
3 minute read
A Clearer Picture
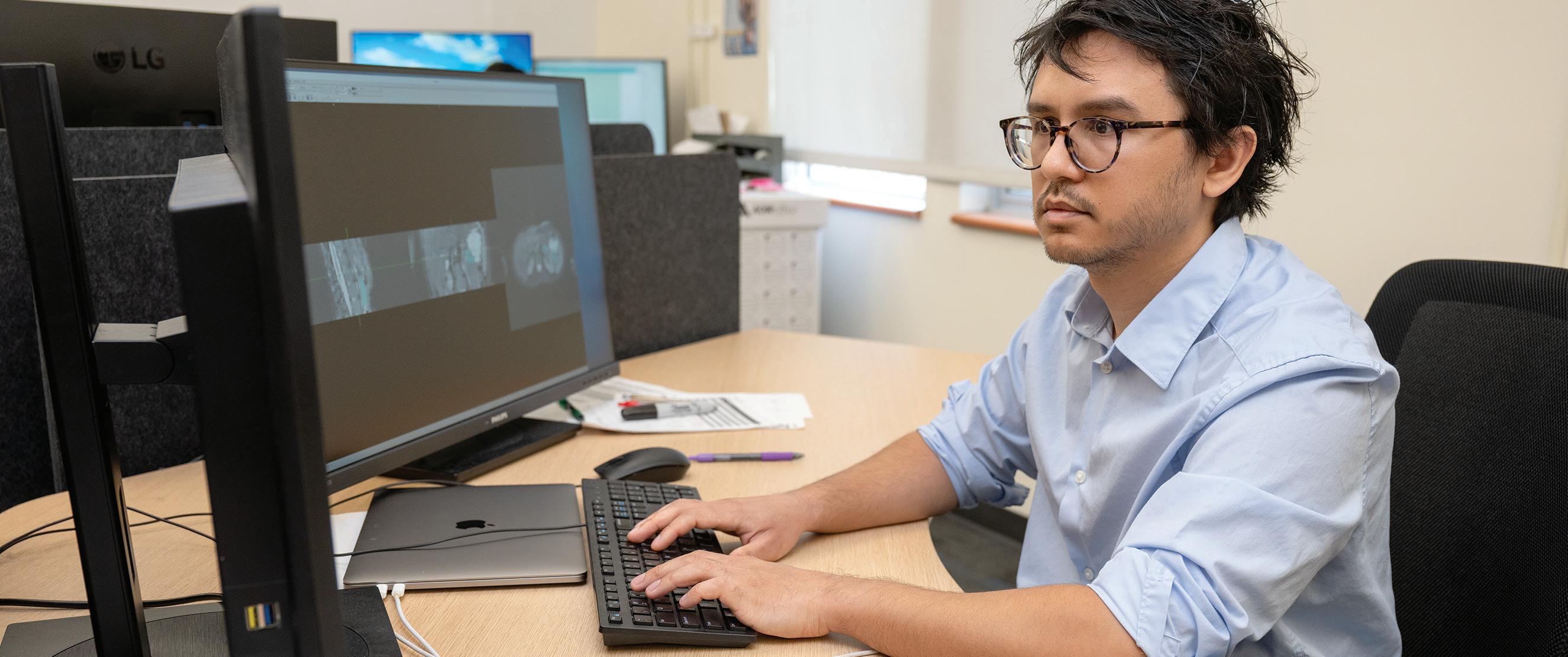
MTSU Computer Science graduate Lucas Remedios wields artificial intelligence (AI) in the fight against a silent killer
A study in Academic Radiology found that, on average, radiologists must interpret one CT or MRI image every three to four seconds to keep their workday on track. It’s a frightening pace considering patients’ lives often depend on scan readings to determine if something looks abnormal.
Help for weary-eyed radiologists has arrived in the form of artificial intelligence (AI) applications making imaging evaluation more precise and efficient, improving diagnostic accuracy. AI can’t replace an experienced radiologist’s clinical judgment; however, it can identify and flag potential abnormalities in scans, enabling human professionals to focus more on complex interpretations.
The key is harnessing mass data—billions upon billions of medical scans collected in a database—to enable AI to do its job. That’s where computer scientists like MTSU graduate Lucas Remedios (’20), currently a Ph.D. student at Vanderbilt University, enter the picture.
As a researcher at the Medical-image Analysis and Statistical Interpretation (MASI) lab at Vanderbilt, Remedios is wielding AI in health care imaging to better understand one of humanity’s most insidious diseases—diabetes.

One question is if Type 1 and Type 2 diabetes— traditionally considered completely separate buckets— really are separate, or if they would be better described as part of a spectrum or gradient of the disease.
“To that end, I’m trying to help characterize what’s happening in the phenotypes [genetic traits] of people who have Type 1 vs. Type 2 diabetes,” Remedios said. “The way I’m approaching it is by looking at abdominal medical images.”
Using anonymous digital scans taken at Vanderbilt University Medical Center, Remedios is part of a team teaching computers to make measurements of organs like livers and pancreata in a standardized, comparable way. It’s work that would take years to accomplish using traditional methods, like having graduate students individually mark up scans. By comparison, Remedios and colleagues are effectively teaching computers how to view and measure images independently and more precisely.
“We achieve a much more fine-grain way of measuring what’s happening in body composition,” he said.
At the heart of his research is the quest to determine if there is a spectrum of the disease—a Type 1 diabetes, a Type 1.5 diabetes that’s somewhere in the middle, a Type 2 diabetes, and perhaps even a Type 2B or Type 2C diabetes—not dissimilar to the way other diseases like breast cancer are diagnosed. The consequences could be life-altering. Presently, if a doctor is treating a patient like they have Type 2 diabetes when they have Type 1, they’re doing that patient a disservice, and treatment should be changed immediately.
“I think, longer-term, appreciating that there may be more than two types of diabetes, and that there’s actually a spectrum of disease, well, that could be very helpful,” Remedios said. “And let’s just say imaging can play a real role in that.”
AI is clearly at the forefront of health care innovation. Data researchers like Remedios on the cutting edge of AI use appear poised to quickly close the gap between aspiration and implementation of new, life-saving technologies.
—Drew Ruble










