WHAT WE KNOW WORKS, RIGHT NOW, FOR OUR PATIENTS















Editor: James Santiago Grisolia, MD
Editorial Board: James Santiago Grisolia, MD; David E.J. Bazzo, MD; William T-C Tseng, MD; Holly B. Yang, MD, MSHPEd, HMDC, FACP, FAAHPM
Marketing & Production Manager: Jennifer Rohr
Art Director: Lisa Williams
Copy Editor: Adam Elder
President: Nicholas (dr. Nick) J. Yphantides, MD, MPH
President–Elect: Steve H. Koh, MD
Secretary: Preeti S. Mehta, MD
Treasurer: Maria T. Carriedo-Ceniceros, MD
Immediate Past President: Toluwalase (Lase) A. Ajayi, MD
East County #1: Catherine A. Uchino, MD
Hillcrest #1: Kyle P. Edmonds, MD
Hillcrest #2: Stephen R. Hayden, MD (Delegation Chair)
Kearny Mesa #1: Anthony E. Magit, MD, MPH
Kearny Mesa #2: Dustin H. Wailes, MD
La Jolla #1: Karrar H. Ali, DO, MPH (Board Representative to the Executive Committee)
La Jolla #2: David E.J. Bazzo, MD, FAAFP
La Jolla #3: Sonia L. Ramamoorthy, MD, FACS, FASCRS
North County #1: Arlene J. Morales, MD
North County #2: Christopher M. Bergeron, MD, FACS
North County #3: Nina Chaya, MD
South Bay #1: Paul J. Manos, DO
South Bay #2: Latisa S. Carson, MD
AT–LARGE DIRECTORS
#1: Rakesh R. Patel, MD, FAAFP, MBA (Board Representative to the Executive Committee) #2: Kelly C. Motadel, MD, MPH #3: Irineo (Reno) D. Tiangco, MD #4: Miranda R. Sonneborn, MD #5: Daniel Klaristenfeld, MD #6: Alexander K. Quick, MD #7: Karl E. Steinberg, MD, FAAFP #8: Alejandra Postlethwaite, MD
ADDITIONAL VOTING DIRECTORS
Young Physician: Emily A. Nagler, MD
Resident: Alexandra O. Kursinskis, MD
Retired Physician: Mitsuo Tomita, MD
Medical Student: Kenya Ochoa
Immediate Past President: Robert E. Wailes, MD
Trustee: William T–C Tseng, MD, MPH
Trustee: Sergio R. Flores, MD
Trustee: Timothy A. Murphy, MD
AMA DELEGATES AND ALTERNATE DELEGATES
District I: Mihir Y. Parikh, MD
District I Alternate: William T–C Tseng, MD, MPH
At–Large: Albert Ray, MD
At–Large: Robert E. Hertzka, MD
At–Large: Theodore M. Mazer, MD
At–Large: Kyle P. Edmonds, MD
At–Large: Holly B. Yang, MD, MSHPEd, HMDC, FACP, FAAHPM
At–Large: David E.J. Bazzo, MD, FAAFP
At–Large: Sergio R. Flores, MD
At–Large Alternate: Bing Pao, MD
CMA DELEGATES
District I: Steven L.W. Chen, MD, FACS, MBA
District I: Vikant Gulati, MD
District I: Quinn Lippman, MD
District I: Eric L. Rafla-Yuan, MD
District I: Ran Regev, MD
District I: Kosala Samarasinghe, MD
District I: Thomas J. Savides, MD
District I: James H. Schultz, MD, MBA, FAAFP, FAWM, DiMM
District I: Mark W. Sornson, MD
District I: Wynnshang (Wayne) C. Sun, MD
District I: Patrick A. Tellez, MD, MHSA, MPH
District I: Randy J. Young, MD
RFS Delegate: David J. Savage, MD
Opinions expressed by authors are their own and not necessarily those of SanDiegoPhysician or SDCMS. SanDiegoPhysicianreserves the right to edit all contributions for clarity and length as well as to reject any material submitted. Not responsible for unsolicited manuscripts. Advertising rates and information sent upon request. Acceptance of advertising in SanDiegoPhysicianin no way constitutes approval or endorsement by SDCMS of products or services advertised. SanDiegoPhysicianand SDCMS reserve the right to reject any advertising. Address all editorial communications to Editor@SDCMS.org. All advertising inquiries can be sent to DPebdani@SDCMS.org. SanDiegoPhysicianis published monthly on the first of the month. Subscription rates are $35.00 per year. For subscriptions, email Editor@SDCMS.org. [San Diego County Medical Society (SDCMS) Printed in the U.S.A.]
FEATURE
4
Brain Health and Dementia: What We Know Works, Right Now, for Our Patients
By Lindsey Yourman, MD and Ian Neel, MD
DEPARTMENTS
2 Briefly Noted: Federal Issues * Physician Wellness * Reimbursement
8
San Diego County Medical Society Holds Annual Board Retreat
By Paul Hegyi, MBA
10
Back from COP28, California Climate Leaders Talk Health Impacts of Warming
By Samantha Young
12
Can Artificial Intelligence Improve Prior Authorization?
By Shannon Firth

10
14
4
Can the Ketogenic Diet Treat Mental Illness?
By Jennifer Henderson
16
Healthcare Workers Push for Their Own Confidential Mental Health Treatment
By Katheryn Houghton
18
Why Patients Need to Come Clean About Cannabis to Their Anesthesiologist
By Max Feinstein, MD
20
Classifieds
Editor’s Note: In the January issue of San Diego Physician , the pictures of medical students Haley Torres and Kiersten Gabaldon were accidentally transposed. We deeply regret the error.
A BIPARTISAN GROUP OF U.S. SENATORS last week announced the formation of a Medicare payment reform working group. The primary goal of this group — which includes Catherine Cortez Masto (D-Nev.), Marsha Blackburn (R-Tenn.), John Thune (R-S.D.), John Barrasso (R-Wyo.), Debbie Stabenow (D-Mich.), and Mark Warner (D-Va.) — is to explore policy solutions to reform and stabilize the Medicare physician payment system and ensure sustained access to quality care for patients. The Senate Finance Committee is also expected to take up the issue of long-term Medicare physician payment reforms this year.
“As the healthcare system has evolved since the inception of the Medicare program, the physician payment system has failed to keep pace with the actual cost of care and the improvements in new services and technologies,” the Senate working group said in a statement. “Medicare Part B is a lifeline for tens of millions of Americans, covering a wide array of services, including primary and outpatient care, preventive services, durable medical equip-
ment, and more. … We believe Congress must make changes to the current Medicare physician payment system to ensure financial stability for providers, improve patient outcomes, promote access to quality care, and incentivize the utilization of emerging healthcare technology.”
The working group will be reaching out to stakeholders in the coming weeks to seek feedback and to begin developing policies that will address Medicare physician payment for the long-term. The California Medical Association (CMA) will be fully engaged in these discussions and will keep physicians informed.
CMA continues to urge Congress to reverse the 3.37% Medicare physician payment cut that took effect on Jan. 1, 2024. If this latest cut is left in place, physician Medicare payments will have been reduced by almost 10% in four years. This is simply unsustainable for our nation’s physicians and the patients they serve.
A BIPARTISAN BICAMERAL GROUP of U.S. Senators and Representatives recently introduced legislation to reauthorize the Dr. Lorna Breen Health Care Provider Protection Act for another five years.
The original legislation was signed into law on March 18, 2022, and was named in honor of Dr. Lorna Breen, a physician from Virginia, who died by suicide in April 2020 due to the stress and trauma of serving on the frontlines caring for COVID-19 patients in New York City during the height of the pandemic.
The law has already provided $100 million in funding for mental healthcare for providers across the country. However, some provisions of the original law are set to expire at the end of this year, making the Dr. Lorna Breen Healthcare Provider Protection Reauthorization Act (S. 3679/H.R. 7153) vital to continuing this good work.
The California Medical Association applauds the introduction of this important legislation.

SPONSORED BY THE CALIFORNIA Medical Association (CMA) and authored by Senator Richard Pan, MD, SB 510 (2021) requires health plans and insurers to reimburse providers for specified COVID-19 testing, related office visits, and immunization services. The law also prohibits health plans and insurers from shifting the financial risk for COVID-19 testing, vaccine administration, and related services to contracted providers, unless both parties have negotiated and agreed to a new contractual provision. Though the law took effect Jan. 1, 2022, it applies retroactively to claims dating back to March 4, 2020, the beginning of California’s public health emergency for COVID-19.
The California Association of Health Plans (CAHP) filed a lawsuit in November 2021 challenging the law’s retroactive application on constitutional grounds. Although CAHP obtained a preliminary injunction that temporarily prohibited the enforcement of the law with respect to pre-2022 claims, the trial court ultimately ruled against CAHP, and held that the law could apply retroactively to March 4, 2020, and dissolved the preliminary injunction. This means that the law, including its retroactive provisions, is fully in effect. Plans and insurers are required to comply
with the reimbursement requirements.
According to guidance issued by the California Department of Managed Health Care (DMHC) (APL 23-021), plans were required to reimburse providers with interest for unpaid or underpaid SB 510 claims by Feb. 12, 2024. Plans that failed to reimburse providers by this date may be subject to enforcement action by DMHC. CMA has heard reports, however, that some plans have still not reimbursed physicians for COVID-19 testing and related services.
