




Dear managed care colleagues,
Welcome to our fall 2025 issue of the Prime Therapeutics Report! In this oncology issue, we focus on trends in oncology treatment and management. Prime Therapeutics is dedicated to bringing our readers valuable updates in managed care trends.
This issue’s cover story (Page 4) explores radiopharmaceuticals, specifically focusing on the rising utilization of these agents and payer management strategies.
Another article (Page 19) focuses on the application of cellular therapy in the treatment of solid tumors. With the first approval for a cellular therapy for solid tumor and a robust pipeline of other potential therapies, the treatment landscape is likely to shift.
In another article (Page 12), we discuss the rising incidence of cancer in younger populations as well as increased survivorship. These changes will require strategic planning from all stakeholders.
This issue also includes a discussion of prophylactic treatment with bispecific antibodies, an update on oncology accelerated approvals, and a brief multiple myeloma update. As always, we’ve rounded out this issue with the oncology pipeline.
To learn more about how we’re supporting transformative payer initiatives, please feel free to contact us at PTReport@PrimeTherapeutics.com. We value any feedback you may have. Enjoy the report!
Sincerely,

Steve Cutts, PharmD Senior Vice President, Specialty and Clinical Solutions Prime Therapeutics


Radiation therapy plays a pivotal role in cancer treatment. It can be delivered either externally or internally, each approach harnessing distinct mechanisms to target and destroy cancer cells.
The use of internal radiation therapy via administration of radiopharmaceuticals is beginning to disrupt the oncology armamentarium. These drugs, which contain radioactive isotopes, are gaining momentum due to their targeted delivery capabilities and technological advancements, which have led to clinical successes in recent years.1 They are categorized as diagnostic (90%), therapeutic (10%) or both.1 In oncology, diagnostic radiopharmaceuticals are used to detect and monitor cancerous lesions by targeted tumorspecific markers and enabling highresolution imaging through modalities such as positron emission tomography (PET). Therapeutic radiopharmaceuticals directly cause systematic, irreparable damage to targeted cells via local delivery of radionuclides to targeted lesions for the treatment of multiple cancer types.1
The new generation of radiopharmaceuticals use a targeting vector to accurately deliver radionuclides to lesions and avoid offtarget deposition.1 Ultimately, this makes it possible to improve the efficiency and biosafety of tumor diagnosis and therapy.1 Research has focused on novel radiopharmaceuticals that address a broad range of disease targets and have demonstrated remarkable in vivo performance.
Lutathera (indicated for gastroenteropancreatic neuroendocrine tumors) and Pluvicto (indicated for prostate cancer) have seen the greatest clinical success, especially compared to prior agents.
The new generation of radiopharmaceuticals use a targeting vector to accurately deliver radionuclides to lesions and avoid offtarget deposition.
adolescent patients with locally advanced/inoperable or metastatic somatostatin receptor (SSTR)positive GEPNETs or pheochromocytoma/paraganglioma (PPGL).4 The extrapolation of efficacy outcomes observed in NETTER1 also contributed to the approval.4
In NETTERP, safety was evaluated in nine pediatric patients, including four with GEPNETs.4 Absorbed radiation doses in target organs and incidence of adverse reactions after the first treatment cycle were the major outcome measures, in addition to shortterm adverse reactions. In NETTERP, the adverse reaction profile was similar to that observed in adults.4
The recommended pediatric Lutathera dose is 7.4 GBq




prostate cancer (mCRPC) who have been treated with androgen receptor (AR) pathway inhibition and taxanebased chemotherapy.5 On the same day, the FDA also approved gallium Ga 68 gozetotide (Locametz), a radioactive diagnostic agent for PET of PSMApositive lesions, including a selection of patients with metastatic prostate cancer for whom Pluvicto is indicated.5 This marked the first radioactive diagnostic agent approved for patient selection in the use of a radioligand therapeutic agent.5
Patient selection for Pluvicto treatment should use Locametz or another approved PSMA11 imaging agent based on PSMA expression in tumors.5 The randomized, multicenter, openlabel VISION trial evaluated the efficacy of Pluvicto plus best standard of care (BSoC) or BSoC alone in men with progressive PSMApositive mCRPC.6 All participants had received a GnRH analog or had prior bilateral orchiectomy and were required to have received at least one androgen receptor (AR) pathway inhibitor and one or two prior taxanebased chemotherapy regimens.6 Patients in the trial received Pluvicto 7.4 GMq (200 mCi) every six weeks for up to a total of six doses plus BSoC or BSoC alone.6 The primary end points of overall survival (OS) and radiographic progressionfree survival (rPFS) demonstrated statistically significant improvement.6 Median OS for the Pluvicto plus BSoC arm was 15.3 months compared to 11.3 months in the BSOC arm.6
Adverse reactions associated with Pluvicto were fatigue, dry mouth, nausea, anemia, decreased appetite and constipation.5,6 Laboratory abnormalities that worsened from baseline in at least more than 30% of patients receiving Pluvicto were decreased lymphocytes, hemoglobin, leukocytes, platelets, calcium and sodium.5,6
The recommended dose of Pluvicto is 7.4 GBq (200 mCi), intravenously, every six weeks for up to six doses, or until disease progression or unacceptable toxicity.5
In March 2025, the FDA expanded Pluvicto’s indication to include PSMApositive mCRPC in patients who have previously been treated with androgen receptor pathway inhibitor (ARPI) therapy and in whom it is considered appropriate to delay taxanebased chemotherapy.7
This label expansion was based on results from the Phase 3 PSMAfore trial.8 The trial randomized patients with PSMApositive mCRPC and progression on one ARPI, and whom were considered appropriate for delay of taxanebased chemotherapy, to receive Pluvicto (7.4 GBq p
[200 mCi] every six weeks for six doses) or a change in ARPI.8 In the Pluvicto arm, median radiographic PFS was 9.3 months compared to 5.6 months in the ARPI arm.8 Median OS was 24.5 months in the Pluvicto arm compared to 23.1 months in the ARPI arm. The safety profile was consistent with prior Pluvicto experience.8
Pluvicto continues to be evaluated in a growing number of clinical trials, including studies in earlier stages of prostate cancer, metastatic hormonesensitive disease, and in combination with other therapeutic modalities. Investigators are also exploring its potential in additional PSMAexpressing tumor types, which could broaden its clinical utility beyond prostate cancer. As evidence builds, Pluvicto is poised to play an increasingly central role in the evolving landscape of precision radioligand therapy.
In June 2025, the FDA approved a label expansion for gallium Ga68 gozetotide (Illuccix) to include patient selection for PSMAtargeted radioligand therapy (RLT) before taxanebased chemotherapy in men with mCRPC.9 Previously, Illuccix was approved for PET imaging of PSMApositive lesions in men with prostate cancer with suspected metastasis who are candidates for initial

89ZrDFOgirentuximab (Zircaix)
Tc99m generator
(Octevy)
fluciclovine (F 18) (Axumin) Blue
F18 (Neuraceq)
Therapeutic
lutetium Lu 177 dotatate Curium Pharma
lutetium Lu 177 zadavotide (LuPNT2002) POINT Biopharma; Lilly
lutetium Lu 177 edotreotide (177LuEdotreotide) ITM
lutetium Lu 177 zadavotide (Lu 177 PSMA I&T) Curium
actinium225 dotatate (RYZ101) RayzeBio; Bristol Myers Squibb
177Lu rosopatamab tetraxetan (TLX591)
212PbDotamtate (AlphaMedix)
I 131 iopofosine (CLR 131) Cellectar Biosciences
lutetium Lu 177 lilotomab (Betalutin)
rosopatamab (CONV01alpha)
(212PbPSV359)
(203PbPSV359)
Abbreviations:
= multiple myeloma;
photon emission computed tomography
definitive therapy, with suspected recurrence based on elevated PSA level, or for selection of patients with metastatic prostate cancer, for whom Pluvicto is indicated.9
In February 2025, the FDA accepted the Biologics License Application (BLA) for 89ZrDFOgirentuximab (Zircaix).10 If granted approval, this diagnostic radiopharmaceutical would become the first commercially available imaging agent to accurately and noninvasively diagnose and characterize clear cell renal cell carcinoma (ccRCC).10 Zircaix works by binding to carbonic anhydrase IX, a validated target protein on 95% of ccRCC cells, to produce images with high tumortobackground ratio and high intra and interreader consistency.10 The BLA’s acceptance was based on results from the Phase 3 ZIRCON study.10,11 Results from the study demonsrated a sensitivity of 86%, specificity of 87% and a positive predictive value of 93% for ccRCC.11
In 2023, the FDA reclassified radiopharmaceuticals from devices to drugs, paving the way for Pharmacy and Therapeutics Committee oversight and enabling 340b procurement.12 Then, in 2025, the Centers for Medicare & Medicaid Services (CMS) made changes to the reimbursement structure for diagnostic radiopharmaceuticals, which had historically been bundled into the cost of the imaging test.13 CMS now reimburses diagnostic radiopharmaceuticals separately when they exceed a perday cost of $630 in the hospital outpatient setting, potentially increasing use and equitable access.13 CMS will determine payment for qualifying radiopharmaceuticals based on mean unit cost data derived from claims and has left the door open to using average sales price data if manufacturers begin reporting it.14
With a changing diagnostic reimbursement structure as well as wholesale acquisition costs of currently approved therapeutic agents nearing $300,000 per therapy course, spend on radiopharmaceuticals is expected to rise. For instance, Pluvicto recorded $1.04 billion in sales in just the first nine months of 2024.15 According to forecasts, the global market is anticipated to grow at an impressive rate, potentially exceeding $13.67 billion by 2033.15
CMS now reimburses diagnostic radiopharmaceuticals separately when they exceed a per-day cost of $630 in the hospital outpatient setting, potentially increasing use and equitable access.
The expanding radiopharmaceutical pipeline presents a promising opportunity for improved patient care along with increased access to cuttingedge imaging, treatment options, personalized treatment and lower radiation exposure.16 There are, however, significant challenges. Projected growth has already resulted in increased demand for pharma service vendors and supply chains that are suited to ensuring timely availability and accessibility of these critical diagnostic and therapeutic medicines.17 Some bottleneck areas in the supply chain may include manufacturing capacity, stringent regulations, short halflives of radiopharmaceuticals, and the need for specialized expertise and infrastructure.17 This year will likely see continued and increased consolidation as companies move forward to secure supply chains and expertise.17
Radiopharmaceuticals are poised for broader adoption, driven by encouraging clinical outcomes, growing pharmaceutical investment in research and development, FDA reclassification of these agents as drugs and updated CMS reimbursement policies. Given the high cost for therapeutic radiopharmaceuticals, payers may want to prioritize management strategies, such as utilization management or prior authorization, to ensure appropriate patient access.
1. Zhang S, Wang X, Gao X, et al. Radiopharmaceuticals and their applications in medicine. Signal Transduct and Target Ther. 2025;10(1). doi: 10.1038/s41392024020416.
2. FDA approves lutetium Lu 177 dotatate for treatment of GEPNETS. U.S. Food and Drug Administration. Published January 26, 2018. Accessed August 21, 2025. https://www. fda.gov/drugs/resourcesinformationapproveddrugs/ fdaapproveslutetiumlu177dotatatetreatmentgepnets.
3. FDA approves lutetium Lu 177 dotatate for pediatric patients 12 years and older with GEPNETS. U.S. Food and Drug Administration. Published April 23, 2024. Accessed August 21, 2025. https://www.fda. gov/drugs/resourcesinformationapproveddrugs/ fdaapproveslutetiumlu177dotatatepediatricpatients12yearsandoldergepnets.
4. Singh S, Halperin D, Myrehaug S, et al. [177Lu]LuDOTATATE plus longacting octreotide versus high dose longacting octreotide for the treatment of newly diagnosed, advanced grade 2–3, welldifferentiated, gastroenteropancreatic neuroendocrine tumours (NETTER2): an openlabel, randomised, phase 3 study. Lancet. 2024;403(10446):2807–2817. doi: 10.1016/ S01406736(24)007013.
5. FDA approves Pluvicto for metastatic castrationresistant prostate cancer. U.S. Food and Drug Administration. Published March 23, 2022. Accessed August 21, 2025. https://www.fda.gov/drugs/ resourcesinformationapproveddrugs/fdaapprovespluvictometastaticcastrationresistantprostatecancer.
6. Sartor O, De Bono J, Chi KN, et al. Lutetium177–PSMA617 for metastatic castrationresistant prostate cancer. N Engl J Med. 2021;385(12):10911103. doi: 10.1056/nejmoa2107322.
7. FDA expands Pluvicto’s metastatic castrationresistant prostate cancer indication. U.S. Food And Drug Administration. Published March 28, 2025. Accessed August 21, 2025. https://www.fda.gov/ drugs/resourcesinformationapproveddrugs/ fdaexpandspluvictosmetastaticcastrationresistantprostatecancerindication.
8. Morris MJ, Castellano D, Herrmann K, et al. (2024, Dec. 21). 177LuPSMA617 versus a change of androgen receptor pathway inhibitor therapy for taxanenaïve patients with progressive metastatic castrationresistant prostate cancer (PSMAfore): a phase 3, randomised, controlled trial. Lancet. 2024;404(10459):1227–1239. thelancet.com/ journals/lancet/article/PIIS01406736(24)016532/ abstract.
9. Rddad Y. FDA expands use of radiopharmaceutical to PreTaxane setting for advanced prostate cancer. Oncology News Central. Published June 24, 2025. Accessed August 21, 2025. https://www.oncologynewscentral.com/drugs/ info/fdaexpandsuseofradiopharmaceuticaltopretaxanesettingforadvancedprostatecancer.
10. Rebbechi S. FDA accepts BLA for TLX250CDX (ZircAix®) for Kidney Cancer imaging, Grants Priority review. Telix Pharmaceuticals. Published February 26, 2025. Accessed August 21, 2025. https://telixpharma.com/newsviews/ fdaacceptsblafortlx250cdxzircaixforkidneycancerimaginggrantspriorityreview/.


