YOUR CALL. Issue 18 nwas.nhs.uk A mother’s love and dedication. Come fly with me. Meet our crew at Manchester airport. Building connections with our Deaf communities.
TO THE LATEST EDITION OF YOUR CALL.
For many, summer is their favourite season as people naturally become more ‘outdoorsy’. It’s an opportunity to relax and unwind and spend time with our loved ones.

This issue has been inspired by the summer – we take a trip to Manchester Airport and shadow our ambulance crew based there.
We speak to our Hazardous Area Response Team to find out why open water can be one of the deadliest places to be. Last summer alone, we attended 81 incidents where people had gotten into trouble in open water or drowned here in the North West.
Also in this edition, we speak to NHS 111 Health Advisor Charlene Richards who, after entering a team poetry competition based on experiences at work, talks about her personal journey with mental health. Her poem ‘Hardest call to take’ won - don’t miss it.
Do you find that talking about your health is easy in theory but difficult in practice? Especially when our brains are so good at coming up with excuses for why we shouldn’t. We speak to some of the men in our service in our men’s health focus, including Senior Paramedic Team Leader Iain Duffy. Iain was diagnosed with bowel cancer less than a year ago and shares his story to raise awareness of the symptoms.
If you have a story to share and would like to feature as a guest writer in the next edition, we would love to hear from you.

YOUR CALL MAGAZINE TEAM
Also in this issue...
WHEN BRILLIANT MINDS COME TOGETHER.
We look at the important role that research plays in developing the NHS into what it is today, as well as what it means for its future.
PRACTICE MAKES PERFECT.
We support hundreds of large-scale public events, including football matches and concerts. We look at what goes into planning such an event like Parklife in Manchester.
ONE MINUTE I’M AN ADULT, THE NEXT A SEVEN -YEAR-OLD CHILD.
A member of our Patient and Public Panel explains how her complex neurological disorders affect her.
LEAVING HUGE SCARS.
As part of our men’s health focus, Associate Director of Estates, Fleet and Facilities Management Neil Maher, and Paramedic Paul Dunbar, talk about their harrowing experiences of post-traumatic stress disorder.
Welcome nwas.nhs.uk nwasofficial @nwasofficial @NWAmbulance
6
12 DO YOU HAVE A STORY TO SHARE WITH US? If so, please get in touch by emailing: communications@nwas.nhs.uk.
14 LinkedIn 13 2
WORKING TOGETHER TO IMPROVE HOSPITAL HANDOVERS FOR PATIENTS.
have come from this joint working is the introduction of direct ambulance admission to the Same Day Emergency Care (SDEC) service at Royal Preston Hospital. This means that where appropriate we can direct patients away from A&E where they can be rapidly assessed, diagnosed and treated without being admitted to a ward, and if clinically safe to do so, will go home the same day their care is provided. This improves patient experience and frees up ambulances to attend to more patients in the community.”
Plans are now being put in place to build on this success and get back together to make more improvements going forward.
Healthcare professionals from NHS trusts across the North West have been working together in a series of events to share ideas and best practice for improving hospital handovers.

The collaboration has helped to reduce the number of handover delays of over 60 minutes in the North West by 47 per cent, only slightly short of its aim of achieving a 50 per cent reduction by 31 March 2023. This aim was chosen because evidence shows that longer hospital handovers increase patient harm and reduce the ability of ambulances to respond to urgent calls.

The joined-up approach which we led alongside NHS health and care quality improvement organisation AQUA and NHS England North West included representatives from 20 NHS trusts covering 26 emergency departments. It involved getting together to come up with innovative ideas and putting them into action. We then worked together to develop new ideas and ways of working before coming back together. Some of the initiatives that have been put in place include managing surges of patients presenting at hospitals over a short period, using daily data to support decision making and going back to basics by looking at ways to make improvements to existing processes.
Sector Manager for South Lancashire Dave Suart, who has been contributing in the events, said: “Improving hospital handover times helps us get to our patients more quickly. One example of the improvements that
Director of Quality, Innovation and Improvement, Maxine Power said: “We know that relationships matter, and I am exceptionally proud of what has been achieved by working together with a group of passionate people with great ideas. Their drive to make changes ultimately provides our patients with a better experience when they use our services.
“Going forward, we will continue to build on what we have achieved so far to involve more partners and keep on learning from each other using the data that we’ve gathered and maximising the collaborative efforts to make a real difference for our patients.”
3
3

4
A mother’s love and dedication.
Yvette Brown, Community Resuscitation Engagement Officer, has a vital role within Team NWAS. Yvette raises awareness about public health and spends her weeks training people how to do effective cardiopulmonary resuscitation (CPR) and how to use a defibrillator.
We sit down with Yvette to talk about how the rare respiratory condition her son, Oliver, was born with guided her towards becoming a paramedic. She says he is the reason she is motivated to help people in her local communities.

