KEEPING THE FAITH: DIAGNOSED WITH BRCA1 AT 23
BRIGIDA MACK
Former TV anchor and current motivational speaker shares her story of hope, faith and love after suffering from multiple miscarriages

PARENTING A CHILD WITH SPECIAL NEEDS
DIABETES IN THE
AFRICAN AMERICAN COMMUNITY: HOW CAN WE MAKE A DIFFERENCE?
We work hard to make navigating your health care easier. Because having the right health insurance means not having to think about it. Helping you give every moment the attention it deserves.
Focus on what matters to you. We’ll help with the rest. That’s the Benefit of Blue®.
 BlueCross BlueShield of South Carolina is an independent licensee of the Blue Cross Blue Shield Association.
BlueCross BlueShield of South Carolina is an independent licensee of the Blue Cross Blue Shield Association.
CONTENTS
10 Keeping the Faith: Diagnosed with BRCA1 at 23
COVER STORIES
22 Diabetes in the African American community: How can we make a difference?
38 Suffering from multiple miscarriages, Brigida Mack shares her story of hope, faith and love
72 Parenting a child with special needs

14 How to improve your self-care?
20 Colletta Orr shares symptoms, diagnosis and treatment for ovarian cancer
26 Men’s Health Corner: Understanding the symptoms, treatments and preventive measures of prostate cancer
30 50 and thriving: Living with vitiligo
34 Alexandria Smith shares the challenges of living with bipolar disorder

44 Bias in healthcare equity is harming Black women

54 Moving Beyond Pain and Heartbreak to Happiness and Love: Adrianna Hannon shares the ups and downs on her journey to motherhood

66 Keeping your diagnosis a secret: “He who conceals his disease cannot expect to be cured."
70 Sugar, sugar, sugar…the dangers of consuming too much
76 The dangers of having visceral or belly fat
We
Signature Programs:
B.S. Speech Pathology

B.S. Biology
B.S. Nuclear Engineering
























































































































B.S. Accounting
B.S. Business Administration
B.S. Agribusiness
B.S. Social Work
B.S. Criminal Justice
Graduate Programs: Ed.D.

MOTIVATATION…
In this edition, we delve into the stories of individuals who have bravely faced and overcome health challenges. We hope these life experiences will offer motivation, encouragement and immense inspiration to all those navigating similar paths. This issue covers a myriad of topics including infertility, ovarian cancer, diabetes, bipolar disorder and much more.
In the realm of infertility, women shed light on their complex journey to motherhood. They share the obstacles they’ve endured ranging from the pain of miscarriages to their struggles against polycystic ovary syndrome and symptoms of endometriosis. Their stories are a powerful reminder that when the human spirit is unwavering, the road to motherhood is indeed possible.
A renowned cancer specialist shares valuable insights on ovarian cancer as we hope to raise awareness and empower women to recognize signs at the outset, and what one can do to lead a proactive approach toward pre-empting the disease through early diagnosis or available treatment.
We are also highlighting the alarming rise of diabetes, especially within the African American community. Our article on diabetes demonstrates the need for better education, prevention and strategies to manage this growing health epidemic.
These are not just stories, but a way of providing solace, hope, encouragement and a reminder that you are not alone on your journey. Many people have fought and won these battles in different parts of the world. If others can win these battles, you can too. I hope you enjoy this Fall 2023 issue as we covered topics that were requested by our readers. Much love to all of you!
Warm regards,

 Teesa Brunson, Ed.D. Editor Motivated Woman
Teesa Brunson, Ed.D. Editor Motivated Woman

PrEP IS FOR WOMEN
What is PrEP?
PrEP stands for Pre-Exposure Prophylaxis. It is a safe and effective daily pill or injectable taken to prevent HIV and can lower your chances of contracting HIV.

Why should women take PrEP?
Women account for 1 in 5 new HIV diagnosis. As of 2019, 18% of newly diagnosed with HIV were women. 227,000 US women are eligible for PrEP but only 10% are taking it.



When does PrEP start working?

Oral PrEP is effective after 20 days for those who have vaginal sex.

Can I take PrEP while pregnant?

Yes. PrEP is safe to take while you are pregnant/ breastfeeding.
Can I take PrEP while on birth control?
Yes. PrEP is safe and does not interfere with your birth control.
Does PrEP protect against other STDs?
No. PrEP does not protect against other STDs. Condoms are the only way to protect against other STDs when sexually active.
How do I pay for PrEP?
PrEP is covered by most insurance companies and Medicaid. Co-pay cards and drug assistance programs for the uninsured are available.
MOTIVATED WOMAN


FALL 2023
Editor in Chief Teesa Brunson
Editorial Manager Delandous Haynes
Contributing Writers Megan Freeman, Bambi Gaddist, Arleatha Jeffrey, LaToya Johnson, Kimberely McClain, Terrianna Mccullough, Elizabeth Mosely-Hawkins, Gwynth Nelson, Anika Thomas, Carmen Thompson, Margaret Williams, April Woodyard Photography Mauricio Richardson, Moonking Moments, Charmarie Photography
Motivated Woman, a biannual magazine, is a leading resource for women’s health illnesses, such as autoimmune disorder, cancer, diabetes, heart disease and obesity. With a primary focus on infertility, Motivated Woman encourages women to share their remarkable stories of overcoming health challenges they faced to inspire and motivate other women who may be battling those same illnesses.

www.motivatedwoman.org info@motivatedwoman.org
Motivated Woman Board of Directors
Jason Barber
Colletta Brabham-Orr
Phillip Ford
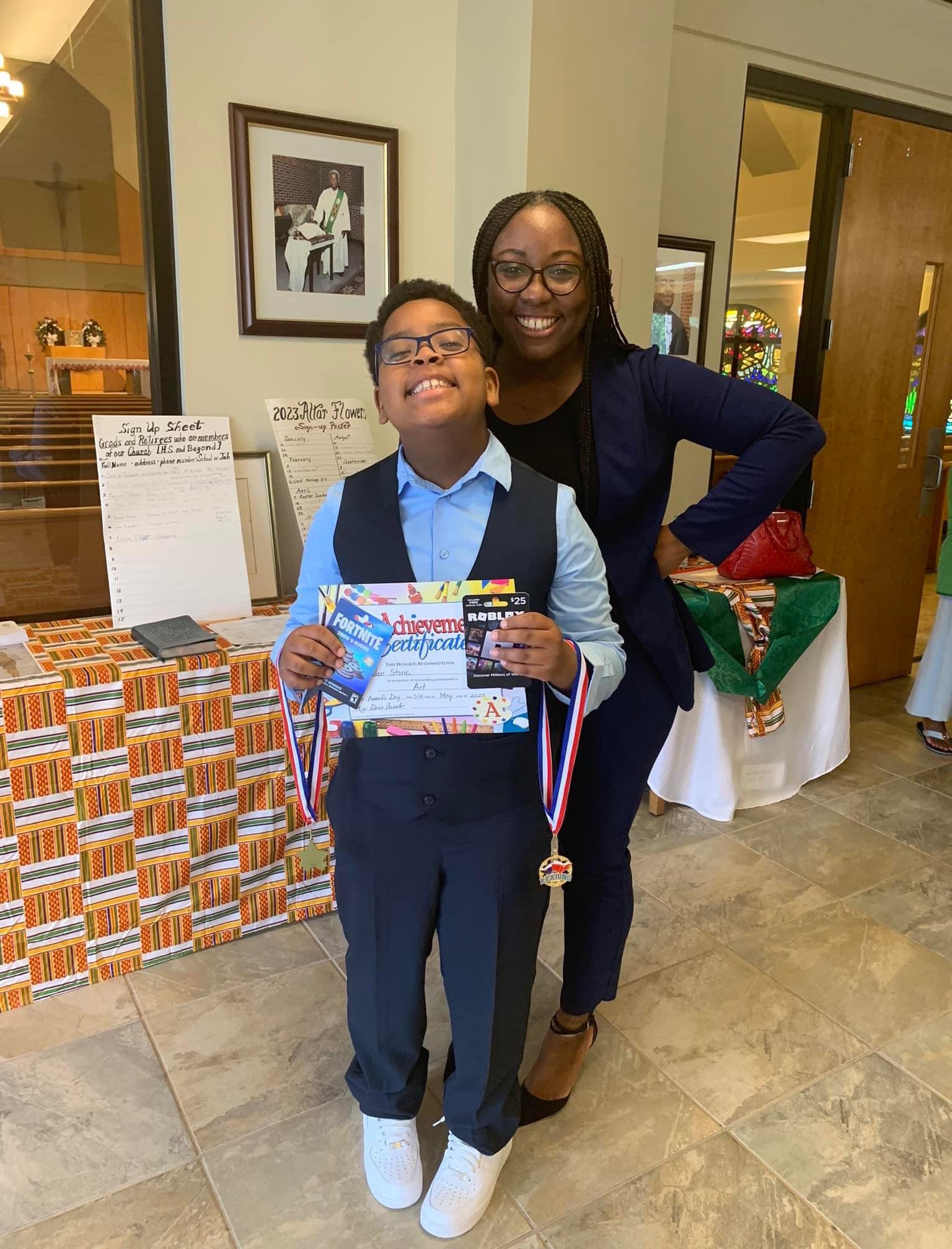
Shavonne Gaskin
Nikki Georgia
Tiffany Goodson
Adrian Scott
Tia Robinson
Anika Thomas
Please visit www.motivatedwoman.org to complete our Magazine Readership Survey.
LOVE Y O U R S E L F FIRST.
As women, we have a tendency to put our own needs last. But there are times that can jeopardize your health and your future. That’s why NoDrama.org offers eight birth control options, all free or low-cost. With virtual appointments, live chat and prescriptions by mail, it’s never been easier to give your life the priority it deserves.

KEEPING THE FAITH: DIAGNOSED WITH BRCA1 AT 23
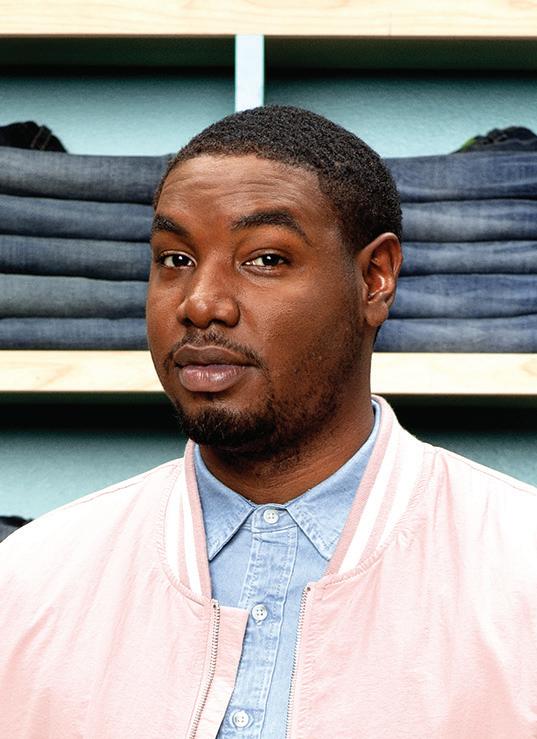
Anika Thomas, 32, shares her personal journey of trying to have another child after testing positive for BRCA1, which is a breast cancer gene that increases the risk of developing breast and ovarian cancer.
 By Anika Thomas
Anika Thomas
By Anika Thomas
Anika Thomas
So, if you want to have more babies, I strongly suggest you have them quickly and back-to-back as the medical recommendation is that we remove your breast and ovaries by age 30 to prevent cancer.
BRCA1 POSITIVE.
Imarinated on the words, almost as if I were taste-testing them or trying them on for size. I knew my mother had breast cancer at a young age. I knew that genetic history could play a part in cancer but until that moment, roughly five months pregnant, I hadn’t truly thought about what this meant.
My doctor explained I had a deleterious genetic mutation that put me at an 80 percent higher risk of breast and ovarian cancer. If one in eight women were diagnosed with breast cancer and one in 78 women were diagnosed with ovarian cancer, I had an 80 percent higher risk than most women. My mind spun. I was never good with numbers, but I knew the odds were not in my favor.
The physician snapped me back to attention stating, “So, if you want to have more babies, I strongly suggest you have them quickly and back-to-back as the medical recommendation is that we remove your breast and ovaries by age 30 to prevent cancer.”
I felt hot, queasy and overwhelmed. I was only 23 years old. I wasn’t married and quite frankly, I had not planned for the baby I was carrying at that moment, let alone having thought of more babies. The nurse gave me information about a genetic counselor, and
then I left. It never dawned on me that I would be hit with my own genetic surprise during routine testing for my son. I got into my car, and I cried because what else was I supposed to do?
I did the one thing I knew to do; I turned to Google. My research taught me BRCA was an acronym for BReast CAncer and the designations of 1 and 2 represented gene 1 or gene 2. These genes produce proteins that help repair damaged DNA. I was confused because I thought the genetic mutation was what caused the damage, but I continued researching. I learned that everyone has two copies of each of these genes, generously provided by each parent.
Immediately, it made sense to me that I inherited the gene from my mother. I felt bad because I knew that she would carry guilt for passing that on to me, even if it was unbeknownst to her.
I was surprised to learn that people who are BRCA 1 positive are not only at a higher risk for breast and ovarian cancer but also several additional types of cancer. This had to be a sick joke, but it wasn’t.
When I found out that people who have inherited a harmful variant in BRCA1 and BRCA2 also tend to develop cancer at younger ages than people who do not have such a variant, I instantly remembered how concerned my physicians were that my mother had been affected by breast cancer in
her 30s, which is relatively young. This was my reality.
I delivered a healthy ninepound eight-ounce baby boy in August of 2014 and every visit to my obstetrician-gynecologist (OBGYN) following that I was asked about my decisions for the next steps and more children. I was 23, and my only choice in my viewpoint was to try to prove I could be a mom to this little boy who deserved the world. Nothing extended past that.
If I tried a little harder, my decisions were aimed toward accomplishing graduate school, gainful employment, a career in my field, and hopefully, eventually marriage with the right person but none of that mattered to my physicians. In 2016, I began getting

Tossing my phone across the bed, I cried, sobbing actually. Here I am, roughly 10 years after accidentally conceiving my first child, I have struggled to intentionally conceive another. The very thing I have been waiting to do, the thing the doctors have been telling me to do, I couldn’t.
mammograms and ultrasounds annually. This was a hassle because I was 25 and my insurance, despite a genetic mutation, fought not to cover me at every turn. In 2018, I began getting a standard mammogram and a 3D mammogram because I was so young that my breast tissue was too dense to be properly screened by a standard imaging machine. I was 25 years old, receiving mammograms twice a year, ultrasounds once a year and a cancer cloud hanging over my head. I adapted to my new normal, understanding that this, albeit expensive and at times overwhelming, was the best way to practice preventative care.
In 2018, my paternal aunt was diagnosed with breast cancer. She remembered my genetic mutation and reached out to me for more information regarding my diagnosis. I shared with her my documents only to have my understanding of what I was navigating dismantled when I found out that my mutation came from my paternal genetics,
despite my father not having breast cancer.
Learning that my mother’s cancer was more than likely connected to her military service rocked my world. I felt like the research I had done was a moot point. When I learned that my paternal grandfather had five female family members, all BRCA 1 positive, multiple of which had breast cancer, some of which died from it, I cried again. I felt defeated. I felt like the chip I carried on my
shoulder since 2014 became a boulder that was chasing me and would inevitably run me over.
I met my now husband in 2019 and married in 2020. I was excited because my life felt like it was coming together. My son was happy and healthy, and my husband and I were ready to grow our family. We were ready, but my body wasn’t. As fate would have it, our family was at a standstill.
Over two years after ending my birth control, I did my usual
on social media, scroll, scroll, like, scroll, scroll, comment, “Congrats!” scroll, scroll, like. Pregnancy announcement after announcement and immense overwhelming sorrow overcame me. Tossing my phone across the bed, I cried, sobbing actually. Here I am, roughly 10 years after accidentally conceiving my first child, I have struggled to intentionally conceive another. The very thing I have been waiting to do, the thing the doctors have been telling me to do, I couldn’t.
Every time I go to the doctor, I am reminded that the medical
recommendation has not changed in the last nine years, and it is still encouraged that I undergo a double mastectomy as well as remove my ovaries to prevent cancer. That’s it. That’s my only option. It is isolating and suffocating to smile and cheer for your friends as they reach life’s milestones. It feels negligent to not take preventative measures watching your mother fight for her life, twice. It feels delusional to risk it all knowing your paternal family has succumbed to such an illness, caused by a genetic mutation that you carry. It feels ungrateful to long
for children when you have a happy and healthy child who many would swap places with you to have in a heartbeat. It feels unfair to have to make such decisions.
So, what do you do when life and time don’t align? Do you gut yourself and eliminate your chances of experiencing the physical manifestation of your love with your person? Do you risk cancer? Something that takes the life and light of so many. Do you question God? You rely on your faith, and you advocate for yourself. I found a new primary care physician who listens and helps me navigate my health. She worked to find me an OBGYN who was well-versed in supporting people with similar medical histories as mine. I continue my preventative care regimen of mammograms and ultrasounds, and I remain hopeful that one day that ultrasound will surprise me in the best way possible.
HOW TO IMPROVE YOUR SELF-CARE?
By Arleatha JeffreySelf-care has been defined as any activity that we do deliberately to take care of our mental, emotional and physical growth. It can include activities that replenish and nourish us to stay balanced in body, mind and spirit, as well as keeping us fit and resilient in times of physical or emotional stress.

Self-care can take various forms and depend on individual preferences, but the common goal is to indulge in activities that promote relaxation, mindfulness and emotional well-being. Here are some examples of how to incorporate self-care in your daily routine:
• Prioritize sleep. Sleep is an
essential activity that most people neglect. Getting enough sleep promotes good mental and physical health and allows the body to rest and recharge. Some activities can promote good sleep hygiene such as cutting off electronic devices before bedtime, avoiding caffeine and establishing a consistent sleep routine.
• Exercise regularly. Physical activity is an excellent way to relieve stress, improve your mood and boost cognitive functioning. Regular exercising such as walking, yoga, dancing or weightlifting can all be essential activities that can keep you motivated and engaged.
• Practice mindfulness meditation. Meditation is a
powerful practice that helps individuals find inner peace and calmness. It involves focusing on the present moment and paying attention to your thoughts, emotions and sensations without judgment. Mindfulness meditation offers many benefits that are designed to reduce stress, anxiety and depression.