Clint Williams, PharmD, MBA
VP, Small Group, Pharmacy and Ancillary Sales
Blue Cross and Blue Shield of Nebraska
A growing number of young people under age 50 are being diagnosed with more than a dozen forms of cancer worldwide.1 This disturbing trend is especially concerning among women. Statistics released earlier this year show that cancer incidence rates in women under age 50 are 82% higher than that of their male counterparts, up from 2002’s 51% difference.1
The number of people between the ages of 15 and 49 being diagnosed with serious cancers, including colorectal, breast, prostate, uterine, stomach and pancreatic, is increasing.1 According to one forecast, cancer incidence for this age group will increase by 30% globally from 2019 to 2030.1 Another analysis from 2004 showed individuals born between 1965 and 1980 have been experiencing larger percapita increases in the incidence of leading cancers combined than any prior generation born between 1908 and 1964.2
A 2025 assessment of cancer trends in incidence and mortality between 2010 and 2019 found 14 cancers had incidence rates that increased in the early onset group, which includes those diagnosed between ages 15 and 49.3 That group saw notable increases in melanoma, cervical, stomach, plasma cell, and bone and joint cancers.3 Some of these cancers — such as breast, colorectal, kidney, uterine and pancreatic — are also increasing in older adults; however, the sharp uptick among younger individuals has raised the greatest concern.3 These are cancers traditionally associated with older age, so their
emergence earlier in life is a shift.3 This assessment also showed a significant increase in total cancer incidence among women age 40 to 49.3 Women under age 50 are being diagnosed with lung cancer at higher rates than men in the same age group — a complete reversal of historical patterns.3
Strikingly, just four cancer types — female breast, colorectal, kidney and uterine — account for 80% of the estimated additional cases.3 This is a huge concentration of burden in a relatively small number of cancer types.3
The incidence and mortality of colorectal cancer is increasing in individuals age 30 to 49, which has already prompted a shift in screening guidelines, which now recommend starting at age 45. With earlyonset cases continuing to rise, further adjustments may be needed.3 The ATOMIC trial presented at the American Society of Clinical Oncology (ASCO) 2025 signals a new standard for dMMR disease, which is more common in earlyonset cases, raising upfront costs with the potential for longterm cost offsets and better quality of life.4
There are also alarming breast cancer trends in the youngest group: individuals age 15 to 29.3 Preventive screening still begins at 40, so cases in these younger cohorts are being caught late at more advanced stages,
The number of people between the ages of 15 and 49 being diagnosed with serious cancers, including colorectal, breast, prostate, uterine, stomach and pancreatic, is increasing.
when clinical symptoms appear.3 Thus, these cases often require more intensive and expensive treatment.3 On top of that, younger patients often face fragmented care. This is where oncology case management and digital tools can play a critical role in improving coordination and outcomes.3

Not only are cancer rates increasing, but these cases are appearing earlier, in more aggressive forms and in populations that require different care models.
Uterine cancer incidence and mortality are increasing across all earlyonset cohorts, and unlike breast and colorectal cancer, there is currently no preventative screening method.3 Although recent immunotherapy approvals are transforming treatment in this space, they’re also driving up costs.3 Integration and coverage of oncofertility counseling, which actually leads to lower longterm overall costs, is especially critical for these patients.3

Providing
Finally, kidney cancer is rising in adults age 30 to 49, while mortality is decreasing.3 This trend is closely linked to obesity rates and incidental detection through imaging.3 Because mortality is decreasing and patients are living longer, survivorship planning is especially important to ensure effective management of longterm health outcomes.3
Together, these cancers highlight the complexity of the challenge. Not only are cancer rates increasing, but these cases are appearing earlier, in more aggressive forms and in populations that require different care models.
Improvements in screening and diagnostic tools may be one contributing factor to the increase in cases. For example, breast tomosynthesis, which has enhanced the ability to detect breast cancer earlier, was introduced in 2011.3 More recently, updated recommendations for patients with dense breast tissue are helping catch cancers that might have been missed with traditional mammography.3 Similarly, colorectal cancer screening guidelines have been revised to start at age 45; this age may drop further as earlyonset cases continue to rise.3
Lifestyle factors are also likely playing a role. Rising obesity rates, sedentary behavior, Western dietary patterns and alcohol consumption have all been associated with increased cancer risk.3 In fact, obesity is a known risk factor for seven of the cancers with rising earlyonset incidence.3 Reproductive trends, including lower fertility rates and higher average age at first birth, may also contribute.3 These have been linked to increased risk for certain cancers, particularly breast and uterine.3
Genetics and epigenetics are almost certainly contributing factors. Inherited mutations like BRCA and Lynch syndrome are wellestablished risk factors.3 However, we now understand more about how earlylife exposures may lead to epigenetic changes that increase cancer susceptibility later in life.3
More survivors mean more people living longer with the physical, emotional and financial impacts of cancer, leading to longterm monitoring, more chronic care management and more pressure on health systems to support survivorship as a distinct phase of care. As previously mentioned, the longterm implications of cancer survival are uniquely challenging for the younger population.
The rise in earlyonset cancers means there will be a growing number of commercial and Medicaid members being diagnosed with cancer, which naturally drives up oncology spend. Paired with an aging Medicare population, the financial pressure on managed care will intensify.
Another key consideration is the evolution of cancer screening guidelines. Health plans will need to stay agile, adjusting coverage policies as recommendations shift and as new technologies, like multicancer early detection tests, gain approval from the U.S. Food and Drug Administration (FDA) and enter the market.
Early identification is where the real opportunity lies. Detecting cancer just one stage earlier can reduce treatment costs by about $50,000 per year and triple
$79,000
$272,000
Stage 1 Stage 2
Detecting cancer just one stage earlier can reduce treatment costs by about $50,000 per year and triple survival rates.
survival rates.1012 This reduction is a powerful case for investing in screening and early intervention — not just from a clinical perspective, but from a costcontainment perspective as well.
Figure 1 illustrates the cost of treating colon cancer at Stage I compared to Stage IV. The cost jumps from $79,000 to $279,000 — more than a threefold increase.12 The earlier cancer is detected and diagnosed, the better the outcomes and the lower the financial burden.
Ultimately, sustainable cancer care will require a proactive, datadriven approach — one that prioritizes prevention, early detection and personalized care strategies across all lines of business.
Treatment patterns and survivorship look different in younger populations. These patients are not typically part of routine screening programs, so they often present with more advanced disease, which can mean more aggressive, multimodal treatment.1012 This treatment pattern can increase clinical complexity and drive up the total cost of care.
There has also been a shift in how younger populations, who tend to be more proactive than their predecessors, engage with their care. They seek out clinical trials, innovative treatment centers and care environments that offer holistic support services and amenities. This can create opportunities and challenges alike for health plans and providers to meet these evolving needs and expectations.
Survivorship is a growing consideration, since younger patients tend to live longer after treatment, which means ongoing care costs and surveillance as well as managing potential recurrences.1012 Posttreatment management can give rise to some confusion between oncology and primary


Solutions like oncoprimary care that allow oncologists and primary care providers to collaborate on patient care are becoming more of a reality.
care providers around who owns this treatment, leading to uncoordinated and duplicative care, which is both costly and inefficient. Solutions like oncoprimary care that allow oncologists and primary care providers to collaborate on patient care are becoming more of a reality.1012
Payers may want to consider some strategies to approach this challenge. Early detection remains the most powerful tool, improving outcomes and significantly
reducing costs. Health plans can play a critical role by ensuring access to primary care, aligning screening policies with current guidelines and staying agile as those guidelines evolve. Automating screening reminders and tracking adherence is essential and can help close gaps. As new technologies such as multicancer early detection tests gain FDA approval, plans must be ready to evaluate and integrate them into their coverage policies. There has been some innovation in how screening is approached. Some health systems are now using artificial intelligence to scan patient data in their electronic health records to flag highrisk patients and recommend appropriate screening. Health plans can help support and scale this kind of proactive identification.
Patient support beyond diagnosis is critical. This support may mean access to clinical trials, oncofertility counseling and addressing social determinants of health that may be barriers to care.