Born on Christmas Day, Oliver was diagnosed with a rare health condition called Coffin-Siris Syndrome (CSS). Symptoms of CCS can range from struggling to breathe, having a thinner airway, rarely crying, and not taking milk. It is estimated to affect around 200 people worldwide.
Oliver showed signs of all these symptoms and after spending the first few months of his life in hospital, Yvette was told he would not live past two years of age.
Yvette and her family took the news hard but she was determined to prove doctors wrong. She became an advocate for Oliver’s health and care and spent the next 20 years attending conferences in other countries, learning everything she could about his condition, and lived with him in hospital for long periods of time.
At the time of Oliver’s diagnosis, Yvette felt incredibly isolated, there was a real lack of understanding of his condition with medical professionals as it was so rare. She was unable to work flexibly in her job at the time which made things harder for her. Throughout all this, however, Yvette focused on her love for Oliver and continued to pursue the best treatment available.
It was through caring for Oliver she met many paramedics and technicians along the way. After experiencing the excellent care they gave to Oliver, she decided the ambulance service was a career path she wanted to take.
“I learned so much about Ollie’s health condition as I wanted to create the best life for him. I had to call the ambulance service regularly and I met some amazing paramedics and technicians. I created a guide about Ollie that I shared with them, which they appreciated. Ollie was always treated with care, compassion, and dignity by them, and it made me realise that I too could do the same for people.”
No parent ever wants to outlive their child, but Yvette has always known she may one day sadly outlive Oliver. As his
full-time carer, Yvette was afraid her eventual loss would be too much to bear. Finding the ambulance service and applying for her current role gave Yvette the chance to build something for herself whilst still caring for Oliver who is now 23 years old.
Yvette could not be prouder of him and how he has faced health hurdles in his life: “Ollie lives on ventilation every night and has carers. We have raised him with love, commitment, care, and support.”
Yvette’s care and commitment to her son extends beyond her role as mum and flows over into her day job. She is passionate about promoting health awareness to people of all ages. She has some handy tools and techniques to help her reach the right people, including a mapping system to identify areas of Greater Manchester which have higher and more frequent cardiac arrests. She strategically targets schools and care homes in these areas and aims to visit one every week to teach them how to do CPR and how to use a defibrillator. Yvette says:
“Cardiac arrests can happen to anyone. No matter what your gender, age, nationality, or background is. Aside of my son being my priority, teaching people the knowledge around CPR and defibrillators is why I get up in the morning.”
Yvette’s training sessions have touched the lives of diverse individuals, from her family members to community members of all ages. Yvette firmly believes that anyone can learn CPR, which is crucial in saving lives.
“The communities I work in are already starting to reach out to me. Engagement is going well, but I am determined to do more.”
5
When brilliant minds come together.
As the NHS marked its milestone 75th year, we caught up with Research Manager Sandra Igbodo to discuss what makes her proud to be part of the NHS and the important role that research plays in developing the NHS into what it is today, as well as what it means for its future.

First joining the NHS more than 20 years ago, Sandra has accumulated a wealth of experience and knowledge from various positions. Since 2010, she has undertaken research management and facilitation roles within mental health trusts, local universities and the National Institute for Health and Care Research (NIHR). She joined team NWAS in 2018 and in her role as research manager works as part of the Research and Development Team to create a thriving research culture at our organisation. Sandra says:
“Research in the NHS is essential to help improve prevention, diagnosis, and treatment of health conditions for all patients. We need to ensure that all our patients, public and staff can participate in research to aid advancements in health care.”
Winning awards for their efforts, Sandra and the team work to seek opportunities for us to host NIHR supported studies, foster new research collaborations and support colleagues and external study teams with undertaking their research. They ensure that research is conducted safely and effectively in line with national research governance standards.
Sandra continues: “Pre-hospital urgent and emergency care research has advanced significantly over the years and there has been a shift in the understanding of ambulance services and the tremendous potential we have in terms of research. Carrying out research in
the pressurised setting of an ambulance service is very challenging but rewarding. From delivering a research study about staff wellbeing to a randomised controlled trial for out-of-hospital cardiac arrest patients, the possibilities are limitless. The research we deliver can enhance the way we provide health care and services, making improvements for our staff and patients.”
Achieving their best performance in relation to NIHR participant recruitment in 2022-23 and hosting the trust’s first national research conference this year, the team has gone from strength to strength, and going forward, they aim to continue to grow research at NWAS to provide even more opportunities to get involved.
The findings of a recent study have been published from a clinical trial that the trust participated in that explored whether diagnostic testing and decision aids, along with clinical judgement and appropriate training, can identify patients at a low risk of a heart attack in the out-ofhospital environment.
Reflecting on being a part of the NHS, Sandra says: “The NHS is an institution that continually strives to enhance the health and wellbeing of all and I’m proud to be able to contribute to this ambition. Whether you’re in a clinical or administrative role, there is a collective sense of purpose in delivering the best health care that we can for our patients.”
6
BUILDING CONNECTIONS WITH OUR DEAF COMMUNITIES.

