The doctor's newspaper Chronicle
Embracing AI's disruption with ethical consideration
AI, healthcare, ethics, and governance were the focus when industry experts weighed in at the Steve Biko Ethics Alive Symposium earlier this month
"A
NY FORM OF AI (artificial intelligence) technology will disrupt what we know as the traditional doctor patient relationship and will make us all think differently in terms of how we embrace this technology,” said Professor Keymanthri Moodley. The distinguished Professor in the Department of Medicine and head of the Division of Medical Ethics and Law, Faculty of Health Sciences at Stellenbosch University, was speaking at the recent Steve Biko Ethics Alive Symposium on ‘AI, Healthcare, Ethics, and Governance’.
AI IN HEALTHCARE
“There’s a lot being said about AI and artificial intelligence so it’s really important to be clear about what we understand when we talk about artificial intelligence,” said Prof Moodley. “What we’re currently working with in the healthcare environment is augmented intelligence rather than artificial intelligence because healthcare professionals are still here in human


form and are still attending to patients on a regular basis with the assistance of AI technology.
“The question is, when we do use AI, does it drastically improve diagnosis and treatment?” Prof Moodley asked. “A number of studies published in international journals show that AI does make a difference, especially in the image-based fields like radiology and dermatology.” A 2017 study published in Nature showed that when the diagnosis of AI technology was compared to 21 board certified dermatologists, there was an equivalent outcome. “In other words, the AI technology could diagnose dermatological conditions as well as a dermatologist.
Another study on radiology showed that the diagnostic precision of AI technology in reading chest X-rays exceeded that of radiologists. Where screening is concerned for breast cancer, mammograms have also been subjected to AI technology and again, these technological advances have shown, in preliminary studies that AI technology is more efficient at reading mammograms for breast cancer than human technicians.
“At Stellenbosch University there is an ongoing project to develop an app that could
help detect tuberculosis at an early stage by listening to the cough of a patient with tuberculosis versus one without tuberculosis. So, before the sputum testing occurs, one could use AI in this regard as well.”
A new development in the UK, DrugGPT is an AI tool that can help doctors prescribing medicine. “We know there are many prescription errors that could occur, drug interactions, side effects, etc, this tool is supposed to be beneficial in reducing medical error in the field of prescribing,” Prof Moodley explained.
“More recently, we’ve seen young people who have had various neurological conditions assisted through advanced technology.” Prof Moodley gave the example of the BRAVO trial – Brain-computer interface Restoration of Arm and Voice through electrocorticography. The overarching goal of the BRAVO trial is to restore speech and communication to people who have lost it. It's also to restore movement and ability to do things like control a robotic arm or computer. A lot of progress has been made in the field in terms of understanding how the brain works and decoding brain activity and trying to tap into neural activity and understand what someone’s been
thinking about or what they're trying to say. A lot of which requires and relies on tools for AI that didn't even exist five years ago.
“In addition to that we have Elon Musk’s Neuralink project, where electrodes are being used to stimulate brain activity in a quadriplegic young patient who is then able to play a game of chess – essentially a groundbreaking human trial. There is quite a bit of mind technology involved and telepathy in terms of moving chess pieces to play the game. Some really out-of-the-box innovative developments that, however, carry with them a number of different concerns. So, this brain computer interface technology is something that we need to look out for,” Prof Moodley cautioned.
AI: THE GOOD, BAD AND UGLY
“While there’s an endless list of good – from democratising healthcare, to revolutionising food safety – you can’t ignore the bad and ugly which is why you should care about AI ethics,” head of Philosophy at the University of Pretoria, Emma Ruttkamp-Bloem said.
Discussing the bad, the AI ethics adviser explained there are concerns around the
Therapy of inflammatory bowel disease has changed: When will we?
continued on page 2


amplification of inequality, threats to social justice and political stability, the quality and integrity of information, privacy and the right to mental integrity, and threats to the environment and ecosystem.
Turning to the ‘ugly’ Ruttkamp-Bloem said AI technology is used by large and powerful corporations to support a business model centred on the commodification of personal data with the core purpose of profit-making (surveillance capitalism).
AI AND ETHICS
“The role of ethics is to enable humans to become the best they can be, enable meaningful technology-society interplay, and enable the integrity of technological processes,” RuttkampBloem said. “The sociotechnical arrangements of our societies ought to be such that they strengthen human agency and enable humans to live dignified lives that they value. This is the core of AI ethics.” AI values and principles – as ethical entitlements – should empower humans to self-determine and realise their fundamental purpose in their interaction with AI technology. This can be achieved if AI ethics is positive ethics that safeguards, ensures, and actualises:

A plea for IBD

N THIS ISSUE of Medical Chronicle, we explore the intersection of artificial intelligence (AI), healthcare, ethics, and governance, exploring both the promises and challenges that arise with the advancement of AI technologies in medicine. Prof Keymanthri Moodley, a distinguished voice in medical ethics, highlights the transformative potential of AI in reshaping the doctor-patient relationship. As AI continues to disrupt traditional practices, Prof Moodley emphasises the importance of ethical considerations in embracing this technology.
On the frontier of medical innovation, researchers at Amsterdam UMC present ground-breaking findings on the use of CRISPR-Cas gene editing technology in the quest for an HIV cure. While these developments offer hope, caution is advised against premature declarations
• Agency: the right to positive liberty
• Autonomy: an environment in which AI actors take up their positive duties to create the means to authentically realise this liberty.
“The tech world has not been trained to concern themselves with moral consequences,” Ruttkamp-Bloem said. “What we need is some kind of mechanism to translate the values and principles into policy actions. And the UNESCO recommendations are the best example.
AI ethics is not just a technical or policy issue, it’s a human issue. We are not regulating technology, we are regulating humans that research, design, develop, deploy, use, and decide not to use this technology. “Ethics is about finding the best thing to do in a particular context, and it isn’t simply about a big list of rules and regulations.
“AI ethics is an enabler of AI governance and ultimately ensures sustainable AI. Not as a competitor or as an add on, but as an integral consideration of what is needed to achieve a life of wellbeing right through the AI lifecycle,” Ruttkamp-Bloem explained. “AI ethics ensures that human rights violations are prevented through placing positive duties on all AI actors to empower humans to live lives of wellbeing. AI ethics is our constant ally and companion when engaging with AI technology at any time during its lifecycle.”
of a functional cure. In another pioneering study led by Johns Hopkins Children’s Center, there are promising outcomes in paediatric HIV care, suggesting the possibility of ART-free treatment for children born with the virus.
Amidst the threat of antibiotic resistance, scientists at Uppsala University unveil a new class of antibiotics effective against multidrug-resistant bacteria, offering a glimmer of hope in combating this global health crisis.
Our CPD articles explore diverse topics, ranging from the impact of long-term diosmectite use on gut microbiota to the comparison of different delivery methods during the second stage of labour.
We also feature an insightful piece by Dr John Wright, advocating for the adoption of modern treatments for inflammatory bowel disease.
Happy reading



CRISPR-Cas sparks hope for HIV cure
While latest research represents proof of concept, scientists caution against premature declarations of a functional HIV cure.
By Nicky Belseck, medical journalistEW RESEARCH UNVEILED ahead of this year’s European Congress of Clinical Microbiology and Infectious Diseases (ECCMID 2024) has ignited hope in the quest for an HIV cure. Conducted by a team of researchers at Amsterdam UMC in the Netherlands, led by Dr Elena Herrera-Carrillo, the study showcases the potential of the latest CRISPR-Cas gene editing technology in eradicating HIV from infected cells. CRISPR-Cas gene editing is a revolutionary technique in molecular biology, celebrated for its precision in altering the genetic code of living organisms. This method, recognised with the Nobel Prize in Chemistry in 2020, operates akin to molecular scissors guided by RNA molecules, enabling targeted modifications to DNA. In the case of HIV, which notoriously integrates its genome into host DNA, the researchers employed CRISPR-Cas to target conserved regions of the virus, achieving promising results in eliminating HIV-infected T cells.
The study’s approach focuses on designing a broad-spectrum therapy capable of combating diverse HIV strains across various cellular contexts. By targeting conserved sequences within the virus genome, the researchers aim to develop a robust and safe combinatorial CRISPR-Cas regimen, potentially leading towards an inclusive ‘HIV cure for all’.
However, logistical challenges arise, primarily concerning the size of the vector used to transport therapeutic CRISPR-Cas components into cells. To address this, the team explored techniques to minimise the vector size, akin to downsizing luggage for a journey, making delivery to infected cells more efficient. Additionally, the study delved into strategies to target HIV reservoir cells, which can rebound when antiretroviral treatment is stopped, by focusing on specific surface proteins present on these cells. Results from the research revealed promising outcomes with the saCas9 CRISPR-Cas system, showcasing remarkable antiviral performance in completely inactivating HIV. Moreover, the study highlights the significance of optimising delivery routes to target most HIV reservoir cells while ensuring safety and efficacy in preclinical models.
Dr Herrera-Carrillo and her team emphasised that while these findings are encouraging, they represent proof of concept and caution against premature declarations of a functional HIV cure. Further optimisation and preclinical studies are imperative to assess the efficacy and safety of the combined cure strategy before considering clinical trials in humans. The ultimate goal is to strike a balance between efficacy and safety, paving the way for a potential cure for HIV.
In essence, this ground breaking research underscores the transformative potential of CRISPR-Cas gene editing technology in the ongoing pursuit of an HIV cure, offering renewed hope for millions affected by this global health challenge.


A Early HIV intervention leads to promising remission in children
Ground breaking research offers hope for ART-Free treatment in paediatric HIV care.
GROUND BREAKING STUDY
co-led by researchers from Johns Hopkins Children’s Center has shown remarkable outcomes for four children born with HIV who were taken off antiretroviral therapy (ART) and remained virus-free for about a year or more without treatment.
These children were part of a group of 54 newborns who received exceptionally early treatment within the first 48 hours of life, a departure from the typical practice of starting treatment weeks or months after birth. Presented at the Conference on Retroviruses and Opportunistic
By Nicky Belseck, medical journalistInfections in Denver last month, the study, sponsored by the National Institutes of Health and the International Maternal Paediatric Adolescent AIDS Clinical Trials Network, aimed to replicate the case of the Mississippi baby, the first documented instance of HIV remission in an infant who received very early HIV treatment. The findings, spearheaded by physician-scientist Dr Deborah Persaud confirmed that ARTfree remission is achievable with very early and effective antiretroviral treatment.

Standard treatment for HIV-positive newborns usually begins weeks after birth, often due to testing delays and limited access to ART drugs, especially in countries with high HIV burdens. However, the study demonstrated that administering ART to newborns immediately after birth can effectively suppress HIV levels in the blood, as evidenced by findings published in Lancet HIV
In a subsequent phase of the trial, six children, now around five and a half years old and primarily from sub-Saharan Africa, were eligible to halt their HIV medication under close monitoring. Four of them experienced remission, defined as undetectable HIV levels for at least 48 weeks off treatment. While one child saw the virus return after 80 weeks, three others remained in remission for 48 to 64 weeks each. Notably, two children in the study experienced detectable HIV levels within weeks, prompting a restart of ART. Fortunately, these children responded well to treatment, with symptoms subsiding.
"This is the first time we’ve been able to successfullyrecreate the case of the Mississippibaby–andinfourchildren", said Dr Persaud
“This is the first time we’ve been able to successfully recreate the case of the Mississippi baby – and in four children,” said Dr Persaud, who is a professor of paediatrics at the Johns Hopkins University School of Medicine. “These results are an important first step to understanding how to curtail HIV reservoirs in children toward ART-free remission and cure for more children living with HIV, ultimately changing the treatment paradigm for this infection that currently afflicts 1.7 million children around the world.” However, she stressed the need for further research to elucidate how very early ART impacts HIV reservoirs, paving the way for improved treatment paradigms in paediatric HIV care. The study's findings offer hope for a future where early intervention could lead to long-term remission or even eradication of HIV in paediatric patients, underscoring the importance of continued research and investment in combating this global health challenge.


Prof Guy Richards MBBCh PhD FCP(SA) FRCP MASSAf
Date: 20 May 2024
Time: 6:00pm
Topic: COPD – Improving outcomes
Speaker: Prof Guy Richards
CLICK TO REGISTER https://bit.ly/CiplaWebinar20May24
Professor Richards is Emeritus Professor of Critical Care and Pulmonology at the University of the Witwatersrand. He qualified in medicine in 1978, specialised in internal Medicine in 1985 and subsequently qualified as a pulmonologist and intensivist. He attained his PhD in Medicine in 1992 and was elected to the Academy of Science of South Africa in 2020. He was made an Honorary Fellow of the SA Thoracic Society in 2022. He was awarded the Mandela Medal

in Gold by the president for distinguished service related to the passing of Nelson Mandela in 2014. He has been awarded best research paper and best publication on a number of occasions at congresses of the SA Thoracic Society and the SA Critical Care Society of Southern Africa, most recently in 2023. He has authored 11 book chapters and 233 peer reviewed, indexed scientific papers and his research has been cited 5130 times. His “h index” is 40.

We make people better and we save lives.
New antibiotic class effective against multidrug-resistant bacteria
Scientists at Uppsala University have discovered a new class of antibiotics with potent activity against multi-drug resistant bacteria and have shown that it cures bloodstream infections in mice.
By Nicky Belseck, medical journalistANTIBIOTIC RESISTANCE HAS emerged as a pressing global health concern, jeopardising the effectiveness of these vital medications that underpin modern medical practices. In response to this looming threat, scientists at Uppsala
University have made a ground breaking discovery – a novel class of antibiotics with potent activity against multi-drug resistant bacteria. Their findings, published in the Proceedings of the National Academy of Sciences (PNAS), offer a glimmer of hope in
Flugon provides immune defence
the battle against antibiotic resistance.
Antibiotics have revolutionised medicine over the past century, playing a pivotal role in combating bacterial infections and safeguarding public health. However, the rampant rise of antibiotic resistance poses
Helps alleviate symptoms of cough, sore throat and a blocked or runny nose
Provides a family offering *
Provides diabetic friendly offerings **
Non- drowsy
Star t strong, stay strong by suppor ting immune health
Different dosage forms available: capsules, effer vescents and syrups







a significant challenge, necessitating the development of new therapeutics to address this critical issue. The research conducted by the team at Uppsala University represents a crucial step forward in this endeavour.
This innovative class of antibiotics targets a protein known as LpxH, utilised by Gram-negative bacteria to synthesise their outermost layer of protection, called lipopolysaccharide. Notably, Gram-negative bacteria encompass several notorious pathogens flagged by the World Health Organization as urgent priorities for novel treatment development, including Escherichia coli and Klebsiella pneumoniae, which have already developed resistance to existing antibiotics.
One of the key advantages of this newly discovered antibiotic class is its ability to effectively combat multidrug-resistant bacteria. In a significant breakthrough, the researchers demonstrated the efficacy of these antibiotics in treating bloodstream infections in a mouse model, showcasing their therapeutic potential. Importantly, since this class of compounds targets a previously unexploited protein, LpxH, there is currently no pre-existing resistance, setting them apart from conventional antibiotics.

The research leading to this discovery was supported by the EU project ENABLE, funded through the Innovative Medicines Initiative's New Drugs 4 Bad Bugs programme (ND4BB). ENABLE brought together a consortium of over 50 European partners from academia and industry to advance early-stage antibiotic development. The success of this project has spurred further efforts in antibiotic discovery and development through ENABLE-2, funded by the Swedish Research Council, the National Research Programme on Antibiotic Resistance, and Sweden's innovation agency Vinnova.



While these findings represent a significant milestone in the fight against antibiotic resistance, further research and development are needed before these compounds can progress to clinical trials. Nevertheless, the discovery of this new class of antibiotics offers renewed hope in the quest for effective treatments against multidrug-resistant bacteria, underscoring the importance of collaborative efforts and innovative approaches in addressing global health challenges.