These are just a few examples of how to maintain self-care for good mental, physical and emotional health. Remember, consistency is the key and focus on what works best for you. Incorporating self-care activities into your daily routine can improve your overall well-being while providing a sense of balance and fulfillment.
Arleatha Jeffrey is a licensed clinical social worker and owner of A Better You Coaching and Counseling, a virtual therapy service that services North Carolina, South Carolina, Virginia and Maryland. More information can be found at www.abetteryoupllc.com.
START TALKING BEFORE SHE HEADS OFF TO SCHOOL.

It’s never too early to have a conversation about alcohol and other drugs.

The sooner you talk about the dangers of underage drinking and substance use, the greater chance you have of influencing your child’s decisions about using alcohol and other drugs. For tips on how—and when—to begin the conversation, visit www.underagedrinking.samhsa.gov


Endometriosis aka “endo”
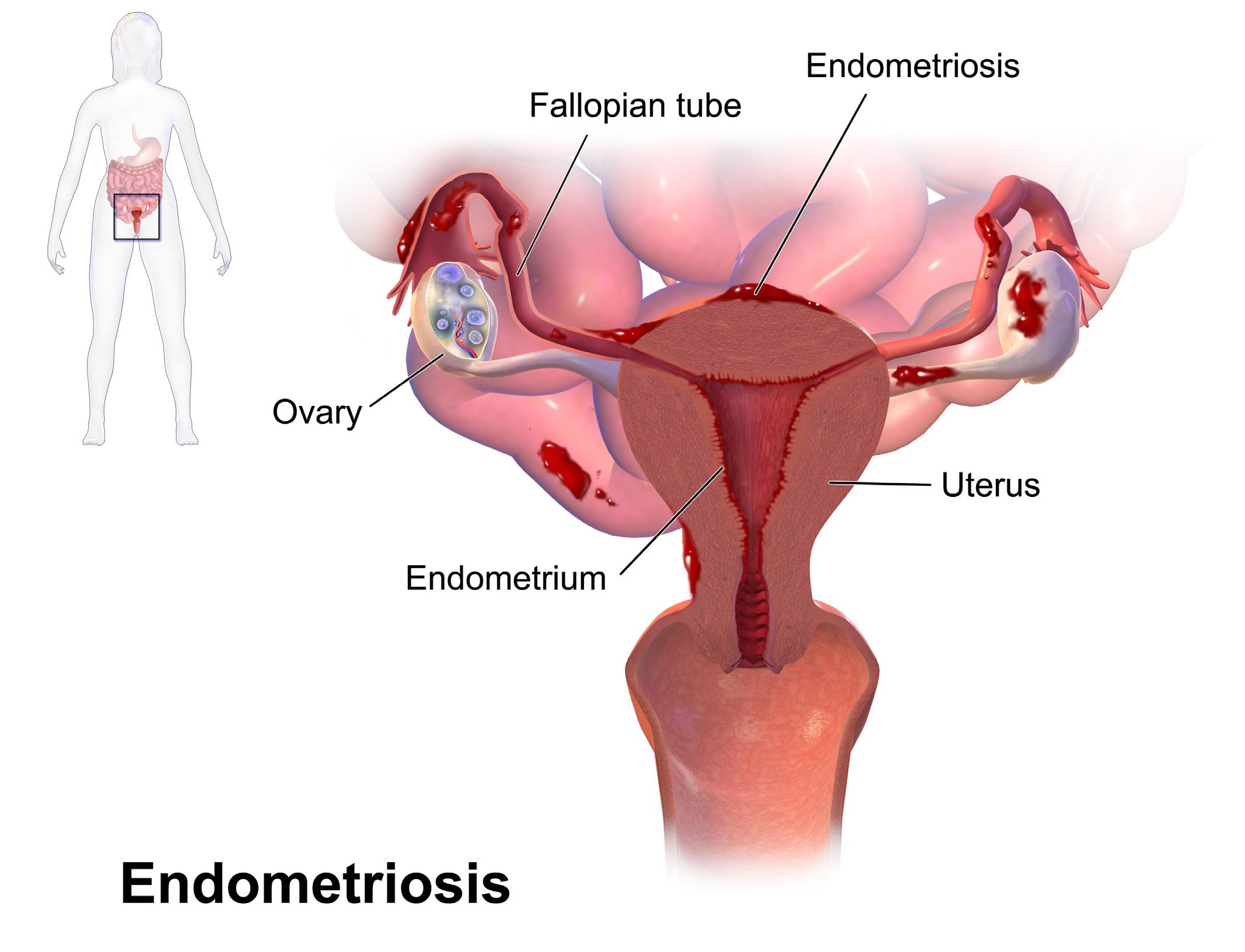
– What is it? Who does it affect? Why Me? These are questions that clouded my thoughts during the journey of experiencing the debilitating pain of endometriosis. Numerous women have dealt with this pain
LIVING WITH ENDOMETRIOSIS: THE STRUGGLES AND TRIUMPHS
By Kimberely McClainsilently for many years. The reason for the silence ranges from thinking, “I have bad periods” to “I only have to deal with this pain for seven days during my cycle.” The reason for my silence was that I had no idea what was going on with me and knew nothing about this disorder when I
was diagnosed at the age of 28. I was only a month away from graduating from my dietetic internship in 2003 when I experienced a deep, dull, debilitating pain in my pelvic area while in the bathroom at the Medical College of Georgia. My emotions were all over the place
as I stood bent over in a stall for three to five minutes not knowing what was happening to me. Once I was able to gain my composure, still with lingering pain, I made my way to my sister’s house and told her that I needed to be seen by a doctor immediately. The next day, I was seen by a gynecologist and was diagnosed with endometriosis – which changed my life forever.
WHAT IS IT?
Endometriosis is a disorder where cells that are similar to the lining of the uterus or endometrium grow outside of the uterus. These cells usually affect the pelvic tissue and can envelop the ovaries and fallopian tubes. Endometriosis can affect nearby organs such as the bladder, bowel and settle behind the uterus as well.
The common symptoms of endometriosis range from excruciating pain with urination or bowel movements during a menstrual period, heavy and irregular periods, spotting and bleeding between menstrual cycles, fatigue and low energy, pain during sex, infertility and diarrhea and constipation during a menstrual period. These symptoms are the common symptoms that women experience; however, symptoms can range from minimal to no symptoms to women experiencing pain from this

If you have never had children or have a menstrual cycle that lasts more than seven days, the chances are more likely for the development of endometriosis.
The common symptoms of endometriosis range from excruciating pain with urination or bowel movements during a menstrual period, heavy and irregular periods, spotting and bleeding between menstrual cycles, fatigue and low energy, pain during sex, infertility and diarrhea and constipation during a menstrual period.
disorder daily.
According to the article, “Management of Endometriosis,” by the American College of Obstetricians and Gynecologists, diagnosis of this disorder is usually done through the most common practice of laparoscopic surgery. Laparoscopic surgery consists of the following characteristics:
• The surgeon uses an instrument to inflate the abdomen slightly with a harmless gas.
• After making a small cut in the abdomen, the surgeon uses a small viewing instrument with a light, called a laparoscope, to look at the reproductive organs, intestines and other surfaces to see if there is any endometriosis.
• If patches of tissue are present, the surgeon examines them to determine whether they are endometriosis and, if so, at what stage they might be.
• In some cases, the surgeon will also do a biopsy, which involves taking a small tissue sample and studying it under a microscope to confirm the diagnosis.
• The most common surgery is a laparoscopy, but sometimes a laparotomy, a surgical procedure involving a larger incision, is used to make a diagnosis.
Healthcare providers may also use imaging methods to produce a “picture” of the inside of the body. Imaging allows them to locate larger endometriosis areas such as nodules or cysts. The two most common imaging tests are

ultrasound, which uses sound waves to make the picture, and magnetic resonance imaging (MRI), which uses magnets and radio waves to make the picture. These types of imaging do not help diagnose small lesions or adhesions as stated in the previous article mentioned by the American College of Obstetricians and Gynecologists.
Treatment of endometriosis depends on the severity of this disorder. Pain medication and hormone therapy are two of the most common treatments for endometriosis. However, hormone therapy must be strategically employed due to estrogen being one of the culprits to fertilize and ignite the growth of endometriosis. Another option is surgery. There are three common surgeries that are performed, and they are a laparoscopy, laparotomy and hysterectomy, according to Medical News Today.
WHO IS AFFECTED?
Endometriosis affects girls and women who have a menstrual cycle. This disorder is much more common in women in their 30s and 40s. If you have never had children or have a menstrual cycle that lasts more than seven days, the chances are more likely for the development of endometriosis. Research has shown significantly lower rates of endometriosis diagnosis in Black (10.1 percent), Hispanic (7.4 percent), and Asian Pacific (11.3 percent) women compared to Whites (17 percent), according
to the article, “Revisiting the impact of race/ethnicity in endometriosis,” published in the National Library of Medicine. Many African American women have suffered in silence for years not knowing that the pain during their cycles was not just a “bad cycle,” it was a condition that could have been addressed years prior through proper medical care and awareness.
LIVING THROUGH ENDOMETRIOSIS

My journey with endo has been an emotional, physical and mental roller coaster. For me, using medication hormone therapy and as a last resort, a hysterectomy, was my mode of treatment; however, the latter did not successfully remove all the endometriosis. I have since changed doctors and continue to suffer through monthly pain. The pain is not as bad, but it is still very noticeable. I encourage all women to be their own advocates. If something does not seem normal with your body, take the time to visit a physician for an examination. I also encourage getting second opinions – don’t just go with the first answer that you are given. My husband and I are thankful that through this experience, we were blessed to conceive and deliver two of the four children that were gifted to us. We continue to deal with the ups and downs of this condition and remain optimistic! My hope is that my story will encourage others and let them know that they’re not alone. There are support
groups for this disorder such as the Endometriosis Association, HealthyWomen and Endo Warriors. Reach out. Thanks for allowing me to tell my story!
Kimberely McClain is a registered and licensed dietitian in the state of South Carolina. She has practiced as a clinical and outpatient dietician for more than 19 years and is the owner and operator of Dynamic Nutrition Solutions, LLC, which provides one-on-one and group counseling sessions on nutrition related topics. Currently, she is an assistant professor in the Department of Family and Consumer Sciences - Nutrition and Food Management program at South Carolina State University.
COLLETTA ORR SHARES SYMPTOMS, DIAGNOSIS AND TREATMENT FOR OVARIAN CANCER
Colletta Orr, an award-winning research scientist, spoke to Motivated Woman on the dangers of ovarian cancer. Orr is a 2002 Voorhees University graduate with a bachelor’s degree in biology. She received a Master of Public Health degree from Capella University, and she is currently a candidate to earn a Doctorate in Public Health from Walden University.

Orr is a trained cancer research scientist with 21 years of experience in research, biology and oncology. She has held positions at Georgetown University Lombardi Cancer Center and the National Cancer Institute in Washington, D.C. She is currently a senior scientist at Merck Pharmaceuticals. Orr also serves as the chief executive officer at Colletta Orr & Associates, where she educates women about breast and ovarian cancer. She is married to Douglas Orr III, and they have one son, Douglas Orr IV. They reside in Rockville, Maryland.
MW: What made you decide to enter this career field?
CO: I became interested in this field after losing my maternal grandmother to ovarian cancer and her mother to breast cancer.
MW: What is ovarian cancer?
CO: Ovarian cancer occurs when abnormal cells in your ovaries or fallopian tubes grow and multiply out of control. Symptoms of ovarian cancer include abdominal bloating or swelling, quickly feeling full when eating, weight loss, discomfort in the pelvic area, fatigue, back pain, changes in bowel habits and a frequent need to urinate.
MW: What are the screening tests for ovarian cancer?
CO: Unfortunately, there currently are no screening tests for ovarian cancer.
MW: What are the treatments for ovarian cancer?
CO: Treatments for ovarian cancer usually involve a combination of surgery and chemotherapy.
MW: Is ovarian cancer curable?
CO: Yes, many women fully recover from ovarian cancer following surgery and/or chemotherapy. Ovarian cancers caused by stromal or germ cell tumors have high survival rates. However, epithelial carcinoma is the most common type of ovarian cancer and has lower survival rates. It also depends on the stage of ovarian cancer at the time of diagnosis.
MW: What are the various stages of ovarian cancer?
CO: Ovarian cancer stages range from Stage 1 through Stage 4. As a rule, the lower the number, the less the cancer has spread. A
higher number means the cancer has spread abundantly through the body.
During Stage 1, cancer is confined to one or both ovaries. With Stage 2, cancer has spread to the uterus or other nearby organs. In Stage 3, it has spread to the lymph nodes or abdominal lining. Lastly, Stage 4 is when cancer has
Listen to your body. No one knows your body better than you do. It might take more than a second, third or fourth opinion to get the answers you need, but keep fighting for the care that you deserve. Lastly, file a formal complaint if you feel you’ve been mistreated by your healthcare provider.
spread to distant organs, such as the lungs or liver.
MW: What is the life expectancy of ovarian cancer?
CO: For all types of ovarian cancer combined, about 78 percent of those with ovarian cancer live for at least one year after diagnosis. More than 60 percent live for at least three years after being diagnosed, and over 50 percent of patients with ovarian cancer are still alive at least five years after diagnosis.
MW: I saw a recent article where it stated the new recommendation to prevent ovarian cancer is for women to have their fallopian tubes removed. Why is this a recommendation for women?
CO: People who are at increased risk of developing ovarian cancer, such as those who carry the breast cancer genetic mutation, are recommended to have a stand-alone surgery to remove fallopian tubes with both ovaries.
MW: Are there potential side effects or risks with having the fallopian tubes removed?
CO: As with most surgeries, there are risks associated with the surgical removal of the fallopian tubes, such as bleeding at the surgery site, reaction to general anesthesia, blood clots, damage to surrounding organs and tissues and infection.
MW: What steps do you recommend women take to determine if they are at risk for the genetic mutations with ovarian cancer?
CO: Women should speak to their primary care physician about genetic testing for hereditary ovarian cancer. This testing looks for mutations in the BRCA1 (Breast Cancer gene 1) and BRCA2 (Breast Cancer gene 2) genes. Your doctor might suggest testing using a multigene panel, which looks for mutations in several genes at the same time, including BRCA1 and BRCA2.
disproportionately affected by high-grade and aggressive ovarian tumors?
CO: The biological underpinnings of this are unclear. There is some evidence that Black women are more likely to inherit DNA changes involved in ovarian cancer, including the BRCA1 and BRCA2 gene mutations.
MW: How would you advise women to better advocate for their health?
CO: Do your research. When you’re in a situation where your doctor is dismissing your symptoms, it’s easy to get flustered and blank on specific concerns. The fix for that is to write it all down. Listen to your body. No one knows your body better than you do. It might take more than a second, third or fourth opinion to get the answers you need, but keep fighting for the care that you deserve. Lastly, file a formal complaint if you feel you’ve been mistreated by your healthcare provider.
MW: Why are Black women
For all types of ovarian cancer combined, about 78 percent of those with ovarian cancer live for at least one year after diagnosis. More than 60 percent live for at least three years after being diagnosed, and over 50 percent of patients with ovarian cancer are still alive at least five years after diagnosis.
DIABETES IN THE AFRICAN AMERICAN COMMUNITY: HOW CAN WE MAKE A DIFFERENCE?
 By Terrianna Mccullough
By Terrianna Mccullough
Diabetes is a persistent medical condition that alters the body's ability to process food into energy. In the African American population, the lack of knowledge regarding diabetes poses a significant health risk to thousands. This can be attributed to a breakdown in communication between healthcare professionals and patients, causing a significant gap in spreading awareness about diabetes. The communication barrier has resulted in a significant amount of misinformation, leading to adverse health outcomes among African Americans. For example, according to an article published by the University of Wisconsin School of Medicine and Public Health, in 2017, African Americans had 2.1 times the risk of death due to diabetes compared to Whites. Therefore, it is crucial to address this gap and create channels of effective communication so that accurate information about diabetes can be provided to patients and the
overall community.
Peggy Johnson of Mullins, S.C., a 68-year-old African American woman battling diabetes for more than 20 years, understands the severity. Johnson recalls before being diagnosed, she lived a “normal life,” tending to children while working
full-time. She recalls that her doctor did not walk her through the impacts of this life-changing disease. “I did not know how this would be more of a lifestyle change rather than an intrusive medication regimen,” Johnson said.
Even though diabetes does not
Black adults in the U.S. are 60 percent more likely than white adults to be diagnosed with diabetes.
-Northwestern Medicine
First and foremost, stop hiding. Take charge of things and make positive changes in your life and in the community. The best way to overcome any health condition in our community is by being honest with how we feel and not hiding it from the ones we love.
have the stigma of being a deadly disease, it is a complicated disease that deserves an explanation of its symptoms, treatment options and factors that cause this disease. Awareness within the African American community about diabetes is real, and much of this is centered on the patient to provider relationship - such as the case with Johnson.
According to the Centers for Disease Control and Prevention (CDC) National Diabetes Statistics Report for 2022, cases of diabetes have risen to an estimated 37.3 million. However, this number may not be accurate due to the lack of individuals who receive frequent checkups and blood work. Lack of access to Black healthcare providers also plays a role in the rise of diabetes.
Suzanne Williams, a nurse at a college in South Carolina, said that if more Black healthcare providers were available, it would encourage people to visit doctors more frequently and establish relationships with their
providers, allowing for comfort in sharing issues or posing questions.
“We need more of us everywhere, and we need to do more for ourselves and our community,” Williams said. “Having a provider that looks like us could encourage people to visit the doctor more frequently and establish relationships with our providers.” Williams added that until Americans, especially African Americans, take ownership of their health, receive affordable insurance and have serious conversations with their family, friends and healthcare providers,
Until Americans, especially African Americans, take ownership of their health, receive affordable insurance and have serious conversations with their family, friends and healthcare providers, only then will we begin to see more greater awareness about diabetes and how it affects the Black community.
only then will we begin to see more greater awareness about diabetes and how it affects the Black community.
Although symptoms of diabetes are not always common across different demographics, a few symptoms are considered part of diabetes Type 1 and Type 2, including increased thirst and urination, increased hunger, fatigue, blurred vision, numbness or tingling in the feet or hands, sores that do not heal and unexplained weight loss. However, symptoms may vary among individuals. Williams said symptoms are a major way in which we can identify diabetes and conquer lifestyle changes needed to live with diabetes. "It is crucial to keep race, ethnicity, gender and pregnancy factors in mind while we converse about the variance in symptoms of this disease."
African Americans have a high risk for Type 2 diabetes. Genetic traits, the prevalence of obesity and insulin resistance all contribute to the risk of diabetes in the African American community.
-National Library of Medicine
Johnson recalls that her symptoms were numbness, sharp pain like a mosquito bite, weight gain and pain in the abdominal area. Being that these symptoms do not completely mirror the usual searches on diabetes symptoms is why it is important to have a specialized healthcare provider to confirm or

rule out if someone has diabetes.
In this journey of coping and fighting with diabetes, Johnson shared practical insights with others who are battling this disease.
“First and foremost, stop hiding. Take charge of things and make positive changes in your life and in the community. The best way to overcome any health condition in our community is by being honest with how we feel and not hiding it from the ones we love,” Johnson said. “Use personal stories to provide awareness to your friends and loved ones. Use this as an opportunity to share information between family members and to have an open dialogue about the power of genetics and health conditions members of the same family may face.”

