3 minute read
Minimally Invasive Gastrointestinal Surgery: Anthony’s Story
In 2015, Anthony Moriva, an otherwise healthy and active individual, began to struggle with shortness of breath. Doctors in his hometown determined that a very large paraesophageal hernia was compressing his lungs and contributing to his shortness of breath. He underwent a minimally invasive surgery to repair his hernia in 2015.
Following surgery, Tony did well for many years. However, in 2018 he began noticing problems when he would eat and drink. He was unable to eat normally and had to lie down to allow food to pass through his system. Tony was experiencing severe abdominal pain and chest pain if he was not extremely careful with what and how much he ate.
Tony’s primary care physician referred him for an upper endoscopy to determine the cause of his abdominal pain and nausea. He was subsequently diagnosed with massive recurrent paraesophageal hernia with near-total intrathoracic stomach and transverse colon consistent with a recurrent type IV paraesophageal hernia. Tony met a few surgeons closer to home to discuss reoperative repair, however they felt that the surgery he required was too complex and referred him to Jon Gould, MD, MBA. Per Tony, the referring surgeon claimed Dr. Gould to be “the best in the state.”
Tony’s journey wasn’t an easy one. While waiting for his scheduled surgery, he was seen in the emergency room close to home for severe abdominal pain and vomiting. A CT scan was performed and revealed that his incarcerated stomach was dilated and fluid-filled, and that he was suffering from gastric organo-axial volvulus. Tony’s scheduled surgery was moved to an earlier date. On January 28, 2022, Tony underwent a laparoscopic repair of a recurrent paraesophageal hernia with mesh, and reoperative Toupet partial fundoplication. Dr. Gould, who performed the surgery, noted that, “This was an unusual recurrence. Tony had a hole in the left side of his diaphragm, and rather than herniating into the mediastinum, the stomach and colon were trapped in his left hemi-thorax. I had to get creative and perform a traditional reconstruction of the hiatus and then primarily repair the large left-sided hole in his diaphragm. I used a large piece of synthetic mesh to buttress my left-sided repair and reinforce the hiatus at the same time. We meticulously sutured this mesh into place.”
Although Tony’s path to surgery has been “a roller coaster ride,” he is incredibly grateful to Dr. Gould for the positive difference this surgery has made in his life. Tony even has fond memories of his hospital stay in the Center for Advanced Care. Tony is thankful to everyone who has been a part of his care, throughout his journey to surgery - Dr. Gould, Abigail (Abby) Schroeder, PA-C, who he states, “has been the best,” the OR staff, and all of his nursing staff as well as the administrative staff in the office. When asked if he was happy that he decided to undergo this surgery, Tony’s response was “No doubt, it has made an amazing difference in the way I feel and what I can do today.” Tony has restarted his daily walks and looks forward to being his active self once more.
Tony has since referred at least three other people to Froedtert for medical care. He believes in the quality of the care he received at Froedtert and MCW but overall feels that, “Not only Dr. Gould, but all surgeons doing the things they do, are nothing short of amazing.”

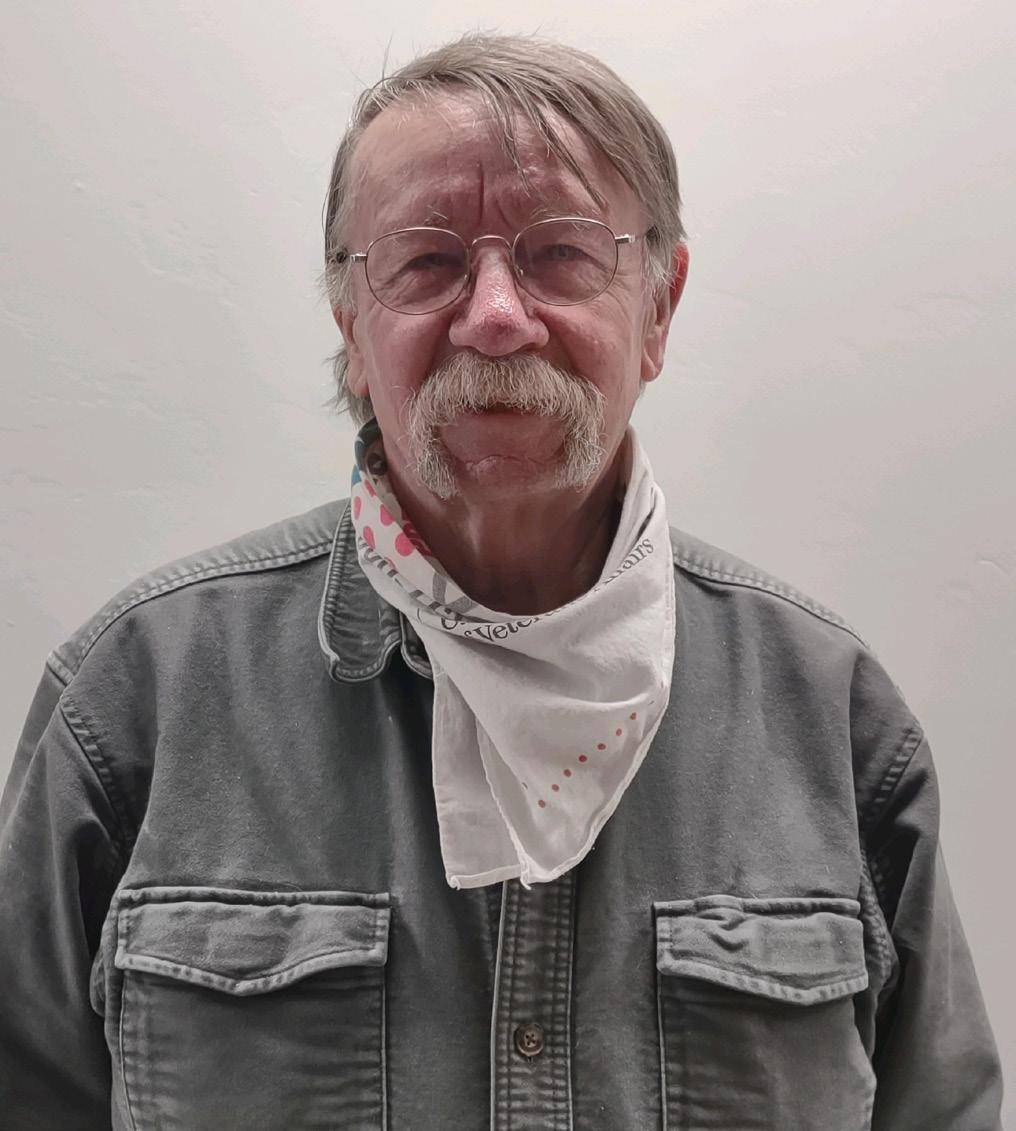
Anthony Moriva.