 Dr Noufal Raboobee Dermatologist
Dr Noufal Raboobee Dermatologist
This webinar is sponsored by iNova Pharmaceuticals
Date: 27 May 2024
Time: 7:00pm
Topic: Understanding the treatment of actinic keratosis: The South African context
Speaker: Dr Noufal Raboobee
CLICK TO REGISTER https://bit.ly/iNovaWebinar27May24
Actinic keratosis is the most common actinic lesion among fair-skinned populations. It is exceedingly common in South Africa due to our high rates of sun exposure. Current president of the Dermatological Society of South Africa, Dr Noufal Raboobee, will place the condition in its local context and explain the optimal treatment approaches currently available.
ABOUT DR RABOOBEE
Dr Raboobee obtained his MBChB at the University of Natal, South Africa in 1983 and went on to complete his FFDerm(SA) though the College of Medicine of South Africa in 1989. He has been in private practice at Westville Hospital for the past 33 years. Dr Raboobee is currently the President of the Dermatological Society of South Africa and the Vitiligo Society of South Africa. He serves on the Medical Advisory board of the Global Vitiligo Foundation and is a member of the International Vitiligo Task Force, contributing to its publications. He has been instrumental in introducing several surgical techniques in vitiligo to South Africa. He has written a book chapter on phototherapy in Moschella and Hurley’s Dermatology in 2020. He has chaired the Psoriasis Advisory Board, during which time the guidelines for

the treatment of Psoriasis were produced and published in the SAMJ by the board members. He currently chairs the committee which is updating the psoriasis guidelines and is a coauthor of the recent update to the international guidelines of vitiligo. He remains on the advisory boards of all the biologics suppliers in South Africa and has has contributed as co-author to the Childhood Atopic Eczema Consensus Document, published in the SAMJ. He has participated in the Advisory Board for Acne during the revision of the guidelines for the use of isotretinoin and has published a photographic series of patients on isotretinoin. He has served as a senior lecturer at the Nelson Mandela School of Medicine, a visiting consultant at King Edward VIII, Inkosi Albert Luthuli and Addington Hospitals in Durban and as an examiner for the College of Medicine of South Africa. Dr Raboobee has participated as an invited faculty member in several congresses held in various countries, the last of which was the World Congress of Dermatology in Singapore in 2023. His special interests include Surgical treatment of Vitiligo, Excimer Laser, biologic therapy of psoriasis and atopic dermatitis, Immunotherapy of viral warts and management of skin cancers.






Dual action; working locally and systemically
Forms a protective coating on the pharynx
Reduces sensitivity of the cough receptors
Relieves local irritation
Reduces the urge to cough
Reduces severity of cough
Thins mucus and helps open airways





Forms a protective barrier against irritants e.g. post-nasal drip
Reduces the urge to cough at night
Diaphoretic effect helps relieve mild fever
Mildly sedative to promote sleep
Not known to be habit-forming
Not known to cause respiratory depression
Omnisient and Altron HealthTech team up for healthcare revolution
Altron HealthTech invites various industry sectors to collaborate on the Omnisient platform to enhance patient and population health outcomes.
OMNISIENT, A SECURE privacypreserving data collaboration platform, and Altron HealthTech, today announced a ground-breaking partnership. The collaboration is set to deliver anonymised patient insights to a wide range of stakeholders including insurers, government bodies, medical researchers, and more, with the overarching goal of enhancing health outcomes for patients.
Through this partnership, Omnisient and Altron HealthTech will leverage a comprehensive source of information while respecting and protecting patient privacy to deliver impactful insights from anonymised data.
Throughthis partnership, Omnisient and Altron HealthTech willleveragea comprehensive source of information whilerespectingand protectingpatient privacytodeliver impactfulinsights fromanonymised data
Leslie Moodley, MD of Altron HealthTech emphasised the synergy between the two organisations, “Omnisient was recognised as a 2023 Technology Pioneer by the World Economic forum, it is this shared passion and pedigree in innovation that makes the partnership so exciting. Altron HealthTech switches over 100 million medical transactions every year which generates a powerful dataset that will benefit both citizens and the institutions that serve them in their health needs. Our desire to deliver on these benefits requires the ability to collaborate with service providers like medical/health insurance organisations, pharmacies, pharmaceutical manufacturers, healthcare institutions, and government. Altron HealthTech takes consumer privacy as seriously as we do the health of patients, which is why we have partnered with Omnisient, who provide a globally recognised Privacy Preserving Data Collaboration solution.”
Omnisient's platform ensures that no personal information is required to facilitate data collaborations between Altron HealthTech and other organisations. The platform uses advanced cryptography for matching anonymised patient records across various data sets, creating a breachrisk-free and secure analytical environment.
Mladen Colic, head of Growth of Omnisient, shared his vision for the partnership, "We're eyeing several impactful applications for Altron HealthTech's data, ranging from minimising insurance risks –which could translate to lower premiums
for consumers – to gaining insights into medication efficacy, and even aiding healthcare providers in optimising facility locations based on real-time demand. These examples scratch the surface of what we aim to accomplish."
Leveraging Omnisient's expansive network, which encompasses over 80 major organisations, Altron HealthTech is poised to accelerate its innovation trajectory, significantly enhancing the potential of this partnership.

Surprising clinical advantages of the flu vaccine
The influenza vaccine not only serves as a vital defence against influenza but also offers unexpected benefits that warrant attention within medical circles.
BEYOND ITS PRIMARY function of preventing influenza infections, flu vaccination has been linked to notable reductions in hospitalisations and mortality rates associated with flu-related complications, particularly among vulnerable populations such as older adults.
A notable 2021 study conducted by researchers at the Centers for Disease Control and Prevention (CDC) revealed that vaccinated adults exhibited a 26% decreased likelihood of intensive care unit admissions and a 31% reduced risk of mortality compared to their unvaccinated
counterparts. These findings underscore the broader protective effects of flu vaccination beyond symptom management, even in cases where vaccine strains may not perfectly match circulating flu viruses due to formulation timelines.
Moreover, emerging evidence highlights

Injection site comfort Precise dosing



Abbott’s INFLUVAC® has been marketed continuously for more than 70 years2
References: 1. Smart Syringe System; Data on file. 2. van de Witte SV, Nauta J, Giezeman-Smits KM, de Voogd JM. Trivalent inactivated subunit influenza vaccine Influvac®: 30-year experience of safety and immunogenicity. Trials in Vaccinology, 2012;1:42-48. S2 Influvac® Subunit 2024 (Suspension for Injection). Each 0,5 ml inactivated influenza vaccine contains: A/Victoria/4897/2022 (H1N1)pdm09-like strain (A/Victoria/4897/2022, IVR-238) 15 μg; A/Thailand/8/2022 (H3N2)-like strain (A/Thailand/8/2022, IVR-237) 15 μg; B/Austria/1359417/2021like strain (B/Austria/1359417/2021, BVR-26) 15 μg. South Africa: T/30.1/581, Botswana: BOT1702969, Kenya: 4273, Namibia: NS2 04/30.1/1530, Mauritius: PB12811/-5/2016, Tanzania: TZ17H0046 and Zimbabwe: PP 2016/18.2/5264. For full prescribing information, refer to the professional information approved by the Regulatory Authority. Abbott Laboratories S.A. (Pty) Ltd, Reg. No. 1940/014043/07, Abbott Place, 219 Golf Club Terrace, Constantia Kloof, 1709. Tel No.: 011 858 2000. Date of publication: January 2024. Promotional Review Number: SAF2297370
additional therapeutic benefits of flu vaccination that extend beyond conventional expectations. Recognised specialists in the field, such as Dr Michelle Barron, senior medical director of infection prevention and control at UCHealth, emphasise the role of flu vaccination in bolstering immune defences against various health threats beyond influenza itself.
Here are four surprising clinical advantages associated with flu vaccination:
1. Cognitive enhancement: Recent research, exemplified by an August 2022 study from the McGovern Medical School at UTHealth, suggests a potential link between flu vaccination and reduced risk of dementia, particularly Alzheimer's disease. This study, involving a sizable cohort of older adults, revealed a remarkable 40% decrease in Alzheimer's disease incidence among vaccinated individuals over a fouryear period, underscoring the vaccine's unexpected neuroprotective effects.
2. Cardiovascular protection: Individuals with a history of cardiovascular disease face heightened susceptibility to flurelated complications, including heart attacks and strokes. Studies, such as the 2018 Canadian study and subsequent research led by the University of Toronto, have demonstrated significant reductions in major cardiovascular events among vaccinated populations, including those with acute coronary syndrome. Mechanistic insights suggest that flu vaccination may mitigate cardiovascular risks by modulating inflammatory processes and stabilising arterial plaques, thereby averting potentially life-threatening complications.
3. Mitigation of complications in chronic conditions: For patients with chronic health conditions like diabetes and chronic obstructive pulmonary disease, flu vaccination represents a crucial strategy for mitigating exacerbations and reducing hospitalisations associated with flu-related pneumonia. Research from institutions such as the University of Minnesota Medical School and the Veterans Affairs Medical Center emphasise the substantial reductions in hospitalisations and mortality rates among vaccinated individuals with respiratory diseases.
4. Longevity enhancement: Compelling epidemiological data, including a comprehensive study conducted in Toronto, suggest that flu vaccination may confer a notable survival advantage, particularly among older adults. The observed 34% reduction in overall mortality underscores the profound impact of flu vaccination on longevity, attributed to both the prevention of flu infections and the attenuation of illness severity in breakthrough cases.
Source: AARP
Multidisciplinary approach in fertility care Highlights from SASREG Congress ‘24
The South African Society for Reproduction and Gynaecological Endoscopy (SASREG) recently concluded its highly anticipated national conference in Umhlanga, KwaZulu-Natal, 08 -10 March 2024.
THE SOUTH AFRICAN SOCIETY for Reproduction and Gynaecological Endoscopy (SASREG) recently concluded its national conference in Umhlanga, KwaZulu-Natal, 08 -10 March 2024. This event brought together reproductive specialist, scientist, embryologist, geneticist, nursing coordinators and psychologists in the field of reproductive medicine to delve into the latest developments and practices shaping modern fertility care.
The conference boasted a scientific programme designed to shed light on the multifaceted approach to contemporary fertility care. From enhanced diagnostics to surgical innovations and discussions on reproductive genetics and legal frameworks, the agenda encompassed various dimensions of reproductive health.
The Friday workshops delved into advanced skills in gynaecological ultrasound and operative hysteroscopy. These hands-
on sessions provided attendees with practical insights and techniques to enhance their proficiency in these critical areas.
Saturday's programme featured indepth discussions and presentations on infertility care, including topics like PCOS management and fertility-sparing surgeries for conditions such as endometriomas and adenomyosis. The debate on evidencebased freeze-all cycles raised discussions on their potential impacts on obstetrical outcomes and epigenetic considerations.
A highlight was lessons learned in fertility preservation in oncology patients over the past 10 years. Prof Michael Grynberg's presentation on the latest European Society of Human Reproduction and Embryology (ESHRE) guidelines underscored the evolving landscape of fertility preservation and its implications for patient care.
The embryology sessions focused on the topic 'add-ons' and their integration into IVF
labs. Experts explored trending literature and global adoption of these techniques. Students presented their latest research, with Samantha Bhengu earning sponsorship from LoRuMiR D for her presentation on 'In vitro embryonic diapause: Predictive potential of seminal oxidative stress in human embryo development'.
The Reproductive Health Group from the University of KwaZulu-Natal under the leadership of Prof Donrich Thaldar presented topics currently under debate in South African law. These discussions included, establishing a dedicated Assisted Reproductive Technology (ART) statutory authority, access of ART to LGBTQ+ patients, and choosing gamete donor.
Sunday's sessions delved into the often-neglected aspects of fertility care, including psychological support for infertile couples and the emerging trends in carrier screening and gender diversity.
Prof Graham Howarth's insights into

medicolegal pitfalls in fertility clinics served as a sobering reminder of the ethical and legal considerations inherent in reproductive medicine.
The conference provided a platform for stakeholders in egg donation agencies to address challenges and underscore their crucial role in facilitating fertility care. Updates on recent legal judgments and court applications in reproductive law, presented by Prof Donrich Thaldar, shed light on the evolving regulatory landscape governing fertility practices.
Recognition was extended to Prof Carin Huyser and Marie-Lena de Beer, honored with lifetime achievement awards for their contributions to embryology training. Dr Paversan Archary and Prof Silke Dyer's ANARA registry, aimed at enhancing IVF outcomes in South Africa, was noted. Lydia Els-Smith was commended for her leadership in creating the SASREG accreditation standards document.





Shaping the future of healthcare amid NHI
While South Africa awaits the President’s sign-off on the National Health Insurance (NHI) bill with bated breath, the 23rd Annual Board of Healthcare Funders (BHF) Conference emerges as a critical platform for industry stakeholders to dissect its implications and strategise the next steps.
THEMED ‘BEYOND BARRIERS: Navigating the Future for Sustainable Healthcare’, industry titans are poised to convene from 4 May to 8 May 2024
to delve deeply into some of the threats to industry sustainability and chart a roadmap to the future the BHF and its stakeholders want. A highlight of this
year's event will be the unveiling of BHFcommissioned research on perceptions around medical schemes and private healthcare. The research conducted an

in-depth analysis of numerous negative comments surrounding the funding industry during the NHI process and objectively tested these for accuracy.
It reveals a narrative that often lacks factual evidence and unfairly portrays the industry in a negative manner. This research not only aims to uncover truths, but also safeguard the long-term sustainability of the industry.
Despite ongoing debates surrounding the NHI bill that the private sector does not support, the conference will debunk these misconceptions head-on, offering evidencebased insights into the critical role private healthcare plays in advancing Universal Health Coverage (UHC) goals.
BHF MD Dr Katlego Mothudi says the industry today is characterised by an integrated approach towards public and private health citizens. “In this respect, the BHF supports UHC and recognises the NHI as one of the mechanisms towards its progressive realisation.” BHF and its members have embraced the principles of the UHC. BHF has actively developed a framework to assist its members in aligning with these principles.
“However, BHF does not support the NHI Bill in its current form due to the unconstitutionality of several of its provisions, its proposed restriction of medical schemes, and the concomitant loss of economic value that will inevitably follow.
“The private health funding sector in South Africa should not be sacrificed in favour of NHI. It is a valuable source of jobs, scarce skills, infrastructure, financial investment, and quality health care. The value it adds to the economy and the support it provides to the public health sector cannot be underestimated.”