Additionally, CMA is hearing some plans have refused to reimburse delegated groups, asserting that SB 510’s prohibition on delegation of financial risk applies only to COVID-19 testing, not related services, such as screening exams. However, the law is clear that “health plans shall not delegate the financial risk to a contracted provider for the cost of enrollee services provided under this section unless the parties have negotiated and agreed upon a new provision of the parties’ contract” (Health & Safety Code 1342.2(a)(6)). Services provided under section 1342.2 include both “COVID-19 diagnostic and screening testing and healthcare services related to diagnostic and screening,” which the law expressly defines to include “hospital or healthcare provider office visits for the purposes of receiving testing,” and “the administration of testing,” among items and services. This is also reiterated in DMHC guidance (APL 22-014) issued in April 2022 regarding SB 510 compliance.
Physicians and physician groups facing plan refusals to pay pre-2022 COVID-19 testing and related services are encouraged to consult with their practice attorney and contact CMA’s Center for Economic Services at (800) 786-4262 or economicservices@ cmadocs.org.

























WHAT
Any news of advances in research about treatment of Alzheimer’s disease and related dementias (ADRD) fill us with hope on our quest to mitigate the immense suffering caused by this disease. At the same time, there is concern about the impending direct-to-consumer marketing of new FDA-approved antiamyloid therapies, which are monoclonal antibody infusions [MAB] that showed statistical significance but unclear clinical significance along with definite risks. The promotion of their availability could provide false hope to desperate patients and families and thereby compound suffering for the more than 100,000 older adults in San Diego County currently experiencing dementia.
As we await more data on the anti-amyloid infusions and infrastructure for their administration (PET imaging for amyloid detection, serial MRIs for amyloidrelated imaging abnormalities, monthly intravenous infusions, lumbar punctures to obtain CSF biomarkers for amyloid-tau ratios), our medical community has the opportunity to reflect on lessons learned from the first wave of Alzheimer’s medications (acetylcholinesterase inhibitors such as donepezil [Aricept]). If one asks clinicians why acetylcholinesterase inhibitors continued to be prescribed even once evidence and our experience showed they were minimally clinically effective 1, many informed and caring clinicians will tell you it was because “we had nothing else to offer.” I’m so grateful to be able to say today that this is no longer true.
Consistent clinical trial evidence 2,3 suggests that psychosocial interventions delivered within a comprehensive dementia care model have not only a statistically significant benefit, but also a clinically significant impact on quality of life for people living with dementia, including the ability to live longer in their home, and can improve wellbeing of care partners. Key components of these models include caregiver education and support, care coordination, physical exercise, social engagement, mentally stimulating activities, and a healthy, balanced diet.
Many of these evidencebased psychosocial interventions are currently accessible to many of our patients and their care partners in San Diego County, right now, today, and include resources that physicians can paste into an After Visit Summary
or patient portal message, recommend for inclusion into interprofessional workflows, or ask their health system to provide patient-facing material on these interventions. These resources include but are not limited to:
• Medical advance care planning
• Legal and financial planning
• Care partner education and support
• Support groups for care partners and individuals with dementia
• Respite and in-home services
• Day centers and PACE programs
• 24-hour hotlines
• Safety resources
• Transportation
In addition, clear documentation in the medical record of a dementia diagnosis (after appropriately counseling the patient and care partner) and of a patient’s primary support person, authorized representative, emergency contact, and/or medical-decision-makers can all help to improve optimal care coordination.
With mounting evidence for the impact that social determinants have on overall health (including brain health), Medi-Cal and Medicare are piloting programs that also make it possible for patients to access components of comprehensive dementia care. For example, in the statewide Medi-Cal Transformation Initiative (formerly known as CalAIM), San Diego’s MediCal managed care plans can offer community supports such as personal care for Activities of Daily Living or Instrumental Activities of Daily Living and Respite care for care partners. In addition, the Centers for Medicare and Medicaid Services (CMS) plan to start testing a new voluntary nationwide model — the Guiding of an Improved Dementia Experience (GUIDE) — where participating providers have the potential to offer home-based care management, 24/7 access to a care team, caregiver education and training, referrals to community resources, and subsidies for respite care.
Research4 suggests that up to half of dementia risk is due to modifiable risk factors (cardiovascular, psychosocial, and health behaviors, specifically), many of which are associated with healthcare disparities and unmet social determinants of health across the lifespan. Upstream, these factors start with early childhood access to education, midlife hearing loss5, and, most markedly, the same cardiovascular risk factors that lead to heart disease (e.g., tobacco use, hyperlipidemia, hypertension, diabetes, etc.) Risk reduction later in life includes adopting a healthier plant-based diet; increasing physical activity6; improving social connections7; and challenging and maintaining brain activity. Refer to Champions for Health website for a patient-facing handout, “Healthy Body Healthy Mind.”
A recent article in The New England Journal of Medicine8 provides inspiration for what could be and what we can start working toward right now to provide the highest standard of gerineuropalliative care. The article discusses how “just as advances in cancer treatments (e.g., immuno-
therapy) have increased the salience of geriatrics and palliative care for treating the whole person, the advent of disease-modifying treatments for dementia makes gerineuropalliative dementia care more pressing, given potentially burdensome treatment protocols and side effects, prognostic uncertainty, and the need to navigate discoordinated healthcare.”
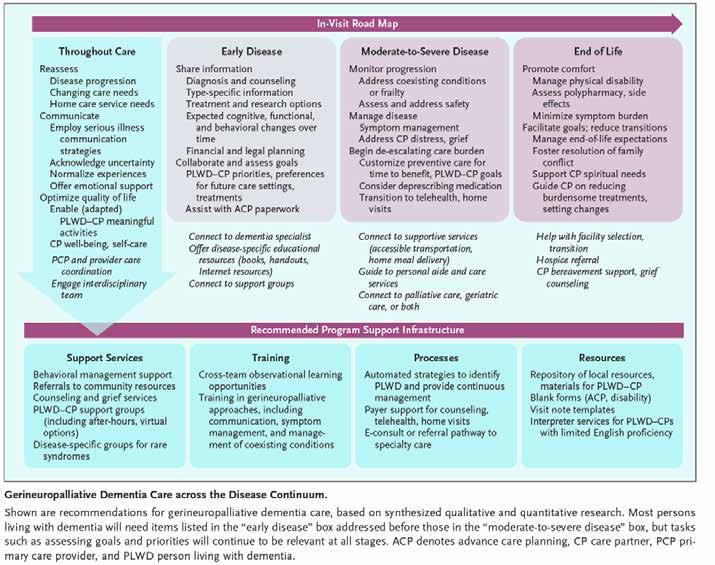

We are hopeful and grateful that when patients and families come to us with concerns about brain health or dementia (regardless of whether they meet medical eligibility criteria and/or can access anti-amyloid medications as we await more data), we will be able to confidently and truthfully say to patients and families, “There is a lot we can offer you, right here, right now.”
(Watch the January 2024 San Diego County Medical Society Bioethics Commission recorded meeting for a balanced perspective of existing studies on the anti-amyloid medications and panel discussion on ethical controversies such as medicine’s role in social determinants of health.) .
Citations and for more information:
1. AD 2000 trial, AD2000 Collaborative Group, Long-Term Donepezil Treatment in 565 Patients with Alzheimer’s Disease (AD2000): Randomised Double-Blind Trial. Lancet. 2004 Jun;363(9427):21052115. DOI: 10.1016/S0140-6736(04)16499-4
2. Haggerty et al. Recommendations to Improve Payment Policies for Comprehensive Dementia Care PMID: Journal of the American Geriatric Society; Volume 68, Issue 11, November 2020, Pages 2478-2485 32975812. doi.org/10.1111/jgs.16807
3. Callahan C, et al; Implementing dementia care models in primary care settings: The Aging Brain Care Medical Home; Aging & Mental Health, Vol 15 2011, Issue 1: Memory Services. https://doi. org/10.1080/13607861003801052
4. Jaffe K; Modifiable Risk Factors and Prevention of Dementia: What Is the Latest Evidence? JAMA Intern Med. 2018;178(2):281-282. doi. org/10.1001/jamainternmed.2017.7299
5. Lin F, Pike J, et al; Hearing intervention versus health education control to reduce cognitive decline in older adults with hearing loss in the USA (ACHIEVE): a multicentre, randomised controlled trial. The Lancet, July 18, 2023 https://www.thelancet.com/journals/ lancet/article/PIIS0140-6736(23)01406-X/abstract
6. Groot C, Hooghiemstra AM, Raijmakers PG, et al. The Effect of Physical Activity on Cognitive Function in Patients with Dementia: A Meta-Analysis of Randomized Control Trials. Ageing Res Rev. 2016 Jan;25:13-23. DOI: 10.1016/j.arr.2015.11.005
7. Saczynski JS, Pfeifer LA, Masaki K, Korf ESC, Laurin D, White L, et al. The Effect of Social Engagement on Incident Dementia: The Honolulu-Asia Aging Study. Am J Epidemiol. 2006 Mar;163(5):433440. DOI: 10.1093/aje/kwj061
8. Harrison K, Boyd N, Ritchie C; Toward Gerineuropalliative Care for Patients with Dementia. N Engl J Med 2023; 389:775-778 (https:// www.nejm.org/doi/full/10.1056/NEJMp2301347

Lindsey Yourman, MD, is the chief geriatric officer of the County of San Diego Health and Human Services Agency, volunteer faculty as an associate professor in the division of Geriatrics, Gerontology, and Palliative Care at UCSD, and a member of the Alzheimer’s Project Clinical Roundtable.
