MAY 2024 Official Publication of SDCMS ‘THE HEART OF SDCMS’ CELEBRATES 20 YEARS OF SERVICE JENNIPHER OHMSTEDE 2004 2024


67th Annual Postgraduate Symposium FAMILY MEDICINE UPDATE 2024 SAN DIEGO ACADEMY OF FAMILY PHYSICIANS SYMPOSIUM PRESENTS 619.540.6307 | sbazzo@sandiegoafp.org www.sandiegoafp.org JUNE 28–30 Paradise Point Resort, San Diego, CA REGISTER TODAY!
Editor: James Santiago Grisolia, MD
Editorial Board: James Santiago Grisolia, MD; David E.J. Bazzo, MD; William T-C Tseng, MD; Holly B. Yang, MD, MSHPEd, HMDC, FACP, FAAHPM
Marketing & Production Manager: Jennifer Rohr
Art Director: Lisa Williams
Copy Editor: Adam Elder
OFFICERS
President: Nicholas (dr. Nick) J. Yphantides, MD, MPH
President–Elect: Steve H. Koh, MD
Secretary: Preeti S. Mehta, MD
Treasurer: Maria T. Carriedo-Ceniceros, MD
Immediate Past President: Toluwalase (Lase) A. Ajayi, MD
GEOGRAPHIC DIRECTORS
East County #1: Catherine A. Uchino, MD
Hillcrest #1: Kyle P. Edmonds, MD
Hillcrest #2: Stephen R. Hayden, MD (Delegation Chair) Kearny Mesa #1: Anthony E. Magit, MD, MPH Kearny Mesa #2: Dustin H. Wailes, MD
La Jolla #1: Karrar H. Ali, DO, MPH (Board Representative to the Executive Committee) La Jolla #2: David E.J. Bazzo, MD, FAAFP
La Jolla #3: Sonia L. Ramamoorthy, MD, FACS, FASCRS
North County #1: Arlene J. Morales, MD North County #2: Christopher M. Bergeron, MD, FACS
North County #3: Nina Chaya, MD
South Bay #1: Paul J. Manos, DO
South Bay #2: Latisa S. Carson, MD
AT–LARGE DIRECTORS
#1: Rakesh R. Patel, MD, FAAFP, MBA (Board Representative to the Executive Committee) #2: Kelly C. Motadel, MD, MPH #3: Irineo (Reno) D. Tiangco, MD #4: Miranda R. Sonneborn, MD #5: Daniel Klaristenfeld, MD #6: Alexander K. Quick, MD
#7: Karl E. Steinberg, MD, FAAFP
#8: Alejandra Postlethwaite, MD
ADDITIONAL VOTING DIRECTORS
Young Physician: Emily A. Nagler, MD
Resident: Alexandra O. Kursinskis, MD
Retired Physician: Mitsuo Tomita, MD
Medical Student: Kenya Ochoa
CMA OFFICERS AND TRUSTEES
Immediate Past President: Robert E. Wailes, MD
Trustee: William T–C Tseng, MD, MPH
Trustee: Sergio R. Flores, MD
Trustee: Timothy A. Murphy, MD
AMA DELEGATES AND ALTERNATE DELEGATES
District I: Mihir Y. Parikh, MD
District I Alternate: William T–C Tseng, MD, MPH
At–Large: Albert Ray, MD
At–Large: Robert E. Hertzka, MD
At–Large: Theodore M. Mazer, MD
At–Large: Kyle P. Edmonds, MD
At–Large: Holly B. Yang, MD, MSHPEd, HMDC, FACP, FAAHPM
At–Large: David E.J. Bazzo, MD, FAAFP
At–Large: Sergio R. Flores, MD
At–Large Alternate: Bing Pao, MD
CMA DELEGATES
District I: Steven L.W. Chen, MD, FACS, MBA
District I: Vikant Gulati, MD
District I: Quinn Lippman, MD
District I: Eric L. Rafla-Yuan, MD
District I: Ran Regev, MD
District I: Kosala Samarasinghe, MD
District I: Thomas J. Savides, MD
District I: James H. Schultz, MD, MBA, FAAFP, FAWM, DiMM
District I: Mark W. Sornson, MD
District I: Wynnshang (Wayne) C. Sun, MD
District I: Patrick A. Tellez, MD, MHSA, MPH
District I: Randy J. Young, MD
RFS Delegate: David J. Savage, MD
Opinions expressed by authors are their own and not necessarily those of SanDiegoPhysician or SDCMS. SanDiegoPhysicianreserves the right to edit all contributions for clarity and length as well as to reject any material submitted. Not responsible for unsolicited manuscripts. Advertising rates and information sent upon request. Acceptance of advertising in SanDiegoPhysicianin no way constitutes approval or endorsement by SDCMS of products or services advertised. SanDiegoPhysicianand SDCMS reserve the right to reject any advertising. Address all editorial communications to Editor@SDCMS.org. All advertising inquiries can be sent to DPebdani@SDCMS.org. SanDiegoPhysicianis published monthly on the first of the month. Subscription rates are $35.00 per year. For subscriptions, email Editor@SDCMS.org. [San Diego County Medical Society (SDCMS) Printed in the U.S.A.]
4

Jennipher Ohmstede, ‘The Heart of SDCMS,’ Celebrates 20 Years of Service to San Diego’s Physicians By Kevin Spillane
DEPARTMENTS
2 Briefly Noted: Advocacy • SDCMS
8 $15 Billion Win for Physicians on Prior Authorization By Kevin B. O’Reilly
10 San Diego Physicians Join CMA’s Annual Legislative Advocacy Day By Paul Hegyi


12
Newsom Offers a Compromise to Protect Indoor Workers From Heat By Samantha Young
14 I’m an Autistic Doctor. Here’s How to Improve Care for Autistic Patients By Thomas Pineo, DO
16
Medical Providers Are Still Grappling With UnitedHealth Cyberattack By Samantha Liss
17
Multiple Sclerosis Predicted by Autoantibody Signature By Judy George
18
Screen Your Gut, Save Your Butt By Adama Dyoniziak 20
Classifieds
SAN DIEGOPHYSICIAN.ORG 1
10 Contents VOLUME 111, NUMBER 5
FEATURE
MAY
Hertzka and Hegyi Lead Medical Students on Whirlwind Tour of State Capitol
NOT TO BE FOOLED, THOUGH ONE OF THEM TRIED, SDCMS PAST PRESIDENT AND legislative committee chair Robert Hertzka and SDCMS CEO Paul Hegyi accompanied six medical students on a whirlwind tour of Sacramento on April Fool’s Day, including meetings with 11 legislative offices and several more at the California Medical Association. Attending were first-year medical students Kenya Ochoa, Anahi Ibarra, Sahana Kumar, Lohita Kollipara, Ben Liebman, and Andres Morales.
The group met with Assemblymembers Jacqui Irwin, Blanca Pacheco, Chris Ward, Dr. Jasmeet Bains, Esmeralda Soria, and Dr. Akilah Weber, as well as State Senators Josh Becker and Monique Limon, and the staff of State Senators Toni Atkins and Catherine Blakespear. The students also met with Lupe Alonzo-Diaz, president and CEO of Physicians for a Healthy California; Stuart Thompson, CMA’s senior vice president of government relations; and Jodi Hicks, CEO of California Planned Parenthood — the highlight of the trip.


2 MAY 2024
ADVOCACY
Above: Left to right: Anahi Ibarra, Andres Morales, Benjamin Liebman, Lohita Kollipara, Robert Hertzka, MD, Assemblymember Jacqui Irwin, Kenya Ochoa, Sahana Kumar, and Paul Hegyi.
San Diego Physicians Catch the Aloha Spirit During SDCMS Mixer at Bali Hai
MORE THAN ONE HUNDRED PEOPLE
enjoyed the San Diego County Medical Society’s “Aloha” mixer held at a San Diego landmark, the Bali Hai Restaurant, in late March. Physicians, spouses, and significant others feasted on delicious complimentary pu pu platters, imbibed the establishment’s legendary Mai Tais and took in one of the most beautiful views of the city of San Diego and its bay.

SDCMS President Nicholas “Dr. Nick” Yphantides greeted the crowd and thanked our special sponsor, US Bank, for its generous participation.
Physicians and medical students appreciated the opportunity to socialize and network with their colleagues during such a relaxed, fun, and tasty event. Be sure not to miss the next physician networking opportunity.





SAN DIEGOPHYSICIAN.ORG 3 (858) 569-0300
TRUST A COMMON SENSE APPROACH TO INFORMATION TECHNOLOGY Trust us to be your Technology Business Advisor HARDWARE SOFTWARE NETWORKS EMR IMPLEMENTATION SECURITY SUPPORT MAINTENANCE Endorsed by SDCMS
www.soundoffcomputing.com

‘The Heart of SDCMS’ Celebrates 20 Years of Service to San Diego’s Physicians
4 MAY 2024
JENNIPHER OHMSTEDE
By Kevin Spillane
SEVERAL DOZEN OF SAN
Diego’s most prominent physician leaders recently gathered at the iconic Tom Hamm’s Lighthouse to honor an individual who prefers to stay in the background but has nevertheless been at the center of our region’s medical community for the past two decades. Doctors recounted stories of the countless ways, both big and small, this person has distinguished herself and repeatedly made a meaningful difference for physicians and patients in San Diego County.
However, the guest of honor was not a physician, a healthcare provider, nor the CEO of a healthcare system. Odds are that you have never heard her name before.
Jennipher Ohmstede, the senior director of governance and operations for the San Diego County Medical Society (SDCMS), received some long overdue public recognition on April 17 at an event commemorating the 20th anniversary of her service to SDCMS and its physicians.
The praise and accolades for Jennipher were widespread, enthusiastic, and touching. Ohmstede was honored with a proclamation from San Diego County sponsored by Supervisor Joel Anderson. Another fan created a poster that Photoshopped Jen’s face into an image of Wonder Woman. Flowers and gifts were plentiful.
Current SDCMS President Nick Yphantides, MD, and President-Elect Steve Koh, MD, were joined by a long list of former presidents and physician leaders gathered to show their gratitude for a woman who is enjoyed and appreciated by all who have worked with her.
Over the past two decades, Jen has proven her talent and is exceptionally well-organized, thoughtful, thorough, and attentive to detail. But she has also distinguished herself with her ability to work with others and bring different stakeholders in San Diego’s medical community together in a constructive manner on important projects.
Technically, Jennipher serves as the organization’s No. 2, the indispensable right hand to CEO Paul Hegyi. But more than one physician described her more accurately as “the heart” of the San Diego County Medical Society.