Anja Shaughnessey, PharmD, PRS, RPh Director, Pharmacy Contracting & Strategy
Point32Health
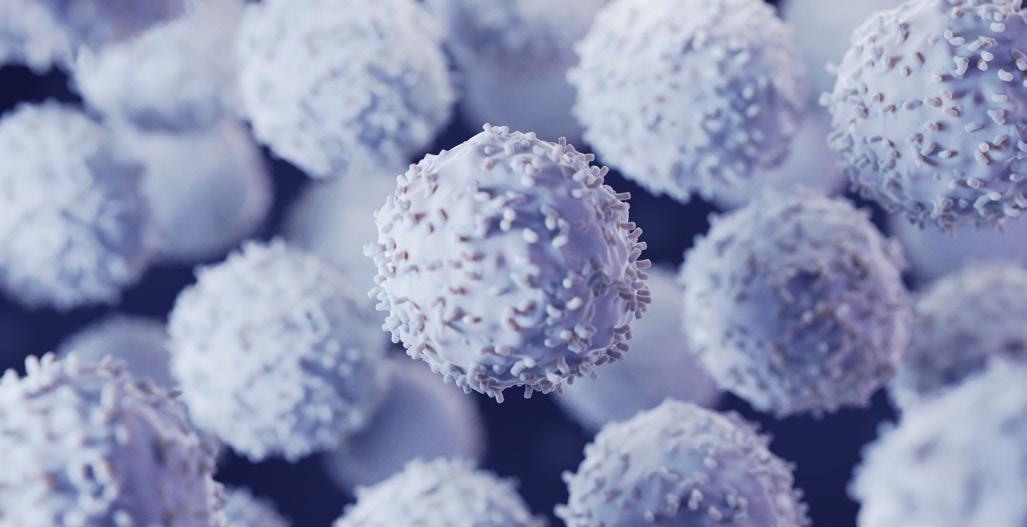
Cellular therapies will undoubtedly reshape the cancer treatment landscape in the coming years. A growth projection from market research firm Nova One Advisor estimates the U.S. CAR (chimeric antigen receptor) Tcell therapy market will surge from $2.45 billion in 2023 to $35.1 billion in 2033.1 More than 30,000 patients in the United States have received CAR Tcell therapy, and these treatments will likely become more accessible to more cancer patients with a wider range of cancer types in the future.2
With the first approval for cellular therapy for a solid tumor and ongoing studies for cellular therapies for different types of solid tumors, researchers have been working to maximize the effectiveness of cellular therapies in this context.
The most promising cellular therapy approaches for solid tumors are using pluripotent stem cells, cotargeting multiple mechanisms of immune evasion, employing multiple costimulatory domains and using CAR ligandtargeting vaccines.3
In February 2024, the U.S. Food and Drug Administration (FDA) granted lifileucel (Amtagvi) accelerated approval, making it the first cellular therapy to be approved for a solid tumor.4 Lifileucel is a tumorinfiltrating lymphocyte (TIL) therapy, the first to
reach the market. Similar to CAR T therapies, lifileucel is manufactured using immune cells from individual patients. To make the final product, a patient’s TIL cells are collected from a portion of their resected tumor and then expanded outside the body before being infused back into the patient.4
Lifileucel is indicated for the treatment of melanoma that has progressed after treatment with certain immunotherapy drugs or targeted therapies.4 Lifileucel’s safety and efficacy were evaluated in a global, multicenter, multicohort, openlabel, singlearm trial in patients with unresectable or metastatic melanoma who had previously been treated with at least one systemic therapy, including a programmed cell death 1 (PD1) blocking antibody and, if BRAF V600 mutationpositive, a BRAF inhibitor with or without a MEK inhibitor.5 Of the 89 patients who received lifileucel, two were excluded because the product did not meet specification, and five were excluded due to product comparability.5 The drug was administered following a lymphodepleting regimen consisting of cyclophosphamide 60 mg/kg daily with mesna for two days followed by fludarabine 25 mg/m2 daily for five days.5 Patients received interleukin2 (IL2), also called aldesleukin, 3 to 24 hours after infusion at 600,000 IU/kg every 8 to 12 hours for up to six doses in order to support
cell expansion in vivo.5 Objective response rate (ORR) and duration of response (DOR) were the main efficacy outcomes. Of the 73 subjects who received lifileucel within the recommended dosing range, ORR was 31.5% and median DOR was not reached.5
The recommended lifileucel dose is 7.5 x 109 to 72 x 109 viable cells.4 Lifileucel comes with a boxed warning for treatmentrelated mortality, prolonged severe cytopenia, severe infection, cardiopulmonary and renal impairment.4 Adverse reactions associated with lifileucel were chills, pyrexia, fatigue, tachycardia, diarrhea, febrile neutropenia, edema, rash hypotension, alopecia, infection, hypoxia and dyspnea.4
In a Phase I pilot study at Moffitt Cancer Center, 20 patients with nonsmall lung cancer (NSCLC) underwent tumor harvest for TIL generation prior to PD1 exposure, then received nivolumab for at least two months while their TILs were generated.6,7 Of those patients, 16 with
Iovance has gone on to open a dedicated
II lung TIL study, IOV-LUN-202 — the largest study of TIL for NSCLC to date.
progression or tumor growth across two scans while on nivolumab were treated with TILs in combination with lymphodepletion chemotherapy and IL2, followed by maintenance nivolumab.6,7 Three of 13 evaluable patients had a confirmed response, including two who had a complete response (CR).6,7 Of those treated with TILs, 11 had a reduction in tumor burden.6,7 Results of this early trial indicated some potential for TIL to achieve durable and meaningful responses in NSCLC.6,7
In the Phase II multicenter, multicohort TIL study, IOVCOM202 from Iovance Biotherapeutics, 28 patients in a cohort for advanced, prior immune checkpoint inhibitor (ICI)treated NSCLC treated with TIL therapy, six showed a response.6,8 All responders were previously treated with multiple lines of therapy, including both chemotherapy and PD1/PD1 ligand ICI therapy.6,8 Iovance has gone on to open a dedicated Phase II lung TIL study, IOVLUN202 — the largest study of TIL for NSCLC to date. The trial is designed for secondline therapy following a progression on firstline chemotherapy and antiPD1 therapy.6,9 In early results, the first 23 patients demonstrated a 26% ORR — one CR and five partial responses (PRs) — and a disease control rate of 82.6%.6,9 A patient death caused the trial to be placed on a partial clinical hold, which has since been lifted.6,10
A Phase II study of TIL therapy for HPVassociated epithelial cancers was conducted, including a cohort of 18 patients with cervical cancer whose tumors were positive for HPV 16 or HPV 18.6,11 Of the 18 patients, five patients responded, including two CRs, ongoing at 67 and 53 months after treatment, and three PRs lasting three months.6,11,12
In another ongoing Phase II multicenter trial from Iovance, C14504, TIL therapy was investigated in patients with ICInaïve advanced cervical cancer that had progressed after at least one prior line of chemotherapy.6,13 ORR was 44% in the 27 patients treated, with one CR, nine PRs and two unconfirmed PRs.6,13 Based on these results, the FDA granted Breakthrough Therapy designation status to expedite development of TIL therapy.6
Despite breast cancer being an unlikely target for TIL therapy, the National Cancer Institute conducted a Phase II study that included 42 patients with metastatic breast cancer refractory to prior therapy.6,14 TIL cultures were generated and selected for reactivity against unique neoantigens identified from the patient’s tumors. Of the 42 patients, 13 had at least one immunogenic somatic mutation identified in their TILs that met their threshold for reactivity to proceed with therapy.6,14 Of the six patients who underwent transfer of enriched neoantigenspecific TILs with pembrolizumab up to four doses, three responded, including one CR, ongoing for 5.5 years, and two PRs lasting six and 10 months.6,14
Cellular therapy for solid tumors is associated with major obstacles, challenges and limitations, including restricted trafficking and infiltration into the tumor site, hypoxic and immunosuppressive tumor microenvironment (TME), antigen escape and heterogeneity, CAR Tcell exhaustion, and severe lifethreatening toxicities.3 The design of these agents will need to surpass traditional architectures to overcome these challenges and broaden the applicability.3
There has been much work and research into addressing these limitations to enhance the safety, effectiveness and applicability of this treatment modality, including a wide variety of engineering strategies and integration of several therapeutic tactics.3
TIL therapy specifically comes with its own set of challenges and obstacles. Since TILs are made with cells from a patient’s own tumor, those who cannot undergo surgery or those without enough resected tumor tissue will not be eligible for treatment.15 The standard TIL approach presents challenges such as the limited number of tumor
Table 1. Novel TIL therapy in active clinical trials6
LYL845, TIL with stemlike qualities Melanoma; NSCLC; CRC
CD40Laugmented TIL EGFR, ALK, ROS1 and HER2genomically altered lung cancer
AGX148, TIL enriched for DP CD8 AGX148/P H762, TIL enriched for double positive CD8 TIL and with siRNA silencing of PD1
TBio4101, TIL selected for neoantigenreactivity
Neoantigenreactive TIL with CISH knockdown
Advanced solid tumors
A Phase 1 study to assess the safety and efficacy of LYL845 in adults with relapsed and/or refractory metastatic or locally advanced melanoma and selected solid tumor malignancies
Clinical trial of CD40Laugmented tumorinfiltrating lymphocytes (CD40L TIL) for patients with oncogenedriven advanced NSCLC (Phase I/II)
Phase 1 randomized openlabel trial investigating adoptive transfer of CD39+CD103+CD8+ tumorisolated T cells (AGX148) alone or combined with siRNA modulation of PD1 (AGX148/PH762) in patients with advanced solid tumors NCT05902520 (AgonOx)
Epigenetic reprogramming technology (EpiR)
Bcell stimulation with CD40L
Cell sorting of CD39+CD103+ (doublepositive) CD8+ T cells, PH762, a silencing RNA that reduces expression of the checkpoint inhibitor PD1
Advanced/metastatic breast carcinoma, CRC, uveal melanoma, cutaneous melanoma, NSCLC, head and neck squamous cell carcinoma
Metastatic gastrointestinal epithelial cancer
IOV4001, TIL with PDCD1 knockout Melanoma; NSCLC
ITIL306, antiFRa CoStaR engineered TILs
Ovarian, fallopian tube, peritoneal carcinomas; NSCLC; RCC
ATL001, clonal neoantigen Tcell product NSCLC
OBX115, IL15expressing TILs Melanoma; NSCLC
Phase 1b study of TBio4101 (autologous selected and expanded TIL) and pembrolizumab in patients with advanced solid tumor malignancies (STARLING)
Phase I/II trial in patients with metastatic gastrointestinal epithelial cancer administering tumorinfiltrating lymphocytes in which the gene encoding CISH was inactivated using CRISPR/Casti system
Phase 1/2, openlabel study of PD1 knockout tumorinfiltrating lymphocytes (IOV4001) in participants with unresectable or metastatic melanoma or Stage III or IV nonsmall cell lung cancer NCT 05361174
Phase 1a/1b, openlabel multicenter study evaluating the safety and feasibility of ITIL306 in subjects with advanced solid tumors NCT 05397093
Openlabel, multicenter Phase I/IIa study evaluating the safety and clinical activity of neoantigen reactive T cells in patients with advanced nonsmall cell lung cancer
TIDAL01, a process to enrich neoantigenreactive TILs
Inactivation of CISH using the CRISPR/Casti system
Transcription activator like effector endonuclease (TALEN) to knock out PDCD1, the gene encoding for PD1
Engineered costimulatory antigen receptor (CoStaR) with folate receptor a (FRa) scFv fused to CD28/CD40 signaling domain
Clonal neoantigen reactive T cells identified PELEUS bioinformatics platform
Membranebound IL15 engineered into TILs using viral transduction and is under the control of carbonicanhydrase 2 drugresponsive element TIL
Phase 1/2, openlabel study to investigate the safety and efficacy of membranebound IL15 expressing tumorinfiltrating lymphocytes (OBX115) in participants with unresectable or metastatic melanoma resistant to checkpoint
Abbreviations: CRC = colorectal cancer; CRISPR = clustered regularly interspaced short palindromic repeats; DP = double positive; EGFR = epidermal growth factor receptor; HER2 = human epidermal growth factor receptor 2; NSCLC = nonsmall cell lung cancer; PD1 = programmed cell death protein 1; RCC = renal cell cancer
reactive T cells; their inefficient engraftment, proliferation and effector function; and their dependence on cytokine IL2.6,15 Other challenges include highdose IL2 toxicity, complex manufacturing processes and immune evasion mechanisms.15 There are some emerging strategies to address these challenges and improve TIL therapeutic efficacy, including checkpoint inhibitor combinations, engineered TIL constructs and metabolic reprogramming.15
For cellular therapies to ultimately prove effective in the treatment of solid tumors, more research and innovation will be critical.
CAR Tcell therapy has demonstrated clinical success for hematologic cancers; however, it has shown significantly lower response rates and minimal complete responses for solid tumors.
The first and only approved cellular therapy for solid tumors, lifileucel, is priced at a wholesale acquisition cost of $515,000 per patient.1 Notably, this list price is slightly higher than existing cell therapies for blood cancers, which typically cost around $500,000 or less.1
For all cellular therapies, these price tags do not include additional costs such as hospital and professional charges and other treatments for underlying conditions while a patient waits for cellular therapy.1
Looking ahead at the evolving cellular therapy landscape, payers should determine how they can prepare for an influx of potential cellular therapy patients and identify strategies for managing these treatments.
An effective cost management approach to cellular therapy should consider all costs associated with care, including monitoring and additional care related to complications. Coverage criteria, reimbursement structures and contracting should be clear to ensure appropriate coverage and accessibility. Payer education about the appropriate population for cellular therapies will be key to ensuring coverage strategies take into consideration which patients are appropriate candidates for these therapies. Prior authorization processes can help determine the appropriate cell therapy, helping lead to more suitable options.

