 virtual ward programmes across England, providing 7,653 virtual beds.
Frimley Health provides acute hospital care to patients in their homes, with 83 per cent of patients estimated to avoid hospital admission. 774 people were cared for between July 2022 and January 2023.
just to the people they directly benefit but also in reducing pressure on wider services.”
The Telehealth Team, run by Mersey Care NHS Foundation Trust, supports around 2,000 patients a day with conditions like COPD, diabetes and heart failure.
According to NHS England, more than 100,000 people have been treated in NHS virtual wards in the last year. 16,000 were treated in January alone.
Virtual wards are used to enable patients to get hospital-level care at home, speed up their recovery and free up hospital beds.
NHS national medical director, Professor Sir Stephen Powis, said: “The advantages of virtual wards for both staff and patients have been a real game-changer for the way hospital care is delivered and so it is a huge achievement that more than 100,000 patients have been able to benefit in the last year alone, with the number of beds up by nearly two thirds in less than a year.
“With up to a fifth of emergency hospital admissions estimated to be avoided through better supporting vulnerable patients at home and in the community, these world leading programmes are making a real difference not
The results of the 2022 NHS Staff Survey have been published.
The survey is one of the largest workforce surveys in the world and has been conducted every year since 2003.



The survey asks NHS staff in England about their experiences working for NHS organisations.
Over 1.3 million NHS employees in England were invited to participate in the survey between September and December 2022, with 264 NHS organisations taking part, including all 215 trusts in England. 636,348 staff responded giving a 46 per cent response rate.
86.9 per cent of respondents said that they feel their role makes a difference to patients and 74 per cent that care of patients is their organisation’s top priority.
57.4 per cent of those who responded would recommend their organisation as a place to work.
62.9 per cent said they were happy with the standard of care provided by their organisation, this is compared to 74.2 per cent in 2020.
Only 56 per cent of respondents said that they feel their organisation acts fairly with regard to career progression or promotion regardless of ethnic background, gender, religion, sexual orientation, disability or age.
8.3 per cent of staff reported that they had experienced discrimination from patients/ service users, their relatives or other members of the public and 9 per cent said that they had experienced it from managers or colleagues.
Importantly, only 25.6 per cent of respondents said they were satisfied with their level of pay. Furthermore, only 26.4 per cent said there are enough staff at their
organisation for them to do their job properly and only 55.6 per cent say they have enough materials, supplies and equipment to do their work.
With regards to staff wellbeing, 44.8 per cent of staff have felt unwell as a result of workrelated stress in the last 12 months and 56.6 per cent have come into work in the last three months despite not feeling well enough to perform their duties.
Responding to the latest NHS Staff Survey results, NHS national director for people, Em Wilkinson-Brice, said: “Our staff have shown time and time again how vital they are to the country, and I would like to thank each and every one of them for the work they do for patients every day.
“In the last 12 months alone, staff have been under unimaginable pressure – they have managed four record-breaking months for attendances in A&E, treated more cancer patients than ever before and faced the twindemic of covid and flu.
“The survey results sadly show a decrease in satisfaction and while it does show improvement in people feeling supported by their line manager and that staff have more opportunities to develop in their careers than last year, we know more needs to be done.
“So the NHS is supporting organisations and systems to focus on those things staff tell us matter to them, such as flexible working, line management, leadership development and career pathways within a compassionate and inclusive culture.”
Nurse Nisha Jose, clinical team leader at Mersey Care’s Clinical Telehealth Hub, said: “People yearn for normality and the comfort of home, yet when they get home, they may become worried.
“With our virtual ward programme, we can do everything that would happen on a hospital ward. We take observations every six hours to identify any issues and we can even carry out ECGs at the patient’s home. It has truly transformed the way we deliver care.”
The NHS in Scotland has become the first in the UK to stop using Desflurane, an anaesthetic, during surgery.
The drug has a global warming potential 2,500 times greater than carbon dioxide.

It is believed that removing it from hospital theatres across NHS Scotland saves emissions equivalent to powering 1,700 homes every year.
The removal of desflurane is the first action of the National Green Theatres Programme which is due to be formally launched in Spring 2023. Part of the NHS Scotland Climate Emergency and Sustainability strategy and hosted by NHS Golden Jubilee, the programme will identify areas where operating theatres can become more environmentally friendly.
Then cabinet secretary for health and social care (now first minister), Humza Yousaf said: “I am immensely proud that we have become the first nation in the UK to stop using environmentally harmful anaesthetics in our NHS.
“Programmes like this are key to our transition to become a net-zero health service, whilst ensuring patient safety remains at the heart of every clinical decision.”
Kenneth Barker, clinical lead for the National Green Theatres Programme, said: “Theatres are high carbon and energy intensive areas that produce high volumes of waste, so reducing the environmental impact of theatres will make a positive difference toward achieving Scotland’s net zero targets.

Audits and compliance capturing are critical components of many industries, and they can be timeconsuming and complex processes. One area where significant improvements can be made is in operational areas, where paper-based systems are still prevalent. That’s where SMS Technology’s operational areas software comes in.
SMS Technology’s operational areas software is an innovative solution for hospitals looking to improve efficiency and accuracy when it comes to audits and compliance capturing. By eliminating the need for paperbased systems, the software simplifies operational areas, making it easier for workers to perform their jobs and for managers to monitor performance.
One of the most significant benefits of SMS Technology’s software is the timesaving factor. With paper-based systems, workers spend a significant amount of time filling out forms and recording data manually. With the software, this time is significantly reduced.
Instead, workers can use handheld devices to record data in real-time, with the information being automatically entered into the system. This not only saves time but also reduces the risk of
errors that can occur when data is entered manually and improves staff morale.
Another significant benefit of SMS Technology’s software is the cost savings. With paper-based systems, hospitals must purchase and maintain supplies such as paper, ink, and printers. These costs can add up quickly, especially for larger hospitals with many workers. With the software, these costs are eliminated, and hospitals can enjoy significant savings over time.
Furthermore, SMS Technology’s operational areas software provides realtime data and insights, enabling managers to make more informed decisions. The software can track key performance indicators (KPIs) such as compliance status, audit results, and corrective action implementation. This information can be used to identify areas for improvement and to make data-driven decisions that can help hospitals optimise their operations. Finally, SMS Technology’s software can be configured to meet specific industry compliance requirements. The software can automate compliance capturing and provide automated alerts for compliance issues or upcoming audits, ensuring that hospitals remain in
compliance with regulatory standards. In conclusion, SMS Technology’s operational areas software is a powerful tool that can help hospitals to streamline their operations, reduce costs, increase morale, and improve compliance capturing and audit results.
By eliminating the need for paper-based systems, hospitals can save time, reduce errors, and access real-time data that can inform decision-making. With the ability to track KPIs and automate compliance capturing, hospitals can identify areas for improvement, optimize their operations, and remain compliant with regulatory standards.
The software is a valuable investment for any company looking to improve efficiency and accuracy when it comes to audits and compliance capturing. L
FURTHER INFORMATION
www.sms-tech.org



When it comes to the nation’s health, we are getting used to seeing big numbers quoted.
One million patients are treated by the NHS every 36 hours. Over seven million people are on the waiting lists. 20 million people have an musculoskeletal (MSK) condition in the UK.
But when you work in the NHS, you know that behind every number is a person with a story. For you, and for them, it’s personal.
And that’s how our journey to rethink how we managed MSK referrals started. Due to organisational boundaries and historical funding, patients needing to access our physiotherapy services were facing waiting times from between 6 to over 26 weeks depending on where they lived.
As a qualified physiotherapist, I was witnessing at first hand the devastating effect long waiting times or incorrect referrals can have on patients. Living with chronic pain impacts on every aspect of someone’s life and restarting the referral process after being referred to the wrong service can delay much needed treatment.
It was our goal to shorten the time between referral to treatment by reducing incorrect referrals.
The first stage was to carry out an audit of the MSK referral process to see why incorrect referrals were happening and what improvements could potentially be made. The audit revealed some surprising results. As many as 3000 referrals were being rejected each year because they were missing key clinical information. This was causing a delay in the system because if a referral is missing vital information, like blood tests or MRI results, it can’t be processed quickly. This also increases the likelihood that the patient will be sent to the wrong clinic. We knew if we could prevent rejected referrals, it would positively impact on waiting times and ensure that specialists’ diaries were filled with patients who they could treat and not need to refer on.
Our 116 GP practices were using a Wordbased proforma referral form at the time, and we decided we could improve the quality of referrals by making the shift from a paperbased referral system to a digital one. The aim being that valuable appointments weren’t
wasted due to incorrect referrals and patient waiting times were kept as short as possible.
I had begun a 12-month Digital Health London Pioneer Fellowship and, with their help, put a business case together to digitally transform the MSK referral process.
We wanted to make it easier and quicker for GPs to make accurate referrals. Going digital would enable electronic patient data to be shared securely and easily between primary and secondary care. This would improve the referral experience and ensure patients attended a consultation at the correct clinic the first time.
Bringing clinical decision making into the GP surgery was also a key ambition and with the help of NEC Rego, we developed a clinical algorithm to make our vision a reality. Consultation was a crucial and integral part of the process. We consulted with a wide range of practitioners and experts in patient care, including GPs, primary care providers, hospital clinician consultants and physiotherapists to set different treatment pathways. We then developed and refined the AI algorithm to ensure the agreed right treatment pathway is in place for each condition we treat.
What happens now is that when the GP is with the patient, they can fill in the referral form then and there. The algorithm E
Our reviews enable Clients to benefit from a detailed forensic review of their Accounts Payable transactions bespoke to their own organisation.
To draw an anology with our own Health, we would compare our reviews to an MRI/scan approach rather than a GP check-up. The depth of our reviews enables the identification of errors previously unknown to the organisation.
STAGE 1 - Identification/detection
• Access to £100,000’s of technology, analytics and resources
• Access to dedicated experienced professionals
• Provides multiple-layer interrogation of transactions with Suppliers
• Specialist expertise in reviewing Supplier transactions and identifying anomalies
STAGE 2 - Verification/validation
• Expert detailed analysis of transactions at individual Supplier level to validate and investigate anomalies

• Obtaining evidence to support initial findings

• We supply the system, processes and resources to recover the errors found on our Clients’ behalf

• Flexible but targeted reporting provides significant additional benefits to Clients
Our Supplier Health Checks are carried out on a NO RECOVERY - NO FEE basis enabling Clients to benefit from a FREE Health Check if no errors are found.
prompts them with a series of questions to consider, ensuring the patient is referred to the correct service to meet their needs, for example a consultant or physiotherapist.
It is pre-populated with info to avoid errors, so we don’t get paediatric referrals for example, as we are an adult service.
Should further diagnostic tests be needed before a consultation with a specialist, the referral tool will prompt the GP to complete this stage. This helps to cut delays and speed up care for the patient.
We receive 50,000 MSK referrals annually from the GP practices covered by our trust and it is clear using the digital referral system has vastly improved the patient experience. We’ve reduced patient waiting times by over a month as triaging cases takes half the time it used to take.
It has also supported GPs by making it easier for them to refer. Although we didn’t mandate switching to the digital, process for the first couple of months almost 80 per cent of GP practices adopted it from the beginning, as it was evident the change substantially improved the referral process for everyone.
Prior to digitising the MSK referral process, GPs would need to pass referrals to the practice administrative team to laboriously complete the paperwork and include all the relevant documentation. What GPs are choosing to do now is, to fill out the referral with auto-loaded clinical attachments in less than 90 seconds during the consultation.
This time saving equates to 3.5 minutes for every patient referred for treatment
which when added up over the course of a year could save up to 3000 GP hours in our area. This is the equivalent of putting another GP into the health service.
The technology works as it is a clear pathway for clinicians to follow, making it easier for GPs and hospitals to manage referrals into secondary care.

As a result of the changes we’ve introduced, we’ve seen over 50 per cent reduction in consultant-to-consultant referrals within the trust as the correct RTT pathways are being used.
Now when a patient speaks to their GP about arthritis or another MSK condition, the doctor can view all their medical data alongside any prior input from the hospital team, giving them the complete picture. This means they can make a more informed decision about which treatment option is most appropriate for their patient when prompted by the questions posed by the digital tool.
This prevents patients being given appointments at the wrong clinic as the
hospital triage team has already assessed which service is most appropriate before the appointment is scheduled. Accurate referrals have increased by 70 per cent as a result and there is a greater consistency of care for the patient.
Going forward, to make sure the clinical pathways continue to be an accurate reflection of current clinical practice we will carry out regular reviews. These will be done in consultation with our practitioners and experts in patient care stakeholders, and NEC Rego, to make sure we are using the very best evidence to continue to provide the best care for our patients.
Redesigning how we managed the MSK referral process has made it easier and quicker for referrals from primary to secondary care and helped us reduce costs by ensuring the right patient is seen by the right specialist the first time. We are confident that our digitalised system has the potential to make a significant financial impact running into millions of pounds over the coming three years. L
We receive 50,000 MSK referrals annually from the GP practices covered by our trust and it is clear using the digital referral system has vastly improved the patient experience. It has also supported GPs by making it easier for them to refer








By adding an MPage for prioritisation to its Oracle Cerner EPR, clinicians working at two hospitals now see real-time patient lists
A digital solution to remove a cumbersome, time-consuming manual process for validating elective surgery waiting lists is paying dividends at the hospitals where it has been introduced.

