
8 minute read
A Clearer Picture
MTSU Computer Science graduate Lucas Remedios wields artificial intelligence (AI) in the fight against a silent killer
Article by Drew Ruble
A study published in Academic Radiology found that, on average, radiologists must interpret one CT or MRI image every three to four seconds to keep their workday on track.
It’s a frightening pace considering patients’ lives often depend on scan readings to determine if something looks abnormal.
Help for weary-eyed radiologists has arrived in the form of artificial intelligence (AI) applications making imaging evaluation more precise and efficient, improving diagnostic accuracy.
Radiology Today recently quoted Bibb Allen, president of the International Society of Radiology, stating that “AI-lite” is already being used extensively in the field in numerous ways, including “computeraided detection for cancer” and “auto-segmentation of organs in 3-D post-processing.”
According to Bibb, AI can’t replace an experienced radiologist’s clinical judgement; but it can identify and flag potential abnormalities in scans, enabling human professionals to focus more on complex interpretations.
Said another way, AI won’t replace the radiologist. But the radiologist who uses AI will replace the radiologist who doesn’t.
The key is harnessing mass data—billions upon billions of medical scans collected in a common database—to enable AI to do its job.
That’s where computer scientists like MTSU graduate Lucas Remedios (’20), currently a Ph.D. student at Vanderbilt University, enter the picture.
As a researcher at the Medical-image Analysis and Statistical Interpretation (MASI) lab at Vanderbilt, Remedios is wielding AI in health care imaging to better understand one of humanity’s most insidious diseases—diabetes.

A DEEPER DIVE
Type 1 diabetes starts in childhood, wherein a person’s immune system kills the insulinproducing cells in their pancreas (thus, the need to supply it with external insulin). Type 2 diabetes is acquired later in life.
At least, that’s the currently accepted medical understanding.
“But there are still big, open questions in the diabetes space,” Remedios said. “I used to hear about diseases like diabetes and think, ‘Oh, they know all about that.’ And the medical field does know a lot about diabetes. But there’s a tremendous amount of unanswered questions as well.”
