Your Guide Through a Healthy Pregnancy

History:
Welcome to MyCHN
Community Health Network (also known as Stephen F. Austin Community Health Network) was established in 2008 to provide accessible and affordable healthcare to Brazoria County communities.. In the beginning, Community Health Network (CHN) had one primary care office with three exam rooms and one medical provider located in Alvin, Texas. Today, CHN has multiple locations that offer various specialties and services across Brazoria County, Galveston County, and Harris County.
Affordable Care for All
CHN accepts most private insurances, Medicaid, Medicare, and CHIP. Uninsured patients may be eligible for discounted self-pay services based on their family size and household income. CHN strives to provide the highest value of care and offers substantial benefits for patients who are uninsured or self-pay. We have controlled the cost of office visits and have kept lab and pharmacy costs far below healthcare providers outside of CHN. Low-income or uninsured patients may apply for discounts to the cost of their care. CHN does not turn away anyone away due to an inability to pay.
Mission:
Our mission is to provide quality care that uplifts, supports, and shapes healthy communities while addressing financial and social barriers.
Vision:
The vision of Community Health Network is to be a leader in providing quality services and programs that enhance the lives of the people in our community.
Values:
The values of Community Health Network are quality care at reasonable costs, education to promote healthy living, access to needed care, transparency in all aspects of our operations, competent and empathetic staff, high professional standards, and commitment to advances

Welcome to MyCHN

Locations
• Adoue Family Health Center (1111 W. Adoue St. Alvin, TX 77511)
• Womenr & Children’s Health Center (218 E. House St. Alvin, TX 77511)
• Bay Area Family Care (1136 Grand Avenue, Bacliff, TX, 77518)
• Pearland Family Health Center (2552 East Broadway St, #102, Pearland, TX 77581)
• Freeport Community Health Center (905 N. Gulf Blvd, Freeport, TX 77541)
• MyCHN League City (2360 Gulf Fwy S #100-C, League City, TX 77573)
• Scarsdale Family Health Center ( 10851 Scarsdale Blvd, Suite 160, Houston, TX 77089)
• Brazoria County Dream Center (792 Brazosport Blvd S, Clute, TX 77531)
• MyCHN Angleton (2020 E Mulberry St, Angleton, TX 77515)

• MyCHN Silverlake (9430 Broadway St Suite 120, Pearland, TX 77584)
• Lake Jackson Family Care (100 Highway 332 West, Suite 1404 (inside brazos mall), Lake Jackson, TX 77566)
Service Departments
BEHAVIORAL HEALTH

We offer in-person and virtual Behavior- al & Mental Health appointments with our Psychiatric and Counseling Staff.
We are committed to finding personalized solutions and practical strategies to match your needs and improve your total well-being.
Services & Conditions:
• Child Psychiatry
• ADHD Services
• Anxiety
• PTSD
• Medicated Assistances Treatment and more.
Group Therapy
CHN offers several therapy groups to help patients connect and grow. Joining a group is an excellent option if you are seeking a connection with others who share similar experiences or would like to find new coping skills and strategies. Therapy groups offer a space to share and receive a broader range of perspectives. These groups can be a great place to work on relationships and social skills. Listed below are some of the groups that are available for enrollment:

• Women’s Support Group
• Co-occurring Disorders/Dual Diagnosis Groups
• Teen Anxiety or Adolescent Girls Group
• Peer Support Parenting Group
• Expressive Art Therapy (Need Ages)
• Bipolar Group
DENTAL
We provide general dentistry services for your entire family. As oral hygiene can significantly influence your overall health, our professional dental team ensures that your teeth are healthy and that you’re always wearing your best smile. Most private insurance plans, CHIP, CHIP Perinatal, Medicaid, Medicare, and other payment options are accepted.
DENTAL SERVICES: EMERGENCY DENTISTRY

GENERAL DENTISTRY
• Bridges
• Crowns
• Dentures
• Fillings
• Fluoride Treatment
• Nightguards
• Sealants
• Teeth Cleanings
ORAL SURGERY
• Tooth Extractions
COSMETIC DENTISTRY
• Teeth Whitneing
PEDIATRIC DENTISTRY
• Child’s First Dental Exam
• Children Dentistry
• Children Conscious Sedation
ORTHODONTICS
• SureSmile
ENDODONTICS
• Root Canal Therapy
PHARMACY
At Community Health Network Pharmacy, we’re committed to the idea that quality pharmacy care means more than just prompt prescriptions. To us, quality care means getting the prescriptions and medications you need with the care and attention you deserve. Our pharmacies are dedicated to the well-being of your family and the well-being of the community. All insurance plans are accepted, including CHIP, Medicare, and Medicaid.
Savings
At CHN pharmacy, we can offer savings that other pharmacies cannot compete with. Our unique program allows us to pass significant savings to our patients.
Pharmacy Services
• Short wait times
• Free mail order available
• Refills by phone or online
• Immunizations
• Medication therapy management
• Multi-dose packaging
• Medication synchronization
• Health screenings
• Free medication counseling
• Easy prescription transfers
Pharmacy Locations:
Freeport Community Health
Angleton Internal Medicine & Primary Care
Scarsdale Family Health
Women’s and Children’s Alvin
Women’s and Children’s League City
Adoue Family Health (Coming Soon)
Pearland Family Health (Coming Soon)
Benefits of Using CHN Pharmacy

Our pharmacies are dedicated to the well-being of your family and the well-being of the com- munity. That’s why we offer services such as immunizations; medication therapy manage- ment, multi-dose packaging, medication synchronization, important health screenings, and expert care.
• Mail Order Available (No Cost to You When You Use CHN Pharmacy)
• Free Medication Counseling
• Easy Prescription Transfers
• All Insurance Plans Accepted (Including CHIP, Medicare, and Medicaid)
• Refills By Phone or Online
• Short Wait Times
Savings When Using CHN’s Pharmacy
Community Health Network can offer savings that other pharmacies cannot compete with. Our unique program allows us to pass significant savings to our patients.
We Accept All Major Insurance Plans
Ask Us About Our Best Price Guarantee
We Accept All Competitor $4 Program Prices
PRIMARY CARE

Well-Adult Exam
Annual wellness exams include blood pressure screening and age-appropriate preventive lab tests. Provides care towards maintaining health, preventing problems, and addressing concerns before health issues occur.

Visit Includes:
• Physical examination
• Checking vitals
• Checking BMI
• Examination of personal and family medical histories
• Discussion of current lifestyle and health choices
• Screenings
• Immunizations
• Establishing a plan for your health
Health screenings may vary depending on age, risk, and gender. During your wellness exam, you may receive screening for high cholesterol, blood pressure, diabetes, breast cancer, cervical cancer, testicular cancer, colon cancer, osteoporosis, and STDs.
Chronic Disease Management
Early diagnosis and treatment of diabetes, high cholesterol, and high blood pressure can improve your quality of life while reducing your future health care costs. Preventative care and proper management of chronic diseases can minimize the effects of a disease.
Visits Include:
· Screenings
· Medication follow up and refills
· Condition monitoring
· Coordinating treatment
· Patient Education
Men’s Services
Provides care towards the goal of optimal male health and well-being.
Visits Include:
• Cancer screening (prostate, testicular, colon)
• Low testosterone treatment
• Enlarged prostate management
• Erectile dysfunction treatment
• Screening and treatment of sexually transmitted diseases
• Routine blood work (screening for diabe -
tes, high cholesterol, etc.)
Acute Care
Acute care is care that is needed for a short period of time and usually completed in a single visit.
Types of Visits:
• Sick visits
• Sprained ankle
• Sore throat
• Minor cuts
• Eye or ear infections
• Minor burns
• Allergies
• Painful urination
• Rashes without fever
• And more
Women’s Services
Services focused on female disease prevention and health promotion. Visit Include:
• MyPrenatal Care
• Well-women exams
• Cancer screening (breast, cervical, colon) Abnormal Pap test management and treatment
• Screening and treatment of STDs
• Contraception and family planning
• General gynecological complaints (acute breast, pelvic pain, irregular/abnormal vaginal bleeding, menopause, etc.)
• Adolescent gynecological complaints
• Preconception counseling
Education and Consultation
A meeting between the patient and a health care professional(s) to understand a patient’s purpose for the appointment, evaluate needs, present a patient-centered diagnosis, and offer education that will benefit the patient.


Types of Visits:
· Well-Adult Exam
· Well-Woman Exam
· Medication
· Lifestyle Changes And More
Community Health Network is thrilled that you have chosen us to support and care for you as an expecting mother. Here’s what to expect from CHN throughout your journey to motherhood:
• Trusting relationship with your MyPrenatal Care team
• Detailed prenatal visits with individualized care (first visit lasting between 60 to 90 minutes)
• Blood and urine collection
• Early blood testing for baby’s gender
• Screening for gestational diabetes
• Pap test (if needed)
• Vaccines (if needed)
• Customized prenatal education
• Prenatal ultrasounds scheduled at one of CHN’s convenient locations

• Timely contact with delivery doctor throughout your care
• Weekend office hours
• Access to CHN’s Dental, Behavioral Health, and Pharmacy services
Routine MyPrenatal Care visit scheduled:
• Every 4 weeks for 6 – 17 weeks of pregnancy
• Every 2 weeks for 28 - 36 weeks of pregnancy
• Every week for 36+ weeks of pregnancy
Meet our Obstetric Care Team
Dr. Yvette Poindexter, MD,

FACOG, MB
Obstetrician-Gynecologist
Chief Medical Officer
LOCATION: MyCHN Silverlake
Dr. Yvette M. Poindexter, FACOG, and her staff are dedicated to providing quality, personalized care for her patients. Dr. Poindexter graduated from The University of Texas Medical Branch in 1993 and Baylor College of Medicine in 1997 in Obstetrics and Gynecology. Embracing a mission-driven organization with strong leadership, empowering members, and providing an outstanding patient experience, Dr. Poindexter develops the culture of excellence at Community Health Network. She delivers Women’s Health and Prenatal Care in Brazoria, Harris, and Galveston County in collaboration with Dr. Antonia Way, Dr. Uchenna Jones-Conley, Dr. Bassem Maximos, Dr. Kingsley Asumugha, Dr. Vien Lam, and Community Health Network’s Women and Children’s Nurse Practitioners and Physician Assistants for obstetrical delivery in the metropolitan, suburban, and rural areas. Dr. Poindexter provides quality Obstetrical and Gynecological care to all women without prejudice and in a caring manner. With over 24 years of experience, she sets the standard for outstanding patient service.
Dr. Kingsley N. Asumugha
Obstetrician-Gynecologist
LOCATION: Scarsdale Family Health Center
Dr. Kingsley N. Asumugha, a 1988 graduate of the University of Arkansas for Medical Sciences College of Medicine, completed his internship at Tulane University School of Medicine in 1989 and his residency in Obstetrics and Gynecology at Albert Einstein Medical Center in 1994. During his training, he developed additional expertise in
Care Team
the management of high-risk pregnancies. He is board certified by the American Board of Obstetricians and Gynecology (ABOG) in 1997 and is a Fellow of the American College of Obstetrics and Gynecology (ACOG). Dr. Asumugha is a member of the American Medical Association, the Texas Medical Association, and the Harris County Medical Society. With over 28 years of experience and extensive training, Dr. Asumugha offers his patients the skilled care of a world-class doctor. Dr. Asumugha has privileges at Memorial Hermann Southeast Hospital, Clear Lake Regional Medical Center, and Houston Methodist Clear Lake Hospital. He has also embarked on several humanitarian medical missions.

Dr. Bassem Maximos
Obstetrician-Gynecologist
LOCATION: League City Women & Children’s Health Center
Dr. Maximos earned his bachelor’s in arts and sciences from La Sierra University in California, the undergraduate campus of Loma Linda University in Grenada, Newark Beth Israel, and St. Barnabas Medical Centers in New Jersey. Dr. Maximos was enrolled in a combined MD/MPH degree program that earned him a master’s degree in Public Health and his medical doctor’s degree in 2003. Dr. Maximos completed two years of residency training at Louisiana State University in New Orleans. After Hurricane Katrina in 2005, he finished his last two years of residency at the University of Medicine and Dentistry of New Jersey

(UMDNJ). Dr. Maximos is board eligible to be certified by the American Board of Obstetricians and Gynecologists (ABOG) in 2009. He is a member of the American College of Obstetricians and Gynecologists (ACOG) and served as the Junior Fellow Vice Vhair and Chair of the New Jersey section from 2005 until he moved to Texas in 2007. He is also a member of the Texas and Galveston County medical societies, the American Association of Gynecologic Laparoscopists and the American Medical Association.
Dr. Antonia Way
M.D. Family Medicine
LOCATION: Scarsdale Family Health Center
Dr. Antonia L. Way received her medical degree at the University of New Mexico in 2010 and completed her residency with the University of New Mexico Department of Family and Community Medicine in 2013. She is board certified in Family Medicine and previously practiced General Medicine in the Webster area. Dr. Way sees a broad spectrum of patients from birth to geriatrics, including Women’s Health. In addition to treating chronic
diseases and disease prevention, Dr. Way also treats musculoskeletal pain with trigger point injections and joint injections. She is interested in preventative medicine and a patient-centered approach to treating the entire family.
Dr. Way’s goal is to engage patients in both preventative and chronic care, practice evidence-based medicine, provide comprehensive care, and teaching patients how to live healthier and happier lives.
Uchenna A Jones-Conley
MD, MBA, FSMB
Family Medicine Physician
LOCATION: Freeport Community Health Center
Dr. Uchenna A. Jones-Conley, MD, MBA received her medical Degree at Wright State university in 2016 and completed her residency with the McGovern Medical School University of Texas at Houston Department of Family and Community Medicine in 2021. She is Board Eligible in Family Medicine. Dr. Jones-Conley treats a broad spectrum of patients ranging from birth to geriatrics. In addition to treating chronic disease, and disease prevention, Dr. Jones-Conley targets Women’s Health and treats musculoskeletal pain. She is interested in preventative and integrative medicine with a holistic approach to treatment.