HEALTHY DISH
This issue’s healthy dish is from author and chef, Christine C. Preston, who takes pleasure in serving, encouraging and spreading love. She embraces the opportunity to do so through sharing clean meal ideas with loved ones. Christine’s recipe book, “Clean Plate, Fresh Slate,” was birthed after she jump-started her weight-loss journey in May of 2020.
• 3/4 cup of grated parmesan
• Small bunch of dried basil
• Seasoning salt, pepper and Italian Seasoning
DIRECTIONS:
• Peel and thinly slice Eggplant (sprinkling a small amount of seasoning salt and pepper on each side); Set aside on a towel to drain excess water, which helps with frying.
• First, preheat the oven to 350 degrees F.
• Sauté' your bell peppers, onions and mushrooms in olive oil; drain and set to the side.
As Christine began making a conscious effort to monitor what she put in her body, she noticed a drastic change in her energy, skin, mood, and of course, her weight. Christine felt it only right to share these new changes, in hopes of encouraging others. She began sharing pictures and recipes of her clean meals on social media for the sole purpose of giving quick, easy and delicious healthy meal ideas. It is Christine’s sincerest prayer that her readers will feel motivated, encouraged and hopeful upon trying out her clean meals. She has coined the statement, “We’ve got this because God’s got us!” She firmly believes that when you make one step, God makes two. “Clean Plate, Fresh Slate” is available on Amazon.
INGREDIENTS:
• 2 eggplants
• 2 eggs
• 1/2 diced bell pepper, 1/2 diced onion and 1/2 cup of chopped mushrooms
• Almond flour for dusting
• 1 jar of Margherita Pizza Sauce
• 1 package of fresh mozzarella cheese cut into cubes
• Dip eggplant slices in egg, then lightly dust in almond flour & fry them in olive oil.
• Spray a baking dish with olive oil spray and spread pizza sauce all over it, evenly.
• Place eggplant slices in the sauce.
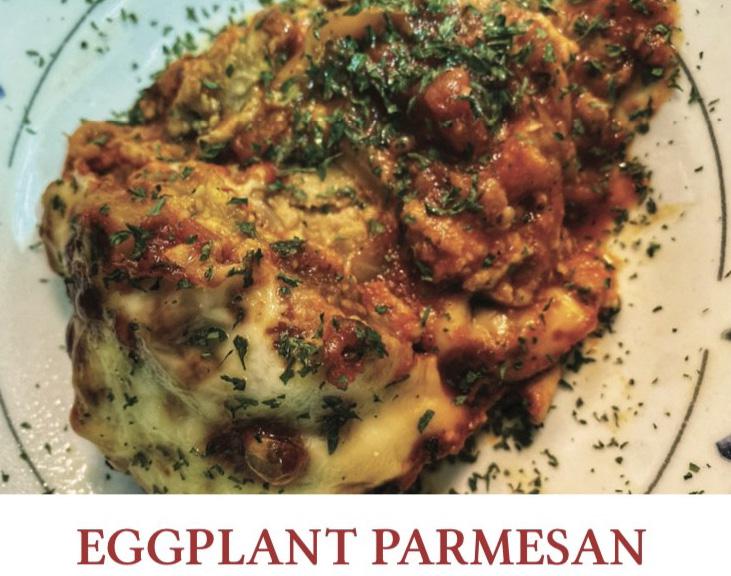
• Spread sautéed veggies over eggplant slices and sprinkle with parmesan cheese.
• Top it with cubes of mozzarella, basil and parmesan.
• Repeat the layering process (For the top layer, spoon remaining sauce and cheese.).
• Cover loosely with foil and bake for 20 minutes; remove foil and bake for another 20 minutes. (Optional: Place under broiler for 3-5 min.)
UNDERSTANDING THE SYMPTOMS, TREATMENTS AND PREVENTIVE MEASURES OF
PROSTATE CANCER
Men all around the world are affected by prostate cancer, which is a serious health issue. It is the most common cancer among men, excluding skin cancer, and is a leading cause of cancer-related deaths in men. In this article, we will delve into the basics of prostate cancer, including its definition, signs and symptoms, risk factors, treatments and preventive measures.
WHAT IS PROSTATE CANCER?
The prostate is a small gland located in the male reproductive system, which is responsible for producing seminal fluid that nourishes and transports sperm. Prostate cancer occurs when abnormal cells in the prostate gland start to multiply uncontrollably, leading to the formation of a tumor. Over time, this tumor can grow and spread to nearby organs or other parts of the body, such as bones, lymph nodes or distant organswhich can lead to serious health complications.
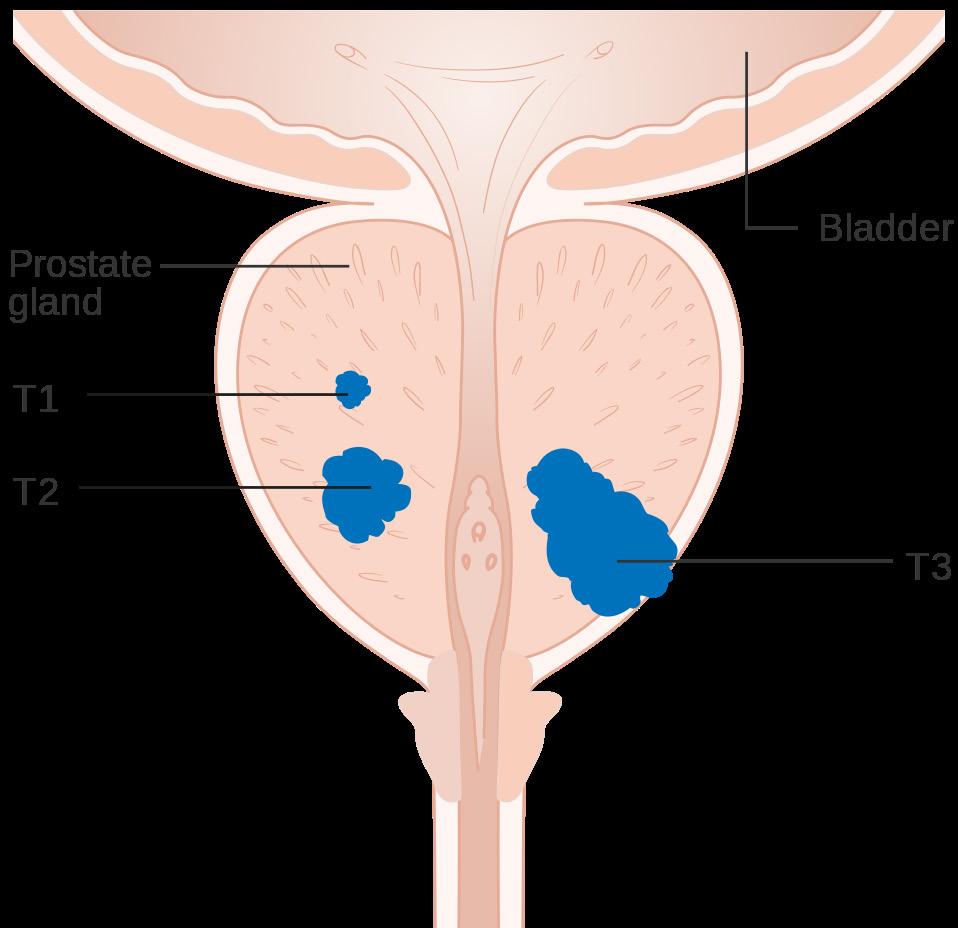
Prostate cancer is typically slow-growing cancer and may not cause symptoms in its initial stages. However, it can become aggressive and spread rapidly in some cases. Men should be aware of the signs and symptoms of prostate cancer and undergo regular screenings to detect it early when it is most treatable.
SIGNS AND SYMPTOMS OF PROSTATE CANCER
In its early stages, prostate cancer may not show any signs or symptoms - but as the cancer progresses - it can cause a variety of issues that may include:
Urinary symptoms. Prostate cancer can affect the urinary system and cause symptoms such as frequent urination, especially at night, difficulty starting or stopping urine flow, weak urine flow, incomplete emptying of the bladder or a sense of urgency to urinate.
Sexual dysfunction. Prostate cancer and its treatments can also affect sexual function. Men may
experience erectile dysfunction, reduced sexual desire or pain during ejaculation.
Blood in semen or urine. Prostate cancer can result in the appearance of blood in the urine or semen. If you notice blood in your urine or semen, it is important to see a healthcare professional for evaluation.
Pain or discomfort. Advanced prostate cancer may cause pain or discomfort in the pelvic area, lower back, hips or thighs. In some cases, the pain may be persistent and worsen over time.
Bone pain. Prostate cancer that has spread to the bones may cause bone pain, especially in the back, hips or pelvis. This may be a sign that cancer has reached an advanced stage and requires prompt medical attention.
These symptoms may not necessarily be indicative of prostate cancer and may also be caused by other conditions. However, if you experience any of these
symptoms, it is crucial to consult a healthcare professional for proper evaluation and diagnosis.
AGE GROUP MOST AFFECTED BY PROSTATE CANCER AND SOME RISK FACTORS
Prostate cancer typically affects older men, with the risk of developing the disease increasing with age. According to the American Cancer Society, the average age at the time of prostate cancer diagnosis is 66, and about six in 10 cases are diagnosed in men aged 65 or older. Prostate cancer is rare in men under 40, but the risk increases significantly after the age of 50.
Family history and genetics also play a role in the development of prostate cancer. Men with a family history of prostate cancer, especially if it involves a father, brother or son, are at a higher risk of developing the disease. Additionally, certain genetic mutations, such as mutations in the BRCA1 and BRCA2 genes, which are commonly associated with breast and ovarian cancer in women, can also increase the risk of prostate cancer in men.
Men, especially those with a family history of prostate cancer, need to be aware of the risk and consider regular screenings and discussions with their healthcare provider about their risk factors and appropriate preventive measures.
TREATMENT OPTIONS FOR PROSTATE CANCER
The treatment options for prostate cancer depend on a range
of factors, including the stage of cancer, the aggressiveness of the tumor, the age and overall health of the patient and the patient's preferences. The main prostate cancer therapies are as follows: Active surveillance. For men with low-risk prostate cancer that is slow-growing and not causing symptoms, active surveillance may be an option. This involves regular monitoring of Prostate-Specific Antigen (PSA) levels, periodic imaging studies and biopsies to assess the progression of cancer. Treatment may be deferred until there are signs of disease progression.
Surgery. Surgery to remove the prostate gland, called a radical prostatectomy, may be recommended for localized prostate cancer. It can be done using different techniques, such as open surgery or minimally invasive techniques like laparoscopic or robotic-assisted surgery. Surgery may be associated with risks,
such as urinary incontinence and erectile dysfunction, and should be discussed thoroughly with the healthcare provider.
Radiation therapy. In this therapy, high-energy rays help to eliminate cancer cells. It can be delivered externally using a machine (external beam radiation therapy) or internally through small radioactive pellets implanted in the prostate (brachytherapy). Radiation therapy may be used as a primary treatment for localized prostate cancer or as adjuvant therapy after surgery to kill any remaining cancer cells.
Hormone therapy. The growth of prostate cancer cells is dependent on male hormones like testosterone.
Hormone therapy, also known as androgen deprivation therapy, aims to lower the levels of male hormones in the body or block their effects on cancer cells. It can be done through medications or surgical removal of the testicles (orchidectomy). Hormone therapy may be used
alone or in combination with other treatments for advanced or high-risk prostate cancer.
Chemotherapy. Drugs are used in chemotherapy to eradicate cancer cells throughout the body. It may be recommended for advanced prostate cancer that has spread to distant organs or has not responded to other treatments. Chemotherapy is usually used in combination with hormone therapy or as a palliative treatment to relieve symptoms and improve quality of life.
Immunotherapy. Immunotherapy is a type of treatment that boosts the body's immune system to recognize and attack cancer cells. It is a newer treatment option for prostate cancer and may be used in certain cases, such as advanced prostate cancer that has not responded to other treatments or in clinical trials.
Targeted therapy. Targeted therapy is a type of treatment that uses drugs to specifically target cancer cells based on their unique characteristics, such as genetic mutations or proteins on their surface. It can be used in combination with other treatments for advanced prostate cancer or as a part of clinical trials.
Palliative care. Palliative care focuses on providing relief from symptoms and improving the quality of life for patients with advanced prostate cancer. It may involve managing pain, addressing the side effects of treatments, providing emotional support and helping with decision-making and advanced care
planning.
PREVENTIVE MEASURES FOR PROSTATE CANCER
While the exact cause of prostate cancer is unknown, there are preventive measures that men can take to reduce their risk of developing the disease. These include:
Regular screenings. Regular screenings, including the PSA blood test and the digital rectal exam, can help detect prostate cancer at an early stage when it is most treatable. Discussing with a healthcare provider about the appropriate timing and frequency of screenings based on individual risk factors is important.
Maintaining a healthy lifestyle. Eating a balanced diet that is rich in fruits, vegetables and whole grains, and low in red meat and saturated fats, can help reduce the risk of prostate cancer. Regular exercise and maintaining a healthy weight also play a crucial role in overall prostate health.
Quitting smoking. Smoking has been associated with an increased risk of developing aggressive forms of prostate cancer. Quitting smoking can not only reduce the risk of prostate cancer but also improve overall health.
Limiting alcohol intake. Heavy alcohol consumption has been linked to an increased risk of prostate cancer. Moderating alcohol intake or avoiding it altogether can be beneficial for prostate health.
Regular follow-up with a
healthcare provider. It is important to have regular check-ups with a healthcare provider to monitor overall health, including prostate health. Discussing any concerns or changes in urinary or sexual function can help detect any potential issues early on.
Managing risk factors. Certain risk factors, such as age, race and family history, cannot be changed. However, being aware of these risk factors and discussing them with a healthcare provider can help in determining the appropriate screening and preventive measures.
Prostate cancer is a common cancer that affects men, particularly those over the age of 50. Men need to be aware of the risk factors, signs and symptoms and available treatment options for prostate cancer. Regular screenings and discussions with a healthcare provider can help with early detection and appropriate management of the disease. Lifestyle modifications, such as maintaining a healthy diet, exercising regularly, quitting smoking and limiting alcohol intake, along with regular follow-ups with a healthcare provider, can also play a crucial role in preventing prostate cancer or managing its risk factors. Men need to take proactive steps to prioritize their prostate health and make informed decisions about their screening and treatment options to ensure optimal outcomes.
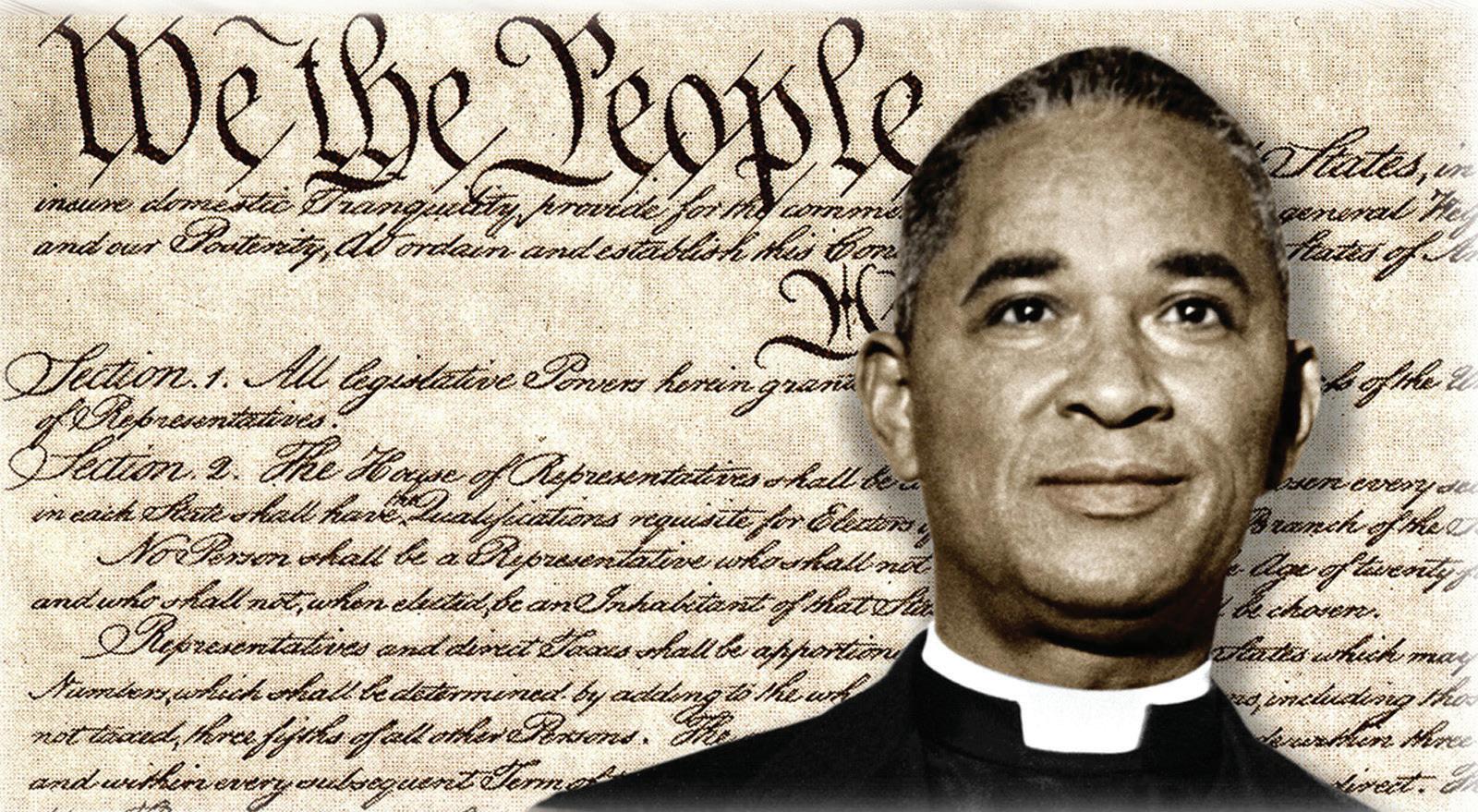
The Pursuit for Social Justice & Racial Accord Never Ends at the CECIL WILLIAMS SOUTH CAROLINA CIVIL RIGHTS MUSEUM
Palmetto State’s First & Only Civil Rights History Museum