By adding an MPage for prioritisation to its Oracle Cerner EPR, clinicians working at two hospitals run by the Calderdale and Huddersfield NHS Foundation Trust (CHFT) now see real-time patient lists – which is speeding up the waiting list validation process, reducing a post-COVID backlog by increasing efficiency and preventing the creation of unnecessary appointments.
Previously, lists were compiled in spreadsheets and sent in bulk for validation and prioritisation every 3-4 weeks. This process created common issues for the hospitals’ validation team, including poor/slow response rates and replies sent on Microsoft Word which then had to be copied to the spreadsheet, creating a risk of mistakes and wasting time.
Adding the Prioritisation MPage to the EPR saved 91 hours of clinicians’ time in one calendar month alone, whilst also preventing 5,000 unnecessary appointments.
The new process is the result of a collaboration between CHFT and a project team from The Health Informatics Service (THIS) - which is hosted by the trust - and representatives from St Vincent’s Health and Public Sector Consulting, which markets itself as a specialist in patient-centred healthcare solutions.
The rationale behind the project was an NHS mandate to provide each patient waiting for elective treatment with a P (priority) number between 2 and 4.
This added impetus to an existing desire to create a streamlined prioritisation and validation process using a digital solution that had already been mooted by THIS and CHFT for the trust’s two hospitals, Huddersfield Royal Infirmary, Huddersfield, and Calderdale Royal Hospital, Halifax, both West Yorkshire.
The project’s aims were to: provide real-time availability of information via a single source of truth; reduce administrative time for clinicians and the validation team; provide clearer visibility of patients’ changing circumstances to aid the prioritisation process; and increase efficiency to reduce waiting list backlogs.
The trust’s validation team, which processes an average of 1,800 patients a week, now records straight into the EPR. Anyone in the process can add comments, and clinicians
have the ability to open the page and view it. The responses are live and actioned.
Neil Staniforth, THIS’s director of digital ops and delivery, says: “The fact that MPage writes directly into the patient’s notes during validation makes the process a one-stop shop, easy and convenient. The result is increased staff satisfaction from a workload perspective among clinicians, and the validation team is pleased with the clarity it provides.
“We think the new process is the best we’ve ever had. The ultimate testimony to the success of this project, is that we know if we said we were going to take the new process away, clinicians would fight us, rather than help us pack it up!” Kirstie Blackham, a member of CHFT’s validation team, says: “We receive validations as soon as the consultant does them and any queries can be sent straight back. This is in comparison to the days and, at times, weeks it could take to send things back and forth via email. The whole process is a lot smoother; all the information is clear and easy to access. Even at this early stage, I feel like this will only speed up as people become more comfortable using it.”
While the time reduction in spreadsheet creation and reconciliation allows more time for validation and review, the time saving for clinicians has halved from 10 minutes per patient to five. For example, in November 2022, 1,097 patients were prioritised, producing a time saving of approximately 91 hours for clinicians. In the same month, 5,524 pathways were closed, freeing up approximately 5,000 appointments that could be offered to other patients.
Neil Staniforth: “The benefits of this are twofold: it clears a backlog and if the appointments had not been
cancelled, the patients concerned would have ultimately been booked for an appointment that was not necessary.”
Other advantages identified from the project include: a measurable end-to-end process – full audit trails are now available on EPR and CHFT’s Knowledge Portal Plus (KP+), identifying where each patient is in the process; improved reporting – although limited reporting is currently available via KP+, MPage enables more varied opportunities; improved clinical governance – all validation and clinical review information is available within the EPR instead of a spreadsheet; and reduction in general managers’ time to filter and distribute data. Previously, GMs were required to filter lists by consultant and distribute to the relevant ones. Data now lands directly into worklists, removing GM involvement.
As well as working within its host trust, THIS provides digital and IT services to health and care providers across the UK in primary, secondary and third sectors, such as NHS health trusts, GPs, laboratories, hospices and not-for-profit healthcare organisations. L
If you are interested in working with THIS, get in touch with us below.

Public Policy Projects is a global policy institute that provides practical analysis and development across different sectors, including health, social care, life sciences, net-zero and climate change.
The report, The Digital Divide: reducing inequalities for better health, investigates the digital divide and sets out a number of steps to be taken to make sure that the introduction of digital is done in a way that benefits all communities.
In the foreword to the report, Richard Stubbs, chief executive officer of Yorkshire and Humber Academic Health Science Network and chair of the report said: “Digital technology undoubtedly presents a significant opportunity to positively transform the delivery of health and care services in England and Wales. However, accelerating the transformation of health care through digital simultaneously carries the potential risk of widening the health inequality gaps that exist within our communities.”
Stubbs said: “Through the process of crafting this report, it has been a privilege to have heard many examples throughout the country where co-produced, thoughtful, and focused interventions are tackling this potential divide head on, with real impact as a result. They are trailblazers for the rest of us to follow, and many of the case studies that we heard are featured in this report. Thank you to all who gave their time to engage in our roundtables.
“There is no doubt that digital is here to stay; the pandemic has demonstrated how rapidly the health service can move to digital channels to ensure the continuation of care delivery. But if we are to truly unlock the power of digital for all our communities, then we must always be watchful of the potential risk that the digital divide brings. And though technology will obviously be part of the change to come, much of what will truly make the difference will come from the way that we engage with our patients and citizens; building trust with communities is essential to the equation, as well as co-production and empowerment that creates good user experience of the new models of digital healthcare delivery.”
The report highlights that the digital divide has a direct negative impact on health inequalities in England and Wales. In this case, “digital divide” refers to the gap between those who are digitally enabled and those who are not. Digital enablement is when people have the devices, connectivity, access, capability, motivation, support and participation to navigate online, and to use digital services. In NHS terms, digital transformation means that health services and information are available and accessible online. Digital enablement and digital engagement are known to have an impact on health. They are also known to have
an impact on social determinants of health, including education, employment, housing and finances. Following on from this, some groups of people are more likely to be digitally excluded and there is an overlap between people who are digitally excluded and those who are at highest risk of health inequalities. People over 70, people with disabilities or long-term health conditions, and people with a lower literacy rate or educational attainment are more likely to be digitally included. On the other hand, research from The Nuffield Trust found that groups of patients likely to be in relatively good health (including younger, white, highly educated, living in more affluent areas) are more likely than other patients to successfully navigate online access to care. The report notes that while several factors contribute to the link between digital exclusion and health inequalities, “the digital divide can be seen to contribute significantly to existing health inequalities”.
The report acknowledges that many public services are increasingly available online, as a result of acceleration during the pandemic, and this includes health services. The pandemic has highlighted the benefits of digital healthcare – the report points out the use of digital and data keep more comprehensive records for patients, better monitor population health, and roll out innovative digital health treatments. During the pandemic, with the need to reduce face-to-face interaction, virtual consultations became normal. However, the report also points out that the pandemic has also revealed inequalities E
The thehighlightsreportthat digital divide has a direct negative impact on inequalitieshealth




in digital access and health. The report states: “If these inequalities in connectivity and access are not addressed, health inequalities will persist and are likely to be exacerbated.” The report highlights that some sections of society were more severely impacted by Covid than others. Statistics from the Office of National Statistics reveal that those living in the most deprived areas of England and Wales are approximately twice as likely to die after contracting the virus as people living elsewhere, and mortality rates for the virus were highest among males of Black ethnic backgrounds.
The introduction of the report states: “Maximizing this opportunity will require digital connectivity to become an area of priority for all stakeholders. Digital innovations and data must also specifically target the reduction of health inequalities. This report makes a series of recommendations which, if implemented, will reduce the health inequalities exacerbated by the digital divide, and make more appropriate use of digital and data to target the health of those in underserved communities, and to identify the areas of greatest need in a population. It is acknowledged that these issues are prevalent across the devolved administrations.”
In preparation for the report, which focuses on the health systems operating in England and Wales, roundtables were held with NHS stakeholders, public health experts, integrated care system (ICS) representatives, local authorities, charities, academia, and medical technology providers.

The report sets out eight recommendations, the first of which is: “The Department for Levelling Up, Housing and Communities should change the English indices of deprivation to encompass digital access and skills”. This recommendation is intended to
improve the measurement and documentation of people who are not digitally engaged.
The second recommendation is: “Integrated Care Boards should be responsible for convening and supporting trusted staff in all public services, including health and care, to assess and support those who want to get online”. This means that support programmes should be context specific, as well as tailored to the specific needs of a community. There should also be walk-in centres that provide access, connection and devices, as well as support on digital skills, confidence and safety.
The third recommendation: “Digital-bydefault must operate in the context of the digital divide” means that all government services including healthcare must be accessible equally by digital and nondigital pathways, as a digital-by-default approach may lead to those who are not digitally engaged being at a disadvantage and widen existing health inequalities.
Fourth comes: “NHS England should make Digital training mandatory for all health and care staff”. This is because health and care staff need to be confident and comfortable to access online systems in order to provide the best care, as digital channels become more prominent. This should also include training on the digital divide and its impact on health outcomes, as well as how to support patients to become digitally engaged.
The fifth recommendation is “NHS England should update their Digital Technology Assessment Criteria (DTAC) to ensure that products and interventions are designed specifically tailored to the needs of those with additional accessibility requirements (particularly those with few digital skills, people with disabilities or long-term health conditions, people over 70 years old, and people with English as a second language).” This means putting a focus on good user experience. It is noted that if a service is not
accessible to those who need it the most, this will worsen existing health inequalities.
“Integrated care systems should instil a culture of real-world evaluation for health interventions” is the sixth recommendation. This means that data on health and social determinants of health should be collected before and after interventions in order to build up a base of evidence that can be used to inform.
The penultimate recommendation is that “All should be given access to all their health and care data with summary analytics, and the information should be easily accessible within the NHS app.” This is intended to create trust in the system.
Finally, “New digital care pathways and other support services must be co-produced with the communities they serve”. This means that in order to ensure that services are useable and appropriate for those using them, end users should be involved at every stage of the design and implementation process.

The report concludes: “To reduce the health inequalities brought to our attention during the Covid-19 pandemic, concerted effort must be made to reduce the digital divide and its impacts on health. As healthcare services and tools become increasingly reliant on digital channels, digital skills have become central to the management of health. Simultaneously, digital access and skills impact upon all the SDOH, and therefore digital competence confers benefit to individuals across a broad range of non-medical factors which influence health outcomes (including housing, employment, education, and financial factors). The digital enablement of the population, where appropriate, must be a priority to ensure that no one is left behind and health inequalities are reduced.
“In order to achieve improved digital access for better health, digital access must first be recognised as a significant determinant of deprivation and health. To address this gap, measurement and documentation of those who are not digitally engaged must be improved. ICSs should convene and support staff in health, care, and other public services to provide digital support to communities, tailored specifically to the needs of the individuals in an area. It must be recognised that while digital access and skills can improve health status it may not be appropriate or safe for everyone to be online, and therefore all government services, healthcare included, must be provided at a high level via offline channels.” L
The report is available here
It is noted that if a service is not accessible to those who need it the most, this will worsen existing health inequalitiesWritten by Glen Hodgson, head of healthcare, GS1 UK
Each year it is estimated that NHS spends £10 billion on medical technologies (medtech). Nearly two million individual products are registered on the UK market with approximately one third of the UK’s annual medtech spend distributed between implants and protheses (17 per cent) and surgical equipment (16 per cent). However, until now there has been no central government plan
On 3 February, the government published the first UK medtech strategy1 – a plan to “align action across all our system partners, and drive improvement in priority areas to deliver effective and meaningful change that benefits patients”.
Medtech is critical to health and social care and no occasion has made this more pertinent than the COVID-19 pandemic.
As capacity pressures increased in hospitals, so too did the demand for medtech products, consequently impacting the supply chain. The strategy was later established to “ensure the health and social care system can reliably access safe, effective and innovative medical technologies that support the continued delivery of high-quality care, outstanding patient safety and excellent patient outcomes in a way that makes the best use of taxpayer money”.
The strategic vision focuses on three central objectives: right product, right price, and right place, and to ensure the strategy is not implemented in isolation, it coincides with nine existing sector initiatives including: regulation, digital, supply and distribution, and procurement and clinical quality.
Although the plan aligns with data and digital sector initiatives, data is firmly placed as a key pillar to the four main priority areas of the strategy which include: resilience and continuity of supply; innovative and dynamic markets; enabling infrastructure; and specific market focuses.
Data holds the key to enabling greater transparency and traceability of medical devices on the UK market, but not just any data, it needs to be standardised, and it needs to start with unique device identification (UDI).
GS1 standards are authorised as UDI issuing entities for many international medical device regulations including those for the EU MDR and US FDA.

The Medicines and Healthcare products Regulatory Agency (MHRA) is in the process of making provisions for medical device legislation in Great Britain (GB), and intends to harmonise the UDI system alongside those of Europe and the US. As such, medical device manufacturers and suppliers will be able to use GS1 standards to comply with forthcoming regulations affecting the GB market.
GS1 standards uniquely identify every person, every product, and every place throughout the supply chain and patient journey. Information is encoded into a barcode and identified using a GS1 Key which can be scanned at the point of care or use. This enables devices to be tracked and traced from the point of manufacture to specific locations and directly to the patient. This level of visibility means that devices can be easily located. Staff spend less time searching for devices, minimising delays to patient care as devices (e.g. ECG monitors) are available quickly when needed. It also makes product recalls easier to manage, reducing the risk of harm to patients and allowing for accurate reporting on adverse events by monitoring patient outcomes at scale.
In each of the priority areas, data has a part to play.
To reduce supply pressures that come with using single-use devices, the government has put emphasis on reusable devices that can be decontaminated or remanufactured instead. By applying UDIs, it is possible to trace such devices throughout the decontamination process to ensure a device has been sterilised before it is placed back into circulation, reducing any contamination risks.
It is estimated that around 500,000 different product types are regularly used in the NHS with around 30,000 different products in any one trust. Without UDI, it becomes difficult for standardised data capture for each device to monitor performance or patient outcomes. This leaves the NHS vulnerable to “high levels of unwarranted variation in product use across the NHS, and barriers to switching between products” which “impacts the ability to achieve the right product, in the right place, for the right price”.
The 2020 Cumberlege Review – First Do No Harm2, emphasised the impact of data on traceability and patient safety. The current decentralised nature of medtech data means there is “no single data standard,
making it difficult to cross-reference data from different sources at a national scale”. UDI will help to standardise data collection and sharing, including encouraging the approach of ‘collect once, use often’, improving data quality for reporting.
This final priority centres on the use of medtech in the community and diagnostics. These products are procured via a separate supply chain to that of secondary care organisations, further limiting product traceability. With a system of unique identification in place to improve traceability, it will become easier to compare device information to help inform choice and reduce variation.
Throughout the plan there is a clear message highlighting the need for a ‘joined-up approach’ to remove operational silos. Collaboration and data are key to driving the success of the medtech strategy. The strategy states: “we will continue to work closely with the devolved administrations, the NHS in Scotland and Wales, Health and Social Care Northern Ireland, and all other health and care organisations across the UK to facilitate delivery of our vision in all parts of the UK, with the aim of improving patient outcomes for all”. L
References: 1. https://www.gov.uk/ government/publications/medical-technologystrategy/medical-technology-strategy
2. https://www.gov.uk/government/ publications/independent-medicines-andmedical-devices-safety-review-report FURTHER INFORMATION
A new 3D anatomy teaching model has been launched which will feature the most expansive skin tone library ever available in global health education. Health Business spoke to some of those involved in the project