Approximately 12 million adults in the UK are Deaf, have hearing loss or tinnitus. An estimated 1.2 million adults in the UK have hearing loss severe enough that they would not be able to hear most conversational speech. When you consider the North West has a population of 7.5 million, it means there are likely tens of thousands of people in the region who are Deaf or hard of hearing.
We have built strong relationships with our Deaf communities over the years, and we recently hosted an engagement session with service users at the Deaf Village North West in Blackburn. In the session, we talked about the various ways Deaf people can access our 999 service when in need of emergency assistance.

This includes the national British Sign Lanuage (BSL) 999 Emergency Video Relay Service which allows Deaf patients and hard-of-hearing people to communicate with us. They can download the app and initiate a call to 999 through a BSL interpreter appearing on their screen.
A Deaf Village North West service user, Habib, says: “I used the BSL 999 app due to having troubles at home that left me extremely anxious and worried, leading to me collapsing due to a panic attack.
“It is extremely useful having the BSL 999 app as it allows us to connect to the ambulance service quickly in an emergency. It has improved my life as before it, I had never been able to contact the emergency services myself. It is so easy to use and gives me peace of mind knowing I have help there without any communication barriers. I feel a lot more confident should I need to call for help in the future. I finally feel safe in my own home.”
Another Deaf Village North West service user, Simon, says:
“Before the BSL 999 app, I would have to ask family members to call which wasn’t ideal as when someone calls on your behalf there can be a communication breakdown, which I have experienced. This app allows me to be more independent and not rely on other people.”
We talked to the group via their BSL interpreter, and we were joined by Paramedic Yvette Brown, who taught the group how to do CPR and how to effectively use a defibrillator during the event of a cardiac arrest.
If you are part of a community group and would like us to visit, please email: Talk.tous@nwas.nhs.uk
Images courtesy of Steven from Deaf Village North West.
7
Come fly with me.
It’s summer - which for thousands of us means jetting off to sandy beaches for some guaranteed sunshine and quality time with the family.

With 54 million passengers passing through Manchester Airport last year, statistically, some are unfortunately going to need some emergency help and this is where our airport team comes in.
Based at the airport itself, the team is made up of five staff, plus six bank staff, and responds to incidents within the airport boundaries, which could mean attending to a patient in a coffee shop at the terminal or waiting to meet an incoming plane with a patient on board.


To experience a typical day, we spent a shift with paramedics Adam Williams and Andy Tompkins.
The team has an office where they can restock their medical bags, charge defibrillators and enjoy a well-
deserved brew and it’s from here that they receive their first call of the day. Incidents are relayed to them via mobile phones but are still logged on the trust’s main system. This first job is for a passenger arriving from Canada who has taken unwell on the flight.
Adam makes sure he has all he needs and we drive around the site on blue lights, passing through a security gate to get ‘air side’. The response car parks on the tarmac underneath the bridge which will connect to the plane once it arrives, and it is inside there that we wait.
Adam explains later that whenever a patient is met off a plane, a member of the border control team attends to check passports.
SUMMER FEATURE 8
The patient, who has coeliac disease, has had a reaction to something he ate and so is suffering from stomach pain and vomiting. Adam checks his blood pressure, temperature and heart and reassures him that unfortunately, it is something that just needs to get through his system and he will feel better in a few hours.

He explains afterwards:
“Falling ill thousands of feet in the air can be really frightening for people and in most cases, it is reassurance that they want and just a check to make sure it isn’t anything serious.”
The next case is a toddler who, while on a flight from Morocco, has developed a high temperature and a mottled rash all over his body. Mum is understandably worried and so the airline staff requested medical assistance to wait for their arrival.