Ian Neel, MD, is an associate clinical professor in the division of Geriatrics, Gerontology, and Palliative Care at UC San Diego. He is the medical director of the geriatric medicine consult service at Senior Behavioral Health as well as the medical consultant for UC San Diego’s Brain Health and Memory Disorders clinic. He is also a member of the Alzheimer’s Project Clinical Roundtable.
THE LAST WEEKEND IN FEBRUARY MARKED THE annual SDCMS Board Retreat. Always a highlight of the year, the annual retreat is an opportunity to dedicate attention to the medical society and develop important relationships among the members.
Led by President-Elect Steve Koh, MD, we had more than 40 participants in the three-day program.
A highlight this year was an extended component on our role in policy development for the California Medical Association (CMA). Kyle Edmonds, MD, instructed the group in best ways to draft policy ideas and how to properly research existing policy, with tips in how to be successful. We then separated into breakout groups and created more than a half-dozen policy ideas to work on over the next year.
Throughout the program, we had in-depth briefings on Proposition 1 by Dr. Koh; Champions for Health from executive director Adama Dyoniziak; candidates for the March primary election by Robert Hertzka, MD; and updates from CMA’s recent Board Retreat by William Tseng, MD.
Another significant element was a panel on dealing with polarizing issues, highlighting a desire to communicate with empathy and diplomacy. Panelists included Bob Wailes, MD, Holly Yang, MD, and Drs. Hertzka and Koh. James Hay, MD, highlighted the work of Braver Angels on this topic and an upcoming seminar they are hosting.













Floods. As Californians increasingly feel the health effects of climate change, state leaders are adopting sweeping policies they hope will fend off the worst impacts — and be replicated by other countries.
Several of them attended the United Nations Framework Convention on Climate Change, known as COP28, late last year, where more than 120 countries signed a declaration acknowledging the growing health impacts of climate change and their responsibility to keep people safe.
“Leaders from around the world are coming to these climate negotiations understanding that climate change is both killing and hurting their people,” said Wade Crowfoot, secretary of the California Natural Resources Agency, who represented California in Dubai.
In August and September 2020 alone, when dozens of wildfires burned around California, as many as 3,000 older residents may have died from wildfire smoke-related causes, according to estimates from Stanford University researchers.
California has taken steps on its own to address climate change and cut greenhouse gas emissions, such as banning the sale of new gas-powered cars and light trucks by 2035 and requiring utilities to provide a growing share of electricity from renewable sources like wind and solar. The policies are intended to reduce the state’s air pollution, which consistently ranks among the worst in the nation — especially in the San Joaquin Valley and the Los Angeles basin — and contributes to the premature deaths of thousands of Californians annually.
Regulators estimate California’s climate policies could
reduce the cost of hospitalizations, asthma cases, and lost work and school days by $199 billion in 2045 alone.
“If we don’t take action, it has an impact on public health. It also has a massive economic impact,” said Liane Randolph, who chairs the California Air Resources Board and also attended the conference.
Crowfoot, Randolph, and another attendee, Christina Snider-Ashtari, Democratic Gov. Gavin Newsom’s Tribal Affairs secretary, spoke with KFF Health News senior correspondent Samantha Young to explain how California is trying to keep its nearly 40 million residents safe. The interviews have been edited for length and clarity.
Q: What is the biggest health threat that climate change poses for Californians, and what is the state doing about it?
Randolph: The biggest challenges are extreme heat and wildfire smoke. And climate change is making the existing health threats worse. For example, heat increases ozone pollution. What is happening is that high-heat days are becoming more common. And while we have reduced ozone levels and nitrogen oxides in the atmosphere, we still end up with days where air quality levels are exceeded because we have more high-heat days that create additional smog.
We have a comprehensive document, called the Scoping Plan, to tackle climate change. The key piece of it is reducing the combustion of fossil fuels because those have public health impacts on the ground for air quality and they have climate impacts. We are moving to zero-emission vehicles, moving to renewable energy, moving to zero-emission space and water heaters. All of these strategies move us away from the combustion of fossil fuels.
California itself cannot tackle climate change worldwide, but what we can do is support new technologies that can then be replicated, ideally, around the country and around the world. We’re encouraging the development of zero-emission vehicles all the way from passenger vehicles to heavyduty vehicles. We’re fostering the market for technologies like heat pumps that allow people to heat and cool their homes without using gas. All of these things need to get support and have a market. We can create markets that can percolate through the rest of the world.
Snider-Ashtari: Many tribes have been relocated to places that don’t have good access to water, and that was by design, by the federal government and the state. So, tribes are already in places where it’s designed to be inhospitable to life. As things get worse, and there are more stressors, less water, hotter summers, Indian country are these islands of vulnerability within California.
A lot of our ancestral food sources that tribes have relied on are either not there or they are there at the wrong time of year. Salmon populations are on the decline. Native people can’t access abalone right now because of ocean acidification and overharvesting. The same thing with seaweed, which is a major supplement to diets. With certain species not able to thrive in a changing climate, you’re just not going to be able
to get the same kind of nutrition in rural California that you would in other places. We will have bigger impacts on the health stressors that Native people already suffer from, like diabetes at higher rates.
One of the things that we’ve been looking at with tribes is reintroducing traditional practices to address climate issues. We’ve been reintegrating cultural burning practices so the smoke will clear out invasive pests and make sure the forest floor is healthy. We can promote forest health to prevent large-scale wildfires, which leads to the pumping of carbon into the atmosphere, and we can create better crops for Native people so they can have their critical food sources. Tribes aren’t going anywhere. The rest of us could move anywhere we want, but tribes — these are our ancestral homelands.
Crowfoot: We are experiencing multiple overlapping health threats. Wildfire, drought, and extreme heat cost lives in California. Wildfire gets a lot of attention, particularly when it’s barreling down on communities, which is a major danger. But less discussed are the smoke impacts from wildfire. During our worst wildfire seasons, weeks of dangerous air blanket the state. For Californians that have preexisting medical conditions, for the elderly, for kids, that is really dangerous.
As it relates to drought, several hundred thousand Californians lose their access to water in their homes during drought because they’re on shallow groundwater wells. That’s a major health impact in the most vulnerable, poorest, most isolated communities in California. And then there’s extreme heat. It’s now the biggest climate-driven killer in California and other parts of the world.
Building our resilience to these climate impacts is a matter of health and safety. We have really clear action plans. We have one on water resilience, specifically on water supply and how we’re going to supplant the loss of water supply in the next two decades. We have one on wildfire. Not only are we improving the ability to fight wildfires, but we’re spending a ton of money protecting communities, improving landscapes. And we have an Extreme Heat Action Plan to improve protections for people, everything from noticing when extreme heat is bearing down, providing places of refuge in communities where people don’t have air conditioning, and trying to get more shade cover at schools and on the streets.
Samantha Young is a senior correspondent for KFF Health News, where this article first appeared, and is an awardwinning journalist with 25 years of experience who covers healthcare politics and policy in California, focusing on government accountability and industry influence. As a former reporter for The Associated Press, Samantha covered the California legislature and the Schwarzenegger administration, statewide political campaigns, and the state’s groundbreaking climate change law.

on patients and clinicians, but artificial intelligence (AI) has the potential to simplify the process, health policy experts said during an online panel discussion hosted by the Kaiser Family Foundation.
Recently the backlash against prior authorization requirements has been growing. “Even when appropriate, prior authorization creates delays to care, and that can [worsen] outcomes, and can affect things like cancer survival,” said Fumiko Chino, MD, a radiation oncologist at Memorial Sloan Kettering Cancer Center in New York City.
One in three physicians blamed the process for resulting in a serious adverse event, such as hospitalizations, permanent impairment, or even death, according to a 2023 survey from the American Medical Association. Even just one day of delay can potentially mean uncontrolled pain for a patient, said Dr. Chino. For patients with cervical cancer, each day of delay “equates to a 1% decreased local control rate,” she said. “If you have a five-day delay, that’s a 5% decreased local control rate.”
Anna Schwamlein Howard, JD, principal for policy development at the American Cancer Society Cancer Action Network (ACS/CAN) in Washington, DC, said delays in care can have
financial costs as well. A patient waiting days for a pain medication to be approved may wind up in the emergency room, which increases costs for both the patient and the payer, an outcome Howard argued is “penny-wise and pound foolish.”
But Troyen Brennan, MD, a former executive at CVS Care and an adjunct professor at the Harvard T.H. Chan School of Public Health in Boston, defended the process, arguing that it cuts down on unnecessary care. About 15% to 30% of all care in the U.S. healthcare system is ineffective, Dr. Brennan said.
Plus, there are “really not any good studies ... showing actual harm,” he argued. “There are a lot of surveys from physicians, in particular, that say that there are tremendous delays, but there’s obviously a response bias associated with this.”