One question is if Type 1 and Type 2 diabetes— traditionally considered completely separate buckets—really are separate, or if they would be better described as part of a spectrum or gradient of the disease.
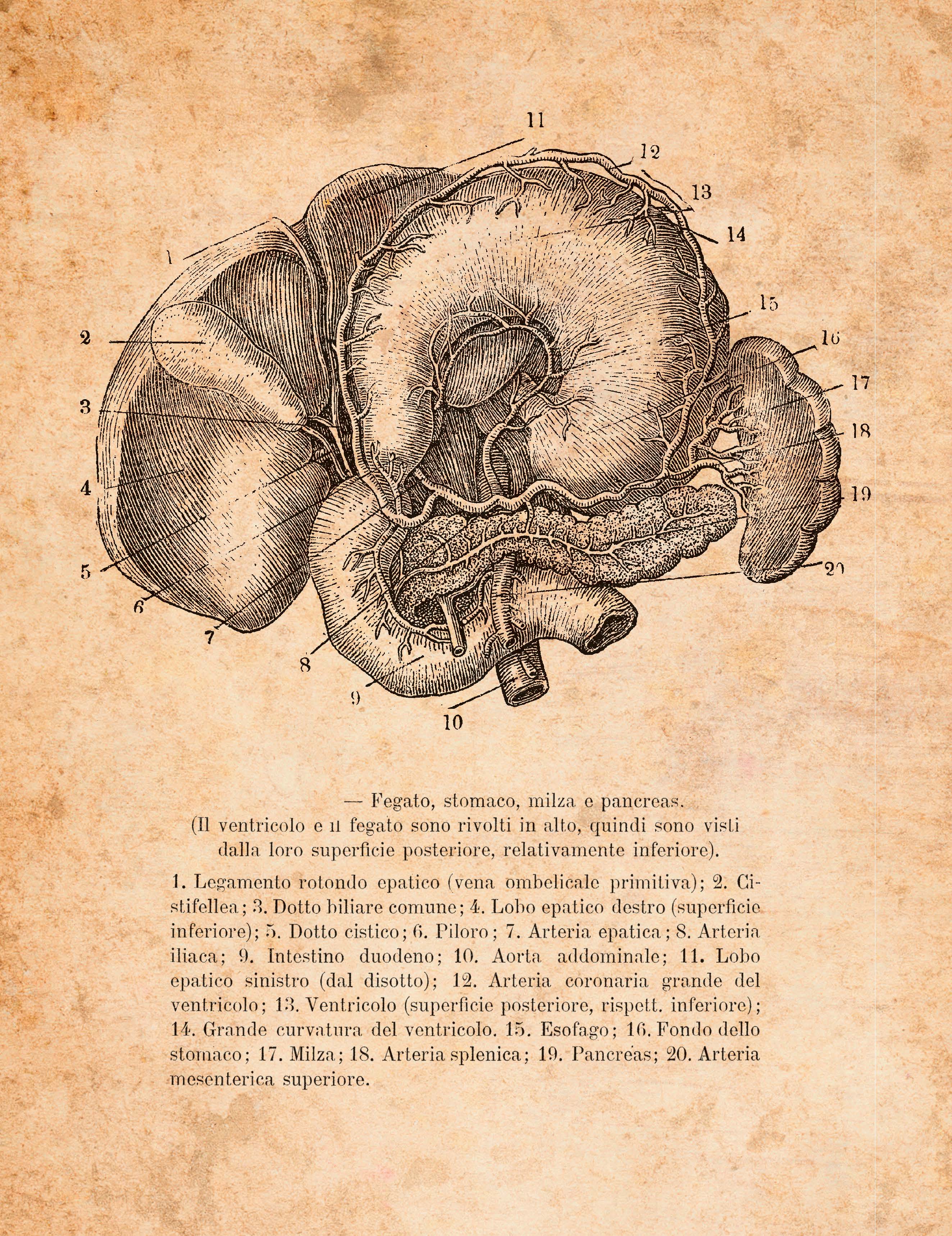
“To that end, I’m trying to help characterize what’s happening in the phenotypes [genetic traits] of people who have Type 1 versus Type 2 diabetes,” Remedios explained. “And the way I’m approaching it is by looking at abdominal medical images.”
Using anonymous digital scans taken at Vanderbilt University Medical Center, Remedios is part of a team teaching computers to make measurements of organs like livers and pancreata in a standardized, comparable way. It’s work that would take years to accomplish using traditional methods, like having graduate students individually mark up scans. By comparison, Remedios and colleagues are effectively teaching computers how to view and measure images independently and more precisely.

“I’m essentially using AI to extract segmentations,” Remedios said. “It’s a way of saying, ‘Here’s exactly where the liver is, the pancreas, the spleen, the kidneys, and also visceral fat around organs, or subcutaneous fat, the pinchable fat, and the skeletal muscle in the abdomen. It’s like a fancy measuring tape—better than when you go to the doctor and they weigh you, look at your height, and calculate a BMI [body mass index]. We achieve a much more finegrain way of measuring what’s happening in body composition.”
Remedios can extract a specific phenotype from the shape information, the volume of the organs, the interplay between the organs, and the fat in the muscle. The mapping of those organs then helps determine what a normal situation would be, versus an abnormal one. That leads to the ability to investigate what is happening in the phenotypes of Type 1 versus Type 2 diabetics and determine if there is crossover, or not.
Some diabetics do have features of the disease that look like both Type 1 and Type 2. Meaning there may indeed be a spectrum of the disease—a Type 1 diabetes, a Type 1.5 diabetes that’s somewhere in the middle, a Type 2 diabetes, and perhaps even a Type 2B or Type 2C diabetes—not dissimilar to the way other diseases like breast cancer are diagnosed. The consequences of better understanding this possible segmentation could be life-altering. Presently, if a doctor is treating a patient like they have Type 2 diabetes when in fact they have Type 1, they’re doing that patient a disservice, and treatment should be changed immediately.