The most recent SDCMS Past President, Lase Ajayi, MD, declared simply, “Jen is the heart of this organization. I could not imagine this organization without her.”
Sherry Franklin, MD, another past president, said, “We used to call her the boss. That place would not run without her. And she made us all feel safe. No matter what we were going through, she was right there. She always had your back.”
Past President Holly B. Yang, MD, told the gathering, “Jen always knows what we need and keeps us from screwing up. There is so much care and love that you provide in so many ways for so many people.”
Stu Cohen, MD, who served as SDCMS president during the financial turbulence of the 2008 Great Recession, recalled, “I loved working with her. We encountered a number of crises during my presidency, and after talking to Jen she would make it seem minor and banal. She had a great sense of humor and made it fun working at the Medical Society.”
Sabrina Bazzo, San Diego Unified School Board member and wife of the beloved David Bazzo, MD, SDCMS past president, noted medical educator,
Jen is the heart of this organization. I could not imagine this organization without her.”
— LASE AJAYI, MD, SDCMS PAST PRESIDENT “
SAN DIEGOPHYSICIAN.ORG 5
“We used to call her the boss. That place would not run without her. And she made us all feel safe. No matter what we were going through, she was right there. She always had your back.”
— SHERRY FRANKLIN, MD, SDCMS PAST PRESIDENT

and local physician leader, stood up to share, “Since Dave was diagnosed with a brain tumor a year ago, it has been a challenging time. But we want to thank Jen for always making sure to include Dave at all events. We are grateful for your inclusion and thoughtfulness.”
Bob Hertzka, MD, a key SDCMS leader for decades and an energetic advocate for the involvement of medical students in both organized medicine and the educational process about state public policy, said, “Jen is the woman who organizes everything. She has been so generous in supporting so many of the activities for our medical students. I have so relied on you.”
Another one of the legendary longtime leaders of the San Diego County Medical Society, James T. Hay, MD, quipped that “(Former SDCMS CEO) Tom Gehring brought Jen on. She has

survived both Tom and Paul Hegyi, both of whom believe all the progress of the Medical Society is because of them. But it’s because of Jen!”
Hegyi and Gehring jointly presented Jen with a playful plaque that said, “To the Real Boss Ohmstede, in humorous recognition of 20 years of service.”
CEO Paul Hegyi acknowledged Jen by saying, “I have always described Jen’s job being like herding cats. She does it to an incredible level. In no other local medical society does anyone else handle all of the details and planning for the physicians. What she does is amazing.”
Jennipher made remarks thanking everyone for their kind words and the honor of their presence and singled out SDCMS’ Brandon Ethridge, director of finance and membership and a 12-year veteran of the organization, for special thanks as “her rock.”
Jennipher’s family moved to San Diego from Texas when she was less than a year old. Jen grew up in Point Loma among a family deeply involved in medicine. Her stepfather was a physician, her mom was a respiratory therapist, and her dad was a surgical technician.
Jen was a marketing assistant for a civil engineering firm when she was brought on as then-CEO Tom Gehring’s second hire in April of 2004 to work for SDCMS. Given her family, Jen very much respected the medical pro-

fession. “The San Diego County Medical Society sounded like an organization that did a lot of good things, and I wanted to be a part of it,” she says.
When asked about her favorite part of her job, Jen enthusiastically responds, “I love working with our board of directors. I think our board is fantastic! We’ve had some amazing presidents and some amazing board members. I like that SDCMS tries to make the practice of medicine better for physicians.”
As for the negative aspects, Jen observes, “I don’t like the burnout I’m seeing with physicians. They are overworked and too often are underpaid. Their work-life balance is beyond challenging.”
Perhaps unsurprisingly, the most trying time for Jen — and the medical society — in her 20 years was during the COVID-19 pandemic. “It was scary,” she says. “I saw the daily data coming out from the County of San Diego, and it caused me to worry about my older relatives and neighbors and friends, and to also be concerned about the enormous burden placed on physicians and other healthcare providers. But I’m so proud of how SDCMS — working closely with the California Medical Association — rose up to make a real difference for San Diego physicians. We helped provide PPE for so many physicians and their offices. We held regular town hall meetings via Zoom for doc-
6 MAY 2024
“


tors, and provided constant communication to keep them as updated and informed as possible.”
Jen cites San Diego County’s massive wildfires of October 2007, which gained national attention, as another particularly challenging crisis. The medical society provided a volunteer hub for San Diego physicians and patients during the wildfires and facilitated almost a hundred physician volunteers, while aggressively keeping local doctors up to date on a daily basis given a constantly shifting situation on the ground.
Jen likes to cook and garden, and she “loves good food and better cocktails,” she says. She is an avid travel buff with her husband, Marty. They have been together for 21 years and married for 18. She has a daughter, Dani, and two stepsons, Bryce and Wesley.
Congratulations to Jennipher Ohmstede on her 20-year anniversary at the San Diego County Medical Society! We can’t wait to see the difference Jen will make — and the successes she will have — in the next decade at SDCMS.




SAN DIEGOPHYSICIAN.ORG 7
Above: Jen and the 2009 San Diego County Medical Society Board of Directors. Right: Jen celebrating with her fantastic family! L to R: son-in-law James Armenta, daughter Dani Toscano, Jen and her “partner-incrime” husband, Marty Ohmstede, and stepson Bryce Ohmstede with his girlfriend Alaina Snow.
Above: SDCMS CEO Paul Hegyi, Marty and Jen Ohmstede, and Angela Shiau and Will Tseng, MD at the 2022 Champions for Health Soiree. Left: Jen and her husband, Marty, dancing at the 2012 SDCMS Gala.
$15 Billion Win for Physicians on Prior Authorization
By Kevin B. O’Reilly
What’s the news: Under the leadership of Administrator
Chiquita Brooks-LaSure, the Centers for Medicare & Medicaid Services (CMS) has released a final rule making important reforms to prior authorization to cut patient care delays and electronically streamline the process for physicians. Together, the changes will save physician practices an estimated $15 billion over 10 years, according to the U.S. Department of Health and Human Services (HHS).
The rule addresses prior authorization for medical services in these government-regulated health plans:
• Medicare Advantage
• State Medicaid and Children’s Health Insurance Program (CHIP) fee-for-service programs
• Medicaid managed care plans and CHIP managed care entities
• Qualified health plan issuers on the federally facilitated exchanges
As a direct result of advocacy from the AMA and other physician organizations, CMS has taken significant steps toward rightsizing the prior authorization process by addressing both technological and operational requirements. The AMA is grateful that the Biden administration is prioritizing such a critical issue for patients and physicians.
“When a doctor says a patient needs a procedure, it is essential that it happens in a timely manner,” said HHS Secretary Xavier Becerra. “Too many Americans are left in limbo, waiting for approval from their insurance company.” The administration’s action, he said, “will shorten these wait times by streamlining and better digitizing the approval process.”
CMS did the right thing in “heeding patients and the physician community in a final rule that makes important reforms in government-regulated health plans’ prior authorization programs for medical services,” said AMA President Jesse M. Ehrenfeld, MD, MPH.
The rule, he noted, “requires impacted plans to support an electronic prior authorization process that is embedded within physicians’ electronic health records, bringing muchneeded automation and efficiency to the current time-consuming, manual workflow.”
Moreover, the administration’s action “will significantly enhance transparency around prior authorization by requiring specific denial reasons and public reporting of program metrics as well as requiring that prior authorization information be available to patients to help them become more informed decision-makers,” Dr. Ehrenfeld said.
In addition, CMS is mandating shortened processing time frames and also requiring that payers give physicians and pa-
tients more prior-authorization-related information. Notably, the $15 billion savings estimate does not account for lower patient costs attributable to timelier delivery of physicianordered care.
Enforcement of these policies, particularly around Medicare Advantage payers, can include CMS sanctions and civil monetary penalties. Starting in 2026, affected payers will have to send prior authorization decisions within 72 hours for urgent requests and within a week for nonurgent requests. For some payers, CMS noted, that would represent a 50% improvement. The AMA strongly advocated faster time frames of 24 hours for urgent requests and 48 hours for standard requests. CMS said it will consider updating its policies in future rulemaking. Why it’s important: While payers claim that prior authorization requirements are used for cost and quality control, a vast majority of physicians report that the protocols lead to unnecessary waste and avoidable patient harm. One-third of the 1,001 physicians surveyed by the AMA reported that prior authorization has led to a serious adverse event for a patient in their care.
More specifically, the AMA survey found that these shares of the physician respondents reported that prior authorization led to:
• A patient’s hospitalization — 25%
• A life-threatening event or one that required intervention to prevent permanent impairment or damage — 19%
• A patient’s disability or permanent bodily damage, congenital anomaly or birth defect, or death — 9%
The Improving Seniors’ Timely Access to Care Act would help fix prior authorization within Medicare Advantage, and the legislation was strongly supported by the AMA, which played a major role in securing enough co-sponsors to ensure the bill passed the House of Representatives in 2022. The legislation, however, stalled in the Senate due to a flawed $16 billion cost estimate from the Congressional Budget Office. The Biden administration’s final rule could mean a big drop in the agency’s $16 billion cost estimate for the legislation, thus upping the odds of congressional passage.
Prior authorization is overused, and existing processes present significant administrative and clinical concerns. Patients, physicians, and employers can learn more about reform efforts and share personal experiences with prior authorization at FixPriorAuth.org.
Kevin B. O’Reilly is senior news editor for the American Medical Association.
8 MAY 2024 PATIENT CARE
Addressing San Diego’s Behavioral Health Crisis With Expert, Compassionate Care
According to the National Alliance on Mental Illness, 1 in 5 U.S. adults experiences mental illness each year, with 1 in 20 experiencing serious mental illness. Each year, 1 in 6 people ages 6 to 17 experiences a mental health disorder, and for individuals ages 10 to 14, suicide is the second leading cause of death in the United States.
“Our communities need help,” says Dr. Fadi Nicolas, chief medical officer of Sharp HealthCare Behavioral Health Services. “When individuals struggle with behavioral health issues, multiple interpersonal problems can arise, causing conflict in school, work, family life, and connecting with peers and friends.”
Sharp Mesa Vista Hospital’s Legacy of Caring for the San Diego Community
As the region’s largest private behavioral healthcare provider, Sharp Mesa Vista Hospital is a critical partner in San Diego County’s efforts to address the ongoing mental health crisis. For over 60 years, Sharp Mesa Vista has treated more than 200,000 people of all ages facing serious mental illness, including substance use disorders.
Sharp is a premier provider of crisis psychiatric evaluations, assessing more than 3,200 patients in county emergency rooms and facilitating over 72,000 outpatient visits each year. Sharp Mesa Vista’s intensive care unit annually cares for nearly 1,000 patients who experience significant mental health conditions.
In addition, Sharp McDonald Center, an addiction treatment facility nearby, cares for patients with substance use disorders. Last year, the U.S. overdose rate topped 112,000 in a 12-month period. The synthetic opioid fentanyl is the number one killer among people ages 18 to 45, nationally and locally. Both behavioral health facilities are dedicated to empowering patients to reach their fullest potential. Experts include board-certified psychiatrists and psychiatric nurse practitioners, registered nurses, addictionologists, child and adult psychologists, social workers, recreational therapists, and additional behavioral health professionals.
“Mental Health Awareness Month is the perfect time to emphasize the importance of caring for our mental health and the mental health of those we love,” says Dr. Nicolas. “Tending to emotional, psychological, and behavioral health needs is essential to our overall wellbeing.”
Programs and Services Include:
After-school cognitive therapy for teens
Adult behavioral health services
Behavioral health support for military veterans
Chemical dependency and substance use disorder programs
• Child and adolescent behavioral health services
• Clinical trials for Alzheimer’s disease and dementia
• Cognitive behavioral therapies
• Dual diagnosis recovery program
Eating disorders treatment
• Electroconvulsive therapy
• Medication-assisted treatment (MAT)
Older adult behavioral health services
• Psychiatric outpatient treatment
Trauma and PTSD recovery