Once off the plane, the little boy is very upset and clingy and clearly unwell. His temperature is high and the rash is getting worse so while his dad and older brother make their way through to passport control, mum waits with Adam for an ambulance.
Later in the day, after tending to an airline worker who has fainted on the tarmac and a car passenger who has an epileptic seizure in a car park, we attend to 85 year old Rose from Sheffield. After arriving back from a girl’s weekend with her daughter and granddaughter, Rose takes a tumble in the arrivals area of the airport hurting her knees and ankles.
Despite being in some discomfort, she manages to tell us all about her adventures in Majorca and reassures us that there were no holiday romances!
With lots of chuckles and smiles, Adam checks her over, gives her a helping hand to walk a few paces and explains to the family
The tarmac actually has a road system that Adam and Andy skillfully negotiate, stopping to allow planes to pass and to pick up any stray items or ‘fod’ as they are known by airport workers. Adam explained that everyone based at the airport has a responsibility to pick up any rubbish or other items off the tarmac if they see them, as there is the risk of them being sucked up into the aircraft’s engine.
Both Adam and Andy tell me how much they love their work and the people they meet. They say the worst part of their job is when they tell an excited holiday maker that they are too ill to fly but rather that then they take seriously ill whilst in the air!
So, if you are heading on your hols this summer and you see one of our team in green at the airport, give them a wave and a hello – they’ll always be happy to see you and will be there if you need them. However, we sincerely hope you don’t. Happy holidays!


9
Cooling off isn’t worth risking your life.
Rivers, lakes, reservoirs and the open sea can seem very inviting during the summer months, especially when we experience heat waves and need an opportunity to cool down. However, open and unsupervised water is not safe, even for the most experienced swimmers, which is why we’ve been working with our Hazardous Area Response Team (HART) to highlight the dangers and sometimes fatal consequences of swimming in open water.
Last summer alone, between June and August 2022 we attended 81 incidents where people had gotten into trouble in open water or drowned. Since the beginning of 2023, we have already attended 47 open water incidents, including some tragic and fatal drownings where young teenagers lost their lives across the region.
As we approach the school summer holidays, our specialist operations teams who attend water related incidents want to warn parents and family members to continue to discourage children and young people from swimming in rivers, lakes and secluded areas of open water.
Special Operations Clinical Lead for HART Joe Tunn, said:
“Our area response team have been trained to provide life-saving medical care in complex and challenging environments. We attend many different high-risk incidents including situations where people have entered open water and got into difficulty, resulting in rescue attempts to get them to safety.
“It can be difficult to perceive the potential risks posed by water, where hazards are often hidden from view and you can’t predict how cold the water might be. If it’s a hot day and you are asked to be careful as the water is cold, to many this might actually sound quite appealing! But entering cold water can cause cold water shock which includes loss of control of breathing and movement, which can quickly lead to people getting into serious difficulties. Swimming in cold water can quickly reduce the stamina of even the strongest swimmers and it is heartbreaking for our staff to know that warmer weather and school holidays will often lead to avoidable tragedies when people enter open water.”
We’re asking the public to think carefully, steer clear of open water and to learn the Royal National Lifeboat Institution (RNLI) ‘FLOAT to live’ advice. If you see someone getting into difficulty in open water, please call 999 immediately.
LIFE SAVING ADVICE:
If you do get into trouble, the advice from RNLI is ‘FLOAT to live’

F - FIGHT your instinct to panic or swim hard
L - LEAN back in the water to keep airway clear
O - OPEN your body up pushing your stomach up
A - ACTIONS gently move hands and feet to keep afloat
T - TIME in 60-90 seconds, you’ll be able to adjust and control your breathing
SUMMER
FEATURE
*RNLI 10
REMEMBER!
The dangers lurking below:
Depth of water can be hard to estimate, and people can often get into difficulty on steep sides, slimy banks, hidden debris and underwater currents, which can result in drowning.
The water doesn’t discriminate; you could be the strongest swimmer but flow and tides can be vicious, change in an instant and sweep you away with it.
The sudden cold can cause your body to go into cold water shock and/or lead to hypothermia, making swimming extremely difficult.

11
PRACTICE MAKES PERFECT.
Throughout the year we support hundreds of large-scale public events, including football matches and concerts. That’s not any different during the summer. Even when we don’t have a large role in providing medical care, we want to make sure the public is kept safe.
One example of this is the annual Parklife Festival in Manchester, which took place over a weekend at the beginning of June. More than 140,000 people visited Heaton Park over the two days.

Ahead of the event, organisers, blue light services and health and local authority agencies, including the council and Transport for Greater Manchester, got together at Manchester Central to run a tabletop exercise to test the safety plans in place.