Sherrell Gibson
MSN, APRN, FNP-C
Women and Children’s Nurse Practitioner
LOCATION: MyCHN Silverlake
Sherrell Gibson, MSN, APRN, FNP-C, is a Family Nurse Practitioner, board certified by the American Academy of Nurse Practitioners. She began her career as an associate degree registered nurse in 2004 and has a nursing career that spans across multiple specialties. Mrs. Gibson earned a Bachelor of Science in Nursing in 2014 while attending The University of Texas at Arlington. For graduate school, she
attended The University of Texas Health Science Center of Houston where she earned a Master of Science in Nursing in 2018. Mrs. Gibson began her career as a family nurse practitioner at Community Health Network and completed specialized training to transition

into a provider for Women and Children’s Services. She then completed focused training and the mentorship program through the American Society for Colposcopy and Cervical Pathology (ASCCP) to become a certified colposcopist in 2021. Mrs. Gibson has a strong passion for health promotion, risk reduction, and disease prevention with a particular interest and skill in Women’s Health, abnormal cervical cancer screening management, contraceptive education, and reproductive health.
Jemyra Calais
MSN, APRN, FNP-C
Women and Children’s Nurse Practitioner
LOCATION: Women & Children’s Health Community Center
Jemyra Calais, MSN, APRN, FNP-C, a Family Nurse Practitioner, is board certified by the American Academy of Nurse Practitioners. She is currently licensed to practice in the state of Texas. Ms. Calais received her Bachelor of Science in Nursing in 2012 from Dillard University in New Orleans, LA. Upon graduating, she acquired an abundance of knowledge in the nursing field ranging from Medical-Surgical, Post Op, NICU, Women’s Health, and Men’s Health. Ms. Calais decided to further her education by receiving her Master of Science in Nursing from South University in Savannah, Georgia. She currently practices as the Women and Children’s Nurse Practitioner at Community Health Network’s Alvin clinic. She is passionate about preventative health and believes teamwork and a positive mindset are critical for maximizing patient outcomes.
Destanee Hamilton
MPAS, PA-C
LOCATION: Scarsdale Family Health Center
Destanee Hamilton, MPAS, PA-C, is a Physician Assistant, certified by the National Commission on Certification of Physician Assistants. She is currently licensed to practice in the state of Texas. Ms. Hamilton received her Bachelor of Science in Biology in 2018 from Baylor University in Waco, Texas. She continued her education at the University of Texas at Southwestern Medical Center in Dallas, Texas, where she earned her Master of Physician Assistant Studies


in 2021. During her time at UT Southwestern, she was awarded the National Health Service Corp Scholarship. Upon graduation, she then began her career as a Family Medicine
Physician Assistant at CHN. Ms. Hamilton is passionate about patient advocacy, preventative health, and chronic disease management. She believeskeeping the patient at the center of care is essential for success.
Margaret Hazelton
MPAS, PA-C
LOCATION: MyCHN League City
Margaret Hazelton is a board-certified Physician Assistant by the National Commission on Certification of Physician Assistants. She is currently licensed to practice in the state of Texas. Margaret received her Bachelor of Science in Biology in 2018 from the Xavier University of Louisiana in New Orleans, LA. She took a year off to gain healthcare experience by becoming an Emergency Medicine Medical Scribe.
Ms. Hazelton continued her education at the University of Texas at Southwestern Medical Center, earning her Master of Physician Assistant Studies in 2021. She then began her career as a Women’s Health provider at Community Health Network’s League City location.

Ms. Hazelton is passionate about building patient-centered relationships that allow the patient to feel comfortable and safe with her as their provider. She believes in providing comprehensive, preventative healthcare to all while also managing chronic diseases.
Hazelton has a particular interest in Women’s Health ranging from routine gynecological exams to prenatal care. She enjoys working closely with the Women’s Health team to provide quality healthcare in a compassionate and supportive environment.
Anneliese Hulse
MSN, APRN, FNP-C
LOCATION: Women & Children’s Health Community Center
Anneliese (Onie) Hulse, MSN, APRN, FNP-C, is a family nurse practitioner who is board certified by the American Academy of Nurse Practitioners and licensed to practice in Texas. She began her career with a bachelor’s degree in nursing that she earned from the University of Texas Health Science Center School of Nursing in Houston in 2015. Her nursing experience includes labor & delivery and antepartum nursing at The Woman’s Hospital of Texas, Houston Methodist, and Clear Lake Regional. She graduated with her master’s degree in nursing from UTHealth Cizik School of Nursing in Houston in 2021. She is passionate about preventive health, evidence-based, patient-centered care, and building lasting patient relationships with those she serves.

TRAN NGUYEN
MSN, RN, APRN, FNC-C
Family Nurse Practitioner
LOCATION: Pearland Family Health Center
Tran Nguyen, MSN, RN, APRN, FNC-C is a Family Nurse Practitioner who is board-certified by the American Academy of Nurse Practitioners. She began her career at Ben Taub General Hospital in the IMU unit, then later worked at Houston Methodist Hospital on the telemetry unit for three and a half years. While working full-time at Methodist, she obtained her master’s degree in nursing from UT Health Science Center at Houston. She has been a Nurse Practitioner since 2018, working with patients of all ages. She can treat a variety of acute and chronic conditions. Her goal is to promote healthy lifestyles to prevent diseases and their complications.

How Your Body Changes
The First Trimester

Motherhood, for many expecting mothers, can spark a storm of emotions ranging from joy and ending in stress. During these changes, the body is in a fury of hormonal and physical changes to prepare for the child. Navigating the emotional and physical changes is overwhelming for anyone. Educating yourself on what to expect during the first trimester, however, can help you be prepared to begin the journey into motherhood.
Emotionally, motherhood could become a source of stress and happiness. Many new or expecting mothers can experience multiple emotions at once: delight, anxiety, exhaustion, etc. What’s important to remember is that any emotion any expecting mother feels is normal. Worrying about balancing work and life or the child’s health is natural. Take time now to begin adjusting your lifestyle and prepare to welcome your new child.
Physically, there are some changes one can expect to happen. Here are some common symptoms you might experience during early pregnancy stages:
· Tender, Swollen Breast
The breasts will start to feel sensitive or sore due to hormonal changes. The tenderness will go down as your body adjusts to the hormones.
· Nausea
While commonly called “Morning Sickness,” nausea can hit at any moment of the day and typically occurs one month after you become pregnant. Avoid having an empty stomach by eating slowly and in small amounts every 1-2 hours. Avoid smelly, fatty food, and drink plenty of fluids.

· Fatigue
The pregnancy hormone progesterone soars, which can make you sleepy. A healthy diet and exercise can increase energy but be sure to rest as much as possible.
· Increased Urination
The amount of blood in the body increases during pregnancy and your kidneys process the extra fluids that end up in your bladder. As such, you might find yourself using the bathroom more often
· Food Cravings/Aversions
You might become more sensitive to certain odors and tastes—changing what you want to eat and what makes you disgusted.
· Constipation
Due to the high progesterone hormone levels, food movement can slow down, causing constipation. Be sure to have plenty of fiber in your diet and drink lots of fluids.
With all these changes, it is vital to consult a medical professional to ensure everything is developing accordingly. During these visits, your provider may ask for your medical history and your family’s medical history. Additionally, there will be exams and tests: pelvic exams to get information regarding the fetus, lab tests such as urine and blood test, blood screenings, genetic test, and other screening tests. If there are any questions, be sure to reach out to your MyPrenatal Care provider to schedule an appointment to alleviate any doubts.
While becoming a mother may seem daunting, it is important to remember that expecting mothers are not alone. These physical changes and emotional turbulence are normal. Seek help from your partner, family, and friends, or your MyPrenatal Care provider. Additionally, support networks are there to help mothers every step of the way.

The Second Trimester
The second trimester starts at 13 weeks into pregnancy. These times are the most enjoyable, with some of the “morning sickness” fading off. It is also said that the second trimester is one of the easiest as your body adjusts to the increased hormone levels. Moreover, some women have noticed their baby’s growth with the arrival of baby bumps. With so many exciting changes occurring, here is what to expect while entering the second trimester of pregnancy. Emotionally, many women feel much less overwhelmed. The first trimester is filled with emotional turmoil as mothers stress over whether they are prepared for a child. During the second trimester, many mothers have gotten used to the idea of being pregnant; moreover, the feelings of exhaustion from the influx of hormones have lessened. The renewed sense of energy and getting used to the idea of being pregnant make many mothers feel much less overwhelmed. There may still be anxiety, but these feelings are normal and can be dealt with by setting yourself up for pregnancy (i.e., learning about your company’s maternity leave policy).
Physically, there still some big changes occurring:
Growing Belly and Breasts
To make room for your growing baby, your uterus will expand, making the belly area grow. Also, breasts will continue to increase in size as well. Pro tips: a supportive bra with wide straps or a sports bra will help with support!

Braxton Hicks Contractions
You might feel mild, irregular contractions—these contractions usually occur in the abdomen as a slight tightness. These contractions generally occur in the afternoon or evening, after physical activity or sex. If these contractions become regular and steadily increase in strength, contact your MyPrenatal Care provider, as this could be a sign of preterm labor.
Skin Changes
The hormonal change during pregnancy increases specific skin cells, resulting in brown patches on your face or a dark line down your abdomen. These changes are common and tend to fade after delivery. It is important, however, to limit sun exposure as it can darken these marks. Finally, stretch marks may appear throughout the body and cannot be prevented. A lot of the stretch marks, however, fade in intensity.
Nasal Problems
With the rise of hormone levels, the body responds by making more blood which causes the
mucous membrane to swell and bleed easily. This can result in stuffiness or nosebleeds. Saline drops, hydration, or humidifiers can help lessen congestion.
Dental Issues
Gums become more sensitive to flossing and brushing, and frequent vomiting can affect your tooth enamel. Switching to a softer brush and rinsing with salt water can help decrease irritation, but it is essential to be up to date with dental care during pregnancy.
Dizziness
The body undergoes changes that affect blood circulation within the body—the result is a feeling of dizziness. Be sure to drink plenty of fluids, avoid standing for long periods, and slowly stand up or change positions.
Leg Cramps
Leg cramps are common and usually occur at night. To prevent leg cramps, have routine stretches before bed while maintaining an active lifestyle. If a cramp does strike, be sure to stretch the affected calf muscle. Hot showers, warm baths, and ice massages have also been shown to help.

Vaginal Discharge
You might notice a sticky, clear, or white vaginal discharge. This is normal, but be sure to contact your MyPrenatal Care provider if the discharge becomes strong smelling, changes colors, or is accompanied by pain/itchiness. These could indicate a vaginal infection.
Urinary Tract Infections
UTIs are common during pregnancy. Be sure to contact your MyPrenatal Care provider if you have a strong urge to urinate or can’t delay urination, experience sharp pain when you urinate, have cloud urine, have strong smelling urine, notice blood in your urine, experience a fever, or a backache. If left untreated, UTIs can become severe and result in a kidney infection.
The second trimester is met with a lot of growth and changes, but it is an exciting and wonderful time. With so many changes, it is essential to stay up to date with your prenatal appointments. These appointments help by ensuring all the growth and symptoms of the second trimester are normal. These appointments also allow expecting mothers to hear their child’s heartbeat and find out the sex. While overwhelming at some points, this trimester
is met with many wonderful opportunities to recognize how much closer you are to meeting
The Third Trimester
Mothers enter the third trimester at 28 weeks of being pregnant and stay in this trimester until delivery day. With the second trimester being considered one of the most comfortable, the third trimester is tiring and uncomfortable. The baby’s size and position limit comfort, and many feel eager to hold their baby. The anticipation builds up, which makes many mothers want to be ready to know what to expect during the third trimester.
Emotionally, expecting mothers could experience some fears regarding delivery. What does childbirth look like? What will happen, and how long will it take? The anticipation, while exciting, can cause anxiety in some expecting mothers. Many may be dealing with the reality of motherhood and think of the future after the baby is here. To help soothe your thoughts, consider journaling down persistent fears and ideas. Consider talking to other expecting mothers to share your excitement and fears; speak to others with positive birth experiences. Physically, there are still changes occurring in the body:
Braxton Hicks Contractions
You might feel mild, irregular contractions—these contractions usually occur in the abdomen as a slight tightness. These contractions usually occur in the afternoon or evening, after physical activity or sex. If these contractions become regular and steadily increase in strength, be sure to contact your health care provider, as this could be a sign of preterm labor.
Backaches
Pregnancy hormones relax the connective tissues that hold your bones together. With the added weight of a child, these changes can be tough on your back. Make sure to sit in chairs with good back support and regular exercise. Wear low-heeled shoes with good arch support,but make sure they are not completely flat.