Also, prior authorization is “fairly heavily regulated,” Dr. Brennan added. If private health plans don’t meet certain requirements — seven days to a decision for standard requests, and 14 days for expedited — they can be fined by the Centers for Medicare & Medicaid Services (CMS) or the Department of Labor.
Estimating costs for both the provider and the insurer, the return on investment of such policies is about 10 to 1, he said. “Does it seem like a reasonable thing for the insurance [company] to continue to do? It does,” he said.
However, due to criticism from legislators, patients, and physicians, he’s seeing a “retreat back away from utilization management” — another term for prior authorization — in cases where there isn’t the same return on investment, and a sharpened focus on more “non-controversial” requests, Dr. Brennan said.
In January, CMS issued a final rule aiming to streamline the prior authorization
process which called on Medicare Advantage plans, state Medicaid and Children’s Health Insurance Program (CHIP) fee-for-service programs, Medicaid managed care plans, and CHIP managed care entities to file prior authorization decisions within 72 hours for expedited requests and seven calendar days for standard requests. The rule also mandates that insurers must publicly report their prior authorization metrics. Prescription drugs are excluded from the rule.
Howard, speaking for ACS/CAN, said her organization “would like to see those timelines sharpened” to 72 hours for non-expedited requests, and 24 hours for expedited requests.
Dr. Brennan went further, suggesting that “this whole process could be completely automated” through computer programs that would take a prior authorization request and “would basically interrogate the electronic medical record and come back with a decision immediately.”
He noted that in dozens of places throughout the final rule, CMS called on the Office of the National Coordinator for Health Information Technology (ONC) to “do your part” in calling for changes to the electronic medical record.
Asked whether AI could improve prior authorization and prevent delays, panelists were cautiously optimistic. “I wouldn’t be afraid of it, sort of ex ante, but you would want






to make sure you’ve got complete transparency,” Dr. Brennan said, adding that ultimately these decisions come down to a discussion between a physician like Dr. Chino and another radiation oncologist. (One large insurer, UnitedHealth, was recently sued in Minnesota by two families who claimed that the insurer used a faulty AI algorithm to deny necessary care to their since-deceased elderly family members.)
Dr. Chino said she welcomed AI with “some caveats,” noting that marginalized populations are more likely to be “missing key elements” in their electronic medical records. “And then you’ve trained a machine based on a data set that is essentially racist.” In an email to MedPage Today, Dr. Chino explained that an AI prior authorization system might “inadvertently flag charts for denials” based on “flawed datasets,” which might then determine that “other patients” — including those coded as high-income and white — are “low risk,” and speed up those approvals.
“So if one group gets faster approvals, it can perpetuate inequity and disparate care,” she said.
Shannon Firth has been reporting on health policy for MedPage Today, where this article first appeared, as its Washington correspondent since 2014.

THE KETOGENIC DIET HAS LONG BEEN KNOWN for its use in treatment-resistant epilepsy, but attention is now turning to its potential benefits in mental illness as well.
Could something as simple as a diet actually improve notoriously difficult-to-treat conditions including major depressive disorder, bipolar disorder, and schizophrenia?
The evidence to date has been less rigorous than goldstandard randomized controlled trials. But new studies are underway, and more clinicians are keen to explore reports of patients whose psychiatric conditions improved when they adhered to a ketogenic diet.
Nonetheless, there are challenges inherent to dietary intervention trials that must be mitigated, and broader buy-in from
patients are going to have more tools to treat their mental health disorders.”
Dr. Ramsey noted that some randomized controlled trials have shown that dietary interventions — albeit not specifically the ketogenic diet — can help improve depression.
For instance, the SMILES trial showed better symptomatic improvement and remission rates with a dietary intervention compared with a control social support group, and the AMMEND study showed greater improvements in symptoms and quality of life for young men on the Mediterranean diet compared with controls.
As for the ketogenic diet specifically, Georgia Ede, MD, a nutritional psychiatrist based in Massachusetts, told MedPage Today that the body of research for its use in psychiatric conditions “is really starting to grow.”
the medical community at large remains to be seen.
“There have to be randomized trials before we can make enthusiastic and evidence-based treatment recommendations,” Drew Ramsey, MD, a nutritional psychiatrist and member of the American Psychiatric Association, told MedPage Today. “That said, I’m hopeful and optimistic that
Dr. Ede co-authored a French study published in Frontiers in Psychiatry in 2022 titled “The Ketogenic Diet for Refractory Mental Illness: A Retrospective Analysis of 31 Inpatients.”
Patients with severe and persistent mental illness (major depressive disorder, bipolar disorder, and schizoaffective disorder), with poorly controlled symptoms were admitted to a psychiatric hospital and placed on a ketogenic diet as an adjunct to conventional care.
Though three patients were unable to adhere to the diet for more than 14 days, the researchers concluded that following the ketogenic diet for treatment-refractory mental illness was “feasible, well-tolerated, and associated with significant and substantial improvements in depression and psychosis symptoms and multiple markers of metabolic health.”
More than 40% of patients experienced remission from their diagnosis, Dr. Ede said, and 64% left the hospital on less psychiatric medication than when they entered.
Among other recent research, a feasibility pilot study of the ketogenic diet in bipolar disorder was recently completed in the U.K.
Findings of the study, published in BJPsych Open last October, found that of 27 participants, 20 completed six to eight weeks of the ketogenic diet. A majority of participants reached and maintained ketosis, indicating adherence to the diet, and adverse events were generally mild and modifiable, the researchers found.
In an email, a spokesperson for the National Institute of Mental Health (NIMH) pointed MedPage Today to two trials that it is supporting in an investigation of the effects of the ketogenic diet on mental illness — one led by researchers based in Maryland, and another by
a team in California.
Deanna Kelly, PharmD, of the Maryland Psychiatric Research Center — a joint program between the University of Maryland School of Medicine and state Department of Health — is leading an inpatient randomized controlled trial of a gluten-free diet in a subgroup of people with schizophrenia.
These patients were found to have high levels of IgG anti-gliadin antibodies. The goal of the trial is to determine whether participants benefit from a gluten-free diet, predicted to result in lower levels of schizophrenia symptoms and antibodies to gliadin.
The inpatient setting enables complete control over what the participants eat, she said. Lending another layer of stringency to the trial is that individuals performing the psychiatric ratings are blinded.
Judith Ford, PhD, of the University of California San Francisco, who also received NIMH funding, and her team will look at whether neural network instability in schizophrenia can be improved by a ketogenic diet. Particularly, they are exploring whether deficient glucose metabolism — at least partially mediated by insulin resistance — contributes to network instability in the disorder, a mechanism underlying accelerated aging and cognitive impairment in patients.
“So far, it’s helping people’s overall intellectual function,” Ford said.
As for current funding opportunities available through NIMH, the agency told MedPage Today that there are not any that “specifically focus on diet and mental health,” but that it would “consider relevant applications submitted under broader funding opportunity announcements.”
A number of researchers pursuing work pertaining to ketogenic diets and mental health have turned to a private organization funding work in this area.
Securing federal funding can be difficult, in part because of the need to show targets of engagement, Kelly said. Even if someone had a cure for depression, she explained, they would have to show, for instance, what links the outcome, improvement in depression, to the brain.
“People have to spend their lives [in order to] understand the target,” Kelly said. “Not everybody can afford that. Sometimes, it’s not really even that clear.”
“That’s why we need other funding agencies to step up and take risks,” she added.
Other hurdles for researchers include added costs for inpatient stays during clinical trials, and the lack of pharmaceutical funding for dietary interventions, Kelly said.
Mackenzie Cervenka, MD, medical director of the Adult Epilepsy Diet Center at Johns Hopkins Hospital in Baltimore and a member of the American Epilepsy Society, noted that potential interest in and promise of ketogenic diets for mental health is due in part to a more than 100-year history of the use of such diets for epilepsy patients.
However, Dr. Cervenka also noted that “awareness that there can be long-term side effects of the diet is important.”
If patients no longer see their doctor for prescription medications, they may not be monitored for potential areas of concern like kidney stones, hyperlipidemia, and bone health, she said.
Dr. Cervenka also noted that short-term studies “might not be sufficient to indicate what the benefits could be in real-world applications.” For instance, “in our experience about 50% [of individuals] will stop the diet within six months, whether they are responders or not,” she said.
This can be due to adherence difficulties, she said, or in the case of patients with epilepsy, not achieving sufficient seizure control, for instance, for the purpose of driving.
Dr. Ramsey also cautioned that it’s important to remember that “not everything works for everybody.”
Ultimately, regarding randomized controlled trials, “we need more,” Dr. Ede said. “Many clinicians will not feel comfortable until we have more.”
Jennifer Henderson is an enterprise and investigative writer for MedPage Today, where this article first appeared.

professionals can get mental health treatment without risking notifying the boards that regulate their licenses.
Too often, healthcare workers wait to seek counseling or addiction treatment, causing their work and patient care to suffer, said Jean Branscum, CEO of the Montana Medical Association, an industry group representing doctors.
“They’ve invested so much time in their career,” Branscum said. “To have anything jeopardize that is a big worry on their mind.”