Many extreme scenarios were discussed, including what would happen if unsafe recreational drugs caused a mass casualty incident, if there was severe transport disruption and even if a sinkhole opened on the main road route to the festival.
Resilience Manager Nick Bell said, “We organised the event to ensure plans are flexible and robust.
“We don’t expect the worst to happen, but it’s important to know that everyone involved knows what they would do if it did and also make sure that the plans are sufficient to keep people safe. On the day, we had detailed discussions about the processes in place, and where there
were any gaps, agencies could go away and reassess in time for the event.
“While NWAS had a minimal number of resources on the site, we still have a major role in keeping people safe. These exercises are vital, and we try to make sure these tests are held before all major events.”
Advanced Paramedic Martin Rolls, acts as the NWAS operational commander at Parklife. He said: “A third-party provider was responsible for the primary medical care for the festival; NWAS was there simply to provide backup in case the worst happened.

“Happily, none of the scenarios we tested for came to fruition. Given how slick and professional the running of Parklife is, it was still impressive to see how plans kicked into place when things didn’t quite go as scheduled. All agencies are there for the safety of festival goers, and that focus remained in place all weekend.”

SUMMER FEATURE
12
Photo credit Sam Neill, Parklife Festival
It goes without saying that our ambulance crews need to know so many different types of conditions and illnesses. Often, they need to think quickly if something changes with the patient they are treating. That may seem obvious for physical conditions such as if someone’s heart rate or breathing drops but what if a 52-year-old suddenly has the demeanour and understanding of a young child?
This is exactly what happens to Beverly Greenwood, one of our Patient and Public Panel members from Northwich in Cheshire and who is also a NHS Governor for mental health and social care. Beverly has various medical conditions and has been diagnosed with three complex neurological conditions; Functional Neurological Disorder (FND), Non-Epileptic Attack Disorder (NEAD) and Dissociative Conversion Disorder (DCD).
Beverly is keen to raise awareness of what may happen to patients if they have a neurological episode, as they can all present in different ways and in some instances may be mistaken as being drunk. This is why she wears a medical bracelet and lanyard to provide guidance to others if something does happen to her and potentially save an unnecessary ambulance call out.

Beverly explains how a DCD episode affects her: “If my body gets under too much stress or I’m ill, my brain takes me to a safe space. One minute I can talk to you as a 52 year old and at some point I can turn into a seven year old and my voice changes and I would have no clue where I am.”
If this happens her husband is often around to reassure her and explain but if she’s on her own it can cause confusion for her and those around her.
On one occasion during the COVID-19 lockdown, Beverly had to travel to hospital in an ambulance alone. When she got in the ambulance she spoke to the crew as an adult but soon after she suddenly changed into a seven year old.
Beverly recalls the sound of her inhaling the nebuliser was like the noise Darth Vader makes in the Star Wars films. So to help make her journey into hospital a more exciting one for a ‘seven-year-old,’ the crew caring for her took on the roles of different Star Wars characters, as she explains:
“They made my journey into hospital an exciting trip because we pretended that the ambulance was a starship and then when we got to hospital one of the crew said to me don’t forget to use your lightsaber, which was my walking stick.”
“This was amazing for me to get a crew like that, they were still treating me, they were still giving me what I needed. I must admit, I’ve been very very fortunate, I’ve always had crews that have been able to think on their feet very, very fast.”
It took Beverly two years to be diagnosed with Dissociative Conversion Disorder by specialist neurologists and has been told that one day she could go into a seven year old and not come out of it.

