34
SF | PULMONOLOGY
May 2021 | Vol. 21 No. 5 www.medicalacademic.co.za
SAD SAD, a complex and silent signature of asthma
This article was independently sourced by Specialist Forum.
Research shows that small airways dysfunction (SAD) is present in 91% of patients with asthma and are involved across almost all disease severities. Patients with severe asthma are especially affected. Untreated SAD has been proposed as a contributing factor to inadequate disease control in 50%–60% of patients.1,2
S
mall airways (internal diameter ≤2mm or internal perimeter of ≤6mm) are located beyond the 7th and 8th generation of the tracheobronchial tree and account for >98% of the cross sectional area of the lung, ending in the alveolar sacs. They have no cartilage to support their structure and collapse easily on constriction.4,5 Asthma is characterised by chronic inflammation and airway hyper‐reactivity leading to cough, wheeze, difficulty in breathing and chest tightness. Recent studies show that inflammation is associated with bronchial hyper-responsiveness, worsening of asthma symptoms and increased exacerbations. Small airways are narrowed in patients with asthma as a result of inflammation. 2,5 Postma et al describe SAD as ‘a complex and silent signature of asthma’. Small airways are considered ‘silent’ because of their relatively low impact on the whole resistance of the respiratory tree compared to larger airways. 2,5
Assessing SAD According to Postma et al although SAD is well recognised in asthma, its role in the severity and control of asthma is unclear. In the AssessmenT of smalL Airways involvemeNT In aSthma (ATLANTIS) study, the team investigated which combination of biomarkers, physiological tests and imaging markers best measure the presence and extent of SAD in asthma patients. 2
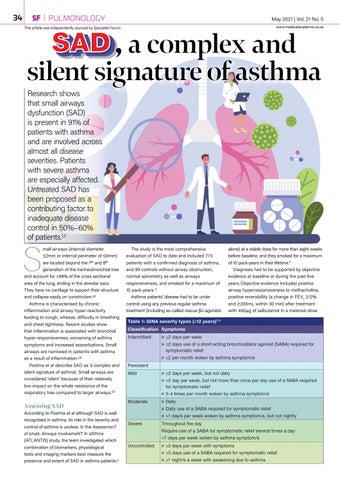
The study is the most comprehensive evaluation of SAD to date and included 773 patients with a confirmed diagnosis of asthma, and 99 controls without airway obstruction, normal spirometry as well as airways responsiveness, and smoked for a maximum of 10 pack-years. 2 Asthma patients’ disease had to be under control using any previous regular asthma treatment (including so-called rescue β2-agonists
alone) at a stable dose for more than eight weeks before baseline, and they smoked for a maximum of 10 pack-years in their lifetime.2 Diagnosis had to be supported by objective evidence at baseline or during the past five years. Objective evidence included positive airway hyperresponsiveness to methacholine, positive reversibility (a change in FEV1 ≥12% and ≥200mL within 30 min) after treatment with 400μg of salbutamol in a metered-dose