Montana, like other states, has a recovery program for health professionals who have a substance use disorder or mental illness. However, medical associations say such programs often come with invasive monitoring, even for voluntary care. And gray areas about when a mental illness should become public breeds fear that seeking care jeopardizes a medical career.
Montana is among the states looking to boost confidential care for health professionals as long as they’re not deemed a danger to themselves or patients. In recent years, at least a dozen states have considered or created confidential wellness programs to offer clinicians help early on for career burnout or mental health issues. States have also reworked medical licensing questions to avoid scrutiny for providers who need mental health treatment. The changes are modeled after Virginia legislation from 2020.
During a legislative committee meeting last month, advocates for Montana medical professionals asked state lawmakers to follow Virginia’s lead. They say the goal is twofold: to get clinicians treatment before patients are at risk and to curtail the workforce burnout that’s partly fueled by untreated stress.
Montana’s existing medical monitoring program, the Montana Recovery Program, is run by the global company Maximus. Montana’s professional advocates had backed another nonprofit to run Montana’s program, which didn’t win the state contract.
The Montana Recovery Program declined a request for an interview, instead referring KFF Health News to the Montana Department of Labor & Industry, which oversees the state’s medical licensing boards. Department staffers didn’t comment by deadline.
In a Medscape survey released this year, 20% of physicians said they felt depressed, with job burnout as a leading factor. The majority said confiding in other doctors wasn’t practical. Some said they might not tell anyone about their depression out of fear people would doubt their abilities, or that their employer or medical board could find out.
Health professionals are leaving their jobs. They’re retiring early, reducing work hours, or switching careers. That further dwindles patients’ care options when there already aren’t enough providers to go around. The federal government estimates 74 million people live in an area without enough primary care services due to a workforce shortage.
Aiming to ensure patient safety, state medical boards can suspend or revoke clinicians’ rights to practice medicine if substance use or psychological disorders impair their work. Those cases are rare. One study found roughly 4,400 actions against the licenses of U.S. physicians for either substance use or psychological impairment from 2004 to 2020.
Nonetheless, workforce advocates say disclosure requirements cause some health professionals to dodge questions
about mental health histories on licensing and insurance forms or forgo care altogether. They’re worried divulging any weakness will signal they shouldn’t practice medicine.
The mental health questions health workers are asked vary by state and profession. For example, nurses in Montana renewing their license are asked if they have any psychological condition or substance use that limited their ability to practice “with reasonable skill and safety” in the previous six months. Along with being asked about substance use on the job, doctors are required to say whether they’ve experienced a mental condition that “might adversely affect any aspect of your ability to perform.”
“When I see that question on my renewal, do I have to report that I was depressed because I was going through a really tough divorce?” Branscum cited as an example of workers’ uncertainty. “You know, my life is turned upside down now. Am I obligated to report that?”
A “yes” wouldn’t immediately result in licensing problems. Those who do report mental health troubles would be flagged by state workers as a potential concern. They could end up before the board’s same screening panel that recommends whether to revoke a license, or be referred to long-term monitoring with regular screening.
Additionally, health professionals are required to report when other clinicians show unprofessionalism or have potential issues that affect performance. Branscum said medical professionals worry that what they say in a counseling session could be flagged for licensing boards, or that a coworker may make a report if they seem depressed at work.
Bob Sise, MD, a Montana addiction psychiatrist and cofounder of the nonprofit 406 Recovery, told state lawmakers that job stressors are playing into workers’ mental health challenges, such as long shifts and heavy patient loads. And with the rising cost of healthcare, physicians feel they’re sacrificing their commitment to healing as they routinely substitute optimal treatment for lesser care that patients can afford.
Dr. Sise said his practice now has roughly 20 health professionals as patients.
“They were able to access care before it was too late,” Dr. Sise said. “But they’re the exception.”
In Virginia, doctors, nurses, physician assistants, pharmacists, and students can join the state’s SafeHaven program. Melina Davis, CEO of the Medical Society of Virginia, said the service offers counseling and peer coaching with staffers available to answer a call 24/7.
“If you only have a moment at 2 a.m., or that’s when you had the chance to first process the death of a patient, then you can talk to somebody,” Davis said.
Those in the program are assured that those conversations are privileged and can’t be used in lawsuits. This year, the state is considering adding medical diagnoses under the program’s confidential protections.
States that have followed suit have slight variations, but most create a “safe haven” with two types of wellness and
reporting systems. Those who seek out care before they’re impaired at work have broad privacy protections. The other defines a disciplinary track and monitoring system for those who pose a risk to themselves or others. Indiana and South Dakota followed Virginia’s lead in 2021.
States are also narrowing the time frame that licensing boards can ask about mental illness history. The American Medical Association has encouraged states to require healthcare workers to disclose current physical or mental health conditions, not past diagnoses.
Last year, Georgia updated its license renewal form to ask doctors if any current condition “for which you are not being appropriately treated” affects their ability to practice medicine. That update replaces a request for seven years of mental health history.
Even outside the “safe haven” framework, some states are grappling with how to grant doctors privacy while guaranteeing patient safety.
The Medical Board of California is creating a program to treat and monitor doctors with alcohol and drug illnesses. But patients’ advocates have argued too much privacy, even for voluntary treatment, could risk consumers’ wellbeing. They told the state medical board that patients have a right to know if their doctor has an addiction.
Davis said states should debate how to balance physicians’ privacy and patients’ safety.
“We in medical professions are supposed to be saving lives,” she said. “Where’s the line where that starts to fall off, where their personal situation could affect that? And how does the system know?”
According to the Montana Recovery Program website, it’s not a program of discipline but instead one “of support, monitoring, and accountability.” Participants may self-refer to the program or be referred by their licensing board.
Branscum, with the Montana Medical Association, said the state’s monitoring program is needed for cases in which an illness impairs a clinician’s work. But she wants that form of treatment to become the exception.
Vicky Byrd, CEO of the Montana Nurses Association, said nurses don’t tend to join the program until they’re forced to in order to keep their license. That leaves many nurses struggling in silence until untreated illness shows up in their work, she said.
“Let’s get them taken care of before it has to go on their license,” Byrd said.
Because after that point, she said, it’s hard to recover.
Katheryn Houghton is a healthcare correspondent for KFF Health News, where this article first appeared. The issues she covers include health policy and politics, access to treatment, and the business of healthcare. She owes her health reporting start to years spent in daily newsrooms, including those of the Bozeman Daily Chronicle and the Daily Inter Lake

ANESTHESIOLOGY RESIDENT MAX FEINSTEIN, MD, explores how marijuana use can complicate medical procedures and the perioperative period. The following is a transcript of a video posted on Dr. Feinstein’s YouTube channel:
Feinstein: If there is one person who you should definitely not lie to about any drug use, it’s your anesthesiologist. My name is Max Feinstein and I’m an anesthesiologist filming here at Mount Sinai Hospital in New York City. In this video, I describe the anesthesiologists’ considerations for patients who consume marijuana. If you find this video interesting or helpful, I’d really appreciate it if you liked it and subscribe to the channel. Let’s dive in.
This video does not contain medical advice. It’s just a YouTube video. But if you need medical advice, you should talk to your doctor. It’s estimated that about 15% of the population in the United States uses marijuana. That’s 25 million people.
News Anchor: It is about that time, 4:20 here on 4/20. We’re going to head back to Hippie Hill in San Francisco’s Golden Gate Park for the main event as we call it. Christien Kafton there right now and folks getting things fired up.
Feinstein: And so that means that an anesthesiologist is virtually guaranteed to encounter patients who use marijuana. Worldwide it’s estimated that about 200 million people use marijuana, so the same concept applies for anesthesiologists across the globe. For marijuana, as with any other drug, anesthesiologists are concerned about the effect that the drug has on the patient’s mind and also on their body in the perioperative period, meaning before, during, and after surgery. Many of the effects of marijuana are wellstudied and the extent of those effects is really dependent on whether the marijuana use is acute or chronic. No pun intended, sorry.
As far as the brain or central nervous system is concerned, marijuana is known to have cross-tolerance with opioid receptors, meaning that patients may have an increased opioid requirement. It’s also been shown that patients who are regular marijuana users have a higher requirement for midazolam, which is a short-acting benzodiazepine in cases with sedation. Midazolam is also frequently given to help patients feel relaxed before surgery. This is the medication that makes up the anesthesia cocktail that people sometimes reference.
There are also documented effects that marijuana has on the heart, namely both acute and chronic use can lead to a higher baseline heart rate. There are also a number of arrhythmias that have been associated with marijuana use that include atrial fibrillation, ventricular tachycardia, ventricular fibrillation, and AV block, to name a few.
The presence of an arrhythmia might be a reason that an anesthesiologist would delay a surgery for further workup and treatment or proceed to surgery with special precautions like electrodes to deliver a shock if needed. It’s also been documented the risk of a myocardial infarction is approximately eight times higher in patients who have used marijuana within the last 60 minutes. When marijuana is inhaled, it can also have effects on a patient’s airway. Namely whether it’s smoked or vaped, marijuana can lead to increased irritation throughout the airway. This can be associated with a number of complications, including airway edema, obstruction, bronchospasm, bronchitis, and emphysema.
