

LETTERS FROM LEADERSHIP

WOMEN’S HEALTH HEALTH JUSTICE
SPINE CARE
CELEBRATIONS CANCER CARE

BRAIN & BEHAVIORAL HEALTH









In all my years at NewYorkPresbyterian, healthcare has never looked more promising. Our doctors are saving lives in new ways that sound like something out of science fiction— breakthroughs that were impossible just a few years ago.
In this magazine, you’ll read about:
· Using ar tificial intelligence, data science, and predictive analytics to detect, prevent, and diagnose heart disease
· Revolutionizing care for women and their families by creating a new Center for Women’s Health in White Plains
· Building a new center for cancer care and ambulatory services—a quantum leap in treating and beating cancer for good
· Tackling America’s mental health crisis by bridging neuroscience and psychiatry and harnessing the power of AI
· Deploying augmented reality, robotics, and other technologies so that spine surgery patients can recover in days instead of weeks
To make these initiatives available to all, we’re weaving equity and health justice into all that we do. We’ve started by analyzing social determinants of health—race, level of education, socioeconomic status, and more— that shape the course of a patient’s life. With that information in hand, we’re giving each patient a fair chance.
Your generous support makes all this possible. On behalf of the patients, families, and everyone at NYP—thank you. I know we will accomplish even more in our next major fundraising campaign.
Together, we can build a better Hospital— and a better future for all.
 Steven J. Corwin, MD President and Chief Executive Officer NewYork-Presbyterian
Steven J. Corwin, MD President and Chief Executive Officer NewYork-Presbyterian

On behalf of the NewYorkPresbyterian trustees, thank you for being part of the NYP family.
I am thrilled to share some of the exciting work happening at NYP with our most loyal supporters. In these pages, you’ll find an interview with Jeanne Gang, one of the greatest living architects, who is designing the new cancer center in Washington Heights.
You’ll read about the technological advancements, clinical discoveries, and pioneering techniques the brilliant minds at NYP are coming up with every day. You’ll learn about how advanced imaging and navigation systems are helping our world-class spine surgeons and how digital tools are helping our psychiatrists deliver much-needed care to more patients. It’s amazing.
And none of these amazing things would be possible without you. Philanthropy is built on your compassion for the lives that will be lengthened and strengthened by what we do. We are grateful for every patient and family whose future will be brighter because of your generosity.

 Jerry Speyer Chair NewYork-Presbyterian Board of Trustees
Jerry Speyer Chair NewYork-Presbyterian Board of Trustees

It’s every cardiologist’s nightmare: A patient has a cardiac condition— and doesn’t get tested until the disease is in an advanced stage.
“Doctors often find themselves saying, ‘I wish I could have treated this patient sooner,’” says Pierre Elias, MD, who is the Medical Director for Artificial Intelligence at NYP, practicing cardiologist at Columbia University Irving Medical Center (CUIMC), and Assistant Professor of Cardiology at Columbia University Vagelos College of Physicians and Surgeons
(VP&S). “We can make a big difference if we can detect cardiac diseases earlier.”
That’s why NYP is leading the digital revolution in heart care in collaboration with our generous supporters and renowned Ivy League partners— Weill Cornell Medicine, VP&S, Cornell Tech, and Cornell Ann S. Bowers College of Computing and Information Science (Cornell Bowers CIS).
Together, we are developing game-changing technologies that use AI to make the prediction, prevention, diagnosis, and treatment of cardiovascular diseases more accurate, accessible, and effective than ever before.
At the CRADLE (Cardiovascular and Radiologic Deep Learning Environment) lab at VP&S, Dr. Elias and Tim Poterucha, MD, Assistant Professor of Medicine in Cardiology at VP&S, and Chris Haggerty, PhD, Director of Data Science at NYP, are leading the development of new ways to leverage deep learning technologies.
Their AI-powered project, called ValveNet, uses an algorithm to analyze every electrocardiogram test result at NYP.
If a patient is identified at high risk of valvular heart disease, their cardiologist can recommend a more comprehensive test to help diagnose undetected cases—before it’s too late. Dr. Elias and his collaborators are arming physicians with information that can nip deadly issues in the bud.
How? With AI, which can help clinicians make decisions by analyzing vast amounts of patient data and identifying subtle patterns that indicate disease.
The goal: to get to a diagnosis—and a cure—faster than ever.
“ We envision a future where physicians receive automated, patientspecific information and suggestions in real-time as they are speaking with their patients to help guide their care,” says Dr. Beecy. “Quickly and precisely tailoring care from one patient to the next is possible with AI.” “
Today, we are capturing more health data than ever and leveraging it to improve patient care more than ever,” says Dr. Elias.
When data scientists and physicians work together, they’re able to meld medicine and machine learning in exciting new ways.
Ashley Beecy, MD, Medical Director for Artificial Intelligence Operations at NYP—a practicing cardiologist at Weill Cornell Medicine as well as a former computer engineer and tech executive—is testing AI tools in disease prediction.
With the NYP Heart Transplantation Program led by Nir Uriel, MD, Director of Advanced Heart Failure and Cardiac Transplantation at NYP, Beecy’s team hopes AI tools in disease prediction will enable physicians to diagnose diseases like cardiomyopathy earlier.
Our doctors are reinventing heart care—and we’re just getting started. With the support of dedicated partners like you, our experts will continue to advance innovations for everyone who walks through our doors, enabling them to lead longer, fuller lives.