As the San Diego region’s largest private behavioral healthcare provider, Sharp Mesa Vista Hospital serves as a critical county partner for mental health services. Learn more at sharp.com/mesavista.
Sharp McDonald Center offers the most comprehensive hospital-based program in San Diego for treating addiction, crossing the entire continuum of care. Learn more at sharp.com/mcdonald.
SAN DIEGOPHYSICIAN.ORG 9
ADVERTISEMENT

San Diego Physicians Join CMA’s Annual Legislative Advocacy Day
By Paul Hegyi
SDCMS SENT A DELEGATION OF NEARLY 20 TO participate in the California Medical Association’s 50th Annual Legislative Advocacy Day on April 10. Over breakfast and lunch, delegates heard from CMA President Tanya Spirtos, CMA Senior Vice President Stuart Thompson, State Senate President Pro Tempore Mike McGuire, and CMA CEO Dustin Corcoran. In between those presentations and after, our delegation met with 11 legislators or their staff spread across two advocacy teams.
This year we prioritized three issues. First, Senate Bill 1120, the Physicians Make Decisions Act, dealing with the use of artificial intelligence by insurance companies in the processing of claims and prior authorization requests: SB 1120 would

require a physician have final approval of any utilization review decisions made or assisted by AI decision-making tools or algorithms used by a healthcare insurer.
Next, Senate Bill 516 is our legislation on prior authorization reform. The process of prior authorization by health insurers often requires patients to wait for treatments that are ordered by their clinician and are within the standard of care for a given diagnosis, there is also no guarantee the authorization will be given. National data from federal regulators shows that insurers reject about one in seven claims for treatment. In many cases where authorization is granted, by the time the health plan has approved the treatment, the patient’s condition has worsened, and a more intensive and costly treatment regimen is needed. Delegates shared their stories dealing with prior authorization, the administrative burdens it puts on their practices, and impacts on patients. Go to https://www.cmadocs.org/priorauth if you’d like to share your own stories.
10 MAY 2024 ADVOCACY
Left: Left to right: Will Tseng, MD; Bing Pao, MD; Jay Doucet, MD; Kenya Ochoa; Sahana Kumar; Timothy Murphy, MD; Edwin Borbon, legislative aide for Assemblywoman Tasha Boerner; Ran Reg, MD; Holly Yang, MD; and Paul Hegyi
Finally, we focused on protecting access to care, specifically looking to preserve the 2023 budget agreement that made historic investments in the Medi-Cal system (implementing this year and in 2025). With growing inflation and the recent pandemic related to healthcare delivery systems, current Medi-Cal reimbursement rates don’t come close to covering the cost of a routine medical visit. To meet California’s goal of universal access to healthcare coverage, it must provide equitable funding to strengthen the overall health system and ensure enough providers to meet the demand for patient care.
Delegates met with either the legislators or representatives for State Senators Toni Atkins, Catherine Blakespear, Brian Jones and Steve Padilla, as well as Assemblymembers David Alvarez, Tasha Boerner, Lori Davies, Brian Maienschein, Marie Waldron, Chris Ward, and Dr. Akilah Weber.
I’d like to thank Drs. Sergio Flores, Robert Hertzka, Quinn Lippmann, Preeti Mehta, Arlene Morales, Tim Murphy, Bing Pao, Ran Regev, Will Tseng, Holly Yang, Jay Doucet, and Romeo Ignacio, and med students Rahel Hintza, Anahi Ibarra Perez, Sahana Kumar, and Kenya Ochoa for participating.
Paul Hegyi is the CEO of the San Diego County Medical Society.




PHONE : 800-919-9141 OR 805-641-9141
FAX: 805-641-9143
EMAIL: JNGUYEN@TRACYZWEIG.COM
TRACYZWEIG.COM
NURSE PRACTITIONERS PHYSICIAN ASSISTANTS LOCUM TENENS PERMANENT PLACEMENT SAN DIEGOPHYSICIAN.ORG 11
PHYSICIANS
Left to right: Sahana Kumar; Holly Yang, MD; Timothy Murphy, MD; Paul Hegyi; Will Tseng, MD; Ran Regev, MD; Kristen Millstein, legislative aide for Sen. Toni Atkins; and Romeo Ignacio, MD.
Left to right: Sahana Kumar; Anahi Ibarra; Sergio Flores, MD; Preeti Mehta, MD; Robert Hertzka, MD; Assemblymember Akilah Weber, MD; Arlene Morales, MD; Kenya Ochoa, Rahel Hintza, Romeo Ignacio, MD; and Quinn Lippmann, MD.
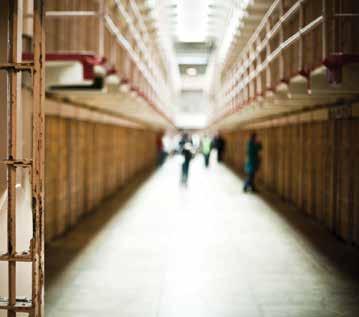
Newsom Offers a Compromise to Protect Indoor Workers From Heat
By Samantha Young
GOV. GAVIN NEWSOM’S ADMINISTRATION HAS compromised on long-sought rules that would protect indoor workers from extreme heat, saying tens of thousands of prison and jail employees — and prisoners — would have to wait for relief.
The deal comes a month after the administration unexpectedly rejected sweeping heat standards for workers in sweltering warehouses, steamy kitchens, and other dangerously hot job sites. The rules had been years in the making, and a state worker safety board voted to adopt them March 21. But in a controversial move, the administration upended the process by saying the cost to cool state prisons was unclear — and likely very expensive.
So the Democratic administration said the rules can proceed but must exempt tens of thousands of workers at 33 state prisons, conservation camps, and local jails, “in recognition of the unique implementation challenges,” said Eric Berg, of California’s Division of Occupational Safety and Health, at a Thursday hearing. A separate regulation will be drafted for correctional facilities, which could take a year, if not longer.
It’s unclear if the standards will become law in time to protect millions of other workers from summer’s intensifying heat. The compromise rules must go through a 15-day public comment period, and legal reviews within 100 days, which could push implementation well into summer. But
that can’t even happen until the original regulation is rejected by the Office of Administrative Law, which has until next month.
“Summer is arriving, and many workers, unfortunately, are going to suffer heat conditions,” said Tim Shadix, legal director at the Warehouse Worker Resource Center. “Some will likely get really sick, potentially even die from heat illness, while we continue to wait for the standard.”
Berg told members of the Occupational Safety and Health Standards Board on April 18 that Cal/OSHA would try to accelerate the timeline and get protections in place for summer.
California has had heat standards on the books for outdoor workers since 2005, and rules for indoor workplaces have been in the works since 2016. The proposed standards would require work sites to be cooled below 87 degrees Fahrenheit when employees are present and below 82 degrees in places where workers wear protective clothing or are exposed to radiant heat, such as furnaces. Buildings could be cooled with air conditioning, fans, misters, and other methods.
The rules allow workarounds for businesses that can’t cool their workplaces sufficiently, such as laundries or restaurant kitchens.
Because the rules would have a sweeping economic impact, state law requires Newsom’s Department of Finance to sign off on the financial projections, which it refused to do last month when it was unclear how much the regulations would cost state prisons. The California Department of Corrections and Rehabilitation said implementing the standards in its prisons and other facilities could cost billions, but the board’s economic analysis pegged the cost at less than $1 million a year.
Department of Finance spokesperson H.D. Palmer couldn’t promise that the compromise rules would be signed off on, but “given that the earlier correctional estimates were the issue before, not having them in the revised package would appear to address that issue,” he said.
Business and agricultural groups complained repeatedly during the rulemaking process that complying with the rules would burden businesses financially. At the April 18 hearing, they highlighted the administration’s lack of transparency and questioned why one sector should be given an exemption over another.
“The massive state costs that are of concern, specifically around prisons in the billions of dollars, are also costs that California employers will bear,” said Robert Moutrie, a senior policy advocate at the California Chamber of Commerce.
12 MAY 2024 WORKPLACE HEALTH AND SAFETY
Labor advocates asked board members not to exempt prisons, saying corrections workers need protection from heat, too.
“It’s a huge concern that prison workplaces all over are being excluded from the heat standard, leaving out not just guards, but also nurses, janitors, and the other prison workers across California unprotected from heat,” said AnaStacia Nicol Wright, an attorney with Worksafe, a workplace safety advocacy nonprofit. “California needs to prioritize the safety and wellbeing of their workers, regardless of whether they work in corrections, a farm, or a sugar refinery.”
Prisons will continue to provide cooling stations in airconditioned areas, and make water stations, fans, portable cooling units, and ice more available to workers, according to the California Department of Corrections and Rehabilitation. Prison housing units, which house roughly 93,000 inmates as of April 17, all can be cooled, usually with evaporative coolers and fans. The department has 58,135 staff members, spokesperson Terri Hardy said.
Only Minnesota and Oregon have adopted heat rules for indoor workers. Legislation has stalled in Congress, and even though the Biden administration has initiated the long