“The bill reduces the role of the private sector, and we want those sections removed,” says Dr Mothudi. In fact, he says weakening any aspect of the private health sector will weaken the national health system rather than strengthen it.
In anticipation of the signing of the bill, many parties in the sector are set to challenge the bill. BHF has invited various legal experts to present a way forward for the industry should the bill be signed.
“We believe BHF members are well positioned to play a critical role in the NHI environment and have urged them to fully adopt UHC principles.
This will see them, amongst others, focus on health governance, understanding and providing bene fits that meet the health needs of the population, and redefining the business of medical aid schemes,” he concludes.
Innovation leading the charge in TB’s last stand
Innovative and ground breaking initiatives have brought tuberculosis to a near standstill, with recent advancements finally gaining the upper hand in the fight against this age-old scourge and placing South Africa on the frontline in eliminating the disease once and for all, writes Bada Pharasi, chief executive officer of The Innovative Pharmaceutical Association South Africa (IPASA).
AS THE GLOBAL HEALTHCARE
sector observed World Tuberculosis Day on 24 March, it serves as a stark reminder of the ongoing battle against TB, a disease that continues to afflict millions worldwide. The South African government, as a member of the United Nations, has pledged to the Sustainable Development Goals, which aims to end the disease as an epidemic by 2030. South Africa is well on track to achieve this, committing to reducing TB cases by as much as 80%, and TB-related deaths by 90% by 2030 compared with 2015 levels.1 With the World Health Organization setting a benchmark to reduce TB-related deaths by 50% by 2025, SA has already met and exceeded this. So much so that in 2022, 280 000 people in the country contracted the disease, down from 552 000 cases in 2015.1
The incidence of TB cases per 100 000 individuals has also significantly decreased. In 2022, 468 out of every 100 000 individuals in South Africa contracted TB, a notable decline from 988 per 100 000 individuals reported in 2015. This represents a 53% decline in TB incidence between 2015 and 2030, aligning closely with the WHO's milestone targets, and placing the country in a favourable position to attain the SDG goal by 2030.1
According to reports by the government, new innovative medical interventions and developments have been linked with this success, including expanded screening activities with TB Health Check, the use of digital chest X-rays for TB screening, and the introduction of an SMS-based TB results notification system to improve a patient’s linkage to treatment.2
Since the initial discovery of the first TB cure in the 1940s, the pharmaceutical industry as part of healthcare has persistently endeavoured to enhance the standard of care for individuals affected by TB. In the past, the conventional approach to preventing TB among individuals exposed to the disease involved administering isoniazid daily for six months or longer. However, over the last decade, this approach has evolved with the introduction of new preventive therapy regimens, which can be taken for shorter durations, ranging from four to just one month.3
While three new medicines developed to treat the disease have been registered in South Africa in the past decade, some presented side effects and the need for long-term use. Fortunately, findings from a study conducted in South Africa on a new experimental medicine, quabodepistat, have shown significant promise. Quabodepistat, when combined with bedaquiline and delamanid, has proven to be safe and efficacious in treating drug-susceptible TB.4 The experimental
new medicine has performed well in a phase 2b/c trial, meaning that it can now proceed to a pivotal phase 2 trial.4 While the eventual availability of these innovative medicines will bolster the fight against the disease with even greater efficacy, navigating through
bureaucratic obstacles remains a significant hurdle for their realisation.
There is a great need to foster an environment that encourages and supports pharmaceutical innovation. This includes increased public and private
partnerships and investment into the research, development, and manufacturing process; the relaxation of policy, regulatory, and financing channels; and, finally, new approaches to bridge the gap between diagnosis and treatment.
Building on nearly a hundred years of experience in diabetes care:
~30 million People living with diabetes trusting our products annually
>7 billion Units produced globally on an annual basis
>100 Countries where our products are used to aid with the management of diabetes












Informed consent in healthcare
A vital component of patient autonomy in South Africa
In healthcare, the principle of informed consent stands as a cornerstone, emphasising the fundamental right of patients to make autonomous decisions about their healthcare.
IN SOUTH AFRICA, a nation deeply rooted in diverse cultural traditions and a complex healthcare landscape, informed consent takes on heightened significance. Within this dynamic context, obtaining informed consent serves as a critical safeguard for both patients and healthcare providers, ensuring transparency, respect for autonomy, and ethical integrity in medical decision-making processes.
UNDERSTANDING INFORMED CONSENT
In essence, informed consent refers to the process through which healthcare professionals engage with patients to provide comprehensive information regarding proposed treatments, procedures, or interventions. This process enables patients to understand the nature, risks, benefits, and alternatives associated with their healthcare choices, empowering them to make informed decisions that align with their values, preferences, and goals. Moreover, informed consent necessitates that patients possess the capacity to comprehend this information and voluntarily consent to or refuse medical interventions without coercion or manipulation.
LEGAL AND ETHICAL FRAMEWORK
In South Africa, the right to informed consent is enshrined in various legal and ethical frameworks, including the National
Health Act of 2003 and the South African Constitution. These statutes underscore the importance of patient autonomy and the duty of healthcare providers to respect patients' rights to self-determination and bodily integrity. Furthermore, professional codes of ethics, such as those outlined by the Health Professions Council of South Africa (HPCSA), mandate that healthcare practitioners prioritise informed consent as an essential component of ethical medical practice.
Healthcareproviders must receive adequatetrainingand supporttoeffectively communicate with patientsfromdiverse backgrounds, utilisingculturally sensitiveapproaches andplainlanguage toconveymedical information
CHALLENGES AND CONSIDERATIONS
Despite the clear legal and ethical imperatives surrounding informed consent,
several challenges persist in its practical implementation within the South African healthcare system. Language barriers, low health literacy levels, and disparities in access to healthcare services pose significant hurdles, particularly in rural and underserved communities. Additionally, cultural beliefs, norms, and historical mistrust of the medical establishment may influence patients' perceptions of informed consent and decision-making processes.
Moreover, the realities of resource constraints and time pressures within healthcare settings can sometimes lead to shortcuts in the informed consent process, potentially compromising the quality and comprehensiveness of information provided to patients. In certain cases, power differentials between healthcare providers and patients may also inhibit open communication and shared decision-making, undermining the principle of autonomy.
PROMOTING INFORMED CONSENT
Concerted efforts are needed at multiple healthcare system levels to address these challenges and uphold the principles of informed consent. Healthcare providers must receive adequate training and support to effectively communicate with patients from diverse backgrounds, utilising culturally sensitive approaches and plain language to convey medical information. Moreover,
integrating decision aids, visual aids, and interpreters can enhance patients' understanding and facilitate meaningful engagement in the consent process.
Two courses on the GoodX Online Short Courses Platform (courses.goodx.co.za) that can significantly aid practitioners in navigating the intricacies of informed consent and addressing communication challenges are:
1. Communication in Healthcare Practice Management.
2. Informed Consent in Healthcare.
The first course provides practitioners with techniques for effective patientprovider communication, including strategies for addressing linguistic barriers to understanding. The second course delves into the legal requirements underpinning informed consent and explores real-world case studies to help practitioners navigate ethically complex situations.
CONCLUSION
In South Africa, informed consent is more than a legal requirement – it embodies a commitment to respecting patients' autonomy, dignity, and rights within the healthcare setting. The importance of practitioners being upskilled in the knowledge necessary to navigate the everchanging legal aspects of informed consent cannot be overstated.

















Diosmectite, a natural colloidal clay, is widely used globally for various gastrointestinal conditions, including acute diarrhoea in both children and adults, as well as adjunct treatment with oral rehydration solution.
D
IOSMECTITE IS USED in the symptomatic treatment of chronic functional diarrhoea and pain associated with functional bowel diseases in adults. Numerous randomised controlled trials
and meta-analyses have demonstrated its efficacy, attributing its benefits to its potent coating properties on the gastrointestinal mucosa, thanks to its leaflet structure and high plastic viscosity.
Pharmacological studies have elucidated diosmectite's mechanisms of action, which include stabilising mucus and protecting the gastrointestinal mucosa against aggressive agents like hydrochloric acid and bile acids.
Smart by Nature.1 Powered by Science.2,3
Diosmectite is a natural therapeutic clay1,4
and pain associated with functional bowel disease in adults5,6,7





Diosmectite also exhibits high adsorption capacity against enterotoxins, bacteria, and viruses, decreases inflammation mediators, reinforces intestinal mucosa barrier, and restores epithelial barrier defects induced by proinflammatory cytokines. Moreover, it reduces hypersensitivity to colorectal distension, making it effective in treating chronic functional diarrhoea and diarrhoeapredominant irritable bowel syndrome (IBS) when administered at doses of 3g three times a day for 2-8 weeks.
Given the prevalence of chronic diarrhoea associated with microbiota alterations, researchers sought to assess diosmectite's impact on the gut microbiome during long-term use. A prospective, open-label, non-comparative, multi-center international study administered diosmectite 3g three times a day over five weeks to evaluate its effect on elemental impurities and the bowel microbiota composition in subjects with chronic functional diarrhoea.
The study confirmed diosmectite's clinical benefit in reducing overall Bristol Stool Scale (BSS) scores, particularly in cases of more severe baseline symptoms. Despite its efficacy in improving transit, there was no observed alteration in the microbiota composition even at the highest resolution attained by complete shotgun sequencing-based metagenomic gene scans. This contrasts with treatments for other chronic conditions like type-2 diabetes or neuropsychological disorders, where drug-microbe interactions can significantly alter the microbiota.
The lack of impact on the microbiota suggests that diosmectite can be safely administered for extended periods (up to five weeks in the study) without causing microbiota-mediated gut symptoms such as bowel distension or intestinal inflammation. However, further investigations are warranted to assess potential modulation of microbiome functions through assessments of gene expression (metatranscriptome) or metabolome. Nonetheless, the study's findings highlight diosmectite's safety and efficacy in chronic diarrhoea management, providing reassurance for its long-term use in clinical practice.
CONCLUSION

In conclusion, diosmectite demonstrates efficacy and safety in managing acute and chronic gastrointestinal transit disorders. Its long-term administration in chronic diarrhoea does not appear to adversely impact the intestinal microbiota composition, as evidenced by this study's findings. Thus, diosmectite stands as a viable treatment option for chronic diarrhoea without posing risks associated with microbiota-mediated gut symptoms.
Perinatal comparisons
Second-stage caesarean section vs vacuum extraction
The comparison between assisted vaginal delivery (AVD), specifically vacuum extraction, and caesarean section (CS) during the second stage of labour presents a nuanced landscape of benefits and risks for both mothers and newborns.
DESPITE A GLOBAL increase in CS rates, AVD, particularly vacuum extraction, remains underutilised, especially in resource-limited settings like sub-Saharan Africa. This is often linked to declining proficiency in AVD skills among healthcare providers. However, evidence suggests that increased AVD utilisation can serve as a cost-effective alternative to high CS rates, particularly in such settings.
Eze et al (2020) conducted a retrospective analysis comparing perinatal outcomes of babies delivered by secondstage CS versus vacuum extraction in a resource-poor setting, particularly Nigeria. The study aimed to address the gap in local data regarding the comparison of AVD and CS during the second stage of labour, providing insights to enhance decisionmaking in obstetric units in similar settings.
The study spanned five years and involved data extraction from the Federal Teaching Hospital of Abakaliki (FETHA) in Nigeria. Among 9 287 births, 559 women met the study criteria, with 211 undergoing AVD and 348 undergoing second-stage CS. The most common indication for both interventions was prolonged second stage of labour. Perinatal outcomes, including foetal death and severe perinatal outcomes, were comparable between AVD and CS groups. However, differences were observed in decision-to-delivery intervals and the likelihood of opting for AVD, with resident doctors showing less inclination toward AVD use. The study's findings align with previous research indicating comparable neonatal outcomes between AVD and CS procedures. However, they contrast with a study conducted in Israel, where CS was associated with poorer neonatal outcomes than AVD. The study underscores the importance of considering individual circumstances and tailoring the choice between AVD and CS, especially in resource-limited settings where maternal aversion to CS is prevalent.
The mode of birth in subsequent pregnancies following VE or secondstage CS. A study conducted at Mulago Hospital in Uganda revealed favourable outcomes associated with VE, including lower infection and haemorrhage rates, shorter decision-to-birth intervals, and reduced risks of birth asphyxia and severe maternal morbidity compared to secondstage CS. Subsequent pregnancies among primigravidas who underwent VE or second-stage CS during their first delivery were compared at Kawempe National Referral Hospital. VE in the first pregnancy was associated with a higher likelihood of subsequent vaginal birth and shorter hospital stays compared to secondstage CS, emphasising the importance of
considering birth mode implications for subsequent pregnancies.
The key recommendations include healthcare providers weighing the benefits of VE in reducing the risk of repeat CS and
subsequent complications, incorporating women's preferences for birth modes into counselling.
Additionally, increasing education and training in vacuum extraction among
healthcare providers, particularly junior doctors, is essential to decrease CS rates worldwide. References























Long-term nitrate therapy in angina management: Revisiting isosorbide-5-mononitrate
The management of angina pectoris, a prevalent symptom of ischemic heart disease, poses a significant challenge in cardiovascular medicine.
This is a summary of a CPD-accredited article available on www.medicalchronicle.co.za
WHILE TRADITIONAL PHARMACOLOGICAL treatments such as beta-blockers, nitrates, and calcium channel blockers have been fundamental, ongoing research continues to explore their efficacy and role in longterm management. Recent studies have
underscored the persistent symptomatic burden of angina despite traditional therapies, prompting investigation into both older agents and anti-inflammatory drugs as potential treatment avenues.
Balla et al's research emphasises the need for exploring alternative treatments for
angina due to the persistent symptomatic burden despite traditional medications.
Additionally, investigations into antiinflammatory agents such as canakinumab have been prompted by evidence suggesting inflammation's role in coronary artery disease progression. However, selecting the optimal treatment for angina remains challenging due to variations in pathophysiologies and comorbidities among patients. There is a growing consensus for a more individualised approach to angina management, surpassing conventional treatment hierarchies. Manolis et al's study on patients' perceptions of stable angina highlights significant differences in how various demographic groups experience and cope with the condition. This study underscores the impact of angina on patients' quality of life, particularly in vulnerable groups such as women, younger patients, and those with recent diagnoses.


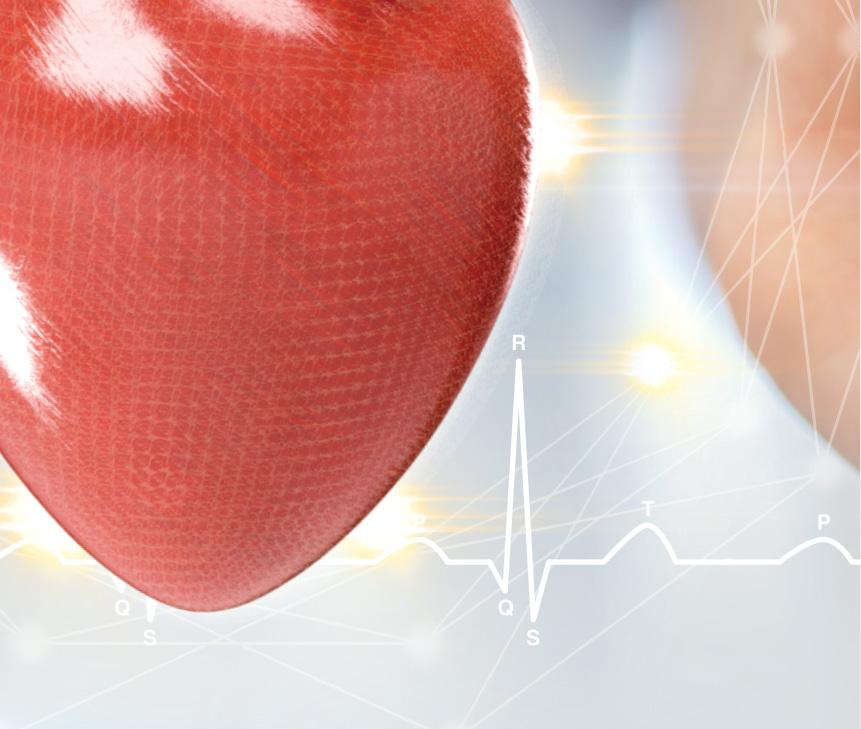



The study by Thadani et al provides valuable insights into the role of longacting nitrates, specifically isosorbide5-mononitrate (IS-5-MN), in angina management. IS-5-MN was found to improve exercise performance without evidence of tolerance development or rebound increase in anginal attacks, making it a viable option for long-term anti-ischaemic therapy. Despite the emergence of newer treatment modalities, nitrates remain fundamental in alleviating symptoms and preventing cardiovascular events in chronic coronary syndromes. However, the optimal choice and sequencing of antianginal drugs remain debatable, requiring tailored drug therapies based on individual patient characteristics and preferences. The pharmacokinetic profile of isosorbide mononitrate indicates its favourable characteristics, making it a viable option for long-term anti-ischaemic therapy. Its straightforward pharmacokinetics and high bioavailability contribute to its efficacy and tolerability across various patient populations. While nitrates have shown efficacy in improving exercise performance and reducing angina attacks, challenges such as limited improvement in quality of life and adverse effects like headaches and hypotension persist. Various regimens, including intermittent and continuous administration, have demonstrated beneficial effects, but considerations must be made regarding tolerance development and adverse effects.
CONCLUSION
Long-term nitrate therapy, remains an essential component in the management of angina pectoris. As our understanding of angina's pathophysiology evolves and newer treatment modalities emerge, adopting a personalised approach is crucial for good patient outcomes. Nitrates continue to provide symptomatic relief and improve exercise tolerance in patients with stable coronary disease, reinforcing their significance in angina management.
The role of inhalation therapy in the management of the common cold
The White Paper outlines expert consensus and usage recommendations regarding inhalation therapy for managing symptoms associated with the common cold.
INHALATION THERAPY INVOLVES inhaling steam or medicated vapours generated from various sources to alleviate symptoms or manage medical conditions. The authors, Natalie Schellack, Retno S Wardani, Tamlyn Govender, Abhay Dhulap, and Prapti Utami discuss the efficacy, methods, benefits, and safety considerations of inhalation therapy.
The common cold, caused by a viral infection in the upper respiratory tract, presents symptoms such as nasal congestion, cough, sore throat, and headache. Inhalation therapy, particularly steam inhalation, is highlighted as a targeted method for delivering relief to the respiratory system, relieving symptoms effectively and rapidly.
Two primary methods of inhalation therapy are described: steam (wet) inhalation and direct (dry) inhalation. The former involves inhaling vapours from hot water, often infused with herbs or essential oils, while the latter entails inhaling vapourised herbal ingredients typically applied through medicated chest rubs.
Twoprimarymethods ofinhalationtherapy are described: steam (wet)inhalationand direct(dry)inhalation
The authors emphasise the benefits of inhalation therapy in providing fast symptomatic relief, thinning and loosening mucus, and preventing symptom exacerbation. The guideline recommendations from various health authorities, including the World Health Organization and the American College of Chest Physicians, endorse inhalation therapy for managing common cold symptoms.
Key herbal ingredients such as menthol, eucalyptus oil, and camphor are commonly used in inhalation therapy and are well-established for their efficacy in relieving cough and cold symptoms. Safety considerations are also addressed, particularly regarding patient profiles, age appropriateness, and the risk of steam inhalation burns, especially in paediatric patients.
The authors highlight the need to promote safe and effective inhalation therapy among healthcare professionals and patients. General tips for safe and effective steam inhalation are provided, including using clean hot water, maintaining proper distance, and following manufacturer's
instructions for steam inhalation devices.
CONCLUSION
The article provides comprehensive insights into the use of inhalation therapy
for managing common cold symptoms, highlighting its efficacy, methods, safety considerations, and guideline recommendations. It stresses the importance of promoting awareness and
proper education to ensure the safe and effective use of inhalation therapy in both clinical and home settings. References



