
3 minute read
SIES 2023 – The Best So Far….
Karen Kempin Nurse Endoscopist/Nurse Practitioner Te Whatu Ora Hutt Hospital Endoscopy Unit Hutt Hospital, Lower Hutt, Wellington, karen.kempin@huttvalleydhb.org.nz
Financial Disclosures: Funding provided from NZGNC Education Grant to attend SIES.
Advertisement
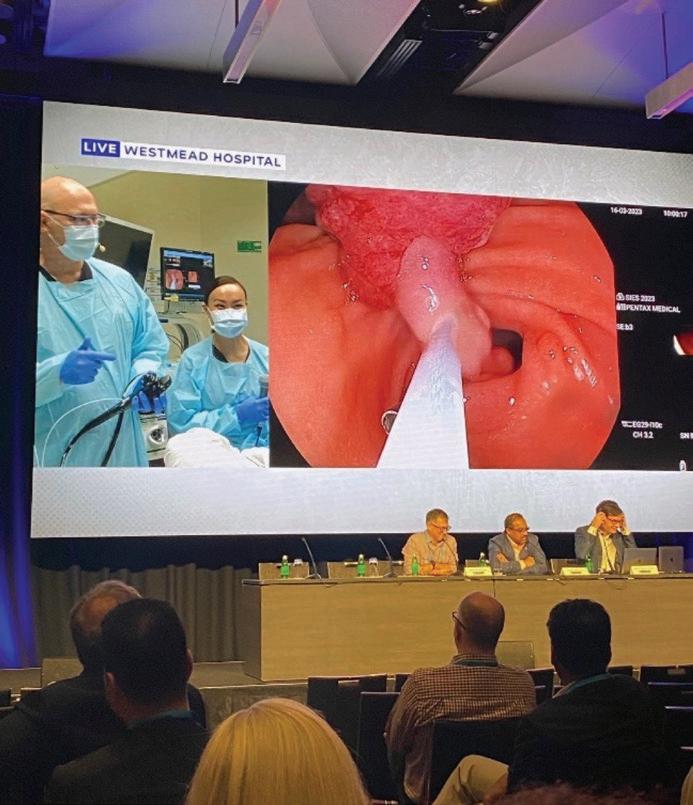
recognised experts in the field. This leads to some robust debates in the endoscopy room and the meeting space as contrasting opinions are voiced and challenged. The live sessions were bookended with didactic presentations of updated guidelines and new research findings, with experts presenting and adding to the content with real world experience. With an emphasis on therapeutic endoscopy the question could be asked, why should endoscopy nurses attend? The SIES Board recognises the team work needed for successful completion of endoscopy procedures and nurses attending have a concurrent program of didactic knowledge and hands on skills development in more advanced procedures like ERCP, haemostasis and perioperative nursing care of patients having complex therapeutic procedures. Often during the live cases there is a focus on the nurse role and equipment used, so there is a huge benefit for nurses to attend
Sydney International Endoscopy Symposium (SIES) started in 2008 as the Westmead Endoscopy meeting and has since evolved into an internationally recognised learning opportunity through using live endoscopy demonstrations of simple and complex procedures. The sudden COVID shutdown in March 2020 cancelled SIES days before their planned program and in 2021 and 2022 they gathered experts and pre-recorded procedures for the SIES Series of on-line evening seminars to keep the learning and skills development moving forward. So for 2023 they were very happy to announce they were back to a fully live program with around 650 health professionals and trade representatives gathered together in the same space, which did lead to some COVID transmission but this is the new normal that the world has to manage.
The SIES focus is on transfer of endoscopy skills but there is also an opportunity for live discussion of best practice points and contrasting viewpoints on how to manage the specific patient case from
As a nurse endoscopist my focus was on the live program but I took time to join the nurses program for a session from Elizabeth (Beth) Wardle giving updates in Infection Prevention and Control in Endoscopy including drying cabinets and flow of dirty equipment in relation to patients and clean equipment. One surprising point she made was that ASNZS 4197 was released almost 10 years ago (2014) and that work has commenced on the next version. While it is great to see the review has begun, it is important to note that New Zealand is included in this standard, with NZ experts on the review panel but many facilities here are still struggling to meet the environment and equipment standards that were mandated in 2014. Big ticket items like drying cabinets and physical works to redesign patient and equipment flows are still not prioritised as vital in New Zealand facilities, but this will come under scrutiny as the update to ASNZS 4187 develops. The Australian Commission on Safety and Quality in Health Care requires compliance by December 2024 with replacement of noncompliant equipment (automated reprocessors and drying cabinets), monitoring of final rinse water by testing, a plan for addressing clean and dirty reusable instrument segregation and design of storage of areas for sterile equipment. While New Zealand does not have a specific group to mandate and monitor these requirements, ASNZS 4187 is a legal document that needs acknowledgement and compliance.

From this year’s program I have made a few changes to my practice, even though I am not attempting EMR/ESD. I am taking more photos, with particular focus on before and after polypectomy. For small polyps with a cold snare I am trying to get a wider margin and irrigating the polypectomy site to flatten the mucosa and check the border for residual polyp tissue. For flatter lesions I am asking to use blue lifting solution more to get good views of the polyp margins to ensure complete resection. These are all small changes I can do within my current scope of endoscopy practice to reduce polyp recurrence for my patients.
On the social side, Sydney of course is a spectacular place to visit and I walked a few km’s each evening to the harbour and around the shops, keeping in mind my weight allowance for the flight home. Catching up with old Aussie friends was another pleasure that I have missed in the COVID restrictions. I would recommend endoscopy nurses attend SIES at least once to experience a program dedicated to showcasing current techniques and up to date best practice in therapeutic endoscopy.