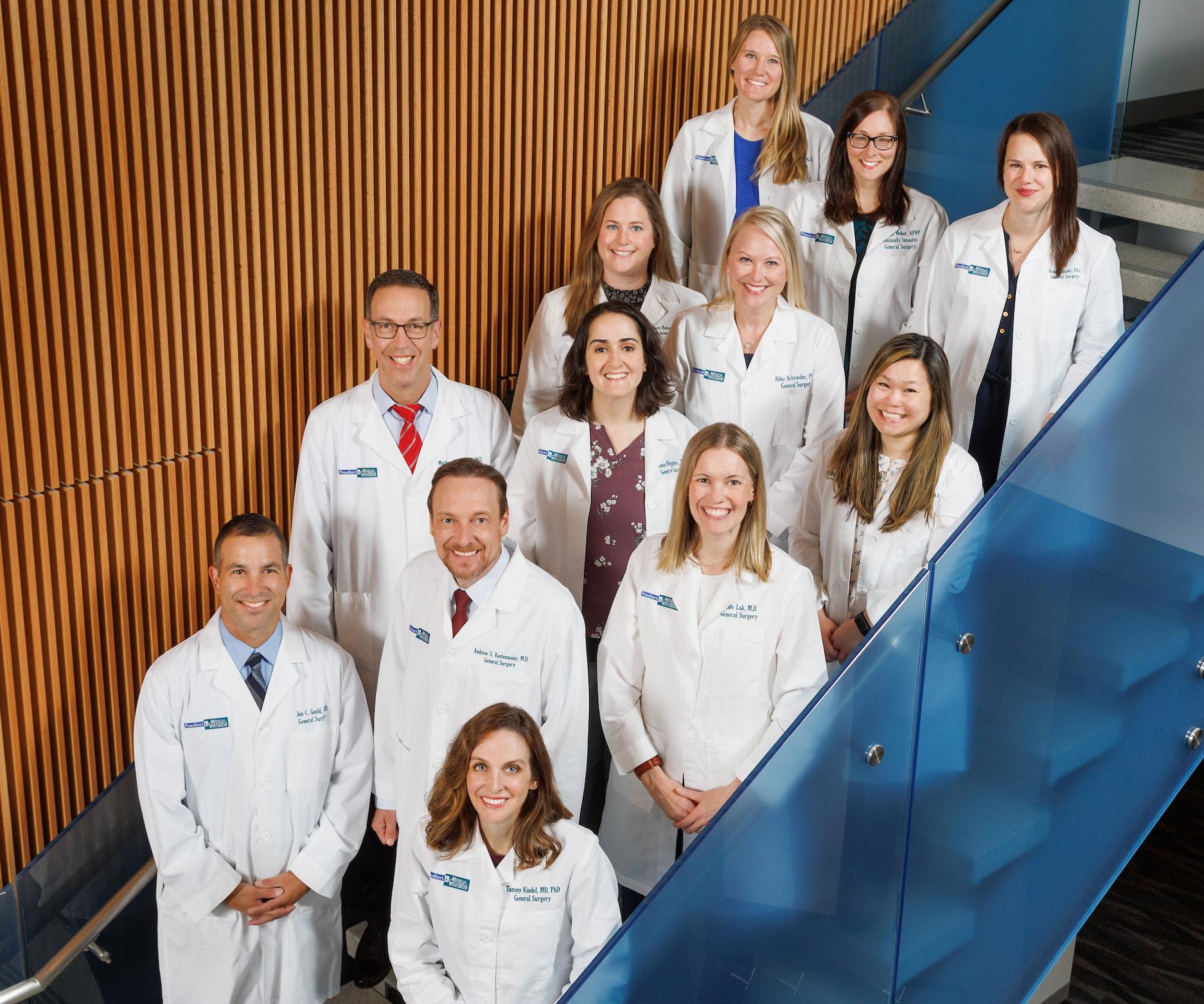
Division of Minimally Invasive & Gastrointestinal Surgery Faculty and APPs. From top left: APPS Kristen Sircher, Michelle Weber, Anna Hausler, Courtney Hanson, Abby Schroeder; Drs. Wen Hui Tan, Matthew Goldblatt, Rana Higgins, Kathleen Lak, Andrew Kastenmeier, Jon Gould, Tammy Kindel. (Not pictured: Dr. Philip Redlich.)









