7 minute read
People with dermatitis at high risk of osteoporosis major fractures
People with dermatitis at high risk of osteoporosis, major fractures
A recent study found that people with atopic dermatitis (AD) or eczema, have an increased risk of fracture - particularly major osteoporotic fractures.1,2
Advertisement
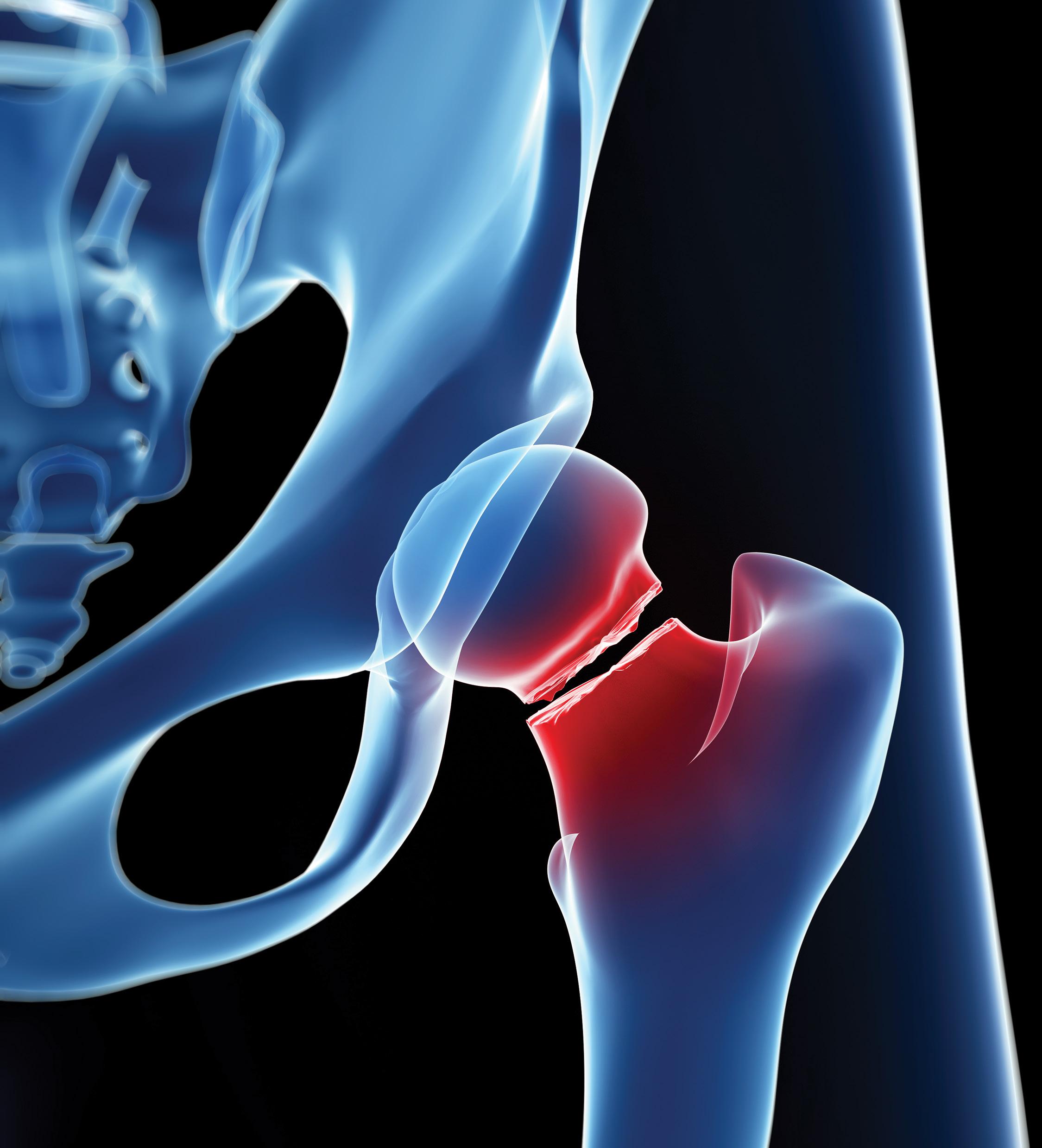
The study by Lowe et al , the largest to date to examine the relationship between AD and fractures, was published in the February 2020 issue of The Journal of Allergy and Clinical Immunology. The team found a strong association between the risk of fracture and the severity of AD. The strongest associations were found in people with severe AD (compared to those without) for spinal, pelvic, and hip fractures.1
The link
AD is a common, chronic, pruritic inflammatory skin disease, occurring in about 10% of adults. Its onset is generally at a young age and follows a relapsing course. AD is often associated with elevated serum immunoglobulin levels and a personal or family history of type I allergies, allergic rhinitis, and asthma.1,2
The International Osteoporosis Foundation defines osteoporosis, which means porous bone, as a disease in which the density and quality of bone are reduced. As bones become more porous and fragile, the risk of fracture increases greatly. The loss of bone occurs silently and progressively. Often there are no symptoms until the first fracture occurs. Reducing fractures is an important public health goal because fractures are associated with increased morbidity and mortality.1,4
According to Garg et al (2014) patients with AD have multiple potential risk factors for decreased bone mineral density (BMD), including using large quantities of topical and systemic corticosteroids (CS). These patients are also at high risk of chronic inflammation. Furthermore, AD is associated with distraction from itch, mental health comorbidities, and sleep disturbance, all of which predispose to fractures and other injuries.3
Haeck et al (2009) found that about 33% of adults with moderate to severe AD have low BMD as measured by dual-energy x-ray absorptiometry. Diseases characterised by chronic inflammatory states are associated with bone loss and skeletal remodeling.5
In another study by Garg and Silverberg (2015), the authors found higher prevalence of fracture and bone or joint injury, and other types of injury, causing limitation among adults with AD. These associations remained significant after controlling for the effects of comorbid atopic disease and psychiatric and behavioural disorders, suggesting a specific association between adult AD and an increased risk of injury.6
AD was associated with higher odds of fracture and bone or joint injury for all individuals 30 years or older, with the largest effect at ages 50 to 69 years. Significant interactions were observed between AD and fatigue or sleep symptoms, such that adults with AD had an increased risk of injury above and beyond the presence of concurrent sleep disturbance or fatigue.6
In addition, adults with both AD and fatigue or sleep symptoms had higher rates of fracture and bone or joint injury compared with those with AD or fatigue or sleep symptoms alone.6
Similarly, adults with both AD and psychiatric and behavioural disorders had higher rates of fracture and bone or joint injury compared with those with AD or psychiatric and behavioural disorders alone. These interactions suggest that adults with more severe AD accompanied by sleep and psychiatric and behavioural disorders comorbidities are at particularly higher odds of fracture and bone or joint injury.6
Wu et al (2017) found that the overall incidence of osteoporosis was 4.72-fold greater in AD patients compared to the non-AD patients (1.82 vs. 0.24 per 1,000 person-years, respectively) after adjusting for potential confounding factors. Osteoporosis risk factors included female gender, age, advanced Charlson Comorbidity Index, depression and use of CS. The dataset analysis showed that AD was significantly associated with subsequent risk of osteoporosis.7
Findings from the new study