Now Accepting On-Site Appointments

Telephone: 803-531-1662/803-347-8001 for additional information. Orangeburg, South Carolina
Reverend Joseph A. DeLaine, a courageous, fearless, faithful man of integrity, was the impetus behind the Clarendon County Briggs petitioners. After this case combined with four others led to Brown v. Board of Education, he frequently became a target and received death threats. In 2004, President George Bush awarded DeLaine, Briggs and Pearson, the Congressional Gold Medal for their efforts which overthrew the 1896 Plessy v. Ferguson and ‘separate but equal’ doctrine and legal segregation; all this years and months before the better known MLK, Rosa Parks, and Montgomery Bus Boycott. This history and legend rightfully places South Carolina as the birthplace of the Civil Rights Movement.
and thriving: LIVING WITH VITILIGO
By Megan FreemanTara Oliver, a quality control specialist who recently celebrated her 50th birthday, was diagnosed at age 28 with the chronic autoimmune disorder vitiligo, which is a condition that causes areas of the skin to lose pigment. Although her journey was not always easy, she has found some crafty ways to protect herself and be confident in the skin she is in.
According to the National Institute of Arthritis and Musculoskeletal and Skin Diseases, vitiligo is an autoimmune disease in which the body’s immune system attacks and destroys the melanocytes. In addition, researchers continue to study how family history and genes may play a role in causing vitiligo. Oliver is not the only one in her family with vitiligo. Her mother was diagnosed with it at age 13.

Sometimes an experience, such as a sunburn, emotional distress or exposure to a chemical, can trigger vitiligo or make it more challenging.
People with the condition have wide-ranging symptoms from having small skin patches of “milky-white” tones in various places on their body to being primarily covered all over like Oliver’s mother.
“There is nothing you can do to avoid the disorder, but steroids may help slow it down. It must take its course. No one spreads the same and the patches can appear differently from person to person,” said Oliver. “My mother has been seen by a variety of specialists, and they all told her the same thing. Once it is finished spreading, it will stop. Because of her experiences, she was able to help prepare me for what was happening when I was first diagnosed.”
Some people have it worse than I do so I continue to walk with confidence. Others may look or stare, but that’s ok; I’m confident in who I am.
-Tara OliverTara Oliver displaying some of the areas where she is affected by vitiligo.

At first, Oliver said she was very self-conscious when she was diagnosed despite having grown up with a mother who has it. “I went through school and through most of my young adult stage never having vitiligo. Then suddenly, I was faced with it. Although my mother was not treated differently and was very confident dealing with vitiligo, it was a very difficult time for me.”
According to the American Academy of Dermatology Association, having vitiligo increases the risk of having other autoimmune diseases like thyroid disease and alopecia areata (hair loss).
“I was diagnosed with thyroid disease after noticing a spot on my ring finger and from there, it turned into vitiligo. I take a 2000 milligram Vitamin D pill and a Levothyroxine daily for treatment. Doctors can prescribe steroid creams, but they do not work as well for me,” says Oliver.
Oliver is a mother of two children, Kiara, 32, Naseal, 22, both who do not have vitiligo. Oliver said, for the longest, her mother thought she would not get it especially after getting through her teenage years. Oliver is now concerned about her children being diagnosed.
“Once I was diagnosed, I became very worried about my children contracting the condition. I continue to worry about my kids to the point where I watch my son like a ‘hawk’ and anything he gets on his skin I must examine.”
Vitiligo affects all races and
sexes equally. It is more visible in people with darker skin tones. Although vitiligo can develop in anyone at any age, macules or patches usually become apparent before age 30 according to the Cleveland Clinic.

Because of the condition, Oliver cannot absorb large doses of sunlight and must take extra precaution using certain skin care items such as lotions and body washes.
Canadian fashion model Winnie Harlow, who has vitiligo, started the skin care line Cay Skin, which Oliver uses and says it does a great job of protecting her skin. Oliver also suggests that women
with vitiligo who like to wear makeup use Kat Von D, a highpigment vegan makeup line that safely covers vitiligo.
Oliver’s advice to other women with vitiligo is for them to be themselves and think of it as a blessing in disguise. “Some people have it worse than I do so I continue to walk with confidence. Others may look or stare, but that’s ok; I’m confident in who I am.”
For those living with vitiligo, Oliver encourages them to get extra tint for car windows for protection from the sun and for those with spots on their lips, use sun-protection Chapstick as skin burns can be severe.
If you’re noticing changes, it could be Alzheimer’s. Talk about visiting a doctor together.
ALZ.org/TimeToTalk

“ Early detection gave us time to adapt together, as a family.”
ALEXANDRIA SMITH SHARES THE CHALLENGES OF LIVING WITH BIPOLAR DISORDER
Alexandria Smith recently launched a blog where she shares her experiences as a wife and mom while also coping with a chronic mental illness. Through her blog, “MomWifeWorshipLife,” she hopes to encourage other women and normalize the importance of self-love and care to remain mentally and emotionally balanced.
After receiving a bachelor’s degree in computer science from South Carolina State University and a master’s degree in computer science from Auburn University, Smith was an educator for more than 15 years. Now a stay-at-home wife and mom to her husband, Stephen, and two girls, Alia and Mia, Smith shared with Motivated Woman her challenges with bipolar disorder.
MW: What is bipolar disorder?
AS: Bipolar disorder is a mental health condition that affects a person's mood and energy levels. People with bipolar disorder experience episodes of extreme highs (mania or hypomania) and lows (depression) that can last for days, weeks or even months.
During a manic episode, a person may feel elated, euphoric or irritable. They may have an inflated sense of self-esteem, talk rapidly, have racing thoughts and engage in risky behavior. During a depressive episode, a person may feel sad, hopeless, and have a lack of interest or pleasure in activities they once enjoyed. They may also have trouble sleeping, eating and concentrating. Bipolar disorder can be treated with medication, therapy and lifestyle changes.
MW: When were you first diagnosed with bipolar disorder?
Bipolar disorder feels like being on a roller coaster that I can’t get off, experiencing recurring highs and lows that are outside of my control.
AS: I was diagnosed with bipolar disorder at the age of 21 after experiencing a traumatic life event.
MW: What were some of the symptoms that you had?
AS: Some of the symptoms that I had were trouble sleeping and eating, hallucinations, racing thoughts and feelings of euphoria.
MW: What does bipolar disorder feel like?
AS: Bipolar disorder feels like being on a roller coaster that I can’t get off, experiencing recurring highs and lows that are outside of my
control.
MW: How does bipolar disorder affect your daily life?
AS: Bipolar disorder affects my ability to maintain full-time employment outside of the home due to experiencing rapid cycles of mania and depression.
MW: What treatments or medications were you prescribed?
AS: I have taken many different medications over the years. I usually take a combination of an antipsychotic, antidepressant and mood stabilizer. I also participate in therapy with my psychologist biweekly and receive treatment from my psychiatrist every four to six weeks for medication management. Additionally, my husband and I participate in ongoing marriage counseling on a bi-weekly basis.
MW: What challenges does bipolar disorder present in your current life as a wife and mother?
It is possible to have a family, career and life that you love even if you have been diagnosed with a mental illness. It does take a great deal of effort and intention to do so, but it is attainable.

AS: Bipolar disorder presents different challenges for me in every stage of life. As a wife and mother, I have had to learn to balance my responsibilities and prioritize selfcare. With anxiety being a major trigger for me, I have to do my best to manage stressful situations so that I do not feel overwhelmed with things that are out of my control.
MW: Who is at risk of developing bipolar disorder? What are the risk factors or triggers for bipolar disorder?
AS: The exact cause of bipolar disorder is not fully understood, but research suggests that it is likely due to a combination of genetic, environmental and neurochemical factors.
While anyone can develop bipolar disorder, some factors can increase a person's risk, including:
• Family history. People with a family history of bipolar disorder are more likely to develop the condition themselves.
• Age. Bipolar disorder can develop at any age, but it often first appears in late adolescence or early adulthood.
• Substance abuse. Substance
abuse can trigger or worsen bipolar disorder symptoms.
• Stressful life events. Traumatic or stressful events, such as the loss of a loved one or a major life change, can trigger the onset of bipolar disorder.
• Medical conditions. Certain medical conditions, such as thyroid disorders, can increase the risk of developing bipolar disorder.
MW: What are the chances of your children inheriting bipolar disorder?
AS: The chances of my children inheriting bipolar disorder are greater than someone who has no family history of the illness; however, it is not guaranteed that they will inherit the disorder simply because I have been diagnosed with it.
MW: I read an article that stated most Black people with bipolar disorder are going undiagnosed and untreated. Why do you think this is?
AS: Unfortunately, there is a great stigma in the African American community surrounding mental illness which can prevent people from seeking help. This can be due to several different factors, such as a distrust of the medical system or a belief that mental illness is a weakness or a result of personal failure. Also, there may be a lack of awareness and education about mental health and bipolar disorder within the African American community. This can lead to a lack of understanding about the symptoms of bipolar disorder and how to seek help for it.
MW: Are there any other details or experiences that you would like to share?
AS: I would like people to know that it is possible to have a family, career and life that you love even if you have been diagnosed with a mental illness. It does take a great deal of effort and intention to do so, but it is attainable.
TOP FIVE BEAUTY BRANDS FOR AFRICAN AMERICANS
The beauty industry has made great progress toward inclusivity and diversity in recent years. Numerous beauty businesses have emerged as pioneers in meeting the specific requirements and aesthetic preferences of African Americans as the importance of representation increases. This article examines the top five beauty companies that have not only revolutionized the industry but also promoted African American beauty and made it a cause for celebration. These companies, with their remarkable products - from Laws of Nature's dedication to clean beauty to Pat McGrath's artistic inventions to Fenty Beauty's game-changing foundations - have revolutionized the beauty business. In addition, we'll highlight two additional African American companies that have made significant contributions to the industry.
FENTY BEAUTY BY RIHANNA

The industry changed forever when global music icon Rihanna's Fenty Beauty line was introduced in 2017. Fenty Beauty, which advertises with the slogan "Beauty for All," upended the market by producing
a wide variety of foundation hues that were appropriate for all skin tones while especially appealing to those with darker complexions. Rihanna's line instantly won praise from all around the world. It offers 50 foundation tones that were previously disregarded by bigname cosmetic companies. Beyond foundation, Fenty Beauty expanded its product line to include a variety of cosmetics such as eyeshadow palettes, highlighters and lipsticks that are all designed to complement a variety of skin tones. Fenty Beauty raised the bar for diversity in the cosmetics sector by honoring and empowering African Americans through their wide selection of products.

PAT MCGRATH LABS
The renowned makeup artist Pat McGrath developed Pat McGrath Labs, which has grown to be associated with high fashion and innovative makeup creations. McGrath changed how people view beauty as the first world-wide creative design director for a beauty brand. The luxurious, innovative and intensely pigmented items from her brand are adored by cosmetics fans all over the world. Pat McGrath Labs is renowned for its limited-edition collections that are in high demand. They provide a variety of vivid eyeshadows, sumptuous lipsticks and captivating highlighters. The company's dedication to diversity is apparent
in the variety of shades it offers, guaranteeing that African American customers are more likely to select products that genuinely meet their beauty requirements.
LAWS OF NATURE COSMETICS

Jasmine Rose established the innovative beauty company Laws of Nature Cosmetics. This Black owned company prioritizes promoting "clean beauty" while catering to the requirements of African American customers. The goal of Laws of Nature is to offer natural, high quality and nontoxic cosmetics that rejoice in the diversified beauty. The brand offers a variety of skincare, lip treatments, concealers, foundations and other cosmetics that are all made with skin-friendly and nourishing components. Laws of Nature places

a strong emphasis on sustainability and makes sure that all its products are free from harmful chemicals and cruelty-free. Laws of Nature has built a devoted following among African Americans by catering to their distinct skin issues, such as hyperpigmentation and textured hair. This company encourages people to appreciate their natural beauty while continuing to maintain environmental sustainability.
UOMA BEAUTY
Sharon Chuter, Nigerian-born founder of Uoma Beauty, created the company intending to develop products that honor the full range of beauty. Uoma, which is Igbo for "beautiful," aims to redefine inclusivity and challenge outmoded beauty norms. A wide range of skin tones is catered for by the brand's foundations, concealers, lipsticks, eyeshadows and skincare items. The 'Say What?!' foundation collection from Uoma Beauty is well-known


for its outstanding selection of 51 hues that cover a wide range of undertones, from deep ebony to fair porcelain. The company's dedication to diversity goes beyond shade selection. Uoma Beauty also embraces cultural variety through the names and packaging of its products, which are inspired by many African tribes and civilizations. Through initiatives like the "#PullUpOrShutUp" movement and other campaigns, Uoma Beauty actively supports social causes and campaigns for diversity and equality within the beauty industry. Uoma Beauty has established itself as a pioneering brand within the African American community thanks to Sharon Chuter's mission of empowering everyone to embrace their individual beauty.