Complete Anatomy 2023 has been launched by Elsevier and was developed after years of research and consultation with anthropologists, ancestral diversity experts, professors, students and 3D artists. The intention was to develop a broad spectrum of skin tones and facial features so students can learn from a model that more closely represents them and the patient populations they will serve, as well as address unconscious bias. Previously, light-skinned bodies have dominated anatomy learning. A study in the Journal of Medical Education and Curricular Development in 2018 found that less than 5 per cent of images in general medical texts included dark skin tones.
A study in the American Journal of Public Health found that racial bias amongst healthcare workers can be linked to poorer patient outcomes for people of colour. One example of this is in skin cancer treatment, for which clinicians are required to look for melanomas on nails, hands and feet. These melanomas can appear differently on different skin tones. Therefore, if a
clinician is not familiar with melanomas on different skin tones, this could lead to an inaccurate or delayed diagnosis. Health Business spoke to Claire Smith, head of anatomy at Brighton and Sussex Medical School and deputy pro vice chancellor (Education and Innovation) at the University of Sussex, Julian Okorocha, year 2 medical student at Brighton and Sussex Medical School and Alan Delmar, product manager at 3D4Medical from Elsevier.
We first asked why they wanted to get involved in this project. Claire said: “At Brighton and Sussex Medical School, we have for a number of years worked to make our curriculum more inclusive. We are currently undertaking research to understand what this means in anatomy, and how to develop best practice in educating future medical and allied healthcare practitioners. Complete Anatomy is one part of this for us. We had worked with Complete Anatomy with the release of the full female model. Before then, the anatomy we often see in textbooks and e-resources has
been built on a male skeleton, but with, for example, breasts added on and hence was not true to the anatomy seen in clinical practice. This new release takes the theme of inclusivity further and now allows us to customize the model being used even more to reflect different skin tones and facial characteristics, in addition to being able to teach on a complete 3D female or male model.”
Conversation turned to how the model was created, with Alan explaining: “Firstly, it’s important to note that beyond the skin customization options, the core anatomy for male and the core anatomy for female stay the same. It was important that in addition to celebrating our differences, we also emphasise the fact that, ultimately, there is more to unite us than differentiate us. This means that, regardless of what visual characteristics the user applies on the model, they will have a consistent learning experience with their classmates.
“When it came to the design of the visual characteristics, our 3D artists had ongoing E





consultation with subject matter experts in the field of ancestral diversity over the course of two years. From speaking to the experts, it quickly became apparent that trying to represent specific population or ancestry groups through our models would fall into stereotype, and not represent of the true range of human diversity. Thus, we designed our customisation options with more of a mixedancestry approach, reflecting the individual beauty that exists in humans as a whole.”
Complete Anatomy 2023 comes after years of research and there were some challenges along the way, as Alan explains: “When it came to the design of our facial characteristics, a unique challenge faced by our 3D artists was representing the broadest possible range of human variation while also relating accurately to the underlying anatomy. This was achieved through painstaking testing and re-iteration of our new set of facial characteristics to ensure top anatomical accuracy.”
He said: “When our medical content team reviewed our existing 3D anatomy models, it became clear that they overly represented Northern-European phenotypes, since this is what the majority of existing anthropological material in this field is based on. Our team had to do some thorough investigation in order to find reference material showing a broader range of human diversity. Through this in-depth review, and along with the guidance of the subject matter experts we worked with, we made subtle changes to the male and female 3D models in order to make them more broadly representative, and less particular to one regional phenotype.”
App

Complete Anatomy is available as an app, which has more than 20 million downloads and more than 3.4 million active users. It is used at more than 500 institutions and clinical organizations globally.
Alan described how it works: “When the user opens the app for the first time, they will be asked to customize their model during the app setup. Firstly, they will select a set of facial characteristics; it was important for us that these are presented with no skin tone applied to resist stereotypical representations. Once a set of facial characteristics is selected, the user will then select a skin tone from a colour wheel. Again, a pre-selected state is avoided, until the user begins swiping through the wheel. Once they have chosen
their skin tone, they click SAVE and they are now ready to learn anatomy on their customized model. It was important for us that we have no default option, so if the user skips the setup, a random set of visual characteristics are applied onto their model.”
Complete Anatomy aims to fight racial bias amongst healthcare workers, which as previously mentioned can be linked to poorer outcomes for patients of colour. One of the most important factors is the benefits it will bring to patient care and the health service in general. Claire said: “The key to ensuring our teaching is inclusive is to look at the populations of patients that the future medical and allied healthcare students will serve. As humans, we are each unique and it’s important to highlight both our similarities and our differences for students. This development within Complete Anatomy means that our teaching is not based on one white male, but represents many individuals from multiple backgrounds. This will therefore improve students’ readiness for diverse practice in the real world.”
Julian added: “The new Complete Anatomy model is a huge step forward in inclusion and diversity in our learning as students. It contributes to the fantastic work of
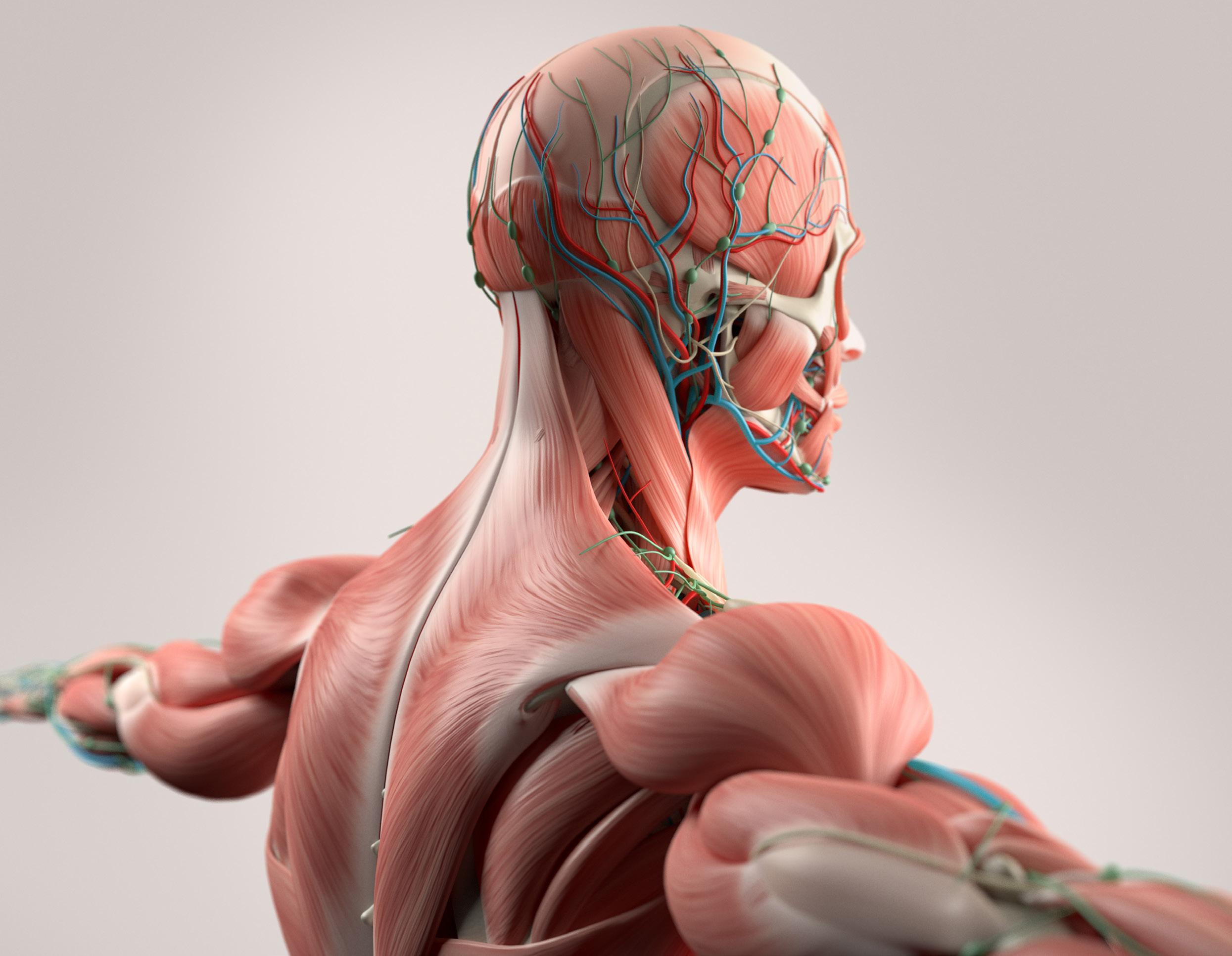
addressing unconscious bias that has for a long time been ingrained within medicine. It is well documented how bias has negatively affected patient outcomes, especially for those who do not fit the stereotypical white and lean representation in the medical learning resources. As a major tool for anatomy learning, the new model normalises the inclusivity of different skin types and facial characteristics. This awareness plays an important role in training competent future doctors, especially when they later learn to recognise and diagnose conditions that might have varying differences in presentation based on skin tone. Overall, diversity in representation is critical for the provision of equitable healthcare for all patients.”
Complete Anatomy 2023 aims to address racial bias in healthcare, and provide a spectrum for students to learn from and therefore improve patient care and outcomes. Providing the most expansive skin tone library ever available in global health education, the cloud-based education platform is on the right track to achieving these aims. L
Complete Anatomy 2023 is available in the Apple Appstore, Windows, and Google Play.

As the NHS approaches 75 years old, it is incredible to think about the achievements of the organisation and its staff, without which it would be nothing but a dream. At the birth of the NHS, IT was unknown as an acronym, and computers had barely left Bletchley Park and the research labs of distinguished universities, never mind made it onto a hospital site, a ward, or unimaginably until the 1980s, every desk. Fast forward to today and the role of computing in the modern NHS cannot be overestimated. Whether supporting communications, imaging scanners, or storage at various locations across a hospital site, they are finding a role in every aspect of patient care, the operational tasks of running a hospital and making it easy for staff to access the resources they need wherever they are. Advances in artificial intelligence are going to play a more significant role in the NHS going forward, and this will offer huge opportunities to increase the speed of diagnoses, in terms of both imaging and testing samples. And whilst some of these services will be provided through cloud technology platforms, the need for localised IT and data centres is as strong as ever.

With such a dependency on IT, the amount of processing, potential energy consumption and
equipment in data centres has increased –this is something that has gained a lot of attention. Hospitals already consider it their responsibility to ensure efficient use of energy across their operations, and understand that they have a role, like every other organisation, to work towards a sustainable future. There are many things that can be done to make a data centre more energy efficient, but the important thing is to understand what is really happening in the data centre. Cooling is one such area. The extreme temperatures we experienced in the UK last year will come again and the trend is undeniably upwards, even if we do not set a new record in 2023. Summer temperatures are rising and periods of intense heat getting longer. All this means that the ambient temperatures are impacting the performance of your cooling infrastructure and there were several high profile cases of data centres having to be shut down across a range of industries in 2022, including the NHS. Use the data you have in your Environmental Management Systems (EMS), Building Management Systems (BMS), Intelligent Power Distribution Units (PDUs) and other systems to make sure what you think is happening in the data centre (DC), is in fact really happening. The data is screaming out to help you! There may be opportunities to consolidate servers, or change environmental controls that will reduce the energy demands of the data centre, its cooling requirements, and make that cooling more efficient. This is not just about reducing costs, or the impact on climate change, but is equally important in respect of business continuity.
If you are looking at your HVAC infrastructure and know you have been putting off the inevitable for too long, then maybe it is time to get a plan together. It may be that over time, the way your infrastructure has grown means that you need to reconsider the current arrangement of your hot and cold air flow in the data centre. Changing your whole cooling infrastructure is not a quick process that you can decide this month, and deliver next. And for data centre managers, the challenge is often making the case for such large capital investments. It takes planning and should form part of a much broader strategic plan for the data centre, that takes account of the future needs of the hospital, staff and patients. In fact, it is important to be aware that even a small change to a cooling system can take six months in the current climate. The reason for this is supply chains remain heavily disrupted by global events and a condenser ordered in March, may not be delivered until September, never mind installed.
The NHS is one of the UK’s most recognised and globally admired institutions. It has been at the forefront of many innovations, and will continue to be long into the future. Technology will have a key role to play, making it possible for more patients to be diagnosed and receive treatment quicker than ever before. We need to care for our data centres, and plan every aspect of their future, so they can fulfil their role in making that future a reality. L
FURTHER INFORMATION
siteltd.co.uk
Chris Dimitriadis, chief global strategy officer at ISACA (Information Systems Audit and Control Association) on how public sector organisations can protect themselves from cyber threats
Public sector organisations in the modern digital economy face an ambitious task in earning – and maintaining – people’s trust. Recent events like high-profile security breaches involving senior government officials, and the ransomware attack on Hackney Council, have fed into a growing distrust in many institutions. And with heightened scepticism about how wellequipped organisations are to protect personal data, building a trusted public relationship is more challenging than ever.
The only path forward is for organisations to make strengthening digital trust – defined by ISACA as “the confidence in the integrity of relations, interactions and transactions among providers and consumers within an associated digital ecosystem” – a central priority, and to strategically work through all obstacles that could impede this pursuit.
What specifically is preventing public bodies from achieving digital trust? According to ISACA’s State of Digital Trust 2022 survey report, the top obstacles are a lack of staff skills or training, lack of alignment of digital trust and strategic goals, lack of leadership buy-in, and lack of budget. Let’s look at each of these areas to see how public bodies can work through these obstacles to achieve digital trust.
Many of the digital trust fields – areas such as cybersecurity, privacy, IT audit, risk management and IT governance – face critical staffing shortages, as the labour supply in those areas often does not keep pace with public sector demand. But in many cases, organisations can find the right employees by being less rigid about criteria for filling these roles. They can then reduce the skills gaps by providing ongoing training and supporting relevant professional certifications while on the job. Organisations also need to strongly promote a culture of collaboration among these
professionals must support each other’s work and ethical considerations related to emerging technology implementations must be considered cross-functionally.
Digital trust is so critical for public sector organisations to succeed that it must be baked into strategic goals from the outset, instead of only being considered once goals already have been established. People rightly expect public bodies to demonstrate urgency in putting plans into action but failing to ensure the necessary security measures are in place can undermine commitments to serve the community. Taking process shortcuts in the name of a near-term goal is likely to lead to a long-term problem that could erode trust with the public and key stakeholders.
While public sector leaders may not understand all the intricacies of the threat landscape or data privacy regulations, they should understand how building and sustaining trust with the public is necessary to achieve their goals.