Shortness of Breath
It is normal to get winded easily. Maintain good posture to help give the lungs room to breathe and slow down.
Heartburn
With the pregnancy hormone relaxing the valve between your stomach and esophagus, stomach acid may reflux into your esophagus and cause heartburn. To prevent heartburn, eat small, frequent meals, and avoid fried foods, citrus, chocolate, and spicy foods.
Spider veins, varicose veins, and hemorrhoids
The increased blood circulation can cause tiny, red-purplish veins to appear on your face, neck, and arms (spider veins). You might also notice swollen veins on your legs (varicose veins). Painful, itchy varicose veins in your rectal area can also occur (hemorrhoids). To help with the swelling, exercise and elevate your legs frequently while incorporating fiber and water into your diet.
Frequent Urination
As the baby moves deeper into the pelvis, you’ll feel more pressure on your bladder. As a result, you find yourself urinating more and sometimes leaking urine when you laugh, cough, sneeze, bend, or lift. Panty liners are a must if this becomes an issue.
As the delivery date comes closer, your MyPrenatal Care provider might ask you to come in more often. These visits will include regular check-ups to monitor weight, blood pressure, and any symptoms you may be experiencing. These

physicals will also occur for your child as the provider will monitor the baby’s position and movement. Additionally, you may need to take vaccinations during your third trimester to help protect your child. Finally, there will be screening tests for various conditions such as: gestational diabetes, iron deficiency anemia, and group b strep. While many mothers are eager to hold their baby, they must ensure they maintain consistent check-ups to make sure their baby is healthy once they arrive.
The Fourth Trimester
Many people think there are only three trimesters in the journey of motherhood. The last trimester (delivery to 12 weeks after delivery) is a critical time for the mother and child. This 12-week period sets the stage for long-term health and well-being while the mother’s body undergoes physical changes. In the fourth trimester, it is not only important to take care of your new baby but of your body as well.
Physically, the body undergoes tremendous stress and changes when delivering the baby. Depending on the delivery method, what to expect varies as new mothers undergo recovery. The largest difference between a c-section recovery and a vaginal birth recovery is the


aftercare to prevent infection.
After a C-section, be sure to treat the incision with care: take it easy and rest whenever possible. Avoid lifting anything heavier than your baby while monitoring your incision for any redness, swelling, or leakage, as it may be a sign of an infection. Be sure to experiment with proper breastfeeding positions that work well with C-section recovery.
For vaginal births, vaginal soreness may occur for a few weeks after delivery, especially after an extensive tear. To help with vaginal soreness, mothers should sit on pillows or padded rings.
If the area is sore, use an ice pack or a chilled witch hazel pack between a sanitary napkin on the area between your vaginal opening and anus (perineum). Sit in a warm bath that just covers your buttocks and hips for five minutes. You can also use cold water if you find it more soothing. Finally, be sure to use over-the-counter remedies for general pain or constipation. Be sure to talk to your health care provider if you experience severe, persistent, or increasing pain.
There are several common postpartum signs and symptoms:
Vaginal Discharge Contractions “After Pains”
Tender Breasts
Hair loss and skin changes
Mood Changes
The early post-partum period is a time of great joy. While the joy is there, it is also a time when new mothers are most vulnerable to Postpartum
Depression or infection. Thus, it is important to prioritize postpartum health. After childbirth, talk with your MyPrenatal Care provider about risks of pregnancy-related complications and if you need any special
follow-up care. Rather than having a single visit after your delivery, have contact with your provider within the first 3 weeks after delivery.
Weight Loss

Within 12 weeks after delivery, have your MyPrenatal Care provider conduct a comprehensive postpartum evaluation.
Although the 4th trimester is focused on keeping the newborn as healthy as possible, it is equally important that we protect our new mothers. By staying up to date with post-partum visits with primary care professionals, mothers can limit their risk of post-partum complications and infections. 4th-trimester care doesn’t only happen for the baby. Mothers must also care for themselves to keep their baby happy and healthy.
Avoiding Postpartum Complications
The early postpartum period is a time of great joy. While joyful, it is also a time when new mothers are at an increased risk for postpartum complications.
Maternal Mortality Rates in the US, 2020
• In 2020, 861 women were identified as having died of maternal causes in the United States, compared with 754 in 2019. The maternal mortality rate for 2020 was 23.8 deaths per 100,000 live births compared to a rate of 20.1 in 2019.
• The maternal mortality rate for non-Hispanic Black women was 55.3 deaths per 100,000 live births which is 2.9 times the rate for non-Hispanic White women.
• Rates for non-Hispanic Black women were significantly higher than rates for non-Hispanic White and Hispanic women.
• There was a significant increase in maternal mortality from 2019 to 2020 for non-Hispanic Black and Hispanic women.
• Rates only increase with maternal age.
MyPrenatal Care is committed to closing the racial disparities and decreasing maternal morbidity and mortality. Thus, it is important to prioritize postpartum health. After childbirth, talk with your provider about the risks of pregnancy-related complications and if you need any special follow-up care.
Rather than having a single visit after your delivery, you should have contact with your provider within the first 3 weeks after delivery. This can be an in-office visit or even by tele-health. However, if your MyPrenatal Care provider determines that you are at high-risk for postpartum complications, the provider may recommend an office visit 3 to 10 days after delivery.
Within 12 weeks after delivery, an appointment should be scheduled with your MyPrenatal Care provider to conduct a comprehensive postpartum assessment. During this assessment,
your provider will evaluate:
• Your mood and emotional well-being
• Screen for postpartum depression
• Assess your comfort and confidence for caring for your newborn
• Assess comfort and confidence with breastfeeding
• Assess material needs (such as stable housing, utilities, food, and diapers) and provide referrals to resources as needed
• Provide guidance regarding sexuality
• Discuss birth spacing (avoiding pregnancy sooner than 18 months after delivery)
• Assess desire for future pregnancies
• Discuss coping options for fatigue and sleep disruption
• Assess and discuss physical recovery from birth
• Chronic disease management (hypertension, diabetes, thyroid disease, etc.)
• Review vaccination history and provide immunizations if needed
• Perform well-woman screening (including PAP test, if needed)
Postpartum Tips!
• Inform all health care providers that you visit that you are postpartum up until your 6th week after delivery.
• Keep all postpartum visits
• Monitor for elevated blood pressure
• Be kind to yourself and ask for help when you need it
• Resume your regular health maintenance with your primary care provider after you have completed the postpartum period.
Baby Blue and Postpartum Depression
The “4th trimester” or postpartum period is both exciting and overwhelming. Having a baby is a life-changing experience and almost every mom faces a period of the “baby blues” due to the roller coaster of hormones, lack of sleep and the struggle to adjust to a new baby in the home. While having the baby blues, a new mom experiences a period of anxiety, feeling down, mood swings, crying spells, and difficulty sleeping. Baby blues can start 2-3 days after delivery and typically lasts for less than two weeks. During this time, take care of yourself and be kind to yourself. Share your feelings with your loved ones and ask do help.
With that said, some moms experience a more severe, long-lasting form of depression known as postpartum depression (PPD). Moms with PPD can experience severe mood swings, irritability, loss of appetite, overwhelming fatigue, and a lack of joy in life shortly after childbirth. PPD affects up to 20% of postpartum moms. It is not a character flaw or a weakness. PPD is not your fault and is nothing to be ashamed of.
If you feel that you may be experiencing postpartum depression (PPD) symptoms, ask yourself the following questions and review your score with your MyPrenatal Care provider:
I have been able to laugh and see the funny side of things.
(0) As much as I always could
(1) Not quite so much now
(2) Definitely not so much now
(3) Not at all
I have looked forward with enjoyment to things.
(0) As much as I ever did
(1) Rather less than I used to
(2) Definitely less than I used to
(3) Hardly at all
I have blamed myself unnecessarily when things went wrong.
(3) Yes, most of the time
(2) Yes, some of the time
(1) Not very often
(0) No, never
I have been anxious or worried for no good reason.
(0) No, not at all
(1) Hardly ever
(2) Yes, sometimes
(3) Yes, very often
I have felt scared or panicky for no very good reason.
(3) Yes, quite a lot
(2) Yes, sometimes
(1) No, not much
(0) No, not at all
Things have been getting on top of me.
(3) Yes, most of the time I haven’t been able to cope
(2) Yes, sometimes I haven’t been coping as well as usual
(1) No, most of the time I have coped quite well
(0) No, I have been coping as well as ever
I have been so unhappy that I have had difficulty sleeping.
(3) Yes, most of the time
(2) Yes, sometimes
(1) Not very often
(0) No, not at all
I have felt sad or miserable.
(3) Yes, most of the time
(2) Yes, quite often
(1) Not very often
(0)
No, not at all
I have been so unhappy that I have been crying.
(3) Yes, most of the time
(2) Yes, quite often
(1) Only occasionally
(0) No, never
The thought of harming myself has occurred to me.
(3) Yes, quite often
(2) Sometimes
(1) Hardly ever
(0) Never
Score: __________________
Staying Healthy During Pregnancy
HEALTHY EATING DURING PREGNANCY
No diet can assure a healthy pregnancy. For the most part, maintaining a healthy diet during pregnancy has the same principles as eating while not pregnant. Have a healthy balance of fruits, veggies, carbs, and proteins. There are some key nutrients that play an important role while pregnant.
Folate and Folic Acid
Folate and folic acid help prevent birth defects. Therefore, it is recommended that you consume anywhere from 400 to 1,000 microgames a day before conception and throughout pregnancy. Good sources of folic acid like fortified cereals, leafy greens, citrus fruits, dried beans, and peas are a good source of folate.

Calcium
Calcium is a crucial component to forming healthy bones. Thus, for a growing baby, it is
important to consume calcium to ensure they are growing strong bones. Calcium also aids in making sure the circulator, muscular, and nervous systems are functioning normally. It is recommended to consume 1,000 milligrams a day (for pregnant teens, 1,300 milligrams a day). Good sources of calcium are dairy sources, but good non-dairy sources includes broccoli, kale, fruit juices, and breakfast cereals fortified with calcium.
Vitamin D
Vitamin D promotes bone strength and helps your baby to grow strong bones like calcium. It is recommended to consume 600 international units a day. Good sources of Vitamin D are fatty fish (salmon), milk, and orange juice.
Protein
Protein plays an important role in promoting your child’s growth during pregnancy. Consuming 75 to 100 grams of protein a day is recommended. Because of protein’s vital role, consuming 71 grams of protein a day is recommended. Good protein sources are lean meats, poultry, fish, and eggs. Vegetarian options include beans, peas, nuts, seeds, and soy products.

Iron
Iron helps prevent iron deficiency anemia. During pregnancy, expecting mothers need double the amount of iron to supply oxygen to their baby. If they do not have enough iron, they could develop iron deficiency anemia as well as other serious health consequences. It is recommended to consume 27 milligrams of iron a day. Good sources of iron include lean red meat, poultry, fish, beans, and iron-fortified cereals.
EXERCISING WHILE PREGNANT
Exercising while pregnant is essential for expecting mother. It helps keep the mind and body healthy to manage the stress of pregnancy as well as promote sleep. Moreover, it helps reduces risks of pregnancy conditions as well as having a c-section. With these benefits, staying active and moving while pregnant is a good idea, but many expecting mothers may still have some questions about staying safe while pregnant. Here are some of the most common questions about exercising while pregnant:
Is it safe to exercise and how much exercise do I need to do?
For most pregnant women, exercising is essential to ensuring the expecting mother and the baby are healthy; however, at your first prenatal check-up, be sure to ask your MyPrenatal Care provider if it is safe to exercise. Once approved, expecting mothers should aim to do 2.5 hours of aerobic activities each week for about 30 minutes each day. These activities should make you sweat a bit and raise your heart rate (such as taking a brisk walk). A good indicator of working too hard is being unable to talk normally during the exercise.
What kinds of activities are recommended during pregnancy?
Be sure to check in with your MyPrenatal Care provider for their recommendation on how much physical activity you can do while pregnant. Moreover, you don’t need a gym or fancy equipment to stay active while pregnant. Some examples of exercise that is safe to do while pregnant are:
• Walking: Taking a brisk walk is a good way to stay active every day!
• Swimming and water workouts: The water helps support baby’s weight and keeps your heart rate steady. This is a good workout for mothers who are experiencing lower back pain.
• Riding a stationary bike: This is a safer option than riding a regular bike;expecting mothers are less likely to fall off a stationary bike.
• Strength training: Lifting weights can help build muscle and make your bones stronger. It is safe to lift weights while pregnant if they’re not too heavy. Be sure to talk to your provider to see if strength training is a good form of working out for you. What activities are unsafe to do during pregnancy?

Be sure to check with your MyPrenatal Care provider when choosing a physical activity. While pregnant, don’t do:
• Activities that may hit your belly: Activities such as hokey, boxing, soccer, or basketball are not safe to do while pregnant.
• Activities that have a lot of bouncing or jerking movements that can cause a fall: Activities such as horseback riding, skiing, gymnastic, or skating are not safe to do while pregnant.
• Any exercise that makes you lie flat on your back (after the first trimester): When you lie on your back you can cause your blood pressure to drop and limit the flow of blood to your baby (such as sit ups)
• Activities that cause you to hit the water with great force: Activities such as water skiing, surfing, or diving.
• Exercising at high altitude unless you already live at a high altitude.
• Activities such as hot yoga or working out during hot, humid days.
• Skydiving or scuba diving.
How to Take Care of Yourself When You Feel Sick During Pregnancy
Nausea is usually the most severe during early pregnancy within the first trimester (which includes up to week 13 of pregnancy) and may even be associated with vomiting. The term “morning sickness” can be misleading. It does not occur only in the morning, as it may last all day.

Natural remedies to try if you experience nausea while pregnant:
• Eating small meals or bland snacks (like hard candies or dry toast)
• Trying ginger products (like ginger candies, ginger teas, or ginger ale)
• Limiting acidic or spicy foods
• Avoiding stuffy rooms or strong odors
• Getting enough rest
• Wearing anti-nausea wristbands
Heartburn & Indigestion occurs in pregnancy due to hormonal changes that allow the esophagus muscles, including the lower esophageal sphincter (LES), to relax more frequently. The result is that more acids may seep back up, particularly when you’re lying down or after you’ve eaten a large meal. Here’s a checklist of natural remedies to try if you experience heartburn or indigestion while pregnant:

• Eat smaller, more frequent meals and avoid drinking while eating. Drink water in-between meals instead.
• Eat slowly and chew every bite thoroughly.
• Avoid eating a few hours before bed.
• Avoid foods and beverages that trigger your heartburn. Typical culprits include chocolate, fatty foods, spicy foods, acidic foods like citrus fruits and tomato based items, carbonated beverages, and caffeine.
• Stay upright for at least one hour after a meal. A leisurely walk may also encourage digestion.
• Wear comfortable rather than tight-fitting clothing.
• Maintain a healthy weight.
• Use pillows or wedges to elevate your upper body while sleeping.
• Sleep on your left side. Lying on your right side will position your stomach higher than your esophagus, which may lead to heartburn.
• Chew a piece of sugarless gum after meals. The increased saliva may neutralize any acid coming back up into the esophagus.
• Eat yogurt or drink a glass of milk to help relieve symptoms once they start.
Gas during pregnancy is a frequent occurrence, which also means that gas during pregnancy is a common concern. The typical person will pass gas approximately 18 times a day. The buildup of gas happens whether you are pregnant or not. However, you may notice more gas during pregnancy due to the hormone progesterone, which causes the muscles throughout your body to relax. Subsequently, your intestinal muscles relax more, which
causes your digestion to slow down. Gas during pregnancy can also increase later in pregnancy when the enlarging uterus places pressure on your abdominal cavity.
Natural remedies to try if you experience Gas while pregnant:
• Avoid or reduce carbohydrate drinks
• Avoid fatty fried foods
• Drink from a glass without using a straw
• Focus on smaller meals throughout the day
• Exercise, which will help stimulate digestion
• Avoid tight clothing around your waist
• Limit or avoid artificial sweeteners
• Drink plenty of water, which will help prevent constipation
• Eat slowly and chew thoroughly
Diarrhea during pregnancy is one of the unfortunate discomforts that may be experienced. Diarrhea literally means “flowing through” and is defined as having three or more loose or liquid bowel movements in a 24-hour period. If you are experiencing three runny, watery bowel movements in one day, the main concern is to stay hydrated. You can lose a significant amount of fluids when experiencing diarrhea during pregnancy. Dehydration can be serious, even deadly. You will need to make sure you are rehydrating yourself. Diarrhea is rarely life-threatening, but it shouldn’t be taken lightly, especially while pregnant.
Here’s a checklist of natural remedies to try if you experience diarrhea while pregnant:
• Eat bland food and drink clear fluids
• Drink a lot of fluids: Drink a minimum of 10 to 12 cups of fluids each day
• Get lots of rest
Constipation during pregnancy is a common problem. Most pregnant women get constipated at some point during their gestational period. Here’s a checklist of natural remedies to try if you experience constipation while pregnant:
• Eat a high-fiber diet. Ideally, you will consume 25 to 30 grams per day of dietary fiber from fruits, vegetables, breakfast cereals, whole-grain bread, prunes, and bran. This helps ensure bulkier stools that are easier to poop.
• Drink a lot of fluids. Drinking plenty of fluids is important, particularly when increasing fiber intake helps ensure softer stools. Drink 10 to 12 cups of fluids each day. It is the combination of a high-fiber diet and plenty of liquids that best help you eliminate your waste. Sweat, hot/ humid climates, and exercise may increase your need for additional fluids.
• Exercise routinely. If you are inactive, you have a greater chance of constipation. Walking,
swimming, and other moderate exercises will help the intestines work by stimulating your bowels. Schedule exercise three times a week for 20-30 minutes each.
Cold or Flu During pregnancy, changes occur in your immune system, heart, and lungs. Additional stress is put on the heart and lungs as the lung capacity decreases and the heart rate increases during pregnancy. During this time, the immune system is also naturally suppressed, making you more susceptible to a cold or the flu during pregnancy. You can take steps as precautionary measures to prevent the cold or flu:
regularly washing your hands, healthy eating habits, getting plenty of rest, and staying away from others who may be ill. The flu vaccination has also been proven safe for both Mommy and the unborn baby and is recommended to be administered early in the flu season. Symptoms of a cold or the flu: headache, runny nose, sore throat, fatigue, shortness of breath, loss of appetite, diarrhea or vomiting, sudden chills or fever, or body aches.
Here’s a checklist of natural remedies to try if you experience a cold or the flu while pregnant:
• Get plenty of rest and sleep
• Drink plenty of fluids
• Contact your MyPrenatal Care provider immediately should a fever arise at or greater than 102 degrees Fahrenheit.
Sinusitis or Allergies while pregnant can be a bit more annoying while a baby is growing inside of you. Largely due to the limited choices you have of medications or remedies when a flare-up occurs.

Here’s a checklist of natural remedies to try if you experience sinusitis or allergies while pregnant:
• Avoiding allergy triggers as much as possible Eat slowly and chew every bite thoroughly.
• Wear a mask while exposed to pollen outdoors.
• Take approved saline nasal sprays and antihistamines when able to A Sore Throat is rarely an indicator of serious illness but can cause discomfort. Symptoms
of a normal sore throat can vary from mild to severe: minor itching, rawness, burning pain, and sandpaper-like scratching. If your symptoms are more severe and are accompanied by a fever or body aches, please contact your MyPrenatal Care provider immediately.

Natural remedies to try if you experience a Sore Throat while pregnant:
• Vitamin C Supplements
• Hot Tea with Lemon
• Increase fluids intake
• Gargle with Warm Saltwater
• Contact your MyPrenatal Care provider immediately should a fever arise at or greater than 102 degrees Fahrenheit.
Congestion seems like it doesn’t go away while pregnant. This hassle is called pregnancy rhinitis. Due in part to hormonal changes, this inflammation of the mucous membranes lining of the nose causes increased blood flow to the nasal passages and enlargement of the nasal veins.
Here’s a checklist of natural remedies to try if you experience congestion while pregnant:
• Increase the humidity levels in the home
• When sleeping, raise the head of the bed or add an extra pillow to elevate the head
• Drink plenty of fluids
• Take warm baths or showers
Headache, Pain, General
Discomfort, Fever Reducer During pregnancy, your body goes through various changes as it creates a tiny new human inside your womb. These changes cause stress to the body, and in turn, various aches and pains may arise and are normal. However, understanding what is normal and what is not normal is what needs to be monitored.
Normal: minor headaches, lower back pain, sciatic nerve pain, leg cramps, round ligament pain (due to the uterus growing), and Braxton-Hicks contractions.
Abnormal: headaches accompanied by blurry vision or light sensitivity, bleeding, menstrual-like cramps, any pain accompanied by fever, or severe pain directed to one side of the body.
Leg Cramps are not uncommon during pregnancy, particularly in the third trimester. Muscle spasms, mainly in the legs, become more frequent during the evening. These cramps can be due to weight gain, changes in circulation, and or pressure from the growing baby, which may “pinch” nerves or blood vessels in the legs.

Natural remedies to try if you experience a Headache, Pain, General Discomfort or want to reduce a Fever while pregnant:
• If approved by your MyPrenatal Care Provider, exercise regularly.