13
“One minute I’m an adult, the next a seven-year-old child.”
Leaving huge scars.
Post-traumatic stress disorder (PTSD) is a mental health disorder that develops in some people who have experienced a shocking, scary, or dangerous event. According to research, one in 10 people in the UK are expected to experience PTSD at some point in their lives and unfortunately for Associate Director of Estates, Fleet and Facilities Management Neil Maher and Paramedic Paul Dunbar, they have experienced it.
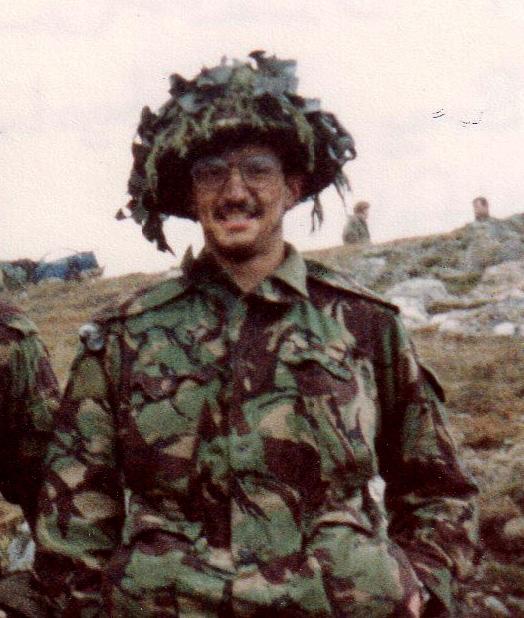
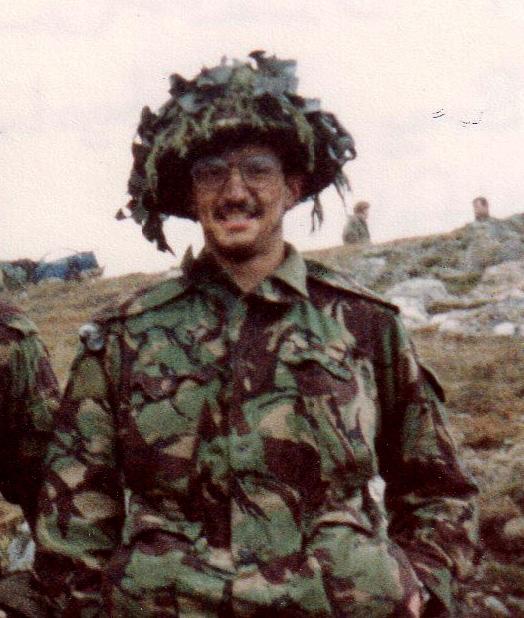
Neil Maher has been part of our green family for 20 years but before he embarked on his ambulance career, he dedicated 10 years of service to the army. During his time in the forces, Neil witnessed a lot of upsetting things, but the Falklands Conflict was something that will never leave him. He said, “I was a young 23-yearold soldier commanding a detachment of even younger soldiers, aged 18 –21. Unfortunately, during a task, six of my colleagues were killed. One was a bright, young man, a friend, who had just gotten married the day before we shipped out. It was a horrible and tragic death and looking back now, I believe was the moment that triggered my PTSD.”

I needed serious help because, in that patient, I could see myself. I went off sick after that job and I haven’t been back working in an ambulance since.”
Both Neil and Paul are now both on the road to recovery after confiding in friends and family and sourcing professional help and want to highlight the importance of this. Neil said, “I learned the hard way and it took 25 years before I got help. I don’t want anyone else to feel like that. We now know so much more about PTSD, there is so much support out there so take it.”
Paramedic Paul Dunbar has spent nearly 20 years doing a job he loves but unfortunately, last year the stress of the job became too much. He explained: “In February last year, I attended a really awful road traffic collison. The passenger had died in such a horrible way. I came away feeling very stressed and angry and I couldn’t alleviate any of the emotions. But I carried on and it was a couple of shifts later that I finally broke on a job. The patient had tipped all their pills into a cup intent on taking their own life. They’d called us before taking them and that was the final straw. I realised
Paul, who has now returned to work in a different role, said: “The fear that became all-encompassing during the last 12 months was almost unbearable. But I’m out the other side now. I don’t feel like a broken person, but I am changed, and I am still working on myself. I would ask all my colleagues to talk about issues they are struggling to reconcile. There are plenty of us in the job who have either been through this or know someone who has. Talk to us, to me. We’re not counsellors, but we can listen and maybe support.”
If you are struggling, confide in loved ones or seek support from your GP.

FOCUS ON: Men’s health 14
One in six people in the UK experience some form of mental health condition and sadly, three times as many men as women die by suicide each year. To raise awareness of men’s mental health, 111 Quality and Assurance Officer Robbie Read shares his experience.