If that is not the case, digital trust champions such as chief information E

MAINTENANCE
Prevent everyday wear and tear with Yeoman Shield’s extensive range of easy-clean, wall and door protection.
Our attractive, maintenance free, hygienic products protect healthcare environments from costly impact damage, making repainting and repair a thing of the past.


Blending with decors, and available in primary dementia-friendly colours, our designs can include signage, to promote the well-being of patients and aid wayfinding.
For more information call 0113 279 5854 or email info@yeomanshield.com
cost effective wall and door protection www.yeomanshield.com
security officers, data privacy officers and risk leaders should engage organisational leaders by communicating in clear, businessfocused language what the business risks are of failing to prioritise digital trust.
Too often there is a disconnect between organisation leaders and technology functions in the language that they speak. Framing these conversations around building digital trust can be an effective way to bridge that divide and gain leadership buy-in.
Prioritising digital trust inevitably requires a significant investment in staffing, tools and ongoing training and professional development for employees. While the public sector is often burdened by budget constraints, the risks of failing to make the necessary security investments must be carefully considered.
Public sector organisations are an attractive target for cyber criminals due to the sheer volume of personal identifiable information they hold. And

while the tactics employed by bad actors are becoming more sophisticated, many organisations are increasingly at risk due to outdated technology, systems, and processes. As we have seen in the fallout of the ransomware attack on Hackney Council, huge investments in time, money, and resources are required to recover from such an incident, but budgets can be better managed when proactive steps are taken in anticipation of threats.
While there is much progress to be made, each of the above obstacles can be
addressed through commitment from public sector leaders and a renewed commitment to cross-functional collaboration.
Without earning and preserving trust from the public and other stakeholders, no amount of digital innovation will be enough for modern enterprises to remain competitive. Whatever factors might currently be holding organisations back from driving toward digital trust must be identified and overcome to set a foundation for sustainable success. L FURTHER INFORMATION
www.isaca.org
While there is much progress to be made, each of the above obstacles can be addressed through commitment from public sector leaders and a renewed commitment to cross-functional collaboration

To ensure that this system is effective, it is vital to have platforms for organisationwide collaboration and knowledge sharing. By bringing together different stakeholders from the breadth of the UK, such as healthcare professionals, regulators, police and other government bodies, we can work together to identify potential risks of fraud and tackle the prevention element as well as detection and subsequent resolution. That is the goal of GovNet Fraud and the upcoming NHS Fraud conference on 16th May: www.nhsfraudconference.co.uk
Tackling fraud together: the importance of data sharing as a part of your fraud prevention and detection plans
Data sharing is not just a good idea, it is essential to the security of the NHS. If each Trust only uses its own data, you only see part of the picture. To this effect, and to keep up with fraudsters, we need to be sharing data across the NHS and with relevant local authorities and external bodies. In other parts of the public sector, we’re making good progress on this - the Cabinet Office’s recent proposal to create a new regulation under the Digital Economy Act 2017, strengthening the ability for government departments to share necessary information to support identity verification and reuse, is a huge step in the right direction but there’s still a long way to go. CIFAS and NHS England will be hosting an open and honest panel session as part of the NHS Fraud conference, giving advice on how to work with the National Fraud Initiative (NFI) in practice, and explanations on how to use the Data Protection Act exemption to aid your investigations.
Understanding prosecution and alternative routes
Fraud investigations are complex and challenging processes. Because of this, Andrew Penhale, head of the Specialist Fraud Division for the CPS, will be demonstrating how to make sure your fraud investigation meets CPS requirements, including the need for thorough evidence gathering and analysis, understanding applicable laws and regulations, creating a clear chain of evidence, and ensuring accuracy throughout the process. In some cases where the investigation reveals the conduct not suitable or significant enough to meet the threshold for prosecution by the Crown Prosecution Service, other civil remedies are available to act as a deterrence and punishment for the offence committed. Simon Hammond, director of claims management for NHS Resolution will explore what alternative civil remedies are available, and what steps you need to take to achieve them.
The importance of fraud within NHS finance
As Mark Cheeseman OBE recently said in his Fraud Focus interview with Alex Rothwell (opposite) – “Fraud is a fact, it’s not a failure. Seeing it as a failure is one of the things that really holds us back because it creates a culture of defensiveness, as though we’ve done something wrong”. To expand on this, Matthew JordanBoyd, director of finance and corporate resources, NHS Counter Fraud Authority will be discussing
how finding fraud must be at the forefront of all NHS finance teams, specifically mandate fraud which has been on the rise in recent years, becoming the biggest threat to the NHS. To instigate the culture shift we need people working at all levels within the NHS to accept that fraud is a part of what we do and will always exist, so it must be drilled home that identifying fraud really is a positive outcome. If we don’t identify it, that’s when we need to re-visit our processes, looking at what other Trusts and public bodies have done differently, and start finding the gaps in our own systems.
As well as identification, fraud prevention is an essential element of any successful counter fraud function and it requires organisations to be proactive in their approach. Prevention can be achieved through a combination of technology, processes, and people: technology can provide real-time insights into potential fraudulent activities, while processes can help ensure that the right controls are in place to prevent fraud from occurring. Finally, people are needed to ensure that these controls are being followed and that any suspicious activity is reported promptly. The NHS Fraud conference closing debate will see Mark Astley, head of NAFN Data and Intelligence Services, National Anti-Fraud Network (NAFN) and Rachael Tiffen, director of public sector, CIFAS discussing a range of different prevention tactics, how to use them and which they’ve found to be most effective.
From prevention and detection to awareness and collaboration, NHS Fraud is a groundbreaking, free-to-attend event that will set the base points to improve the NHS’s national response to fraud. The conference is designed to let you network, ask questions, debate, discuss and engage with 200 other counter-fraud professionals within the NHS, local government and other public bodies. Complimentary tickets are available now. Health Business readers can book here and view the full agenda here

The NHS is one of the largest organisations in the UK and it is essential that it has a strong and unified system in place for detecting and preventing fraud, bribery and corruption
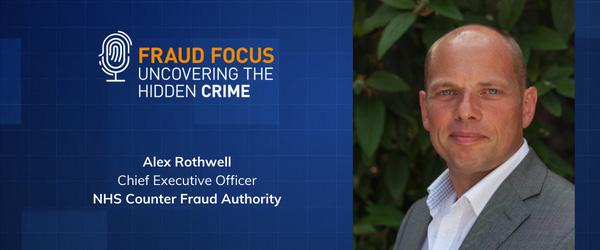
Fraud Focus is a monthly show for the Counter Fraud community, where leading experts in the industry share their insights and opinions on all things fraud
Last month Mark Cheeseman OBE, interim chief executive of the Public Sector Fraud Authority caught up with Alex Rothwell, CEO of the NHS Counter Fraud Authority for an open, honest conversation about Alex’s passion for data sharing; the role that social engineering still plays in a tech-driven world; the need to change our internal culture so that finding fraud is seen as a good thing rather than a failure; and where he thinks future threats may lie. Watch the full interview here.
How did you start working in counter fraud?
I joined the NHS as CEO in November 2021, off the back of a 30-year policing career that began back in the very early 1990s.
My career has gone in many different directions including organised crime, a spell running the Metropolitan Police’s Cyber Crime Unit and I also briefly ran the Fraud Squad there as well. But what really got me to where I am now was my time with the City of London Police and the national lead force for fraud, which helped the Home Office shape the future of policing and their response to fraud.
It was great to work alongside the Home Office and some really great people in policing and the private sector. In many ways this was a good segway to join the NHS, where I think a little bit more commercial focus is required. It’s a big organisation!
Why is fighting fraud important to you?
If I look at this through the lens of the health service – one of the largest employers in the world – we get the largest share of government funding by department. That is a fraud risk in itself, whether you like it or not. If we haven’t got processes in place to deal with that risk, there are obvious consequences and it’s a lot of money that could otherwise be spent on healthcare. In my business every penny you lose to fraud is money that’s not being spent on making people get better.
Do you have any catchphrases or sayings that sum up your learnings from the past 30 years’ experience?
There’s a concept in policing called the Peelian Principles, established by the founder of the Metropolitan Police Service, Sir Robert Peele. He said, “The test of police efficiency is the
absence of crime and disorder, and not the visible evidence of police action in dealing with them”. This makes a lot of sense in a policing context, but when you apply it to fraud it makes less sense because fraud is a hidden crime. I think the test of efficiency for fraud is actually the visibility of fraud professionals getting out there and dealing with it - sort of an anti-Peelian principle.
A second one, is something a colleague said recently that stuck with me: “Absence of evidence is not evidence of absence”. It’s easy to say, “We haven’t got any fraud here” if you haven’t actually looked.
What do you see as the some of the current threats? I could list a whole load of specific fraud threats but there are a couple of things that really stand out for me.
In the current climate there are so many risks for governments and businesses: geopolitics, climate change, cyber security etc. and unless we ensure that countering fraud is embedded as a discipline at all levels, my worry is that it will be ignored. In my policing career we always used to ask ourselves, “What’s happening now that I’m not actually aware of?”. We need to have processes in place to look at emerging threats and see what will be on the horizon in the coming months or years. It’s so easy to let that slip.
To expand on the idea of scanning the horizon, what future fraud risks do you anticipate?
I read that the other day that £2 billion worth of cryptocurrency was stolen last year, but it was stolen through social engineering and a lack of
knowledge on behalf of the owners. This is a great example of criminals exploiting new, niche subjects that not many people truly understand. These are the sorts of threats that I think we need to keep an eye on, for example AI and identification technologies that can be used to prove who we are etc. We need to work on fraud proofing these technologies as we go and as they come into play, not once they’re already embedded in our day to day.
What do you think are the most important points when it comes to dealing with fraud?
There are a few things that really stand out for me: We need to create really strong cross-departmental functions, just like the Public Sector Fraud Authority, with government-related Fraud Ministers who really understand and support what we’re trying to do, so that they can translate it into really sound policy. We need to change the culture around fraud so that people know
1) Finding fraud is a good thing and 2) we need to accept that there is always going to be fraud. We have to embed both of these in the culture of any organisation, and it’s up to everyone to get this message out there.
Data sharing is the other one that I’m really passionate about and I think that’s probably where the future lies, to tackling fraud at scale. Easier said than done, though, isn’t it?
To watch the full videocast, and to get a monthly Fraud Focus interview delivered straight to your inbox, visit https://register. govnet.co.uk/fraud-focus-episode-4





Top-fix Version Coming Soon! With a new profile, end brackets and screws
Anti-ligature gliders cannot be removed from the track

Three load-release weights to choose from
For more information on this new reduced-ligature track, to receive a sample or demonstration contact Grant on 01268 570900 or email enquiries@yewdale.co.uk
Following his appearance at the Digital Health Rewired conference in March, Professor Ben Goldacre explains why information governance is not enough when it comes to protecting privacy


The NHS holds an incredibly rich dataset containing the medical records of more than 65 million patients going back for decades. These detailed records have the potential to help understand the benefits and hazards of different treatments, monitor and improve clinical services and drive life sciences innovation.
Yet this poses an ethical problem, which Professor
Ben Goldacre, director of the Bennett Institute for Applied Data Science was commissioned to investigate. “The same data that could do good work also contains the most private secrets of every citizen in the country,” says Goldacre. “The challenge is this: how do we get lots of analysts doing lifesaving work on the data, whilst also managing the risks when lots of people have access to confidential information?”
This dilemma was illustrated by the General Practice Data for Planning and Research (GPDPR) scheme in
2021, which intended to gather patient data held by GP surgeries in England and feed it into a central NHS database. Promises that the data would be anonymised were not enough to reassure the public about the privacy risks and millions opted out of the scheme, leading to it being withdrawn.
“We lost public trust, and so many people opted out that we lost a lot of data,” explains Goldacre. “The reality is that when you remove names and addresses from people’s records, it does something to prevent their data being misused, E
NHSTheholds an incredibly rich dataset containing the medical records of more than 65 million patients going back for decades
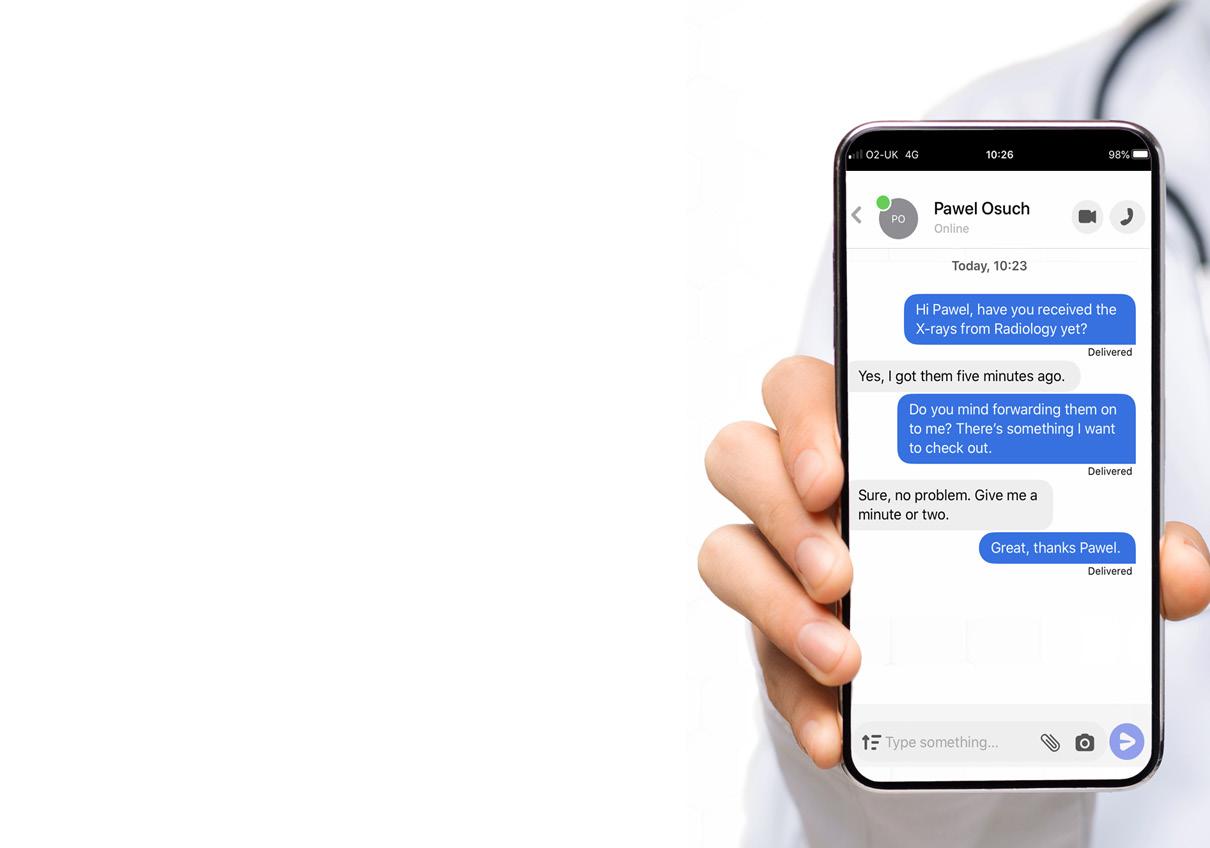








but it isn’t enough to ensure their privacy.”
To resolve this issue, Goldacre was asked by the secretary of state in 2021 to conduct a major review into the safe use of health data. The result was the Better, broader, safer: using health data for research and analysis report, known as the Goldacre Review.