BLACK OPAL BEAUTY
A dermatologist and a chemist developed Black Opal Beauty to cater to the unique skincare and cosmetic requirements of people of color. Black Opal Beauty has established itself as a reliable brand among African American customers by concentrating on developing products that celebrate and accentuate skin rich in melanin. A seamless fit for a variety of skin tones is guaranteed by the brand's vast selection of foundation colors that accommodate varying undertones. Foundations, powders, concealers, primers and skincare items that address hyperpigmentation and other common issues are all part of Black Opal Beauty's extensive product collection. Due to the company's commitment to research and development, they have been
able to design formulae that are specifically tailored to the special skincare requirements of African Americans. Black Opal Beauty strives to empower people by enhancing their natural beauty and supporting skin health with a strong focus on quality, efficacy and variety. The beauty industry has recently seen a profound transformation toward inclusivity and diversity, with some businesses setting the standard for recognizing and celebrating African American beauty. These companies have challenged beauty standards and offered products that address the different requirements of African Americans, from the groundbreaking offerings to the dedication of clean beauty products. These top five beauty firms' commitment to excellence has revolutionized the market, encouraged people to embrace their individual beauty and cultivated a feeling of pride in the African American community.
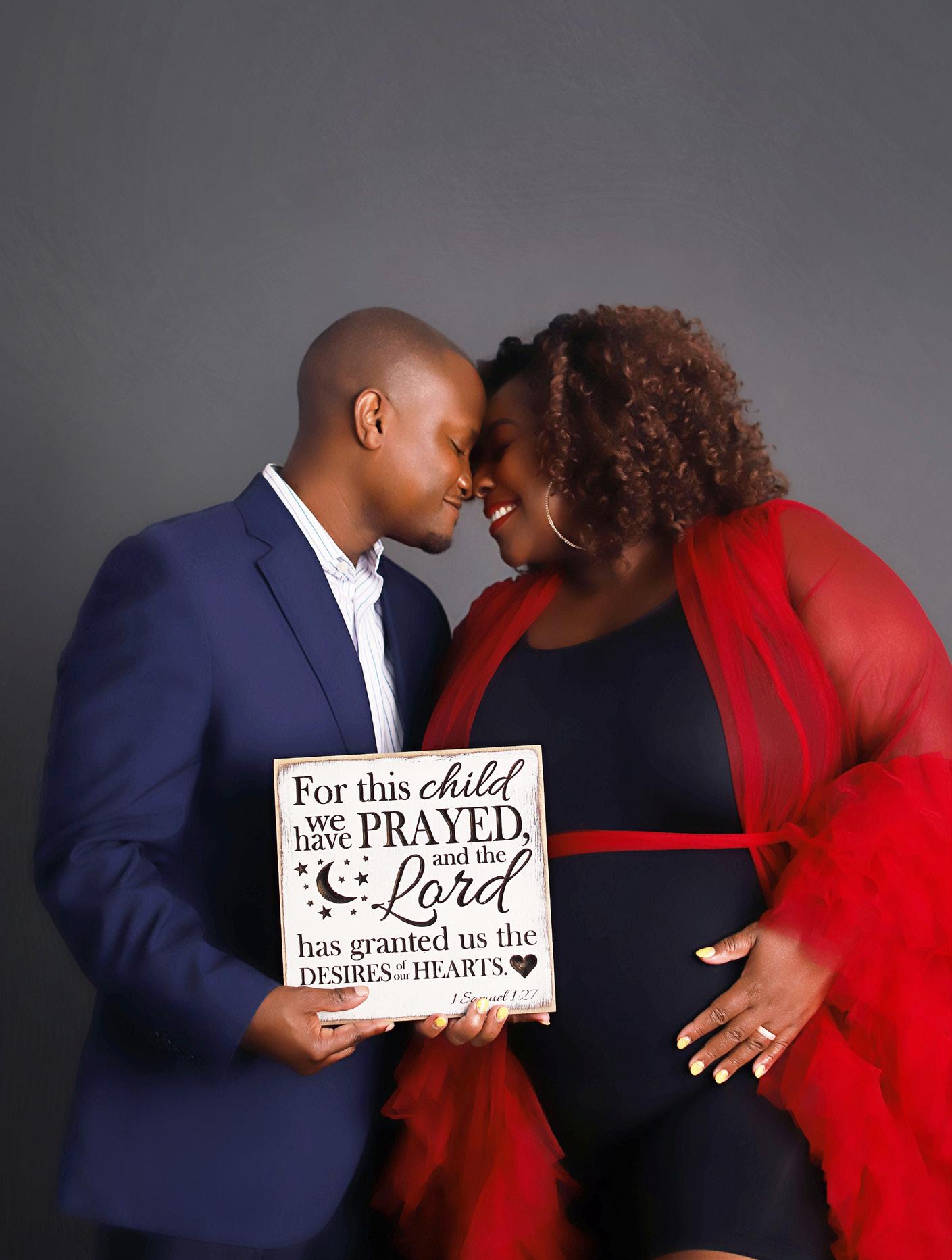
SUFFERING FROM MULTIPLE MISCARRIAGES, BRIGIDA MACK SHARES HER STORY OF HOPE, FAITH AND LOVE
 By Elizabeth Mosely-Hawkins
By Elizabeth Mosely-Hawkins
As an award-winning former journalist with 20 years of experience in television news, Brigida Mack could hurdle with ease the common challenges of working in the newsroom – early mornings, late evenings, tight deadlines and occasional heart-wrenching tragedies to report. It was part of the job. No big deal.
But when life, as it so often does, makes us the headline in our own personal journey, Brigida wanted nothing more than to change the channel to a story other than her distressing saga. She would discover, however, that her story of tragedy would become a tale of triumph for her and hundreds of others.
Brigida, who lives in Charlotte with her husband Reuben, has suffered from multiple miscarriages while on her journey to motherhood. She’s not alone. One in eight couples will struggle with infertility.
Ironically, while growing up, Brigida said she had an inclination that she would be unable to conceive children.
“In hindsight, I think part of it was God bringing me face-to-face with my deepest fear - and having to navigate that. Sometimes God doesn’t move the mountain. Sometimes it’s about showing you that you are strong enough to climb it. You are strong enough to overcome your greatest fear,” Brigida said.
It would take her several years, hours of therapy and many moments of choosing herself first to attain that wisdom.
About a year after she married in 2015, the then 36-year-old and her husband began trying for a baby. It did not take the pair too long to get pregnant, she
In hindsight, I think part of it was God bringing me face-toface with my deepest fear - and having to navigate that. Sometimes God doesn’t move the mountain. Sometimes it’s about showing you that you are strong enough to climb it. You are strong enough to overcome your greatest fear.
 Mack, and husband, Reuben, during the pregnancy journey
Image courtesy of: Charmarie Photography
Mack, and husband, Reuben, during the pregnancy journey
Image courtesy of: Charmarie Photography
recalled. She embraced all the early joys that accompanies one when they learn they are pregnant. At 10 weeks, though, she suffered a miscarriage. She was devastated.
Having not shared the loss with her family, friends or co-workers, Brigida swiftly scheduled a dilation and curettage (D and C) procedure the Saturday after the loss. The procedure is usually done to remove pregnancy tissue from inside the uterus during a miscarriage.
She only gave herself a day and a half to rest and returned to work the following Monday. Despite what she might have been feeling emotionally or physically, she resolved to keep going and power through. She would repeat this pattern many times after each fetal loss.
“A critical misstep. A flat-out mistake, but at the time, you don’t know what you don't know,” said Brigida. “I wasn’t giving myself any time to recover, to grieve, to process. I just jumped back into life,” she explained.
In June 2017, the couple learned they were pregnant again. She was surprised, but this time the joy she had from her first pregnancy was replaced with trepidation. She took note of the fear and – again powered through. They had plans to attend a wedding that evening before jetting off to Cozumel for vacation the very next day.
They’d only been in Cozumel for one day when during a trip to
the restroom, Brigida recognized blood stains dotting her underwear. She knew at the moment there was nothing that could be done, being thousands of miles from home. She consulted medical advice through her healthcare provider’s telemedical service to determine how best she might care for herself.
When she returned to North Carolina the following weekend, instead of visiting her doctor, Brigida attended an event for which she was scheduled to serve as mistress of ceremony. While speaking at the
event, standing before a large crowd and in her formal gown, Brigida began to experience cramp-like pain. At this moment, she knew she was miscarrying the baby. Yet, she powered through. She valued her commitments and since she was representing the television station she worked for at the time, she felt obligated to continue.
Brigida decided to seek medical help. Instead of returning to her regular obstetrician gynecologist (OBGYN), she sought a second opinion from a new OBGYN.
She wanted a physician whom she believed would provide her professional care and serve as her advocate. She found that in Dr. Octavia Cannon, a Black woman. For the first time, Brigida felt seen. Dr. Cannon then referred her to reproductive endocrinologist Dr. Matrika Johnson, who was also a Black woman. This medical team duo became instrumental in Brigida’s well-woman care and on her quest to become a mother.
In her advice to women, especially minorities, Brigida strongly encourages them to form a medical team that fully represents them.
“I would encourage women of color to make sure that you have what you need to be advocated for, in the event that you cannot,” she
advised.
Not giving up on their dream of expanding their family, Brigida and Reuben immediately began fertility treatments. She also began taking additional steps to help increase her chances of pregnancy. She reduced the use of certain plastics, as some studies suggest it contributes to infertility, and she cut back on eating sugar-laden foods. She even eliminated the use of certain health and beauty products to avoid toxic chemicals because studies have also shown that can disrupt your endocrine system.
Brigida first underwent three intrauterine insemination treatments or IUI, which is a type of artificial insemination procedure. Two out of three were successful but neither pregnancy advanced beyond 12 weeks.

The fourth pregnancy was the longest she had. Yet, just before the 12-week mark, they learned the baby’s heartbeat had stopped.
Once again, Brigida was devastated. The loss was more unbearable than the others, as she and her family were coping with the death of father-in-love, who
I’ve learned there is peace in the pivot. When you have to change your life. When you have to walk away from things. When you have to pivot to make peace from this journey instead of seeing it as so adversarial, there is peace in the pivot, and there has been a lot of peace that has come with making that pivot.The Macks are all smiles right after the birth of miracle baby, Lincoln.
suddenly passed away six months prior in Kenya. Still tough as nails, Brigida powered through.
One year later, she said her world shattered into pieces. Her mind and body could no longer sustain the demands of her busy career along with the continuous suffering from multiple losses. It was time for Brigida to face her hurt. She could no longer power through.
She took six weeks of family medical leave. Brigida said the first week, she just slept. She was in a state of depression and imposed self-isolation to deal with the pain. Other than her husband, she still had not shared with her family

anything about her experiences. Only one friend was aware of the miscarriages and infertility issues.

After six weeks, Brigida, who
always dreamed of becoming the next Barbara Walters, made the decision not to renew her television contract. She wanted to rest. She wanted to heal.
As she began to heal with intense therapy, something began to happen within her. She recognized for the first time her worth and realized she no longer had to power through. Her peace returned.
“I’ve learned there is peace in the pivot. When you have to change your life. When you have to walk away from things. When you have to pivot to make peace from this journey instead of seeing it as so adversarial, there is peace in the pivot, and there has been a lot of
Once you have walked this road, which is not always a straight line, you really are acutely aware of how much of a miracle it is for you to get to take home a healthy baby. I worked hard to develop a strong mindset to reduce my anxiety.Mack at 39 weeks pregnant Mack with son, Lincoln
peace that has come with making that pivot,” said Brigida.
In gaining the courage to finally tell her family and friends, an opportunity to share her story to a wider audience unfolded. Brigida began to share her story on social media, gaining followers who adored her authenticity and looked forward to her advice.
“If one person feels less alone and feels seen by sharing my story, then all of my vulnerability is worth it,” said Brigida. “I feel so overwhelmed by the support I have received from those who have connected to my story.”
As Brigida began adjusting to life after television and as an influencer, she was ready to try conceiving again. Set to begin in vitro fertilization (IVF) with her now new team of doctors, Brigida discovered she was pregnant before she started the IVF treatments. She was in disbelief.
Given the high-risk nature of pregnancy because of her age and history of miscarriages, her new (and current) OBGYN, Dr. Natasha Denny, referred her to a Maternal Fetal Medicine Specialist to closely monitor her high-risk pregnancy. While her medical team provided her with optimal care, Brigida had to administer on her own. With four pregnancy losses on her mind, she dealt with the intense anxiety that often comes with pregnancy after previous losses.
From her experience with
therapy and her faith in God, she developed a personal regimen of meditation, prayer and resiliency to maintain a positive mental awareness.
“Once you have walked this road, which is not always a straight line, you really are acutely aware of how much of a miracle it is for you to get to take home a healthy baby,” said Brigida. “I worked hard to develop a strong mindset to reduce my anxiety."
On November 29, 2022, Brigida
gave birth to their miracle baby, Lincoln.
As she watches Lincoln grow with amazement, she holds onto this hope for his future.
“I hope that he knows how loved he is and how much we wanted him,” said Brigida. “We are honored that we are his guiding light. I just hope that we can raise a good, kind human.”
BIAS IN HEALTHCARE EQUITY IS HARMING BLACK WOMEN
By Gwynth NelsonIt has become a soundthe-alarm, call to action, everybody get-on-board situation. Black women must selfadvocate for their health. I'm not sure if there ever was a time that this wasn't the case, given the history of medical injustices and inequalities toward people of color, but the urgency of now is that we have so many more tools to help us live healthier lives. Yet, Black women are being diagnosed with cancer, diabetes, high blood pressure and high cholesterol at higher rates than any other race.
The number of birthing women we lose due to maternal health care disparities across America is an absolute travesty, especially prevalent in the South. And where mental health and wellness is concerned, student suicide is at an all-time high as Black girls are twice as likely to contemplate suicidal thoughts than Black boys.
The truth is that a mental health and wellness crisis is happening on HBCU campuses and in culde-sacs all over this country, and unfortunately, Black people are less likely to seek and receive treatment. Far too many Black women are dying – too young, too soon, and dare I say, too needlessly.
We must do everything possible to eliminate barriers to wellness and good health. Education and self-advocacy are two ways to do this. The work we do at South Carolina Institutes of Innovation and Information (SCIII), which is an initiative and vision inspired by the late Sen. John L. Scott, Jr.,
focuses on revolutionizing and cultivating the state's seven fouryear HBCUs' overall capabilities and contributions for the citizens and residents of the state. Through this work, we can be a knowledgebased ally.
Specifically, at The Wellness and Community Health Institute (WACH) at Clinton College, our focus is to foster innovation and educational opportunities related to fields and industries associated with careers promoting communities' wellness and health. We can share that by choosing to go into the field of medicine; it will help lessen the shortage of nurses of color.

There is a dire need for culturally competent nurses that understand and empathize with women of color, and specifically with Black women. The Institute of Teaching and Nursing (TITAN) at Claflin University is successfully addressing this need in both nursing and education. With SCIII being on the campuses of these schools, we are in a unique position to help educate our college-age women to begin this process of self-advocacy early in life.
Soon is not soon enough. We must be efficient and bold about advocating for the health of Black Women. Research has shown that Black women of color are becoming the victims of health crises earlier in life than ever, and sooner than
The truth is that a mental health and wellness crisis is happening on HBCU campuses and in cul-desacs all over this country, and unfortunately, Black people are less likely to seek and receive treatment.
approximately 23 percent of breast cancers identified in Black women are diagnosed before age 50, compared to 16 percent of all breast cancers in white women. This represents a decade sooner and a significant gap in the recommended age for screening.
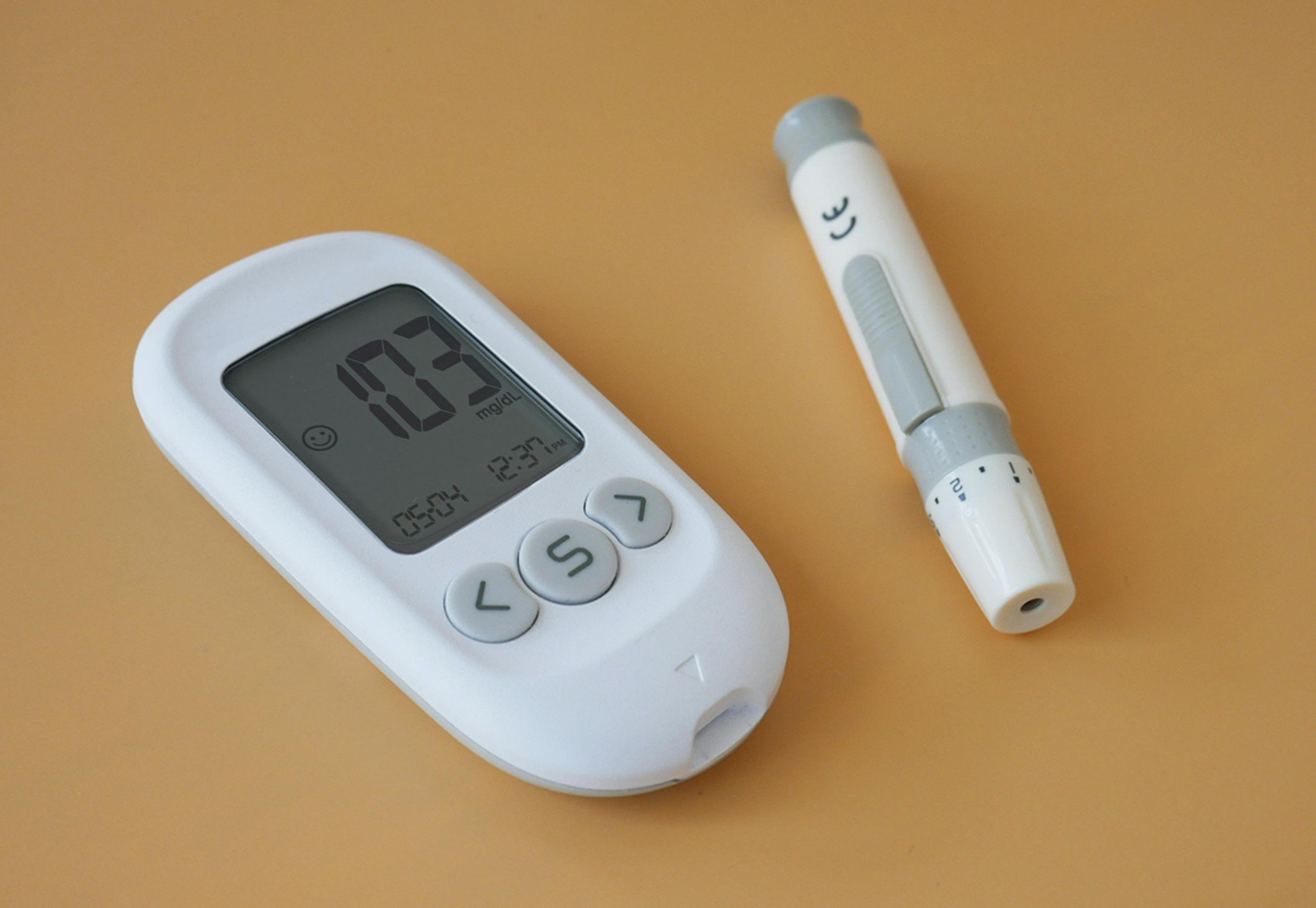
any other race or ethnic group. Just look at the recommended age of 50 for women to be screened for breast cancer. This has been changed to age 40 considering
Advancing equity in healthcare is needed in efforts to support black women. Did you know there is such a thing as VIP births - where money affords a premiere experience for women giving birth? This is just another way privilege can impact a woman's birthing experience. Yet, looking back at what tennis champion Serena Williams went through with her health scare after delivering her daughter should be enough to let us know that knowing
Additional findings uncovered that white patients are viewed as more intelligent and more likely to follow professional advice and that some doctors believe that Black people will abuse drugs, specifically pain medication. your body and pushing past being ignored or the inaction of your provider should never be a deterrent to you. This is an indication that even Black women with money and access can be ignored. This happens when we are not believed when we tell our doctors that we are in
pain. Studies have shown that many doctors believe Black people are more tolerant of pain - with some going as far as believing that our nerve endings are less sensitive, and our skin is thicker.

This racial bias in pain perception means it will appear as a lack of sufficient and less accurate pain treatment. Additional findings uncovered that white patients are viewed as more intelligent and more likely to follow professional advice and that some doctors believe that Black people will abuse drugs, specifically pain medication. As Black women, we cannot remain silent with what has been dubbed the silent epidemic. Spreading the word about selfadvocacy matters because we are only given one body and must care for it by all means necessary.
Nelson, Ph.D., is the executive director for South Carolina Institutes of Innovation and Information (SCIII). SCIII aims to help bridge the gap among students, community and industry leaders, and raise the profile of the state's HBCUs.