Robbie has struggled with his mental health since a young age but when the pandemic hit in 2020, it became too much and he knew something had to change. He said, “I’ve struggled with my mental health since I can remember. A difficult childhood meant that I’ve been carrying depression, anxiety and some compulsive behaviours right into adulthood. As a teenager, I selfharmed and started making plans for suicide.”
Robbie’s school noticed the signs and he started therapy. He said, “I eventually started counselling at school and was fortunate in that this was helpful for me for at that time. But I felt ashamed and soon discontinued the counselling. Back then, I had little to no understanding of mental health. I just thought that these feelings would eventually go, or they were just a normal part of growing up, not understanding the impact that trauma had on children and young people.”
Robbie continued to struggle with anxiety, feeling low and the occasional thoughts of self-harm and suicide as he reached adulthood. He felt ashamed of these thoughts so buried them. But when the COVID-19 pandemic hit, Robbie’s mental health struggled more than ever. He told us, “When the pandemic hit, my family and I, like countless others, were deeply impacted by separation, fear and sadly, the deaths of several loved ones. Having
My climb back up from rock bottom.
just started working for team NWAS, with the impact the pandemic had on the service and us as individuals, as well as the stresses in my own personal life, I felt as if I had hit rock bottom. Near the end of 2020, I took some time off work due to my worsening mental health. I felt very guilty for taking time off work during such a decisive time for the service and the world, but was grateful to be back in therapy, receiving help from family, friends, my GP and from work.”
After some time, Robbie was able to come back to the job he loves. He said: “I’m fortunate that all these levels of support helped me to recover and come back to work. I can now say that I rarely suffer from my mental health now. I still have my off days and moments, but speaking up and seeking help has really helped me to recover and move forward with my life.”
Another one of the coping mechanisms Robbie feels has greatly aided his recovery is his love of walking. He told us, “Something that really helped me was getting out in nature. I’m an avid hill walker and have spent a lot of time climbing the UK mountains. Getting out on the mountains has really helped to improve my physical and mental wellbeing. I’m currently preparing to do the Yorkshire Three Peaks challenge in September with some colleagues to raise money for our service’s charity.”
If you are struggling, you can contact Samaritans on 116 123 or seek advice from your GP.
FOCUS ON: Men’s health
15
A diagnosis of bowel cancer is difficult to process at any time of life but if it comes when you feel healthy, happy and on top of the world, the news can be devastating for the person and their family.

Last December, Senior Paramedic Team Leader Iain Duffy was still on a high after celebrating moving into his new house with his wife Andrea, who is also a paramedic. They celebrated Christmas and New Year in their new home and Iain was a year into his two-year secondment as a clinical lecturer at the University of Cumbria. It was during this time that Iain first noticed blood in his stools.
He says: “I remember finding the blood at the beginning of December and thinking, that isn’t quite right. I kind of just got on with my life and celebrating the festivities with friends and family.
“Towards the end of December, the blood became more prevalent, and I knew something wasn’t normal for me. In January this year, I went to see my GP who advised me it is likely haemorrhoids.
“This didn’t feel right to me. I remembered my brother getting sent for bowel screening as he has reached a certain age so I asked the GP if I could be screened. Thirteen days later I had a colonoscopy.”
It was during the colonoscopy that Iain noticed a big lump on the wall of his bowel on the screen.
“I had been having a laugh and a joke with the clinician performing my colonoscopy when the mood changed. I looked at the screen and I saw the lump. It was black and white and to me, it looked like necrotic tissue. They took a biopsy.
“Other people in the facility who had had the procedure the same morning as me were leaving the facility, but I had been asked to stay. The doctor came to see Andrea and me and told us that they had found something, and they needed to test it.
“Whilst the doctor couldn’t confirm the diagnosis at that point, I knew it was cancer.”
Iain and Andrea had prepared themselves mentally for receiving the diagnosis and when they did, it still hit them hard. But Iain knew he had the support of Andrea, his family and his friends and colleagues at team NWAS and in the university. He credits them for getting him this far in his treatment.
Iain went on to have scans and surgery to remove the tumour, which was done by keyhole. Iain continues: “There was a risk I could have been left with a stoma bag after the procedure, but my surgeon felt it wasn’t necessary. My bowel healed fine after it, but they did also remove 23 lymph nodes in that area to see if the cancer had spread.”
FOCUS ON: Men’s health
“As a paramedic, it’s hard being the patient.”
16
Iain’s story
The waiting period for Iain and Andrea was stressful, it dragged on and of course, they worried: “It is hard to train your mind out of thinking that cancer is everywhere,” Iain says. When they got the news that five of the lymph nodes that had been removed were cancerous, they were devastated. Iain’s oncologist advised the best course of treatment for him would be to have six months of chemotherapy.
Iain is currently on cycle five of eight chemotherapy sessions which has been tough and has left him with a reduced immune system. “I have been getting sickness and diarrhoea, scalp sensitivity, spots on my tongue (like the ones you get in tonsilitis) and severe neuropathy.

“They have had to alter the type of chemotherapy I was having due to the concerns around the neuropathy symptoms. I am now on tablet form and not an IV drip which seems to be lessening my symptoms to a degree.”
Throughout his chemotherapy and to raise awareness of the disease, Iain has been cycling one mile on his exercise bike on each of his treatment days to raise money for Cancer Research. He passed his 100 miles milestone a couple of weeks back with 68 miles to go.