ONE QUESTION IS IF TYPE 1 AND TYPE 2 DIABETES—TRADITIONALLY CONSIDERED COMPLETELY SEPARATE BUCKETS—REALLY ARE SEPARATE.
“I think, longer-term, appreciating that there may be more than two types of diabetes, and that there’s actually a spectrum of disease, well, that could be very helpful,” Remedios said. “And let’s just say imaging can play a real role in that.”
AI imaging could also lead to an earlier diagnosis of diabetes—or even forecast its likelihood of developing.

That’s the opinion of Jack Virostko, a mentor to Remedios who focuses on diabetes research at the University of Texas health care system. Virostko earned his Ph.D. in Biomedical Engineering at Vanderbilt, did his postdoctoral work there, became a junior faculty member, then left for Texas in 2015. But he still does collaborations on projects with Vanderbilt, including on the imaging side and the diabetes side, and he serves on Remedios’ Ph.D. thesis committee.
According to Virostko, modern medicine diagnoses diabetes pretty late in the game.
“Generally speaking, by the time that you go into your doctor’s office and they do an A1C measurement, a blood test that measures the average blood sugar/glucose, and your A1C is elevated, they say, ‘Alright, you have diabetes.’ And you say, ‘OK, so I guess I just got diabetes.’ And they say, ‘No, we don’t know for sure when you got it. But this has been developing over years, if not decades.’ ”
The imaging measurements Virostko and fellow researchers like Remedios are working on could help doctors identify that a patient is on a pathway to getting diabetes much earlier in the process than those standard blood measurements currently in use.
“We start by building a big database of what a normal human body looks like inside from head to toe, and then we start to look for discrepancies,” he said. “Now a doctor can look for things that are a little bit different from the typical. And perhaps say, ‘Let’s have a radiologist look at this and see if they see anything that’s off.’ . . . And maybe we identify this years and years before they’re traditionally diagnosed.”
REMEDIOS IS PART OF A TEAM TEACHING COMPUTERS TO MAKE MEASUREMENTS OF ORGANS LIKE LIVERS AND PANCREASES IN A STANDARDIZED, COMPARABLE WAY.
A WORLDWIDE CURE
Remedios’ work pulls exclusively from millions of anonymous medical images at one hospital— Vanderbilt. Imagine the medical understanding that could be achieved once AI has access to interpret billions of scans from around the world, identifying suspicious areas that may not be obvious to the human eye. Doctors could much more easily correlate that data to identify patterns that are predictive of diabetes, or any other disease.
“The hope for us, specifically, is that we are able to characterize something new about these classes of diabetes,” Remedios said. “If I’m lucky, there’s a big discovery to be made. But if not, I’m working alongside thousands of other scientists around the world trying to chunk away little by little to build the knowledge so that we can eventually make big leaps forward.”
Virostko said one key to such medical discovery is inspiring more researchers like Remedios with a computer science background to get involved in health care projects.
IMAGINE THE MEDICAL UNDERSTANDING THAT COULD BE ACHIEVED ONCE AI HAS ACCESS TO INTERPRET BILLIONS OF SCANS FROM AROUND THE WORLD.

“Lucas is really smart, really driven, and really grasps new things well,” Virostko said. “Some people who have a high level of technical training like Lucas tend to become a little bit siloed. But I think Lucas does a great job of learning new things and being curious about things.
“People like that can be really successful because they have the technical chops, but then they also have a broad curiosity and a broad ability to learn new things. And they realize they can apply their skill set to real-life problems.”
AI is clearly at the forefront of health care innovation. Data researchers like Remedios on the cutting edge of AI use appear poised to quickly close the gap between aspiration and implementation of new, lifesaving technologies.