The evolution of dexamethasone From neurosurgery to modern therapeutics
Dexamethasone, a potent glucocorticoid with long-acting properties, has etched its mark as one of the most indispensable medications in the realm of neurosurgery.
ITS JOURNEY FROM a rheumatological remedy to a cornerstone in treating brain tumours showcases the dynamic interplay between medical innovation and therapeutic adaptation.
In 1958, Glen E Arth synthesised dexamethasone, a 16-alpha-methylated analogue of cortisone, primarily for managing rheumatoid arthritis. However, it was Joseph Galicich, a resident in neurosurgery at the time, who recognised its potential beyond rheumatology. Galicich administered dexamethasone to patients post-craniotomy for tumour excision, witnessing remarkable improvements in paresis, resolution of midline shift, and reduced mortality rates. His advocacy for clinical trials propelled dexamethasone into
oncological therapeutics expands to encompass immunotherapy, the immunosuppressive effects of dexamethasone present a conundrum. How does one manage symptomatic relief without compromising the efficacy of oncological treatments? Despite its enduring presence in medical practice for over six decades, dexamethasone's role in the modern context prompts a re-evaluation, particularly in the face of emerging neuro-oncological paradigms.
Today, dexamethasone is available in various formulations, including intravenous, oral, nasal, ophthalmic, and topical creams, catering to a spectrum of diseases ranging from multiple myeloma to psoriasis. While chronic therapy with glucocorticoids such as dexamethasone is associated with
adoption in medical management. The mechanism of action of dexamethasone, like other corticosteroids, is multifaceted, targeting multiple drug receptors. Its anti-inflammatory prowess primarily stems from its role as an agonist of ligand-bound glucocorticoid receptors, orchestrating signalling pathways that mitigate inflammation. However, the poly-pharmacology of dexamethasone extends beyond anti-inflammatory effects, encompassing interactions with mineralocorticoid receptors, which contribute to side effects such as salt and water retention. Since its inception into the market in 1959, dexamethasone has emerged as one of the premier orally bioavailable corticosteroids, alongside prednisone. With a track record spanning
Medical Chronicle has hosted many successful webinars over the past year. From product launches to CPD-accredited talks, we’ve done it. To be part of these popular events, hosted on platform that requires no downloading, contact:
to severe allergies, asthma, and brain swelling. Its versatility has rendered it a favoured choice among physicians, evident in its ‘off-label’ use in severe Covid-19 cases to alleviate pneumonia symptoms. The RECOVERY clinical trial, validating dexamethasone's efficacy in severe Covid-19, serves as a testament to the enduring legacy of this medication. As medical practitioners navigate the evolving landscape of therapeutic interventions, dexamethasone stands as a testament to the enduring adaptability and efficacy of pharmacotherapy.
REFERENCES
Vazquez S, Gold J, Spirollari E, Akmal S, Hanft SJ. The story of dexamethasone and how it became one of the most widely used drugs in neurosurgery.


Critical care antimicrobials break new ground
To ensure the accessibility and timely administration of essential medicines at South African hospitals, Pharma Dynamics, has launched three new generic antimicrobial products.
1.
FORURI (FOSFOMYCIN), for the treatment of uncomplicated urinary tract infections (UTIs) caused by sensitive E.Coli in adult and adolescent women, and for prophylaxis in diagnostic and surgical transurethral procedures in adult men.
2. Cusyn (daptomycin), indicated for complicated skin and skin structure infections (cSSSI). It is also used to treat Staphylococcus aureus bloodstream (SAB) bacteraemia.
3. Cytagil IV (tigecycline), a glycylcycline related to the tetracycline class of antibiotics, indicated for the treatment of the following severe life-threatening infections in adults eg complicated skin and
skin structure infections and complicated intra-abdominal infections.
Elani van Zyl, critical care product manager for Pharma Dynamics, says the high prevalence of these infections in critical care settings is what prompted them to make more affordable, generic treatments available.
“UTIs are among the most common infectious diseases in the world, especially in developing countries like South Africa where the prevalence ranks highest at 68%. In sub-Saharan Africa, UTIs affect mainly women with 25-30% of those between the ages of 20 and 40 experiencing recurrent infections of three or more a year.“ Staphylococcus aureus is one of the
leading causes of community-acquired and hospital-acquired bloodstream infections ranking second after Escherichia coli. Hospital mortality is high, and reports have indicated that this may range between 15% and 40%. By adhering to treatment guidelines, it is possible to reduce mortality by up to 50%.”
“The introduction of more generic antibiotics into the market offers numerous advantages, such as cost savings, accessibility and resistance management.
“Generic antibiotics are often more affordable than brand-name equivalents, which can significantly reduce healthcare costs for both patients and healthcare systems. Furthermore, increasing the
availability of generic antibiotics also ensures a stable supply, reducing the risk of shortages that can occur with specific brand-name medications.
“Having a variety of antibiotics available, including generics, allow for antibiotic stewardship programmes to rotate medications strategically. This approach can help in reducing the development of antibiotics resistance by minimising the selective pressure on specific antibiotics.”
The introduction of Foruri, Cusyn and Cytagil will improve access to essential treatments and positively impact health outcomes for patients, explains van Zyl.


Join Medical Chronicle for a free, one-hour, CPD-accredited webinar on Unraveling Allergy Mysteries: Unlocking the Power of the new EAACI Guidelines for Diagnosing IgE-Mediated Food Allergies
The webinar is sponsored by Thermo Fisher Scientific

Dr Magnus Borres
Pediatric allergist, MD, MPH, PhD
Date: 13 May 2024
Time: 7:00 pm – 8:00 pm (SAST)
Topic: Unraveling Allergy Mysteries: Unlocking the Power of the new EAACI Guidelines for Diagnosing IgE-Mediated Food Allergies
Presenter: Dr Magnus Borres
CLICK TO REGISTER: https://bit.ly/ThermoFisherWebinar13May24
Dr Magnus Borres is a Swedish Board-certified specialist in Paediatrics since 1988. He is subspecialist in Paediatric Allergology and Immunology as well as in School Health. He has had Pediatric Asthma & Allergy clinic during the last 30 years, presently at Uppsala University hospital, Uppsala, Sweden. Due to his interest in Public Health issues, he has been Director of School Health and Director of Child Health Services (well-baby clinics). He has also been Chief of Department of Pediatrics in Sweden. He is the Global Medical Director Allergy at Thermo Fischer Scientific, Uppsala, Sweden. He graduated from Uppsala University, Medical Faculty 1982 . He then acquired a Master of Public Health degree from Johns Hopkins Medical Institutions, Baltimore, MD in 1984 through a Fulbright Scholarship. After returning
ChronicleMED

to Sweden, he received his PhD degree in 1991 from Linköping University in Paediatric Allergology & Immunology. He now holds a position as adjunct Professor in Pediatrics at the Department of Maternal and Child Health, Uppsala University. His focus in pediatric allergy research is allergy diagnostics. Magnus has published over 190 peer-reviewed scientific publications and as well as 12 book chapters. His recent publications are concerning the clinical utility of IgE testing towards allergen components with focus on food – and respiratory allergies. He has given numerous national and international lectures to medical and lay audiences and is a Fellow of American Academy of Allergy, Asthma, and Immunology.


Understanding the role of zinc in human health
Zinc, an indispensable mineral, is integral to various physiological processes, available naturally in select foods, added to others, and offered as a dietary supplement.
ZINC IS AVAILABLE in lozenges, over-the-counter cold remedies, and denture adhesive creams, emphasising its diverse applications in healthcare.
The significance of zinc in cellular metabolism is multifaceted. It acts as a catalyst for numerous enzymes, contributing to immune enhancement, protein synthesis, DNA replication, wound healing, and cellular signalling. Moreover, zinc supports optimal growth and development across all life stages and, interestingly, is crucial for maintaining the sense of taste.
In the human body, zinc levels approximate 1.5g in women and 2.5g in men, primarily stored in skeletal muscle and bone. Maintaining zinc homeostasis involves intricate processes of absorption, excretion, and reabsorption within the gastrointestinal tract, influenced by dietary intake.
Clinical assessment of zinc status often relies on serum or plasma zinc levels, typically ranging from 80-120mcg/ dL in healthy individuals. However, these measures have limitations, as they can be influenced by various factors such as age, sex, time of blood draw, and physiological conditions.
Ageplaysa significantrolein thepresentation ofzincdeficiency symptoms
Dietary supplements offer a convenient means to address zinc deficiency, available in various formulations and combinations. Zinc absorption from supplements varies depending on the compound, with citrate and gluconate forms exhibiting higher bioavailability. Notably, concurrent intake of iron supplements may impede zinc absorption.
Zinc deficiency is more prevalent in low-income and middle-income countries, affecting approximately 17% of the global population. Manifestations of deficiency encompass a spectrum of health issues, impacting multiple systems including the skin, bones, reproductive, digestive, and immune systems.
Age plays a significant role in the presentation of zinc deficiency symptoms. In infants and children, signs may include diarrhoea, alopecia, delayed growth, and susceptibility to infections. Pregnant individuals and their infants are particularly vulnerable, facing increased risks of morbidity and adverse birth outcomes.
Furthermore, zinc deficiency can lead to sensory impairments, delayed wound healing, and cognitive dysfunction in older adults, underscoring its relevance across the lifespan.
In conclusion, understanding the pivotal role of zinc in human health is imperative for medical practitioners to effectively assess and manage patients' nutritional needs. Heightened awareness
of zinc deficiency and its diverse manifestations is essential for promoting optimal health outcomes globally.
Source: National Institutes of Health
DID YOU KNOW?
It is estimated that about 2 billion people worldwide are zinc deficient 1
In 1999 it was estimated that approximately 45.3% of children aged 1–9 years in South Africa, had an inadequate zinc status 2 A zinc deficiency may lead to:3
• impaired immune function
• mental lethargy
• loss of appetite
• low weight gain
• slow growth
ZINC is an essential mineral involved in numerous aspects of cellular metabolism, and has multiple important roles within the body:3
• Immune support
• DNA synthesis and cell division
• Support of normal growth and development
Daily intake of zinc is necessary, as the body has no specialized zinc storage system.3 Zinc supplementation to maintain a normal serum


Join Medical Chronicle for a free, one-hour, CPD-accredited webinar on Rational use of medications for insomnia
The webinar is sponsored by Pharma Dynamics

Dr Alison Bentley BSc 1978, MBBCh 1982, PhD 2007
Date: 23 May 2024
Time: 6:00pm
Topic: Rational use of medications for insomnia
Presenter: Dr Alison Bentley

CLICK TO REGISTER: https://bit.ly/PharmaDynamicsWebinar23May24
Dr Bentley is a general practitioner who has been seeing patients with sleep problems, both adults and children, off and on over the last 30 years. She ran the first private diagnostic sleep laboratory in South Africa from 1990 to 1998. After joining Wits University she was head of the Wits Dial.a.Bed Sleep Laboratory in the School of Physiology for 10 years. She was the founding chairperson of the Sleep Society of South Africa in 1996 and is the current chairperson of the new South African Sleep Society for Sleep and Health. She served two terms representing Africa on the governing council of the World Association of Sleep Medicine (WASM). She has supervised more than 30 postgraduate students, has over 30 published peer-reviewed articles and two book chapters as well as writing articles for and editing the newsletter for doctors - Sleep Matters for the last 14 years. She has presented over 40 formal invited presentations at local and international conferences. She is currently in private practice and runs a home-based apnea screening company. She recently opened the first clinical sleep research and training clinic in South Africa – the Restonic Ezintsha Sleep Clinic in Parktown, Johannesburg.
ChronicleMED