what’s
1. CAR Tcell therapy market size to hit USD 127.53 billion by 2033. BioSpace. Published July 22, 2024. Accessed August 21, 2025. https://www.biospace.com/cartcelltherapymarketsizetohitusd12753billionby2033.
2. Secondary cancers following CAR Tcell therapy are rare, Penn Medicine analysis shows. PennMedicine. Published February 7, 2024. Accessed August 21, 2025. https://beblog.seas.upenn.edu/ secondarycancersfollowingcartcelltherapyarerarepennmedicineanalysisshows.
3. Albelda SM. CAR Tcell therapy for patients with solid tumors: key lessons to learn and unlearn. Nat Rev Clin Oncol. 2023;21:47–66. doi: 10.1038 DP CD8/ s41571023008324 https://www.nature.com/articles/ s41571023008324.
4. FDA grants accelerated approval to lifileucel for unresectable or metastatic melanoma. U.S. Food and Drug Administration. Published February 16, 2024. Accessed August 21, 2025. https://www.fda.gov/ drugs/resourcesinformationapproveddrugs/ fdagrantsacceleratedapprovallifileucelunresectableormetastaticmelanoma.
5. Chesney J, Lewis CD, Kluger H, et al. Efficacy and safety of lifileucel, a onetime autologous tumorinfiltrating lymphocyte (TIL) cell therapy, in patients with advanced melanoma after progression on immune checkpoint inhibitors and targeted therapies: pooled analysis of consecutive cohorts of the C14401 study. J Immunother Cancer. 2022;10(12):e005755. doi: 10.1136/ jitc2022005755/.
6. Tseng D, Lee S. Tumorinfiltrating lymphocyte therapy: A new frontier. Transplant Cell Ther. 2025;31(3):S559–S609. doi: 10.1016/j.jtct.2024.11.014.
7. Choy A. New therapy for nonsmall cell lung cancer. SciWorthy. Published July 21, 2022. Accessed August 21, 2025. https://sciworthy.com/ newtherapyfornonsmallcelllungcancer/.
8. Thomas SS. TIL therapy in combination with pembrolizumab shows promise in patients with immunotherapynaïve, advanced melanoma. ASCO Daily News. Published May 31, 2024. Accessed August 21, 2025. https://dailynews.ascopubs.org/do/ tiltherapycombinationpembrolizumabshowspromisepatientsimmunotherapynaive.
9. Chesney JA, Schoenfeld AJ, WiseDraper T, et al. Trial in progress: A phase 2 multicenter study (IOVLUN202) of autologous tumorinfiltrating lymphocyte (TIL) cell therapy (LN145) in patients with metastatic nonsmall cell lung cancer (mNSCLC). American Association for Cancer Research Annual Meeting 2022. https://www.iovance. com/uploads/Chesney_IOVLUNTiPposter_AACR20221806publication.pdf.
10. Iovance Biotherapeutics announces FDA has lifted clinical hold on the IOVLUN202 registrational trial in nonsmall cell lung cancer. Iovance Biotherapeutics. Published March 4, 2024. Accessed August 21, 2025. https://www.globenewswire. com/newsrelease/2024/03/04/2839362/0/en/ IovanceBiotherapeuticsAnnouncesFDAhasLiftedClinicalHoldontheIOVLUN202RegistrationalTrialinNonSmallCellLungCancer.html.
11. Stevanovic S, Draper LM, Langhan MM, et al. Complete regression of metastatic cervical cancer after treatment with human papillomavirustargeted tumorinfiltrating T cells. J Clinical Oncol. 2015;33(14):1543–1550. doi: 10.1200/ JCO.2014.58.9093.
12. Stevanovic S, Helman SR, Wunderlich JR, et al. A phase II study of tumorinfiltrating lymphocyte therapy for human papillomavirusassociated epithelial cancers. Clin Cancer Res. 2019;25(5):1486–1493. doi: 10.1158/10780432. CCR182722.
13. Jazaeri AA, Zsiros E, Amaria RN, et al. Safety and efficacy of adoptive cell transfer using autologous tumor infiltrating lymphocytes (LN145) for treatment of recurrent, metastatic, or persistent cervical carcinoma. J Clin Oncol. 2019;37(15_suppl):2538. doi: 10.1200/ JCO.2019.37.15_suppl.2538.
14. Zacharakis N, Huq LM, Seitter SJ, et al. Breast cancers are immunogenic: immunologic analyses and a phase II pilot clinical trial using mutationreactive autologous lymphocytes. J Clin Oncol. 2022;40(16):1741–1754. doi: 10.1200?JCO.21.02170.
15. Chen R, Johnson J, Rezazadeh A, et al. (2025, Aug. 4). Tumourinfiltrating lymphocyte therapy landscape: prospects and challenges. BMJ Oncol. 2025;4(1):e000566. doi: 10.1136/bmjonc2024000566.


Simone Ndujiuba, PharmD, BCOP
Clinical Oncology
Pharmacist, Senior Principal
Prime Therapeutics
Bispecific antibodies (bsAbs) are used to enable novel mechanisms of action or therapeutic applications that could not be achieved using convention IgGbased (immunoglobulin Gbased) antibodies.1 They have two distinct binding domains that can bind to two antigens or two epitopes of the same antigen simultaneously.1 Unlike typical monoclonal antibodies that target one epitope, bsAbs target two antigens or epitopes, enabling them to cause multiple physiological or antitumor responses, which may be connected or independent from one another.1
Most indevelopment bsAbs aim to treat cancer, but others focus on chronic inflammatory, autoimmune and neurodegenerative diseases; vascular, ocular and hematologic disorders; and infections.1 There are currently 11 approved bsAbs with oncology indications.1
Teclistamabcqyv (Tecvayli) was the first BCMA (Bcell maturation antigen)directed bsAb approved for the treatment of relapsed and refractory multiple myeloma.2 The drug achieves deep and durable response rates; however, there are concerns regarding its acute toxicity profile, particularly the risk of cytokine release syndrome (CRS) and immune effector cellassociated neurotoxicity syndrome (ICANS).2 These concerns are not singular to teclistamab.2 CRS and ICANS are the two main adverse events of clinical interest associated with bispecific antibodies in general.3 CRS is an acute systemic inflammatory condition occurring in response to immune therapy that engages
There are currently 11 approved bsAbs with oncology indications.
T cells and/or other immune effector cells. It can occur within minutes to hours, with the median range across bsAb products approved by the U.S. Food and Drug Administration (FDA) being 5 to 48 hours. Mild CRS may present as fever, fatigue, headache, rash, diarrhea, arthralgia or myalgia. Patients with severe CRS may present with hypotension, peripheral/pulmonary edema, cardiac collapse or multiorgan failure. Severity is most commonly graded using scoring systems developed for grading CRS associated with CAR T therapy (Table 1).
In a retrospective study of patients with Bcell nonHodgkin lymphomas (BNHLs) treated with investigational or commercial bsAbs, CRS of any grade occurred in 57.1% of patients.3 By grade, 22.5% of patients experienced Grade 1 CRS, 32.1% experienced Grade 2 and 2.4% experienced Grade 3, with no instances of Grade 4 CRS.3 Notably, no difference in CRS risk was
demonstrated when assessing baseline demographics, bsAb drug, presence of bulky disease, ECOG, weight or BMI, baseline blood pressure, history of diabetes, use of granulocyte colonystimulating factor, and prior bendamustine exposure.3 In a multivariate analysis with histologic subtype, the association of bone marrow involvement of lymphoma and CRS risk had reduced significance.3 Ultimately, more research is required to effectively identify patients who are at high risk of CRS with bsAbs. The literature indicates that CRS associated with bsAbs is less severe.
Guidance regarding CRS management is limited and inconsistent. Guidelines from the Lymphoma Research Foundation Panel in 2024 recommend premedication with dexamethasone over other corticosteroids due to lower incidence of CRS. To treat Grade 2 or more severe CRS, the panel recommends dexamethasone with tocilizumab for refractory cases.4 The International Myeloma Working Group states that prophylactic use of tocilizumab has been evaluated to reduce the incidence of cytokine release syndrome and recommends tocilizumab for the treatment of Grade 1 CRS.5 According to guidelines from the National Comprehensive Cancer Network (NCCN), general recommendations are only available for management of CRS related to CAR T therapy.6 The NCCN guidelines state that tocilizumab may be considered

for CRS prophylaxis prior to the first dose of a bsAb for multiple myeloma, with a note that the guideline recommendations will be expanded in the future based on emerging clinical data and consensus opinion.6 Table 2 outlines some available consensus recommendations on managing toxicity associated with CD3xCD20 bsAb therapy.4
The FDA has approved tocilizumab (Actemra) for the treatment of Grades 3 and 4 CRS based on retrospective data.7 Recommended dosing is 8 mg/kg IV over one hour (not to exceed 800 mg per dose), repeated every eight hours if no improvement in signs or if symptoms of CRS are observed.7 The limit is a maximum of three doses in a 24hour period, with a maximum of four doses total.7 There are three approved biosimilars for tocilizumab, two of which are also approved for the treatment of CRS.
The MajesTEC1 trial was a Phase I/II trial evaluating the use of prophylactic tocilizumab to reduce CRS.8,9 Participants were patients with relapsing/refractory multiple myeloma who had been previously treated with at least three prior lines of therapy.8,9 A total of 24 patients received 8 mg/kg prophylactic tocilizumab administered
Get the latest report
Dive into award-winning GLP-1 research, pipeline trends, cost-saving solutions and more in this new strategy brief.
within four hours of the initial teclistamab stepup dose.8,9 In the prophylactic tocilizumab group, CRS incidence was 25% overall: 8.33% Grade 1, 16.67% Grade 2, and no Grade 3 or 4 events.8,9 In the nonprophylaxis group, CRS incidence was 72.1% — 50.3% Grade 1, 21.2% Grade 2 and 0.6% Grade 3 with no Grade 4 events.8,9 In both groups, all events resolved without teclistamab discontinuation.8,9
In the ongoing OPTec trial, tocilizumab use is evaluated with teclistamab, specifically in the outpatient setting with the goal of increasing access to community centers.10 As of the last data readout, 11 patients have completed the stepup dosing, and no patients have experienced CRS or ICANS or required hospitalization.10
In both trials, there was no alteration in oncology treatment efficacy when tocilizumab was used prophylactically.810
Another study investigated tocilizumab as prophylaxis for patients with multiple myeloma treated with bsAbs teclistamab, elranatamab, linvoseltamab or talquetamab.11 A single tocilizumab dose was administered to 119 patients prior to the first bsAbs dose.11 Results showed a low overall CRS rate, and the best overall response rate (ORR) was 65.7%. Individual CRS rates were 8.9% for teclistamab, 12.5% for elranatamab, 0% for linvoseltamab and 13% for talquetamab.11 For 10 of 12 CRS events, the grade was limited to 1, with the remainder at Grade 2.11 No CRS events Grade 3 or higher were observed. While the overall ICANS rate was low, it was similar to rates without prophylactic tocilizumab.11