There are also hematologic considerations or blood considerations for patients who use marijuana and also take the medication warfarin. Warfarin is a powerful blood thinner that is sometimes prescribed for people who have heart
valve replacements, clotting disorders, or a heart rhythm called atrial fibrillation. It’s also the main ingredient used in rat poison, but that’s neither here nor there. Warfarin is a blood thinner that is metabolized through an enzyme made in the liver. That enzyme is called CYP3A4. Marijuana has the effect of inhibiting CYP3A4’s activity, meaning that there is less metabolism of warfarin, meaning that more warfarin is present in a patient’s blood, which means that a patient could be more prone to bleeding during surgery.
As I already alluded to, marijuana does alter some of the enzymes in a patient’s liver that are responsible for metabolism of medications. There is actually a very long list of medications whose metabolism is altered by marijuana. That list includes warfarin, clopidogrel, NSAIDs (or non-steroidal anti-inflammatory drugs), immunosuppressants, fentanyl, oxycodone, codeine, and steroids.
In a kind of funny-titled study about the effect that marijuana has on patients and their post-operative pain, it was found that patients who regularly use marijuana have significantly higher post-operative pain scores as compared to the patients who don’t use marijuana. This probably has to do with the fact that many of the medications that are given for pain control are actually metabolized by enzymes that are interfered with by marijuana.
There is also a recommendation to consider increasing the dose of medication that is provided for patients who are regular users of marijuana for the reasons that we’ve already talked about. Given the propensity for marijuana that’s smoked or vaped to irritate a patient’s airway, anesthesiologists should have everything ready to take care of a hyperreactive airway.
Everything that I mentioned in this video is evidencebased and all of the studies that I have cited are included in the description below. If you found this video interesting, you might want to check out this video where I go through all of the medications that are commonly used as part of a general anesthetic. Thanks very much for watching. I’ll see you next time.



Dr. Feinstein is a PGY-4 anesthesiology resident at the Mount Sinai Hospital in New York City, where he is also chief resident of teaching. His YouTube channel focuses on perioperative medicine, especially the role of the anesthesiologist. This transcript originally appeared in MedPage Today




PSYCHIATRIST AVAILABLE! Accepting new patients for medication management, crisis visits, ADHD, cognitive testing, and psychotherapy. Out of network physician servicing La Jolla and San Diego. Visit hylermed.com or call 619-707-1554.
COUNTY OF SAN DIEGO PROBATION DEPT.
MEDICAL DIRECTOR: The Probation Medical Director plays a pivotal role in the medical management team, spearheading the Justice-Involved California Advancing and Innovating Medi-Cal (CalAIM) program. This initiative targets individuals with a history of incarceration, who face elevated risks of harm. California’s groundbreaking approval on January 26, 2023, allows Medicaid services to be extended to aid in their transition back into society. The Medical Director’s responsibilities encompass CalAIM’s implementation, oversight of clinical programs, and seamless integration of services for justice-involved youth. This leadership role involves collaboration with various stakeholders, ensuring quality healthcare, behavioral support, and a successful return to the community. https://www.governmentjobs.com/careers/ sdcounty/jobs/4193564/medical-director-probation23034008u?keywords=medical%20director&pagetype=j obOpportunitiesJobs
PART-TIME CARDIOLOGIST POSITION AVAIL-
ABLE: Cardiology office in San Marcos seeking part-time cardiologist. Please send resume to Dr. Keith Brady at uabresearchdoc@yahoo.com.
INTERNAL MEDICINE PHYSICIAN: Federally Qualified Health Center located in San Diego County has an opening for an Internal Medicine Physician. This position reports to the chief medical officer and provides the full scope of primary care services, including diagnosis, treatment, and coordination of care to its patients. The candidate should be board eligible and working toward certification in Internal Medicine. Competitive base salary, CME education, four weeks paid vacation, year one, 401K plan, no evenings and weekends. Monday through Friday, 8:00 am to 5:00 p.m. For more information or to apply, please contact Dr. Keith Brady at: uabresearchdoc@ yahoo.com.
FAMILY MEDICINE/INTERNAL MEDICINE PHYSI -
CIAN: San Diego Family Care is seeking a Family Medicine/Internal Medicine Physician (MD/DO) at its Linda Vista location to provide outpatient care for acute and chronic conditions to a diverse adult population. San Diego Family Care is a federally qualified, culturally competent and affordable health center in San Diego, CA. Job duties include providing complete, high quality primary care and participation in supporting quality assurance programs. Benefits include flexible schedules, no call requirements, a robust benefits package, and competitive salary. If interested, please email CV to sdfcinfo@sdfamilycare.org or call us at (858) 810-8700.
MEDICAL CONSULTANT (MD/DO): The County of San Diego is currently accepting applications from qualified candidates for Medical Consultant-Public Health Services. Vacancies are in the Public Health Services, Epidemiology and Immunization Services Branch (EISB) and Tuberculosis (TB) Control and Refugee Health Branch. Salary: $183,747.20–$204,900.80 annually. An additional 10% for Board Certified Specialty and 15% for relevant sub-specialty. For job posting information visit https:// www.governmentjobs.com/careers/sdcounty?keywords =23416202PHS.
MEDICAL DIRECTOR, FULL-TIME: FATHER JOE’S
VILLAGES: Join us in ending homelessness! We are a dynamic team that runs an FQHC. The Medical Director oversees clinical aspects of the primary care, psychiatry, dental and behavioral health. This position will be a mix of clinic and admin time and will have direct reports (Dental Director, Director of Behavioral Health, and frontline primary care/psychiatry providers). Reports to the Chief Medical Officer, who is responsible for all aspects of the clinic. The Medical Director is a counterpart to the Clinic Director (who oversees admin staff, MA/RN team, billing, PSRs, etc.). See FJV Jobs to apply.
SEEKING MEDICAL DIRECTOR : subcontracted position: 4-8 hours per month. Responsibilities: 1. Support case conferences, refractory SUD, co‐occurring conditions, specialty populations. 2. Conduct clinical trainings on issues relevant to staff (e.g., documentation, ASAM Criteria, DSM‐5, MAT, WM, co‐occurring conditions) 3. Provide oversight and clinical supervision. 4. Refer co‐occurring conditions. 5. Lead Quality Improvement functions (e.g., Quality Improvement Projects, clinical team meetings, etc.). 6. Attend annually 5 hours of continuing medical education on addiction medicine. Required by contract
with San Diego County BHS, position is for a Physician licensed by CA Medical Board or CA Osteopathic Medical Board. Contact Name: Jennifer Ratoff: e-mail: jratoff@ secondchanceprogram.org, phone: 619-839-0950
PSYCHIATRIST SPECIALIST: The County of San Diego is currently accepting applications from qualified candidates. Annual Salary: $258,294.40. Note: An additional 10% is paid for Board Certification, or 15% for Board Certification that includes a subspecialty. Why choose the County? 1. Fully paid malpractice insurance; 2. 13 paid holidays; 3. 13 sick days per year; 4. Vacation: 10 days (1-4 years of service); 15 days (5-14 years of service; 20 days (15+ years); 5. Defined benefit retirement program; 6. Cafeteria-style health plan with flexible spending; 7. Wellness incentives. Psychiatrist-Specialists perform professional psychiatric work involving the examination, diagnosis, and treatment of specialty forensics, children/adolescents and or geriatric patients. This is the specialty journey level class in the series that requires a fellowship or experience in child and adolescent psychiatry or forensic psychiatry. For more information visit our website at sandiegocounty. gov/hr or select this link to go directly to the Psychiatrist Specialist application.
PRIMARY CARE PHYSICIAN: Imperial Valley Family Care Medical Group is looking for Board Certified/Board Eligible Primary Care Physician for their clinics in Brawley & El Centro CA. Salaried/full time position. Please fax CV/ salary requirements to Human Resources (760) 355-7731. For details about this and other jobs please go to www. ivfcmg.com
ASSISTANT, ASSOCIATE OR FULL PROFESSOR (HS CLIN, CLIN X, ADJUNCT, IN-RESIDENCE)
MED-GASTROENTEROLOGY: Faculty Position in Gastroenterology. The Department of Medicine at University of California, San Diego, Department of Medicine (http:// med.ucsd.edu/) is committed to academic excellence and diversity within the faculty, staff, and student body and is actively recruiting faculty with an interest in academia in the Division of Gastroenterology. Clinical and teaching responsibilities will include general gastroenterology. The appropriate series and appointment at the Assistant, Associate or Full Professor level will be based on the candidate’s qualifications and experience. Salary is commensurate with qualifications and based on the University of California pay scales. In-Residence appointments may require candidates to be self-funded. For more information: https://apol-recruit.ucsd.edu/JPF03179 For help contact: klsantos@health.ucsd.edu
DERMATOLOGIST NEEDED: Premier dermatology practice in La Jolla seeking a part-time BC or BE dermatologist to join our team. Busy practice with significant opportunity for a motivated, entrepreneurial physician. Work with three energetic dermatologists and a highly trained staff in a positive work environment. We care about our patients and treat our staff like family. Opportunity to do medical/surgical and cosmetic dermatology in an updated medical office with state-of-the art tools and instruments. Incentive plan will be a percentage based on production. If you are interested in finding out more information, please forward your C.V. to jmaas12@hotmail.com
INTERNAL MEDICINE PHYSICIAN: Healthcare Medical Group of La Mesa located at 7339 El Cajon Blvd is looking for a caring, compassionate, and competent physician for providing primary care services. We require well-organized and detail-oriented with excellent written and oral communication skills, and excellent interpersonal skills to provide high-quality care to our patients. We provide a competitive salary, paid time off, health insurance, 401K benefits, etc. We provide plenty of opportunities to refine your clinical competency. Our CEO Dr. Venu Prabaker, who has 30 years of teaching experience as a faculty at multiple universities including Stanford, UCSD, USC, Midwestern, Western, Samuel Merritt, Mayo, etc., will be providing teaching rounds once a week. You will also get plenty of opportunities to attend other clinical lectures at many of the 4- to 5-star restaurants in San Diego. We also have a weekly one-hour meeting for all the staff for team building and to create a “family atmosphere” to improve productivity and thereby create a win-win situation for all. Visit us at caremd.us.