process of establishing national heat standards for outdoor and indoor work, they may take years to finalize.
Seven workers died in California from indoor heat between 2010 and 2017. Heat stress can lead to heat exhaustion, heatstroke, cardiac arrest, and kidney failure. In 2021, the Centers for Disease Control and Prevention reported that 1,600 heat-related deaths occurred nationally, which is likely an undercount because healthcare providers are not required to report them. It’s not clear how many of these deaths are related to work, either indoors or outdoors.
“These are not overly cumbersome things to implement, and they are easy ways to keep people safe and healthy,” said Jessica Early, patient advocacy coordinator at the National Union of Healthcare Workers. “Now is the urgent time to make our workplaces safer and more resilient in the face of rising temperatures.”
Samantha Young is a senior correspondent for KFF Health News, where this article first appeared, and she covers healthcare politics and policy in California, focusing on government accountability and industry influence.




SAN DIEGOPHYSICIAN.ORG 13
Are you looking to streamline your practice, curtail costs and enhance patient care? Look no further! OfficeGenieSolutions offers comprehensive virtual support services tailored to meet the needs of your healthcare practice. Here's what we offer REFERRALS/PRIOR AUTHORIZATIONS VIRTUAL PHONE SERVICE VIRTUAL MEDICAL SCRIBING Experience the convenience and efficiency of virtual support services with OfficeGenieSolutions. Contact us today to learn more and take your practice to the next level! (888) 405-1412 info@officegeniesolutions.com (213) 886-8445 www officegeniesolutions com

I’m an Autistic Doctor.
Here’s How to Improve Care for Autistic Patients
There Are Robust Resources Available to Help By Thomas Pineo, DO
IN 1983, AT THE AGE OF 13 I SIGNED UP FOR A paper route. Every morning, I rose early, got on my bike, picked up the papers, and delivered them to my subscribers. After that, I headed off to school and my other activities. I was once described as a hyperactive child, but, after starting that paper route, my mother was relieved to see me “settle down” for the first time in my life.
I delivered those papers without fail every day, through the warmth of summer, the cold and dark of winter, and the wet and rainy days of spring and fall. My father drove me if the weather was too severe, but mostly, I worked alone. And I did it all for 5 cents per paper and $14 per week. I had a job, and I loved it!
It would be another 40 years before I would recognize my own autistic traits in that paper route. Those traits included the joy of the repetitive motion of my bike, the sensory gratification of the wind in my face, the calming effect that morning activity brought to my schoolwork, the comfort of a daily routine, and the determination needed
to not give up. When I was diagnosed with autism in my 50s, I joined the lost generation of autistic adults who missed out on an autism diagnosis as a child. The prevalence of autism in children is 2.78%, but neurodivergent traits (including autism, OCD, ADHD, dyslexia, and others) can be found in 15–20% of the
14 MAY 2024
population. I am not alone; there are many other undiagnosed autistic and neurodivergent adults. In fact, autistic adults are about 30 times less likely than children to be diagnosed.
As a physician, understanding autism and neurodivergence has helped me see how sensory and communication differences affect patient care. I recently cared for an elderly patient in the hospital with profound anxiety. He complained about how loud the hospital was and that he could hear conversations up and down the halls, all day and all night. We talked about sound hypersensitivity, I offered him a set of earmuffs, and he smiled and thanked me. The next morning, I walked into the room as he was dozing with the earmuffs in place. When I gently woke him, he said he had slept well for the first time in years.
Healthcare providers need to watch out for neurodivergent traits in their patients. Healthcare is busy and we may not have access to comprehensive psychological evaluations to figure out which of our patients is autistic. We need to ask about sensory issues and be on the lookout for autistic traits.
Jonna Eriksson, MD, PhD, developed a rapid screen, which is a short autism screening questionnaire comprising the first five questions of the RAADS-14 Screen. This could be useful in busy healthcare settings, like
hospitals or emergency departments. GIFTS is an acronym to help you remember the questions.
Groups: It is difficult for me to work and function in groups.
Interpretation of expectations: It is hard for me to know what others expect of me.
Feeling: It is difficult for me to understand how other people are feeling when we are talking.
Textures: Some ordinary textures that do not bother others feel very offensive to me when they touch my skin.
Social: I don’t know how to act in social situations. Each question is scored using the following answers: True now and when young (3 points), True only now (2 points), True when young (1 point), and Never true (0 points). 4 or more points out of 15 has a sensitivity of 93% and a specificity of 45–49% for autism.
When you encounter a patient with Autistic traits, create Autistic SPACE:
Sensory: Ask about sensory accommodations, like ear plugs or headphones; sunglasses; lowering the lights; and a weighted blanket. Find out whether the patient has an aversion to certain foods or fabrics.
Predictability: Give plenty of notice with planned tests or procedures. Narrate your work so that patients always understand what is about to happen to them.
Acceptance: Don’t judge autistic traits as something that should be hidden or in
need of correction. Rather, accept them as a normal part of human variation.
Communication: Verbal and nonverbal communication differences between healthcare personnel and autistic patients are common. Ask questions to confirm understanding.
Empathy: Contrary to stereotypes, autistic people do not lack empathy. We can be deeply affected by healthcare challenges. Be prepared to give more time and support during your encounter with autistic people.
Recognizing and supporting autistic patients will not only improve communication but will also improve satisfaction and create trust. Don’t be afraid to talk to your patients about autistic traits. Breaking down stigma requires awareness and discourse.
I continue to bring the same joy of routine and determination to patient care as I brought to my paper route 40 years ago. And yes, I still love to ride my bike. Autistic traits can bring struggles, but they are also GIFTS.
Autism is a fascinating and complex condition, and autistic people have many rich stories to tell. There are simple things, like hearing protection and light dimmers, that healthcare systems can do to improve the care of autistic people. Learn more about autism and work with your healthcare institution to create autistic SPACEs.
Online autism screening tools include the Autism Quotient (AQ) or the Ritvo Autism & Asperger Diagnostic Survey-14 (RAADS-14). Helpful resources can be found at the Association for Autism and Neurodiversity and The Autism Society. <Lisa: let’s end here for print, since the last two are links>Further information can be found in Caring for hospitalized Autistic adults and Is this autism? A guide for clinicians and everyone else.