SOUTH CAROLINA INSTITUTES OF INNOVATION & INFORMATION

STRENGTHENING SOUTH CAROLINA'S HBCUS
South Carolina Institutes of Innovation & Information (SCIII) is focused on revolutionizing and cultivating South Carolina's seven four-year HBCUs.
www.sciii.net
WOMEN FACE A HIGHER SOCIETAL PRESSURE ABOUT APPEARANCE
By Margaret WilliamsIt is human nature to compare yourself to others, constantly attempting to be the best version of yourself, but why are women subjected to so many double standards? Women are expected to build each other up and be the best version of themselves; drawing the line between constant competition and consistent confidence is becoming smaller and smaller and harder to maintain.
It is no question that women face a higher societal pressure when it comes to their appearance; young girls are brought up to be aware of their every outward appearance. Through dress codes, social media’s constant “body goals,” unrealistic beauty standards and body-shaming,
women have been self-aware of how the outside world views them for as long as they can remember.
In 2012, the Body Positivity Movement gained popularity across social media. This movement consists of praising your body for its physical appearance regardless of what beauty standards have deemed worthy or not. It no longer matters if you think you are too skinny, too short, or too old because outward appearance is not what places value on your character. This movement has created a community for women to appreciate their bodies, but it has also put yet another pressure on women to constantly be positive and praise themselves, regardless of if they truly feel positive about

Women are still competitive. Although there is more representation of women in the media, it doesn’t mean that there is no competition for women to be the best version of themselves.
themselves.
On the other hand, the Body Neutrality Movement is a movement that works toward eliminating the association of body and physical appearance. This movement began around 2016 as an alternative to body positivity. By disassociating appearance from self-worth, it opens space to accept bodies for their functions and purpose without forcing your mind to reject beauty standards and put a positive light on something someone may be insecure about.
Both movements are efforts to change the double standard women are born into, which have been life-changing for some. But have these movements really changed anything, or have they created yet another standard for women?
Research has shown that most girls have a negative body image starting at the age of 13, and this population only grows as they get older. According to Dr. Nicole Matros, a clinical psychologist at the University of South Carolina, when it comes to body image and
our culture today, “people need to be critical reviewers of social media, because there are advocates trying to shift the narrative and it can be helpful to find those people, but anyone posting pictures of bodies in general are a red flag.” When asked if there is a changing narrative on women relationships, Matros said, “It depends on the intent, sometimes people have good intent, but the impact can be harmful or hurtful. There are women who build each other up- but there are some who unintentionally hurt each other, so people need to know themselves and remain critical thinkers.”
Instead of pushing for new movements, trends or standards, there are other solutions to change how women view themselves and each other. College students are at the forefront of this issue, as they are constantly living in a world full of comparisons.
Caroline McNealey, 21-year-old college student, referring to social media said, “It does more harm than good because it is just another way to compare yourself to others. It [social media] is not realistic because people are only showing the highlights of their lives.” This goes to show that although social media is an outlet for people to connect, it is not realistic.
Another college student, Tara Keenan, 20, spoke about women’s relationships. “Women are still competitive. Although there is more representation of women in the media, it doesn’t mean that there

is no competition for women to be the best version of themselves.”
Although these movements have created communities for underrepresented women, they have also created another mold women are expected to fit intoloving and appreciating yourself with no insecurities. This narrative is portrayed all over social media, resulting in another form of competition that those who struggle with loving every piece of themselves cannot achieve. Instead of hyper focusing on these movements and outside resources, as a culture, we need to stop looking at these issues at a surface level and look at the intent. Seeing these movements at the core of the intent and identifying if they are doing more benefit or harm for women at the individual level may result in a more positive outcome.
Research has shown that most girls have a negative body image starting at the age of 13, and this population only grows as they get older.
The Center for Disease Control reports that each year about 264,000 women in the United States are diagnosed with breast cancer and 16 percent of those women die from breast cancer.
KNOWLEDGE GIVES YOU THE OPTIONS: KNOWING YOUR OPTIONS BEFORE THE DIAGNOSIS OF BREAST CANCER CAN SAVE YOUR LIFE
By April WoodyardHere is a story of two similar women and their journey from detection to diagnosis of breast cancer.
Sharon, a 50-year-old African American mother of three children, goes into an imaging center for a screening mammogram after being told by her primary care physician that she has not had a mammogram in three years. Life has gotten a bit stressful, and she simply has not made the time to see the doctor for a physical. After all, she has not had any health issues as far as she knows. She is not even taking any prescription medication. She is 5’6’, and the last time she stepped on the scale, she weighed 190 pounds, for which she quickly subtracted

the three to five pounds for her clothing and shoes.
The imaging center has her fill out a questionnaire before the mammogram is done. One of the questions is regarding her family history. She can only remember that her Aunt Christine had breast cancer around age 44 or 45. Her maternal grandmother also had breast cancer, but she can’t remember the age. She already dreads this test and the compression that she must endure, so she is not too enthusiastic to be there. She survives the test and is happy that she doesn’t have to be nagged by her primary care physician. She checks that off the list of many things she has not done this year.
Five days later, Sharon gets a
call from the imaging center. They inform her that the radiologist saw something unusual and asked if she could return for an ultrasound
scan of her breasts. Sharon is a little concerned but not enough because she doesn’t get around to returning to the imaging center until two months later for additional testing due to the unavailable appointment times.
A technician performs the ultrasound and then Sharon waits for the doctor to come back into the room to talk to her. The radiologist, the healthcare professional who reads the mammograms, comes into the room, and tells her that something was seen on the mammogram and ultrasound that appears to be a benign, “complicated cyst.” He recommends that she follows up in six months to confirm that it does not change. Sharon trusts that radiologist because she has faith in her caregivers and so she agrees to return in six months. Unfortunately, Sharon discovers a lump in her breast while taking a shower three months later. She panics and immediately requests a visit with her primary care physician.
The primary care physician confirms that there is a lump in the breast and after reviewing the image results (the mammogram and ultrasound results done three months ago), it appears that the lump is in the same area. The primary care physician immediately informs the radiologist, and Sharon is scheduled for an ultrasound guided core biopsy of the lump. After waiting intensely for five to seven days after the biopsy was performed, the primary care
physician calls Sharon back and confirms that the lump is cancerous, and it appears to be Stage 2 breast cancer.
Sharon, like many other women, never saw the importance of having a clinical breast exam every year. She examined her breast periodically throughout the year, but she always felt like her breasts were just “lumpy all over.” She wasn’t aware that she was at a higher risk for breast cancer and that she needed to be tested to see if she had a gene mutation due to her family history of a female diagnosed on or before the age of 45. She never even mentioned
her family history until the day she filled out the questionnaire for the recent screening mammogram. She did not realize that although she had not been diagnosed with any illnesses, that obesity was a risk factor for breast cancer. Sharon never knew that she should have been having screening tests more frequently due to her risk even before age 40.
One in eight women will be diagnosed with breast cancer in their lifetime. According to the American Cancer Society, the five-year survival rate is greater for women diagnosed with early stage, localized breast cancer (this

is invasive breast cancer and not ductal carcinoma in situ, which is the presence of abnormal cells inside a mild duct in the breast, and this does not include triple negative breast cancer). The Center for Disease Control reports that each year approximately 264,000 women in the United States are diagnosed with breast cancer and 16 percent of those women die from breast cancer. Sixteen percent does not seem like a lot to some until it’s a loved one or even their own prognosis. Breast cancer is the second leading cause of death in women.
Melody has a different story. She is also a 50-year-old African American mother. However, she has been having breast imaging and exams every year since she was 35. Her sister was diagnosed with breast cancer at age 45. Melody has some medical issues that are related to her family history. She has diabetes and high blood pressure, but they are both controlled with medications. Her primary care physician calculated her lifetime risk for breast cancer when she was 35 years old, and Melody had a risk of over 20 percent. She was advised that she should consider clinical breast exams (a breast exam by a doctor) once or twice a year and she was also given the option to have mammograms alternating with MRIs of the breasts each year due to her family history and personal history of having very dense breasts. She also had genetic testing and tested positive for a gene mutation
that increased her risks for breast cancer to over 40 percent by age 70.
Melody had a small lump discovered during her annual physical by her primary care physician. Her primary care physician then ordered “diagnostic imaging” (imaging including mammogram and ultrasound). A small suspicious mass was noted in the breast that had not been present on the mammogram the year prior. The radiologist recommended a biopsy considering the member’s family history and personal history of a gene mutation. The pathology revealed early-stage breast cancer, Stage 1. Melody has a greater prognosis due to the steps that were taken prior to her diagnosis.
I have been a health care provider for more than 25 years, specializing in breast cancer for more than 11 years. I named my business Caretaker’s Heart Speaks because I am a caring individual with a huge heart, and I have to speak out about how we fight breast
cancer! There is a great need in the community for people to be educated on this disease and to be empowered to navigate through the healthcare system effectively to get appropriate screening and monitoring for breast cancer. There is so much work to be done, but it is my passion to do my part in helping people understand how impactful this can be in reducing the number of people who die from breast cancer each year. I am committed to this task, and I take immense joy in joining in the fight to make a difference in this world!
April Woodyard, breast care consultant, is the owner of Caretaker’s Heart Speaks, a breast care consulting business that supports, advocates for and educates women before and after the diagnosis of breast cancer. Visit chsbreastcare.com for more info.

One in eight women will be diagnosed with breast cancer in their lifetime. According to the American Cancer Society, the five-year survival rate is greater for women diagnosed with early stage, localized breast cancer.
MOVING BEYOND PAIN AND HEARTBREAK TO HAPPINESS AND LOVE: ADRIANNA HANNON SHARES THE UPS AND DOWNS ON HER JOURNEY TO MOTHERHOOD
By Elizabeth Mosely-HawkinsAt 15 years old, Adrianna Hannon made a conscious decision that defined how she would respond to life’s challenges well into her adulthood.
The Columbia, South Carolina native began menstruating between nine and 11 years old. Instead of memories playing with her dolls or racing through the backyard with her siblings and friends, Hannon recalled that, at 12 years old, she began experiencing serious menstrual complications.
“I started having really bad pains every time my menstrual cycle would come on. They would be really heavy. I was just miserable,” said Hannon.
To help regulate her infrequent, heavy-flow periods and to reduce the stabbing pains associated with cramps, her family physician placed her on oral contraceptives. To her disappointment, the birth control pills offered her no relief.
In search of answers to ease her pain, Hannon visited an obstetriciangynecologist (OBGYN) at the Medical University of South Carolina in Charleston, South Carolina. The doctor explained to the teen-aged Hannon that she had symptoms of polycystic ovary

syndrome, premenopausal and endometriosis.
“I had lots of scar tissue in my uterus. It was horrible,” she added.
It was then the OBGYN revealed to Hannon and her concerned mother that the diagnoses would likely make it difficult for her to get pregnant.
Hannon became increasingly disappointed and developed a “get over it” mindset. She began to settle on the idea that she would never have kids.
“Okay, I’m going to live my best life. In some facet, I’m going to work with children and be the best of who I am,” she recalls reasoning with herself.
A few years went by and Hannon graduated from Columbia High School. This was a particularly memorable time in her life as she had met her boyfriend, now husband, Jermaine, at a rival basketball game during her senior year.

The two headed to college. Jermaine went to South Carolina State University on a football scholarship and Adrianna was accepted to the College of Charleston. The pair adjusted to college life and to each other well. Hannon, however, could not adapt to her cycles. They were inconsistent or never showed up. And when they did, she said they produced unbearable pain and caused excessive bleeding, much like the flow of urinating while standing.
Her periods disrupted her life. She missed days from class to
nurse her pains and to avoid the potential embarrassment of walking around campus with blood-stained clothes. She could not enjoy simple college experiences like attending campus gatherings, athletic events or parties. So, she again developed the “get over it” mentality and made the difficult choice to leave college at the end of her freshman year.
That same year, doctors tried to persuade her to have a hysterectomy. They were convinced that she could not conceive. She strongly disagreed as she thought that at 17 years old, she was too young to make that
That was the worst experience of my life. Can you imagine being over 20 weeks, carrying this baby that you just know is going to be here within a matter of weeks? Then experiencing a stillborn.Hannon with her family at the beach
decision. Besides, even though the odds were against her, there remained a chance that she could possibly become a mother one day.
At 19, however, her periods just stopped, and so did any thoughts of having a baby. That old mentality showed up again; she “got over it.”
In May 2003, Jermaine and Adrianna married. Jermaine knew the couple would likely not have children and assured Adrianna that he undoubtedly wanted a life with her.
When she first revealed to Jermaine that she would be unable to have kids, he responded saying, “My little swimmers are going to swim.” Adrianna giggled recalling Jermaine’s loving response.
Filled with hope of building a life together, the two moved to Houston, Texas, for Jermaine to begin working on a master’s degree from Texas Southern University. Adrianna was determined to earn her bachelor’s degree, so she enrolled at the university. Life began to move on, until one day, she felt a familiar ache - a sharp abdominal pain. She was confident her period was returning. It did, but then the following month it didn’t.
Jokingly, her husband speculated that she was pregnant. In jest, the couple took a pregnancy test. To their surprise, it was positive. A visit to the doctor at the University of Texas Houston Hospital confirmed her pregnancy.
“With the amount of scar tissue and the number of cysts you have, there is no way you should be
pregnant,” Adrianna remembers the medical tech telling her. Nevertheless, we were excited. However, pregnancy came with several health challenges. At six months, Adrianna was placed on bed rest and was diagnosed with borderline toxemia and gestational diabetes. Later, she would also develop pre-eclampsia. The pregnancy issues were minor in comparison to the joy Adrianna possessed. After all, she was carrying a life. Something she never thought was possible.
The birth of her first child, Abigail, happened in May 2004.
Four years later – and in a new state (Arizona) – the pair was excited to learn of their second natural pregnancy. Again, the couple was shocked by the news, but elated about their expected bundle of joy.
At 25 weeks, their joy morphed to heartbreak. Adrianna suffered a fetal demise, when at one pound, Addison London, was stillborn. The
grief from the loss of her child was devastating. Their sorrow deepened once the family learned about an Arizona law that required a burial for a stillborn fetal over one pound.
“That was the worst experience of my life. Can you imagine being over 20 weeks, carrying this baby that you just know is going to be here within a matter of weeks? Then experiencing a stillborn,” Adrianna rhetorically asked.
Baby Addison was cremated in April 2009.
The family’s grief was comforted seven months later with the discovery of a rainbow pregnancy. The term refers to babies born after the loss of a miscarriage, stillbirth or other types of infant loss.
While carrying the baby, the doctor labeled Adrianna high-risk due to her previous medical history. The physician scheduled a delivery at seven months as a precaution and to reduce the risk of Adrianna losing her baby. While in labor, the baby turned in the womb, making it difficult for the doctor to reach him. Though she’s not sure what happened, Adrianna said the baby had bruises on his forehead and shoulders, though no aides were used to assist the delivery. On July 9, 2010, Hannon's third child entered the world, a son named Jayden.
Three days later, she noticed the composition of his face changed. He had extreme jaundice and was inconsolable. Adrianna, who at the time of the birth, was working toward earning a master’s degree in special education, knew her child
Coming from being told that you cannot have kids and being reminded of my fate with each pain and complication from my periods to getting pregnant – I see now it has all prepared me to be a better parent.

might have developmental delays. She made a mental note that she would monitor him.
The following month, the family moved to Fulton, California. Adrianna became a stay-at -home mom to keep close watch of her son. Over time, Adrianna speculated that he had autism from some of the behaviors he displayed. A few months later, the doctor diagnosed Jayden with Autism Spectrum Disorder.
And then, the Hannons learned they were pregnant again. Collin was born on July 12, 2012. Finally, the baby of Hannon house, Myles, was born on May 3, 2015.
The adult Adrianna, who grew up with the belief that she would never have children, is now the mother of four gifts from God.
Through all her challenges, the pain and even the heartbreak of losing a baby, Adrianna admits in hindsight that it was all worth it.
“Coming from being told that
you cannot have kids and being reminded of my fate with each pain and complication from my periods to getting pregnant – I see now it has all prepared me to be a better parent,” said Adrianna.