RADY CHILDREN’S HOSPITAL PEDIATRICIAN POSITIONS: Rady Children’s Hospital of San Diego seeking board-certified/eligible pediatricians or family practice physicians to join the Division of Emergency Medicine in the Department of Urgent Care (UC). Candidate will work at any of our six UC sites in San Diego and Riverside Counties. The position can be any amount of FTE (fulltime equivalent) equal to or above 0.51 FTE. Must have an MD/DO or equivalent and must be board certified/eligible, have a California medical license or equivalent, PALS certification, and have a current DEA license. Contact Dr. Langley glangley@rchsd.org and Dr. Mishra smishra@ rchsd.org.
PER DIEM OBGYN LABORIST POSITION AVAILABLE:
IGO Medical Group is seeking a per diem laborist to cover Labor and Delivery and emergency calls at Scripps Memorial Hospital in La Jolla. 70 deliveries/month. 24-hour shifts preferred but negotiable. Please send inquiries by email to IGO@IGOMED.com.
MEDICAL CONSULTANT, SAN DIEGO COUNTY: The County of San Diego, Health and Human Services Agency’s Public Health Services is looking for a Board Certified Family Practice or Internal Medicine physician for the Epidemiology and Communicable Disease Division. Under general direction, incumbents perform a variety of duties necessary for the identification, diagnosis, and control of communicable diseases within the population. This position works closely with the medical and laboratory community, institutional settings, or hospital control practitioners. Learn more here: https://www.governmentjobs. com/careers/sdcounty?keywords=21416207
KAISER PERMANENTE SAN DIEGO PER DIEM
PHYSIATRIST: Southern California Permanente Medical Group is an organization with strong values, which provides our physicians with the resources and support systems to ensure they can focus on practicing medicine, connecting with one another, and providing the best possible care to their patients. For consideration or to apply, visit https://scpmgphysiciancareers.com/specialty/ physical-medicine-rehabilitation. For questions or additional information, please contact Michelle Johnson at 866-503-1860 or Michelle.S1.Johnson@kp.org. We are an AAP/EEO employer.
PRIMARY CARE PHYSICIAN POSITION: San Diego Family Care is seeking a Primary Care Physician (MD/DO) at its Linda Vista location to provide direct outpatient care for acute and chronic conditions to a diverse adult population. San Diego Family Care is a federally qualified, culturally competent and affordable health center in San Diego, CA. Job duties include providing complete, high quality primary care, and participation in supporting quality assurance programs. Benefits include flexible schedules, no call requirements, a robust benefits package, and competitive salary. If interested, please email CV to sdfcinfo@ sdfamilycare.org or call us at (858) 810- 8700.
FAMILY MEDICINE OR INTERNAL MEDICINE PHYSICIAN: TrueCare is more than just a place to work; it feels like home. Sound like a fit? We’d love to hear from you! Visit our website at www.truecare.org. Under the direction of the Chief Medical Officer and the Lead Physician, ensure the provision of effective quality medical service to the patients of the Health center. The physician is responsible for assuring clinical procedures are continually and systematically followed, patient flow is enhanced, and customer service is extended to all patients at all times.
PUBLIC HEALTH LABORATORY DIRECTOR: The County of San Diego is seeking a dynamic leader with a passion for building healthy communities. This is a unique opportunity for a qualified individual to work for a Level 3 Public Health Laboratory. The Public Health Services department, part of the County’s Health and Human Services Agency, is a local health department nationally accredited by the Public Health Accreditation Board and first of the urban health departments to be accredited. Public Health Laboratory Director-21226701UPH
NEIGHBORHOOD HEALTHCARE MD, FAMILY PRACTICE AND INTERNISTS/HOSPITALISTS: Physicians wanted, beautiful Riverside County and San Diego County- High Quality Family Practice for a private-nonprofit outpatient clinic serving the communities of Riverside County and San Diego County. Work full time schedule and receive paid family medical benefits. Malpractice coverage provided. Be part of a dynamic team voted ‘San Diego Top Docs’ by their peers. Please click the link to be directed to our website to learn more about our organization and view our careers page at www.Nhcare.org.
PHYSICIAN WANTED: Samahan Health Centers is seeking a physician for their federally qualified community health centers that emerged over forty years ago. The agency serves low-income families and individuals in the County of San Diego in two (2) strategic areas with a high density population of Filipinos/Asian and other lowincome, uninsured individuals — National City (Southern San Diego County) and Mira Mesa (North Central San Diego). The physician will report to the Medical Director and provide the full scope of primary care services, including but not limited to diagnosis, treatment, coordination of care, preventive care and health maintenance to patients. For more information and to apply, please contact Clara Rubio at (844) 200-2426 EXT 1046 or at crubio@samahanhealth.org.
PART-TIME CARDIOLOGIST AVAILABLE AFTER
7/4/23: Dr. Durgadas Narla, MD, FACC is a noninvasive cardiologist looking to work 1-2 days/week or cover an office during vacation coverage in the metro San Diego area. He retired from private practice in Michigan in 2016 and has worked in a San Marcos cardiologist office for the last 5 years, through March 2023. Board certified in cardiology and internal medicine. Active CA license with DEA, ACLS, and BCLS certification. If interested, please call (586) 206-0988 or email dasnarla@gmail.com
PRACTICE FOR SALE
GASTROENTEROLOGY GI PRACTICE FOR SALE: Looking to expand or move? Established 25+ years Gastroenterology GI office practice for sale in beautiful San Diego County, California. 500 active strong patient relationships and referral streams. Consistent total gross income of $600,000 for the past couple years; even through the pandemic. Located in a professional medical building with professional contract staff. All records and billing managed by a professional service who can assist with insurance integration. Office, staff & equipment are move-in ready. Seller will assist Buyer to ensure a smooth transition. Being On-Call optional. Contact Ferdinand @ (858) 752-1492 or ferdinand@zybex.com
OTOLARYNGOLOGY HEAD & NECK SURGERY SOLO
PRACTICE FOR SALE: Otolaryngology Head & Neck Surgery solo practice loc ated in the Ximed building on the Scripps Memorial Hospital La Jolla campus is for sale. The office is approximately 3,000 SF with 1 or 2 Physician Offices. It has 4 fully equipped exam rooms, an audio room, one procedure room, one conference room, one office manager room as well as in-house billing section, staff room and a bathroom. There is ample parking for staff and patients with close access to radiology and laboratory facilities. For further information please contact Christine Van Such at 858-354-1895 or email: mahdavim3@gmail.com
OFFICE SPACE / REAL ESTATE AVAILABLE
MEDICAL OFFICE FOR SALE OR SUBLEASE: A newly remodeled and fully built-out primary care clinic in a highly visible Medical Mall on Mira Mesa Blvd. at corner of Camino Ruiz. The office is approximately 1000 sq ft with 2 fully equipped exam rooms, 1 office, 1 nurse station, spacious and welcoming waiting room, spacious reception area, and ADA accessible restroom. All the furniture and equipment are new and modern design. Ample parking. Perfect for primary care or any specialty clinic. Please contact Nox at 619-776-5295 or noxwins@hotmail.com. Available immediately.
EL CAJON RENOVATED MEDICAL OFFICE AVAIL-
ABLE: Recently renovated, turn-key medical office in freestanding single-story unit available in El Cajon. Seven exam rooms, spacious waiting area with floor-to-ceiling windows, staff break room, doctor’s private office, multiple admin areas, manager’s office all in lovely, droughtresistant garden setting. Ample free patient parking with close access to freeways and Sharp Grossmont and Alvarado Hospitals. Safe and secure with round-the-clock monitored property, patrol, and cameras. Available March 1st. Call 24/7 on-call property manager Michelle at the Avocado Professional Center (619) 916-8393 or email help@avocadoprofessionalcenter.com.