SAN DIEGOPHYSICIAN.ORG 15
Dr. Pineo is a hospitalist and medical director at UPMC Community Osteopathic Hospital in Harrisburg, Pa.
Medical Providers Are Still Grappling With UnitedHealth Cyberattack
‘This Was Way More Devastating Than COVID’ By
TWO MONTHS AFTER A CYBERATTACK ON A UnitedHealth Group subsidiary halted payments to some doctors, medical providers say they’re still grappling with the fallout, even though UnitedHealth told shareholders on Tuesday that business is largely back to normal.
“We are still desperately struggling,” said Emily Benson, a therapist in Edina, Minn., who runs her own practice, Beginnings & Beyond. “This was way more devastating than COVID ever was.”
Change Healthcare, a business unit of the Minnesota-based insurance giant UnitedHealth Group, controls a digital network so vast it processes nearly 1 in 3 U.S. patient records each year. The network is a critical conduit for shuttling information between most of the nation’s insurance companies and medical providers, who submit claims through it to get paid for treating patients.
For Benson, the cyberattack continues to significantly disrupt her business and her ability to pay her seven other clinicians.
Before the hack brought down the system, an insurance company would process a provider’s claim, then send a type of receipt known as an “electronic remittance,” which details the amount the provider was paid and whether the claim was denied. Without it, providers don’t know if they were paid correctly or how much to bill patients.
Now, instead of automatically handling those receipts digitally, some insurers must send forms in the mail. The forms require manual entry, which Benson said is a time-consuming process because it requires her to match up service dates and details to divvy up pay among her clinicians. And from at least one insurer, she said, she has yet to receive any remittances.
“I’m holding on to my sanity by a thread,” Benson said.
The situation is so dire, Alex Shteynshlyuger, MD, a urologist who owns a practice in New York City, said he had to transfer money from his personal accounts to pay his office bills.
“Look, I am freaking out,” Dr. Shteynshlyuger said. “Everyone is freaking out. We are like monkeys in a cage. We can’t really do anything about it.”
Roughly 30% of his claims were routed through Change’s platform. Except for Medicare and certain Blue Cross plans, he said, he has been unable to submit claims or receive payment from any insurers.
The company is encouraging struggling providers to reach out to the company directly via its website, said Tyler Mason, vice president of communications for UnitedHealth Group.
Samantha Liss
“I don’t think we’ve had a single provider that hasn’t been helped that’s contacted us,” Mason said. As part of that help, UnitedHealth has sent providers $7 billion so far, according to him.
Ever since the February cyberattack forced UnitedHealth to disconnect its Change platform, the company has been working “day and night to restore services” and has made “substantial progress,” UnitedHealth CEO Andrew Witty told shareholders April 16.
“We see a fairly normal claims receipts and payments flow going on at this point,” Chief Financial Officer John Rex said during the shareholder call. “But we’ll really want to be careful on that because we know there are certain care providers out there that may have been left out of it.”
Rex said the company expects full operations to resume next year.
The company reported that the hacking has already cost it $870 million and that leaders expect the final tally to total at least $1 billion this year. To put that in perspective, the company reported $99.8 billion in revenue for the first quarter of 2024, an 8.6% increase over that period last year.
Meanwhile, the House Energy and Commerce Health Subcommittee held a hearing April 16 seeking answers on the severity and damage the cyberattack caused to the nation’s health system.
Subcommittee chair Brett Guthrie (R-Ky.) said a provider in his hometown is still grappling with the fallout from the attack and losing staff because they can’t make payroll. Providers “still haven’t been made whole,” Guthrie said.
Rep. Frank Pallone Jr. (D-N.J.) voiced concern that a “single point of failure” reverberated around the country, disrupting patients’ access and providers’ financial stability.
Lawmakers expressed frustration that UnitedHealth failed to send a representative to the Capitol to answer their questions. The committee had sent Witty a list of detailed questions ahead of the hearing but was still awaiting answers.
As providers wait, too, they are trying to cover the gaps. To pay her practice’s bills, Benson said, she had to take out a nearly $40,000 loan — from a division of UnitedHealth.
Samantha Liss is a veteran journalist who has covered the business of healthcare since 2012. She is a correspondent for KFF Health News, where this article first appeared.
PRACTICE MANAGEMENT 16 MAY 2024
Multiple Sclerosis Predicted by Autoantibody Signature
Blood Samples Reveal Signs of MS Years Before Clinical
Diagnosis By Judy George
A SPECIFIC AUTOANTIBODY SIGNATURE WAS seen in a subset of people with multiple sclerosis (MS) long before clinical symptoms appeared, blood samples showed.
A distinct set of autoantibodies emerged in approximately 10% of MS patients up to five years before symptoms were seen, reported Michael Wilson, MD, of the University of California San Francisco, and co-authors. The autoantibodies appeared to bind to both human cells and common pathogens, and were associated with higher levels of serum neurofilament light (NfL).
The autoantibody profile was preserved over time, suggesting an immunologically active preclinical period years before clinical onset, Dr. Wilson and colleagues wrote in Nature Medicine
This signature may be a starting point to further characterize this patient subset and could be clinically useful as an antigen-specific biomarker for high-risk patients with clinically isolated or radiologically isolated syndromes, they added.
“We know B cells — the cells that make antibodies — are crucial for MS disease progression,” said co-author Colin Zamecnik, PhD, also of UCSF. “As a result, we believed that profiling the antibodies in patients who have or go on to develop MS would give us insight into the disease and reveal a possible biomarker,” he told MedPage Today
The findings suggest that a subset of people who develop MS have antibodies against a common protein domain prevalent in humans and viruses, Zamecnik noted.
“These patients exhibit these antibodies many years before onset, and when tested at the time of their first disease flare, have them in both their blood and cerebrospinal fluid,” he continued. “We believe it’s possible that these patients are exhibiting cross-reactive response to a prior infection, which agrees with much current work in the literature around multiple sclerosis disease progression.”
The study assessed data from the Department of Defense Serum Repository, the same source that previously helped establish a link between Epstein-Barr virus and MS. The repository stores blood from more than 10 million U.S. armed service members when they apply to join the military. The researchers used phage display immunoprecipitation sequencing (PhIP-Seq) to screen blood samples for autoantibodies.
The Department of Defense cohort contained 250 MS patients five years before and one year after first symptom onset, and 250 controls matched for age, sex, race, or ethnicity, and serum collection dates. The researchers validated their find-
ings in a sample from the prospective UCSF ORIGINS cohort, which included 103 patients who had their first attack and were subsequently diagnosed with relapsing-remitting MS.
Overall, serum NfL levels were higher in people with MS years before their first clinical flare compared with matched controls. In the Department of Defense cohort, 10% of people with MS had an abundance of autoantibodies and a distinct immunogenic cluster motif that’s present not only in humans but several human pathogens including Epstein-Barr virus, hepatitis C virus, Pseudomonas aeruginosa, Escherichia coli, and Aspergillus fumigatus. This pattern was seen both before and after these people were diagnosed with MS.
In the ORIGINS cohort, 10% of people diagnosed with MS had the same autoantibody pattern. The pattern predicted an MS diagnosis; across both cohorts, all people with this autoantibody pattern had MS.
The role of autoantibodies in MS remains unclear, and many candidate autoantigens have not survived validation studies, Dr. Wilson and colleagues pointed out. But other rare demyelinating diseases like neuromyelitis optica spectrum disorder and myelin oligodendrocyte glycoprotein antibody-associated disease were originally part of the MS spectrum and were definitively separated only after diseasespecific autoantibodies were identified, they added.
What occurred in the 10% subset of MS patients versus the remaining 90% is unclear. The sample size was small, and genetic or other associations could not be determined. And while similarity existed between this motif and those found in other infectious agents, this study measured antibodies to only a limited set of antiviral antigens, Dr. Wilson and coauthors acknowledged.
Nonetheless, the researchers are optimistic that these findings might lead to earlier diagnosis and treatment for some MS patients. “Imagine if we could diagnose MS before some patients reach the clinic,” said UCSF co-author Stephen Hauser, MD. “It enhances our chances of moving from suppression to cure.”
Judy George covers neurology and neuroscience news for MedPage Today, where this article first appeared, and she writes about brain aging, Alzheimer’s, dementia, MS, rare diseases, epilepsy, autism, headache, stroke, Parkinson’s, ALS, concussion, CTE, sleep, pain, and more.
NEUROLOGY
SAN DIEGOPHYSICIAN.ORG 17
Screen Your Gut, Save Your Butt
By Adama Dyoniziak
ON MARCH 9, CHAMPIONS FOR HEALTH PARTICIPATED in the Screen Your Gut — Save Your Butt 5K Race Walk sponsored by the California Colorectal Cancer Coalition (C4) in Mission Bay Park. The president of C4, Stony Anderson, MD, stated, “Colorectal cancer (CRC) kills more Californians than any other cancer, other than lung cancer. With screening, most of these deaths can be prevented. For every 70 people screened for CRC, we will prevent one person from dying from CRC, but only if people get tested. The best test is the one that gets done.”
“Cancer runs in my family,” said Magdalena. “My maternal grandmother had brain cancer, my aunt had breast cancer, my mom has blood cancer and is getting chemotherapy, and my sister just recently passed from colon and liver cancer. I knew I had to be my own advocate, especially for my five children.” After her positive FIT test, Project Access helped Magdalena S. follow up with a free colonoscopy and upper endoscopy.
Magdalena began to have symptoms that were like her sister’s before her sister was diagnosed, so she was very anxious to get the test done and see her results. Magdalena heard of Project Access and was relieved when she was accepted because she was uninsured and did not have the funds to get a colonoscopy and endoscopy. Robert Goldklang, MD, her gastroenterologist with Genesis Healthcare partners, explained the procedure and reassured her about the negative results.
Magdalena decided that if she could save someone’s life by participating in the 5K walk, she wanted to help someone else live. “I did the walk for my sister’s memory,” she says. “She was constantly on my mind when my husband Uriel and I were walking. My sister and I were very close, especially when we came to the U.S. 26 years ago. When we were older, we would help each other with babysitting each other’s children, with monthly expenses. We were there for each other. There was a time when we all lived together in a one-bedroom apartment. Even though money was very tight, we would use fast-food coupons and take turns treating to ensure that the children could eat and have a good time.”
Magdalena was super grateful to the kind staff at Project Access, who she said always answered all her questions, which made the experience all that much easier. “Thank you to Dr. Goldklang, his staff, and my [Project Access] case manager for helping me when I was very anxious about my health. You gave me peace of mind that I do not have colon cancer.”