Are your patients struggling to maintain their sleep throughout the night?
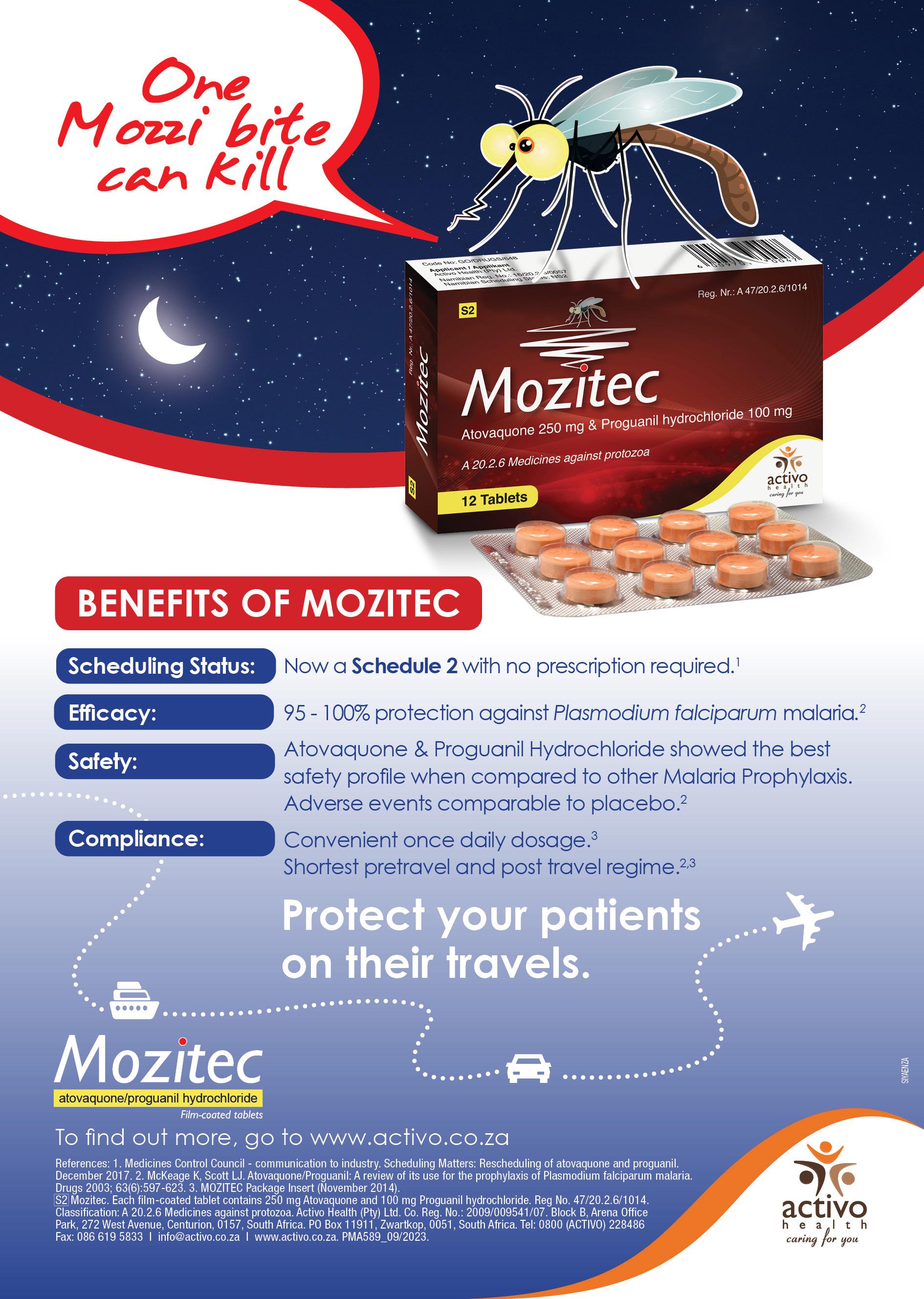
African health ministers pledge to end malaria deaths
In a landmark gathering held in Yaoundé, Cameroon, Health Ministers from African nations bearing the brunt of malaria have committed to intensified efforts to eradicate the disease and halt related fatalities. This commitment is particularly crucial as the African region accounts for a staggering 95% of global malaria deaths.
THE MINISTERS CONVENED to sign a declaration outlining their resolve to provide robust leadership and increased domestic funding towards malaria control programmes. They also pledged to prioritise investment in data technology, adopt the latest technical guidance in malaria control and elimination, and bolster efforts at both national and subnational levels. Furthermore, the ministers committed to ramping up health sector investments to enhance infrastructure, workforce capacity, and programme implementation. They emphasised the importance of multi-sectoral collaboration and the establishment of partnerships for funding, research, and innovation. Importantly, they expressed unwavering dedication to accelerating the reduction of malaria mortality and holding each other accountable for the commitments outlined in the declaration. The conference, cohosted by the World Health Organization (WHO) and the Government of Cameroon, brought together key stakeholders including global malaria partners, funding agencies, scientists, and civil society organisations. Its objectives encompassed reviewing progress and challenges in achieving WHO's global malaria strategy targets, discussing strategies for mitigating challenges and securing funding, and establishing a roadmap for increased political commitment and societal engagement in malaria control.
The African region is home to 11 countries bearing approximately 70% of the global malaria burden. Progress against malaria in these nations has stagnated since 2017, attributed to various factors including humanitarian crises, limited access to quality health services, climate change, and biological threats like insecticide and drug resistance. While South Africa is not one of the 11 high malaria-burden African countries, it does face the challenge of elimination. Globally, funding for malaria control remains insufficient, with only half of the required budget available in 2022. Moreover, despite significant progress in recent decades, the number of malaria cases surged in 2022, particularly in the African region, where the burden remains disproportionately high. Dr Tedros Adhanom Ghebreyesus, WHO director-general, underscored the urgency of addressing critical gaps in funding, access to tools for prevention, diagnosis, and treatment, and the impact of the Covid-19 pandemic on malaria efforts. He emphasised that with political leadership, country ownership, and collaborative efforts, progress against malaria can be revitalised. To accelerate malaria control efforts, WHO and the RBM Partnership to End Malaria introduced the ‘High burden to high impact’ approach in 2018. This targeted strategy focuses on
political will, strategic information, better guidance and policies, and coordinated national responses. Dr Matshidiso Moeti, WHO Regional Director for Africa, hailed the ministerial declaration as a demonstration of strong political will to
reduce malaria's burden in the region. She emphasised the need for renewed urgency and commitment to achieve a malaria-free future. In conclusion, WHO calls for robust commitment, increased funding, sciencedriven responses, climate change
mitigation, research and innovation, and strengthened partnerships to accelerate progress against malaria.
Could menstrual pain be endometriosis?
Endometriosis, a chronic condition affecting the reproductive system, presents significant challenges for women, both in terms of physical discomfort and potential infertility.
UNDERSTANDING THIS CONDITION is crucial for accurate diagnosis and effective treatment.
SYMPTOMS AND DIAGNOSIS
Endometriosis manifests through various symptoms, with the severity ranging from mild discomfort to debilitating pain.
Key indicators include painful periods, chronic pelvic pain, painful intercourse,
ovarian cysts, and infertility. However, it's essential to note that these symptoms are not exclusive to endometriosis and may overlap with other conditions. Diagnosing endometriosis often requires surgical intervention. While symptoms such as dysmenorrhea may suggest endometriosis, they can also occur in a significant portion of the female population. Therefore, conservative therapy, including anti-
inflammatory drugs and birth control, may be initially prescribed. However, if symptoms persist or worsen, surgical evaluation becomes necessary. Minimally invasive gynaecologic surgery (MIGS): These procedures, including laparoscopic and robotic surgeries, provide patients with faster recovery times, reduced pain, and lower infection risks. For patients with refractory pain, infertility, or large


endometriomas, surgical intervention offers a viable solution to alleviate symptoms and improve quality of life. Treatment options: Various treatment modalities exist to manage endometriosis symptoms effectively. Hormonal therapies such as birth control pills and gonadotropin-releasing hormone agonists or antagonists help regulate hormonal fluctuations, thereby reducing the growth of endometrial tissue. Additionally, non-pharmacological approaches such as anti-inflammatory medication, heat therapy, dietary modifications, and regular exercise offer complementary benefits in symptom management.
LOOK OUT FOR THE BIG 5
There are five common signs of endometriosis. Here’s what you should watch out for:
1. Painful periods. Women with endometriosis often have debilitating pain that can prevent them from working or taking care of themselves or family members.
2. Chronic pelvic pain. Sometimes, women have chronic and severe pelvic pain even when they don’t have their periods. This can be due to advanced or refractory disease and scarring.
3. Painful intercourse. Dyspareunia can be due to endometriosis beneath the uterus. During penetration, women with endometriosis might have intense, localised pain.
4. Ovarian cysts. While many ovarian cysts are normal and will resolve without treatment, endometriomas are another hallmark of endometriosis. They can become large and painful and may need to be surgically removed.
5. Infertility. About 25% to 50% of women living with infertility have endometriosis, which can lead to infertility by causing scar tissue as well as damage and inflammation to the fallopian tubes. Research also shows that endometriosis can affect egg quality and reduce the number of eggs in the body.
Conclusion: Endometriosis poses significant challenges for women's health, often requiring a multidisciplinary approach for diagnosis and treatment. As medical practitioners, recognising the hallmark symptoms and understanding the diagnostic process are crucial steps in providing comprehensive care to patients with endometriosis. By incorporating minimally invasive surgical techniques and evidencebased therapies, healthcare professionals can effectively alleviate symptoms and improve the quality of life for individuals living with endometriosis. Encouraging early intervention and proactive management strategies will empower patients to seek timely treatment and achieve optimal health outcomes.
Source: Johns Hopkins Medicine
Enter the era of oral treatment for MS
Multiple sclerosis (MS) is a complex autoimmune disorder affecting the central nervous system (CNS), characterised by inflammation leading to various neurological symptoms.
OVER THE YEARS, management of MS has relied heavily on diseasemodifying drugs (DMDs), typically administered via injections, to alleviate symptoms and slow disease progression. However, the advent of oral therapies marks a significant milestone in MS treatment, offering patients a more convenient and potentially effective option.
UNDERSTANDING THE MECHANISMS OF MS AND THE NEED FOR INNOVATIVE THERAPIES
MS pathology involves inflammation, demyelination, and neuronal loss within the CNS, resulting in a range of debilitating symptoms. Current treatment strategies aim to modulate the immune response and reduce inflammation to prevent further damage to nerve fibres and preserve neurological function. However, the reliance on injectable therapies poses challenges in terms of patient adherence and tolerability.
ENTER FINGOLIMOD: A GAMECHANGER IN MS TREATMENT
Fingolimod, also known as FTY720, emerges as a ground breaking oral therapy for MS. It belongs to a novel class of sphingosine 1-phosphate (S1P) receptor modulators, offering a promising alternative to traditional injectable DMDs.
MECHANISM OF ACTION
Fingolimod exerts its therapeutic effects by modulating S1P receptors, thereby regulating the migration of lymphocyte subsets into the CNS and exerting direct effects on neural cells, particularly astrocytes. Upon administration, fingolimod undergoes phosphorylation to form its active moiety, fingolimod phosphate, which binds to lymphocytic S1P1 receptors, preventing the egress of autoaggressive T cells into the CNS.
CLINICAL EFFICACY
Clinical trials have demonstrated the superior efficacy of fingolimod compared to placebo and traditional injectable therapies in reducing relapse rates, slowing disease progression, and preserving neurological function in patients with relapsing-remitting MS. In September 2010, the US Food and Drug Administration (FDA) granted approval for fingolimod as a first-line treatment for relapsing forms of MS, making it the first oral DMD to receive regulatory approval in the United States.
SAFETY PROFILE AND LONG-TERM CONSIDERATIONS
While fingolimod offers promising therapeutic benefits, its safety profile warrants careful consideration. Adverse events, including first-dose bradycardia
and atrioventricular block, have been reported, necessitating close monitoring, particularly in patients with pre-existing cardiac conditions. Long-term studies are ongoing to assess the safety and efficacy of fingolimod over extended treatment durations.

CONCLUSION
Fingolimod represents a paradigm shift in MS treatment, offering patients a convenient and effective oral therapy option. Its novel mechanism of action, coupled with favourable clinical outcomes, underscores its potential as a cornerstone therapy for relapsing forms of MS. As research in MS continues to evolve, fingolimod stands as a testament to the transformative power of innovation in improving the lives of patients with neurological disorders.
References available on request.



Therapy of inflammatory bowel disease has changed When will we?
A plea for our patients. An opinion from the real world.
WHILE INFLAMMATORY BOWEL
disease has been known for over 100 years, the treatment commonly employed today harks back to the modalities
of the 1970-80s. The advent of truly disease modifying agents capable of putting patients in full remission has not been fully accepted by the health care
practitioners or funders. The ongoing use of old, toxic and ineffective agents needs to end and the medications available for the past 26 years accepted as the standard

care for these symptomatic patients.
IN PRACTICE

The existence of inflammatory bowel disease (IBD), mainly ulcerative colitis and Crohn’s disease, has been known for over 100 years.1 Treatment had two arms, anti-inflammatories such as prednisone to dampen down the symptoms and inflammation, and surgery to remove it. These approaches are toxic and/or mutilating and neither addresses the underlying disease process which is immunological in origin and not well understood.2
The first attempts to modify the disease process was with the use of immunosuppressants such as azathioprine in the 1980s. After a year of therapy one could expect 42% of patients to remain in remission as compared to 7% on placebo.3 Clearly azathioprine was better than placebo but 60% of patients did not benefit at all. Furthermore 6% could not tolerate the treatment, either because of nausea and vomiting or pancreatitis and there was also a low cancer risk. Certainly the use of prednisone and surgery used to have a role to play but in reality, were simply toxic blips on the patient's progressive decline.4,5
On 24 August 1998 our patient's world changed. Infliximab (Remicade, Revellex) was marketed. This anti-TNF (Anti-Tumour Necrosis Factor) agent could miraculously turn the inflammatory process off and within days restore to patients a normal life in quality and duration. These anti-TNF agents and other newer drugs targeting different paths in the immune cascade have been shown to be similarly effective. Research on the best agent for each disease phenotype is ongoing but for the vast majority of patients complete disease control is now possible. What has become apparent is that one of the critical factors is getting the dose right. The measurement of blood levels from the beginning of therapy maximises the effectiveness of these agents. Normally one can expect a patient on an adequate dose to be substantially better within days of starting therapy. If the patient remains ill as determined clinically, endoscopically and biochemically, blood drug levels need to measured and dose optimised. If the levels are already optimum a different agent is probably indicated. Most of the biologicals have been shown to need a specific level for maximum effectiveness but for the small molecules such as tofacitinib the data is not yet convincing.6
The question that needs to be asked is why, after 25 years of experience and the ever-increasing variety of powerful agents
Theuseofoldagentssuch asprednisone,mesalamine, azathioprineandmethotrexateare counterproductive.Theyhavelittleorno effectontheunderlyingdiseaseand have numerous side effects.

available, not all patients have access to these agents? Initially the price of R20 000 a month was an obvious deterrent. Real and perceived side effects further complicated the decision making and delayed the use of these agents. Fortunately the price for the cheapest agent has now reduced to R3 500 a month. Although still expensive, for a life modifying agent this is more affordable.
So again why are patients with inflammatory bowel disease not started on modern therapy on the day of diagnosis? These are chronic diseases with a very small chance of spontaneous remission. In the pre-biological era 20% of patients had relapses every year after 20 years of disease.7 Studies have shown that the earlier the treatment is started the better the outcome.8
There are several reasons for the non-use of these agents:
1. While the cost of the cheapest agent may be manageable most of new agents are still costing R5 000 and R7 500 a month.
2. The main side effect remains an increased susceptibility to tuberculosis. In South Africa with our prevalence of tuberculosis this remains a factor. Nevertheless, with the use of initial serological tests, chest x-rays and clinical judgement, the risk can be mitigated. Fortunately the newer agents have a much lower or no risk of tuberculous infection.9
3. In a strange twist of logic there remains a belief that patients need to earn the new therapies. This means they need to have been treated with largely ineffective therapy for three months prior to commencing modern medicine. This dictum is attractive
to conservative risk averse doctors and cost averse funders. To the patient with abdominal cramps, diarrhoea and sometimes faecal incontinence this delay is impossible to justify.
4. The final factor to consider is the longterm life modifying benefit of these agents. The risk of colon cancer is related to the amount of inflammation in the bowel and the extent of disease. Patients on biologics with normal mucosa have a reduced risk of colon cancer.10 Similarly patients with normal bowel walls do not get the strictures, fistulas and surgical complications that previous patients had to endure. When one reviews older patients treated over the years with prednisone, immunosuppression and surgery it is a tragedy that they did not have access to modern medical therapy. Even more bizarre, many patients in South Africa continue to be treated in this unacceptable fashion. So how should patients with possible IBD be managed in 2024.
There are two groups of patients:
The first is the acutely ill patient with cramps, diarrhoea and possible pyrexia. The first factor to consider is an infective process which, if viral, usually settles down in a few days without treatment. When bacteria are suspected after investigation, antibiotics may be required. In either case the symptoms will usually resolve in five to seven days. When symptoms continue after this, further investigation is usually required. Endoscopy of the colon is normally the next step which with the assistance of histology should diagnose IBD. If the disease activity indices indicate severe disease (a Mayo score >8 or a CDAI >250) it is time to
start a modern biological agent with careful attention to drug blood levels. Conversely if the disease is mild local therapy or even a short course of systemic prednisone may suffice.11
The second group is the patient with months or years of intermittent cramps and diarrhoea. A faecal calprotectin may separate organic from functional disease but inevitably colonoscopy will be needed. Once again, a visual diagnosis of inflammatory bowel disease with assistance of histology should finalise the diagnosis. If IBD is confirmed modern biologics need to be commenced along with the normal monitoring of drug levels. It would seem that all patients with established inflammatory bowel disease need to be started on modern therapy at diagnosis. Interestingly the University of Chicago website states that, “Biological drugs have become the standard of care for people with moderate to severe Crohn’s disease or ulcerative colitis.”12 The use of old agents such as prednisone, mesalamine, azathioprine and methotrexate are counterproductive. They have little or no effect on the underlying disease and have numerous side effects. Similarly routine endoscopy in asymptomatic patients has been replaced with faecal calprotectin done every few years. More expensive imaging with CAT scans and MRI are seldom needed and generally indicate a failure of medical therapy. The new disease management is very different from that of the past with less surgery, endoscopy and hospital admissions. In summary these diseases are now totally manageable with little risk of serious complications so why do we resist? As Winston Churchill said, “When
the facts change, I change my mind. What do you do…...?” In conclusion all our patients deserve to be treated with modern agents. They have already been available for 25 years.
REFERENCES
1. Historical aspects of inflammatory bowel disease J B Kirsner 1 J Clin Gastroenterol. 1988 (10)3:286-97.
2. Guidelines for the management of inflammatory bowel disease in adults. M J Carter, A J Lobo, S P L Travis, (BSG) Gut 2004;53(Suppl V).
3. Surgical management of Crohn’s disease: a state of the art review Elise Maria Meima – van Praag, Christianne Johanna Buskens, et al. Int J Colorectal Dis. 2021; 36(6): 1133–1145.
4. Inflammatory Bowel Disease. Wikipedia
5. A double blind controlled study of azathioprine in the treatment and maintenance of remission in Crohn's disease. Candy S, Wright JP, et al. Gut 1995;37:674-8
6. Optimising Therapies Using Therapeutic Drug Monitoring: Current Strategies and Future Perspectives. Peter M. Irving, Krisztina B. Gecse, Gastroenterology. 2022 162,5, 1512-1524.
7. Outcome of Ulcerative Colitis 20 Years after Diagnosis in a Prospective Population-based Inception Cohort from South-Eastern Norway, the IBSEN Study. Iril Lovise Monstad, Inger Camilla Solberg, Milada Cvancarova et al. Journal of Crohn's and Colitis. 2021,15,969–979.
8. Early Intervention in Ulcerative Colitis: Ready for Prime Time? Virginia Solitano, Ferdinando D’Amico, Eirini Zacharopoulou et al. J Clin Med. 2020, 9 2646.
9. Risk of tuberculosis in patients treated with TNF-α antagonists: a systematic review and meta-analysis of randomised controlled trials Zheng Zhang, Wei Fan, Gui Yang et al. BMJ Open. 2017; 7(3): e012567.
10. Effect of Biologics on the Risk of Advanced-Stage Inflammatory Bowel Disease-Associated Intestinal Cancer: A Nationwide Study
Ryo Seishima, Koji Okabayashi, Hiroki Ikeuchi et al. J Gastroenterol. 2023 Jul 1;118(7):1248-1255.
11. Steroid use and misuse: a key performance indicator in the management of IBD Jonathan Blackwell, Christian Selinger, Tim Raine et al. Frontline Gastroenterol. 2021; 12(3): 207–213.
12. Biologics and Inflammatory Bowel Disease www.uchicagomedicine.org › conditions-services › inflammatory-bowel-disease › treatment › biologicsand-inflammatory-bowel-disease-ibd-crohns-colitis
The principles of harm reduction
The concept of Harm Reduction includes abstinence as one of the possible goals for substance abusers. However, many clients are unwilling to pursue the goal of abstinence because for them, abstinence represents a submission to a ‘Symbolic Controlling Authority’.
MODERATION GOALS ARE more acceptable because they reflect an autonomous choice that offers a way out of the ‘Submit or Rebel’, bind.
The goal is to support the client, in going as far as they possibly can towards the harm reduction ideals of ‘optimal health’, self-sufficiency, self-actualisation, and satisfaction in the world of relationships.
RELATIONSHIP IS THE KEY TO SUCCESSFUL HARM REDUCTION
By accepting the client’s definition of the problem as the legitimate starting point for intervention, harm reduction addresses that which motivates the client to seek help, meet the client’s needs and facilitates a positive treatment alliance.