According to Lowe et al the aim of their study was to bolster ‘limited’ evidence of a link between AD and osteoporosis. Their study included data from 526 808 people with AD and 2 569 030 people without AD. They also looked at whether fracture risk varies with AD severity.1
They found strong evidence of an association between AD and increased hip, pelvic, spinal, and wrist fractures after adjusting for calendar period, index of multiple deprivation, and asthma (implicitly adjusted for age, sex, general practice, and date of cohort entry).
There was weaker evidence for an increase in proximal humeral fractures. For any fracture, the hazard ratio (HR) comparing the risk of fracture in those with and without AD was 1.10.
The greatest increased risk was seen for spinal fracture (HR 1.18). The unadjusted absolute rate for any fracture in those with AD was 1428 fractures per 100 000 personyears, an excess of 164 fractures per 100 000 person years compared with matched individuals without AD.
After further adjusting for potential mediators (BMI, smoking, harmful alcohol use, and high-dose oral glucocorticoid use), the association between AD and fracture was slightly attenuated (eg HR for any fracture in those with AD compared with those without after additionally adjusting for potential mediators of 1.07) compared with HR adjusted for calendar period, index of multiple deprivation, and asthma of 1.10. The team found similar attenuation of effect estimates across all of the major osteoporotic fractures investigated.
The team recorded minimal change in effect estimates for the association between AD and fracture in most sensitivity analyses. However, when those with a previous history of any type of fracture were excluded from analyses of specific fracture outcomes:
1. For pelvic, wrist, and proximal humeral fractures, the HRs comparing fracture risk in those with and without AD were reduced
2. For spine and hip fractures, HRs were attenuated, but the increased risk of fracture remained.
AD severity and fracture risk
Risk of fracture increased with increasing AD severity. For example, there was a 6% increase in the risk of spinal fracture in people with mild eczema, a 22% increase in those with moderate eczema and a 109% increase in those with severe eczema. The greatest magnitude of increased risk was for spinal fracture in those with severe eczema (HR 2.09), followed by pelvic (HR 1.66) and hip (HR, 1.50) fractures.
The team found varying evidence depending on specific fracture outcomes for age modifying the effect of AD on fracture risk, with some statistical evidence that age modified the effect of AD on spinal (P 5 .0007) and hip (P 5 .0043) fractures.
Similarly, evidence for sex modifying the effect of AD on fracture risk varied depending on specific fracture outcome, with some evidence of a slightly greater risk of hip, wrist, and any fracture associated with AD in men than in women.
Conclusion
AD is associated with an increase in fracture risk, particularly among people with severe disease. The increased risk was most pronounced for major osteoporotic fractures. Spinal fracture risk more than doubled in those with severe AD compared with those without AD, whereas hip fracture rates increased by 50% and pelvic fracture rates were increased by 66%.
References
1. Lowe KE, Mansfield KE, Delmestri A et al. Atopic eczema and fracture risk in adults: A populationbased cohort study. The Journal of Allergy and Clinical Immunology, 2020.
2. Eichenfield LF. Tom WL, Berger TG et al. Guidelines of care for the management of atopic dermatitis. J Am Acad Dermatol, 2014.
3. Garg N and Silverberg JI. Association between eczema and increased fractures, bone or joint injury in adults: a US population-based study. JAMA Dermatol, 2014.
4. International Osteoporosis Foundation. What is osteoporosis?
5. Haeck IM, Hamdy NAT, Timmer-de Nik L et al. Low bone mineral density in adult patients with moderate to severe atopic dermatitis. Br J Derm, 2009.
6. Garg N and Silverberg I. Association Between Eczema and Increased Fracture and Bone or Joint Injury in Adults: A US Population-Based Study. JAMA Dermatol, 2015.
7. Wu C-Y, Lu Y-Y, Lu C-C et al. Osteoporosis in adult patients with atopic dermatitis: A nationwide population-based Study. PLoS One, 2017.
8. International Osteoporosis Foundation.Osteoporosis in South Africa. SF