Since 2008, Project Access has facilitated $27 million in care for 9,600plus uninsured patients just like Magdalena by providing free consultations and surgeries — all thanks to the dedication of our volunteer specialty physicians. Volunteer your services: Contact us at adama.dyoniziak@championsfh.org or call (858) 300-2780.
Adama Dyoniziak is the executive director of Champions for Health.
18 MAY 2024
CHAMPIONS FOR HEALTH
Above: Project Access patient Magdalena S. and her husband, Uriel S., with Champions staff. Right: Dr. Robert Goldklang.


SAN DIEGOPHYSICIAN.ORG 19 Customized insurance solutions for members The CMA Insurance Program is administered by Lockton Affinity, LLC d/b/a Lockton Affinity Insurance Brokers LLC in California #0795478. Coverage is subject to actual policy terms and conditions. Policy benefits are the sole responsibility of the issuing insurance company. The California Medical Association will receive a royalty fee for the licensing of its name and trademarks as part of the insurance program offered to the extent permitted by applicable law. Not available in all states. Visit LocktonAffinityCMA.com to schedule a 15-minute call with Lockton Affinity’s dedicated team. Together, we will determine the policies you need to be fully protected. Info@LocktonAffinityCMA.com | (800) 278-8130 The CMA Insurance Program, administered by Lockton Affinity, offers key benefits: Using group purchasing power, CMA members get exclusive, comprehensive coverage at discounted rates. Unique coverage offerings help safeguard yourself, your loved ones, your business and your livelihood. Access to newly available Medical Malpractice insurance.
CLASSIFIEDS
PRACTICE ANNOUNCEMENTS
PSYCHIATRIST AVAILABLE! Accepting new patients for medication management, crisis visits, ADHD, cognitive testing, and psychotherapy. Out of network physician servicing La Jolla and San Diego. Visit hylermed.com or call 619-707-1554.
OPPORTUNITIES
PHYSICIAN
COUNTY OF SAN DIEGO PROBATION DEPT. MEDICAL DIRECTOR: The Probation Medical Director plays a pivotal role in the medical management team, spearheading the Justice-Involved California Advancing and Innovating Medi-Cal (CalAIM) program. This initiative targets individuals with a history of incarceration, who face elevated risks of harm. California’s groundbreaking approval on January 26, 2023, allows Medicaid services to be extended to aid in their transition back into society. The Medical Director’s responsibilities encompass CalAIM’s implementation, oversight of clinical programs, and seamless integration of services for justice-involved youth. This leadership role involves collaboration with various stakeholders, ensuring quality healthcare, behavioral support, and a successful return to the community. https://www.governmentjobs.com/careers/ sdcounty/jobs/4193564/medical-director-probation23034008u?keywords=medical%20director&pagetype=j obOpportunitiesJobs
PART-TIME CARDIOLOGIST POSITION AVAILABLE: Cardiology office in San Marcos seeking part-time cardiologist. Please send resume to Dr. Keith Brady at uabresearchdoc@yahoo.com.
INTERNAL MEDICINE PHYSICIAN: Federally Qualified Health Center located in San Diego County has an opening for an Internal Medicine Physician. This position reports to the chief medical officer and provides the full scope of primary care services, including diagnosis, treatment, and coordination of care to its patients. The candidate should be board eligible and working toward certification in Internal Medicine. Competitive base salary, CME education, four weeks paid vacation, year one, 401K plan, no evenings and weekends. Monday through Friday, 8:00 am to 5:00 p.m. For more information or to apply, please contact Dr. Keith Brady at: uabresearchdoc@ yahoo.com.
FAMILY MEDICINE/INTERNAL MEDICINE PHYSI -
CIAN: San Diego Family Care is seeking a Family Medicine/Internal Medicine Physician (MD/DO) at its Linda Vista location to provide outpatient care for acute and chronic conditions to a diverse adult population. San Diego Family Care is a federally qualified, culturally competent and affordable health center in San Diego, CA. Job duties include providing complete, high quality primary care and participation in supporting quality assurance programs. Benefits include flexible schedules, no call requirements, a robust benefits package, and competitive salary. If interested, please email CV to sdfcinfo@sdfamilycare.org or call us at (858) 810-8700.
MEDICAL CONSULTANT (MD/DO): The County of San Diego is currently accepting applications from qualified candidates for Medical Consultant-Public Health Services. Vacancies are in the Public Health Services, Epidemiology and Immunization Services Branch (EISB) and Tuberculosis (TB) Control and Refugee Health Branch. Salary: $183,747.20–$204,900.80 annually. An additional 10% for Board Certified Specialty and 15% for relevant sub-specialty. For job posting information visit https:// www.governmentjobs.com/careers/sdcounty?keywords =23416202PHS.
MEDICAL DIRECTOR, FULL-TIME: FATHER JOE’S VILLAGES: Join us in ending homelessness! We are a dynamic team that runs an FQHC. The Medical Director oversees clinical aspects of the primary care, psychiatry, dental and behavioral health. This position will be a mix of clinic and admin time and will have direct reports (Dental Director, Director of Behavioral Health, and frontline primary care/psychiatry providers). Reports to the Chief Medical Officer, who is responsible for all aspects of the clinic. The Medical Director is a counterpart to the Clinic Director (who oversees admin staff, MA/RN team, billing, PSRs, etc.). See FJV Jobs to apply.
SEEKING MEDICAL DIRECTOR : subcontracted position: 4-8 hours per month. Responsibilities: 1. Support case conferences, refractory SUD, co‐occurring conditions, specialty populations. 2. Conduct clinical trainings on issues relevant to staff (e.g., documentation, ASAM Criteria, DSM‐5, MAT, WM, co‐occurring conditions) 3. Provide oversight and clinical supervision. 4. Refer co‐occurring conditions. 5. Lead Quality Improvement functions (e.g., Quality Improvement Projects, clinical team meetings, etc.). 6. Attend annually 5 hours of continuing medical education on addiction medicine. Required by contract with San Diego County BHS, position is for a Physician licensed by CA Medical Board or CA Osteopathic Medical
Board. Contact Name: Jennifer Ratoff: e-mail: jratoff@ secondchanceprogram.org, phone: 619-839-0950
PSYCHIATRIST SPECIALIST: The County of San Diego is currently accepting applications from qualified candidates. Annual Salary: $258,294.40. Note: An additional 10% is paid for Board Certification, or 15% for Board Certification that includes a subspecialty. Why choose the County? 1. Fully paid malpractice insurance; 2. 13 paid holidays; 3. 13 sick days per year; 4. Vacation: 10 days (1-4 years of service); 15 days (5-14 years of service; 20 days (15+ years); 5. Defined benefit retirement program; 6. Cafeteria-style health plan with flexible spending; 7. Wellness incentives. Psychiatrist-Specialists perform professional psychiatric work involving the examination, diagnosis, and treatment of specialty forensics, children/adolescents and or geriatric patients. This is the specialty journey level class in the series that requires a fellowship or experience in child and adolescent psychiatry or forensic psychiatry. For more information visit our website at sandiegocounty. gov/hr or select this link to go directly to the Psychiatrist Specialist application.
PRIMARY CARE PHYSICIAN: Imperial Valley Family Care Medical Group is looking for Board Certified/Board Eligible Primary Care Physician for their clinics in Brawley & El Centro CA. Salaried/full time position. Please fax CV/ salary requirements to Human Resources (760) 355-7731. For details about this and other jobs please go to www. ivfcmg.com
ASSISTANT, ASSOCIATE OR FULL PROFESSOR (HS CLIN, CLIN X, ADJUNCT, IN-RESIDENCE)
MED-GASTROENTEROLOGY: Faculty Position in Gastroenterology. The Department of Medicine at University of California, San Diego, Department of Medicine (http:// med.ucsd.edu/) is committed to academic excellence and diversity within the faculty, staff, and student body and is actively recruiting faculty with an interest in academia in the Division of Gastroenterology. Clinical and teaching responsibilities will include general gastroenterology. The appropriate series and appointment at the Assistant, Associate or Full Professor level will be based on the candidate’s qualifications and experience. Salary is commensurate with qualifications and based on the University of California pay scales. In-Residence appointments may require candidates to be self-funded. For more information: https://apol-recruit.ucsd.edu/JPF03179 For help contact: klsantos@health.ucsd.edu
DERMATOLOGIST NEEDED: Premier dermatology practice in La Jolla seeking a part-time BC or BE dermatologist to join our team. Busy practice with significant opportunity for a motivated, entrepreneurial physician. Work with three energetic dermatologists and a highly trained staff in a positive work environment. We care about our patients and treat our staff like family. Opportunity to do medical/surgical and cosmetic dermatology in an updated medical office with state-of-the art tools and instruments. Incentive plan will be a percentage based on production. If you are interested in finding out more information, please forward your C.V. to jmaas12@hotmail.com
INTERNAL MEDICINE PHYSICIAN: Healthcare Medical Group of La Mesa located at 7339 El Cajon Blvd is looking for a caring, compassionate, and competent physician for providing primary care services. We require well-organized and detail-oriented with excellent written and oral communication skills, and excellent interpersonal skills to provide high-quality care to our patients. We provide a competitive salary, paid time off, health insurance, 401K benefits, etc. We provide plenty of opportunities to refine your clinical competency. Our CEO Dr. Venu Prabaker, who has 30 years of teaching experience as a faculty at multiple universities including Stanford, UCSD, USC, Midwestern, Western, Samuel Merritt, Mayo, etc., will be providing teaching rounds once a week. You will also get plenty of opportunities to attend other clinical lectures at many of the 4- to 5-star restaurants in San Diego. We also have a weekly one-hour meeting for all the staff for team building and to create a “family atmosphere” to improve productivity and thereby create a win-win situation for all. Visit us at caremd.us.