THE BENEFITS OF HARM REDUCTION ASSOCIATED WITH SUBSTANCE ABUSE
Substance abuse varies along a continuum of negative consequences. Harm reduction seeks to assists users in modifying their use in the direction of reduced harm through:
• Needle exchange programmes and fentanyl testing to prevent infections and overdoses
• Medication-assisted treatment and opioid substitution therapies for withdrawal and cravings
• Safer use education and non-judgmental messaging to promote support-seeking
• Supervised consumption for safer drug use
• Access to naloxone for opioid overdose reversal
• Scientifically proven alternatives to smoking for nicotine/tobacco users.
This approach avoids and I quote, “The pitfalls of more global and arguable questions such as ‘Am I an addict’ or ‘Do I have a disease’?”
This approach helps to maintain a more concrete and molecular focus on discovering the specific harmful aspects of substance use and helps develop specific goals to address them. Harm Reduction implemented appropriately focuses on small incremental steps in the direction of harm reduction as legitimate goals.
These might be steps towards abstinence or moderation. It might also address other issues that motivate patients such as resolving ambivalence about substance abuse, using safer alternatives, preventing overdose and the resolution of emotional and interpersonal issues that promote substance use.
The Harm Reduction Model (Week 13: Addiction and Substance-Related Disorders Flashcards | Quizlet)
Harm reduction interventions are evidence-based public health interventions that can be used to support clients who use psychoactive substances such as alcohol, tobacco and other drugs.
It is important to work around the goals the client is motivated to pursue that will lower the threshold to entry by the client for treatment. Small steps may lead to other small steps as people’s confidence in their ability to change increases, they learn that positive change is possible.
DE-STIGMATISING SUBSTANCE USE
The principle of harm reduction recognises that much of the harm associated with substance use is due to society dealing with substance users in a stigmatising, devaluing, coercive and punitive ways.
The negative attitude may exist not only in the treating providers, but in the substances users themselves.
In the treating providers, they have a potential to ‘contribute to negative counter transference reactions that may be expressed in punitive angry reactions to clients who are substance users’.
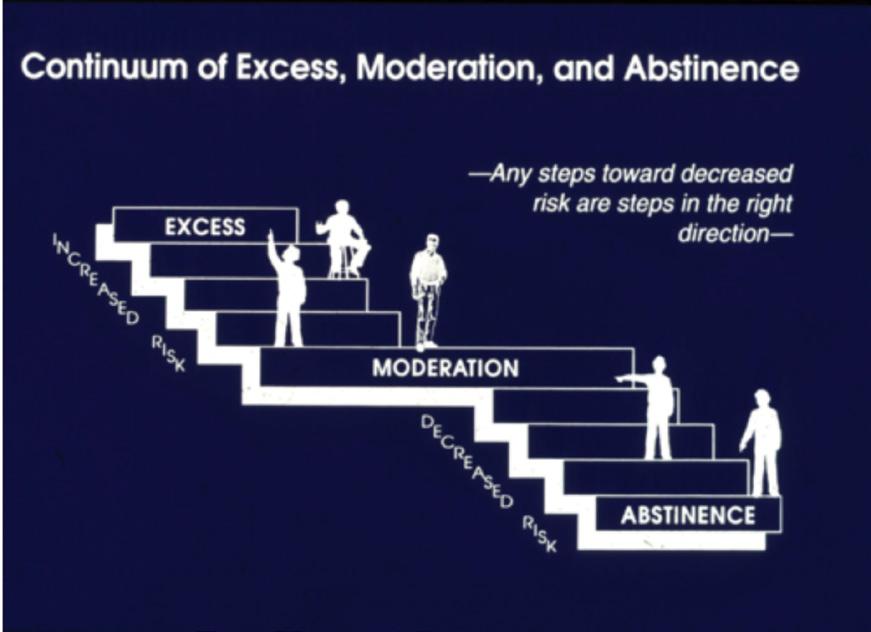
TREATMENT IMPLICATIONS
These principles have the potential for improving the treatment of active substance users at two levels.
1. “As an umbrella concept, harm reduction suggests the need for an integrated treatment


system with linkages across the spectrum of treatment modalities that are matched to the needs of the people along the spectrum of diversity.
2. As a therapeutic principle, harm reduction has implications for how therapy is conducted in the room with clients at every stage of psychotherapy. Starting with the initial engagement and assessment, through the processes of goal setting and the facilitating of change.”
ENGAGMENT AND ESTABLISHING A THERAPEUTIC FOCUS
“It is important to recognise that the therapeutic alliance is the cornerstone of psychotherapy, and it serves to anchor the client in the treatment programme by creating a context of relative safety in which work of therapy can proceed”.
One of the core slogans of the harm reduction movement is ‘start where the client is at’. The therapeutic focus is around the client’s reason for coming for treatment.
It is important not to meet the client with prior assumptions. Prior assumptions about the client should be seen as counter transference reactions that have the possibility of derailing the treatment from the onset. It is important to make harm reduction position explicit at the outset and is a way to counter the client’s expectations of being treated coercively.
Every attempt must be made to prevent the client from being ambivalent about the action of substance abuse. [Journal of Substance Abuse Treatment, Vol 25, Issue 4, December 2003, Pages 249-256].
FOUNDATIONAL PRINCIPLES
CENTRAL TO HARM REDUCTION
“Harm reduction incorporates a spectrum of strategies that include safer use, managed use, abstinence, meeting people with substance use disorders (SUD), ‘Where they are at’, and addressing conditions of use along with the use itself.”
Harm reduction demands that interventions and policies designed to serve the people with SUD reflects specific individual and community needs. There
is no universal definition or formula for implementing harm reduction.
The principles that are central to harm reduction
1. Accepts that licit and illicit substance (tobacco, drugs etc) use is part of the world. It is necessary to work to minimise its harmful effects rather than simply ignore or condemn them.
2. SUD is a complex, multifaceted phenomenon that includes behaviours from severe use to total abstinence. However, there are some ways of using substances that are clearly safer than others.
3. A criteria for successful interventions and policies should promote quality of individuals and the community life and wellbeing and not necessary the association of substance abuse.
4. Calls for non-judgemental, non-coercive provision of services and resources to people with SUD and the communities which they live to assist them in reducing attendant harm.
5. Important to include people with SUD and those with a history of SUD routinely have a real voice in the co-creation of programmes and policies designed to serve them.
6. There must be an emphasis and the need to affirm that people who use these substances themselves as, “Primary agents of reducing the harms of their drug use and seeks to empower people with SUD to share information and support each other in strategies which met their actual conditions of use.”
7. The programme employed must recognise the realities of poverty, class, racism, social isolation, post trauma, sex-based discrimination and other social inequalities affect both people’s vulnerability to and capacity for effectively dealing with substance related harm.
8. The foundational principles must not attempt to minimise or ignore the real and tragic harm and danger that can be associated with licit and illicit substance use. [National harm Reduction Coalition, Manhattan and Oakland].
Preventing and managing pink eye outbreaks
In light of recent reports from the KwaZulu-Natal Department of Health regarding an outbreak of pink eye in select areas of the province, it is crucial to understand the nature of this condition and the steps necessary for prevention and management.

DR NISHEN GOUNDER, a general practitioner at Netcare Medicross Malvern, provides invaluable insights into pink eye, its causes, symptoms, and preventive measures to curb its spread within communities.
UNDERSTANDING PINK EYE
Pink eye, or conjunctivitis, is characterised by inflammation of the conjunctiva, the thin membrane covering the whites of the eye and the inner eyelid. It can stem from viral or bacterial infections, allergic reactions, or environmental irritants.
Dr Gounder emphasises the discomfort associated with pink eye, including itching, pain, swelling, fluid discharge, and a gritty sensation akin to having sand in the eye.
MODES OF TRANSMISSION
Both viral and bacterial forms of pink eye are highly contagious and easily spread through close contact and contaminated hands, particularly in communal settings like schools or workplaces. Dr Gounder stresses the importance of public cooperation in preventing further transmission.
VIRAL VS BACTERIAL PINK EYE
Viral pink eye, often accompanying symptoms of the common cold, manifests with mild discomfort that typically resolves within one to two weeks without specific treatment. Conversely, bacterial pink eye exhibits distinctive features such as yellow, white, or green discharge, requiring antibiotic intervention to alleviate symptoms effectively.
RECOGNITION OF SERIOUS SYMPTOMS
Certain symptoms warrant immediate medical attention, including severe eye pain, vision disturbances, sensitivity to light, or severe headaches accompanied by nausea. Medical professionals should be vigilant in identifying and addressing such indications promptly.
Top tips for prevention and treatment:
1. Promptly consult a general practitioner if pink eye is suspected and adhere to prescribed treatment.
2. Ensure the issuance of a sick note during the recovery period.
3. Emphasise stringent hygiene practices, including frequent handwashing and sanitisation, to prevent transmission.
4. Minimise contact with individuals exhibiting pink eye symptoms and avoid sharing personal items.
5. Discontinue contact lens usage upon suspicion of pink eye.
6. Seek immediate medical advice for severe symptoms or vision changes.
7. Provide tailored guidance to
immunocompromised patients for optimal management.
8. Practice thorough hand hygiene and prevent cross-contamination at home if diagnosed with pink eye.
9. Prioritise paediatric care by promptly addressing symptoms in infants and young children.
CONCLUSION
In conclusion, proactive measures by medical professionals, coupled with public awareness and cooperation, are pivotal in mitigating the spread and impact of pink eye outbreaks. By adhering to stringent hygiene protocols, promptly seeking medical advice, and adopting preventive measures, communities can effectively combat the transmission of pink eye and safeguard public health.

















Over half of doctors suffer abuse from patients
Over half of the doctors who responded to a Medical Protection Society (MPS) survey (58%) say they have experienced or witnessed verbal abuse, physical violence or damage to their work premises from patients or their relatives in the past 12 months, with a quarter (24%) saying such abuse is impacting their mental wellbeing.
IN THE MPS survey of more than 660 healthcare practitioners, a third (34%) said they have seen more abuse recently, than during the Covid-19 pandemic. Nearly two-thirds (65%) said incidents of abuse were not taken seriously by the authorities, while 80% of respondents who were considering leaving the healthcare profession cited an increase in abuse as an influence for their decision.
The release of the survey results come in the tragic aftermath of the murder of Dr Michael Isabelle, who was killed at his Dobsonville practice in Soweto late last month. Healthcare practitioners who took part in the survey commented anonymously about their experiences of being threatened and abused at work.
One healthcare practitioner said: “I have regularly witnessed patients abusing doctors and saying that doctors have taken an oath to serve and should therefore accept abuse.”
Another said: “I have been verbally abused and threatened by my last patient because of the unavailability of the medication I prescribed.”
Another added: “Due to fatigue and everyday stressors, no one has the energy to report issues to HR or management instead you find yourself too depressed to work in that environment.”
MPS, which protects the professional interests of over 30 000 healthcare practitioners in South Africa, said the survey results show the worrying impacts of violence at work.
Dr Volker Hitzeroth, medicolegal consultant at MPS, said: “These survey results make for sombre reading and demonstrate how abuse and violence at work can severely impact healthcare practitioners’ mental wellbeing. This is on top of a range of other pressures which make for an extremely challenging environment – including staff, medicine and equipment shortages as well as load-shedding.
“What is perhaps worse is the notion that abuse is now just ‘part of the job’, with healthcare practitioners accepting that there is no accountability for the perpetrators of abuse, and little support available to help them tackle the effects of it on their mental wellbeing.
“Experiencing and witnessing incidents of physical, sexual or verbal abuse can have a lasting and profound impact on mental wellbeing and this can be damaging for the individual as well as for patient care. It
DOCTORS WHO PARTICIPATED IN THE MPS SURVEY COMMENTED ANONYMOUSLY:
“Patients become abusive when they do not want to pay for medical services rendered to them.”
“Sadly there isn’t a forum to discuss these issues and there is no avenue for accountability.”
“After Covid-19 people are under enormous pressure, emotionally and financially. They tend to lash out because of that.”
“I have been verbally abused and threatened by my last patient because of the unavailability of the medication I prescribed.”
“Due to fatigue and everyday stressors, no one has the energy to report issues to HR or management instead you find yourself too depressed to work in that environment.”
“Families and patients expect to be seen immediately for routine treatment and refuse to accept that other patients might have more urgent needs. Doctors are expected to be super-human.”
“I have regularly witnessed patients abusing doctors and saying that ‘doctors have taken an oath to serve’ and should therefore accept abuse.”
“Abuse from patients and families are common. But they are abusive because they are scared and frustrated. It is understandable. The way to handle it is by building a rapport and trust. The problem lies in numbers. If I have a bit of time with patients and family, that can be done easily. When I have 20 patients waiting, no stock and zero morale in the unit, it is hard to do.”
“In my experience there is zero attempt on the part of the authorities or the hospital groups to protect healthcare workers from abuse by patients and/or their relatives.”
“Patients and families are aggressive and confrontational. I sometimes feel threatened.”
can also result in healthcare practitioners needing to take time off work, and even quitting medicine altogether.
Dr Hitzeroth said the survey results highlighted the need for more to be done to tackle patient abuse and improve support for doctors who experience such behaviour.
“We need to see more local mental wellbeing resources established so those healthcare practitioners struggling due to abuse and violence at work, and other wellbeing issues, can access appropriate support. “It is also clear that we need a greater security presence at all healthcare facilities, clear signage telling patients that abuse is not acceptable, and warnings to patients when they see a doctor that abuse will not be tolerated. Management of both private and public facilities also need to start taking a firm and consistent line when dealing with patient abuse so that when something happens there is a swift and clear response to ensure the behaviour is never repeated.
“In addition, MPS will share these survey results with the HPCSA and raise the possibility of the regulator strengthening its National Patients’ Rights Charter (as set out in Guidelines for Good Practice in the Health Care Professions), by introducing clearer responsibilities for patients and their
accompanying family members to refrain from any form of abuse, threats, or violence and detail what steps may be taken in the event such acts occur.”
Dr Hitzeroth continued: “In our survey, 80% of respondents who are considering leaving the healthcare profession cite increasing abuse from patients or their families as an influence for their decision, while 68% who are looking to leave South Africa to work elsewhere cite abuse as an influence. “If we don’t do more to tackle this issue, sadly we may lose many more healthcare workers at a time when the profession can least afford it.”
BACKGROUND
• For further information contact pressoffice@medicalprotection.org
• Medical Protection offers an independent counselling service to members in South Africa experiencing work-related stress, or stress that they feel could impact their practice. This is a benefit of membership. More information is available at https:// www.medicalprotection.org/southafrica/ help-advice/counselling-service
• The MPS survey was completed by 662 medical professionals in South Africa. The survey was in the field in October 2023.
KEY FINDINGS
• 44% of doctors in South Africa say they have experienced or witnessed verbal or physical abuse from patients or their relatives in the past 12 months.
• 5% say they have experienced or witnessed physical abuse from patients or their relatives in the past 12 months.
• 9% say they have had property or healthcare premises damaged by patients or their relatives.
• 34% say they have seen more abusive behaviour from their patients and their families recently, than during the Covid-19 pandemic.
• 80% of respondents who are considering leaving the healthcare profession cite increasing abuse from patients or their families as an influence for their decision.
• 68% of respondents who are considering leaving South Africa to work elsewhere cite increasing abuse from patients or their families as an influence for their decision.
• 24% said verbal or physical abuse from patients or their relatives has impacted their mental wellbeing.
• 65% said incidents of abuse from patients or their relatives were not taken seriously by the authorities and the Health Professions Council of South Africa.
FDA alert: Avoid specific topical pain relief products
The US Food and Drug Administration (FDA) is cautioning medical professionals against the use of certain topical analgesic products commonly used for pain relief before, during, or after various cosmetic procedures such as microdermabrasion, laser hair removal, tattooing, and piercing.
THIS WARNING COMES as the FDA has issued six warning letters to companies marketing these products illegally, in violation of federal regulations.
Some of these products contain

•
•
•
•
lidocaine at concentrations exceeding the permitted levels for over-the-counter topical pain relief medications. When applied before or during cosmetic procedures, particularly in a manner that increases absorption



through the skin, these high-concentration lidocaine products pose serious health risks.
Potential adverse effects include irregular heartbeat, seizures, breathing difficulties, and the possibility of




interactions with other medications or dietary supplements being taken by consumers.