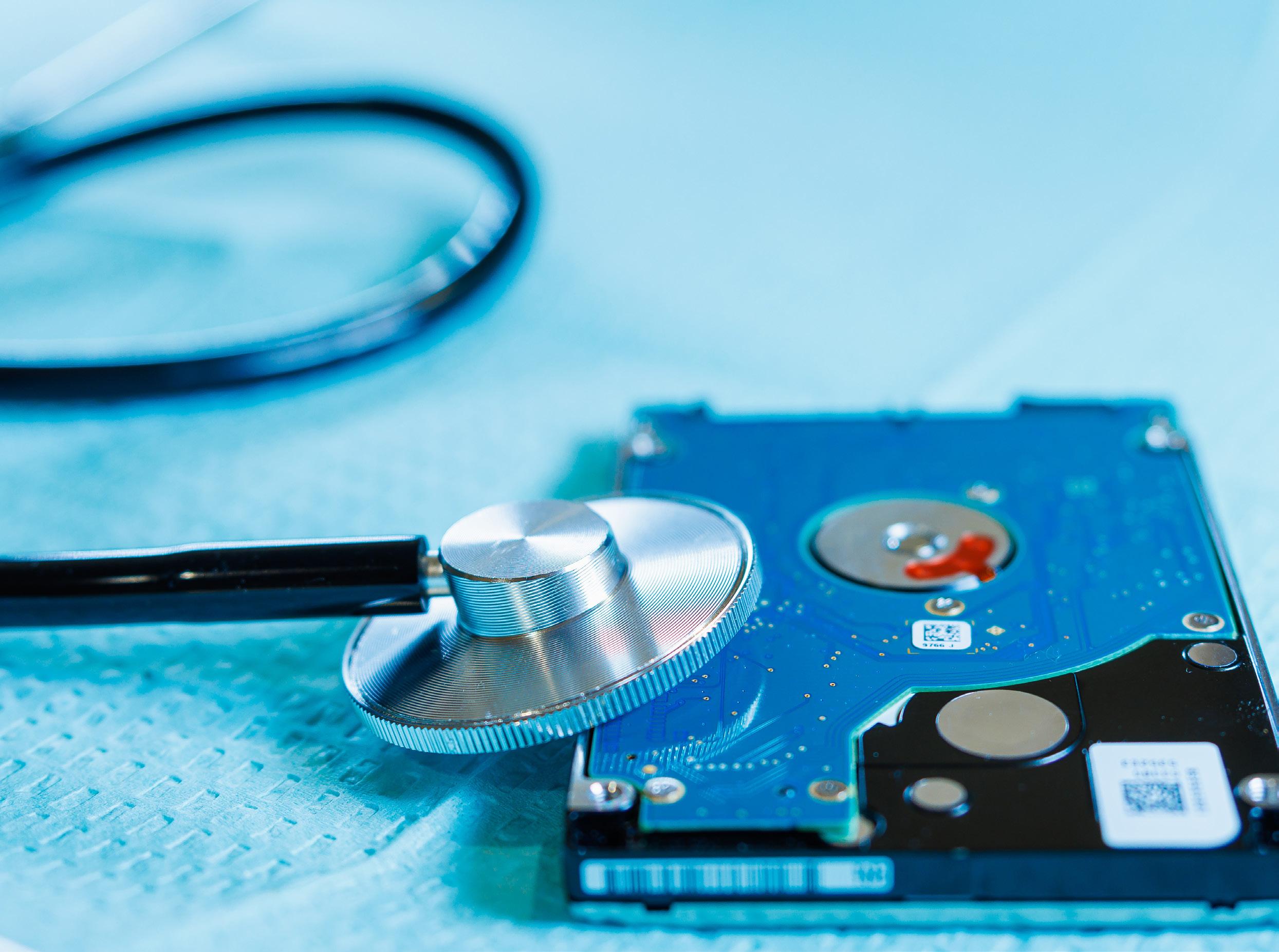
Reassuring the public
“It’s not just enough to tell people to trust the good work you’re doing with data. You have to take practical steps and prove to them what systems and platforms you’ve got to protect their privacy. You need to show rather than claim,” asserts Goldacre. Historically there has been a lot of reliance on information governance to protect health data, but according to Goldacre this is not sufficient. “We have lots of rules for people who want to access data so we can assess whether they’re trustworthy. That was the only way in the past that the system could think of allowing the privacy risks of letting people download the full history of millions of patients’ medical records onto their own machines,” he says. “Those rules create huge delays and obstructions, which has caused tremendous frustration for analysts and researchers.” Instead, the Goldacre Review recommended the use of trusted research environments (TREs), which keep all patient data on a central machine. This would allow NHS
analysts and researchers to work within that secure environment, rather than downloading data onto their own machines. “TREs are commonly used in other sectors, and absolutely perfect for the problem we face, because they allow lots of people to work on the data without having to worry so much about it being misused,” continues Goldacre. They also manage some of the duplication and inefficiencies that happen when people work with data.
“When everybody is working on the same data in thousands of different places, they’re all duplicating that data curation work,” adds Goldacre. “That’s a spectacular waste of money, but also a risk because those hundreds and thousands of people doing the same job behind closed doors can’t learn from the great work people have done on data curation in other settings or see it and evaluate its quality.”
The Government’s Data Saves Lives strategy published last year, adopted TREs as the normal way of working with health and social care data. There is a firm ministerial commitment to only reactivate the GP patient data collection when they have a TRE built on best practice. An example of best practice quoted in the report is OpenSafely, a secure analytics platform for NHS electronic health records (EHRs) run by Goldacre’s team on 58 million patient’s GP data for the past three years. The other is the ONS TRE that has been running on census and other data for the past two decades.
Next on the horizon is implementing the Goldacre Review’s recommendations to create standard training, job descriptions and clear career progression for data analysts in the NHS.
“The NHS analyst community has outstanding pockets of excellence but suffers from being dispersed across hundreds of trusts and local areas,” says Goldacre. “If you want excellence to spread, you need to have clear lines of communication and good quality training so different people in different places are speaking the same language.”
Ultimately Goldacre’s vision is to see data used more efficiently so as to provide better, safer patient care.
“I don’t think the big gains in quality of life and life expectancy are going to come from single new pills. I think they’ll come from improving the efficiency and logistics of delivery of care in the health service. And that’s supported by the better use of data,” he concludes. L
“If you want excellence to spread, you need to have clear lines of communication and good quality training so different people in different places are speaking the same language.”

Knowing your organisation is operating at the highest possible standard is a great feeling, but how can you make sure it’s happening consistently in all parts of the organisation?
It’s no secret that as an organisation you look for reliable, committed suppliers who are constantly evolving and improving, and that’s exactly what our clients want from us. We wanted to be able to demonstrate to our clients that when they work with us they are receiving the very best products and service. Whether we’re keeping their data secure, delivering training to their staff or designing the most effective software we want them to feel confident that they are receiving the highest standard, and that’s where ISO accreditation comes in.
The International Organisation for Standardisation sets official standards which cover a wide range of business areas worldwide, everything from supply and production to management and training. Each standard is agreed by an international panel of experts, each with proven experience in their field We’re very proud to say that we hold three ISO accreditations, ISO 9001 Quality, ISO 27001 Information Security and ISO 14001 Environmental Management. In the seventeen years since we first gained ISO 9001, we’ve been regularly participating in the ISO process and have never incurred a non-conformity in any of our accreditation checks. Each accreditation is re-assessed every three years and usually involves three or four days of work. At the end of the inspection, you are either re-accredited or given a breakdown of areas which have not conformed and receive a timeframe in which to address the issues before a re-examination. At that point it’s a pass or fail, which in this case means your accreditation is revoked. But having a certificate on the wall, only means so much, what does working with an accredited company like Asckey really mean for our clients?
piece of
When it comes to measuring standards, many organisations choose to focus only on specific parts of their business. At Asckey, we decided to do it differently. We decided that if we were going to be accredited in something, then we wanted it to be across all areas of our organisation. For all of our accreditations, it means we

meet the standard across our organisation, from our sales processes and the literature we produce to our demonstrations and the way we train our staff and clients. If every single aspect of the business is covered then not only are we confident in what we’re doing and how we do it, but our clients can share that confidence too.
When it comes to ISO 27001, Information Security, it means that the data you share with us is safe in our hands, at all levels. It demonstrates that we take your data security seriously and we’re constantly evolving our security processes to ensure we stay ahead of the curve. Our reputation rests on keeping information secure, so it’s not something we’re going to take lightly. Our Information Security Policy is constantly being reviewed to ensure protection from potential internal and external threats. When it comes to our electronic systems, we‘re vigilant about information security across the board, whether that’s our physical premises, alarm systems, computer equipment or entry codes, everything is included. All members of the team are expected to prioritise information security, from backing up and storing data to securing laptops and managing confidential data at client sites. ISO 27001 is such a critical area for us that we’re committed to keeping it at the forefront of everything we do, wherever we are.
We’re passionate about delivering effective training, whether it’s internally or for our clients. ISO 9001, Quality, shows that irrespective of the product you buy from us you can guarantee that the process of training will be logical and relevant. Whilst our training courses may differ, the quality of them does not.
Not only that but being a ‘Quality’ organisation demonstrates the standard of our products and services and the importance we place on our business performance, our ethical and professional manner and our desire to listen to our clients and get things right first time. It means continually improving our services, processes and working with suppliers who share our values and expectations. In short, ISO 9001 is an indicator that we’re constantly striving to be at the top of our game and want to work with people who feel the same. The accreditation means we can say with pride that Asckey is synonymous with Quality, and that’s quite an accolade.
In today’s world we all have a social responsibility to support the green agenda. As a business our carbon footprint is relatively small, but it’s still important that we identify areas where we can improve processes and procedures in order to reduce our environmental impact. Investing the time in committing to ISO 14001, Environmental Standard is one way we’re doing this. Under ISO 14001, we ensure we’re a paperless workplace, and one which guarantees the responsible use of energy, including conserving and improving energy efficiency. Our teams are encouraged to help reduce the overall carbon footprint whether that’s through recycling, turning lights off or reviewing and improving out Impacts and Aspects Register. It’s easy to say you’re doing your bit for the planet, but it’s another to prove that you’re consistently striving to do so. It does take time, but it matters to us, to our staff and to our clients and therefore it’s something that we’re passionate about. The accreditation gives us a real feeling of achievement, that we’re making a difference and continue to take steps in the right direction.
The nature of the services we provide necessitate that our clients entrust us with data that is critical to their organisation. We regularly tell people that we take our job seriously but being able to evidence this and provide that added level of reassurance is great for them and us. Being fully accredited across the business gives us the peace of mind that we really are delivering what we say we will – and that really matters. Why not get in touch and find out how we could support your organisation.L
Energy, squeezing the most out of software and hardware to optimise the “E” in BEMS. Aside from our design and install packages, we offer green maintenance services that deliver sustainability without sacrificing Return on Investment (ROI).

Relying on Powell Systems BEMS
Our client base includes major health facilities in the UK and Ireland. Our team is proud to be involved in providing the country’s best scientists with the corresponding best in facilities. Among these are labs that must always be at a certain pressure or areas where the CO2 is suppressed to desirable levels that keep the researchers alert.
While good efficiency is par for our course, extracting maximum efficiency out of buildings is what we aim to routinely deliver. On top of this, investors, building owners and architectural designers count on Powell Systems for innovative solutions that further reduce their operating costs. In this arena, we have proprietary methodologies supported with leadingedge technology. Our robust team spirit has built a thirty-year track record of cuttingedge projects and satisfied clients. We are driven by a business philosophy of collaborating closely with our clients. We don’t just work for you; we work with you. This approach ensures that your project requirements are fully developed, and only the best products and services are delivered.
Every building has equipment installed to make them comfortable, convenient and safe. Older buildings may be controlled by simple devices like timers counting down to an optimum Start. Newer buildings will have more sophisticated controls for weather compensation, CO2 sensing and optimum Start/Stop. These would be matched to the building’s purpose and intertwined with energy management. A computer-based Building Energy Management System (BEMS) is the key to unified implementation. The BEMS
“intelligence” algorithms decide the best possible action after evaluating the real-time data feed from its remote sensors. Acting as the brain, the BEMS does the checking, computing, decision-making and controlling. With its hardware and software working continuously 24/7, maximum operational/ functional efficiency can be achieved by the building’s Facilities Management team. One of Powell Systems’ latest innovations uses advanced remote access to monitor a client’s BEMS from their head office. It is then routinely tweaked to perform better in a cycle of continuous improvement.
In today’s construction industry, there is intense focus on sustainability and reducing carbon footprint. Strict new requirements have been added to legislation and regulation. Using best value net-zero solutions, the Powell Systems team has successfully achieved and even exceeded compliance for our clients across the health spectrum.
It’s now necessary to provide robust points of interface for PV cells, EV charging facilities and other emission-reducing components. We offer a wide range of manufacturers’ hardware configured to merge with new or existing equipment. These innovative uses of materials and equipment help to achieve net-zero building objectives as well as improve aesthetics and atmosphere.