RADY
CHILDREN’S HOSPITAL PEDIATRICIAN POSI -
TIONS: Rady Children’s Hospital of San Diego seeking board-certified/eligible pediatricians or family practice physicians to join the Division of Emergency Medicine in the Department of Urgent Care (UC). Candidate will work at any of our six UC sites in San Diego and Riverside Counties. The position can be any amount of FTE (full-time equivalent) equal to or above 0.51 FTE. Must have an MD/ DO or equivalent and must be board certified/eligible, have a California medical license or equivalent, PALS certification, and have a current DEA license. Contact Dr. Langley glangley@rchsd.org and Dr. Mishra smishra@rchsd.org.
PUBLIC HEALTH SERVICES MEDICAL CONSULTANT M.D., D.O: MEDICAL CONSULTANT-21416207 | JOB DETAILS TAb | Career Pages (governmentjobs. com)<https://www.governmentjobs.com/careers/
sdcounty/jobs/3148610/m-d-d-o-medical-consultant21416207?keywords=medical%20consultant&pagetype=j obOpportunitiesJobs
PER DIEM OBGYN LABORIST POSITION AVAILABLE: IGO Medical Group is seeking a per diem laborist to cover Labor and Delivery and emergency calls at Scripps Memorial Hospital in La Jolla. 70 deliveries/month. 24-hour shifts preferred but negotiable. Please send inquiries by email to IGO@IGOMED.com.
MEDICAL CONSULTANT, SAN DIEGO COUNTY: The County of San Diego, Health and Human Services Agency’s Public Health Services is looking for a Board Certified Family Practice or Internal Medicine physician for the Epidemiology and Communicable Disease Division. Under general direction, incumbents perform a variety of duties necessary for the identification, diagnosis, and control of communicable diseases within the population. This position works closely with the medical and laboratory community, institutional settings, or hospital control practitioners. Learn more here: https://www.governmentjobs. com/careers/sdcounty?keywords=21416207
KAISER PERMANENTE SAN DIEGO PER DIEM
PHYSIATRIST: Southern California Permanente Medical Group is an organization with strong values, which provides our physicians with the resources and support systems to ensure they can focus on practicing medicine, connecting with one another, and providing the best possible care to their patients. For consideration or to apply, visit https://scpmgphysiciancareers.com/specialty/ physical-medicine-rehabilitation. For questions or additional information, please contact Michelle Johnson at 866-503-1860 or Michelle.S1.Johnson@kp.org. We are an AAP/EEO employer.
PRIMARY CARE PHYSICIAN POSITION: San Diego Family Care is seeking a Primary Care Physician (MD/DO) at its Linda Vista location to provide direct outpatient care for acute and chronic conditions to a diverse adult population. San Diego Family Care is a federally qualified, culturally competent and affordable health center in San Diego, CA. Job duties include providing complete, high quality primary care, and participation in supporting quality assurance programs. Benefits include flexible schedules, no call requirements, a robust benefits package, and competitive salary. If interested, please email CV to sdfcinfo@ sdfamilycare.org or call us at (858) 810- 8700.
FAMILY MEDICINE OR INTERNAL MEDICINE PHYSICIAN: TrueCare is more than just a place to work; it feels like home. Sound like a fit? We’d love to hear from you! Visit our website at www.truecare.org. Under the direction of the Chief Medical Officer and the Lead Physician, ensure the provision of effective quality medical service to the patients of the Health center. The physician is responsible for assuring clinical procedures are continually and systematically followed, patient flow is enhanced, and customer service is extended to all patients at all times.
PUBLIC HEALTH LABORATORY DIRECTOR: The County of San Diego is seeking a dynamic leader with a passion for building healthy communities. This is a unique opportunity for a qualified individual to work for a Level 3 Public Health Laboratory. The Public Health Services department, part of the County’s Health and Human Services Agency, is a local health department nationally accredited by the Public Health Accreditation Board and first of the urban health departments to be accredited. Public Health Laboratory Director-21226701UPH
NEIGHBORHOOD HEALTHCARE MD, FAMILY PRACTICE AND INTERNISTS/HOSPITALISTS: Physicians wanted, beautiful Riverside County and San Diego County- High Quality Family Practice for a private-nonprofit outpatient clinic serving the communities of Riverside County and San Diego County. Work full time schedule and receive paid family medical benefits. Malpractice coverage provided. Be part of a dynamic team voted ‘San Diego Top Docs’ by their peers. Please click the link to be directed to our website to learn more about our organization and view our careers page at www.Nhcare.org.
PHYSICIAN WANTED: Samahan Health Centers is seeking a physician for their federally qualified community health centers that emerged over forty years ago. The agency serves low-income families and individuals in the County of San Diego in two (2) strategic areas with a high density population of Filipinos/Asian and other lowincome, uninsured individuals — National City (Southern San Diego County) and Mira Mesa (North Central San Diego). The physician will report to the Medical Director and provide the full scope of primary care services, including but not limited to diagnosis, treatment, coordination of care, preventive care and health maintenance to patients. For more information and to apply, please contact Clara Rubio at (844) 200-2426 EXT 1046 or at crubio@samahanhealth.org.
20 MAY 2024
PHYSICIAN POSITIONS WANTED
PART-TIME CARDIOLOGIST AVAILABLE AFTER 7/4/23: Dr. Durgadas Narla, MD, FACC is a noninvasive cardiologist looking to work 1-2 days/week or cover an office during vacation coverage in the metro San Diego area. He retired from private practice in Michigan in 2016 and has worked in a San Marcos cardiologist office for the last 5 years, through March 2023. Board certified in cardiology and internal medicine. Active CA license with DEA, ACLS, and BCLS certification. If interested, please call (586) 206-0988 or email dasnarla@gmail.com
PSYCHIATRIST AVAILABLE! Accepting new patients for medication management, crisis visits, ADHD, cognitive testing, and psychotherapy. Out of network physician servicing La Jolla & San Diego. Visit hylermed.com or call 619-707-1554.
PRACTICE FOR SALE
GASTROENTEROLOGY GI PRACTICE FOR SALE: Looking to expand or move? Established 25+ years Gastroenterology GI office practice for sale in beautiful San Diego County, California. 500 active strong patient relationships and referral streams. Consistent total gross income of $600,000 for the past couple years; even through the pandemic. Located in a professional medical building with professional contract staff. All records and billing managed by a professional service who can assist with insurance integration. Office, staff & equipment are move-in ready. Seller will assist Buyer to ensure a smooth transition. Being On-Call optional. Contact Ferdinand @ (858) 752-1492 or ferdinand@zybex.com
OTOLARYNGOLOGY HEAD & NECK SURGERY SOLO PRACTICE FOR SALE: Otolaryngology Head & Neck Surgery solo practice loc ated in the Ximed building on the Scripps Memorial Hospital La Jolla campus is for sale. The office is approximately 3,000 SF with 1 or 2 Physician Offices. It has 4 fully equipped exam rooms, an audio room, one procedure room, one conference room, one office manager room as well as in-house billing section, staff room and a bathroom. There is ample parking for staff and patients with close access to radiology and laboratory facilities. For further information please contact Christine Van Such at 858-354-1895 or email: mahdavim3@gmail.com
OFFICE SPACE / REAL ESTATE AVAILABLE
OFFICE SPACE FOR SUBLEASE, SOUTHEAST SAN DIEGO: 3 patient exam rooms, nurse’s station, large reception area and waiting room. Large parking lot with valet on-site, and nearby bus stop. 286 Euclid Ave - Suite 205, San Diego, CA 92104. Please contact Dr. Kofi D. SefaBoakye’s office manager: Agnes Loonie at (619) 435-0041 or ams66000@aol.com
MEDICAL OFFICE FOR SALE OR SUBLEASE: A newly remodeled and fully built-out primary care clinic in a highly visible Medical Mall on Mira Mesa Blvd. at corner of Camino Ruiz. The office is approximately 1000 sq ft with 2 fully equipped exam rooms, 1 office, 1 nurse station, spacious and welcoming waiting room, spacious reception area, and ADA accessible restroom. All the furniture and equipment are new and modern design. Ample parking. Perfect for primary care or any specialty clinic. Please contact Nox at 619-776-5295 or noxwins@hotmail.com. Available immediately.
EL CAJON RENOVATED MEDICAL OFFICE AVAILABLE: Recently renovated, turn-key medical office in freestanding single-story unit available in El Cajon. Seven exam rooms, spacious waiting area with floor-to-ceiling windows, staff break room, doctor’s private office, multiple admin areas, manager’s office all in lovely, droughtresistant garden setting. Ample free patient parking with close access to freeways and Sharp Grossmont and Alvarado Hospitals. Safe and secure with round-the-clock monitored property, patrol, and cameras. Available March 1st. Call 24/7 on-call property manager Michelle at the Avocado Professional Center (619) 916-8393 or email help@avocadoprofessionalcenter.com.
OPERATING ROOM FOR RENT: State of the Art AAAASF Certified Operating Rooms for Rent at Outpatient Surgery of Sorrento. 5445 Oberlin Drive, San Diego 92121. Ideally located and newly built 5 star facility located with easy freeway access in the heart of San Diego in Sorrento Mesa. Facility includes two operating rooms and two recovery bays, waiting area, State of the Art UPC02 Laser, Endoscopic Equipment with easy parking. Ideal for cosmetic surgery. Competitive Rates. Call Cyndy for more information 858.658.0595 or email Cyndy@roydavidmd.com