Dr Jill Furman, director of the Office of Compliance in the FDA’s Centre for Drug Evaluation and Research, emphasised the unacceptable risks associated with these products, asserting that they should not be available for purchase. Despite previous FDA warnings to consumers regarding similar products, dangerous items continue to be found online and in retail outlets. The FDA underscores the absence of evidence demonstrating the safety of these products.












Furthermore, the prolonged and widespread application of lidocaine, especially on damaged or inflamed skin, or when the skin is covered, can result in severe injury. The FDA advises consumers to refrain from using over-the-counter pain relief products containing lidocaine concentrations exceeding 4%, applying them excessively on large skin areas or on irritated or damaged skin, and avoiding wrapping treated skin with plastic or dressings, as these practices can elevate the risk of serious side effects.
The FDA is cognisant of adverse events linked to these products and encourages consumers and healthcare providers to report any such events to the MedWatch Adverse Event Reporting programme for appropriate action. The companies in receipt of warning letters are urged to respond within 15 days, either by addressing the outlined issues or providing evidence to support their compliance with regulations. Failure to do so may result in legal repercussions, including product seizure and injunctions against manufacturing and distribution. Moreover, certain companies have been placed on import alert to prevent their products from entering the US market and reaching consumers.
Managing GORD in the elderly
Gastroesophageal reflux disease (GORD) poses a significant challenge among the elderly population, often presenting with atypical symptoms that may lead to underreporting and underdiagnosis.
UNLIKE THEIR YOUNGER counterparts, elderly individuals are more likely to experience symptoms such as dysphagia, respiratory issues, and vomiting rather than the classic heartburn and regurgitation. This discrepancy increases the risk of missed diagnoses and complicates the management of GORD in older adults, who frequently present with advanced erosive esophagitis and related complications.
Understanding the nuances of GORD in the elderly population is crucial for effective diagnosis and management. While the diagnostic approach aligns with general protocols, there are unique considerations for older patients, including comorbidities and frailty. Despite a decrease in the proportion of elderly GORD patients over recent years, the prevalence remains substantial, especially among nursing facility residents and primary care clinic attendees. Notably, symptoms may vary widely among elderly individuals, with approximately 8% of men and 15% of women over 65 experiencing daily GORD symptoms.
SYMPTOMS
Symptoms of GORD in the elderly may be masked or overshadowed by other health issues, leading to underreporting and diagnostic challenges. This underscores the importance of recognising atypical symptoms and conducting thorough evaluations in older patients presenting with suspected GORD. Endoscopic examination becomes particularly vital for elderly individuals exhibiting alarm symptoms or those at risk of Barrett's oesophagus, a potential complication of GORD.
Elderly patients with GORD often present a paradox – less severe symptoms alongside more severe mucosal damage. Despite experiencing less heartburn, they frequently exhibit severe erosive esophagitis, suggesting altered disease mechanisms with age. Physiological and structural changes in the ageing oesophagus contribute to this phenomenon, including declines in oesophageal motility and increases in hiatal hernias prevalence.
DIAGNOSIS
Diagnostic work-up for GORD in the elderly mirrors that of younger patients, albeit with heightened vigilance for alarm symptoms and risk factors for complications. Upper endoscopy becomes increasingly crucial in this population due to the higher likelihood of GORD-related complications. Additionally, the management of GORD in older adults emphasises tailored approaches based on individual frailty levels, aiming to alleviate symptoms, promote mucosal healing, and prevent complications. Proton pump inhibitors (PPIs) play a central role in GORD management among the elderly, offering effective symptom relief
and mucosal healing. Despite concerns about potential adverse effects, including interactions with other medications and risks of conditions such as osteoporosis and pneumonia, PPIs remain a cornerstone of treatment. Careful monitoring and individualised dosing strategies help mitigate risks while ensuring optimal therapeutic outcomes.
CONCLUSION
In conclusion, navigating GORD in the elderly requires a nuanced approach that acknowledges the complexity of symptom presentation, the potential for underdiagnosis, and the unique physiological changes associated with aging. By adopting comprehensive diagnostic strategies and tailored management plans, healthcare
providers can effectively address GORD in older adults, improving quality of life and minimising complications.
REFERENCE
Kurin M, Fass R. Management of Gastroesophageal Reflux Disease in the Elderly Patient. Drugs Aging. 2019 Dec;36(12):1073-1081. doi: 10.1007/s40266-01900708-2. PMID: 31541359.


























SAFP reviews diagnosis, management of AR
Allergic rhinitis (AR) represents a prevalent chronic condition affecting 10% to 40% of the population globally. The implications of AR extend beyond mere discomfort, significantly impacting productivity and quality of life (QoL).
AR POSES SERIOUS health risks, exacerbating conditions such as asthma, rhinosinusitis, and otitis media, and increasing susceptibility to viral illnesses while disrupting taste, smell, and sleep quality. Of particular concern are the repercussions on children, including chronic fatigue, daytime sleepiness, learning difficulties, and mood disorders like depression. Despite its profound impact, AR remains underdiagnosed and inadequately managed, especially in children, where symptoms may be misattributed to viral infections.
AR frequently coexists with asthma, a phenomenon known as the united airway concept, with AR serving as a risk factor for asthma development and poor disease control. Effective AR management not only improves patients’ QoL but also enhances the control of comorbidities like asthma, ultimately reducing the economic burden of asthma treatment and mitigating the need for hospital-level interventions.
Recognising the global significance of AR, the World Allergy Organization has deemed it a public health concern. While comprehensive guidelines exist, tailored recommendations are necessary for South Africa due to unique local factors:
1. Economic considerations: SA, a resourceconstrained setting, prioritises infectious diseases over chronic conditions like AR in public health spending. However, untreated or inadequately managed AR carries significant economic costs due to absenteeism and reduced productivity.
2. Practical challenges: Accessing healthcare facilities poses difficulties for many due to factors like distance, singleparent households, and work constraints.
3. Health literacy and cultural beliefs: Poor health literacy and entrenched traditional beliefs can hinder treatment adherence and health-seeking behaviour.
The South African Allergic Rhinitis Working Group have provided AR recommendations tailored to the SA context.
EPIDEMIOLOGY
AR affects 10% to 40% of children and adults worldwide, with the majority developing symptoms before age 20. Urbanisation, pollution, and climate change contribute to increasing prevalence rates, particularly in low- and middle-income countries like SA.
PATHOPHYSIOLOGY
AR results from a Type 1 hypersensitivity
reaction in the nasal mucosa. Allergen exposure triggers immunoglobulin E (IgE)mediated mast cell activation, leading to acute and chronic allergic symptoms. Priming, characterised by increased nasal responsiveness to allergens, exacerbates the allergic response and can be mitigated with intranasal corticosteroids (INCS).
DIAGNOSIS
Diagnosis relies on clinical assessment and allergic sensitisation tests. AR symptoms include nasal congestion, rhinorrhoea, sneezing, and itching, often accompanied by non-nasal manifestations like allergic conjunctivitis and asthma exacerbations. Cognitive dysfunction and sleep disturbances further impact QoL.
Clinical evaluation should assess for atopy signs, nasal mucosal abnormalities, and concomitant allergic diseases like eczema and asthma. Comorbidities such as chronic rhinosinusitis and otitis media should be evaluated, with imaging reserved for select cases.
SEVERITY CLASSIFICATION
In South Africa, the widely adopted Allergic Rhinitis and Its Impact on Asthma (ARIA) guidelines categorise symptoms as intermittent or persistent, with severity classified as mild or moderate-severe. However, these guidelines are not without limitations, prompting the need for cautious interpretation. Considering the diverse presentations of AR, an array of conditions must be considered to guide appropriate diagnostic testing.
Objective laboratory testing plays a crucial role in identifying high-risk patients, guiding allergen avoidance strategies, and tailoring treatment, including allergen immunotherapy (AIT). However, indiscriminate use of specific IgE testing is discouraged when history and examination adequately suggest AR.
Emphasising shared decision-making fosters treatment adherence, essential for achieving optimal outcomes in AR management. Practical demonstrations of treatment techniques, alongside written educational materials, facilitate patient understanding and compliance. Additionally, incorporating validated tools to assess medication adherence enhances treatment success.
PHARMACOLOGICAL TREATMENT
Intranasal corticosteroids (INCS): Is the preferred pharmacological choice for all AR forms due to their efficacy across various
THE 7 MANAGEMENT PILLARS OF AR:
1. Education: Patient education forms the cornerstone, emphasising the chronic nature of AR and the available therapeutic options, considering factors such as cost, efficacy, ease of use, and side effects.
2. Allergen avoidance: Practical strategies to minimise allergen exposure play a crucial role in symptom management.
3. Nasal irrigation: Nasal rinsing with saline solutions is a simple yet effective adjunct therapy, aiding in the removal of allergens and inflammatory mediators.
4. Pharmacological treatment: Intranasal corticosteroids, oral and intranasal antihistamines, and leukotriene receptor antagonists constitute the mainstay of pharmacotherapy.
5. Allergen immunotherapy (AIT) Evaluation: Consideration of AIT should be based on individual patient characteristics and treatment response.
6. Therapy response monitoring: Regular assessment of treatment response informs ongoing management decisions.
7. Referral to specialists: Referral to allergists or otolaryngologists may be warranted in cases requiring specialised care.
symptoms. They're used intermittently for seasonal AR and continuously for perennial cases. Patients should be re-evaluated after two-four weeks of initial treatment. In cases of persistent symptoms, combining INCS with antihistamines is recommended.
Common side effects of INCS include local irritation such as nasal dryness, burning sensation, bloody nasal secretions, and nosebleeds. Proper spray technique, avoiding nasal septum, can minimise these effects. Newer INCS formulations boast enhanced safety and efficacy profiles, with negligible systemic absorption compared to older counterparts.
Intranasal antihistamines (INAHs): Act quickly and are more effective than oral antihistamines in AR symptom control. They are particularly suitable for children. However, their availability in South Africa is limited. A novel combination nasal spray of mometasone/olopatadine has recently become available, offering an alternative option for teenagers and adults.
Topical nasal decongestants: These agents, containing phenylephrine, oxymetazoline, or xylometazoline, provide short-term relief by constricting nasal blood
vessels. However, they should be used sparingly and for short durations (5-10 days) to avoid rebound congestion, especially when nasal congestion predominates. Combining with INCS is advisable.
Leukotriene receptor antagonists (LTRA): LTRA’s efficacy is comparable to oral antihistamines, particularly in managing night-time nasal symptoms. However, they are less effective than INCS in overall symptom improvement and quality of life enhancement, making them secondary options. Allergen immunotherapy (AIT): AIT, the only disease-modifying treatment for AR, aims at desensitising patients to common allergens. It significantly reduces AR symptoms, medication dependency, and progression to asthma. Both sublingual (SLIT) and subcutaneous (SCIT) routes are effective, requiring accurate allergen identification and potential allergen provocation testing.
Assessment of treatment response: Assessing treatment response is crucial for refining management. Visual analogue scales (VAS) or standardised tests such as the CARAT, RCAT, ARCT, or SNOT facilitate consistent evaluation. Referral to specialists should be considered for poor treatment response, atypical symptoms, or comorbidities.
Indications for referral and surgery: Referral to specialists is warranted for cases with poor treatment response, atypical symptoms, or significant comorbidities. Surgery is rarely needed for ‘pure’ AR but may be considered for severe cases or to address complications like chronic otitis media or nasal polyps.
Multi-morbidities: AR often coexists with other disorders, including asthma, atopic dermatitis, and sleep disorders. Treating AR can lead to improvement in associated comorbidities.
CONCLUSION
In conclusion, AR poses significant morbidity and warrants a multifaceted treatment approach involving education, allergen assessment, pharmacological intervention, AIT, and specialist involvement when necessary. Effective management requires careful consideration of treatment response and associated comorbidities.
REFERENCE
Richards, G., McDonald, M., Gray, C., et al. Allergic rhinitis: Review of the diagnosis and management: South African Allergic Rhinitis Working Group. South African Family Practice. 2023;65(1), 11 pages. doi: https://doi.org/10.4102/safp.v65i1.5806
RECOMMENDED BY THE SA ALLERGIC RHINITIS (AR)
WORKING GROUP 2023:

INCS* are the treatment of choice for AR INAH** act rapidly within 15 minutes
ecific reference was made to the INCS/INAH combination of mometasone/olopatadine as contained in Ryaltris®.
FAST RELIEF, LASTING COMFORT TM
Comprehensive Relief in Allergic Rhinitis 2,3
Rapid symptom relief within 15 minutes
Better quality of life (QoL) vs monotherapy
Dual benefits of olopatadine and mometasone

Statistically significant improvements in ocular and nasal symptoms
Well tolerated

*Intranasal corticosteroids
References:
**Intranasal antihistamines


1. Richards GA, McDonald M, Gray CL, et al. Allergic rhinitis: Review of the diagnosis and management: South African Allergic Rhinitis Working Group. S Afr Fam Pract. 2023;65(1), a5806. https://doi.org/10.4102/safp.v65i1.5806. 2. Patel P, Salaptek AM, Tantry SK. Effect of olopatadine-mometasone combination nasal spray on seasonal rhinitis symptoms in an environmental exposure chamber study. American College of Allergy, Asthma & Immunology. 2019;122(2):160-166.e.1. 3. Gross GN, Berman G, Amar NJ, et al. Efficacy and safety of olopatadine-mometasone combination nasal spray for the treatment of seasonal allergic rhinitis. Ann Allergy Asthma Immunol, 2019;122:630-638.
S2 RYALTRIS® (Nasal spray). Reg. no. 53/21.5.1/0457. Each spray delivers 600 μg olopatadine (as olopatadine hydrochloride) and 25 μg mometasone furoate (as mometasone furoate monohydrate). Contains the preservative benzalkonium chloride 0,02 % w/w. Sugar free. For full prescribing information refer to the professional information approved by the South African Health Products Regulatory Authority. Date of revision: 18 July 2022.
HCR: Glenmark Pharmaceuticals South Africa (Pty) Ltd. 2nd Floor, Building D, Stoneridge Office Park, 8 Greenstone Place, Greenstone, Edenvale, Gauteng, 1609. (Office) +27 11 564 3900. www.glenmarkpharma.com. ZAR/03/2024/03
Glenmark, touching the lives of patients for over three decades


Dr Jireh Serfontein
Date: 15 May 2024
Time: 7pm
Topic: Managing sexual dysfunction in a diabetic patient
Presenter: Dr Jireh Serfontein
CLICK TO REGISTER: https://bit.ly/AccordWebinar15May24
Exploratory studies have found a high rate of erectile dysfunction among South African men in the 18 to 60 age range. Are you equipped with the knowledge you need to treat patients with ED? In this webinar, sexual health expert Dr Jireh Serfontein will outline the treatment paradigm for patients with ED with reference to commonly used medications. Dr Serfontein is a medical doctor with a special interest in sexual health and HIV management. She has been part of the team at My Sexual Health since the very beginning


and has been practicing sexual health medicine since 2013. Dr Serfontein completed her Master’s Degree in Sexual Health through the University of Sydney, Australia and holds a Diploma in HIV Medicine through the Colleges of Medicine in South Africa. She is regularly approached for her expert opinion by newspapers and magazines and has been a guest on several radio talk shows.