• Rest with your legs elevated
• Wear support stockings
• Massage your calves and feet.
• Take Warm baths in Epsom salt.
Insomnia and Sleep Aids It is important to know that lack of sleep or insomnia is not harmful to your baby. Insomnia is very normal and typically affects approximately 78% of all pregnant women. Insomnia is inadequate or poor-quality sleep due to: hormonal changes, difficulty falling asleep, waking up frequently during the night, difficulty returning to sleep, or unrefreshing sleep. This can be related to multiple reasons: increasing size of the abdomen, back pain, heartburn, frequent urination, and anxiety. Here’s a checklist of natural remedies to try if you experience insomnia: Try new sleeping positions; If you are a back sleeper, in the second and third trimester, make sure to sleep on your side (the left side is best for circulation).
• Try new sleeping positions; If you are a back sleeper, in the second and third trimester, make sure to sleep on your side (left side is best for circulation).
• Get a pregnancy pillow to support your head and body during your sleep.
• Prepare yourself for bedtime by taking a warm bath or changing the thermostat to be at a more comfortable temperature.
• If cleared by your provider exercise regularly during the day to “tire you out” by bedtime.
• Try to limit fluid intake in the evening to limit
urination frequency (when healthy and in the 1st and 2nd trimester.
For more information and additional Questions, contact your MyPrenatal Care provider!
Recommendations for Medications During Pregnancy
All medications should be consulted with your MyPrenatal Care provider before consumption. The over-the-counter medications in this list are generally safe for most pregnancies. Please contact us immediately if your symptoms last more than 3 consecutive days or worsen at any point.
Symptoms During Pregnancy During Breastfeeding
Nausea
Hard candies such as peppermints or sour candies may help. Sour food tends to keep food down and focus away from the feeling.
Heartburn, Indigestion, Gas
Eating small frequent meals. Avoid greasy, spicy, and acidic foods. Limit carbonated sugary soda, tea, and caffeine. Avoid lying down within 3 hours of eating.
Diarrhea
Make sure to drink plenty of water, juice, and broth, to rehydrate yourself and replace the electrolytes your body has lost.
Constipation
Increase fluid intake to 64oz daily. Add fiber to your diet.
Cold or Flu
Drink plenty of fluids and rest. Eat and drink clear liquids only.
Benadryl, Dramamine, Emetrol, Bonine, Eat a lemon or add lemon to your water
Tums, Rolaids, Maalox, Mylanta, Zantac, Pepcid, Gas-X
Sour candies or teas
Same as pregnancy
Kaopectate, Imodium, increase water intake, bananas, white rice, applesauce, and toast
Only natural nonmedications.
No Kaopectate, Imodium, or Pepto Bismol
Metamucil, Milk of Magnesia, high-brand diet, increase water intake
Tylenol, approved electrolytes, rest.
Monitor symptoms and contact your MyPrenatal Care provider should a fever arise at or greater than 102 degrees Fahrenheit
Same as pregnancy, continue to nurse your baby
Symptoms During Pregnancy During Breastfeeding
Cough or Sore Throat
Get ample rest and drink plenty of fluids to limit your already weakened immune system from attack of a virus or bacterial infection.
Sinusitis or Allergies
Wear a mask while dusting, sweeping, or outside during pollen seasons.
Congestion
When resting, elevate your head by adding more pillows to prop your head higher than your body.
Headache, Pain, General Discomfort, Fever Reducer
Try to reduce your stress levels and get more rest. Your body is creating a tiny human and it is a lot of work.
Leg Cramps
Try elevating your feet when resting and massage your feet and calves with mild pressure.
Insomnia or Sleep Aid
Try to tire yourself out by getting enough (approved) exercise during the day and limit water intake in the evenings to limit night-time urination.
Robitussin (plain), Mucinex (during 2nd and 3rd trimester), Vicks Vapor Rub, Warm saltwater gargle, Cough Lozenges, Chloraseptic Spray, Tylenol
Saline Nasal Spray, Nasal Irrigation, Nasal Strips, Claritin, Zyrtec, Benadryl, Tylenol
Saline Nasal Spray, Nasal Irrigation, Nasal Strips, Benadryl, Humidifier, Elevate head while sleeping
Same as pregnancy
Saline Nasal Spray, Nasal Irrigation, Nasal Strips, Claritin, Tylenol
Saline Nasal Spray, Nasal Irrigation, Nasal Strips, Humidifier, Elevate head while sleeping
Tylenol, Increase Water Intake, Icy-hot (hot or cold compress),
Same as pregnancy
Epsom Salt Bath, Eat a Banana a day (if not allergic),
Benadryl, Tylenol PM, Unisom, Chamomile tea, Warm Baths, limit water in the evening hours
Antibiotics Seek care from your MyPrenatal Care Provider
Same as pregnancy
Chamomile Tea and Warm Baths.
Be aware! Antihistamines like Benadryl can decrease milk production.
Seek care from your MyCHN provider
Frequently Asked Questions
MORNING SICKNESS: NAUSEA AND VOMITING OF PREGNANCY
How common is nausea and vomiting of pregnancy?
Nausea and vomiting during pregnancy is a very common condition. Although nausea and vomiting during pregnancy often is called “morning sickness,” it can occur at any time of the day. Nausea and vomiting during pregnancy is usually not harmful to the developing baby, but they can seriously affect your life, including your ability to work or do your normal daily activities.
When does nausea and vomiting of pregnancy start?
Nausea and vomiting during pregnancy usually starts before 9 weeks of pregnancy. It goes away by the second trimester (13 weeks of pregnancy) for most women. For some women, it lasts for several weeks or months. For a few women, it lasts throughout the entire pregnancy.
What is the difference between mild and severe nausea and vomiting during pregnancy?
Some women feel nauseated for a short time each day and may vomit once or twice. This usually is defined as mild nausea and vomiting during pregnancy. In more severe cases, nausea lasts several hours each day, and vomiting occurs more frequently. Deciding to seek treatment depends on how much nausea and vomiting during pregnancy affects your life and causes you concern, not whether your condition is “mild” or “severe.”
What is hyperemesis gravidarum?
Hyperemesis gravidarum is the most severe form of nausea and vomiting during pregnancy. It occurs in up to 3% of pregnancies. This condition may be diagnosed when a woman has lost 5% of her pregnancy weight and has other problems related to dehydration (loss of body fluids). Women with hyperemesis gravidarum need treatment to stop their vomiting and restore body fluids. Sometimes treatment in a hospital is needed.
Am I at risk of severe nausea and vomiting of pregnancy?
If you have any of the following factors, your risk of severe nausea and vomiting during pregnancy may be increased:
• Being pregnant with more than one baby
• Past pregnancy with nausea and vomiting (either mild or severe)
• Your mother or sister had severe nausea and vomiting during pregnancy
• History of motion sickness or migraines
• Being pregnant with a female fetus
Could another medical condition cause nausea and vomiting during pregnancy?
Some medical conditions can cause nausea and vomiting during pregnancy. These include an ulcer, food-related illness, thyroid disease, or gallbladder disease. Your MyPrenatal Care provider may suspect that you have one of these conditions if you have signs or symptoms that do not usually occur with nausea and vomiting of pregnancy:
• Nausea and vomiting that occurs for the first time after 9 weeks of pregnancy
• Abdominal pain or tenderness
• Fever
• Headache
• Enlarged thyroid gland (swelling in the front of the neck)
Can nausea and vomiting of pregnancy affect my baby?
Having nausea and vomiting during pregnancy usually does not harm your health or your baby’s health. It does not mean your baby is sick. It can become more of a problem if you cannot keep down any food or fluids and begin to lose weight. When this happens, it can sometimes affect the baby’s weight at birth. You also can develop problems with your thyroid, liver, and fluid balance.
When is the best time to treat nausea and vomiting during pregnancy?
Because severe nausea and vomiting during pregnancy is hard to treat and can cause health problems, many experts recommend early treatment so that it does not become severe.
What can I do to feel better if I have nausea and vomiting during pregnancy?
Diet and lifestyle changes may help you feel better. You may need to try more than one of these suggestions:
• Take a multivitamin.
• Try eating dry toast or crackers in the morning before you get out of bed to avoid moving around on an empty stomach.
• Drink fluids often.
• Avoid smells that bother you.
• Eat small, frequent meals instead of three large meals.
• Try bland foods. For example, the “BRATT” diet (bananas, rice, applesauce, toast, and tea) is low in fat and easy to digest.
• Try ginger ale made with real ginger, ginger tea made from freshly grated ginger, ginger
capsules, and ginger candies.
• If you vomit a lot, it can cause some of your tooth enamel to wear away. This happens because your stomach contains a lot of acid. Rinsing your mouth with a teaspoon of baking soda dissolved in a cup of water may help neutralize the acid and protect your teeth.
Is there medical treatment for nausea and vomiting during pregnancy?
If diet and lifestyle changes do not help your symptoms, or if you have severe nausea and vomiting during pregnancy, medical treatment may be needed. If other medical conditions are ruled out, certain medications can be given to treat nausea and vomiting during pregnancy:
Vitamin B6 and doxylamine-Vitamin B6 is a safe, over-the-counter treatments that may be tried first. Doxylamine, a medication found in over-the-counter sleep aids, may be added if vitamin B6 alone does not relieve symptoms. A prescription drug that combines vitamin B6 and doxylamine is available. Both drugs taken, alone or together, have been found to be safe to take during pregnancy and have no harmful effects on the baby.
Antiemetic drugs-If vitamin B6 and doxylamine do not work, “antiemetic” drugs may be prescribed. These drugs help relieve nausea and prevent vomiting. Many antiemetic drugs have been shown to be safe to use during pregnancy. Others have conflicting or limited safety information. You and your MyPrenatal Care provider can discuss all of these factors to determine the best treatment for your personal situation.
What may happen if my nausea and vomiting are severe, or I have hyperemesis gravidarum?
You may need to stay in the hospital until your symptoms are under control. Lab tests may be done to check how your liver is working. If you are dehydrated from loss of fluids, you may receive fluids and vitamins through an intravenous line. If your vomiting cannot be controlled, you may need additional medication. If you continue to lose weight, sometimes tube feeding is recommended to ensure that you and your baby are getting enough nutrients.
GLOSSARY
Dehydration: A condition that results from loss of water from the body.
Fetus: The developing organism in the uterus from the ninth week of pregnancy until the end of pregnancy.
Hyperemesis Gravidarum: Severe nausea and vomiting during pregnancy can lead to weight loss and body fluids.
Nausea and Vomiting of Pregnancy: A condition that occurs in early pregnancy, usually starting before 9 weeks of pregnancy.
Nutrients: Nourishing substances supplied through food, such as vitamins and minerals.
BLEEDING DURING PREGNANCY
What can cause bleeding during pregnancy?
Vaginal bleeding or spotting during pregnancy can have many causes. Some are serious, and some are not. Bleeding may occur early or late in pregnancy. Many women have vaginal spotting or bleeding in the first 12 weeks of pregnancy. Bleeding of the cervix may occur during sex. An infection of the cervix also can cause bleeding. Slight bleeding often stops on its own. However, bleeding during pregnancy may mean something more serious. You may have a higher chance of going into labor too early (preterm labor), having an infant who is born too small, or having a miscarriage.
How is bleeding during early pregnancy checked?
If you are bleeding in early pregnancy, your MyPrenatal Care provider may do a pelvic exam. You will be asked how much blood you have passed and how often bleeding has occurred. Your provider also will ask whether you have had any pain and, if so, its location and severity. A blood test may be done to measure human chorionic gonadotropin (hCG). Your body makes this substance during pregnancy. You may have more than one test because hCG levels increase throughout pregnancy. Your blood type also will be checked to see if you need treatment for Rh sensitization. Ultrasound may be used to find the cause of the bleeding.
Sometimes the cause is not found.
When does a miscarriage happen?
Miscarriage can occur at any time in the first half of pregnancy. Most often, it occurs in the first 13 weeks. It happens in about 15-20% of pregnancies.
What are the signs and symptoms of miscarriage?
The following signs and symptoms may indicate a miscarriage:
• Vaginal bleeding
• Cramping pain felt low in the abdomen (often stronger than menstrual cramps)
• Tissue passing from the vagina
• Many women who have vaginal bleeding have little or no cramping. Sometimes the bleeding stops, and the pregnancy goes on. Other times the bleeding and cramping may become stronger, leading to miscarriage.
Is treatment needed after a miscarriage?
If some tissue stays in the uterus, bleeding often continues. Your MyPrenatal Care provider may then recommend one or more treatment options. Medication may be used to help you pass the tissue. The tissue may be removed by dilation and curettage (D&C). It also may be removed by a suctioning device. This is called suction curettage. Sometimes more than one option is needed
What is an ectopic pregnancy?
An ectopic pregnancy occurs when the fertilized egg does not implant in the uterus. Instead, it implants somewhere else, often in one of the fallopian tubes. An ectopic pregnancy causes pain and bleeding early in pregnancy.
What risks are associated with ectopic pregnancy?
A significant risk with this type of pregnancy occurs if the fallopian tube ruptures. A rupture needs prompt treatment. There may be internal bleeding. Blood loss may cause weakness, fainting, pain, shock, or death.
What is placental abruption?
The placenta is attached to the uterine wall. It may detach from the wall before or during labor. This may cause vaginal bleeding. It often causes pain, even if bleeding is light or not seen. When the placenta becomes detached, the fetus may get less oxygen. Prompt care is needed.
What is placenta previa?
When the placenta lies low in the uterus, it may cover the cervix. That means it partly, or completely blocks the opening. This is called placenta previa. It may cause vaginal bleeding. This type of bleeding often occurs without pain.
Can bleeding be a sign of labor?
Late in pregnancy, vaginal bleeding may be a sign of labor. A small amount of mucus and blood is passed from the cervix just before or at the start of labor. This is called “bloody show.” It is common. It is not a problem if it happens within 3 weeks of your due date. If it happens earlier, you may be going into preterm labor. Other signs of preterm labor include the following:
• Vaginal discharge
• Change in type of discharge (watery, mucus, or bloody)
• Increase in the amount of discharge
• Pressure in the pelvis or lower abdomen
• Low, dull backache
• Stomach cramps, with or without diarrhea
• Regular contractions or uterine tightening 46
• If you have any of these signs or symptoms, contact your MyPrenatal Care provider right away.
TOBACCO, ALCOHOL, DRUGS, AND PREGNANCY
Why is smoking dangerous during pregnancy?
If you smoke during pregnancy, your baby is exposed to harmful chemicals such as tar, nicotine, and carbon monoxide. Nicotine causes blood vessels to constrict, so less oxygen and nutrients reach the fetus. Carbon monoxide decreases the amount of oxygen the baby receives.
How can smoking during pregnancy put my baby at risk?
The risks of preterm birth and problems with how the placenta attaches to the uterus increase in women who smoke during pregnancy. Also, infants born to women who smoke during pregnancy tend to be smaller than those born to nonsmokers. They are more likely to have asthma, colic, and childhood obesity. They also have an increased risk of dying from sudden infant death syndrome (SIDS).
How can secondhand smoke affect my baby during pregnancy?
Breathing secondhand smoke from cigarettes smoked by other people nearby can increase the risk of having a low-birth-weight baby by as much as 20%. Infants who are exposed to secondhand smoke have an increased risk of SIDS and are more likely to have respiratory illnesses than those not exposed to secondhand smoke.
What help is available if I want to quit smoking?
If you are pregnant and you smoke, tell your MyPrenatal Care provider. He or she can help you find support and quitting programs in your area. You also can call the national “quit line” at 1-800-Quit-Now.
Can I use nicotine gum or the patch to help me quit smoking when pregnant?
Nicotine replacement (such as nicotine gum or the patch) or prescription medications for quitting smoking need to be used with caution during pregnancy. Over-the-counter nicotine replacement products should be used only if other attempts to quit have not worked and you and your MyPrenatal Care provider have weighed the known risks of continued smoking against the possible risks of these products. Smokeless tobacco, electronic cigarettes, and nicotine gel strips are not safe substitutes for cigarettes.
Why is drinking during pregnancy dangerous for my baby?
When a pregnant woman drinks alcohol, it quickly reaches the fetus through the placenta. In an adult, the liver breaks down the alcohol. A baby’s liver is not fully developed and is unable to break down alcohol.
What are fetal alcohol spectrum disorders?
“Fetal alcohol spectrum disorders” is a term that describes different effects that can occur in infants when a woman drinks during pregnancy. These effects may include physical, mental, behavioral, and learning disabilities that can last a lifetime.
What is fetal alcohol syndrome?
Fetal alcohol syndrome (FAS) is the most severe alcohol spectrum disorder. FAS can cause growth problems, mental or behavioral problems, and abnormal facial features.
What amounts of alcohol can cause FAS?
FAS is most likely to occur in infants whose mothers drank heavily (3 or more drinks per occasion or more than 7 drinks per week) and continued to drink heavily throughout pregnancy, but it also can occur with lesser amounts of alcohol use. Even moderate alcohol use during pregnancy (defined as one alcoholic drink per day) can cause lifelong learning and behavioral problems in the child.
Is there an amount of alcohol that is safe to drink during pregnancy?
There is no safe level of alcohol use during pregnancy. Alcohol can affect the fetus throughout pregnancy. It is best not to drink at all while you are pregnant. If you did drink alcohol before you knew you were pregnant, you can reduce the risk of further harm to the baby by stopping drinking.
How can my drug use affect my baby during pregnancy?
A drug’s effects on the fetus depend on many things: how much, how often, and when during pregnancy it is used. The early stage of pregnancy is the time when the main body parts of the fetus form. Using drugs during this time in pregnancy can cause birth defects and miscarriage. During the remaining weeks of pregnancy, drug use can interfere with the growth of the fetus and cause preterm birth and fetal death.
What are some of the problems related to substance abuse?
These problems include work, relationship, and family issues; drunk-driving arrests and car crashes; or medical problems caused by the substance. Substance abuse can lead to dependence (addiction).
Why is it important to tell my MyPrenatal Care provider if I have used drugs during pregnancy?
It is important to be honest so that you get the help you need for yourself and your unborn baby. Drug testing of your hair or urine during pregnancy or during labor may be done if your provider suspects that you have used specific substances and if you have a complication during pregnancy or delivery that suggests drug use. The baby also can be tested after birth.
Will the results of my drug tests be kept confidential?
Some states consider drug use during pregnancy to be a form of child abuse. In some states, if a drug test result shows that you have used certain substances, it must be reported to state authorities. You should be informed about this testing and consent to it before it is done. How your consent is obtained also varies from state to state.
How can drug use affect my baby after he or she is born?
Drugs used after birth can be passed to the baby through breast milk.
What is addiction?
Addiction is a disease with three or more of the following signs and symptoms:
• Tolerance - Not having the same effect with continued use of the same amount and the need to use greater amounts of the substance to get “high.”
• Withdrawal symptoms after stopping use of the substance
• Using larger amounts of the substance or using it over a longer period
• Desire or unsuccessful attempts to cut down or control substance use
• Spending a great deal of time using or obtaining the substance or recovering from its use
• Reducing or giving up important social, work, or recreational activities because of substance use
• Continuing to use the substance despite knowing that you have a problem
• Making excuses to continue using the drug instead of meeting your home or work responsibilities
Why
is it important for pregnant women
who are
addicted to certain drugs, including pain medications and narcotics, to seek treatment to quit rather than quit on their own?
Withdrawal from these drugs can cause miscarriage or other harm to the fetus.
Can I take my prescription medication during pregnancy?
Some prescription medications are safe to take during pregnancy. Others have known risks. If you are taking a prescription medication and become pregnant, tell your MyCHN provider. Do not stop taking a medication prescribed for you without first talking to your MyPrenatal Care provider.
Community Health Network is so happy to welcome you and your new baby to our family. We are committed to putting our heart into you and your child’s care. The following sections will help you better understand what to expect as your child grows up. At CHN, we offer various pediatric services to help new mothers and fathers ensure their child is growing up happy and healthy. Our pediatric team is here to deliver quality care and preventative exams to protect your child. CHN offers newborn care, Well-Child Exams, immunizations, and important health exams for your child. We have even expanded our services to include pediatric dental services! Be sure to flip through our packet for more important information regarding our services, what to expect as your child grows up, and much more.

Meet Your Pediatric Providers
Dr. Shari A. Jackson

Pediatrician
Location: MyCHN League City
Dr. Shari Jackson received her medical doctorate from the University of Texas Health Science Center at San Antonio in 1999. Dr. Jackson completed her pediatrics residency at the University of Texas Medical Branch in Galveston in 2002. After residency, Dr. Jackson served proudly in the U.S. Army as a general pediatrician at Ft. Bragg, North Carolina. She was an Officer in Charge of the Pediatric Clinic at Womack Army Medical Center and Medical Director of the Exceptional Family Members Program. This program linked soldiers who had special-needs children with worldwide assignment stations that could accommodate their medical needs. Dr. Jackson has been a general pediatrician with Community Health Network since 2014 and continues her love of teaching medicine to the next generation of physician assistants and nurse practitioners. Dr. Jackson is board certified in Pediatrics and a diplomate of the American Board of Pediatrics, and a fellow of the American Academy of Pediatrics. Dr. Jackson has been recognized as one of the top pediatricians in the Alvin-Manvel area for four consecutive years in 2018, 2019, 2020, and 2021.
Dr. Mary Beth Keith
M.D. Pediatrician
Location: Women & Children’s Health Center
Dr. Mary Beth Keith received her medical degree from the University of Texas Health Science Center Houston (now McGovern Medical School) in 2015. She completed her Pediatric residency at McGovern Medical school in 2018, where she had the honor of receiving the Best Teaching Resident award. She is board certified by the American Academy of Pediatrics. Since completing her residency, she has practiced general pediatrics in the Greater Houston area.Dr. Keith believes in providing compassionate and empathetic care to her patients because she knows this enables them to live healthy lives. She has a special interest in breastfeeding, infant care, preventative medicine, and global health.

Dr. Antonia Way
M.D. Family Medicine
LOCATION: Scarsdale Family Health Center
Dr. Antonia L. Way received her medical degree at the University of New Mexico in 2010 and completed her residency with the University of New Mexico Department of Family and Community Medicine in 2013. She is board certified in Family Medicine and previously practiced General Medicine in the Webster area. Dr. Way sees a broad spectrum of patients from birth to geriatrics, including Women’s Health.
In addition to treating chronic diseases, and disease prevention, Dr. Way also treats musculoskeletal pain with trigger point injections and joint injections. She is interested in preventative medicine and a patient-centered approach to treating the entire family.
Dr. Way’s goal is to engage patients in both preventative and chronic care, practice evidence-based medicine, provide comprehensive care, and teaching patients how to live healthier and happier lives.