PRIME LOCATION – MEDICAL BUILDING LEASE OR OWN OPPORTUNITY IN LA MESA: Extraordinary opportunity to lease or lease-to-own a highly visible, freewayoriented medical building in La Mesa, on Interstate 8 at the 70th Street on-ramp. Immaculate 2-story, 7.5k square foot property with elevator and ample free on-site parking (45 spaces). Already built out and equipped with MRI/CAT ma-
chine. Easy access to both Alvarado and Sharp Grossmont Hospitals, SDSU, restaurants, and walking distance to 70th St Trolley Station. Perfect for owner-user or investor. Please contact Tracy Giordano [Coldwell Banker West, DRE# 02052571] for more information, (619) 987-5498.
POWAY MEDICAL OFFICE SPACE FOR LEASE
2/1/2024: Fully built out, turnkey 1257 sq ft ADA-compliant suite for lease. Great location in Pomerado Medical/ Dental Building, next to Palomar Med Center Poway campus. Building restricted to medical/allied health/dental practices, currently houses ~26 suites. Ideal for small health practice as primary or satellite location. Lease includes front lobby, reception area, restrooms, large treatment area, private treatment/exam rooms. Located on second floor, elevator/stair access. Bright, natural lighting; unobstructed views of foothills. On-site parking; nearby bus service. Flexible lease terms available from 3-5 years at fair market rate. Contact Debbie Summers at debjsummers3@gmail.com (858) 382-8127.
KEARNY MESA OFFICE TO SUBLEASE/SHARE: 5643
Copley Dr., Suite 300, San Diego, CA 92111. Perfectly centrally situated within San Diego County. Equidistant to flagship hospitals of Sharp and Scripps healthcare systems. Ample free parking. Newly constructed Class A+ medical office space/medical use building. 12 exam rooms per half day available for use at fair market value rates. Basic communal medical supplies available for use (including splint/cast materials). Injectable medications and durable medical equipment (DME) and all staff to be supplied by individual physicians’ practices. 1 large exam room doubles as a minor procedure room. Ample waiting room area. In office x-ray with additional waiting area outside of the x-ray room. Orthopedic surgery centric office space. Includes access to a kitchenette/indoor break room, exterior break room and private physician workspace. Open to other MSK physician specialties and subspecialties. Building occupancy includes specialty physicians, physical therapy/occupational therapy (2nd floor), urgent care, and 5 OR ambulatory surgery center (1st floor). For inquiries contact kdowning79@gmail.com and mgamboa@ortho1.com for more information. Available for occupancy projected as February 2024.
LA JOLLA/UTC OFFICE TO SUBLEASE OR SHARE: Modern upscale office near Scripps Memorial, UCSD hospital, and the UTC mall. One large exam/procedure room and one regular-sized exam room. Large physician office for consults as well. Ample waiting room area. Can accommodate any specialty or Internal Medicine. Multiple days per week and full use of the office is available. If interested please email drphilipw@gmail.com
ENCINITAS MEDICAL SPACE AVAILABLE: Newly updated office space located in a medical office building. Two large exam rooms are available M-F and suitable for all types of practice, including subspecialties needing equipment space. Building consists of primary and specialist physicians, great for networking and referrals. Includes access to the break room, bathroom and reception. Large parking lot with free parking for patients. Possibility to share receptionist or bring your own. Please contact coastdocgroup@gmail.com for more information.
NORTH COUNTY MEDICAL SPACE AVAILABLE: 2023 W. Vista Way, Suite C, Vista CA 92082. Newly renovated, large office space located in an upscale medical office with ample free parking. Furnishings, decor, and atmosphere are upscale and inviting. It is a great place to build your practice, network and clientele. Just a few blocks from Tri-City Medical Center and across from the urgent care. Includes: multiple exam rooms, access to a kitchenette/break room, two bathrooms, and spacious reception area all located on the property. Wi-Fi is not included. For inquiries contact hosalkarofficeassist@gmail.com or call/ text (858)740-1928.
PHYSICIAN OFFICE SPACE FOR LEASE. 1500 Sq ft. 3 exam room. Large private office. Large reception area and patient prep room. New upgraded flooring. Private entrance. Located in Rancho Bernardo in prime central location. Easy access to interstate 15. Palomar /Pomerado within 10 min. Security card access during off hours. $2,500/month. Contact: (619) 585-0476. Ask for Peg.
HILLCREST OFFICE TO SUBLEASE OR SHARE: Gorgeous office located across from Scripps Mercy hospital. Office is approximately 2000 sq. ft. with procedure/effusion room. Office is fully staffed and looking to add a new provider. We currently have Rheumatology/Pulmonary/Allergy specialists but can accommodate any specialty or Internal Medicine. Multiple days per week and full use of office is available. If interested please reach out to Melissa Coronado at Melissa@sdpulmonary.com or call (619) 819-7224.
SUBLEASE AVAILABLE: Sublease available in Del Mar off 5 freeway. Share rent. 2100 sq ft office in professional building. Utilities included. Great opportunity in a very desirable area. 858-342-3104.
CHULA VISTA MEDICAL OFFICE: Ready with 8 patient rooms, 2,000sf, excellent parking ratios, Lease $4,000/ mo. No need to spend a penny. Call Dr. Vin, 619-405-6307 vsnnk@yahoo.com
OFFICE SPACE AVAILABLE IN BANKERS HILL: Approximately 500sq feet suite available to lease, includes private bathroom. Located at beautiful Bankers Hill. For more details, please call Claudia at 619-501-4758.
OFFICE SPACE IN EL CENTRO, CA TO SHARE: Office in El Centro in excellent location, close to El Centro Regional Medical Centre Hospital is seeking Doctors of any specialty to share the office space. The office is fully furnished. It consists of 8 exam rooms, nurse station, Dr. office, conference room, kitchenette and beautiful reception. If you are interested or need more information please contact Katia at 760-427-3328 or email at Feminacareo@gmail.com
OFFICE SPACE / REAL ESTATE WANTED
MEDICAL OFFICE SPACE WANTED IN HILLCREST/ BANKERS HILL AREA. Mercy Physicians Medical Group (MPMG) specialist is looking for office space near Scripps Mercy Hospital. Open to lease or share office space, full time needed. Please respond to rjvallonedpm@sbcglobal. net or 858-945-0903.
MEDICAL EQUIPMENT / FURNITURE FOR SALE
UROLOGY OFFICE CLOSING 6/2023—EQUIPMENT
AVAILABLE: Six fully furnished exam rooms including tables (2 bench, 3 power chair/table, 1 knee stirrup), rolling stools, lights, step stools, patient chairs. Waiting room chairs, tables, magazine rack. Specialty items—Shimadzu ultrasound, SciCan sterilizer, Dyonics camera with Sharp monitor, Medtronic Duet urodynamics with T-DOC catheters, Bard prostate biopsy gun with needles, Cooper Surgical urodynamics, Elmed ESU cautery, AO 4 lens microscope. RICOH MP-3054 printer with low print count. For more information contact: r.pua@cox.net.
NON-PHYSICIAN POSITIONS AVAILABLE
RESEARCH SCIENTISTS: (non-tenured, Assistant, Associate or Full level): The University of California, San Diego campus multidisciplinary Organized Research Units (ORUs) https://research.ucsd.edu/ORU/index.html are conducting an open search. Research Scientists are extramurally funded, academic researchers who develop and lead independent creative research programs similar to Ladder Rank Professors. They are expected to serve as Principal Investigators on extramural grants, generate high caliber publications and research products, engage in university and public service, continuously demonstrate independent, high quality, significant research activity and scholarly reputation. Appointments and duration vary depending on the length of the research project and availability of funding. https://apol-recruit.ucsd.edu/JPF03713/apply
PROJECT SCIENTISTS: Project Scientists (non-tenured, Assistant, Associate or Full level): The University of California, San Diego, Office of Research Affairs https:// research.ucsd.edu/, in support of the campus multidisciplinary Organized Research Units (ORUs) https:// research.ucsd.edu/ORU/index.html is conducting an open search. Project Scientists are academic researchers who are expected to make significant and creative contributions to a research team, are not required to carry out independent research but will publish and carry out research or creative programs with supervision. Appointments and duration vary depending on the length of the research project and availability of funding. https://apolrecruit.ucsd.edu/JPF03262/apply
OFFICE MANAGER: 1. Hiring, Training, Managing staff on procedures/policies. Monitors continuing compliance and office statistics. Oversee stocking/maintenance of supplies, retail. Equipment/ facilities management. Daily bookkeeping, collections. 2. Ensure smooth/efficient patient flow with increasing production/collections. 3. Create a friendly environment where patients expectations are exceeded, where staff can work together as a team. 4. Ensure staff working at maximum productivity/efficiency. Salary: 60-70K depending on experience/qualifications. Benefits: healthcare reimbursement, PTO, retirement, employee discount, bonuses, commission. Contact: info@ manageyourage.com
ASSISTANT PUBLIC HEALTH LAB DIRECTOR: The County of San Diego is currently accepting applications for Assistant Public Health Lab Director. The future incumbent for Assistant Public Health Lab Director will assist in managing public health laboratory personnel who perform laboratory activities for the purpose of identifying, controlling, and preventing disease in the community, as well as assist with the development and implementation of policy and procedures relating to the control and prevention of disease and other health threats. Please visit the County of San Diego website for more information and to apply online.
SAN DIEGOPHYSICIAN.ORG 21 CLASSIFIEDS



San Diego County Medical Society
92123
$5.95 | www.SanDiegoPhysician.org PRSRT STD U.S. POSTAGE PAID DENVER, CO PERMIT NO. 5377
8690 Aero Drive, Suite 115-220 San Diego, CA
[ Return Service Requested ]