Another study evaluated the safety of outpatient teclistamab initiation in subjects with tripleexposed relapsedrefractory multiple myeloma using prophylactic tocilizumab.2 On Day 1, before the first teclistamab dose, all patients received tocilizumab (8 mg/kg). Results showed that use of prophylactic tocilizumab reduced CRS incidence and severity of CRS with a low rate of admission.2 CRS occurred in two subjects, all Grade 1, and no ICANS cases were reported.2 These data support the use of prophylactic tocilizumab in the outpatient administration of teclistamab stepup dosing.2
Notably, while the CRS grade that occurred with prophylactic tocilizumab was low, CRS cases associated with teclistamab are similarly low grade.
Drug Manufacturer
3. Bispecific antibody: Oncology pipeline mosunetuzumabagxb (Lunsumio)
teclistamabcqyv (Tecvayli) Genmab; Johnson & Johnson
navicixizumab (OMP305B83) Mereo BioPharma; OncXerna Therapeutics
zanidatamabhrii (Ziihera) Zymeworks; Jazz Pharmaceuticals
elranatamabbcmm (Elrexfio) Pfizer
talquetamabtgvs (Talvey) Johnson & Johnson; Genmab
volrustomig (MEDI5752) AstraZeneca
rilvegostomig
(Imdelltra) Amgen
etentamig (TNB383B) TeneoBio; TeneoOne
petosemtamab (MCLA158) Merus
surovatamig (TNB486) TeneoBio; TeneoTwo
epcoritamabbysp (Epkinly) Genmab; AbbVie
amivantamabvmjw (Rybrevant) Janssen; Genmab
acasunlimab (BNT311) BioNTech; Genmab
BNT327 BioNTech; Biotheus
xaluritamig (AMG 509) Amgen; Xencor
blinatumomab (Blincyto) Amgen; Onyx Pharmaceuticals
Abbreviations:
Studies looking at dexamethasone as prophylaxis for CRS instead of tocilizumab have found dexamethasone to be just as effective as tocilizumab at a significantly lower price.
Studies looking at dexamethasone as prophylaxis for CRS instead of tocilizumab have found dexamethasone to be just as effective as tocilizumab at a significantly lower price.
In an evaluation of prophylactic dexamethasone in Cycle 1 of the EPCORE NHL1 Phase 2 trial of epcoritamabbysp (Epkinly) in relapsed/refractory follicular lymphoma, 49% of patients in the dexamethasone cohort experienced any grade CRS, 91% of which were Grade 1 and none of which were Grade 3 or 4.12
A retrospective study evaluated dexamethasone administered between stepup doses of talquetamabtgvs (Talvey) in 13 patients with relapsed/refractory multiple myeloma compared to 13 patients receiving standard of care prophylaxis.13 In that study, CRS occurred in 31% of patients receiving dexamethasone compared to 77% of those receiving standard of care.13 Treatment response remained high in the dexamethasone group, and infection and readmission rates were low.13
In a retrospective analysis of 242 patients with relapsing/ refractory multiple myeloma receiving teclistamab, 30 patients received dexamethasone, and 38 patients received tocilizumab for CRS treatment.14 Of those receiving dexamethasone, 42% experienced recurrent CRS after a subsequent teclistamab dose.14 Of those
receiving tocilizumab, 16% received recurrent CRS after a subsequent teclistamab dose.14 Both groups had a median of one dose and median duration of CRS of one day. Disease response was not affected by either CRS treatment modality.14
A study compared the use of outpatient stepup dosing using prophylactic dexamethasone compared to standard of care inpatient observation in patients with multiple myeloma treated with teclistamab or talquetamab.15 Patients in the outpatient arm were given prophylactic dexamethasone, 8 mg, on the day after each stepup dose of the bsAb.15 Recurrent CRS occurred in 32% and 46% of outpatient dexamethasone patients and standard of care patients, respectively.15
Ultimately, the study results showed that bsAb stepup dosing for multiple myeloma can be given safely in an outpatient setting.
CRS prophylaxis and/or treatment with either tocilizumab or dexamethasone do not negatively affect bsAb efficacy. It is important to consider that dexamethasone can be a costeffective option for CRS management at just over $1 per dose, compared to a dose of tocilizumab for a 75kg patient at over $2,500. Grade 1 CRS can often be effectively treated with just one dose of dexamethasone, and the utilization of dexamethasone for CRS management facilitates outpatient bsAb administration. While prophylaxis with tocilizumab is effective, a costbenefit analysis would need to be conducted to determine incremental value compared to dexamethasone.
Payers need to consider some factors when looking at management options for prophylactic tocilizumab. Generalizability is limited, as the studies included small cohorts, and prophylaxis was for only one dose. Prophylaxis may result in reduced need for CRS treatment. Notably, the price of tocilizumab could be as much as $4,700 for one dose. However, biosimilars will have more competitive pricing. More research and consensus around the appropriate population for CRS prophylaxis will help create appropriate strategy and management in this area. To identify candidates for prophylaxis, payers will need clear guidelines about which patients are at risk for highergrade CRS. Universal definition for potential risk factors is key.
1. Klein C, Brinkmann U, Reichert JM, et al. The present and future of bispecific antibodies for cancer therapy. Nat Rev Drug Discov. 2024;23:301–319. doi: 10.1038/ s41573024008966.
2. Jadot G, LeBlanc R, Ahmad I, et al. Tocilizumab prophylaxis for outpatient administration of teclistamab in relapsed/ refractory multiple myeloma. J Clin Oncol. 2025;43(16_ suppl): doi: 10.1200/JCO.2025.43.16_suppl.e19504.
3. Yang X, Ahmed I, Nachar V, et al. Risk factors for cytokine release syndrome in patients receiving bispecific antibodies for Bcell lymphoma: A singlecenter, retrospective cohort study. Blood. 2024;144(Supplement 1):4477. doi: 10.1182/blood2024211076.
4. Crombie JL, Graff T, Falchi L, et al. Consensus recommendations on the management of toxicity associated with CD3xCD20 bispecific antibody therapy. Blood. 2024;143(16): 1565–1575. doi: 10.1182/ blood.2023022432.
5. IMWG immunotherapy committee consensus guidelines and recommendations for optimal use of Tcellengaging bispecific antibodies in multiple myeloma. International Myeloma Foundation. Published May 2024. Accessed Aug. 21, 2025. https://www.myeloma.org/resourcelibrary/ imwgimmunotherapycommitteeconsensusguidelinesrecommendationsoptimaluset.
6. Thompson JA, et al. Management of immunotherapyrelated toxicities, version 2.2024 featured updates to the NCCN guidelines. J Natl Compr Canc Netw 2024;22(9):582–592. doi: 10.6004/jnccn.2024.0057.
7. FDA approves Genentech’s Actemra (tocilizumab) for the treatment of CAR T cellinduced cytokine release syndrome. PharmaLive. Published August 30, 2017. Accessed Aug. 21, 2025. https://www.pharmalive.com/ fdaapprovesgenentechsactemraforthetreatmentofcartcellinducedcytokinereleasesyndrome/.
8. Van de Donk NWCJ, et al. Longerterm followup of patients (pts) receiving prophylactic tocilizumab (toci) for the reduction of cytokine release syndrome (CRS) in the phase 1/2 MajesTEC1 study of teclistamab in relapsed/ refractory multiple myeloma (RRMM). 2024 ASCO Annual Meeting. Congress Hub. Published 2024. Accessed Aug. 21, 2025. https://www.congresshub.com/oncology/am2024/ teclistamab/donk#slides.
9. Martin TG, Mateos MV, Nooka A, et al. Detailed overview of
incidence and management of cytokine release syndrome observed with teclistamab in the MajesTEC1 study of patients with relapsed/refractory multiple myeloma. Cancer. 2023;129(13):2035–2046. doi: 10.1002/cncr.34756.
10. Rifkin R, Schade H, Simmons G, et al. Optec: A phase 2 study to evaluate outpatient stepup administration of teclistamab in patients with relapsed/refractory multiple myeloma (RRMM): Updated results. Blood. 2024;144(Supplement 1):4753. doi: 10.1182/ blood2024207295.
11. Kowalski A, Lykon J, Diamond BT, et al. Tocilizumab prophylaxis for patients with multiple myeloma treated with bispecific antibodies. Blood Adv. 2025. doi: 10.1182/ bloodadvances.2025019611.
12. Vose J, Vitolo U, Lugtenburg P, et al. EPCORE NHL1 follicular lymphoma (FL) cycle (C) 1 optimization (OPT) cohort: Expanding the clinical utility of epcoritamab in relapsed or refractory (R/R) FL. 2024 ASCO Annual Meeting I. J Clin Oncol. 2024;42(16_suppl):7015. doi: 10.1200/JCO.2024.42.16_suppl.7015.
13. Bag A and Shah MR. Exploring steroid prophylaxis to mitigate CRS: Enhancing access to bispecific antibodies in RRMM. 2025 ASCO Annual Meeting I. J Clin Oncol 2024;43(16_suppl):e1953. doi: 10.1200/JCO.2025.43.16_ suppl.e19537.
14. Davis JA, Snyder J, Rice Mikhaila, et al. Dexamethasone for the management of CRS related to teclistamab in patients with relapsed/refractory multiple myeloma. Blood Cancer J. 2024;15(1):32. doi: 10.1038/s4140802501222y.
15. Ferreri CJ, Knight M, Davis D, et al. Prophylactic dexamethasone (dex) with outpatient stepup dosing (SUD) of bispecific antibodies (BsAb) in multiple myeloma (MM) vs standard of care (SOC) inpatient observation. 2025 ASCO Annual Meeting I. J Clin Oncol. 2025;43(16_ supple):e19506. doi: 10.1200/JCO.2025.43.16_suppl.e19506.