OPERATING ROOM FOR RENT: State of the Art AAAASF Certified Operating Rooms for Rent at Outpatient Surgery of Sorrento. 5445 Oberlin Drive, San Diego 92121. Ideally located and newly built 5 star facility located with easy freeway access in the heart of San Diego in Sorrento Mesa. Facility includes two operating rooms and two recovery bays, waiting area, State of the Art UPC02 Laser, Endoscopic Equipment with easy parking. Ideal for cosmetic surgery. Competitive Rates. Call Cyndy for more information 858.658.0595 or email Cyndy@roydavidmd.com
PRIME LOCATION – MEDICAL BUILDING LEASE OR OWN OPPORTUNITY IN LA MESA: Extraordinary opportunity to lease or lease-to-own a highly visible, freeway-oriented medical building in La Mesa, on Interstate 8 at the 70th Street on-ramp. Immaculate 2-story, 7.5k square foot property with elevator and ample free onsite parking (45 spaces). Already built out and equipped with MRI/CAT machine. Easy access to both Alvarado and Sharp Grossmont Hospitals, SDSU, restaurants, and walking distance to 70th St Trolley Station. Perfect for owneruser or investor. Please contact Tracy Giordano [Coldwell Banker West, DRE# 02052571] for more information, (619) 987-5498.
POWAY MEDICAL OFFICE SPACE FOR LEASE
2/1/2024: Fully built out, turnkey 1257 sq ft ADA-compliant suite for lease. Great location in Pomerado Medical/ Dental Building, next to Palomar Med Center Poway
campus. Building restricted to medical/allied health/dental practices, currently houses ~26 suites. Ideal for small health practice as primary or satellite location. Lease includes front lobby, reception area, restrooms, large treatment area, private treatment/exam rooms. Located on second floor, elevator/stair access. Bright, natural lighting; unobstructed views of foothills. On-site parking; nearby bus service. Flexible lease terms available from 3-5 years at fair market rate. Contact Debbie Summers at debjsummers3@gmail.com (858) 382-8127.
KEARNY MESA OFFICE TO SUBLEASE/SHARE: 5643
Copley Dr., Suite 300, San Diego, CA 92111. Perfectly centrally situated within San Diego County. Equidistant to flagship hospitals of Sharp and Scripps healthcare systems. Ample free parking. Newly constructed Class A+ medical office space/medical use building. 12 exam rooms per half day available for use at fair market value rates. Basic communal medical supplies available for use (including splint/cast materials). Injectable medications and durable medical equipment (DME) and all staff to be supplied by individual physicians’ practices. 1 large exam room doubles as a minor procedure room. Ample waiting room area. In office x-ray with additional waiting area outside of the x-ray room. Orthopedic surgery centric office space. Includes access to a kitchenette/indoor break room, exterior break room and private physician workspace. Open to other MSK physician specialties and subspecialties. Building occupancy includes specialty physicians, physical therapy/occupational therapy (2nd floor), urgent care, and 5 OR ambulatory surgery center (1st floor). For inquiries contact kdowning79@gmail.com and mgamboa@ortho1.com for more information. Available for occupancy projected as February 2024.
LA JOLLA/UTC OFFICE TO SUBLEASE OR SHARE:
Modern upscale office near Scripps Memorial, UCSD hospital, and the UTC mall. One large exam/procedure room and one regular-sized exam room. Large physician office for consults as well. Ample waiting room area. Can accommodate any specialty or Internal Medicine. Multiple days per week and full use of the office is available. If interested please email drphilipw@gmail.com
ENCINITAS MEDICAL SPACE AVAILABLE: Newly updated office space located in a medical office building. Two large exam rooms are available M-F and suitable for all types of practice, including subspecialties needing equipment space. Building consists of primary and specialist physicians, great for networking and referrals. Includes access to the break room, bathroom and reception. Large parking lot with free parking for patients. Possibility to share receptionist or bring your own. Please contact coastdocgroup@gmail.com for more information.
NORTH COUNTY MEDICAL SPACE AVAILABLE: 2023
W. Vista Way, Suite C, Vista CA 92082. Newly renovated, large office space located in an upscale medical office with ample free parking. Furnishings, decor, and atmosphere are upscale and inviting. It is a great place to build your practice, network and clientele. Just a few blocks from Tri-City Medical Center and across from the urgent care. Includes: multiple exam rooms, access to a kitchenette/break room, two bathrooms, and spacious reception area all located on the property. Wi-Fi is not included. For inquiries contact hosalkarofficeassist@gmail.com or call/ text (858)740-1928.
PHYSICIAN OFFICE SPACE FOR LEASE. 1500 Sq ft.
3 exam room. Large private office. Large reception area and patient prep room. New upgraded flooring. Private entrance. Located in Rancho Bernardo in prime central location. Easy access to interstate 15. Palomar /Pomerado within 10 min. Security card access during off hours. $2,500/month. Contact: (619) 585-0476. Ask for Peg.
HILLCREST OFFICE TO SUBLEASE OR SHARE: Gorgeous office located across from Scripps Mercy hospital. Office is approximately 2000 sq. ft. with procedure/effusion room. Office is fully staffed and looking to add a new provider. We currently have Rheumatology/Pulmonary/ Allergy specialists but can accommodate any specialty or Internal Medicine. Multiple days per week and full use of office is available. If interested please reach out to Melissa Coronado at Melissa@sdpulmonary.com or call (619) 819-7224.
SUBLEASE AVAILABLE: Sublease available in Del Mar off 5 freeway. Share rent. 2100 sq ft office in professional building. Utilities included. Great opportunity in a very desirable area. 858-342-3104.
CHULA VISTA MEDICAL OFFICE: Ready with 8 patient rooms, 2,000sf, excellent parking ratios, Lease $4,000/ mo. No need to spend a penny. Call Dr. Vin, 619-405-6307 vsnnk@yahoo.com
OFFICE SPACE AVAILABLE IN BANKERS HILL: Approximately 500sq feet suite available to lease, includes private bathroom. Located at beautiful Bankers Hill. For more details, please call Claudia at 619-501-4758.
OFFICE SPACE IN EL CENTRO, CA TO SHARE: Office in El Centro in excellent location, close to El Centro Regional Medical Centre Hospital is seeking Doctors of any specialty to share the office space. The office is fully furnished. It consists of 8 exam rooms, nurse station, Dr. office, conference room, kitchenette and beautiful reception. If you are interested or need more information please contact Katia at 760-427-3328 or email at Feminacareo@ gmail.com
OFFICE SPACE / REAL ESTATE WANTED
MEDICAL OFFICE SPACE WANTED IN HILLCREST/ BANKERS HILL AREA. Mercy Physicians Medical Group (MPMG) specialist is looking for office space near Scripps Mercy Hospital. Open to lease or share office space, full time needed. Please respond to rjvallonedpm@sbcglobal. net or 858-945-0903.
UROLOGY OFFICE CLOSING 6/2023—EQUIPMENT
AVAILABLE: Six fully furnished exam rooms including tables (2 bench, 3 power chair/table, 1 knee stirrup), rolling stools, lights, step stools, patient chairs. Waiting room chairs, tables, magazine rack. Specialty items—Shimadzu ultrasound, SciCan sterilizer, Dyonics camera with Sharp monitor, Medtronic Duet urodynamics with T-DOC catheters, Bard prostate biopsy gun with needles, Cooper Surgical urodynamics, Elmed ESU cautery, AO 4 lens microscope. RICOH MP-3054 printer with low print count. For more information contact: r.pua@cox.net.
NON-PHYSICIAN POSITIONS AVAILABLE
RESEARCH SCIENTISTS: (non-tenured, Assistant, Associate or Full level): The University of California, San Diego campus multidisciplinary Organized Research Units (ORUs) https://research.ucsd.edu/ORU/index.html are conducting an open search. Research Scientists are extramurally funded, academic researchers who develop and lead independent creative research programs similar to Ladder Rank Professors. They are expected to serve as Principal Investigators on extramural grants, generate high caliber publications and research products, engage in university and public service, continuously demonstrate independent, high quality, significant research activity and scholarly reputation. Appointments and duration vary depending on the length of the research project and availability of funding. https://apol-recruit.ucsd.edu/ JPF03713/apply
PROJECT SCIENTISTS: Project Scientists (non-tenured, Assistant, Associate or Full level): The University of California, San Diego, Office of Research Affairs https:// research.ucsd.edu/, in support of the campus multidisciplinary Organized Research Units (ORUs) https:// research.ucsd.edu/ORU/index.html is conducting an open search. Project Scientists are academic researchers who are expected to make significant and creative contributions to a research team, are not required to carry out independent research but will publish and carry out research or creative programs with supervision. Appointments and duration vary depending on the length of the research project and availability of funding. https://apolrecruit.ucsd.edu/JPF03262/apply
OFFICE MANAGER: 1. Hiring, Training, Managing staff on procedures/policies. Monitors continuing compliance and office statistics. Oversee stocking/maintenance of supplies, retail. Equipment/ facilities management. Daily bookkeeping, collections. 2. Ensure smooth/efficient patient flow with increasing production/collections. 3. Create a friendly environment where patients expectations are exceeded, where staff can work together as a team. 4. Ensure staff working at maximum productivity/efficiency.
Salary: 60-70K depending on experience/qualifications. Benefits: healthcare reimbursement, PTO, retirement, employee discount, bonuses, commission. Contact: info@ manageyourage.com
ASSISTANT PUBLIC HEALTH LAB DIRECTOR: The County of San Diego is currently accepting applications for Assistant Public Health Lab Director. The future incumbent for Assistant Public Health Lab Director will assist in managing public health laboratory personnel who perform laboratory activities for the purpose of identifying, controlling, and preventing disease in the community, as well as assist with the development and implementation of policy and procedures relating to the control and prevention of disease and other health threats. Please visit the County of San Diego website for more information and to apply online.