‘Eat less – move more’, myth or fact?
Debunking health myths – Understanding the truth behind the 'Eat less – move more' mantra in a webinar by Dr Wayne May.
If you missed the CPD-accredited webinar presented by acclaimed endocrinologist Dr Wayne May on dissecting the widespread belief - 'Eat Less, Move More', go to https://vimeo.com/event/4054845 to view the replay. You will still be eligible for a CEU. This webinar was sponsored by Acino.
BIO
Dr Wayne May is a UCT graduate currently working as a fulltime endocrinologist in private practice at the Kingsbury Hospital in Cape Town. He works with his wife, a diabetologist, in the Diabetes Life Clinic, which is a multidisciplinary clinic treating patients living with diabetes. He has a special interest in weight management and in 2005 helped form the Cape Town Bariatric Clinic (previously known as the Chrysalis Clinic), which is an accredited multidisciplinary clinic managing patients through the process of bariatric surgery, as well as looking at non surgery options. He is the author on the section on weight management for the South African. Diabetes Guidelines (SEMDSA) 2012, 2017 and 2023 and is the current co-chair of the first SA Obesity Guidelines. He is also SCOPE accredited by the World Obesity Federation, which is an internationally recognised certification in obesity.
Atherogenic dyslipidaemia and residual Risk
Stay ahead with leading insights on atherogenic dyslipidaemia and patient care.
If you missed this rare opportunity to learn from the acclaimed Dr Martine Joffe, about Atherogenic Dyslipidaemia and Residual Risk, go to https://vimeo.com/event/4057051 to view the webinar replay. You will still be eligible for a CEU. This webinar was sponsored by Austell.

Dr Martine Joffe
BIO
Dr Joffe graduated from the University of the Witwatersrand in 2002, where she was awarded the faculty prize for the best student in obstetrics. She completed her internship and the Johannesburg General Hospital and community service at the Sebokeng Hospital. She served as a medical officer in the department of anaesthesiology for a short time. In 2005 she joined a family practice where she continues to work today. In 2009 she completed an advanced course in Diabetes management through the CDE. Since then she has been involved in the management of people with diabetes on a chronic basis. In 2013 she received an award from the CDE for most improved HBA1C for patients under her care. She has been working in the field of diabetes for many years, and has recently completed a postgraduate diploma, with distinction, in diabetes thorough the university of South Wales. She is passionate about holistic care and works closely with the members of an award winning diabetes care team to ensure the best care for her patients.







May be taken any time of the day6


Intercourse is possible again the next day6 Accessible and affordable to more South African men.7



Food allergy diagnosis:
Redefine your understanding of food allergies. Discover what’s fundamental, what’s false and step into the future with Prof Claudia Gray. Prof Gray discusses food allergy diagnosis in length, debunking myths, and looking at future challenges.
BIO
Prof Claudia Gray is a paediatrician with subspecialist accreditation in allergology and subspecialty training in paediatric pharmacology. She undertook her medical degree at the University of Cape Town, specialised in London, and subsequently returned to South African soil to work in the field of allergology. Claudia has a private paediatric and allergology clinic at Vincent Pallotti Hospital in Cape Town. She is also a part time consultant at the Allergy and Asthma clinic at Red Cross Children’s Hospital, and an Associate Professor in Paediatrics at the University of Cape Town. Her research interests are in allergy pharmacology, and in food allergies in eczema patients, on which she based her PhD. Claudia thoroughly enjoys teaching and presents regularly at local and international conferences. She has over 100 publications in local as well as international high-impact international journals. She is on the editorial team of the journal Current Allergy and Clinical Immunology and co-editor/co-author of the new 2017 South African Allergy Handbook and, more recently, the book Food Allergies in a Nutshell. Claudia is a regular examiner at the postgraduate Diploma in Allergy and Allergy Fellowship exams and is honorary secretary of the Allergy Society of South Africa. She is also the author of several children’s books and has a passion for educating and enlightening the young. Claudia has been heavily involved in South Africa’s World Allergy Week campaign in 2021 and 2022.



This year’s conference theme is: “INTEGRATING
EXPERTISE: THE ROLE OF MULTI-DISCIPLINARY TEAMS IN ONCOLOGY.”
dates: 10 – 12 May 2024
venue: Indaba Hotel and Conference Centre, Johannesburg
REGISTER ATTENDANCE:



Prof Claudia Gray Paediatrician and Allergologist MBChB (UCT, summa cum laude); FRCPCH (London); MSc (Clin Pharm) (Univ Surrey, distinction); Diploma Paed Nutrition (London ), Diploma in Allergy (Southampton), PhD (Paediatric allergy), FAAAAI (USA)
Current management of hypercholesterolaemia
to watch the replay. You will still be eligible for a CEU. This webinar was sponsored by Activo Health.
We look at best practices in managing hypercholesterolaemia with Prof Frederick Raal. Medical Chronicle hosted a free, onehour, CPD-accredited webinar on Current management of hypercholesterolaemia.

BIO
Director, Carbohydrate and Lipid Metabolism Research Unit, Faculty of Health Sciences, University of the Witwatersrand, Johannesburg, South Africa, Professor Derick Raal is a distinguished Professor and director of the Carbohydrate and Lipid Metabolism Research Unit, Faculty of Health Sciences, at the University of the Witwatersrand. After obtaining his MBBCh degree cum laude in 1981, he obtained his Master of Medicine in 1991, his PhD in 2000 and his Doctor of Science in 2022. He has received numerous postgraduate awards including the TH Bothwell Research Prize, the FJ Milne award, and the Vice Chancellor’s Research Award. He is a NRF A-rated scientist, is recognised as a Web of Science highly cited researcher and has authored or co-authored over 350 original articles and book chapters. He is particularly interested in lipid disorders and has been integrally involved in the management of familial hypercholesterolaemia (FH). The major focus of his research remains the clinical, biochemical, genetic and therapeutic management of this condition and he continues to conduct studies with novel therapies such as ANGPTL3-inhibitors in this patient group.













The demise of general practice
Are we witnessing the demise of general medical practice?

GENERAL PRACTICE [PRIMARY HEALTHCARE]
has undergone huge changes over the past 10 to 15 years and continues to change at a rapid pace. There have been inroads into the General Practice space, disrupting the relationship between patients and their Health Professional for years. New modalities of care have disrupted the continuity of care [a hallmark of General Practice] and has distorted the trust patients had with their General Practitioner. Patient care, despite the inroads into the primary care space, has not really got any better.
Has General Practice lost its way? We must acknowledge that general practice is in crisis. We are witnessing the attrition of General Practice. The discipline is underfunded and under resourced. The allocation of funds to general practice is about 6% of the GDP spend on health and yet we are expected to have a viable Primary healthcare entry point into the healthcare system. Are we serious?
Patients are facing unacceptably poor access to primary care and to a Health Professional of their choice.
Before Universal Healthcare (NHI) is implemented, Government needs to review the short-term challenges that are constraining General Practice. One of the major Health system challenges that can negatively impact NHI, is the deficiency of Human Resources for Health. The questions we pose, are the new rules and policies admitting all disciplines and corporates into the primary care space, going to address this shortage. The focus and services are mainly in the metropolitan centres.
How do we recruit more Family Practitioners, train them and retain them in
the health system? Are we able to prevent outward migration of health professionals (Brain Drain) especially in a health system that is unstable, unsustainable and a platform that cannot support NHI?
Current challenges include the need for more funding to create more jobs and employ qualified practitioners, we need to identify ways to distribute general practitioners equitably across the country so that ‘under doctored’ areas receive a balanced portion of general practitioners [Primary Care Practitioners]. The question we need to ask: Are the new entrants in the Primary Healthcare space, prepared to serve in the peri-urban and rural areas? Did we think of this before we opened the flood gates to an influx into the primary care space. To address these challenges, we need to encourage integrated care systems and team-based care to distribute the workforce, decrease inappropriate workload and increase access into the healthcare system. There is a long way to go to make general practice more sustainable and fit for purpose.
INVASION INTO GENERAL PRACTICE AND DISRUPTION OF THE CONTINUITY OF CARE
The inroads into General Practice (Primary Healthcare) by various stakeholders and the ‘demise’ of General Practice, is due to the disruption of the “Continuity of Care” by the Family Practitioner with whom the patient has developed a caring and trusted relationship over the years.
The concern is the declining provision of the continuity of care in General Practice. This is the hallmark of General Practice and has been allowed to erode. This ongoing relationship between General practitioner and their patients is foundational to Primary Care. A useful definition of Continuity of Care distinguishes three subsets: Informational continuity; management continuity and relational continuity.
Electronic medical records have made remarkable advances in both informational and management continuity.
Relational continuity can be defined as the relationship between a single practitioner and the patient that extends beyond specific episodes of illnesses or diseases. It implies that a patient will preferentially or exclusively see the healthcare professional with whom they have established a relationship, and the healthcare professional will take care of the patient outside the episode of illness as well.
Relational continuity results in accumulated knowledge of the patient and
care consistent with the patient’s needs.
It facilitates improved communication and a sustained sense of responsibility. It brings an increased sense of Trust between patient and clinicians.
Patients want continuity of relationship with a Primary Health Practitioner and the practitioner also wants this and the resultant healthcare outcomes are improved by the continuity of the relationship.
THE CAUSE OF THE DECLINE
Relational continuity is co-constructed or co-produced through interaction between patients and clinicians and is facilitated or obstructed by how services are organised or managed. Demand-side factors, such as increased complexity of patient management, devolution of work from secondary to primary care and greater patient expectations have increased the workload of General Practitioners.
Simultaneously, supply-side issues of work force shortages and an increasing trend towards part-time work have increased reliance on temporary workers and resultant fragmentation of care.
Multiple different health workers and increased number of part-time workers complicates the concept of continuity of care but does not negate it totally.
Another factor is that excessive workload applies pressure on general practitioner’s ability to provide continuity of the relationship.
GENERAL PRACTICE AND NEW HEALTH DELIVERY STRUCTURES
Primary Care Networks and Integrated care systems offer an opportunity to integrate care around people.
Integrated Care should prioritise and simplify the patient interface with Universal Healthcare (NHI) by improving access, facilitating triage and referral across the healthcare system including General Practitioners. Both in the state funded and private sectors the role of the General Practitioner has been on the decline for some time. In the public sector, for example, the primary care role has become increasingly dominated by nursing staff under the direction of nurse managers.
CHALLENGES OF PRIMARY CARE ARE RISING
Demand and complexity of primary care is increasing, driven by rising number of patients living with chronic, multi-morbid diseases, requiring long-term support.
In these patients the opportunity and development of a relational continuity of care, with long-term chronic care will result in better outcomes within cost frameworks.
The General Practice dilemmas are seen

globally. In the UK, similarly to sub-Saharan Africa, there are underfunding and underresourced health systems.
There are different challenges between urban and rural areas. This is like the issues and challenges we see in developing economies. A confounding variable is the impact of the social determinants of health and its influence on the relationship continuity between the users and the Primary Healthcare system.
This demise of continuity erodes patient trust in the health system and has a negative impact on the healthcare outcomes.
What needs to change to build a better future is a strategy based on investment in general practice and primary healthcare, with a lens on the need to improve access to healthcare, which is the underlying principle of Universal Healthcare (NHI).
Primary care does hold the health system together in developing countries. If this interphase of care is poorly managed, the impact is long waiting times for treatment, corridor care, long waiting times in congested emergency care units and poor health outcomes and unnecessary inhospital congestion.
This catastrophe is by design. Governments do not plan and redesign and realign the health system for the increased patient volumes when access to care is planned to increase. We are regularly underinvesting in health, with health systems under-resourced, health systems underequipped, underfunded and poor governance. We encounter a political agenda and not a health agenda. What we are seeing is a ‘sick care’ system and not a ‘healthcare’ system.
As the service gets worse, the powers that are start spinning a narrative that erodes the patient’s trust in general practice and attributes the problem to the service provider, who are really doing their best to keep the service afloat.
What we see is the poor care is being normalised. There is a constant feeling of being on the backfoot and daily ‘firefighting’.
The general practitioners are elbow deep trying to survive. The inroads into the primary care spaces are by competitors who are well resourced. The door has been opened to unfair competition in the primary care sector, possibly due to perceived shortcomings in policy reforms by the HPCSA in South Africa.
To quote Dr Ellen Walch, previous cochair of the Doctor Association of the UK, “I would be lying if I said General Practice is not at crisis point, but it is salvageable if those in charge are prepared to listen to the GP’s.” We echo similar sentiments in South Africa.
Tackling nutrition education in under-resourced communities
One in nine South Africans are affected by diabetes, according to the International Diabetes Federation. Diets high in sugar and carbohydrates are a key cause of diabetes, especially in low-income communities where processed foods are more accessible and affordable. Non-profit organisation, The Noakes Foundation, has conducted a study in Dunoon, an informal settlement in the Western Cape, to highlight how nutrition education initiatives in under-resourced areas can address the health challenges and social stigma associated with diabetes.

IABETES IS OFTEN viewed as a death sentence in low-income communities because there is a lack of understanding about how to manage it.
Our research explored the best ways to inform, engage and support people in these communities when it comes to healthy nutrition, and the benefits of a low-carb, high-fat diet in managing diabetes,” says Jayne Bullen, chief operating officer at The Noakes Foundation, which aims to challenge mainstream scientific thinking around the link between nutrition and chronic diseases.
In partnership with Eat Better South Africa (EBSA), a non-profit organisation dedicated to supporting local public healthcare systems by establishing individual and familyfocused food security networks, the study assessed the impact of EBSA's nutrition education programme by examining behaviour and metabolic health changes in type 2 diabetes patients. The programme aimed to reduce consumption of refined sugars and carbohydrates, while promoting accessible, nutrient-dense alternatives.
As part of the study, participants shared details about their lived experiences through focus group discussions and one-on-one interviews – offering insights into how diabetes patients in under-resourced communities need to be supported. “Participants often felt a sense of isolation, because they don’t want to be a burden to loved ones. They found it difficult to maintain a different diet than the rest of their household. Often, people around them were not supportive of their lifestyle changes and holistic approach to their diabetes diagnosis. The
support group aspect of the programme provided that sense of community and made their journeys to better nutrition easier,” explains Bullen.
Participants highlighted a lack of support from healthcare professionals about dietary interventions as a treatment for diabetes. “When participants initially received their diagnosis, most of them weren’t aware that diabetes is a disease they could manage with a healthy lifestyle,” says Bullen.
The participants’ blood markers, blood pressure and body measurements were recorded throughout the programme. Baseline test results indicated high levels of blood glucose (sugar) levels. Following the programme, significant reductions in weight, waist circumference, and blood pressure were recorded for women. The study also found that the programme had a positive effect on participants’ dietary habits, resulting in them consuming more animal proteins and less refined carbohydrates and sweets.
“Based on the outcomes, it is clear when people are empowered with knowledge and support, they are more likely to actively manage their diabetes through dietary changes. We are proud to be conducting research that shows the positive impact of holistic diabetes management to address the medical, social and emotional needs of people in under-resourced communities,” she adds.
To find out more about how the Noakes Foundation is challenging the accepted science and supporting research that empowers individuals to make the best dietary choices available to them, visit https://thenoakesfoundation.org/