Lindsay Speicher, JD Senior Project Manager, Specialty Prime Therapeutics
Approval through the U.S. Food and Drug Administration (FDA) accelerated approval pathway is conditional, and traditional approval depends on results from a required confirmatory trial verifying actual clinical benefit. Table 1 shows the new oncology drugs approved via the accelerated approval pathway since our fall 2024 update.1
The FDA grants traditional approvals to drugs that were previously approved via the accelerated approval pathway upon completion of a confirmatory trial demonstrating clinical benefit. Table 2 outlines the oncology accelerated approval drugs that have received traditional approval since our fall 2024 update.2
In April 2025, the FDA granted traditional approval to nivolumab with ipilimumab for the firstline treatment of adult patients with unresectable or metastatic hepatocellular carcinoma (HCC).3 Efficacy results from CheckMate 9DW, a randomized, openlabel trial of 668 adults with unresectable or metastatic HCC, informed the approval.3 Patients who had histologically confirmed HCC, ChildPugh Class A, ECOG performance status 0 or 1, and no prior systemic therapy for advanced disease were randomized to receive either nivolumab 1 mg/kg as an intravenous infusion with ipilimumab 3 mg/kg IV every three weeks for a maximum of four doses, followed by singleagent nivolumab 480 mg IV every four weeks, or investigator’s choice of lenvatinib or sorafenib.3
Table 1. Current oncology accelerated approvals awaiting traditional approval1
Drug Accelerated approval indication
zongertinib (Hernexeos)
dordaviprone (Modeyso)
sunvozertinib (Zegfrovy)
linvoseltamabgcpt (Lynozyfic)
datopotamab deruxtecandlnk (Datroway)
telisotuzumab vedotintllv (Emrelis)
avutometinib capsules; defactinib tablets (Avmapki Fakzynja CoPack)
Treatment of adult patients with unresectable or metastatic NSCLC whose tumors have HER2 (ERBB2) tyrosine kinase domainactivating mutations, as detected by an FDAapproved test, and who have received prior systemic therapy
Treatment of adult and pediatric patients 1 year of age or older with diffuse midline glioma harboring an H3 K27M mutation with progressive disease following prior therapy
Treatment of adult patients with locally advanced or metastatic NSCLC with EGFR exon 20 insertion mutations, as detected by an FDAapproved test
Treatment of adult patients with relapsed or refractory multiple myeloma who have received at least four prior lines of therapy, including a proteasome inhibitor, an immunomodulatory agent and an antiCD38 monoclonal antibody
Treatment of adult patients with locally advanced or metastatic, nonsquamous NSCLC with high cMet protein overexpression [>50% of tumor cells with strong (3+) staining], as determined by an FDAapproved test, who have received a prior systemic therapy
Treatment of adult patients with locally advanced or metastatic NSCLC with high cMet protein overexpression [>50% of tumor cells with strong (3+) staining)], as determined by an FDAapproved test, who have received a prior systemic therapy
Treatment of adult patients with KRASmutated recurrent LGSOC who have received prior systemic therapy
encorafenib (Braftovi) In combination with cetuximab and mFOLFOX6, for the treatment of patients with mCRC with a BRAF V600E mutation, as detected by an FDAapproved test
zenocutuzumabzbco (Bizengri)
zenocutuzumabzbco (Bizengri)
zanidatamabhrii (Ziihera)
Accelerated approval date Project completion
08/08/2025 11/30/2029
08/06/2025 07/31/2031
07/02/2025 07/31/2026
07/02/2025 06/30/2027
06/23/2025 11/30/2029
05/14/2025 06/30/2029
05/08/2025 06/30/2028
12/20/2024 05/31/2025
Treatment of adults with advanced unresectable or metastatic pancreatic adenocarcinoma harboring a NRG1 gene fusion with disease progression on or after prior systemic therapy 12/4/2024 08/31/2026
Treatment of adults with advanced unresectable or metastatic NSCLC harboring a NRG1 gene fusion with disease progression on or after prior systemic therapy 12/4/2024 08/31/2026
Treatment of adults with previously treated, unresectable or metastatic HER2+ (IHC 3+) BTC, as detected by an FDAapproved test 11/20/2024 09/30/2029
asciminib (Scemblix) Treatment of adult patients with newly diagnosed Ph+ CML in chronic phase 10/29/2024 06/30/2028
afamitresgene autoleucel (Tecelra)
Treatment of adults with unresectable or metastatic synovial sarcoma who have received prior chemotherapy, are HLAA+*02:01, A*02:02P, A*02:03Por A*02:06Ppositive and whose tumor expresses the MAGEA4 antigen as determined by FDAapproved or cleared companion diagnostic devices 08/02/2024 12/31/2025
Abbreviations: BTC = biliary tract cancer; EGFR = epidermal growth factor receptor; HER2 = human epidermal growth factor 2; HLAA = human leukocyte antigen A; IHC = immunohistochemistry; KRAS = Kirsten rat sarcoma virus; LGSOC = lowgrade serious ovarian cancer; MAGEA4 = melanomaassociated antigen 4; mCRC = metastatic colorectal cancer; NRG1 = neuregulin 1; NSCLC = nonsmall cell lung cancer; Ph+ CML = Philadelphia chromosomepositive chronic myeloid leukemia


Among all randomized patients, median overall survival (OS) was 23.7 months in the nivolumab plus ipilimumab arm compared to 20.6 months in the investigator’s choice arm.4 Overall response rate (ORR) was 36.1% and 13.2% in the nivolumab plus ipilimumab and investigator’s choice arms, respectively.4 Adverse reactions associated with nivolumab plus ipilimumab were rash, pruritus, fatigue and diarrhea.3
The recommended dose is 1 mg/kg of nivolumab with ipilimumab 3 mg/kg intravenously every three weeks or a maximum of four doses.3 This is followed by nivolumab 240 mg IV every two weeks or nivolumab 480 mg IV as a single agent every four weeks.3
Also in April 2025, the FDA granted traditional approval to nivolumab plus ipilimumab as a firstline treatment of adult and pediatric patients with unresectable or metastatic microsatellite instabilityhigh (MSIH) or mismatch repair deficient (dMMR) colorectal cancer (CRC).5 This approval was granted based on results from CheckMate 8HW, the largest Phase 3 trial of immunotherapy patients with MSIH/dMMR CRC.5 In the trial, nivolumab plus ipilimumab met the dual primary end points of progressionfree survival (PFS) compared to nivolumab monotherapy across all lines of therapy and to chemotherapy in the firstline setting.5
The FDA granted traditional approval to larotrectinib (Vitrakvi) in April 2025 for the treatment of adult and pediatric patients with solid tumors that: have a neurotrophic receptor tyrosine kinase (NTRK) gene fusion without a known acquired resistance mutation; are metastatic or where surgical resection is likely to result in severe morbidity; and have no satisfactory alternative treatments or that have progressed following treatment.6
First granted accelerated approval by the FDA in November 2018, larotrectinib has demonstrated clinically meaningful and durable responses across a range of NTRK fusionpositive solid tumors in the LOXOTRK14001, SCOUT and NAVIGATE confirmatory trials.6 The data analysis across these trials included pediatric and adult patients with unresectable or metastatic solid tumors with an NTRK gene fusion.6 Included patients were required to have progressed following systemic therapy for their disease or would have required surgery with significant morbidity for locally advanced disease.6 ORR and duration of response (DOR) were the major efficacy outcomes.6 In the pooled efficacy results, ORR was 60% with a complete response rate of 24% and a partial response rate of 36%.6 Of those with a complete response, 5% were pathological complete response.6 The median DOR was 43.3 months.6
Adverse events associated with larotrectinib, including laboratory abnormalities, were increased aspartate aminotransferase (AST) and alanine transaminase (ALT), anemia, hypoalbuminemia, musculoskeletal pain, leukopenia, lymphopenia, neutropenia, hypocalcemia, fatigue, vomiting, cough, constipation, pyrexia, diarrhea, nausea, abdominal pain, dizziness and rash.6 Reported serious adverse events included central nervous system problems, bone fractures and liver problems.6
In March 2025, the FDA granted traditional approval to pembrolizumab (Keytruda) with trastuzumab, fluoropyrimidine and platinumcontaining chemotherapy for the firstline treatment of adults with locally advanced unresectable or metastatic HER2positive gastric or gastroesophageal junction (GEJ) adenocarcinoma whose tumors express PDL1.7 The KEYNOTE811 multicenter, randomized, doubleblind, placebocontrolled trial evaluated efficacy in 698 patients with HER2positive advanced gastric or GEJ adenocarcinoma that had not previously been treated with systemic therapy for metastatic disease.8 Of the 698 participants, 85% had tumors expressing PDL1 with a CPS>1 using the PDL1 1HC 22C3 pharmDx kit.
All patients were randomized to either pembrolizumab 200 mg or placebo in combination with trastuzumab and either fluorouracil plus cisplatin or capecitabine plus oxaliplatin.8 There was a statistically significant improvement in OS and PFS in patients randomized to receive pembrolizumab in combination with trastuzumab and chemotherapy compared to placebo.8 For patients with tumors that were PDL1 CPS>1, the median PFS was 10.9 months and 7.3 months in the pembrolizumab and placebo arms, respectively.8 Median OS was 20.1 months in the pembrolizumab arm and 15.7 months in the placebo arm. ORR was 73% and 58% in the respective arms.8 Finally, median DOR was 11.3 months and 9.6 months in the respective arms.8
The FDA granted traditional approval to acalabrutinib (Calquence) with bendamustine and rituximab for adults with previously untreated mantle cell lymphoma (MCL) who are ineligible for autologous hematopoietic stem cell transplantation (HSCT).9 Acalabrutinib also received
The FDA granted traditional approval to acalabrutinib (Calquence) with bendamustine and rituximab for adults with previously untreated mantle cell lymphoma (MCL) who are ineligible for autologous hematopoietic stem cell transplantation (HSCT).
traditional approval as a single agent for adults with previously treated MCL.9
The ECHO trial evaluated efficacy in 598 patients with untreated MCL who were at least 65 years old and were not intended to receive HSCT.10 These patients were randomized 1:1 to receive acalabrutinib plus bendamustine and rituximab (acalabrutinib plus BR) or placebo plus BR. PFS was statistically significantly longer in the acalabrutinib arm compared to the placebo arm.10 Median PFS was 66.4 months in the acalabrutinib plus BR arm and 49.6 months in the placebo plus BR arm.10
Serious adverse reactions occurred in 69% of patients who received acalabrutinib plus BR, and fatal adverse reactions occurred in 12%.9,10 More than 2% of patients reported serious adverse reactions, including pneumonia, COVID19, pyrexia, second primary malignancy, rash, febrile neutropenia, atrial fibrillation, sepsis and anemia.9,10
The recommended acalabrutinib dose is 100 mg taken orally approximately every 12 hours until disease progression or unacceptable toxicity.9
In September 2024, the FDA granted full approval to selpercatinib (Retevmo) for adult and pediatric patients age 2 and older with advanced or metastatic medullary thyroid cancer (MTC) with a RET mutation, as detected by an FDAapproved test, who require systemic therapy.11 LIBRETTO531, a randomized, multicenter, openlabel study, evaluated selpercatinib’s efficacy.12 Adult and adolescent patients with advanced or metastatic RETmutant MTC were randomized 2:1 to receive either selpercatinib (160 mg twice daily) or physician’s choice of cabozantinib (140 mg once daily) or vandetanib (300 mg once daily).12 Patients randomized to the control arm were stratified based on RET mutation and intended treatment.12
While the selpercatinib arm did not achieve median PFS, the drug’s clinical benefit was supported by a prespecified analysis of patientreported comparative side effect impact.12 Patients in the selpercatinib arm reported less time with severe side effects than those who received physician’s choice.12 Adverse reactions associated with selpercatinib were hypertension, edema, dry mouth, fatigue and diarrhea. Common Grade 3 or 4 laboratory abnormalities associated with selpercatinib were decreased lymphocytes, increased alanine aminotransferase, decreased neutrophils, increased alkaline