Her case was complex. She was nearing her due date—and had rheumatic heart disease, damaged heart valves, and placenta accreta spectrum, a rare condition that can cause fatal bleeding after delivery.
Shortly after her arrival at NewYork-Presbyterian/ Columbia University Irving Medical Center, she was put on temporary life support, and a multidisciplinary team of exceptional physicians took action.
Within a week, she had safely delivered her preterm baby and undergone a successful triple valve replacement surgery—a testament to NYP’s unparalleled care for the highest-risk pregnancies.
No single doctor can bring together all of the care a patient with a complicated case needs. At NYP, doctors connect across specialties, providing care that is as thorough as it is personalized. As we continue pushing the boundaries of what’s possible, your contributions enable our cuttingedge care for women in state-of-the-art facilities, equipping many of the world’s best specialists to work together for every person they treat. With your help, our patients can overcome health challenges with resilience.
Gynecologic surgery stands as a shining example of the innovative approach we hope to bring to a new scale. Women undergo gynecologic surgery for various reasons—including treatment of a condition like endometriosis, management of chronic pain, or to address fertility challenges—yet our goal is to offer all of them the same patientcentered care.
Dr. Arnold P. Advincula, Chief of Gynecologic Specialty Surgery at the Sloane Hospital for Women at NYP, is a world-renowned surgeon who has developed minimally invasive surgical instruments and techniques that offer superior patient outcomes, including faster recovery times.
“ There’s so much happening in the lives of the women we help,” says Dr. Advincula. “After receiving care at NYP, our patients can go back to their families and back to work more quickly with a significantly higher quality of life.”
Dr. Advincula has refined minimally invasive gynecologic procedures including the robotassisted laparoscopic hysterectomy, which removes a patient’s uterus through small

incisions, resulting in reduced blood loss, shorter hospital stays, and quicker recoveries.
Every day, teams across Columbia and Weill Cornell continue to explore new horizons as they layer on new technologies that are smarter and safer than ever before.
NYP has long led the way in women’s health—and now we are taking our commitment to a new level by unveiling a state-of-the-art Center for Women’s Health in White Plains, New York. This exceptional facility will offer access to a diverse range of specialized physicians, all at a single location.
“As soon as you set foot in the facility, it’ll feel like it exudes wellness,” says Dr. Advincula. “We’re creating a spa-like experience where many of our major subspecialties will have a presence, whether virtual or in-person. For those with limited time and fewer resources who live outside of New York City, it’ll take the stress away from needing to go into the city. Through this space, we’re bringing care to patients where they are, we’re giving them more
options to address their overall wellness, and we’re staying cutting-edge.
The spacious and serene facility will offer comfortable waiting areas and patient rooms, innovative operating and imaging spaces, and private rooms for telehealth and lactation. Abundant natural light and outdoor resting areas will further enhance the patient experience.
Your generosity enables us to harness the latest medical technologies and support our patients holistically, with well-being at the forefront of our priorities. The women’s healthcare of tomorrow is happening today at NYP—and our dedicated community of supporters is making it possible.
9 NewYork-Presbyterian
Above: NYP/Weill Cornell’s Ja Hyun Shin, MD, and Eloise Chapman-Davis, MD, are using minimally invasive gynecologic surgical approaches including advanced laparoscopic and robotic procedures to treat and help women recover faster.When architect Jeanne Gang sets out to design a building, she thinks about relationships: between the building and its surroundings, between the site’s history and its future, and between the natural and built environments. But most of all, she considers the relationship between the spaces within the building and the needs of the people who will use it.
The Chicago-based architect’s buildings— which span continents and have transformed landscapes—are, first and foremost, designed to improve the lives of those who interact with them.
So, when she set out to design NYP’s newest