Powell Systems is a BEMS engineering company, with a big emphasis on the “E” for

Powell Systems designed the BEMS for Royal Marsden Hospital’s Oak Cancer Centre in Sutton. It is integrated into the labs and other spaces of the Centre to provide close control and comfort in this very dynamic hospital environment. The development of this complex BEMS project required careful coordination with the different operations, including the Centre’s patient-centred day care.
The London School of Hygiene & Tropical Medicine collaborates with the Medical Research Council Unit halfway across the world in The Gambia. Here, we again demonstrated our expertise in BEMS for high performance laboratories, and in remote sensing. This gave the London School the ability to remotely monitor the system, thus providing positive support to The Gambia from their facility in London.
Since every building is unique in its requirements, each client’s project needs its own bespoke control network: it’s never a clone of a BEMS from a previous job. Our in-house knowhow ensures that every one-off BEMS configuration we install is optimised around your investment and sustainability targets.
Powell Systems continue to be recognised in this growing field, winning accolades over the years. We work with you to lift your game in balancing cost equations involving design, installation, maintenance, and day-to-day operations against available technology, future proofing, or even change of purpose.
Get in touch, and take advantage of the decades of control systems experience that make Powell Systems one of the strongest players in the BEMS space. L
The trust runs Stepping Hill Hospital, as well as NHS services across Stockport.
The 22-page green plan sets out a commitment to protecting the environment, in its capacity as a large local organisation, as well as its capacity to look after and improve health for local people.
The plan holds the trust to targets to reduce its carbon emissions and their impact on the environment.
The foreword to the plan, by chair Professor Tony Warne and chief executive Karen James OBE states: “Stockport NHS Foundation Trust provides hospital care for children and adults across Stockport and the High Peak, as well as community health services across Stockport. We care about our patients and their families, the communities we
serve and the environment. We recognise the impact that our clinical activities have on climate change and are committed to the net zero ambitions of the NHS.

“Our Green Plan sets out our aims and commitment to improve the environment for our communities and become a sustainable healthcare provider. Through this plan, we will reduce our carbon emissions; reduce landfill waste and improve local air quality. Together, we will work with local partners to create a better environment for our patients and community.”
Stockport NHS Foundation Trust’s Green Plan runs in line with the Trust’s objective to support the health and wellbeing of the local communities and utilise resources in an efficient and effective manner. The Green Plan lists the progress and future actions required to reduce the Trust’s impact on the environment, while at the same time addressing the climate emergency.
The trust has an ambition for the emissions it controls to be net zero by 2040 and for an 80 per cent reduction compared to a 2012/13 baseline by 2032. For other emissions that the trust can influence, net zero should be reached by 2045, with an 80 per cent reduction by 2039. Steps that have already been taken include the introduction of four new electric vans, which are E
trustThehas an ambition for the emissions it controls to be net zero by 2040





transporting goods including prescriptions, post and pathology samples to and from the hospital. There are also new charge points for visitor and staff electric vehicles. There have also been new recycling stations installed around the hospital site.
The Trust Strategy 2020-2025 had as one of its five strategic objectives: “investing in our future by using our resources well” and the green plan is linked to this.
The NHS Delivering a net zero National Health Service has its own ambitions, including developing a low carbon organisation and workforce; reducing the carbon footprint; developing lower carbon care models; reducing local air pollution through sustainable transport; and reducing waste and moving to zero landfill.
Other NHS ambitions include reducing water use and including sustainable drainage solutions for new builds; lower carbon procurement and catering, including action to reduce single use plastics; and sustainable building design and climate change adaptation.
Stockport’s Green Plan has also taken these ambitions into account and the trust commits to: reduce greenhouse gas emissions by 80 per cent by 2032; a net zero carbon footprint by 2040; all trust vehicles to be ultra-low or zero emission; and a 75 per cent cut in business travel emissions by 2030. Other ambitions include zero waste to landfill; phasing out single use plastics in catering and purchasing to take account of social value weighting.
Recognising that they are the largest provider of healthcare and one of the largest employers in Stockport, the trust aims to reduce local air pollution by expanding low carbon models of care, investing in low carbon vehicles, encouraging lower carbon options for travel and minimising emissions from operations.
The trust also recognises that acute trusts are part of a wider system of health and care and must work together with others to deliver for local people. This includes nationally with the National Health Service, and locally with the Greater Manchester Integrated Care System and devolution project and ONE Stockport.
Achievements
In acknowledging the achievements so far, the trust has reduced its carbon footprint by 26.1 per cent since 2013 and waste output has reduced by 18 per cent.
To achieve this, projects have been implemented to reduce building energy, such as investing over £600,000 in LED lighting upgrades in 2019-2021; installing cost effective duplex stainless steel plate heat exchangers to improve energy efficiency and minimise waste water pollution and reducing mechanical ventilation by improving airflow and natural ventilation through the installation of new windows. Other measures include increasing insulation of roof spaces and exposed pipe work and valves; a boiler replacement programme; voltage optimisation; and use of an intelligent building management system to support heating control optimisation.

The trust also aims to reduce local air pollution, taking into account the size and
impact of its fleet. Plans are underway to replace current vehicles with an electric fleet. Recycling drop-off points and the separation of cardboard, scrap metals, furniture and electrical waste, and improvements to waste compactors, collection bins and holding areas, have contributed to improved recycling. Total waste tonnage has reduced from 1197 tonnes in 2012/13 to 981 tonnes in 2021 – a reduction of 18 per cent.
Single-use plastics have been removed from retail outlets and takeaway items are all recyclable.
Paul Featherstone, director of estates for Stockport NHS Foundation Trust said: “We are the second largest employer in Stockport, and we are committed to improving the health of our local population, both of which make tackling climate change and other environmental threats vital. Our new Green Plan sets out a very clear set of goals which we intend to meet so we can live up to this responsibility. We’ve already made a positive start, and we intend to build on these achievements in the coming years to make sure we’re looking after both the local and the global environment. ”
Stockport NHS Foundation Trust’s Green Plan is detailed, well thought out and well planned. It is likely that targeted implementation of this plan will reduce the waste and carbon emissions of the trust and therefore improve the lives of the local community and patient care. L
Total waste tonnage has reduced from 1197 tonnes in 2012/13 to 981 tonnes in 2021 – a reduction of 18 per cent
We are actively supporting the NHS decarbonisation programme and delivering lower cost energy for the healthcare sector
seeing a reduction of around 17,900m of raw water used annually by the old steam system.
Helping Rotherham NHS Foundation Trust save money and cut carbon emissions
Delivering energy management to hospitals since 1938, Veolia currently provides services that cover around 43,000 UK hospital beds and support the energy requirements for around 8.1 million inpatients each year, annually saving over 120,000 tonnes of CO2 emissions.
Veolia cuts carbon and energy costs for Eastbourne District General Hospital Healthcare buildings are energy hungry and energy supplied to the UK’s hospitals has become increasingly expensive which is why Veolia’s “Building a Zero Carbon Future” programme offers innovative solutions. A secure energy supply is essential to maintain a modern patient care environment for the hospital which has 457 beds and treats more than 470,000 patients per year. With energy consumption in hospitals growing steadily, the access to reliable and clean energy is important to ensure the delivery of essential healthcare services for disease prevention and treatment.
As the NHS is funded mainly through tax payers’ money, funding is limited. To meet this energy demand and achieve carbon and energy cost savings, we manage projects covering the design, delivery, and installation of a range of energy upgrades. These will guarantee the hospital meets the NHS carbon reduction targets for 2030 and is supported by a 24/7 operations and maintenance contract. The energy plant upgrades include desteaming the site, solar arrays giving a of 1.1MWp renewable electricity, improved ventilation systems, and a dual stage heat pump system to supply 3.2 MWth of low carbon heat with N+1 redundancy that gives system availability in the event of component failure. To ensure the heat is efficiently used, the project covers the fitting of insulated roofing, replacing older single glazed windows with high efficiency double glazing, and insulating cladding, along with insulated roofing.
Achieving big energy and carbon savings for Royal Berkshire Hospital
Veolia is now increasing energy savings at the Royal Berkshire Hospital in Reading following a 15-year extension to the existing contract. Royal Berkshire Hospital provides acute hospital services for over 500,000 people across Reading. To meet NHS targets of reducing its carbon footprint 80 per cent by 2032, and becoming zero carbon by 2040, the hospital needed to reduce energy use, while guaranteeing stable supplies of heat, electricity and hot water.
We worked closely with the hospital’s team to convert the site from steam to a Low Temperature Hot Water (LTHW) system to make big operational efficiencies. The system, installed in ten plant rooms across the site, consists of three LTHW hydrogenready boilers and associated 44 LTHW heat exchangers. We updated the hospital’s combined heat and power (CHP) heat rejection and recovery system, by replacing the steam waste heater boiler with a LTHW exhaust gas exchanger. The £8 million project is delivering immediate carbon savings. One significant improvement is a closed loop water system requiring minimal top up,
Veolia works with Rotherham NHS Foundation Trust to save money and cut their carbon emissions. By delivering a 20-year Energy Performance Contract (EPC) Veolia will achieve annual savings of over £1 million by implementing a wide range of improvements at the 500-bed Rotherham Hospital. The Trust’s commitment to maintaining a modern patient care environment for the 430,000 patients seen annually requires a secure, reliable, and cost-efficient energy supply. To achieve this goal whilst also reducing the carbon footprint, the Trust has embarked on an ambitious project that covers the design, delivery, installation, commissioning, and operation of a combined heat and power plant, replacement of seven 40-year-old boilers, and installation of a chiller plant for effective air conditioning. This includes upgrading the lighting system to take advantage of the latest low-energy and LED technology. The installation of 7,000 new fittings will not only improve lighting levels but also have a positive impact on patient treatment and outcomes. In addition to these measures, the project will also include insulation of pipes and valves and the installation of a battery energy storage system to further reduce energy consumption. Veolia, a leading provider of energy and waste management services, will guarantee these energy-saving measures and provide a comprehensive 20-year maintenance service. This partnership will ensure that the Trust continues to provide high-quality patient care while also reducing its environmental impact.
By investing in energy-efficient technology and partnering with Veolia, the Trust is taking a proactive approach to reducing its carbon footprint and ensuring a sustainable future for its patients. This project is an excellent example of how organisations can balance their commitment to providing quality services with their responsibility to protect the environment. L
FURTHER INFORMATION
veolia.co.uk

100% recycled and recyclable medical clothing made in the UK


Did you know, standard NHS scrubs are made using plastic sourced in Saudi Arabia, shipped to China to be manufactured using fossil fuels before behind shipped all the way to the UK?


This is extremely wasteful.
Upcycled Medical does things differently. We recover plastic from the ocean and landfill to create high-quality medical garments made right here in the UK.

1 set of scrubs = 30 plastic bottles (0.5kg of plastic waste)
We have the lowest verifiable carbon footprint in the world, and our zero-waste production process saves: Order
in CO2 emissions in water usage in energy 36% 34% 39%
NHS Providers recently published a report entitled: “No more sticking plasters: repairing and transforming the NHS estate”. HB investigates
The report examines the state of capital funding and allocations across the NHS provider sector. The report highlights the condition of the estate and argues for strategic capital investment at system and national level with the intention of driving productivity, improving patient care and enabling transformation across the NHS. The report begins: “Appropriate capital funding is needed to bring long neglected parts of the NHS estate into the 21st century for staff and patients. From fixing leaking roofs and broken boilers, to transforming estates to make them fully digitised and sustainable, and enhancing diagnostic capacity, capital investment has the potential to transform the NHS – improving patients’ experience and making it more efficient and effective.”
In 2021/22, NHS Providers spent 75 per cent of the Department of Health and Social Care’s (DHSC) capital budget,
In
which is used to finance capital investment in the NHS. Just over half of the capital expenditure is used for land and buildings and the rest is used for plant, equipment and transport, and information technology. The capital regime is split between operational capital covering day-today investments such as maintenance renewal and nationally allocated capital covering strategic projects like new hospitals and hospital upgrades. According to the report: “Following significant cuts in public spending, the NHS capital budget was raided between 2014/15 and 2018/19 as DHSC prioritised day-to-day spending at the expense of vital long-term investment. In the short term it was easier to cut investment than day-to-day spending.
During this period DHSC transferred £4.3bn from the capital budget into the revenue pot.” The report states that capital investment
across the NHS over the current Spending Review (SR) period (2022/23 - 2024/25) is expected to average £8 billion a year, compared to annual capital spending between 2010-19, which averaged £3 billion.


The report mentions “years of prolonged underinvestment in estates and facilities across the NHS” and concern around the capital maintenance backlog. The report claims: “the level of the maintenance backlog and the extent of dilapidated infrastructure ultimately reduces the ability of trusts to transform their estate and make vital productivity improvements.”
Since 2010/2011, the maintenance backlog has more than doubled and is now at £10.75 billion. This is how much needs to be invested to restore assets to a suitable working condition.
The total cost to eradicate the highest maintenance risk was £1.89 billion in 2021/22 – this is four times the 2013/14 level. On top of this, the proportion of the backlog which presents a high or significant risk has increased to 52 per cent. In this case, “high risk” means repairs which E
spentNHS2021/22,Providers 75 per cent of the Department of Health and Social Care’s (DHSC) capital budget
Fordingbridge are industry leaders in canopies and external builds designed to enhance healthcare and emergency service facilities throughout the year as weather protective solutions.



Maximise healthcare environments with a range of Fordingbridge canopy solutions offering excellent safeguarding measures, weather protection, and ensuring impressive canopy coverage, even in those seemingly inaccessible spaces.

We offer the design and build of:

• Bespoke canopies •
• Turnkey solutions •
• Optimised walkways •
• Sustainable buildings •
must be carried out urgently to “prevent catastrophic failure or major disruption to clinical services” and “significant risk refers to repairs which demand priority management and short-term spending”. However, the number of estates and facilities related safety incidents fell by over 40 per cent when compared to 2020/2021.
The report also points out the risk presented by reinforced autoclaved aerated concrete (RAAC) which was used for flat roof construction between the 1960s and the 1980s. The concrete was expected to have a lifespan of around 30 years, but some trusts have been using the materials for more than 50 years. 14 hospitals currently have RAAC planks, and they will need extensive building work to prevent their closure. Seven of these are at a critical level of risk, while only two of them are included in the New Hospital Programme.