Through her trials, Adrianna has discovered that the best approach to dealing with life’s challenges is not “getting over it,” but choosing to understand the lesson that God wants to teach.
Adrianna and her family live in Indiana. Abigail is a freshman at Indiana University -Bloomington, and the boys all attend public school. She also realized her dream of becoming an educator. Adrianna owns the educational consultancy, Ahann On Approach, and serves as an advocate for Autism Spectrum Disorder.
A study by the American Journal of Obstetrics and Gynecology reported that 40 percent of Black women who were told they had Pelvic Inflammatory Disease (PID) actually had endometriosis.”
-Resilient Sisterhood Project

IMPOSTER SYNDROME AND WOMEN OF COLOR
By LaToya JohnsonJoyceRoché has received worldwide recognition for her achievement in the world of business. A published author and a current board member of Macy’s, she has held numerous titles such as president and chief executive officer of Girls Incorporated and the first African American female to serve as vice president for Avon.
Despite the numerous achievements that she has made in corporate America as a woman of color, she gave the following quote
to the Huffington Post in 2019: “The impostor fears had a greater impact on me early in my career. As I entered corporate America, I faced many unknowns. Being a woman of color in business at a time when very few women were in positions of power, I had to learn by trial and error how I was supposed to perform. This made me so afraid of being wrong or ‘looking dumb’ that I stayed quiet in meetings. I wanted to make sure everything I said was perfect before I would

Women of color who experience Imposter Syndrome are feeling it not only as a woman against their male counterparts but also as a minority.
chance saying anything, and often found myself hearing a guy saying what I had been thinking but was too afraid to say. I did learn fairly early on that my being quiet and not voicing opinions only served to create doubts in the minds of others about my abilities. So, I faced the fear and began taking risks to counter any questions about my abilities and me.” This is one example of what it may look like for women of color to experience Imposter Syndrome.
In the first article in this series, we learned that Imposter Syndrome was identified by psychologists Pauline R. Clance and Suzanne A. Imes in 1978 and described as a condition in which individuals suffer from consistent feelings of self-doubt, insecurity and incompetence, despite their qualifications, previous successes and numerous experiences they may have had.
Initially studied in highachieving women, this concept has been applied to various aspects of women and men’s lives over the decades. In addition, Imposter Syndrome is now being researched in specific populations such as high
school students, college students and mothers. In this article, we are going to look at what Imposter Syndrome may look like for women of color.
HOW DOES IMPOSTER SYNDROME AFFECT WOMEN OF COLOR?
Often, women of color at some point in their life will have worn the title of “The First.” Think of Phillis Wheatley, the first Black woman to publish a book in 1770. Maybe Mary Jane Patterson comes to mind as the first Black woman to earn a college degree in 1862. Can one even begin to imagine the pressure
that Dr. Rebecca Crumpler had to go through as the first Black woman to earn a medical degree in 1864? What do you think Charlotte E. Ray felt among what was undoubtedly a room full of white men as she became the first woman to earn a law degree in 1872?
“If they don’t give you a seat at the table, bring a folding chair” is a sentiment constantly stated in today’s culture. However, it is no surprise that Shirley Chisolm coined this phrase as the first Black woman to be elected to Congress in 1968.
Fifty-five years later, women of color are not only bringing a folding chair, but we are also
When walking into spaces in which you do not see yourself represented, it is easy to see how Imposter Syndrome can develop.
bringing several seats and building additional tables. Although the idea of Imposter Syndrome had not come into existence yet, I am sure that these women had bouts of anxiousness, doubt and uncertainty in varying degrees, despite the strong women we know they had to be.
Yes, women collectively have reported higher rates of experiencing Imposter Syndrome. But how Imposter Syndrome is experienced is going to have significant differences when you look at race. Let’s think about it; yes…there are ample studies that show how White Women have reported experiencing Imposter Syndrome. However, what many of these reports fail to mention is that even though they may feel these inadequacies, they still have a level of privilege that women of color will just not have access to.
Women of color who experience Imposter Syndrome are feeling it not only as a woman against their male counterparts but also as a minority. It is almost as if the levels of anxiety, inadequacies and uncertainties are amplified. When walking into “spaces,” White women may typically have to deal with being the few or only woman in the room. Women of color, on the other hand, must not only deal with being the few or only in the room as a woman, but they may also be of the few or only person of color in the room. In an interview given in the article “Why Imposter Syndrome Hits Women and Women
of Colour Harder” (Nance-Nash, 2020), Brian Daniel Norton shares the following quote: “When you experience systemic oppression or are directly or indirectly told your whole life that you are less-than or undeserving of success and you begin to achieve things in a way that goes against a long-standing narrative in the mind, imposter syndrome will occur.” When walking into spaces in which you do not see yourself represented, it is easy to see how Imposter Syndrome can develop.
Unfortunately, Norton’s quote holds some truth as American Society continues to contribute to this problem when looking at the following statistics:
• According to the United States Department of Labor (Roux, 2021), Black women earn 63 cents for every $1 earned by White, non-Hispanic men. Asian women earn 87 cents; White, non-Hispanic women earn 78 cents; American Indian and Alaskan Native women earn 60 cents; and Hispanic women earn 55 cents for every $1 earned by a White, nonHispanic man.
• Black mothers have higher labor force participation at 58.8 percent than mothers of other groups (55.7 percentWhite mothers; 56.4 percentHispanic mothers; 56.8 percentmothers from all other groups), according to a 2021 article from the U.S. Department of Labor.
• Black women make up just one
percent of named executive officers. Currently, there are 44 women who serve as chief executive officers in Fortune 500 companies. Of these 44 women, only five are women of color. Of these five, only two are Black women…Rosalind “Ros” Brewer, chief executive officer of Walgreens Boots Alliance, Inc., and Thasundra Duckett, president and chief executive officer of the Teachers Insurance and Annuity Association (TIAA).
• There has never been a Black woman that has served as governor in the United States. The closest we came was when five women ran in 2022, which were Danielle Allen (Massachusetts); Stacey Abrams (Georgia); Connie Johnson (Oklahoma); Deidre DeJear (Iowa); and Mia McLeod (South Carolina).
Experiencing micro aggressions from fellow colleagues, being on the receiving end of racist and misogynistic remarks and being judged based on stereotypes (e.g., the Angry Black Woman; the “token hire”; being bougie, ghetto, and/ or ratchet, etc.) can cause havoc on one’s psyche even among the strongest woman of color. These are just a few of the societal issues that can cause a woman of color to experience Imposter Syndrome. If left unchecked, it can lead to one’s personal life and serious issues can affect one’s health such as anxiety, stress, insomnia, weight gain and
inability to focus (Nance-Nash, 2020).
WHAT SHOULD WOMEN OF COLOR DO?
In offering suggestions of what women of color should do, I wanted to take a different angle about recommendations. What better way than to hear from well-known and recognized women of color who have shared their struggles with Imposter Syndrome? Here are words of wisdom that we can all consider minimizing to eliminate the characteristics of Imposter Syndrome:
• Justice Sonia Sotomayor – first Latina to serve on the United States Supreme Court: “I’m not a classic impostor-syndrome person because I have that initial insecurity but I’m capable of stepping outside of it and proving to myself it’s wrong.”
• Viola Davis – first Black woman to win the “Triple Crown of Acting” (Academy Award, Emmy Award, and Tony Award): “As Black women, we're always given these seemingly devastating experiences—experiences that could absolutely break us. But what the caterpillar calls the end of the world, the master calls the butterfly. What we do as Black women is take the worst situations and create from that point.”
• First Lady Michelle Obama –first Black woman to serve as First Lady of the United States: “It takes time and maturity and successes under your belt to realize that you’re good enough.”
In the next article in this series, we are going to look at how being a mother can potentially cause feelings of Imposter Syndrome.

LaToya Johnson, Ph.D., is an assistant professor and currently serves as the academic program coordinator for the Family and Consumer Sciences Business/ Multidisciplinary program at South Carolina State University. She has been an educator on the secondary and post-secondary levels for more than 18 years.

Fenessa
BECOMING Shampale
when you have the courage to dismantle the idea of perfection you start living without limitations
stop underestimating your strength
unstitching your insecurities acknowledges that you deserve the chance to embrace who you are

all the flaws all the healing all the pain
love every part of you the only person you need to fall into is yourself
water your garden love every flower growing inside of you you were blooming all along
becoming the woman you've always wanted to be is the most liberating act of self-care
there may be times when you feel lost don't lose yourself laugh dance breathe sing read turn towards the things that nourish your soul
A SECRET:
By Bambi W. GaddistAs I opened my telephone one day in January, I noticed a text from a long-time friend and public health colleague from Washington, DC. We met one another when she served as the HIV/AIDS director of an initiative supported by the Congressional Black Caucus Foundation. We hit it off from the beginning and she still seems like a “sister from another mother.” As I began to read the content of her text, I felt my heart sink for a second and my immediate response was to reach out in a phone call. You know sometimes a text just doesn’t seem like an appropriate response
when someone is experiencing an emotional tsunami. She seemed so strong, and I was witnessing an obvious spirit of strength. I really wanted to console her, but I felt awkward and frankly didn’t want to say the wrong thing. I was grateful that she trusted me enough to confide in me and that felt special. Honestly, I strive to be that person that someone might trust enough to reach out to if they are vulnerable and need unbiased support.
My friend shared news from a very recent doctor’s visit. She sounded bewildered as she disclosed having her annual “gyn” that was “clear” -- only to find a lump during her normal self-breast check less than 30 days later. She’s been diagnosed with aggressive triplenegative breast cancer and was informed that this particular type of cancer has become more prevalent among African American women. Black women have a greater risk of a triple-negative diagnosis, which has a poor prognosis, according to a 2021 news release by Penn Medicine News. According to the new release, triple-negative breast cancers are less likely to be identified through screenings because the women have dense breast tissue. The dense tissue makes it more difficult to identify cancer through screening. It is vital that all women and especially those receiving a diagnosis of “dense breast” commit themselves to checking their breasts routinely.

Her physicians let her know that six months of chemotherapy were required before considering any form of reconstructive surgery. Within days, she and her medical team were orchestrating decisions about radiation therapy, chemotherapy and other life alternating choices. Since her form of breast cancer was highly aggressive or “fast-moving,” the recommended therapies required immediate attention.
I could hear and feel a deep sense of loss as she accepted the fact that her pending vacation to Belize
“He who conceals his disease cannot expect to be cured.”
must be canceled and prayerfully rescheduled for another time.
From the moment we talked about her unexpected diagnosis, I witnessed a metamorphosis. Lisa is “sassy” and always manifested a tenacious and queen-warrior spirit, but this type of optimism was inspiring to say the least. While surfing through my Facebook page a few days later, a post from her page popped up. She had officially
announced her diagnosis to the world or at least to her friends and her friends’ friends. She shared information about the next steps coming from her medical team of two phenomenal oncologists of color. Since that day, I’ve witnessed first-hand how she has transformed her diagnosis into an opportunity to educate anyone willing to listen.
In the days following her “diagnosis,” she made the difficult
The reality we face as caregivers includes the unique challenge of helping clients whose instinct is to ‘run for cover’ only to resurface months later manifesting severe symptoms due to untreated HIV infection.
-Bambi Gaddistdecision to cut her shoulder length curls. Several weeks later, facing the realities of chemotherapy, four “angels” presenting as men from The ELITE Boxing and Fitness Club, hosted a community FU Cancer event where they joined her as she removed the remainder of her hair. During that Instagram moment, she created a platform that could become a pathway for individuals living in fear, shame and anger. I thought, “now this is what taking charge looks like in real time.”
Being a part of Lisa’s life journey before and since her breast cancer diagnosis has been a blessing. I want to be there for her, and she is allowing me to do so. However, it makes me reflect on the more than 40 years I’ve devoted to my personal calling in the arena of HIV/AIDS prevention, intervention and linkage to medical care. I’ve remained focused on my mission of HIV prevention which began in 1986 when I was 32 years of age with

Triple-negative breast cancers are less likely to be identified through screenings because the women have dense breast tissue. The dense tissue makes it more difficult to identify cancer through screening.
-Penn Medicine News
energy to spare. I am now almost 68 years of age (and thirty-six years later) still struggling with an age-old question that remains unresolved in the Black community.
African Americans in our state and throughout the United States remain over-represented in the rate of HIV/AIDS compared to other populations. In South Carolina, African American men make-up 45 percent of new HIV cases and 44 percent of People Living with HIV/AIDS (PLWHA) compared to men of other races. Among women, Black women comprise 19 percent of new HIV cases and 14 percent of women living with HIV/AIDS. Young Black gay men of color, ages 18-29 years of age, represent the majority of new cases, while African Americans over the age of 50 comprise the majority of PLWHA.
As former CEO of the South Carolina HIV Council/ Wright Wellness Center, the first
community-based, alternative HIV/ STD testing site in South Carolina, I keep asking myself, “how is it that after 40-plus years of being so disproportionately over-represented in HIV statistics do we rarely focus on this health disparity?” Most Black citizens rarely acknowledge this epidemic outside of World AIDS Day, National Black HIV/ AIDS Awareness Day and/or National Women and Girls HIV/ AIDS Awareness Month, if that. Ask yourself, when was the last time HIV was a topic of discussion or concern within your home, church, mosque or social circle?
It brought to mind the Ethiopian proverb that says, “He that conceals his disease cannot expect to be cured.” What a profound and compelling statement, as I reflect on 40-plus years serving clients that experienced an unexpected HIV diagnosis. Experiencing family and community stigma, coupled with the threat of losing a job or
spiritual/social support are other traumatic realities after disclosing one’s HIV status. Far too often clients retreated after the initial HIV diagnosis and some refused medical care, while others resurfaced days, weeks, months and sometimes years after they first tested positive for HIV. Even when case managers were successful in linking clients to medical care (a “health home”), many struggled staying in care. The reality we face as caregivers includes the unique challenge of helping clients whose instinct is to “run for cover” only to resurface months later manifesting severe symptoms due to untreated HIV infection.
Educating oneself and making HIV testing an annual part of prevention are critically important decisions. Linking into HIV medical care and treatment soon after diagnosis can help forecast better health outcomes. Until there’s a cure, one thing is certain, biomedical advances in treatment

means HIV is no longer a death sentence. Whether the health condition is HIV, diabetes, high blood pressure, cancer, depression or any health reality we might face, overcoming fear and taking control must be our quest. We must fight like Lisa and others to avoid going into a state of “dissonance” or denial. Listening to untrained individuals who received their medical degree “from the streets” can delay access to life-saving information and treatment. Finally, “waiting to see” and trying out “fad” cures can cost us our quality of life or our lives.
Researchers have credible data to support our contention that treating one’s illness in secrecy can have devastating outcomes. Hiding our medicine, lying about why we missed work and excessive worrying about rejection from our religious or social support circles are merely examples of the toll hiding takes on our mental health and the body’s ability to heal. Let’s not forget the trauma experienced when a loved one passes unexpectedly with no warning signs and/or no one who can explain the “why” behind a family member’s early departure from this earth.
In closing, by no means am I suggesting that anyone is obligated to divulge everything to everybody about their private health information. Everyone deserves privacy. I am suggesting that everyone needs a “safe space” to process an unanticipated diagnosis. Our community must confront our
ambivalence and any contradictory ideas about how best to confront unforeseen illness. The Black community historically sought to take care of one another. When did we decide to stop caring for others based on a diagnosis?
Now more than ever, our community can and must create a new legacy of courage. Not one steeped in fear, mistrust and avoidance behavior. We must demonstrate for the next generation how Black families respond to unforeseen health conditions and unplanned diagnoses. As Black southerners, we must not become part of the historic legacy of health care denial or ever wage war against our own community based on a health diagnosis.
We must mobilize our minds and community to create spaces within our homes, faith communities and states where people who desperately need access to confidential and caring support find shelter. Behaviors are learned and ignoring symptoms is taught. Lack of insurance coverage should not be the deciding factor in whether we seek medical care and treatment. Let us reimagine what our community would look like if health care access was part of our political and religious platforms. We will stand hand in hand with faith communities and fight for Medicaid expansion because healthcare access and equity are a human right. Faith communities would use their unique voice and play a vital role in promoting
health care advocacy, creating support systems for an individual or family healing after diagnosis and demonstrating to the world what “Good Samaritans” truly look like. Thank you, Lisa, and so many of my sheroes and heroes that are paving the way.
Bambi W. Gaddist, DrPH., is a published author and consults with a host of national and local organizations including the Centers for Disease Control and Prevention. She is cofounder and former CEO of the South Carolina HIV Council. She has committed the past 40 years of her professional life working in the areas of human sexuality with a specific focus on HIV/AIDS/STI community level mobilization, behavioral intervention and research, technical assistance/capacity building and the elimination of other health disparities.

SUGAR, SUGAR, SUGAR… THE DANGERS OF CONSUMING TOO MUCH
By Carmen ThompsonAccording to the American Heart Association’s website, American adults consume an average of 17 teaspoons of added sugar every day, which is more than two to three times the recommended amount for men and women. This adds up to approximately 60 pounds of added sugar consumed annually – that’s six, 10-pound bowling balls, folks!
The numbers are even worse for children and young adults aged two to 19 years of age, who consume 16 teaspoons of added sugar per day. American kids consume 66 grams per day, equaling more than 53 pounds of added sugar per year.
American adults consume an average of 17 teaspoons of added sugar every day, which is more than two to three times the recommended amount for men and women. This adds up to approximately 60 pounds of added sugar consumed annually.

Overall, Americans consume a lot of added sugar from beverages to convenience foods, to yogurt and sandwiches. What can we do? Read the nutrition facts label for added sugar grams. The American Heart Association recommends no more than 36 grams of added sugar per day for men and less than 25 grams per day for women.
So how can this work? Try diluting your sugar drinks with half water; add berries, cucumbers or citrus fruits. Beverages lead the way when it comes to sugar content, from soft drinks to juices and energy drinks, to coffee and tea. Cut back
The United States Department of Agriculture Dietary Guidelines suggest for healthy women to consume at least 25 grams per day of fiber and men 30 grams per day.
on the amount you drink daily by adding at least one 16-ounce bottle of water to your day.
Reading the Nutrition Facts Label can help identify how much added sugar is in food products. The information includes the serving size, carbohydrates and calories in bold letters. Under total carbohydrates, dietary fiber, total sugars and added sugars are listed. Fiber is needed to help with digestion, fullness, elimination of waste and may reduce risk of some chronic diseases. The United States Department of Agriculture Dietary Guidelines suggest for healthy women to consume at least 25 grams per day of fiber and men 30 grams per day. Eating one cup of cooked beans and two to three servings of fruit can provide 25 grams of fiber.
According to the Food and Drug Administration, total sugars include sugars naturally present in many nutritious foods and beverages. This includes sugar in milk and fruits as well as added sugars which may be in the

products. Added sugars include sugars that are added during the processing of foods, such as sugars from syrups and honey and sugars from concentrated fruit or vegetable juices. An intake of more than 25 to 36 grams of total sugars can lead to weight gain, make individuals feel sluggish and increase chances of developing chronic diseases.
As stated earlier, many Americans already consume more than the recommended amount of added sugars. If you would like to change this, speak with your primary care provider to let them know of your plans and talk to them about incorporating daily exercise. Some medications are based on weight for dosage; therefore, any change in weight status should be given to your primary care provider to maintain a continuum of care. As you gradually reduce the intake of added sugars, monitor how you feel as you make this change, maintain the recommended intake of fiber and use MyPlate.gov as a guide for dietary intake.
Carmen Thompson, MS, RDN, LD, has worked as a registered dietician nutritionist (RDN) for more than 20 years. She is currently an assistant professor at South Carolina State University, where she is the director of the Didactic Program in Dietetics.