center for cancer care and other critical ambulatory services, part of the Columbia University Irving Medical Center campus at West 165th Street and Fort Washington Avenue, she found unique inspiration.
“It ’s a storied hospital and very famous for its excellent care. It’s such an important part of New York,” Gang says. “That was a really great starting point.”
She and her team at the architecture and urban design practice Studio Gang have been tapped for projects ranging from towering skyscrapers to intimate community centers. But the patient care center was the team’s first foray into healthcare.
Gang felt a natural connection with NYP.
“I had always been interested in places that are about healing. And in many ways, a lot of our work is about healing with communities,” Gang says. “But I never thought I would have an opportunity to work on something like this and with an organization that provides such a high quality of care.”
Working with Gang and her trailblazing team, which included close collaboration with Ballinger as medical architect and interior designer, NYP is designing a first-of-its-kind facility that will set a new standard and transform the healthcare experience for all—putting patients and the community at the center of everything.
Located in one of the most diverse neighborhoods in the country, the new building’s expanded capabilities will increase patient access to preventative screenings and clinical trials, furthering NYP’s health equity mission.
You’ve likely interacted with Gang’s work before at the Richard Gilder Center for Science, Education, and Innovation, the American Museum of Natural History’s new wing, whose undulating curves were informed by the way natural forces like wind and water erode geologies, creating porous and often intriguing formations.
Then there’s the Solar Carve Tower at 40 Tenth Avenue in Manhattan, a building with geometric glass panels that are sculpted to allow more sunlight to reach people as they stroll along the High Line.
In Brownsville, Brooklyn, a firehouse intermixes form and function to allow for in-house trainings and spaces where rescue workers can recharge while keeping close to their community.
NYP’s newest patient care center has been conceived with the same care and thought.
“Hospitals can be intimidating,” Gang says. “This one will feel much more accessible and calming.”
Typically, patients at facilities that treat cancer and other critical illnesses—often feeling ill and tired—have to travel from floor to floor, building
to building, and throughout the city for various parts of their treatment. This new facility is a onestop approach to healthcare.
Gang is focusing on seamless navigation. From the moment a patient crosses the threshold, they’ll know where to go. Exam, treatment, and diagnostic spaces will be collocated to cut back on elevator travel.
The net effect will be a deep sense of ease.

“ We really started this design by thinking about the patients— their arrival and experience. We are trying to make them feel less anxious about coming to receive treatment. We want to give patients and their families a stronger sense of agency,” Gang says.
11 NewYork-Presbyterian
The building will also allow for new technologies and innovation—a cornerstone of NYP’s healthcare mission—to find a home within the physical plant.
“From a resiliency standpoint, we’re thinking a lot about flexibility,” Gang says. “New technology will come, and the building will need to accommodate that. So the grids we’re designing are flexible for the future. From the ceiling heights to the spans of the floors, there’s capacity to adapt.”
A cancer center of this size and stature requires space for mechanical and technical elements. The building stack puts much of the mechanical equipment on a middle floor to maximize views and sunlight for patients on the upper floors. Gang, a master of shaping natural light, will use energy-efficient glass to reduce glare and maintain a comfortable interior temperature.
“Having access to daylight, greenery, water, and nature—what we often call biophilia— makes you feel good,” Gang says. Green space will be visible nearly everywhere, and ample views out to the Hudson River will provide a built-in ‘wow’ factor.”
Patients and visitors can find moments of rest and reflection in a number of areas, including private cozy nooks, seats by windows with stunning city and river views, and a tranquil café.
Ultimately, Gang wants the building to fulfill NYP’s #1 guiding principle: to put patients first.

The center is designed to build confidence. It will make people feel like themselves.” “
“
This new building represents our vision of providing comprehensive, multidisciplinary patient care. From inviting interiors that mitigate stress and promote integrated care to ample space for innovative cancer research and groundbreaking clinical trials, we’re considering each patient’s overall well-being to maximize their chances of achieving a positive outcome. And we’re not only thinking of patients, but also their families and communities as well as our physicians, providers, staff and trainees. Our accessible and inclusive spaces will create exciting opportunities for collaboration, investigation, and discovery.”
 Dr. Anil K. Rustgi Director of the Herbert Irving Comprehensive Cancer Center NewYork-Presbyterian/ Columbia University Irving Medical Center
GANG’S NEW YORK: From left, Solar Carve on the High Line, the Rescue Company 2 firehouse in Brooklyn, Upper West Side’s Gilder Center. Below: a rendering of the cancer care building.
Dr. Anil K. Rustgi Director of the Herbert Irving Comprehensive Cancer Center NewYork-Presbyterian/ Columbia University Irving Medical Center
GANG’S NEW YORK: From left, Solar Carve on the High Line, the Rescue Company 2 firehouse in Brooklyn, Upper West Side’s Gilder Center. Below: a rendering of the cancer care building.




Even before COVID-19, a silent pandemic was escalating across the country. Anxiety, depression, and suicide rates were on the rise among both adults and children, and our nation’s psychiatric care system struggled to meet the widespread need.
The isolation and stress of quarantine proved to be the tipping point for America’s mental health crisis.
That’s when NYP, a global leader in both brain and behavioral health, sprang into action, developing visionary ways of bringing care to patients who needed help fast.
Thanks to our supporters, our advancements in mental health are leading us toward a more promising future.

In 2020, Francis Lee, MD, PhD, Psychiatrist-in-Chief at NYP/ Weill Cornell Medical Center, led a team at Weill Cornell Medicine (WCM) including Conor Liston, MD, PhD, a neuroscientist and psychiatrist in the Feil Family Brain and Mind Research Institute and the Department of Psychiatry at NYP/Weill Cornell Medical Center, to create START (Symptom Tracker And Resources for Treatment).
This AI-powered digital tool screens users for behavioral health symptoms, provides instant feedback, and connects them with a provider or recommends treatments.
The first users? NYP’s front-line workers, who used START to monitor their own mental health as they cared for COVID-19 patients at the peak of the pandemic. Right away, demand doubled for employee counseling services.
START became a model for using AI to rapidly assess behavioral health symptoms and access treatments. It also paved the way for other innovations like MAYA, a smartphone app that helps users manage mental health conditions like anxiety and depression using cognitive behavioral therapy principles.

“MAYA is building the evidence base for the success of mobile-based mental health services,” says Dr. Lee. “In clinical trials, MAYA users reported reductions in anxiety and depression symptoms that persisted for at least six weeks after using the app. Very few mental health apps have achieved these types of sustained outcomes.”
Next, Dr. Lee and his colleagues plan to personalize START and MAYA for different patient populations by tailoring the content to monitor symptoms of more mental health conditions, from pre- and post-natal depression and anxiety to bipolar disorder. Plans to more tightly link START with MAYA show promise to get more users on board, too.
As COVID-19 subsided and daily activities resumed, our physicians made a dismal discovery: Many more people than we knew had been silently battling mental health conditions—including a significant number of young people. In response, NYP has doubled down on providing the very best treatments and therapies to all patients.
We start by meeting people where they are. To help people with obsessive-compulsive disorder (OCD), NYP physicians at the New York State Psychiatric Institute and Columbia University Irving Medical Center are participating in IMPACTOCD (Improving Providers’
Assessment, Care, Delivery, and Treatment of ObsessiveCompulsive Disorder), a program that provides education, screening, and treatment in community locations people already know and trust.
By training front-line clinicians across New York to diagnose and treat OCD, NYP is empowering trusted providers to use the best evidence-based treatments.
Continued on next page >
We’re also treating children where they already are rather than requiring them to visit a mental healthcare facility. Under the leadership of Warren Y.K. Ng, MD, Medical Director of Outpatient Behavioral Health and Director of Clinical Services for the Division of Child and Adolescent Psychiatry at NYP/CUIMC and NYP Morgan Stanley Children’s Hospital, NYP provides mental health screening, treatment, education, and more at 14 schools across Upper Manhattan.
NYP’s school-based mental health programs are a beacon of light and hope,” says Dr. Ng. “Our mental health providers are helping kids and supporting teachers. And they’re providing both treatment and education so mental health becomes less stigmatized.”
We are also meeting children where they are by providing telepsychiatry services and integrating mental health services within primary care programs in seven locations. These programs are nurturing kids’ well-being, overcoming stigma to provide behavioral healthcare, and building family and community resilience.
There is still tremendous work ahead, particularly in addressing the worsening youth mental health epidemic. That’s why we’re deepening our commitment by opening the new Center for Childhood and Adolescent Behavioral Health at NYP Westchester Behavioral Health in White Plains, New York. The new facility and its programs are funded by a visionary and transformative gift from the Steven & Alexandra Cohen Foundation.
At the Center, we’ll redefine psychiatric care for young people with customized mental health support. Kids and teens will be able to access
services for a full spectrum of conditions through expanded child and adolescent inpatient units, a new state-of-the art ambulatory behavioral health center, and expanded telehealth offerings and community programming. We’ll also connect families with providers local to them and share our latest learnings and innovations with practitioners, patients, and caregivers across the country. We’ll address our patients’ time-sensitive needs quickly, and they’ll get care specific to their age.
Together with our supporters, we’re opening up access to mental healthcare for more people than ever. Your generosity has helped catalyze the development of new and best-in-class solutions. NYP has been on the front lines of mental health in America for decades; now, we can do even more to bring together the brightest minds and the best technologies to drive toward a better future for our country’s mental health.
“I am eternally grateful to NewYork-Presbyterian for the generous, comprehensive, and outstanding clinical care my son received. At times, especially when we had to make tough decisions about next steps, I felt as though they cared about our son as though he were their own.”
– Mother of a young psychiatric patient at NewYork-Presbyterian
NYP on the Front Lines of the American Mental Health Crisis


When he arrived at NYP’s emergency department, he was months behind on rent, struggling at work, and facing hunger. We addressed his clinical needs—and the social challenges contributing to his poor health.
With the help of the Center for Community Health Navigation Patient Navigator Program, led by Director Patricia Peretz, MPH, and in partnership with a local community-based organization, we connected the patient with resources he needed in his community: food pantry access, recertified food stamps, rental assistance approval, and a new housing opportunity.
That’s how the path to good health is built—by seeing the whole picture of a person’s wellbeing and taking action to address the structural inequities that surround them. Through the Dalio Center for Health Justice, NYP is not only able to address these root causes, but also share our metrics and models with hospitals around the country to help further health justice for all.
“Patient Navigators are experts in building trust with patients,” says Tiffany Sullivan, Senior Vice President and Chief Operating Officer of Physician Services at NYP. “Including social determinant of health screening within their
workflow is a natural fit and allows us to deliver holistic care to patients seen in the emergency department.”
It begins with the right questions and the right data—and the support of donors like you.
Powered by the Dalio Center and NYP’s Division of Community and Population Health, in 2022 NYP launched an innovative new process with a standardized screening and referral tool across our hospital system that enables healthcare workers to identify what is preventing patients from meeting basic needs. From there, we can refer them to local organizations ready to help.
We have a long history of partnering with community-based organizations across New York City to address health disparities,” says Davina Prabhu, Vice President, Operations, Ambulatory Care Network and Division of Community and Population Health at NYP. “As part of this effort, we have been able to build upon these strong relationships to support patients across the enterprise who have unmet social needs.”
Addressing these social needs—including food security, housing, and access to transportation— is critical for equitable health outcomes: 80 percent of health is driven by social, behavioral, and environmental factors known as social determinants of health. These factors are the root cause of health injustice.
“Our work in social determinants of health touches on what the Dalio Center is most passionate about,” says Julia Iyasere, MD, MBA, Senior Vice President for Health Justice and Equity and Executive Director of the NYP Dalio Center. “We’re building trust with
patients by asking questions about their lives, and then addressing the needs they highlight, rather than making assumptions about them based on their zip code or census data.”
And social determinant screening is just the beginning.
By collecting more information from patients, we can help them meet their immediate needs and better manage their long-term health.
Thanks to innovations in predictive modeling and predictive analytics, our physician-scientists are using AI to create fair, unbiased mathematical models that predict patients’ futures based on historical data. Once fully developed and trained to perform equitably, these models have the potential to determine someone’s risk of developing medical conditions and detect disease early, making it easier for doctors to prevent and treat them.
“
As we think about the future of healthcare, many people point out two big spaces—health justice and innovation,” says Amelia Shapiro, MBA, Vice President of the Dalio Center. “The Dalio Center advances both of these important areas as we leverage data to improve patient health.”
By uniting our dedication to health justice with the power of big data and AI-enhanced analytics, the Dalio Center can help us propel care—and health—to new heights for all people, both within and beyond our hospital walls.

Because of NYP’s leadingedge advancements in spine care, a child with severe scoliosis can play at recess with his classmates. A woman with degenerative spinal disease can go home the day after her surgery. And a man with debilitating back pain can enjoy golfing, skiing, and jogging again.
“ We can make such a big impact in a person’s life,” says Ronald A. Lehman, Jr., MD, Director of Degenerative, Minimally Invasive, and Robotic Spine Surgery of NYP Och Spine and a professor of orthopedic surgery at VP&S. “People with disabling conditions can get back to living how they want to. And the difference we’re making is not just for our patients— it’s for their whole families.”
By combining machine learning, advanced surgical technology, and interdisciplinary expertise, NYP’s physicians are streamlining the toughest challenges in spine surgery. Our generous supporters are helping us change how patients experience spine care—from Manhattan to Brooklyn, Queens, and Westchester and beyond.
Spinal issues, whether minor or severe, can cause debilitating pain and loss of function—and traditional spinal surgeries carry uncertainty and risks. That’s why NYP is pioneering minimally invasive approaches to alleviate pain and help patients heal faster. Our innovative approaches make surgeries safer and more effective.
To enable these superior outcomes, our physicians start by harnessing AI to synthesize preoperative imaging, demographics, and medical history—creating a customized plan for each patient.
Patient data contains valuable information—like the exact locations of the nerves and bones in the spine—so we use advanced technologies to find patterns across the data and plan surgeries precisely. Because we know more, patients know more about what’s to come.
“Our multidisciplinary approach and technological advancements help us diagnose with incredible accuracy where a patient’s pain is coming from,” says Roger Härtl, MD, Co-Director of NYP Och Spine, who is also Director of Spinal Surgery and a professor at

the Weill Cornell Medicine Brain and Spine Center. “That way, we can tailor our surgical approach to the problem, which prevents surgery from going beyond what a patient needs, reduces the risk of complications, and quickens recovery time.”
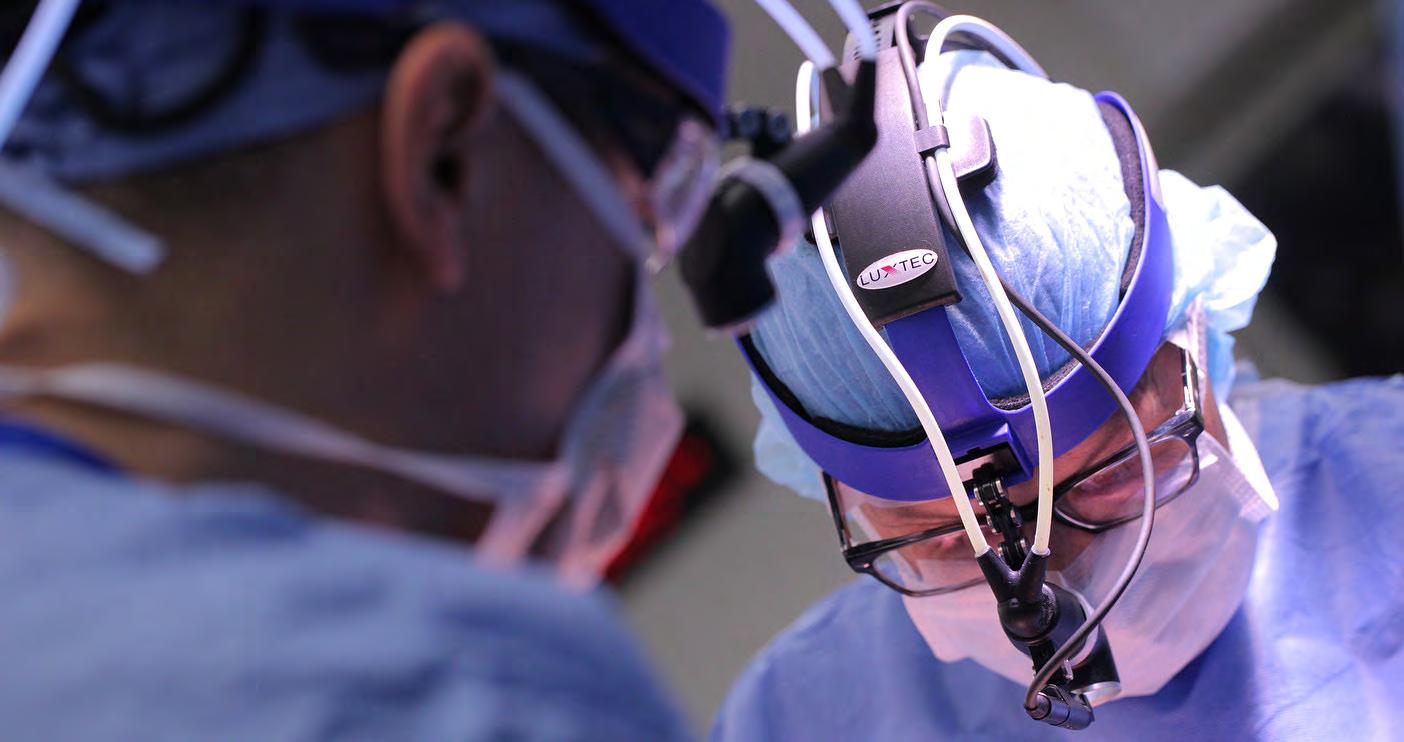
Equipped with advanced imaging, 3D navigation systems, and robotic assistance, our surgeons’ procedures are safe, effective, and minimally invasive.
As they navigate the delicate structures around the spine, physicians use advanced imaging and navigation systems to get real-time support customized to their own skills and expertise— including 3D images of patient anatomy and tracking of where all the surgical instruments are in the patient’s body. Robotic assistance helps guide instruments like spinal screws
with greater precision and enhances the way surgeons can meticulously complete the most intricate surgical tasks.
Even as we pioneer the most sophisticated spine surgery in the country, we’re looking to the future, too.
The next frontier: augmented reality. This developing technology, which we are beginning to use, is poised to improve patient outcomes even more by overlaying virtual information onto the surgeon’s field of vision through a wearable headset or the operating microscope, making the work of planning incisions, finding critical structures in the patient’s anatomy, and placing implants more precise and effective than ever before.
Today, NYP’s physicians are driving the future of spine care. State-of-the-art technology helps them at every stage, from identifying candidates for surgery to designing a surgical strategy. With innovations like augmented reality on the horizon, the promise of even greater rigor and less invasive procedures is closer every day. We’ll get there with the ongoing support of our dedicated donors.
Thanks to you, NYP’s physicians will continue to perform the most complex spine surgeries with their unmatched combination of compassion and skill, giving new hope to every patient they see.

The future of medicine is in motion at NYP, where investments in our mission are fueling change every day. From simple solutions to soaring skyscrapers, every achievement at NYP happens because of supporters like you. Thanks to your generosity, our major campaign is already opening doors and improving lives, and we’ve only just begun. Here are the events, celebrations, conferences, and unveilings that tell the story of the power of philanthropy in action at NYP.




1 Plates for Pediatrics Benefits NYP Komansky Children’s Hospital
Held in collaboration with Saks Fifth Avenue, NYP Komansky Children’s Hospital’s 11th Plates for Pediatrics benefit raised funds to help the hospital provide innovative care to children. The dazzling event was hosted by NYP/Weill Cornell Pediatricianin-Chief Sallie Permar and featured celebrity chair Anderson Cooper.
2 Ribbon Cutting Inaugurates New Spine Unit
NYP opened a new inpatient unit dedicated to spine care at NYP/Weill Cornell Medical Center, part of a foundational gift of $50 million from the Jane and Daniel Och Family Foundation. We have already begun to expand the renowned Och Spine program across the New York metro area including Westchester, Manhattan, Brooklyn, and Queens.
3 Dalio Center for Health Justice Hosts First Conference
The Dalio Center for Health Justice’s Inaugural conference at the Brooklyn Museum featured compelling discussions about race, racism, and health led by speakers including bestselling author and activist Heather McGhee, JD, Dalio Center founder Ray Dalio, and NYP Chief Executive Officer Steven J. Corwin, MD.
4 The W. P. Carey Foundation Supports Tomorrow’s Healthcare
Thanks to a transformational gift from the W. P. Carey Foundation, NYP is establishing the W. P. Carey Residency Program and the W. P. Carey Scholars, which will prepare incoming physician leaders to shape medicine’s future. The W. P. Carey Foundation also powers NYP healthcare workers and friends to raise crucial funds through the TCS New York City Marathon.
5 Strategic Partnerships Promote Health for Children and Families
A $35 million gift from the Steven and Alexandra Cohen Foundation will allow NYP to expand behavioral health services for children and adolescents. There have been some fun and games, too: The iconic New York Mets and NYP partnered to promote health and wellness inside the ballpark and beyond, from community cancer screenings and blood drives to interactive experiences throughout Citi Field.
6 Lang Youth Medical Program Celebrates Graduation
NYP was proud to celebrate the Lang Youth Medical Program graduates, who completed the six-year college prep and health sciences enrichment program. Now in its 10th year, the initiative gives underserved students a pathway for success into medical and science careers.
7 “In the Heights” Murals Unveiled at NYP/CUIMC
The walls of the hospital have come alive in full bloom, thanks to award-winning composer, lyricist, and actor Lin-Manuel Miranda. The beloved long-time NYP supporter, along with his family and Warner Bros. Entertainment, gifted two stunning murals that were painted by Danny Peguero, a local visual artist and designer, to NYP/CUIMC.
8 NYP Gathers to Rally Around Future Vision
NYP came together for the first time in three years to celebrate its inspiring vision for ushering in the future of medicine. Speakers including NYP Chief Operating Officer Brian Donley, MD, and Chair Jerry Speyer outlined the Hospital’s mission and thanked front-line workers. NBC’s Al Roker, his wife Deborah Roberts, and Lin-Manuel Miranda expressed how much NYP has meant to them.