The government has already committed to removing RAAC from the NHS estate by 2035 and has allocated £685 million to mitigate the risks.
The report claims: “There are major opportunities to transform the NHS estate to become more sustainable, efficient and digitised.”
Of course, a major talking point is that the NHS plans to become the world’s first net zero national health system.
Part of this plan means that the carbon footprint of emissions controlled by the NHS should be net zero by 2040. Major infrastructure projects like building new hospitals need to take this into account.
The report also points out that there are day-to-day changes that can be made to reduce the NHS’s carbon footprint. However, it continues: “major investment is required to improve energy efficiency across the NHS estate and enable trusts to reduce their carbon footprint.”
Funding has been announced to decarbonise the NHS, including via the Public Sector Decarbonisation Scheme operated by the Department of Business, Energy and Industrial Strategy (BEIS). There are already projects involving installation of air and ground source heat pumps; improving energy efficiency through double glazing, loft and cavity wall installation; installing LED lighting, and setting up solar panels to produce renewable electricity and some NHS trusts have already progressed on their net zero journey.
The report recommends that the government should continue to explore how the NHS can maximise values from land disposal, as well as how to use the wider estate more efficiently for the benefit of staff, patients and communities.
The report concludes: “This report has highlighted the significant and wide-ranging benefits of investment in health infrastructure. However, many parts of the NHS estate are in extremely poor condition. Trusts need major operational capital investment to drive substantial and long overdue improvements
to service capacity, increase productivity, improve the safety and experience of patients and staff, and to prevent the further deterioration of the NHS estate.”
The evidence shows that the NHS is in urgent need of repair, however, as the
report points out, this cannot be done without the investment to pay for it. M
FURTHER INFORMATION
Read the report here
Funding has been announced to decarbonise the NHS, including via the Public Sector Decarbonisation Scheme operated by the Department of Business, Energy and Industrial Strategy (BEIS)
Modern microbial threats such as Covid 19, Monkeypox , C. diff and C. auris demand a forwardthinking, future proof solution.

Hooper Services is proud to present EvaClean's PurTabs as a multi-purpose disinfectant to lead us safely into tomorrow!


Sodium Dichloro Isocyanurate (NaDCC) releases hydrochlorous acid (HOCl) in watera formulation with four times the antimicrobial killing power of bleach, but without the chemical exposure risks!

EPA registered to kill COVID-19, Monkeypox, TB, C. diff, C. auris and many other dangerous pathogens!
023 9263 0276
sales@hooperservices.co.uk




Unit A3, Mountbatten Business Park, Jackson Close, Farlington, Portsmouth PO6
Safe for surfaces, people and the environment, with the lowest toxicity rating, a neutral pH, and HMIS of 0/0/0.

EPA registered for electrostatic application! The only chemistry with no waiting time to reenter after spraying.
Continuously active disinfectant. Killing power for up to 24 hours!
We are more aware of infection control than ever before. Covid, flu, mpox, though below their peak, are still around and we can’t get complacent. Here are some top tips for infection control in your building

People visiting medical facilities, whether it be the hospital, GP or another location, are likely already ill or injured and therefore are more susceptible to infection. For this reason, it is important that healthcare facilities meet the highest standards of cleanliness and infection control.
Infections can increase the amount of time it takes for a patient to recover, or worse, and therefore increases pressure on the NHS.
Of course, regulations are in place on the prevention and control of infection. The Care Quality Commission states that all providers of healthcare and adult social
care should meet or exceed the Code of Practice on the prevention and control of infections and related guidance. The Code states: “Good infection prevention (including cleanliness) is essential to ensure that people who use health and social care services receive safe and effective care. Effective prevention and control of infection must be part of everyday practice and be applied consistently by everyone.
“Good management and organisational processes are crucial
to make sure that high standards of infection prevention (including cleanliness) are developed and maintained”.
First and foremost, all providers of health care should have an effective Infection Prevention and Control (IPC) policy, which is relevant to the location/specialism etc. The IPC policy should be regularly updated and available to all staff.
Cleaning contractors should have a general cleaning schedule, which includes the frequency of cleaning specific areas, fixtures and fittings. Of particular note here are items that are touched frequently, such as keyboards, telephones, door handles and light switches. The policy should also include the use of, training in and disposal of PPE. The government recently announced an E
All providers of health care should have an effectivePreventionInfection and Controlpolicy(IPC)





extension to the free provision of PPE for all health and social care workers for COVID-19 infection control. The scheme has been extended until 31 March 2024 or until the stocks for COVID-19 supply are depleted (whichever is sooner).
Disposal of clinical waste is an important area to consider. Bins should be easily accessible to staff and operated with a foot pedal. Waste should be assessed and separated properly. Medicine waste should also be stored in a designated bin and collected by an appropriate waste contractor and staff need to know which medicines to dispose of in each bin. Hand washing is highly important. Handwashing facilities must be available for all staff to adequately wash their hands in hot water using the correct technique. Liquid soap, paper towels and alcohol gel should be available.
It is important that staff are properly trained on infection control, this includes handwashing technique, use of disposable aprons and gloves, and recognising signs of infection.
Visitors
It is important for visitors to also contribute to infection prevention. Healthcare staff and cleaning teams can do everything right, but remember that visitors can bring in infection too and they are unlikely to know as much about it as those working in the environment. Educating visitors is very important and can help protect your patients and reduce infection in your area.
Clear signage should be displayed reminding people to wash their hands or use alcohol gel. In high-risk areas, for example, those visiting vulnerable patients, verbal instruction can be used to ensure every precaution is taken to reduce spread of infection. People may not be admitted to a high-risk area if they do not take infection control measures. Hand washing facilities and alcohol gel should be provided for visitors, whether patients coming in for an outpatient or other appointment or relatives visiting someone on a ward. Everyone in a healthcare facility (staff, patients and visitors) should wash their hands when they are visibly dirty, after using the toilet, after sneezing, after contact with body fluid, before and after handling food and when visiting patients with diarrhoea. Masks can also be provided and encouraged for visitors to reduce the spread of air-borne infections.
Patients in hospital can also be encouraged to remind their visitors to
help prevent infection, for example, asking people not to visit if they are unwell, asking them not to sit on the bed and trying not to have too many visitors.
When inviting patients for outpatient appointments, include details of your infection control measures. For example, you can remind people not to attend the appointment if they are showing signs of sickness that are not related to the reason they are attending. Relatives should not visit if they are ill – particularly if they are showing signs of diarrhoea and vomiting or flu.
Patients, visitors and staff can also make a report if they notice an area that is dirty.
Everyone is responsible for infection control in healthcare facilities to reduce the risk to patients and reduce pressure on the NHS. Therefore it is important that everyone has the education, training and means to be able to effectively act on infection prevention and control and ensure effective measures are taken and are in place. L

Patients in hospital can also be encouraged to remind their visitors to help prevent infection, for example, asking people not to visit if they are unwell, asking them not to sit on the bed and trying not to have too many visitors
The Security Event (TSE), the UK’s no.1 award-winning commercial, enterprise and domestic security event returns to the NEC Birmingham on 25-27 April 2023. This year’s event is set to bring even more exclusive products and launches of the latest security products and solutions from some of the biggest and best names in the security industry
Also on offer is 50+ hours of accredited CPD content providing a comprehensive overview of the changing security landscape, new measures and regulations, and the practical knowhow for security installations and protection of people, places and assets. Attendees will experience live product demonstrations to get hands-on with the most cutting edge technologies, and can enjoy a host of unrivalled networking opportunities across three spectacular days of innovation, collaboration and education.
The UK’s largest showcase of exhibitors and supporters Spearheaded and supported by an alliance of key global security brands, our founding partners — Anixer, Assa Abloy, Comelit, Honeywell, TDSI, Texecom, Tyco, Videcon — will be exhibiting some of their latest launches, products and projects which are set to revolutionise the sector and working practices. Event exclusives feature product showcases from leading security solution providers including: 3xLOGIC, AMAG Technology, Amalock, CAME, CIE, CQR, Dahuah, Deister Electronic, Dynamic CCTV, Fastlane, Fortus, Gallagher, Hanwha, Hikvision, Hytera, ICS Security Solutions, Pacom, Paxton, Quality Essential Distribution, Suprema, WEYTEC, ZK Teco, and many more. The show has grown exponentially since its launch, now covering an incredible 16,000+ sqm, with over 250 exhibitors offering
10,000+ products and solutions, and joined by over 10,000 security installers, integrators, consultants, and end users. Representing a 61 per cent increase of exhibitors from its last edition in 2022, over 100 exhibitors will be newcomers. With many exclusive brands on board, attendees will be able to find all the latest and innovative solutions under one roof.
The Security Event was developed with keen input from major industry players to deliver a world-class exhibition dedicated to support UK security professionals. Our broad range of recognised event sponsors continues this collaborative approach to constructing an inclusive platform that provides outstanding value to exhibitors and visitors alike. Providing an unmissable opportunity to speak directly to the industry experts, the knowledge sharing and insight on offer will be invaluable to thousands of organisations to ensure competency within their workforce and compliance within their business.
Brand-new for April 2023, Professional Security Officer Live will be launching at The Security Event. With security guarding proven to be one of the most effective measures to ensure the safety of people, property and assets, the show will recognise the vital

role of front-line security professionals. Covering all security guarding needs for industrial and construction sites, corporate offices, major live events, shopping centres, airports, and many more; discover the latest technology, equipment and innovations to equip security guards and officers.
Running alongside professional security Officer Live, visitors are invited to attend our new Professional Security Officer Conference geared towards the latest policies, evolving demands, high-risk environments and challenges facing security guarding today. Featuring pivotal keynote speakers, case studies and presentations, attendees will boost their working knowledge and keep up-to-date with crucial security guarding issues, regulations and guidance at this must-see conference.
New! Physical Security Zone and Live Security Testing
This exciting new zone will highlight the latest physical and perimeter security products and solutions and feature interactive demonstrations and workshops. Industry leaders will be on hand to give their expert advice and guidance on how to mitigate risk by deterring, delaying and detecting threats, intrusions or attacks. Keynote speakers and panellists will share their keen insights and experience on the latest trends and challenges in physical security.
In association with Element and supported by Secured by Design, Live Security Testing will also be taking place across the three days at 11am and 2pm. Attendees will experience first-hand how different physical security solutions perform in real-world scenarios to highlight their effectiveness at mitigating serious threat. From surveillance systems and access control systems, to intrusion detection and asset management and protection, industry-leading products from major vendors will be put to the test live, helping visitors make informed decisions in selecting the best products for their own security needs.
Designing Out Crime Zone, in association with Secured by Design
This specialised zone is dedicated to showcasing the latest innovative policing
techniques and solutions for reducing criminal activity and enhancing security in public spaces to keep local communities safe. Constructed in collaboration with Secured by Design and Police Crime Prevention Initiatives, this highly-specialised feature within The Security Event is a unique opportunity to explore best practice, deep dive into new methods and procedures for tackling crime in the community, and highlight the increasing risk of cyber threats on the public.
Attendees will gain insight into the latest research into successful crime prevention through carefully considered public space design that discourages criminal activity and promotes safety, and get hands-on with a range of products and technologies which can be integrated into the design of community areas to both prevent and detect acts against public security.
The Security in Practice conference is dedicated to providing security professionals with skills and knowledge for the protection of people and assets in today’s complex security environment. With a focus on providing practical, actionable information that security professionals can utilise in the day-to-day work, the conference will cover a broad programme of topics: risk management, incident response, physical security, cyber security and more.
A key emphasis for the conference is realworld case studies, with best practice shared by security professionals who have successfully implemented security measures in a range of settings, including government, corporate, private sector, and non-profit organisations. Attendees can learn from the achievements and challenges of their peers, and gain valuable insight into how to effectively apply security measures in their own organisations.
The Security Event 2023’s focussed seminar programme covers a range of topics crucial for security professionals to stay up-todate on, including cyber security, physical security, risk management and emergency preparedness. Led by industry experts and key players sharing vital knowledge and real-world experience, attendees will learn essential skills and foresight to stay current in their field, and ready and able to effectively protect their organisations from threat. With ever-evolving security regulation, guidance and law essential within the industry, The Security Event’s seminar programme will guarantee attendees abide to the highest industry standards, and apply new legislation and security requirements in their work.
content
Our education programme features the latest case studies, workshops and seminar sessions to keep you up-to-date with the latest issues and developments in security. Free-to-attend, our programme has been formally recognised as professional development where you can claim accredited CPD points with The Security
Institute. Members of Chartered Security Professionals (CSyPs) and Fellows (FSyl) or guests looking to top up their CPD points should take advantage of our outstanding accredited CPD offerings. For 2023, we have partnered with CPDMe who will be available onsite to facilitate collection of certificates of attendance and assist guests in building their CPD points portfolio.
Newly announced! Figen
Murray to share the Martyn’s Law - Protect Duty
On day one of the Security in Practice Conference, we will be joined by Figen Murray the mother of Martyn Hett, who at 29 years old was killed in the terrorist attack at the Manchester Arena in May 2017. Figen is the force behind Martyn’s Law, a proposed legislation that requires publicly accessible locations to bring in security measures against the threat of terrorism. Martyn’s Law will hopefully form part of the Protect Duty. Figen has also been presented with the Outstanding Contribution Award at the 2020 Counter Terror Awards for her efforts in stopping terrorism.
To meet the business needs of security professionals, The Security Event is bringing back CONNECT+ Live for another fantastic year of specialised networking. Matching the visitor’s buying requirements and needs with carefully curated exhibitors, the CONNECT+ Live team of matchmaking experts will fast-track access to key suppliers and integrators. Visitors can save valuable time and effort by making invaluable contacts through this outstanding and ever-popular hosted meeting programme.
The Security Event will feature countless opportunities to connect with new and

existing contacts, industry peers, business leaders and professional experts. Back by popular demand for 2023, The Security Event will host networking reception drinks at the end of each day of the show. Unwind and meet industry peers and professionals, enjoy a drink with friends and colleagues, and make those vital new connections in an informal and affable setting.
As a key part of The Safety & Security Series, The Security Event, alongside Professional Security Officer Live, will again be uniquely co-located with four other industry-leading events: The Fire Safety Event, The Health & Safety Event, The Workplace Event and National Cyber Security Show. With just one registration, attendees can cover the entire buying chain of the safety and security of people, property and assets. This series of shows is guaranteed the biggest of their kind in the UK, with over 33,000 SQM of total floor space, 800+ exhibitors, and one unmissable opportunity.
We also offer FREE PARKING for all visitors, saving you time and money, and giving you the flexibility to travel safely to and from the event across the full three days of the show. L
For more information and to register for your FREE pass visit
www.thesecurityevent.co.uk


The convenience of a mechanical key system plus the access permission and tracking capability of an electronic access control system come together with CyberLock. With a CyberLock system, it no longer matters where the lock is. Electronic access control is possible.