Uchenna A. Jones-Conley

MD, MBA, FSMB
MD, Family Medicine Physician
LOCATION: Freeport Community Health Center
Dr. Uchenna A. Jones-Conley, MD, MBA received her medical Degree at Wright State university in 2016 and completed her residency with the McGovern Medical School University of Texas at Houston Department of Family and Community Medicine in 2021. She is Board Eligible in Family Medicine. Dr. Jones-Conley treats a broad spectrum of patients ranging from birth to geriatrics. In addition to treating chronic disease, and disease prevention, Dr. Jones-Conley targets Women’s Health and treats musculoskeletal pain. She is interested in preventative and integrative medicine with a holistic approach to treatment.
Sherrell Gibson
MSN, APRN, FNP-C
Women and Children’s Nurse Practitioner
LOCATION: MyCHN Silverlake
Sherrell Gibson, MSN, APRN, FNP-C, is a Family Nurse Practitioner, board certified by the American Academy of Nurse Practitioners. She began her career as an associate degree registered nurse in 2004 and has a nursing career that spans across multiple specialties. Mrs. Gibson earned a Bachelor of Science in Nursing in 2014 while attending The University of Texas at Arlington. For graduate school, she attended The University of Texas Health Science Center of Houston where she earned a Master of Science in Nursing in 2018. Mrs. Gibson began her career as a family nurse practitioner at Community Health Network and completed specialized training to transition into a provider for Women and Children’s Services. She then completed focused training and the mentorship program through the American Society for Colposcopy and Cervical Pathology (ASCCP) to become a certified colposcopist in 2021. Mrs. Gibson has a strong passion for health promotion, risk reduction, and disease prevention with a particular interest and skill in Women’s Health, abnormal cervical cancer screening management, contraceptive education, and reproductive health.
Jemyra Calais
MSN, APRN, FNP-C
Women and Children’s Nurse Practitioner
LOCATION: Women & Children’s Health Community Center
Jemyra Calais, MSN, APRN, FNP-C, a Family Nurse
Practitioner, board certified by the American Academy of Nurse Practitioners. She is currently licensed to practice in the state of Texas. Ms. Calais received her Bachelor of Science in Nursing in 2012 from Dillard University in New Orleans, LA. Upon graduating, she acquired an abundance of knowledge in the nursing field ranging from Medical-Surgical, Post Op, NICU, Women’s Health, and Men’s Health. Ms. Calais decided to further her education by receiving her Master of Science in Nursing from South University in Savannah, Georgia. She currently practices as the Women


and Children’s Nurse Practitioner at Community Health Network’s Alvin clinic. She is passionate about preventative health and believes teamwork and a positive mindset are critical for maximizing patient outcomes.


Anneliese Hulse
MSN, APRN, FNP-C
Women’s and Children’s Nurse Practitioner
LOCATION: Women & Children’s Health Community Center
Anneliese (Onie) Hulse, MSN, APRN, FNP-C, is a family nurse practitioner who is board certified by the American Academy of Nurse Practitioners and licensed to practice in Texas. She began her career with a bachelor’s degree in nursing that she earned from the University of Texas Health Science Center School of Nursing in Houston in 2015. Her nursing experience includes labor and & delivery and antepartum nursing at The Woman’s Hospital of Texas, Houston Methodist, and Clear Lake Regional. She graduated with her master’s degree in nursing from UTHealth Cizik School of Nursing in Houston in 2021. She is passionate about preventive health, evidence-based, patient-centered care, and building lasting patient relationships with those she serves.
Destanee Hamilton
MPAS, PA-C
Women’s and Children’s Nurse Practitioner Physician Assistant
LOCATION: Scarsdale Family Health Center
Destanee Hamilton, MPAS, PA-C, is a Physician Assistant, board-certified by the National Commission on Certification of Physician Assistants. She is currently licensed to practice in the state of Texas. Destanee Ms. Hamilton re- ceived her Bachelor of Science in Biology in 2018 from Baylor University in Waco, Texas. She continued her education at the University of Texas at Southwestern
Medical Center in Dallas, Texas, where she earned her Master of Physician Assistant Studies in 2021. During her time at UT Southwestern, she was awarded the National Health Service Corp Scholar- ship. Upon graduation, Destanee she then began her career as a Family Medicine Physician Assistant at CHN.’s Freeport Family Health Center. Destanee Ms. Hamilton is passionate about patient advocacy, prepreventative health, and chronic disease management. She believes keeping the patient at the center of care is essential for success. and will continue practicing in the Northern Region.
Margaret Hazelton MPAS, PA-C
Women’s and Children’s Nurse Practitioner
Physician Assistant
LOCATION: MyCHN League City
Margaret Hazelton is a board-certified pPhysician a As- sistant by the National Commission on Certification of Physician Assistants. She is currently licensed to practice in the state of Texas. Margaret received her Bachelor of Science in Biology in 2018 from the Xavier University of Louisiana in New Orleans, LA. She took a year off to gain healthcare experience by becoming an Emergency Medicine Medical Scribe. After a year, Ms. Hazelton continued her education at the University of Texas at Southwestern Medical Center, earning her Master of Physician
Assistant Studies in 2021. She then began her career as a wWomen’s hHealth provider at Community Health Network’s League City location. after graduation.
Ms. Hazelton is passionate about building patient-centered relationships that allow the patient to feel comfortable and safe with her as their provider. She believes in providing comprehensive, preventative healthcare to all while also managing chronic diseases. Hazelton has a particular interest in Women’s Health ranging from routine gynecological exams to prenatal care. She enjoys working closely with the Women’s Health team to provide quality healthcare in a compassionate and supportive environment.

Welcome to the World of Parenting!
Newborns Are Delightful and Tiring
• Newborns may sleep only a few hours at a time.
• A newborn’s ability to hear, see, smell, and feel grows every day.
• Parents can help crying babies calm down by making them feel warm, close, and comfortable —just like it was in the womb.

• Since all parents can get upset from crying babies, it’s important to know when and how to ask for help.
• Friends and family can share the delight and the work of caring for newborns.
Your baby is finally here. Congratulations!
Baby’s Sleep and Mother’s Rest
Newborns usually sleep 16 to 17 hours a day, but they may sleep for only a couple of hours at a time.
• Many babies wake up every 2 to 4 hours, day or night.
• New mothers need plenty of rest after childbirth to get their strength and energy back.
• Mother and baby can take a nap at the same time.
• As the new father supports mom during her recovery, he can enjoy getting to know this new addition to the family!
INFORMATION FOR MOMS
Becoming a parent brings big changes to your life, more than you might have imagined!
You May Feel Tired Much of The Time
Your body is recovering from pregnancy and childbirth. At times, you may wonder if you will be able to make it through the first month. This is common and normal. Let family and friends help with meals, shopping, cleaning, and if you have other children, take care of them. Don’t entertain visitors as well!


You May Have Wild Mood Swings
As your body begins to adjust, you may go from great highs to hopeless lows. This is common during the first weeks after giving birth, but please let people know if you feel down or overwhelmed. Your feelings deserve attention and support from your family, friends, and doctors. If you think you need help, ask for it. Taking care of your emotional and physical health also helps your baby.
You May Feel Lonely
Some of your links to family and friends will get stronger, while others may weaken. Some people will understand what you are going through, and others won’t. Your baby needs and will demand much of your attention, time, and energy. If you are a mom who also works outside of the home, chances are you are not seeing friends from work at this time. Try reaching out to family and friends or find other new mothers who live near you.
INFORMATION FOR DADS
It’s A New Life for You
Your role as a father will bring about some big changes in your life. The physical, emotional, and financial demands of being a dad can cause stress. You also may feel a little left out during the first few weeks since much of the attention is on your new baby and the mom. By becoming actively involved with your new baby, feelings of stress and being left out will decrease. You will begin to:
• Enjoy the pleasure of being a dad
• Strengthen your relationship with your baby’s mother
• Contribute to the well-being of your baby
Ways For You to Be Involved
Your baby already knows who you are from hearing your voice before birth.
• As you hold your baby in your arms, enjoy the feeling of your baby cuddling up to you.
• Have fun as you spend time talking to your new baby
• If you have older children, they will need your support now while their mother is tired and focused on the new baby.
WHEN YOUR BABY CRIES A LOT
Sometimes, we just don’t know why babies are crying! So, what can you do? Think about what it was like when your baby was in the womb and try to create a similar experience.
• Calmly hold your baby close to your shoulder or chest. Inside the womb, it was warm and cozy.
• Swaddle (wrap) your baby in a blanket.
• Quietly sing or talk to your baby, softly play calm music. Voices heard through the womb were very comforting.
• Gently rock your baby or go for a quiet walk. Before birth, your baby was used to floating quietly.
There will be a few times when babies will continue to cry until either sleep finally arrives or they become quiet, yet alert. Comforting babies when they cry does not spoil them. In fact, many babies learn how to calm themselves just by knowing that someone will calm them. Sometimes, babies will continue to fuss after their parents have tried everything! They are crying because they have had all the excitement they can handle now. This is when it’s best to quietly hold your baby, or put your baby in a safe place, like the crib, and wait until all is calm.
Crying Babies Upset Parents
All parents get upset when their baby cries. With all this crying, try to stay patient. Your baby can sense when you are upset or tense. After trying all the many ways that usually calm your baby, it’s ok to let your baby cry. It’s ok to place your baby, face up, in the crib to calm down. It’s ok to let your baby cry sometimes and give yourself time to calm 59

down. Do something that you enjoy and find calming. Have a cup of tea or coffee, listen to music, call a friend or spouse, read, or meditate. These feelings of stress are natural and will pass.
If your baby’s crying is getting to be too much, and it does get to this point for many parents, reach out for help. Talk with a friend or relative who has been through this or call your MyPedi Care provider.
Stages of Childhood Development NEWBORN
After the delivery of a child, families are beaming with joy and excitement to start caring for their newborn. Unfortunately, the build-up of the birth can lead many to expect joy without recognizing the stress behind caring for the baby. Although there is immense joy when raising a newborn, there is a lot of development for the baby during these first 3 months. While these developments are signs of a healthy child, they could potentially stress parents out if they are unprepared for what to expect while raising a newborn.
Developments to expect: Motor Skills
The newborn’s movement right out of the womb may be a little wobbly and jerky. Soon after being born, however, your baby will have more control over its movements. They will lift their head and chest while lying down on their stomachs, reach out for a toy and grasp it, or stretch and kick their legs.


Hearing
The first months leaving the womb is when a newborn is sensitive to noise levels. Expect your baby to begin to respond to you and your voice with a smile or a gurgle. They will also start to notice external sounds and look towards them.
Vision
The baby will focus on your face, especially the eyes while breastfeeding. At 1 month, the baby will begin to look at bold colors and patterns. Babies develop much more eye coordination by two months and can track distant objects. Soon, the baby will begin to recognize familiar objects and people at a distance.
Communication
By 2 months, the baby might coo and repeat vowel sounds when you talk or gently play together. With these developments, parents can play an important role as their newborns adjust to their new settings.
Parents can:
Hold the baby
Touch can help their newborn develop feelings of safety, security, and love. Let your baby grasp your little finger and touch your face.
Speak freely
Simple conversations are essential as they lay the groundwork for the language. Sing, read stories out loud, ask questions and respond to your baby’s coos and gurgles. Remember that your tone of voice also lets the baby learn about emotions.
Change positions
Hold your baby facing outward and place your baby on their tummy to play, with close supervision.

Entertain your child with colorful toys or interesting noises to encourage your baby to lift their head. It is important, however, to keep these sessions short as many newborns get fussy or frustrated on their tummies.
Respond quickly to tears
Crying spells peak, for most newborns at about 6 weeks after birth and then gradually declines. Regardless of their crying, respond quickly without worrying about spoiling your baby with too much attention.
It is good to note that these developments don’t happen on a specific timeline. Each child is vastly different and can mature at different rates. While the rates may differ among children, it is good to take note of any delays in your child’s growth. You should consult your MyPedi
Care provider if you notice these red flags after 3 months:
• Hasn’t shown improvement in head control
• Doesn’t respond to loud sounds
• Doesn’t smile at people or the sound of your voice
• Doesn’t follow moving objects with their eyes
• Doesn’t notice their hands
• Doesn’t grasp and hold objects.
Remember that every child is different in their growth. However, it is important to trust your instincts as a parent most of the time. This can help prevent future problems from developing.
INFANTS
After the first 3 months, newborns have begun to get used to living in the outside world. These 3 months also help parents adjust to their new lives with their baby. After those initial 3 months, children are considered infants (0-1 years). The new label entails new developmental milestones parents can expect to happen for their child. While these milestones are common among infants, every child’s timeline to reach them is different and should not alarm parents if they aren’t achieved immediately.
Following the newborn stage, babies will begin to develop critical cognitive skills. One of the most exciting for parents is language learning: babies will listen and understand the names of people or things. Also, they may increase the amount they babble or, if you’re lucky, even respond by saying “ma-ma” and “da-da.” With language learning, babies will also begin to