“No matter how the chemo has affected me, I have done the cycle and Andrea has done two miles each treatment day to support me and spur me on. There have been a few times it has got to 10pm at night and we have forgotten but we have got on the exercise bike and done it.
“My take-home message is, I had no other symptoms other than blood in my stools. I felt healthy, I felt fine but please if you spot something that isn’t quite right, push and push until you get the help you need.”
THE STATS: SYMPTOMS CAN INCLUDE:
• Bowel cancer is the fourth most common cancer in the uk and the second biggest cancer killer.
• Nearly 43,000 people are diagnosed with bowel cancer every year in the UK.
• There are around 268,000 people living in the UK today who have been diagnosed with bowel cancer.
• More than 94% of new cases are diagnosed in those aged over 50 and nearly 56% of those aged 70 or over.
• Bowel cancer can affect anyone of any age with 2,600 new cases diagnosed each year in those under 50.
• 1 in 15 men and 1 in 18 women will be diagnosed with bowel cancer during their lifetime. Bowelcanceruk.org.uk
• Bleeding from your bottom and/or blood in your poo.
• A persistant and unexplained change in bowel habit.
• Unexplained weight loss.
• Extreme tiredness for no obvious reason.
• A pain or lump in your tummy.
If you have any of these symptoms for three weeks or more, see your GP.
For help and support visit: bowelcanceruk.org.uk
17
From military to medic.
Many of our team are armed forces veterans who come and work for us. We are incredibly proud of our armed forces network members, and we love the opportunity to tell their stories.
Scott decided to make his career change from military to medic after hands-on experience of helping the service during the COVID-19 pandemic.
In 2021 and 2022 we received assistance from the military. More than 100 servicemen and women joined us to support our response crews with our clinicians and attend to less serious incidents.
Enter Scott, a member of the 1 Regiment, Royal Logistic Corp, who was deployed as part of the cohort.
“When I did the first year of the deployment to assist the ambulance service in Liverpool, I thought I could see myself doing this,” he
Scott had given 10 years to the army but was ready to call time on his military career. And it was not only the ambulance service that took his fancy but also the North West.
He applied for an emergency medical technician apprenticeship and began his course after relocating from Oxfordshire last September.

And so far, he reports no regrets: “I absolutely
“Because I haven’t come from an academic background, the classroom element at the beginning was a bit of a challenge. My experience in the army means I’m more hands-on, so I feel I came into my own when the practical side of the course out on the road started.
“I love that it’s different every day and you get to help people. There’s a good structure, it’s uniformed and there’s great camaraderie. You could be anywhere, and you’ll see somebody in the same uniform as you and you’ll be able to say hi. Oh, and you also get to drive an ambulance on blue lights to help people!”
Scott is due to complete his apprenticeship later this year and hopes to extend his career here in the North West.
18
Hardest call to take.
We know that our staff members handle a number of urgent and often difficult calls to our services daily. So, when our NHS 111 team at Middlebrook in Bolton were encouraged to enter a poetry competition based on their experiences at work, Health Advisor Charlene Richards took the opportunity to dig deep into her own personal journey with mental health.
Here, 46-year-old Charlene talks about the inspiration behind her winning poem and the type of scenario a 111 call handler experiences.

Charlene says: “Having worked in 111 since January 2022 after my sister Suzanne, who also works for the service encouraged me to join, I have taken every type of call you can think of. When the opportunity came to write a poem, I wouldn’t normally put myself forward, but I decided to advocate for my own experiences, letting people in mental health crisis know it’s ok not to be ok.”
Charlene opened up about her own experience with mental health, in which she has lived with anxiety for many years. Knowing her triggers, Charlene was able to seek support from the team at 111 during periods of intense symptoms.
She said: “Around Christmas time, I was really starting to struggle with feelings of anxiety which became present at work. My manager found me amid a break down and took me to a quiet, calming space to allow me to feel what I was feeling. 111 mental health clinicians also supported me throughout the self-blame and doubt, they reminded me that my feelings were valid, to take the time and not feel guilty about my experience.”
This has helped Charlene prepare for mental healthrelated calls that come through to the service. Although difficult at times, her poem shows she understands the mindset of a person in crisis and is able to approach with compassion, care and support.
Hardest call to take
I hear the sorrow in your voice
I truly hear your pain
I know what you are going through
I too have felt the same.
You tell me that you want to die
My heart just breaks in two
I try to stay calm as I can
And pray in breaking through.
You say you’re lost, nobody cares
The system let you down
Your feelings resonate with me, But I don’t make a sound.
I made it through the darkness
Family and friends showed me the light
And I know if you let yours in
With their help, you too can shine bright.
19