CyberKey: An electronically programmed key that overcomes the many limitations of a mechanical key. It can access a wide range of different locks, that can be individually time and date restricted. There is no limit on the quantity or design of CyberLocks the CyberKey can open. If lost – it can be disabled.
sales@sellox.co.uk
sellox.co.uk
+44 (0) 1273 741528


Locations covered: United Kingdom, Ireland, Switzerland, & Asia

T & T Global Recruitment Ltd was established and registered in the UK and in India in 2018. We have license and approval from the External Affairs Ministry, Government of India to recruit and supply Medical, Allied Health Care and other skilled professionals to the UK and other Countries in the world.



The UK Government has a Code of Practice (CoP) for NHS international recruitment that ensures hiring practices match the exceptional standard of healthcare the service provides. The CoP sets out how UK health and social care employers can ethically recruit from overseas and promotes high standards of ethical practice in the international recruitment and employment of health and social care personnel. T & T Global Recruitment has completed this portfolio and in this list.
T & T Global Recruitment has been recruiting for NHS and other Health Care settings (Nursing & Care Homes) in the UK and other Countries. We provide help and support to potential candidates a very comprehensive service throughout the recruitment process including professional body registration, English language test support, interview preparation, Visa service and pre departure support.
Our Services:
Study Abroad
Overseas Recruitment
Medical Tourism
Training & Development

The NHS must embrace the agency workforce. During this staffing crisis, recruitment agencies and temps are playing a crucial role in keeping wards open and the wheels of the NHS turning, writes Yerin Seo, senior campaigns advisor at the Recruitment and Employment Confederation
The pressure of working in frontline NHS and social care roles, especially within the context of the current staff shortages is well recognised by the public now. We have grown used to seeing images of striking nurses and doctors on TV, and the ensuing debates in parliament and the media. The high number of people out of work due to long-term illness and the long length of waiting lists are frequently in the news. The connection between a health service that isn’t equipped well enough to deal with patients quickly and people not being well enough to work is documented in ONS statistics. So we know the sector’s importance on our labour market and potential for economic growth. The high number of vacancies across the sector at all levels is a concern for patients. Our data shows vacancies for nurses and care workers average at around 80,000 to 100,000 each quarter. The likes of nursing assistants, public health managers and medical practitioners are also in high demand.
The UK’s world-class temporary workforce has come into its own to keep the heart of the NHS beating at a regular pace. The NHS and the care sector will always rely on contingent staffing because healthcare is unpredictable –this makes temps vital for patient safety. Temporary staff fill around 15,000 nursing, medical and related support role vacancies every quarter. At NHS England, an astonishing five million hours of shifts are supported by the contingent workforce each month. Despite the significant contribution they make, the way that agencies and agency workers are perceived by the public, media and politicians is often based on misconception and inaccuracy.
In England, the majority of recruitment agencies adhere to the rules and price caps set out within the NHS procurement frameworks – introduced and set in 2016. To be an ‘approved supplier’, agencies must go through a rigorous tender process. This is by no means an easy task, especially for SMEs. The bar is set high to ensure all suppliers maintain strong standards and compliance before they can supply workers to the NHS. This often includes evidence of historic activities and ISO (International Organization for Standardization) certificates. For example, during the tender process, agencies often E


classUK’sTheworld-temporary workforce has come into its own to keep the heart of the NHS beating at a regular pace



have to demonstrate that they have previously supplied workers to fill in particular roles, meeting ‘hours threshold’. This can be a challenge for many SMEs.
The small number of agencies that successfully jump all the hoops are awarded with contracts. And even after an agency makes it on to a framework, they are subject to a series of audits and strict terms and conditions. One of these terms is price caps, the maximum amount an agency can charge per hour for supplying a worker. In emergencies, agencies can go above this rate but that is not the norm on a framework. And the pay to an agency is broken down to cover a number of different things – it’s not all profit! The vast majority of the money goes to the worker, it’s their hard-earned wages, after all. Then there are things such as national insurance and employer’s pension contributions. At the end, the agency is left with a thin margin.
For example, to supply a healthcare assistant, agency fee on frameworks is capped at just over £2 out of an £18 hourly rate. And out of this margin, agencies pay a framework fee, train people, must meet strict compliance standards and pay for their 24/7 operation. In this scenario it is difficult to agree with the more prevalent narrative that agencies are making fortunes and taking the advantage of the staff shortages.
The REC has always encouraged its members to supply on framework. Being an REC member is even considered favourable as part of the tender process when getting onto an NHS framework in England and Wales. But a review into frameworks and price caps is a long overdue, as there has not been one since they started in 2016. We have had five different health secretaries in that time. With the lack of a review or an update, it’s increasingly difficult to meet the changing
demand of the sector and reflect economic influences such as inflation. And over time, the agencies going above and beyond to follow the rules have been squeezed. This is because the price caps have not changed despite inflation and the national minimum wage going up each year. This leads us to why some agencies supply off framework. There is a consistent narrative from NHS England and the Department for Health and Social Care (DHSC) that they want a reduction of agency spend. This combined with other factors means some NHS Trusts wait until the very last minute to turn to agencies for staffing support, at which point an off framework agency is often the only option. That is because no agency on a framework can supply within that tight timeframe while remaining within the price caps. Even as a worker, it is harder to reject a higher pay offer from an off framework agency if the same shift is being offered by an on framework agency for a significantly lower pay rate for the same exact job.
Combined with the financial difficulty and the growing number of off framework agencies, many small agencies have gone out of businesses over time, with others struggling. This means a smaller external staffing market for NHS England amid severe worker shortages. Recruitment agencies are an important part of solving worker shortages and getting a better workforce plan for the NHS. By thoroughly engaging and consulting
with them, the public sector can enjoy a procurement system that delivers value for money for taxpayers, efficiency and quality. The REC’s door remains open. We are ready to play our part in solving the difficult problem of healthcare staff shortages. The REC has been calling for a long-term workforce strategy for the sector for long time, so we welcome the news of its imminent publication from the DHSC. But without the expertise of recruitment and retention experts, a workforce strategy is unlikely to be effective. L
The REC is the voice of the recruitment industry, speaking up for great recruiters. We drive standards and empower recruitment businesses to build better futures for great candidates and themselves. We are champions of an industry which is fundamental to the strength of the UK economy.


FURTHER INFORMATION
Find out more about the Recruitment & Employment Confederation at www.rec.uk.com
Recruitment agencies are an important part of solving worker shortages and getting a better workforce plan for the NHS

We provide a variety of furnishings including lounge chairs, high back armchairs and more which are great for a wide range of users.


With our wide range of styles and colours we can help you create the right atmosphere for your care home without compromising on comfort or safety and all our upholstered furniture is available in a range of easy to clean and hygienic fabrics or faux leathers

Please browse to see our full range or contact our sales team to discuss your requirements further


Rosehill’s bestselling The Hamilton Patient & Visitor Chairs are a high quality and durable choice for your ward or waiting room. The chairs have a profiled seat for maximum comfort and an ergonomically designed back rest with a removable seat to help for easy cleaning. Optional extras include wheels, variable seat depth cushions to ensure the correct posture for multi-patient use, armpads and filled in sides. Order

With health sector vacancies at a record high, one NHS trust in Kent is battling back by offering more than 300 fully-paid apprenticeships, from nursing to administrators
Last year, 76 people enrolled onto apprenticeships at Kent Community Health NHS Foundation Trust (KCHFT). They joined an army of colleagues already on apprenticeship programmes, including registered nurses, nurse associates, physiotherapists, dental nurses, occupational therapists, business administrators and chartered managers.

Margaret Daly, deputy director of people and organisational development at KCHFT, said: “Apprenticeships provide an excellent way to earn, gain work experience and achieve nationally-recognised qualifications at the same time. They are not just for those starting a career, but also for those switching careers or wanting to further their learning and development.
“Over the past five years we’ve more than doubled the number of apprenticeships we offer, including 26 different programmes ranging from level two to level seven Master’s degrees. Our promise is to offer rewarding careers that attract, develop and retain talented people from all backgrounds.”
When physiotherapy apprentice, Paul Rothwell, 37 from Kings Hill, was made redundant from his design job, it sparked a complete career change.
“I spent seven years in design and sales when I was made redundant during lockdown. It was challenging at the time, but ultimately it set me back on a career
path I thought I’d left behind. It got me questioning what I would do if I could go back in time and choose a different degree. I would have chosen physiotherapy. I’d always been into fitness and exercise and I’d even qualified as a personal trainer, but it was always just a hobby.”
When a role came up at KCHFT for a therapy assistant at Tonbridge Cottage Hospital, Paul had the skills to successfully apply.
“I worked there for two years with the ambition of getting enough experience to apply for a physio apprenticeship as soon as it came up, which is exactly what I did.
It was tough though, having a unique career background meant I had to be really thorough in outlining my experience and skills. I was incredibly grateful to my manager who supported me through the application and interview stages.”
Paul will qualify as a physiotherapist in four years’ time on completion of his apprenticeship programme. E




Benefits to the team and the apprentice
Sheree Kempton is community hospital therapy lead at Tonbridge Cottage Hospital and is Paul’s manager. She says that having apprentices in the team is extremely valuable. “They are a real asset to the team and it gives the opportunity for senior therapists to share their knowledge and experience. One of the brilliant things about apprenticeships is you gain vital clinical experience throughout the course, not just while on placements.”
Unable to commit to a full-time university course, Lauren Shaba, 28, from Ashford, wasn’t sure how realistic her dream of becoming a nurse was until she saw the nursing degree apprenticeship opportunity at KCHFT and successfully applied.

Now in her final year of the fouryear programme, Lauren encourages others to consider an apprenticeship as a way of achieving their goals.
“My advice to anyone is to ask as many questions as possible. Having the option to work whilst studying allows you to develop the practical skills you need for your chosen profession while completing the qualification, which can only be a positive.”

Four years, ago James Page, 36, swapped a career in teaching to train as an occupational therapist. Now he’s almost fully qualified and has a job already waiting for him, thanks to an apprenticeship with KCHFT’s Clinical Academy.
As part of the programme, James had the opportunity to experience a split placement which involved the design and development of a wellbeing garden at the trust’s Heathside Centre in Coxheath.
“It was a really exciting project and the idea behind it was to provide OT students, like me, with innovative placements where we can put our learning into practice. I was involved in the initial research stage and was able to apply my occupational therapy skills to look at how people interact with their working environments to create a really fantastic wellbeing space for the trust and it’s service users too.”
Apprenticeships aren’t just for people starting a new career.
Passionate about supporting young people to be happy and healthy, Andy McKechnie swapped his role in teaching two years ago to join KCHFT’s East Sussex School Health Team as operations manager. Now he’s embracing new skills through a two-year Systems Thinking Apprenticeship to broaden his skills even further.
“I’m really interested in understanding how different systems work and the way in which people work together to improve outcomes. This course is really helping to develop my problem-solving skills and I’ve been really supported by my manager and team. It’s been great to be able to bring this new learning straight into practice.” Being a positive role model for her children and having more self-confidence are just two reasons why 37-year-old Hayley
Marcham, catering compliance manager at Tonbridge Cottage Hospital, is completing her second apprenticeship at the trust.
“It’s been so rewarding to develop new skills and it’s helped me understand what I’m capable of. As a result, I’ve had more confidence to push myself and take on new challenges at work.”
For Hayley, the chance to study for a degree in chartered management also offered an opportunity to achieve something outside of work.
“I really love my job in facilities, but the apprenticeship gives me time to focus on me and my personal development. It also has a really positive impact on my children. They’re immensely proud that their mummy works in the NHS and they think it’s brilliant that I’ve gone back to ‘school’.”
KCHFT is one of the largest NHS community health providers in England, serving a population of about 1.4 million across Kent and 600,000 in East Sussex and London. It employs more than 5,000 staff, including doctors, community nurses, physiotherapists, dietitians and many other healthcare professionals.
The trust provides wide-ranging NHS care for people in the community, in a range of settings including people’s own homes; nursing homes; health clinics; community hospitals; minor injury units and in mobile units. L
“It’s been so rewarding to develop new skills and it’s helped me understand what I’m capable of.”
AVer is dedicated to offering top-of-the-line cameras with patient-centred design and cutting-edge Artificial Intelligence, as well as optics and image processing technologies for the applications of Telehealth, Telemedicine, Tele-ICU, and OR Live Surgery Broadcast.

With over 20 years of research, development and manufacturing excellence, AVer is a proud recipient of numerous international design, innovation, application, and service awards centered on exceptional product usability, reliability and customer satisfaction, sustaining our market leadership position as a reflection of our drive to craft quality products and services.
Our easy-to-use, affordable and meaningful technology
solutions coupled with our unparalleled customer support and best warranty programs, enables you to accelerate learning in the classroom and increase competitive advantage for your business. Our product portfolio is deeply rooted in exceptional customer-centric product research and design, providing you intelligent solutions with excellent value. Spanning four separate continents with 15 international offices serving over 100 countries through 700 employees worldwide, our farreaching international presence and extensive network of reliable distribution channels continue to empower us to serve our customers on a global scale with unsurpassed service and dedicated support. L
INFORMATION TECHNOLOGY
4C Strategies is an independent ICT consultancy specialising in technology and infrastructure projects.

The company covers all aspects of technology and infrastructure in the enterprise environment, with consultants showing demonstrable experience in helping clients to procure new technologies to meet their business requirements, providing endto-end support on ICT projects by delivering a portfolio of consultancy services to meet client requirements, from audit and strategy through to procurement, implementation and resourcing.
4C Strategies has been assisting organisations in the healthcare industry for over 20 years. Expertise covers
all aspects of IT technology and infrastructure, including: digital strategy, IT and technology strategy, data centres, servers and storage, patient data security, desktop telephony, Microsoft Teams and wide area networks.
Trevor Nelms, Director from West London Mental Health Trust, said: “4C Strategies has assisted in a range of complex ICT projects, from inception through to deployment, and demonstrated a rare ability to bring together technical expertise with business acumen and tight project management skills.”
Contact one of 4C Strategies’ qualified healthcare technology consultants today. L
FURTHER INFORMATION
Tel: 01858 438938
nhs@4c.co.uk www.4c.co.uk