develop bonds of love and trust with their parents as they begin recognizing them through sight and sound. Here are some positive parenting tips to help your baby develop during this time:
Talk to your baby
Answer when they make sounds by repeating them and adding words.
Read to your baby
Spend time cuddling and holding your baby—this will help them feel cared for and secured.
Play with your baby
The best time to play with babies is when they are alert and relaxed. Be sure to give them breaks if they get fussy or are tired.
Take care of yourself
Physically, mentally, and emotionally. Being a parent isn’t easy. Taking breaks and care of yourself allows you to be a positive and loving parent!
With the new developments, it is essential to keep your baby safe:
Never shake your baby when holding them. At this stage, babies still have weak neck muscles that can support their neck—if shaken, you can damage their brain or cause death.
Put your baby to sleep on their back to prevent sudden infant death syndrome.
Protect your child from secondhand smoke by not letting people smoke in your home. To ensure your child is healthy and developing correctly, be sure to take them to their well-baby visits. These visits typically happen when a child is: 1, 2, 4, 6, and 9 months old.
TODDLERS
After the first year, babies develop from infants to toddlers. The two years of toddlerhood, from 1 to 3 years of age, are filled with tremendous amounts of growth. Before, they were dependent infants, but now they are toddlers who desire more and more
independence. While it sounds nice, many parents call these times the terrible twos as babies become more and more defiant. With all this growth and maybe even headaches, it is essential to know the developmental milestones your child will be undergoing as they make their way to childhood. During these years, toddlers are moving around more and becoming aware of their surroundings. As a result, toddlers become increasingly curious about their surroundings, object, and other people. Because of the child’s growing curiosity, these years are often called the “terrible twos” as many toddlers become much more defiant of their parents. In these “terrible twos”, however, toddlers develop their cognitive abilities to form simple phrases and sentences. Additionally, toddlers will be able to follow simple directions, imitate the actions of others, and express a wide range of emotions.
Tips to ensure your child’s safety:
· Do NOT leave your child near or around water without supervision. Drowning is the leading cause of injury and death among this age group.
· Keep sharp objects and kitchen appliances out of reach of your toddler.
· Ensure your toddler is sitting when eating and chewing their food thoroughly to prevent choking.
· Encourage your toddler to not put pencils or crayons in their mouth.
· Keep your child’s care seat rear facing as long as possible.
 These safety tips consider children’s growing curiosity and help keep them safe as they 63
These safety tips consider children’s growing curiosity and help keep them safe as they 63
explore. It is also essential, moreover, to keep toddlers healthy. To keep children healthy, toddlers must get plenty of sleep. The CDC recommends 11-14 hours per 24 hours (including naps) as well as letting your toddlers be as active as possible. Not only does it make them sleep, but it is also a vital part of letting them grow strong! Also, it is important to limit screen time as much as possible. The biggest issue parents may be facing, however, is their toddler being picky eaters. Pickiness is a common trait among this age group. Parents are encouraged to be patient and offer their children small bites of food before turning it away. While these toddler years may be difficult for parents, we must recognize the tremendous amount of growth occurring during these years. Toddlers take their first steps, say their first sentence, and become more curious in two years. Although it may be stressful sometimes, these years are vital in making sure your child is developing into a healthy child.
PRESCHOOLERS
In the last legs of a baby’s road to childhood, ages 3-5 years old are considered the pre- schoolers. Here a child begins to reach milestones that extend beyond the family dynamic. While many of them have begun to develop more practical skills such as communication and motor skills, there are still important physical and emotional developments occurring that parents should be aware of.
As a part of early childhood, a preschooler’s world is beginning to expand beyond their household. They will carry their desire for independence from the ter- rible twos into these years. Now, preschoolers will be interested in adults and children outside the family. They will continue to explore and ask more questions. The interactions preschoolers have with their family, and other people will begin to shape their personality and ways of thinking. They will also refine their motor skills and coordination enough to start riding a tricycle, using safety scissors, helping dress themselves, and playing with other children.
With so much social growth occurring, parents should continue the same habits they did during the first years of their child’s life. They should continue to read to their child and let them help with simple chores Preschoolers should also be encouraged to make friends and make simple decisions such as choosing their snack.
While these small interactions help develop your child, there are some extra steps to ensure your child is safe and healthy during their preschool years:

·Teach your child how to be safe around strangers
· Eat meals with your child whenever possible and limit the amount of sugar, fats, and salt
· Keep the television outside of the bedroom while limiting screen time to an hour a day
· Make sure they’re getting enough sleep (10-13 hours per 24-hour day)
· Tell your child to stay out of traffic and not to run/play in the street
With all the information and independence, these years can seem overwhelming. Although changes are occurring at a rapid pace, these are the years where parents can see their children begin to grow into their own. Parents will be given a chance to see their children personality and watch them make friends. With this milestone in childhood, preschoolers are developing important social and emotional skills to become functional children in the world.
PARENT’S GUIDE TO SAFE SLEEP
Did You Know?
• About one in five sudden infant death syndrome (SIDS) deaths occur while an infant is in the care of someone other than a parent. Many of these deaths occur when babies who are used to sleeping on their backs at home are then placed to sleep on their tummies by another caregiver. We call this “unaccustomed tummy sleeping.”
• Unaccustomed tummy sleeping increases the risk of SIDS. Babies who are used to sleeping on their backs and are placed to sleep on their tummies are 18 times more likely to die from SIDS.
• You can reduce your baby’s risk of dying from SIDS by talking to those who care for your baby, including childcare providers, babysitters, family, and friends, about placing your baby to sleep on his back during naps and at night.

Who Is At Risk For SIDS?
• SIDS is the leading cause of death for infants between 1 month and 12 months of age.
• SIDS is most common among infants that are 1-4 months old. However, babies can die from SIDS until they are 1 year old.
• Know The Truth…SIDS Is Not Caused By:
• Immunizations
• Vomiting or choking
What Can I Do Before My Baby Is Born To Reduce The Risk of SIDS?
Take care of yourself during pregnancy and after the birth of your baby. During pregnancy, before you even give birth, you can reduce the risk of your baby dying from SIDS! Don’t smoke or expose yourself to others’ smoke while you are pregnant and after the baby is born. Alcohol and drug use can also increase your baby’s risk for SIDS. Be sure to visit a physician for regular prenatal checkups to reduce your risk of having a low birth weight or premature baby.
MORE WAYS TO PROTECT YOUR BABY
Do your best to follow the guidelines on these pages. This way, you will know that you are doing all that you can to keep your baby healthy and safe.
• Breastfeed your baby. Experts recommend that mothers feed their children human milk for as long and as much as possible, and for at least the first 6 months of life, if possible.
• It is important for your baby to be up to date on her immunizations and well-baby check- ups.
Where Is The Safest Place For My Baby To Sleep?
The safest place for your baby to sleep is in the room where you sleep, but not in your bed. Place the baby’s crib or bassinet near your bed (within arm’s reach). This makes it easier to breastfeed and bond with your baby. The crib or bassinet should be free from toys, soft bedding, blankets, and pillows.
Talk about safe sleep practices with everyone who cares for your baby! When looking for someone to take care of your baby, including a childcare provider, a family member, or a friend, make sure that you talk with this person about safe sleep practices. If a caregiver does not know the best safe sleep practices, respectfully try to teach the caregiver what you have learned about safe sleep practices and the importance of following these rules when caring for infants. Before leaving your baby with anyone, be sure that person agrees that the safe sleep practices explained in this brochure will always be followed.
What Can I Do Reduce My Baby’s Risk
Follow these easy and free steps to help you reduce your baby’s risk of dying from SIDS: Safe Sleep Practices
• Always place babies to sleep on their backs during naps and at nighttime. Because babies sleeping on their sides are more likely to roll onto their stomachs accidentally. The side position is just as dangerous as the stomach position.
• Avoid letting the baby get too hot. The baby could be too hot if you notice sweating, damp hair, flushed cheeks, heat rash, and rapid breathing. Dress the baby lightly for sleep. Set the room temperature in a range that is comfortable for a lightly clothed adult.
• Consider using a pacifier at nap time and bedtime. The pacifier should not have cords or clips that might be a strangulation risk.
• Safe Sleep Environment
• Place your baby on a firm mattress covered by a fitted sheet that meets current safety standards. For more about crib safety standards, visit the Consumer Product Safety Commission’s Web site at http://www.cpsc.gov.
• Place the crib in an area that is always smoke-free.
• Don’t place babies to sleep on adult beds, chairs, sofas, waterbeds, pillows, or cushions.
• Toys and other soft bedding, including fluffy blankets, comforters, pillows, stuffed animals, bumper pads, and wedges, should not be placed in the crib with the baby. Loose bedding, such as sheets and blankets, should not be used as these items can impair the infant’s ability to breathe if they are close to his face. Sleep clothing, such as sleepers, sleep sacks, and wearable blankets, are better alternatives to blankets.
Is It Ever Safe To Have Babies On Their Tummies?
Yes! You should talk to your childcare provider about making tummy time a part of your baby’s daily activities. Your baby needs plenty of tummy time while supervised and awake to help build strong neck and shoulder muscles. Remember to make sure that your baby has tummy time at home with you.

Tummy To Play and Back To Sleep
• Place babies to sleep on their backs to reduce the risk of SIDS. Side sleeping is not as safe as back sleeping and is not advised. Babies sleep comfortably on their backs, and no special equipment or extra money is needed.
• “Tummy time” is playtime when infants are awake and placed on their tummies while someone is watching them. Have tummy time to allow babies to develop normally.
What Can I Do to Help Spread The Word About Back To Sleep?
• Be aware of safe sleep practices and how they can be made a part of our everyday lives.
• When shopping in stores with crib displays that show heavy quilts, pillows, and stuffed animals, talk to the manager about safe sleep and ask them not to display cribs in this way.
• Monitor the media. When you see an ad or a picture in the paper that shows a baby sleeping on her tummy, write a letter to the editor.
• If you know teenagers who take care of babies, talk with them. They may need help with following the proper safe sleep practices.
• Set a good example – realize that you may not have slept on your back as a baby, but we now know that this is the safest way for babies to sleep. When placing babies to sleep, be sure to always place them on their backs.
If you have questions about the health and safety of your child, talk to your child’s pediatrician. If you have questions about safe sleep practices in the early education and childcare settings, please contact Healthy Child Care America at the American Academy of Pediatrics at childcare@aap.org.
Infants Are Amazing
HOW DO INFANTS LEARN?
In the very beginning, it may seem that your baby does nothing but eat, sleep, cry, and fill her diapers. But your infant is learning too. She can see and hear what is happening around her and can communicate her needs and interests to others. Parents can help their babies learn by playing with them.
Infants have the ability to see faces and objects of different shapes, sizes, and colors. They can tell the difference between the voices of their parents and others. We’re surprised when they mold their bodies into our arms or shoulders. We marvel at how they came into the world able to suck, communicate certain needs by crying, and sometimes calm down on their own. Most infants can do all of these things as soon as they are born.
You Are Your Baby’s First Teacher
First experiences have a significant effect on the future. That’s why you are so important to your baby’s growth and development. The growth of your baby’s brain is affected by the care and experiences you provide. Loving attention helps new brain cells connect in ways that help infants:
• Feel secure and confident.
• Make sense of new ideas and information.
• Grow healthy bodies.
Things To Watch For
Your baby has a different style or personality from all other babies. It’s fun to get to know your baby’s likes, needs, and abilities. Find out how your baby relates to other people and situations.
• Some infants like more activity, some like less.
• Some infants are louder when they laugh or cry, some are quieter by nature. All infants let us know when they have had enough. Some ways your baby may tell you that it’s time for a nap are:
• Avoids making eye contact
• Becomes sleepy or fussy, may cry a lot
• Coughs or spits
Take Care of Yourself
Children grow faster in their first year than at any other time in their lives. This will take a lot of your time and energy. You must be healthy and happy to give your child the best start possible. When you feel good about yourself, you will be helping your baby feel happy and secure. This is why you need to find the time to take care of yourself. Let people know when you need support or help. After you are rested, you will have more energy, and you will be able to have more fun with your baby.
Others Who Care For Your Baby
Developing a close bond with parents and family members is important. It helps infants form positive relationships with others.
• By letting other people hold and talk with your baby when you are around, your baby learns how to relate to other people.
• When you cannot be with your baby, it is best if the same few trusted people are the caregivers. Your baby will learn to expect and enjoy their company and kindness.
• If you decide to leave your baby with a relative, friend, or professional child care provider, make sure that the caregiver and surroundings adequately provide a healthy, safe and comforting environment. This way, you will feel confident about the safe and loving care being provided.
A Strong Start for Life
Infants spend the first year learning to feel secure about being loved. Love, —expressed in the ways mentioned here and in many other ways by you, —will give your child the physical strength to fight illness, the emotional strength to feel confident, and the ability to learn new things.
How Often and How Much Should Your Baby Eat?
Breastfed babies generally eat more frequently than those who are formula fed. Newborns usually nurse on their mothers’ breasts every 2 to 3 hours; as they age, the time between feedings will increase as the capacity of their stomachs becomes larger. By contrast, formula-fed newborns will start out by eating approximately every 3 to 4 hours during the first few weeks of life.
When you hold your baby to feed her a bottle, watch for cues that she is full instead of using the clock as a guide. It’s more important that you are attentive to clues or signals from your baby that indicate she’s hungry. These are called hunger cues. When she wants to eat, she may become more alert, put her hands or fingers on or in her mouth, make sucking motions, stick out her tongue, smack her lips, kick, squirm, or begin rooting (moving her jaw and mouth or head in search of your breast). If she starts crying, this is usually a late signal that she wants to eat.
Whether breastfeeding or formula feeding, most parents worry about whether their babies are getting enough to eat. Because babies suck not only for hunger but also for comfort, this can be hard to know at first. Even when babies no longer act hungry, some parents worry about whether all of their nutritional needs are being met.