phosphatase, increased blood creatinine, decreased calcium and increased aspartate aminotransferase.11
The recommended dose for pediatric patients is based on body surface area for patients age 2 to 11 and based on weight for those age 12 and older.11
In the event the confirmatory trial for an acceleratedapproval drug fails to demonstrate actual clinical benefit, the drug may be withdrawn from the market.
Since our last update, two drugs have been withdrawn from the market (see Table 3).13
Gilead voluntarily withdrew sacituzumab govitecanhziy (Trodelvy) from the market for urothelial cancer (UC) after a confirmatory study did not meet its primary end point.14 Results from the TROPiCS04 trial showed the treatment failed to improve OS in patients with metastatic UC (mUC), and a higher number of deaths from adverse events were noted in the Trodelvy arm than the group that received the physician’s choice treatment.14
Takeda withdrew mobocertinib (Exkivity) for adult patients with EGFR Exon 20 insertion mutationpositive locally advanced or metastatic NSCLC whose disease has progressed on or after platinumbased chemotherapy.15 The Phase 3 EXCLAIM2 confirmatory trial did not meet its primary end point, failing to fulfill the confirmatory data requirements of the accelerated approval granted by the FDA.15 The Phase 3 multicenter, openlabel study investigated the safety and efficacy of mobocertinib as a monotherapy versus platinumbased chemotherapy.15
In January 2025, the FDA issued a new draft guidance for accelerated approvals titled “Accelerated Approvals and Considerations for Determining Whether a Confirmatory Trial is Underway.”16 The FDA may require a study be underway prior to approval or be initiated
Table 2. Recent traditional approvals: Accelerated approval oncology drugs2
Drug
ipilimumab (Yervoy)
nivolumab (Opdivo)
larotrectinib (Vitrakvi)
nivolumab (Opdivo)
ipilimumab (Yervoy)
nivolumab (Opdivo)
pembrolizumab (Keytruda)
In combination with nivolumab, for the treatment of patients with HCC who have been previously treated with sorafenib 03/10/2020 04/11/2025
In combination with ipilimumab, for the treatment of patients with HCC who have been previously treated with sorafenib 03/10/2020 04/11/2025
Treatment of adult and pediatric patients with solid tumors that have a NTRK gene fusion without a known acquired resistance mutation; are metastatic or where surgical resection is likely to result in severe morbidity; and have no satisfactory alternative treatments or that have progressed following treatment 11/26/2018 04/09/2025
In combination with ipilimumab, is indicated for the treatment of adult and pediatric patients age 12 years and older with MSIH or dMMR mCRC that has progressed following treatment with fluoropyrimidine, oxaliplatin and irinotecan 07/10/2018 04/08/2025
In combination with nivolumab, is indicated for the treatment of adult and pediatric patients age 12 and older with MSIH or dMMR mCRC that has progressed following treatment with fluoropyrimidine, oxaliplatin and irinotecan 07/10/2018 04/08/2025
For the treatment of adult and pediatric patients age 12 and older with MSIH or dMMR mCRC that has progressed following treatment with a fluoropyrimidine, oxaliplatin and irinotecan
In combination with trastuzumab and fluoropyrimidine and platinumcontaining chemotherapy, for the firstline treatment of patients with locally advanced unresectable or metastatic HER2+ GEJ adenocarcinoma
07/31/2017 04/08/2025
05/05/2021 03/19/2025
acalabrutinib (Calquence) Treatment of adult patients with MCL who have received at least one prior therapy 10/31/2017 01/16/2025
selpercatinib (Retevmo) Adult and pediatric patients age 12 and older with advanced or metastatic RETmutant MTC who require systemic therapy 05/08/2020 09/27/2024
Abbreviations: dMMR = DNA mismatch repair deficient; GEJ = gastroesophageal junction; HCC = hepatocellular carcinoma; HER2 = human epidermal growth factor 2; MCL = mantle cell lymphoma; mCRC = metastatic colorectal cancer; MSIH = microsatellite instabilityhigh; MTC = medullary thyroid cancer; NTRK = neurotrophic receptor tyrosine kinase
Table 3. Withdrawn accelerated approvals13
sacituzumab govitecanhziy (Trodelvy)
mobocertinib (Exkivity)
Treatment of adult patients with locally advanced or metastatic NSCLC with EGFR exon 20 insertion mutations, as detected by an FDAapproved test, whose disease has progressed on or after platinumbased chemotherapy 09/15/2021 07/15/2024 Drug
Treatment of adult patients with locally advanced or mUC who have previously received a platinumcontaining chemotherapy and either PD1 or PDL1 inhibitor 04/13/2021 11/22/2024
Abbreviations: EGFR = epidermal growth factor receptor; mUC = metastatic urothelial cancer; NSCLC = nonsmall cell lung cancer; PD1 = programmed death receptor1; PDL1 = programmed deathligand 1
Gilead voluntarily withdrew sacituzumab govitecan-hziy (Trodelvy) from the market for urothelial cancer (UC) after a confirmatory study did not meet its primary end point.
within a specified time period after the date of approval.16 This guidance provided clarity regarding the FDA’s interpretation of whether a study is “underway” and policies for implementing this requirement.16
Since the accelerated approval pathway often relies on surrogate end points, concerns about the predictive value for clinical benefits remain.17 Of the new drugs that have received accelerated approval since the pathway’s inception in 1992, about 80% have been in oncology.17 Authors of a research letter published in the Journal of the American Medical Association noted that confirmatory trials for drugs that receive accelerated approvals should address clinical benefit more consistently to boost confidence in the safety and efficacy of products that receive accelerated approval.17 Further demonstrating this point, the European Society of Medical OncologyMagnitude of Clinical Benefit Scale assessed 102 cancer drug indications approved through the accelerated pathway from 1992 to 2022. The assessment concluded that only 12% of the pivotal trials were associated with substantial clinical benefit.18 Among the confirmatory trials, 44% and 40% demonstrated statistically significant improvements in overall survival and quality of life, respectively.18
Payer coverage and spending for treatments with unconfirmed clinical benefit can be challenging. Research suggests Medicare spending across 10 oncology drug indications that lacked clinical benefit rose to an estimated $569 million, of which $171 million
corresponded to voluntarily withdrawn indications, and $398 million corresponded to indications that were reevaluated by the FDA. These scenarios can cause payers to incur high costs for drugs that may eventually be withdrawn.
A recent data assessment of Tufts Medical Center’s Specialty Drug Evidence and Coverage Database, which includes coverage policies for specialty drugs at 18 large U.S. commercial health plans, evaluated coverage patterns for accelerated approval drugs.19 The results showed that 97% of policies provided some degree of coverage for accelerated approval drugs, and 89% of active coverage decisions were for oncology indications.19
Traditional approvals may help payers make more informed coverage and formulary decisions to effectively manage these therapies. Without concrete proof of clinical benefit, payers face challenges managing the costs associated with market withdrawals. Timely confirmatory results and verification of clinical benefit are critical to managing these accelerated approvals to improve outcomes and mitigate economic burden on payers.

1. Ongoing | Cancer accelerated approvals. U.S. Food and Drug Administration. Updated August 12, 2025. Accessed August 21, 2025. https://www.fda.gov/ drugs/resourcesinformationapproveddrugs/ ongoingcanceracceleratedapprovals.
2. Verified clinical benefit | Cancer accelerated approvals. U.S. Food and Drug Administration. Updated April 11, 2025. Accessed August 21, 2025. https://www.fda. gov/drugs/resourcesinformationapproveddrugs/ verifiedclinicalbenefitcanceracceleratedapprovals.
3. FDA approves nivolumab with ipilimumab for unresectable or metastatic hepatocellular carcinoma. U.S. Food and Drug Administration. Updated Apr. 11, 2025. Accessed August 21, 2025. https://www.fda. gov/drugs/resourcesinformationapproveddrugs/ fdaapprovesnivolumabipilimumabunresectableormetastatichepatocellularcarcinoma.
4. Yau T, Galle PR, Decaens T, et al. Nivolumab plus ipilimumab versus lenvatinib or sorafenib as firstline treatment for unresectable hepatocellular carcinoma (CheckMate 9DW): an openlabel, randomised, phase 3 trial. The Lancet. 2025;405(10492):1851–1864. https://www.thelancet. com/journals/lancet/article/PIIS01406736(25)004039/ fulltext.
5. U.S. Food and Drug Administration approves Opdivo® (nivolumab) plus Yervoy® (ipilimumab) as a treatment for patients with previously untreated microsatellite instabilityhigh or mismatch repair deficient unresectable or metastatic colorectal cancer. Bristol Myers Squibb. Published April 8, 2025. Accessed August 21, 2025. https:// news.bms.com/news/details/2025/US FoodandDrugAdministrationApprovesOpdivonivolumabplusYervoyipilimumabasaTreatmentforPatientswithPreviouslyUntreatedMicrosatelliteInstabilityHighorMismatchRepairDeficientUnresectableorMetastaticColorectalCancer1/default.aspx.
6. U.S. FDA grants full approval of VITRAKVI® (larotrectinib) for adult and pediatric patients with NTRK gene fusionpositive solid tumors. Bayer. Published April 10, 2025. Accessed August 21, 2025. Accessed August 21, 2025. https://www.bayer.com/en/us/newsstories/ approvalofvitrakvi.
7. FDA approves pembrolizumab for HER2 positive gastric or gastroesophageal junction adenocarcinoma expressing PDL1 (CPS>1). U.S. Food and Drug Administration. Published March 19, 2025. Accessed August 21, 2025. https://www.fda.gov/ drugs/resourcesinformationapproveddrugs/ fdaapprovespembrolizumabher2positivegastricorgastroesophagealjunctionadenocarcinoma.
8. Janjigian YY, Kawazoe AK, Bai Y, et al. Pembrolizumab plus trastuzumab and chemotherapy for HER2positive gastric or gastroesophageal junction adenocarcinoma: interim analyses from the phase 3 KEYNOTE811 randomised placebocontrolled trial. The Lancet 2025;402(10418):2197–2208. https://www.thelancet.com/ journals/lancet/article/PIIS01406736(23)020330/ abstract.
9. FDA approves acalabrutinib with bendamustine and rituximab for previously untreated mantle cell lymphoma. U.S. Food and Drug Administration. Published January 16, 2025. Accessed August 21, 2025. https://www.fda. gov/drugs/resourcesinformationapproveddrugs/ fdaapprovesacalabrutinibbendamustineandrituximabpreviouslyuntreatedmantlecelllymphoma.
10. Dreyling M, Mayer J, Belada D, et al. Highrisk subgroups and MRD: an updated analysis of the phase 3 ECHO trial of acalabrutinib with bendamustine/rituximab in previously untreated mantle cell lymphoma. Blood. 2024;144(Supplement 1):1626. doi: 10.1182/ blood2024200290.
11. FDA approves selpercatinib for medullary thyroid cancer with a RET mutation. U.S. Food and Drug Administration. Published September 30, 2025. Accessed August 21, 2025. https://www.fda.gov/drugs/ resourcesinformationapproveddrugs/fdaapprovesselpercatinibmedullarythyroidcancerretmutation.
12. Hadoux J, Elisei R, Brose MS, et al. Phase 3 trial of selpercatinib in advanced RETmutant medullary thyroid cancer. N Engl J Med. 2023;389(20):1851–1861. doi:10.1056/ NEJMoa2309719.
13. Withdrawn | Cancer accelerated approvals. U.S. Food and Drug Administration. Updated December 2, 2024. Accessed August 21, 2025. https://www.fda. gov/drugs/resourcesinformationapproveddrugs/ withdrawncanceracceleratedapprovals.
14. Armstrong A. Gilead withdraws ADC Trodelvy in bladder cancer after trial failure. Published October 18, 2024. Accessed August 21, 2025. Biospace. https://www. biospace.com/business/gileadwithdrawsadctrodelvyinbladdercanceraftertrialfailure.
15. Takeda provides updated on EXKIVITY® (mobocertinib).) Takeda. Published October 2, 2023. Accessed August 21, 2025. https://www. takeda.com/newsroom/newsreleases/2023/ takedaprovidesupdateonexkivitymobocertinib/.
16. Accelerated approval and considerations for determining whether a confirmatory trial is underway. U.S. Food and Drug Administration. Updated January 6, 2025. Accessed August 21, 2025. https://www.fda.gov/ regulatoryinformation/searchfdaguidancedocuments/ acceleratedapprovalandconsiderationsdeterminingwhetherconfirmatorytrialunderway.
17. McCormick B. Concerns persist over reliance on surrogate end points in FDA accelerated approvals. American Journal of Managed Care. Published July 14, 2025. Accessed August 21, 2025. https://www.ajmc.com/ view/concernspersistoverrelianceonsurrogateendpointsinfdaacceleratedapproval.
18. Jenei K, Booth CM. The delicate balancing act of accelerated approval for cancer medicines—speed, certainty, and benefit. JAMA Netw Open. 2025;8(3):E252040. doi: 10.1001/ jamanetworkopen.2025.2040.
19. LaMountain F, Beinfeld M, Chambers JD. Despite criticisms of accelerated approval pathway—commercial payers defer to FDA. Center for the Evaluation of Value and Risk in Health. Published March 14, 2024. Accessed August 21, 2025. https://cevr.tuftsmedicalcenter.org/news/ despitecriticismsofacceleratedapprovalpathwaycommercialpayersdefertofda.
Oncology spend is projected to reach $409 billion by 2028. You deserve a partner that can help you manage high-cost claimants, optimize site-of-care strategies and improve health outcomes.
Prime’s Insights+ platform and our expert clinical teams guide better decision-making and deliver scalable solutions tailored to your needs — no matter your market or member population.
Let’s reimagine cancer care together.
$3,413
average oncology drug claim cost for commercial plans
The high cost of cancer care is a big challenge...

...but Prime is ready to help.
98%
provider satisfaction rate — highest in the industry
EXPLORE OUR ONCOLOGY SOLUTIONS
Multiple myeloma is a blood cancer that affects the plasma cells found in bone marrow.1,2 These cells produce antibodies, which play a key role in helping the immune system fight off infection.1,2 Multiple myeloma causes these plasma cells to mutate and grow uncontrollably, producing an abnormal antibody called M protein.1,2 The multiplication of these cells causes a decrease in red blood cells, white blood cells and platelets, often leading to anemia, excessive bleeding and a compromised immune system.1,2 Multiple myeloma is associated with other complications, including bone damage, hypercalcemia and kidney damage.1,2
This cancer is relatively uncommon in the United States — a person’s lifetime risk of contracting multiple myeloma is 1 in 132 (0.76%).3 Novel agents have led to increased rates of deep, longlasting remission.2 However, because nearly all patients become resistant to therapy, multiple myeloma is considered an incurable disease. In 2025, there will be an estimated 36,110 new multiple myeloma cases with 12,030 expected deaths.3
In July 2025, the U.S. Food and Drug Administration (FDA) granted accelerated approval to linvoseltamabgcpt (Lynozyfic).4 Linvoseltamab is a bispecific Bcell maturation antigen (BCMA)directed CD3 Tcell engager for adults with relapsed or refractory multiple myeloma who have received at least four prior lines of therapy, including a proteasome inhibitor (PI), an immunomodulatory agent (IMiD) and an antiCD38 monoclonal antibody.4
Linvoseltamab’s efficacy was evaluated in the LINKERMM1 openlabel, multicenter, multicohort trial that included patients who had previously received at least three prior therapies, including a PI, an IMiD and an antiCD38 antibody.5 Patients with prior BCMAdirected bispecific antibody therapy, prior bispecific Tcell engaging therapy or prior BCMA CAR Tcell therapy were excluded.5 Results showed an objective response rate
In July 2025, the U.S. Food and Drug Administration (FDA) granted accelerated approval to linvoseltamab-gcpt (Lynozyfic).
(ORR) of 70%, and with a median followup of 11.3 months among responders, the estimated duration of response (DOR) was 89% at nine months and 72% at 12 months.5
Linvoseltamab comes with a boxed warning for lifethreatening cytokine release syndrome (CRS) and neurologic toxicity, including immune effector cellassociated neurotoxicity (ICANS).4 In the LINKERMM1 clinical trial, CRS occurred in 46% of patients, and neurologic toxicity, including ICANS, occurred in 54% of patients.4,5 Less than 1% of patients experienced Grade
3 CRS and 8% experienced Grade 3 or 4 neurologic toxicity.4,5 Due to these risks, linvoseltamab is available only through a restricted program under a Risk Evaluation and Mitigation Strategy (REMS).4
The recommended linvoseltamab dosage includes stepup doses of 5 mg, 25 mg and 200 mg, followed by 200 mg weekly for 10 doses, followed by 200 mg biweekly.4 The dosing frequency is decreased to 200 mg every four weeks in patients who have achieved and maintained a very good partial response or better at or after Week 24 and received at least 17 doses of 200 mg.4
In February 2025, the FDA approved generic lenalidomide capsules, indicated for the treatment of multiple myeloma, several other blood cancers and myelodysplastic syndrome (MDS), in multiple strengths.6 Starting in 2026, Amneal will be granted a license to manufacture and sell the product, referencing Revlimid.6 The generic is approved in strengths of 2.5 mg, 5 mg, 10 mg, 15 mg, 20 mg and 25 mg.6

In July 2025, the FDA announced it had extended the Biologics License Application (BLA) review period for belantamab mafodotin (Blenrep) combinations for the treatment of patients with relapsed or refractory multiple myeloma who have received at least one prior line of therapy.7 The new expected approval decision date in October 2025 provides the FDA time to review additional information.7
Results from the DREAMM7 and DREAMM8 Phase 3 trials supported the BLA.7 These trials evaluated efficacy of belantamab mafodotin combinations in relapsed or refractory multiple myeloma.7 There were statistically significant and clinically meaningful progressionfree survival results for belantamab mafodotin combinations
versus triplet standardofcare combinations in both trials.7 In DREAMM7, there was statistically significant and clinically meaningful overall survival compared to daratumumabbased triplet.7
Treatments for multiple myeloma can be very expensive, sometimes ranging from $200,000 to $500,000. Due to the high price tag, this area requires critical strategic planning for payers. Utilization management tends to be key in this category; “somewhat aggressive” to “very aggressive” utilization management has been reported by payers representing 64% of commercial lives as well as 74% of Medicare payers.8 Ultimately, management strategies will be critical to mitigating costs as the multiple myeloma treatment landscape becomes more complex and costly.
anitocabtagene autoleucel (KITE772)
arlocabtagene autoleucel (BMS986393)
Myers Squibb; Juno Therapeutics
zevorcabtagene autoleucel (CT053)
Other
belantamab mafodotin (Blenrep) GSK; Seagen
daratumumab; hyaluronidase (Darzalex Faspro)
Johnson & Johnson; Halozyme Therapeutics SC
iberdomide (CC220) Celgene; Bristol Myers Squibb Oral
mezigdomide (CC92480) Celgene; Bristol Myers Squibb Oral
etentamig (TNB383B) Teneobio; TeneoOne
vonsetamig (REGN5459) Regeneron
agent; antiBcell maturation antigen Pending (10/23/25)
AntiCD38 antibody; endoglycosidase Pending (3Q 2025) CRL (8/1/2025)
Cereblon E3 ligase modulator Phase 3
Cereblon E3 ligase modulator Phase 3
1. What is multiple myeloma? American Cancer Society. Updated February 28, 2025. Accessed August 21, 2025. https://www.cancer.org/cancer/multiplemyeloma/about/ whatismultiplemyeloma.html.
2. Understanding multiple myeloma. Multiple Myeloma Research Foundation. Accessed August 21, 2025. https:// themmrf.org/multiplemyeloma/.
3. Key statistics about multiple myeloma. American Cancer Society. Updated February 28, 2025. Accessed August 21, 2025. https://www.cancer.org/cancer/types/multiplemyeloma/about/keystatistics.html.
4. FDA grants accelerated approval to linvoseltamabgcpt for relapsed or refractory multiple myeloma. U.S. Food and Drug Administration. Updated July 2, 2025. Accessed August 21, 2025. https://www.fda. gov/drugs/resourcesinformationapproveddrugs/ fdagrantsacceleratedapprovallinvoseltamabgcptrelapsedorrefractorymultiplemyeloma.
5. Bumma N, Jagannath S, Lee HC, et al. Linvoseltamab for treatment of relapsed/refractory multiple myeloma. J Clin Oncol. 2024;47(22):2702–2712. doi: 10.1200/JCO.24.01008.
6. McNulty R. FDA approves generic lenalidomide capsules in multiple strengths. AJMC. Published February 19, 2025. Accessed August 21, 2025. https://www.ajmc.com/ view/fdaapprovesgenericlenalidomidecapsulesinmultiplestrengths.
7. GSK announces extension of US Food and Drug Administration review period for Blenrep (belantamab mafodotinblmf) in relapsed/refractory multiple myeloma. GSK. Published July 23, 2025. Accessed August 21, 2025. https://www.gsk.com/engb/media/pressreleases/ gskannouncesextensionofusfoodanddrugadministrationreviewperiodforblenrepbelantamabmafodotinblmfinrelapsedrefractorymultiplemyeloma/.
8. Changing payer management dynamics at play in oncology. MMIT Network. Updated April 18, 2024. Accessed August 22, 2025. https:// www.mmitnetwork.com/thoughtleadership/ changingpayermanagementdynamicsplayoncology/.
drug list
dasatinib (amorphous formulation) Xspray CML
lurbinectedin (Zepzelca)
(Blenrep)
(Revuforj)
cemiplimabrwlc (Libtayo) Regeneron
(extensivestage, firstline maintenance)
tafasitamabcxix (Monjuvi) Incyte MZL
durvalumab (Imfinzi) AstraZeneca
imlunestrant Lilly
sevabertinib Bayer
Gastric and gastroesophageal junction cancers (resectable, earlystage and locally advanced)
cancer (HR+, HER2)
NSCLC (advanced, ERBB2 mutations, prior systemic therapy)
pertuzumab (biosimilar to Genentech’s Perjeta) Organon; Henlius Breast cancer (HER2+)
tabelecleucel Pierre Fabre; Atara Biotherapeutics
cedazuridine/decitabine (Inqovi) Otsuka
vepdegestrant Arvinas; Pfizer
EpsteinBarr virusassociated posttransplant lymphoproliferative disease (age > 2)
AML (newly diagnosed, intensive induction ineligible, plus venetoclax)
Breast cancer (advanced or metastatic, HR+, HER2, ESR1mutated, secondline, monotherapy)
Abbreviations: AML = acute myeloid leukemia; BCG = Bacillus CalmetteGuerin; BLA = Biologics License Application; BPd = pomalidomide plus dexamethasone; BT = Breakthrough Therapy; BVd = bortezomib plus dexamethasone; CIS = carcinoma in situ; CML = chronic myeloid leukemia; ERBB2 = erythroblastic oncogene B2; ERT = endocrine receptor therapy; ESR1 = estrogen receptor 1; FT = Fast Track; HER2 = human epidermal growth factor receptor 2negative; HER2+ = human epidermal growth factor receptor 2positive; HR+ = hormone receptorpositive; MZL = marginal zone lymphoma; NDA = New Drug Application; NPM 1 = nucleophosmin 1; NSCLC = nonsmall cell lung cancer; OD = Orphan Drug; PR = Priority Review; R/R = relapsed or refractory; RTOR = RealTime Oncology Review; sBLA = supplemental Biologics License Application; SCLC = small cell lung cancer; sNDA = supplemental New Drug Application