PARENTING A CHILD WITH SPECIAL NEEDS: “AUTISM IS NOT SOMETHING TO BE FIXED”
By Megan FreemanSarah J. Riddle, 35, is the mother of three boys and her first-born, three-year-old, August (Auggie), is autistic. She explains that raising three young children is challenging enough, but she and her husband, Christopher, put in
extra work to care for a child with special needs.
Autism Spectrum Disorder (ASD) refers to a broad range of conditions characterized by challenges with social skills, repetitive behaviors and speech and non-verbal communication.
Riddle said Auggie was diagnosed with autism after turning two through the Sense to Know study at Duke Health. “The biggest sign was Auggie still not saying any words at two-years-old and making very little eye contact. He is a pandemic baby, and I just thought he had a personality that he liked to keep to himself, but it turns out they were early signs of autism,” Riddle said. “Some of the positive early signs were knowing all his shapes, letters and numbers before he was two.”
As a mother, Riddle said originally, she did not feel much of anything and nothing changed about her finding that information out. “Now as I have had a year to process it, I am worried for his future, about what kind of support he will need. He still is not talking, which makes communication more difficult, although he is an excellent non-verbal communicator,” Riddle said.
According to the Centers for Disease Control, autism affects an
estimated one in 36 children in the United States. After his diagnosis, Riddle and her husband had to find him specialists and change his care. She said they learned a lot from Auggie’s speech and occupational therapists. For example, at home, they have learned to slow down and make sure they have Auggie’s attention before trying to talk.
“He is an autistic three-year-old, but he is also very much a typical three-year-old in terms of pushing boundaries and getting into mischief, but he is very practical and likes to know his routines and rules.”
The Autism Society said ASD typically appears during early childhood and the autism experience is different for everyone. While there is no known single cause of the condition, early diagnosis helps a person receive resources and support to live fully.
Riddle is also the mother of one-year-old twin boys, Miles and Ethan. Riddle worries about the twins because in Auggie’s case, he had very typical development and then went through a regression. “His regression was around 13 months, and the twins have passed that threshold, but autism is a spectrum, and they might still be autistic, even though right now they are talking and making eye
The biggest sign was Auggie still not saying any words at two-yearsold and making very little eye contact. He is a pandemic baby, and I just thought he had a personality that he liked to keep to himself, but it turns out they were early signs of autism.
Autism is not something to be fixed; those affected by autism have a different way of thinking and need extra assistance with functioning in our world. Early intervention is key. Starting play therapies early can hopefully make a difference down the road.
contact and seemingly just much more interested in other people than Auggie ever was,” Riddle said.
She said Auggie loves to study and likes to do his alphabet and numbers the most, but mostly, he loves reading books.
“He loves watching television, listening to music and swinging at the playground," Riddle said. Auggie’s brothers easily annoy him because they want to play with whatever he is playing with. "They also eat his snacks and mess up his toys, which he really dislikes." Although Auggie is agitated by many things his brothers do, Riddle thinks they may eventually have a great relationship. “I have seen
Auggie stroking their hair in a loving way, so I think one day they might become friends.”
Riddle wants to encourage mothers with young kids who have autism. “The road will be challenging, but you can do it. As a parent, you know your kid best and as long as you are treating them with respect and compassion, you can handle anything,” Riddle said.

“Autism is not something to be fixed; those affected by autism have a different way of thinking and need extra assistance with functioning in our world. Early intervention is key. Starting play therapies early can hopefully make a difference down the road.”

COULD IT BE SCIATICA? UNDERSTANDING THE SYMPTOMS AND TREATMENTS
Sciatica is a medical condition that affects the sciatic nerve, which is the longest nerve in the human body. The sciatic nerve runs from the lower back through the hips, buttocks and down to the legs, providing sensation and control to the lower body. Sciatica occurs when there is compression or irritation of the sciatic nerve, leading to pain, tingling and numbness in the affected areas.
WHAT CAUSES SCIATICA?
Sciatica can be caused by a variety of factors. The most common cause of sciatica is a herniated or bulging disc in the spine. The discs in normal condition act as cushions between the vertebrae. When a disc bulges or herniates because of damage or degeneration with age, it can press on the sciatic nerve, causing pain and discomfort.
Other causes of sciatica include spinal stenosis, which is the narrowing of the spinal canal that contains the spinal cord and nerves, and it puts pressure on the spinal cord or nerves causing sciatica symptoms.
Another cause is degenerative disc disease, which is the breakdown of the discs between the vertebrae. As the discs degenerate, they can lose their ability to act as shock absorbers, and the vertebrae can rub against each other, causing pain and inflammation in the surrounding nerves.
Spondylolisthesis, which is the slipping of one vertebra over another, can put pressure on the surrounding nerves, including the sciatic nerve causing sciatic symptoms. A variety of factors such as injury, degeneration or genetics
can make this happen.
WHAT ARE SOME SYMPTOMS OF SCIATICA?
The primary symptom of sciatica is pain, which can range from mild to severe. The pain is usually felt in the lower back, buttocks and down the back of the leg. Some people may experience a sharp, shooting pain that makes it difficult to move. Others may feel a constant, dull ache that worsens with movement. In addition to pain, sciatica can also cause tingling, numbness and weakness in the affected leg.
WHAT DOES SCIATICA PAIN FEEL LIKE?
Sciatica pain can feel like a variety of sensations, depending on the severity and location of the compression on the sciatic nerve. The pain can be sharp, shooting or burning, and it is often felt in the lower back, buttocks and down the back of the leg. Some people may experience a pins-andneedles sensation or numbness in the affected leg. Others may feel weakness or a loss of control in their legs, making it difficult to walk or stand.
DOES SCIATICA OCCUR SUDDENLY OR DOES IT DEVELOP OVER TIME?
Sciatica can occur suddenly or develop over time. In some cases, the condition may be triggered by an injury or accident. Other times, it may develop gradually over time due to wear and tear on the spine or as a result of degenerative changes.
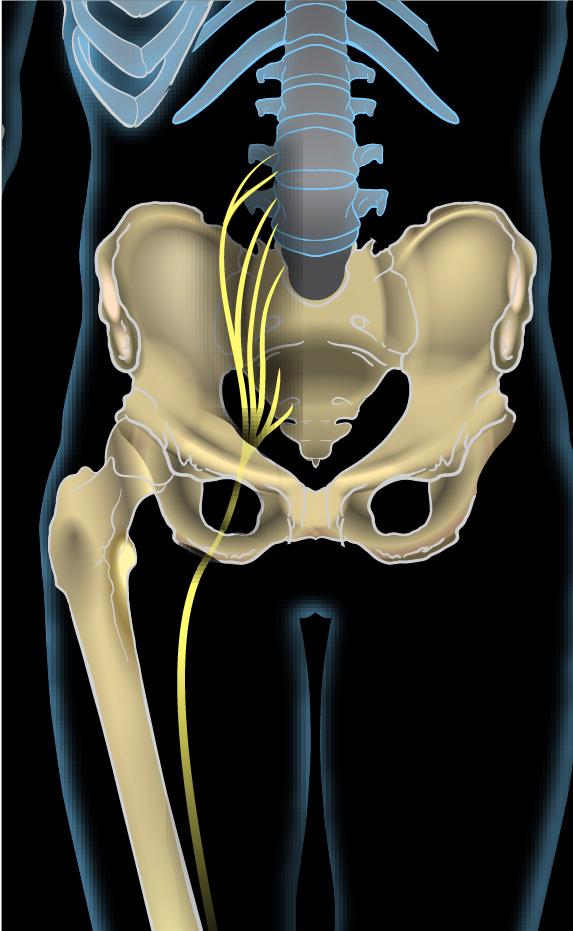
WHAT ARE THE RISK FACTORS FOR SCIATICA?
Several factors can increase the risk of developing sciatica. These include age, as the risk of developing sciatica increases with age, being overweight or obese, having a sedentary lifestyle, smoking, which can lead to decreased blood flow and oxygen to the spine, and having a job that involves heavy lifting or extended periods of sitting.
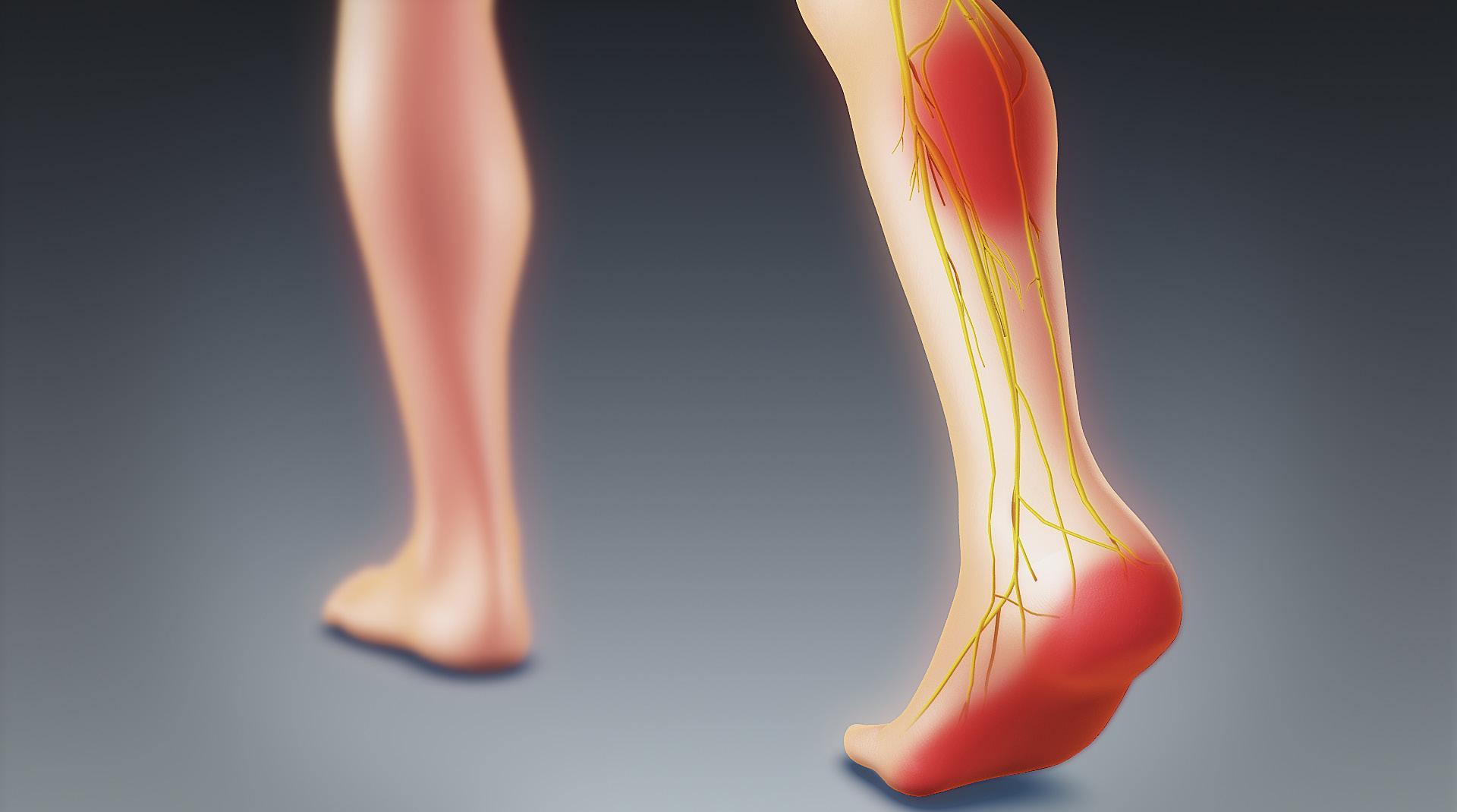
HOW IS SCIATICA DIAGNOSED?
Diagnosing sciatica typically involves a physical examination and a review of the patient's medical history. The doctor may also order imaging tests such as an MRI or CT scan to evaluate the spine and look for any abnormalities or compression on the sciatic nerve. In some cases, electromyography (EMG) or nerve conduction studies may be ordered to evaluate nerve function.
WHAT ARE TREATMENTS FOR SCIATICA?
The treatment for sciatica depends on the underlying cause of the condition. In many cases, sciatica can be treated with conservative measures such as rest, ice and over-the-counter pain medications. Physical therapy and exercise may also be recommended to improve flexibility and strength in the affected area. If conservative treatments do not provide relief, more advanced treatments such as steroid injections or surgery may be recommended.
Alternative and complementary treatments including acupuncture,
chiropractic care, massage therapy and herbal supplements can also work for sciatica. While these treatments may offer some relief from sciatica symptoms, their effectiveness varies. It is important to discuss alternative treatments with a healthcare professional before trying them to know of any potential risks or side effects.
HOW CAN YOU REDUCE THE RISK OF SCIATICA?
Several steps can be taken to reduce the risk of developing sciatica.
• Maintaining good posture and practicing proper lifting techniques can help reduce strain on the back and prevent injuries.
• Exercising and stretching can also help improve flexibility and strengthen the muscles in the back and legs.
• Maintaining a healthy weight can also help reduce pressure on the spine and decrease the
risk of developing sciatica.
CAN SCIATICA BE PREVENTED?
While sciatica cannot always be prevented, some steps can be taken to reduce the risk of developing the condition. As already mentioned, maintaining a healthy weight, practicing good posture and staying physically active can all help reduce risks.
If you have a job that involves heavy lifting or extended periods of sitting, it is important to take breaks and stretch regularly to reduce the strain on your back.
If you are experiencing symptoms of sciatica, it is important to seek medical attention to determine the underlying cause and explore treatment options that can help relieve your pain and improve your quality of life.
THE DANGERS OF HAVING VISCERAL OR BELLY FAT

Visceral fat, also known as belly fat or abdominal fat, is the type of fat that accumulates around the abdomen and is stored within the abdominal cavity. Unlike subcutaneous fat, which is stored beneath the skin and can be pinched, visceral fat is stored deep within the body, surrounding vital organs such as the liver, pancreas and intestines. Although some amount of visceral fat is necessary to cushion and protect the organs, excess visceral fat can be dangerous and has been linked to various health problems.
DANGERS OF VISCERAL FAT
Let’s dive deeper and explore what dangers excessive visceral fat can cause to your health.
Type 2 Diabetes. Visceral fat produces hormones and other chemicals that can interfere with insulin production, leading to insulin resistance, a precursor to Type 2 diabetes. Insulin resistance occurs when the body's cells become resistant to the effects of insulin, a hormone that regulates blood sugar levels, causing high blood sugar levels. Cardiovascular Disease. Excess visceral fat increases your risk of heart disease and stroke by producing inflammatory chemicals that can damage blood vessels. These inflammatory chemicals are also responsible for increasing blood pressure and promoting the formation of blood clots.
High Blood Pressure. When visceral fat accumulates around the abdomen, it compresses blood vessels, leading to high blood pressure. High blood pressure increases the risk of heart disease and stroke by putting additional stress on the heart and blood vessels.
Sleep Apnea. Belly fat can cause sleep apnea, a condition where breathing repeatedly stops and starts during sleep, leading to poor sleep quality. Sleep apnea has been linked to several health problems, including high blood pressure, heart disease and stroke.
Certain Cancers. Studies have shown a link between excess visceral fat and an increased risk of colon, breast and pancreatic cancers. The exact mechanism behind
this link is not yet clear, but it is believed that visceral fat produces hormones and other chemicals that promote cancer growth.
Now that we have understood the dangers of visceral fat, let's look at some exercises that can help reduce it.
EXERCISES TO REDUCE VISCERAL FAT

Planks. Planks are a great exercise to target your core muscles and help reduce belly fat. To do a plank, get into a push-up position, but instead of lowering your body, hold it in a straight line from your head to your toes. Engage your core muscles, breathe deeply and hold for as long as you can. Repeat for three sets.
Bicycle Crunches. Bicycle crunches are a variation of the traditional crunch that targets your oblique muscles, which are located on the sides of your abdomen. To perform a bicycle crunch, lie on your back, put your hands behind your head and budge your knees. Straighten your left leg while raising your shoulders off the floor and bring your left elbow to your right knee. Repeat on the other side, alternating for three sets.
Mountain Climbers. Mountain climbers are a high-intensity exercise that works your entire body, including your abdominal muscles. To do mountain climbers, get into a push-up position and bring one knee toward your chest, then switch legs in a running motion. Continue alternating for 30 seconds, rest for 10 seconds and repeat for three sets.

Russian Twists. Russian twists target your oblique muscles and help tone your core. Sit on the floor with your feet flat on the floor and your knees bent to perform Russian twists.
Lift your feet off the ground while sloping your back slightly. With both hands holding a weight or a medicine ball, turn your torso to the right until the weight touches the
ground. Twist to the left, touching the weight to the ground on the opposite side. Repeat for three sets. Burpees. Burpees are a full-body exercise that can help you burn calories and reduce belly fat. Start in a standing position and lower your body into a squat with your hands on the floor to perform a burpee. Bring your feet back to the squat position by kicking them into the push-up position. Stand up and jump as high as you can, then repeat for three sets.
These exercises, combined with a healthy diet, can help you reduce belly fat and improve your overall health. It's crucial to keep in mind that decreasing fat from a specific location of the body, or "spot reduction," is not achievable. To reduce visceral fat, you need to reduce your overall body fat percentage by engaging in regular exercise and maintaining a healthy diet.


SOME LIFESTYLE TIPS TO REDUCE VISCERAL FAT
In addition to exercise and diet, there are other lifestyle changes you can make to reduce visceral fat. Here are some tips: Get enough sleep. A rise in abdominal fat has been associated with insufficient sleep. Aim for seven to eight hours of sleep per night to reduce your risk of visceral fat accumulation. Manage stress. Chronic stress has been linked to an increase in belly fat. To assist in relieving stress, try stress-relieving exercises like deep breathing, yoga or meditation.
Avoid sugary drinks. Sugary drinks, including soda and juice, might cause the accumulation of belly fat. Choose water or unsweetened beverages instead.
Eat more fiber. Fiber-rich foods such as fruits, vegetables and whole grains can help you feel fuller for longer, reducing your overall calorie intake and helping to reduce belly fat.
Strength train. Strength training exercises, such as weightlifting, can help you build muscle, which can increase your metabolism and help you burn more calories. Aim for twice a week or more of strength training.
Visceral fat is a dangerous type of fat that can lead to various health problems such as Type 2 diabetes, cardiovascular disease, high blood pressure, sleep apnea and certain cancers. Engaging in regular exercise, maintaining a healthy diet and making lifestyle changes, such as getting enough sleep, managing stress and strength training, can help reduce visceral fat and improve your overall health. Remember to consult with a healthcare professional before starting any exercise program or making significant lifestyle changes.
DISCLAIMER:
This content is only general information and does not substitute for a qualified medical opinion. Always consult your doctor or a specialist for any further information.
DID YOU KNOW



PrEP can be about 99% e ective in preventing HIV?*