9 NYP Celebrates Milestones in Youth Behavioral Care
The Center for Youth Mental Health celebrated its 10th anniversary and a new name with a dinner that raised $4 million for young people and their families. The dinner was hosted by Steven J. Corwin, MD, NYP Chief Executive Officer; Anna Wintour, Chief Content Officer of Condé Nast and Global Editorial Director of Vogue; Sienna Miller; and Dr. Alexandria (Zandy) Forbes, President and Chief Executive Officer of MeiraGTx.
10 Comedy Event Supports Children’s Health
The NYP Morgan Stanley Children’s Hospital Comedy Night raised more than $700,000 to help build a new neuro-NICU at the hospital thanks to the incredible support of Morgan Stanley employees, including Drew Ertman and Aly Kerr.
11 Neurosurgeon Honored With Special Recognition
At the Plaza Hotel, Philip E. Stieg, PhD, MD, and Neurosurgeon-in-Chief of the NYP/Weill Cornell Medical Center, accepted the Maurice R. Greenberg Distinguished Service Award in honor of his groundbreaking career and contributions at NYP and Weill Cornell Medicine.
12 Ophthalmologist Honored With Special Recognition
The fourth Seymour Milstein Distinguished Service Award was presented to Dr. Stanley Chang, the K.K. Tse and Ku Teh Ying Professor of Ophthalmology at VP&S, at the Rainbow Room for his revolutionary surgical approaches.




13 Impactful Cross-Cultural Program Marks Key Anniversary
For the 30th anniversary of the NYP Lower Manhattan Hospital Chinese Community Partnership for Health, community members and staff gathered to celebrate the program’s impact. Founded by NYP’s Eric Poon, MD, the program helps residents overcome language and cultural barriers to address unmet healthcare needs.
14 Annual Luncheon Supports OB-GYN Advancements
At the 16th gathering of this celebration of OB-GYN physicians, two exceptional NYP clinicians, Sidney Wu, MD, and Yelena Havryliuk, MD, were honored for their contributions to NYP and their field. Longtime NYP partner CHANEL announced a generous new donation that will expand telehealth services for new mothers.
15 NYP Makes Strides in Hudson Valley
At the NYP Hudson Valley Hospital, President Stacey Petrower, MPA, welcomed Pawan Rastogi, MD, Division Chief, Gastroenterology, to discuss the tremendous investments we are making within the hospital, medical group, and community, including key advances in GI health.

Visit nyp.org/giving
NYP’s amazing team who made this magazine possible.

















We are in a seminal moment, a moment of change. The way I practiced medicine in the last 20-something years is not going to be relevant in five years.

I have family that I adore and I refuse to leave a world to them that is more inequitable than the world I entered. My responsibility is to leave behind something much better than what I had.
You realize how much of a difference you’re making in people’s lives, and not just that person, it’s their family, it’s their grandkids who aren’t born yet. You really have a significant impact on how that person can get back to living the life they want to live.
NYP offers personalized care. We make costly, innovative medicines available to patients of all backgrounds. And we make it easier for people to access the healthcare they need.
NIR URIEL, MD, MSC, FACC
Director of Advanced Heart Failure, Cardiac Transplantation, and Mechanical Circulatory Support Programs, NewYork-Presbyterian
JULIA IYASERE, MD, MBA
Senior Vice President of Health Justice and Equity, NewYork-Presbyterian
Executive Director, NewYork-Presbyterian
Dalio Center for Health Justice
Assistant Professor of Clinical Medicine, NewYork-Presbyterian/Columbia University
Irving Medical Center
RONALD A. LEHMAN, JR, MD
Director of Degenerative, Minimally Invasive, and Robotic Spine Surgery, NewYork-Presbyterian Och Spine
Professor of Orthopedic Surgery, Columbia University Vagelos College of Physicians and Surgeons
DEEPA KUMARAIAH, MD, MBA
Senior Vice President and Chief Medical Officer, NewYork-Presbyterian
Assistant Professor of Medicine, Columbia University Irving Medical Center
We are so proud to share with you all of the incredible, life-changing work happening at NewYorkPresbyterian. The innovations, advancements, and sky-high projects you’ve read about in these pages are happening because of the passionate, dedicated, principled people who have devoted their lives and careers to them—and because of you. Every one of these incredible achievements is possible because of the power of philanthropy. Every time you support NYP, you are doubling down on an investment not only in current healthcare, but also in the healthcare that’s to come. The world will be a better place for future generations because you care right now. We are forever grateful for your partnership.”
 Sheila Kelly Senior Vice President and Chief Development Officer NewYork-Presbyterian
Sheila Kelly Senior Vice President and Chief Development Officer NewYork-Presbyterian

BROOKLYN
NewYork-Presbyterian Brooklyn Methodist Hospital
MANHATTAN
NewYork-Presbyterian/Columbia University Irving Medical Center
NewYork-Presbyterian/Weill Cornell Medical Center
NewYork-Presbyterian Allen Hospital
NewYork-Presbyterian Lower Manhattan Hospital
NewYork-Presbyterian Och Spine Hospital
QUEENS
NewYork-Presbyterian Queens
WESTCHESTER
NewYork-Presbyterian Westchester (formerly Lawrence Hospital)
NewYork-Presbyterian Westchester Behavioral Health
WESTCHESTER-PUTNAM
NewYork-Presbyterian Hudson Valley Hospital