Again, don’t panic. Your baby will let you know when she’s had enough or wants more. In most cases, she’ll consume about 90% of the available breast milk during the first 10 minutes of feeding on each breast. Then she might move away from the breast or simply doze off. Among the many advantages of breastfeeding is that it tends to be cued or on-demand feeding, meaning that, in a sense, your baby will take charge of her own feedings. If you watch your baby’s responses, you should be able to figure out when she’s full. She may turn her head or give other signals that she’s no longer interested in eating. The formula-fed baby will also let you know when she’s had enough. You might notice her becoming distracted while drinking from the bottle, or she might start fidgeting or turning her head. She may close her mouth tightly. As your baby gets a little older and her eye-to-hand coordination
gets better, she might try to knock the bottle or spoon out of your grip.
On the other hand, if your baby finishes a bottle and starts smacking her lips or begins to cry, she probably wants more. On average, by the end of the first month, she should be taking in at least 4 ounces of formula per feeding. At 6 months of age, she’ll consume 6 to 8 ounces per feeding.
You can also rely on your baby’s diapers to give you clues on whether she’s getting enough to eat. In the first month of your newborn’s life, she should wet her diaper 6 or more times a day and have 3 to 4 (often more) bowel movements each day. Your baby should also appear satisfied for a couple of hours after each feeding if she’s consuming adequate amounts of food.
What if your baby almost always seems hungry—or if she doesn’t appear to have the appetite you think she should?
If that’s the case, talk to your pediatrician. The doctor will be able to answer specific ques- tions or respond to your concerns about whether your baby is getting enough nourishment and is growing normally. During each office visit, the pediatrician is already keeping track of your baby’s weight gain and monitoring whether her weight is continuing to increase steadi- ly. For instance,
• From months 1 through 4 of life, your baby should gain about 1 1⁄2 to 2 pounds each month while growing about 1 to 1 1⁄2 inches.
• Between 4 and 7 months of age, she’ll add another 1 to 1 1⁄2 pounds per month and grow about 2 to 3 inches in length.
• By 8 months, the average boy will weigh between 14 1⁄2 and 17 1⁄2 pounds, while girls will probably weigh about a half-pound less.
• At 1 year of age, the typical child weighs about 3 times her birth weight.
• Breastfed babies tend to be chubbier than formula-fed babies during the first 4 to 6 months of life. Then they usually become leaner than formula-fed babies by 9 months to 1 year of age.
THE PERIOD OF PURPLE CRYING, EXPLAINED It Has Nothing to Do With Your Baby’s Coloration.
A baby’s first cries after birth likely warmed your heart. They were, after all, the first sounds you heard your infant make.
Fast-forward a few weeks, and the crying might not be as reassuring. In fact, it may be downright difficult to endure some days and could leave you wondering if the constant sobbing and screaming is normal, —or even healthy. The good news is that your baby is probably perfectly fine. The bad news? The crying may get worse before it gets better. At around two months of age, babies start crying so frequently that experts have dubbed this stage the “Period of PURPLE Crying” and developed a whole program around the concept. Some more good news: Understanding what the PURPLE program is all about can help the whole family get through this teary time.
WHAT DOES PURPLE STAND FOR?
The name didn’t come about because some babies turn the shade of a plum after extreme bouts of wailing. PURPLE is an acronym developed to help parents better anticipate and understand this stage of life where babies cry around the clock (or at least it feels that way to exhausted moms and dads). The letters stand for:
• Peak of crying. Baby is wailing a lot. The most crying may happen in baby’s second month, with less crying in months three to five.
• Unexpected. There’s no rhyme or reason as to why baby starts and stops crying.
• Resists soothing. Rocking, singing, bouncing, swaying—you may not be able to do anything—we repeat, anything—to help soothe baby and ease the sobbing.
• Pain-like face. Baby may appear to be in pain when crying, even when he’s not.
• Long lasting. The crying can seem never ending. In fact, baby may cry for five hours a day or more.
• Evening. The late afternoon and evening may be when baby cries the most.
WHY WAS THE PERIOD OF PURPLE CRYING PROGRAM CREATED?
When experts looked at how much babies cry during the first months of life, they found that peak periods of crying correlated with the increased incidences of the shaken baby syndrome (SBS), brain injury, and head trauma caused by forcibly shaking an infant. Experts believe the reason for the correlation is that some parents find themselves unable to manage 71
the endless crying and shake their babies in an attempt to get them to stop. Tragically, the complications associated with SBS can be deadly.
The PURPLE program was developed to help parents manage during this high-crying stage and reduce the cases of SBS, says Julie Noble, program director for the Period of PURPLE Crying at the National Center on Shaken Baby Syndrome. “It was a priority that the program takes a child developmental approach that aimed to support caregivers and increase their understanding of normal infant crying.”
Trained health professionals, such as nurses and pediatricians, deliver the program to new parents and caregivers in medical settings. Parents typically leave the hospital with a booklet and DVD that further explains the PURPLE period, and they can also go to PurpleCrying. info to learn more.
Some preliminary research shows that the program’s implementation has reduced SBS-related hospitalizations. One survey found that 91 percent of parents agree that the PURPLE program helped them feel less frustrated when the baby was crying.

WHY DO BABIES CRY SO MUCH DURING THE PURPLE PERIOD?
“Doctors actually aren’t entirely sure why crying increases during this period, but they have found that humans aren’t the only ones that go through this stage. Other breasted species also whimper, mewl and bleat more during the first months of life”, says Adam Zolotor, MD, an associate professor of family medicine at the University of North Carolina. Experts do know that increased crying is normal during this stage of life. That said, if the crying seems excessive or if you have a gut feeling something more serious is the matter, see a doctor. “Babies have a limited way of communicating, and crying is a way to let us know something’s wrong, whether the child has a fever, is constipated, or has an intolerance to formula,” Zolotor says.
WHAT CAN YOU DO TO SOOTHE A CRYING BABY?
If your infant is wailing, first make sure there’s not an obvious reason for the cries, like a wet diaper that needs changing or a hungry tummy. Then, try these techniques to help ease the tears:
• Swaddle baby. Use a big, thin blanket to securely wrap up your infant. You can ask a nurse or your pediatrician to show you how to swaddle correctly if you’re not sure how to do it.
• Aid digestion. Hold baby so she’s on her left side and gently rub her back to help her 72
digest herfood.
• Rock or sway. Hold baby in your arms and walk, sit or stand while making these calming motions, which may remind babies of how they felt in the womb.
• Use noise. Calming sounds, such as white noise machines or the whir of a fan, can soothe crying babies.
• Try a pacifier. The act of sucking can help soothe many babies. If none of these methods work, don’t panic. According to the PURPLE program, about 10 percent of the time, there’s nothing that can be done to ease a baby’s crying—and that’s okay.
“As a parent, we feel like we always have to do something, but sometimes there is just nothing you can do, and it’s best to walk away, especially if you’re getting frustrated or angry,” says Christine Baker, the program coordinator of the Period of PURPLE Crying at Seattle Children’s Hospital. If you find you’re feeling too exhausted or stressed to deal with your newborn’s cries, ask a partner, family member, or friend to hold the baby while you take a break.
If you’re watching the baby by yourself, don’t feel guilty about walking away. Place your infant in a safe space, such as a crib or bassinet, and go into the next room until you’ve calmed down. Remember, while the crying may seem endless now, there is a light at the end of this tear-filled tunnel, and your little one will soon grow out of this sobbing stage
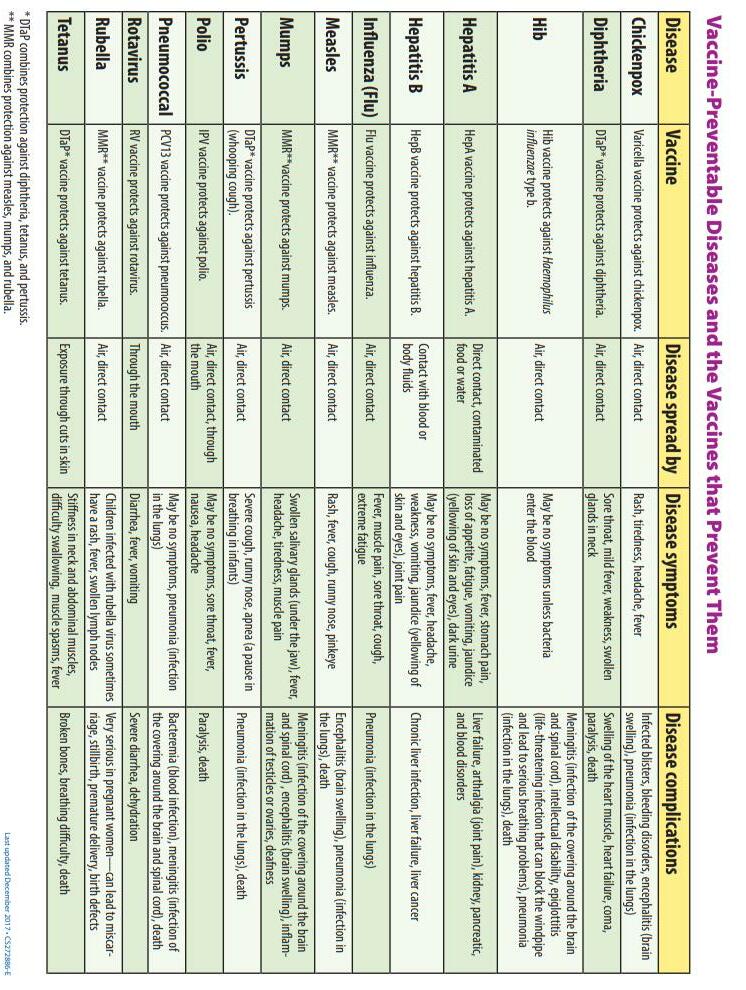

IS YOUR MOUTH READY FOR PREGNANCY?
- Have you been to the dentist in the past year?
A dental check-up is as important as seeing your prenatal doctor. Germs that cause cavities in your mouth can be passed to your baby.
- Are your gums tender or do they bleed when you brush?
Pregnancy can increase the way your gums react to germs in the mouth. Brush along the gum line and floss daily.
- Do any of your teeth feel loose?
Loose teeth can be caused by gum disease and should be treated by a dentist or dental hygienist.
- Do you have morning sickness?
Stomach acid can damage teeth. Rinse your mouth with a mixture of water and baking soda. Wait 1 hour before brushing and use toothpaste with fluoride.

- Do you feel pain in your mouth when you eat or drink?
Pain can be a sign of problems in your mouth.
It is safe to have your teeth treated when you are pregnant
CAVITY FREE STARTS AT PREGNANCY
If your mouth is not clean and healthy, germs that cause cavities can be passed to your baby
- Brush with fluoride toothpaste every morning and night.
- Floss your teeth once a day
- Have your teeth cleaned and cavities filled before your baby is born.
- After your baby is born, avoid sharing saliva:
- Do not taste your baby’s food with the same spoon your baby uses during feeding.
- Do not clean your baby’s pacifier with your mouth.
Healthy Mouth for Mom
Healthy Mouth for Baby

• Breastfeeding and breast milk are the best choices for baby

- When possible, feed your baby only breast milk for the first 6 months
- Before other foods are added, breast milk alone does not cause cavities
• Start other healthy foods at 6 months and continue to breastfeed for 12 months or as long as mother and child wish
- Once other foods including formula, are started, teeth can get cavities quickly
- Limit how often sweet foods are given
• Start good habits early by cleaning your baby’s mouth to keep it healthy
- Wipe your baby’s gums with a clean cloth after morning and evening feeding
- When teeth first come in, brush them in the morning and before bedtime witha small soft toothbrush and tiny smear of toothpaste containing fluoride
Take your baby for a dental visit by age one
Sugar liquids rot your sleeping baby’s teeth. Here are some ideas to protect your baby’s teeth at bedtime.
• Hold your baby while bottle feeding.
• Wipe the teeth of gums when finished.
• Put your baby to sleep by rocking, cuddling, or singing.
• Put your baby to sleep without a bottle or sippy cup.
Baby Bottles + Bedtime = Cavities
LIFT THE LIP
Check your child’s mouth and teeth once a month so that problems can be found when they are small.
1. POSITION - Place your child’s head in your lap or in your arms so you can see the teeth and all parts of the mouth.
2. CLEAN - Remove food from teeth and gums using a clean, soft cloth or soft toothbrush.
3. LIFT - Use your fingers to lift your child’s lips to look for white or brown spots on any of the teeth - signs of tooth decay. If you see any color changes, contact a dentist.
4. LOOK INSIDE - Look at all mouth areas for unusual colors, cuts, or sores. If you see any of these, contact a dentist.
MY CHILD’S FIRST DENTAL VISIT
Having dental visits twice a year beginning by age one helps my child:
- Grow up healthy
- Be a better learner
- Be pain-free
- Have fewer dental emergencies
- Lower dental costs for my family if I see white or brown spots on my child’s teeth, I can ask a dental professional to check.
The first dental visit for my child might include:
- Asking about my family’s dental experiences, eating habits, and toothbrushing routine
- Looking at my baby’s teeth and mouth
- Painting fluoride on teeth to make them strong
- Working with me to create a plan for keeping my baby’s teeth cavity-free
To find a dentist for my child, I can:
- Ask my child’s doctor
- Ask my local health department, childcare provider, Head Start program, or another parent
- Check out these websites: (insurekidsnow.gove, aapd.org, mouthhealthy.org)
TOOTHPASTE TIPS
- Use toothpaste with fluoride
- Keep Toothpaste out of child’s hands, treat it like medicine
- Help your child brush
- Best to spit but not rinse after brushing
- Use the right amount of toothpaste:
1st Tooth-Age 2
(slight smear)
Age 3-5
(small pea-size amount)
Age 6 and Over
(pea-size amount)
CHOOSE THE RIGHT CONTAINER
NURSING - Breast milk is best
‘I like being close to mom”
Baby Bottle - newborn to 1 year
- Breast milk is best - Water with fluoride
- Formula - No juice or other sweet drinks
“I want to be held when I drink my bottle”
Baby Cup - ages 6 months to 2 years
- Milk - Water with fluoride
- No more than 1/2 cup of 100% fruit juice a day
“I sit up, I use cup”
Kid Cup - ages 2 years and up
- Milk at meals
- Water with fluoride between meals
- No more than 1/2 cup of 100% fruit juice a day
“I sit down when I drink”
Travel Mug - for traveling only
- Water with fluoride - No valves
-No juice or other sweet drinks
“I save my travel mug for car trips”
Fruit Juice Has The Same Amount of Sugar as Soda Pop!
Amount of Sugar in 1/2 cup:
Soda: Colas - 3 teaspoons Mountain Dew - 4 teaspoons
Juice: Apple - 3 teaspoons Grape - 5 teaspoons
Milk: Regular - 11/2 teaspoons Chocolate - 4 teaspoons
BRUSHING UP FOR HEALTHY TEETH
Toothbrushing is as easy as 1, 2, 3.
MAKE IT FUN
- Use your child’s favorite toothbrush and toothpaste
- Sing or tell a story
- Brush to the count of 5 in each area
MAKE IT SIMPLE
- Find a comfortable spot to brush
- Brush your teeth to show how it is done
- Guide your child’s hand to brush all side of each tooth
MAKE IT EVERYDAY
- Start brushing as soon as the first tooth comes in



- Brush each morning and after the last food at night
- Create a routine by making a calendar of each tooth
Brushing morning and night. Keep your child’s smile bright.
Cavities can cause pain. Your child may use actions instead of words to show they are hurting. You can find out by watching how your child behaves.


- Friendly
- Sleeps well
- Healthy
- Eager to learn new things
- Eats crunchy fruits and vegetables
- Shy, withdrawn
- Tired and cranky
- Sick often
- Slow to learn new things
- Avoid crunchy fruits and vegetables
Cavities are an infection.
If not treated, they can make your child sick. Take your child to a dentist for treatment.
TASTY TREATS FOR TEETH


Grapes of other fresh fruit

String cheese or other cheeses, whole grains
Carrot, celery, or other fresh vegetables
Sweet Treats for Special Occasions:
Choose somehting that leaves the mouth quickly.
Example: Bite size chocolate that melts away instead of a Sucker that coats teeth in sugar over a longer time.
Dried fruit snack or other sticky sweet
Cracker, chips or other starchy food

Cookies, cupcakes or other baked goods

 Cavity Free Try This:
Tooth Decay Not This:
Cavity Free Try This:
Tooth Decay Not This: