FROM FROZEN TO FOCUSED
EXPERIENCES OVER STUFF CAREGIVING THROUGH CLOSED DOORS

FROM FROZEN TO FOCUSED
EXPERIENCES OVER STUFF CAREGIVING THROUGH CLOSED DOORS

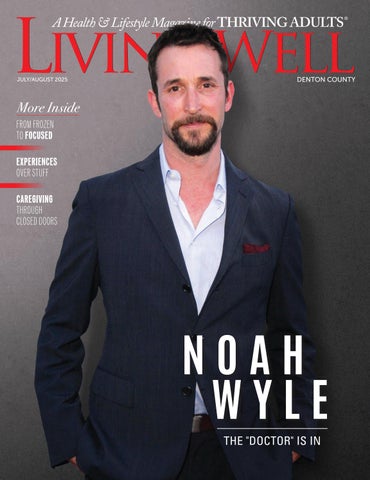
THE "DOCTOR" IS IN

Denton Rehab is a locally owned and operated skilled nursing facility that is licensed by the State of Texas and certified to participate in both the Medicare and Medicaid programs. Our core management team has worked together for years and has decades of experience providing compassionate healthcare.
When you require professional, dependable, skilled nursing care to regain your health and strength, chose the expert team at Denton Rehab. We invite you to stop by and meet our friendly staff.

We’re excited to show you our beautiful new community in Denton, located on six beautiful acres conveniently located next to Medical City Denton.
Our facility has 94 private beds with ensuite and shower. We have two suites that include ensuite, shower and a living area.
Our new community has three living areas, two dining areas, a private dining area for families, cultural center, sitting parlor, beauty shop, activities center, whirlpool room, therapy gym, and eight covered outdoor areas to relax and view nature and the beautiful, landscaped grounds. Our state-of-the-art kitchen uses green technology to provide healthier, more delicious food.
Denton Rehab’s nurses and certified nurse aides provide around-theclock care. Doctors and nurse practitioners make rounds three times a week while our medical director makes rounds twice a week. Our number one goal is helping you recover and rebuild your life. Our Focus is You!
Texas Hip and Knee Center Fellowship Co-Director and Faculty at the Anne Burnett Marion School of Medicine at Texas Christian University
Dr. David Shau is a native Texan, born in Fort Worth, TX. He graduated high school in Flower Mound, TX, and attended the University of Texas at Austin, where he studied biomedical engineering. Dr. Shau then ventured out-of-state to work at leading academic orthopedic surgery centers, including Vanderbilt University, Emory University, and University of California, San Francisco, before being recruited to return home to practice at the premier DFW joint replacement group, the Texas Hip and Knee Center (THK).
Dr. Shau has quickly built his practice through connecting with his community, committing to quality service, and delivering excellent patient care. He utilizes a variety of techniques and approaches for hip and knee care, including direct anterior hip replacements, and offers technology-assisted surgeries, such as Mako Technology for partial and total joint replacements. He also specializes in revision joint surgeries and enjoys complex, challenging cases. As a result of dedicating himself to his craft, his partners at THK promoted him to Fellowship Co-Director early in his practice. Dr. Shau also serves as a Physician Development Coach and is an Assistant Professor at the Burnett School of Medicine at TCU, where he enjoys his roles as a teacher, mentor, and coach.
In his free time, he enjoys food, sports, music, and spending time with his wife and daughter. For more information on Dr. Shau’s care philosophy and the techniques/approaches offered for hip and knee care, please visit DavidShauMD.com.




Every issue of LIVING WELL Magazine gives us the opportunity to spotlight stories that resonate, and this edition is filled with voices and topics that remind us why living well means something different to each of us.

Gracing the cover, we profile actor Noah Wyle, whose return to medical drama in The Pitt offers a raw, authentic portrayal of life inside a modern emergency room. Wyle’s evolution—from his career-defining run on ER to his creative leadership role today— reflects a deeper commitment to both his craft and the real-life healthcare professionals who inspired him along the way. His story is one of perspective, empathy, and the power of art to reflect and respond to the world around us.
In these pages, you’ll also find practical, encouraging advice on overcoming overwhelm, a state that many of us can relate to in today’s always-on world. Sometimes, the first step is simply to take one small step forward—and this thoughtful piece offers strategies for doing just that.
If laughter truly is the best medicine, then you’ll appreciate our lighthearted take on aging starting on page 28. Laughing Our Way Through Aging shines a much-needed spotlight on the humor found in the everyday absurdities of growing older. It’s a fun—and honest—reminder that while we can’t stop the clock, we can certainly choose how we respond to it.
We also touch on the increasingly popular philosophy of valuing experiences over material things on page 46. Whether it’s travel, time with family, or simply creating memories close to home, these experiences often become the richest investments we make.
As always, it’s our privilege to bring you these stories—stories that celebrate resilience, joy, and the countless ways people throughout Denton, Texoma, and beyond are writing their own living well narratives.
Enjoy the issue—and here’s to making every day a little more meaningful.
Live well,
PRESIDENT & CEO
SAM HOUSTON
VICE PRESIDENT & CFO SPRING HOUSTON
EDITOR, FEATURE WRITER & SOCIAL MEDIA
SONDRA BARR
ART DIRECTOR
VANESSA FRYER
ACCOUNTS MANAGER JENNIFER BEAVERS
WEBSITE LYDIA ROGERS
ADVERTISING & SALES
TEXAS: Denton County, Dallas County, Collin County
TEXAS & OKLAHOMA: Texoma Area
WRITE TO US:
Tell us who you would like to see featured on the cover, or what subjects you would like covered in upcoming editions of LIVING WELL MAGAZINE at info@livingwellmag.com
SUBSCRIPTIONS & CUSTOMER INQUIRIES
Houstons of Dallas Publishing, Inc. 102 E. Broadway, #901 Prosper, TX 75078
www.LivingWellmag.com
Phone: (214) 507-1000 Fax: (855) 248-2132
LIVING WELL MAGAZINE is a source for quality educational articles on living a healthy, vibrant life. Our focus is on connecting our readers with the latest information on a host of topics relevant to their evolving life. From cutting edge medical news and procedures to top-tier financial, legal and lifestyle information. Connecting readers to leading medical and business professionals in their community in Texas and Oklahoma.
JULY/AUGUST 2025 All advertisements in this Magazine are placed by third parties. We do not control or endorse either the advertisements or their content. Further, we do not
refers to the name of this Magazine, and all versions of Living Well Magazine as well as Houstons of Dallas Publishing, Inc.






Total
Headache

By SONDRA BARR
Noah Wyle never intended to wear a stethoscope again.
After his record-setting, 254-episode run as Dr. John Carter on ER—a role that made him a household name and earned him Emmy and Golden Globe nods—he vowed to steer clear of any medical role that might seem like déjà vu. But then the world changed. And so did Wyle.
“I wasn’t working. Nobody was working,” Wyle told PBS News’ Geoff Bennett. “And I get a lot of my sense of balance from going to work every day and being creative... I didn’t realize how much I really needed that until I didn’t have an opportunity to do it.”
During that same time, Wyle started receiving messages from healthcare workers who had found inspiration in ER. Some had chosen medicine because of Dr. Carter. Others, deep in the trenches of COVID-19, were simply reaching out in desperation. “They were saying things like, ‘Carter, where are you?’” he recalled in Variety. “‘It’s really hard out here.’”
Those messages lit a spark. The result? The Pitt, a gritty, real-time medical drama streaming on Max, where Wyle stars as Dr. Michael “Robby” Robinavitch—and also serves as executive producer and writer.
“I felt a certain responsibility to continue to be part of their medical journey,” he told Katie Couric. “Every show after COVID needed to reflect those radical changes. And I hadn’t really seen one yet do that.”
Unlike most series, The Pitt doesn’t rush through plot points. Each of its 15 episodes unfolds over a single hour, following one relentless shift in the ER. There’s no music score to manipulate emotions, just raw, fluorescent-lit reality. “It feels more like doing a play,” Wyle said to PBS. “It feels very live.”
Authenticity was non-negotiable. Cast members underwent a two-week medical bootcamp—“They went home with their suture kits and sewed up chickens,” Wyle told Couric—and the writing team shaped episodes around real-world interviews with medical professionals. “We ask, ‘What’s not on TV that needs to be?’” Wyle explained to PBS. “Then we take what we’ve got and somehow end up with a show.”
This commitment to realism extends to the emotional terrain as well. One of the season’s most talked-about moments is Dr. Robby’s quiet breakdown, where he crumbles under the weight of his own unprocessed trauma. “That breakdown scene was why I wanted to do the show,” Wyle told Variety. “I just invited the world to watch it.”
It’s a moment that resonates with Wyle’s own journey—one that’s been deeply shaped by empathy and activism.

I KNEW SO MANY PEOPLE MORE DESERVING OF THE SUCCESS.
Born in Hollywood to an orthopedic nurse mother and an engineer father, Wyle was raised in a house steeped in art and social awareness. “Our house was a bit of a salon,” he said in an interview for Th Thread. “We were always being taken to the theater or gallery openings… I was marinated in a cultural soup that I didn’t even know I was being marinated in.”
He caught the acting bug during a high school play. “It was the first time somebody outside my family told me I was good at something,” he recalled in Th Thread. “And I just chased that dopamine hit for the next 45 years.”
Success came early and fast. He was just 22 when ER premiered. “I used to say I was living in an apartment with a cat and a ficus, and I walked off that show 15 years later, married with two kids,” Wyle told Th Thread. “Jumped on one train, one man got off the train. Totally different guy.”
But fame also came with a side of imposter syndrome. “I knew so many people more deserving of the success… I immediately thought, I need to democratize this success, amortize it among everybody that I know in order to feel a bit more deserving of it,” he said in the same documentary.
That drive to give back stuck. Over the years, Wyle has lent his name, time, and heart to causes ranging from animal rescue to international human rights. After witnessing Human Rights Watch’s efforts in Macedonia to document war crimes during the Balkan conflict, he joined their California board. “It was law and medicine working hand in hand to bring justice,” he recalled in Th Thread. “And I really loved the way they conducted those interviews.”
He’s also a long-time supporter of animal rights, inspired in part by actor and activist James Cromwell. “I had this big piece of property... so I was taking all these animals that were being rescued off of highways,” Wyle shared. “I had cows and chickens and pigs and emus.... And I still have a few.”
These days, Wyle lives atop a mountain with his wife— “a Capricorn,” he jokes to Th Thread and their animals. “When you’re born with the name Noah, kind of goes with the territory.”
At 54, Wyle finds himself not only back in scrubs, but also at the helm of one of the most acclaimed shows of his career. “It’s been amazing to just have the perspective of longevity and to be able to be a resource,” he told PBS. “If anything, I’m just trying to boost their confidence, alleviate their anxieties, and remind them that this is a different type of show. You can paint with a much finer brush because we are all links in a chain.”
Still, not everything has gone smoothly. A potential revival stalled due to legal disputes with Michael Crich ton’s estate. “I’ve never felt less celebratory of that achievement than I do this year,” he admitted to riety. “It taints the legacy, and it shouldn’t have.”
But the setback led to unexpected creative free dom. “We pivoted as far in the opposite direction as we could in order to tell the story we wanted to tell,” he said. “Not for litigious reasons, but because we didn’t want to retread our own creative work.”
With The Pitt, he’s doing more than revisiting old territory—he’s reimag ining it through a lens shaped by experience, intention, and deep compassion. “It’s been the most gratifying thing I’ve ever done in my life,” Wyle told “It really has been a dream.”
And for Wyle, living well means more than success—it means being of service, telling stories that matter, and giving voice to those who too often go unheard. Wheth er in scrubs or not, he’s still answering the call.
AND I JUST CHASED THAT DOPAMINE HIT FOR THE NEXT 45 YEARS.










Dr. Courtney is a board-certified orthopedic spine surgeon located in Plano, Texas. A Louisiana native, he attended Louisiana State University for medical school, and completed residency at Texas A&M followed by a fellowship at the Florida Neck and Back Institute.
SPECIALTIES:
• Back Pain
• Neck Pain
• Spine Pain
• Disc Replacement
• Microdiscectomy
• Spinal Fusion
• Minimally Invasive Surgery
• Steroid Injections
• Physical Therapy
“I believe in treating each of my patients with honesty, dignity, and respect. My patients come away from our shared interactions feeling confident, assured that they are truly in the best hands. Throughout my career, I have remained laser-focused on providing world-class care and innovation to the patients I treat on a daily basis. I look forward to getting to know you!”






Texas Back Institute (TBI) has served the North Texas area in spine care for over 45 years. An uncompromising desire to put patients first and provide individualized spine care has helped change the treatment options available to patients for neck and back pain.
Today, TBI is a leader in artificial disc replacement, minimally invasive spine surgery, complex revision surgery, and treatment of spinal deformity. TBI has trained hundreds of surgeons, scientists, and allied health professionals now practicing worldwide. Its research institute employs state-of-the-art technology and is actively involved in many clinical trials, including artificial disc replacement, minimally invasive technologies, and robotic spine surgery. Texas Back Institute has remained one of the most academic practices in spine care. It is one of the largest multidisciplinary spine centers in the world, providing comprehensive care for neck and back pain. With a fully dedicated staff of board-certified orthopedic spine surgeons, neurosurgeons, physiatrists, and physical therapists, the TBI team works together to support its mission of helping patients get back to life. The 26 physicians at Texas Back Institute are leaders in the surgical
and nonsurgical treatment options for back and neck pain, from the most common outpatient procedures to the most complex cases. Thanks to the unmatched expertise of the medical staff, the advanced diagnostic testing, and an unparalleled commitment to patient care, the Texas Back Institute physicians can identify the potential cause of your pain and create a treatment plan specific to your needs.
Texas Back Institute has developed several spine specialty programs. These include the Minimally Invasive Spine Surgery Center, Center for Disc Replacement, Scoliosis and Spine Tumor Center, and Complex Back Surgery Center. These programs give patients access to highly-trained care teams who focus specifically on these areas of spine care, allowing patients in the North Texas area access to treatment options for their individual problems from physicians with extensive experience in these areas.
“At Texas Back Institute, finding the right solution for each patient and offering the least invasive treatment is core to our belief and the foundation for all treatment plans.” Dr. Michael Duffy.


ALLIANCE
3025 N. Tarrant Pkwy., Ste. 220 Fort Worth (Alliance), TX 76177
ARGYLE
310 FM 407E, Ste. 100 Argyle, TX 76226
DALLAS
12222 N. Central Expy. Pavilion II, Ste. 310 Dallas, TX 75243
DENTON
3537 S. Interstate 35, Ste. 308 Denton, TX 76210
FLOWER MOUND
4370 Medical Arts Dr. River Walk Bldg. III, Ste. 230 Flower Mound, TX 75028
FORT WORTH
1650 W. Rosedale St. Ste. 301 Fort Worth, TX 76104
FRISCO
5575 Frisco Square Blvd. Ste. 400 Frisco, TX 75034
LEWISVILLE
500 W. Main St., Ste. 380 Lewisville, TX 75057
MCKINNEY
4510 Medical Center Dr., Ste. 106 McKinney, TX 75069
NORTH RICHLAND HILLS
4351 Booth Calloway Dr., Ste. 404 Fort Worth, TX 76180
CENTRAL PLANO
4001 W. 15th St. Ste. 455 Medical Office Bldg. III Plano, TX 75093
PLANO
6020 W. Parker Rd. Ste. 200 Plano, TX 75093
ROCKWALL
3164 Horizon Rd. Ste. 100 Rockwall, TX 75032
SASCHE
4650 President George Bush Turnpike, Ste. 100 Sachse, TX 75048
By RACHEL FOSTER
Are you feeling overwhelmed and stuck? We’ve all been there at some point: sitting at the edge of a task we know we need to do, maybe even want to do, yet somehow... we just can’t begin. Instead, we stare at the list, scroll our phones, reorganize the junk drawer—anything to avoid the one thing we promised ourselves we’d tackle today.
This isn’t laziness. It’s overwhelm.
Overwhelm is a shape-shifter. It can look like exhaustion, anxiety, perfectionism, or distraction. But underneath it all is usually one core feeling: This is too much, and I don’t know where to start. Once that mental wall goes up, it’s incredibly hard to scale. The more you stare at the thing you need to do, the heavier it gets. Before long, even the idea of starting feels impossible. But here’s the secret most productive people don’t talk about: they hit that wall too. They just learn how to gently climb over it instead of waiting for it to disappear. And you can, too.
The first step to moving through a mental block isn’t action— it’s awareness. Overwhelm thrives in vagueness. The more abstract your thoughts are, the more your brain spins in circles. Try asking yourself: What exactly feels overwhelming right now? Is it the size of the task? The fear of doing it wrong? Not knowing how to begin? Writing it down—yes, with pen and paper—can help bring clarity. When you see your thoughts in black and white, they become easier to manage. The mess in your mind turns into something you can work with.
One of the most common causes of mental paralysis is perfectionism. We imagine the final product—the flawless report, the spotless house, the perfectly worded email—and suddenly, nothing feels good enough to even begin. That vision becomes a trap. Instead, try shrinking the task. Lower the bar. Tell yourself you’re only going to do a bad version of it—just to get started. Write the messy first paragraph. Fold one shirt. Answer one email. Doing something—even poorly—creates momentum, and momentum creates motivation. You don’t need to tackle the mountain today. Just take one step.
When you’re juggling a dozen tasks in your mind, your brain doesn’t know where to focus, so it doesn’t. It freezes. Instead of trying to do it all, pick one thing. Not the most urgent or most important—just something small that you can complete right now. Finishing even a minor task can quiet the mental noise and give you a boost of confidence. You’ve already proven you can get something done. That’s a win.
Here’s a tough truth: waiting for motivation is a trap. It’s easy to believe we need to feel ready to start—but more often, starting is what creates that feeling. Think of your brain like an engine that needs a little warm-up. The first few minutes may feel clunky and uninspired, but once you begin, something shifts. The fog lifts, the ideas come, and what felt impossible starts to feel doable. So instead of waiting for motivation to strike, just start. Even if it’s awkward. Even if you don’t feel like it. Especially if you don’t feel like it.
Sometimes, the mental block has a physical root. Cluttered spaces can make your mind feel just as messy. Try taking five minutes to tidy your workspace or clear off your desk. Even small changes in your environment can signal to your brain that it’s time to shift gears. The same goes for mental clutter. If your thoughts are bouncing between errands, emails, and things you forgot to do last week, do a quick brain dump. Write down everything that’s on your mind. Get it out of your head and onto the page so you can focus on what’s in front of you.
In an age of constant pings, notifications, and background noise, focus is harder to come by—and more precious than ever. When you’re overwhelmed, even the smallest distraction can pull you off course. Create a distraction-free zone, even if it’s just for 25 minutes. Silence your phone. Close unnecessary tabs. Let others know you’re in “focus mode.” Set a timer if that helps—knowing you only have to concentrate for a short burst can reduce the mental resistance to starting.
Breaks are not a sign of weakness. They’re a sign that you understand how your brain works best. But not all breaks are created equal. Scrolling social media might offer a momentary escape, but it often leaves you feeling even more drained. Try a short walk, stretching, a few deep breaths by a window, or making a cup of tea. These kinds of restorative breaks help your mind reset and prepare to re-engage with the task at hand.
The voice in your head matters more than you think. When you’re behind, struggling, or stuck, it’s easy to turn on yourself. “Why am I like this?” “What’s wrong with me?” “I should have finished this by now.”
But shame doesn’t motivate—it immobilizes. Try changing the script. Talk to yourself the way you would to a friend. “I’m doing the best I can.” “This is hard, but I’ve done hard things before.” “One step at a time.” Kindness isn’t selfindulgent. It’s productive. It creates a safe space for your brain to take risks and try again.
When the starting point feels impossible, shift your focus to the end. Imagine the relief of clicking “send,” the satisfaction of a clean space, the pride of completing a project. Let that image pull you forward. Sometimes, it’s not the task itself that motivates us—it’s the feeling of having done it.
The biggest lie overwhelm tells is that it’s permanent. That you’ll always feel stuck. That this task will never get done. That your brain will be foggy forever. But it’s not true. This is just a moment. A hard one, yes—but temporary. You will move forward. You will get through the task. And with every wall you climb, you build the strength to tackle the next one a little more easily.
So if you’re staring at that mental block today—breathe. Pick one small thing. Begin badly. Be kind. Protect your focus. And remember: you’ve done this before. You’ll do it again. One step at a time.

Southwest Foot & Ankle Center is a respected group of board certified foot and ankle surgeons. They are fellow trained surgeons, and board certified in wound care and reconstructive surgery. All physicians have also completed an intense residency and fellowship in the area of limb salvage, and foot and ankle surgery. The team at Southwest Foot & Ankle Center strive to make each patient’s experience personable. Our outcomes are of perfection and meticulous in surgery. As a result, patients from all over the country seek to be treated by DFW Wound Care Center.
MIS—Minimally Invasive Surgery
Heel Pain (Plantar Fasciitis) Stem Cell Therapy
Toenails

Custom Orthotics & Braces
Laser Therapy for Pain, Swelling, Arthritis, and Wounds




By ANNA REED

They carry you to the kitchen each morning, support you on evening walks through the neighborhood, and hold you steady through decades of life’s milestones. Yet, for all they do, feet are often the most ignored part of our bodies—until they demand attention.
For those of us entering life’s wiser decades, foot health is no longer just about comfort. It’s about mobility, independence, and preserving our quality of life.
When Foot Pain Isn’t Just “Part of Aging”
It’s common to assume that foot pain is just one more item on the aging checklist. But while it’s true that our feet change over time—arches can flatten, padding thins, joints stiffen—pain is not something you’re meant to endure. It’s a message. And it’s one that shouldn’t be ignored. Consider heel pain. A common culprit is plantar fasciitis, often felt as a stabbing sensation first thing in the morning. Left untreated, it can escalate to the point where every step is a challenge. Conditions like bunions or hammertoes may start small but can gradually deform your foot, limit your shoe choices, and reduce your mobility. And let’s not forget neuropathy, a numbing or tingling often associated with diabetes, which can lead to falls or wounds that won’t heal.
Here’s the truth: many of these conditions are manageable, and often treatable—especially when addressed early by a foot specialist. A good specialist doesn’t just treat the pain; they look for the source and provide a plan to prevent recurrence. That makes a world of difference when you’re trying to stay active and independent.
Few people realize just how crucial healthy feet are to balance. Your feet are your body’s foundation. If they’re unstable, it sets off a chain reaction. You might start compensating in your hips or knees, which throws off your posture and increases the risk of a fall.
Falls are no small matter. According to the CDC, one in four Americans aged 65 or older will experience a fall each year, often leading to serious injury. Sometimes the cause is simple: a loss of sensation in the feet, a painful joint, or an uneven gait—all things a foot specialist can evaluate and help improve.
Let’s talk shoes. It’s easy to keep wearing the same size and style you did 20 years ago, but our feet evolve over time. Arches flatten, toes may spread, and ligaments lose some elasticity. And yet, many people still try to squeeze into shoes that no longer suit their feet.
If your closet is full of stylish shoes that sit unused because they now hurt to wear, you’re not alone. But style and comfort don’t have to be mutually exclusive. Start by getting your feet measured once a
year. A proper fit—combined with features like arch support and a wider toe box—can prevent a world of problems.
A foot specialist can also assess how you walk and recommend custom orthotics if needed. These aren’t your grandmother’s shoe inserts—they’re designed to support your unique foot structure, improve posture, and ease pressure points.
Feet often give the first clues about other health issues. Discolored or thickened toenails might indicate a fungal infection or circulation problem. Cold, numb feet could be a sign of vascular disease. Ulcers or wounds that don’t heal might point to diabetes. These aren’t just cosmetic concerns; they’re early warning signs.
A foot specialist knows what to look for and when to investigate further. For example, they may catch signs of poor circulation before your primary doctor does, or notice a gait abnormality that’s causing hip pain. These small discoveries can lead to big improvements in your overall well-being.
Good foot health doesn’t require a major lifestyle overhaul—just intentional, consistent care. Wash your feet daily, dry them thoroughly (especially between the toes), and moisturize the soles and heels to prevent cracking. Check for any new calluses, blisters, or skin changes.
When sitting for long periods, elevate your feet to reduce swelling. Stretch your ankles and toes regularly to maintain flexibility. And if something hurts or looks suspicious—don’t wait. That’s exactly the moment to see a specialist.
Early care can make the difference between a small issue and a serious one. And there’s no shame in seeking help for your feet. You wouldn’t ignore back pain or blurred vision—why treat your feet any differently?
Your feet are your foundation. They’ve walked with you through every stage of life, carried the weight of responsibility, and kept you moving forward. As you enter your 50s, 60s, and beyond, they deserve attention, respect, and care.
Don’t wait until the pain stops you in your tracks. Whether it’s discomfort that won’t go away, changes in how you walk, or simply questions about what’s normal—consulting a foot specialist can keep you active, safe, and steady on your feet for years to come.
Because a strong foundation doesn’t just support the body. It supports your freedom.
Macular Degeneration
Diabetic Eye Disease
Retinal Vein & Artery Occlusions
Flashes & Floaters
Retinal Tears & Detachments
Macular Pucker/Epiretinal
Membrane
Macular Holes
Uveitis

At Texas Macula & Retina, our mission is to provide exceptional eye care with a focus on the diagnosis, treatment, and management of retinal disorders.
Dr. Adams is a board-certified Ophthalmologist and Ophthalmic Surgeon specializing in Vitreoretinal Surgery. His principal areas of interest include age-related macular degeneration, diabetic retinopathy, retinal detachment repair, macular surgery, retinal lasers, and secondary intraocular lens implantation.
Dr. Adams and his team are committed to preserving and improving the vision and overall quality of life for our patients by offering the most advanced and personalized retina care available.

(Before You Mistake Your Chihuahua for a Squirrel Again)
By MATTHEW K. ADAMS, MD, MBA
Let’s face it, aging is full of surprises. One day you’re reading the morning paper just fine, and the next you’re squinting at the toaster trying to figure out if that’s the bagel button or the nuclear launch code.
As a retina specialist here in North Texas, I spend my days helping people see clearly, and my nights wondering why so many folks wait way too long to get their eyes checked. So if you’re over 60, grab a glass of iced tea, pull up your recliner, and let’s go over the 10 signs you might want to give your friendly neighborhood retina doctor a call.
1. You Thik the TV Remote is Your Phone

can be a sign of trouble in the retina. Unless you’re in a disco (which I respect), call us. Time is vision when it comes to treating a retinal tear or detachment.
If you’ve ever tried to answer your Roku remote like it’s your iPhone, don’t worry, we’re not judging. But if it’s happening because you can’t see it clearly, your eyes might be trying to tell you something.
2. Straight Lines Are Looking More Like Roller Coasters
No, your wallpaper isn’t warping, and your house isn’t haunted. Wavy, distorted, or “melting” lines can be a sign of macular degeneration, a common condition we see in our older patients.
3. You’ve Got More Floaters Thn a Pool Party in July
A few floaters are normal. But if you suddenly see a storm of black specks, cobwebs, or flashes of light, especially if they come on quickly, you may have a retinal tear or detachment. That’s not a “wait and see” situation; that’s a “call us right now” kind of deal.
4. Reading the Menu Requires a Flashlight, Magnifying Glass, and Prayer
If dim lighting feels like the enemy and your reading glasses aren’t cutting it anymore, there could be more going on than just aging lenses. Conditions like cataracts or diabetic retinopathy can sneak up and blur your world.
5. You Keep Hitting the Curb, and Not in a Cool, Skater-Way
Peripheral vision loss isn’t just inconvenient, it can be dangerous. Whether it’s from glaucoma or a retinal condition, we can help before your mailbox gets taken out again.
6. Your Grandkids Keep Winning at Hide and Seek (and Thy’re Not Even Trying)
If you feel like you’re seeing less of your grandkids, not emotionally, but literally, your visual field might be shrinking. That’s worth a check.
7. Your Eyes Are Doing Thir Own Light Show
Flashes of light that look like lightning bolts, sparkles, or camera flashes
8. You’ve Got a Family History of Eye Disease
High blood pressure, diabetes, and family history of vision problems? You’ve hit the genetic jackpot, my friend. Even if you feel fine, you need regular retina exams. Prevention beats laser surgery any day.
9. You’ve Started Adjusting Your Glasses…
But Thy’re Not on Your Face
We’ve all done the forehead glasses shuffle, but if you’re constantly struggling to see even with your prescription, something’s up.
10. You Just Have a Feeling Something’s Off
Call it gut instinct, intuition, or that voice in your head saying, “maybe I should get this checked out.” If you feel like your vision’s changed, even subtly, it’s always worth a quick check up.
So, What’s the Worst That Could Happen?
Here’s the thing: many serious eye conditions, including retinal tears, vein occlusions, and macular degeneration, can be treated if caught early. But if you wait too long? That Sunday crossword might be replaced with blank stares and blurry shapes for the rest of your life.
At Texas Macula and Retina, we specialize in helping seniors across North Texas keep their vision sharp, so you can keep enjoying sunsets, grandkid selfies, and the fine print on your prescription bottles (which, let’s be honest, could be bigger).
Don’t Let Your Vision Take a Backseat
If any of these signs sound familiar, or if you just want peace of mind, come see us. We promise not to lecture you (too much), and we’ll make sure your eyes are in good shape for the road ahead. And yes, we do have big-print magazines in the waiting room. Because whether you’re 65 or 95, good vision is key to living independently, confidently, and joyfully. Call Texas Macula and Retina today and let’s keep your future in focus.

By SAMANTHA BROOKS
They raised you. Held your hand through skinned knees, school plays, heartbreaks, and hard lessons. They were strong, capable, the ones who seemed to know how the world worked. But now, the roles have quietly shifted—and not without turbulence. You see the red flags: missed medications, strange bruises, spoiled food in the fridge, bills unpaid. You worry about the stove left on, the stairs climbed in the dark, or the long drives that feel more perilous with every mile.
And yet, when you bring it up—gently, lovingly—they resist. They insist they’re fine. That you’re overreacting. That it’s their house, their life. What happens next often feels less like caregiving and more like a tugof-war. But beneath it all is something powerful: love. Messy, exhausting, enduring love.
If you’re navigating the delicate—and at times heartbreaking—reality of caring for a parent who is resistant to help while making unsafe choices, you’re not alone. This emotional terrain is both common and complicated, especially for those already juggling careers, children, and personal challenges of their own. It can feel like you’re carrying too much, stretched too thin. And still, you press on—because they’re your parent.
So how do you care for someone who doesn’t want to be cared for? How do you help without overstepping? And what do you do when their choices are putting them in danger?
One of the most important first steps is to understand what’s behind your parent’s resistance. Often, it’s not about being stubborn—it’s about fear, pride, or grief.
Losing independence is one of the hardest emotional transitions in life. Accepting help might feel like surrendering autonomy or admitting weakness. Many older adults associate care with decline, or with being seen as a burden. Others might fear losing their home or privacy. And for those with early cognitive decline, the situation becomes even more layered and fraught.
That resistance, however, doesn’t erase the very real risks. Falls, medication errors, isolation, and poor nutrition are among the leading causes of decline—and they often go unaddressed until a crisis occurs.
It’s tempting to dive straight into solutions—hiring help, installing safety equipment, taking away the car keys. But often, the most powerful tool you have is conversation. Not a lecture, but an honest and compassionate dialogue.
Try starting with curiosity. Ask how they’re feeling, what they’re worried about, what they want. Validate their fears instead of rushing past them. Avoid language that sounds controlling or condescending, and instead frame your concerns in terms of care and respect.
Phrases like “I’m not trying to take away your freedom—I’m trying to help you stay safe and independent for as long as possible,” can shift the tone dramatically. Remind them you’re on the same team, not opposing sides.
You won’t win every disagreement—and trying to control everything can fracture the relationship. Instead, prioritize the most urgent safety

issues. If your parent occasionally wears mismatched clothing, it might not be worth the emotional cost of a confrontation. But if they’re mixing up medications or wandering at night, those are red lines.
Start small. Introducing a part-time housekeeper or meal service might be easier to accept than a live-in caregiver. Sometimes easing into support makes the bigger changes feel less overwhelming.
Sometimes, you’re just too close. Hearing hard truths from a child can be more difficult than hearing it from a neutral third party. This is where professionals can be incredibly valuable.
Primary care physicians, home health nurses, social workers, or elder care specialists can provide assessments and guidance in a way that feels more objective and less personal. Hearing “Your daughter is right” from a doctor often carries more weight than any number of well-intentioned lectures from you.
It’s also wise to familiarize yourself with community resources. Many regions offer elder care support programs, transportation services, adult day centers, and in-home assessments. The Administration for Community Living (ACL.gov) and the National Association of Area Agencies on Aging (n4a.org) are good starting points.
There’s no manual for this part of life. No guidebook for how to balance your parent’s needs with your own marriage, your job, your health, your kids. And one of the most damaging myths is that you’re supposed to do it all. You are not failing if you need help. You are not selfish if you’re exhausted. You are not unloving if you say, “I can’t do this all by myself.”
Set realistic limits. Be honest about what you can do and where you need support. If your parent refuses help but won’t allow anyone else to step in, you might need to make peace with letting some consequences unfold. As painful as that sounds, enabling unsafe behavior can be more harmful in the long run.
Taking breaks, getting enough sleep, and caring for your own emotional well-being isn’t a luxury—it’s essential. You can’t pour from an empty cup.
When your parent is consistently making dangerous decisions and refuses help, and you have genuine concerns about their capacity, you may need to explore legal options. A medical evaluation can help determine whether they’re still able to manage their affairs.
If cognitive decline or a medical condition is affecting their judgment, you may need to consider powers of attorney, guardianship, or conservatorship. These are not decisions to make lightly—but they exist for situations where a loved one’s safety is genuinely at risk.
It can also be wise to have conversations about advance directives, living wills, and health care proxies before a crisis occurs. These documents offer clarity during medical emergencies and ensure that your parent’s wishes are honored.
It’s easy to let frustration and fatigue take center stage. But underneath it all, this is a season shaped by deep emotion—grief for what’s changing, fear of what’s coming, and an ache to do the right thing.
Some days, your patience will wear thin. Some days, guilt will creep in. Some days, you’ll just need to sit in the car and cry. That’s okay. That’s normal.
But as much as this journey demands of you, it also has the potential to be a time of connection, healing, and even unexpected beauty. A walk around the block. A shared memory. A rare laugh. These moments don’t solve everything—but they anchor you in what matters.
You’re not alone in this. There are millions walking this path alongside you. Reach out. Ask for help. Give yourself the same grace you’re trying to extend to your parent.
And remember: love, even when it’s complicated, is still love.




By OLIVIA GRANT
There’s something deeply reassuring about having a doctor or health care professional you genuinely trust. Whether it’s a physician who listens without rushing, a nurse who remembers your family’s names, or a specialist who helped you through a difficult diagnosis, these relationships often shape some of life’s most vulnerable and important moments. For many people, gratitude for their doctor runs deep—but when it comes to expressing that appreciation, it’s not always clear where to start.
A heartfelt “thank you” goes a long way. In the middle of a packed waiting room, during a follow-up appointment, or even through a simple note, acknowledging a health care provider’s dedication can brighten their day more than you might imagine. Many physicians carry the emotional weight of their patients’ struggles, successes, and fears. A sincere word of thanks is more than polite—it’s uplifting and affirming.
If you’re looking to go beyond a spoken thank-you, consider writing a handwritten card. In these digital times, a physical note stands out. Keep it simple and personal—share how their care made you feel or how it made a difference. You don’t need to use big words or write a long letter. Just speaking from the heart is enough. Health care professionals often keep these kinds of notes for years. They’re reminders of why they chose their path in the first place.
Another impactful way to show appreciation is by leaving a public review. Google, Yelp, and even health care-specific platforms like Healthgrades or Zocdoc can be great places to let others know about the positive experiences you’ve had. These reviews are often what someone sees when they’re searching for a new provider. Your honest words might help another person feel more confident walking into their first appointment.
Don’t underestimate the value of sharing your praise within your local community, too. Our region, including this magazine, hosts annual “Top Doc” or “Best of” polls and casting a vote for a trusted provider is another meaningful way to show your appreciation. These local honors often reflect the voices of real patients, not just professional peers, and they can be a boost for a doctor’s morale and reputation. It’s one more way to say, “You made a difference in my life—and others should know.”
If your health care provider works as part of a larger clinic, hospice provider, practice, or hospital system, you might also consider sending a note to their supervisor. A quick email or letter recognizing exceptional care—whether it was a physician, nurse, medical assistant, or front desk staff—can reinforce a culture of kindness and attentiveness within that organization. Professionals who consistently go above
and beyond deserve to be recognized not just by patients, but within their own workplace as well.
For those who are more active on social media, a simple shoutout (while respecting privacy and avoiding sharing personal medical details) can also have a ripple effect. Mentioning your gratitude for great care and tagging the clinic or organization helps amplify your appreciation while encouraging others to consider the provider you value so highly. Just be sure to keep any identifying medical information private—your kind words don’t need to include specifics to be meaningful.
Of course, not all thanks have to be written or spoken. Referring friends and family to your trusted provider is one of the most powerful compliments you can offer. If someone you know is looking for a new doctor, specialist, or therapist, sharing your positive experience can ease their concerns and help them find a good fit. Word-ofmouth is a powerful force in building trust, especially in matters as personal as health.
And if you’re ever inclined to show appreciation through a small gesture—perhaps a thank-you card during the holidays, a coffee gift card, or a treat left at the front desk—it’s always appreciated. Just check ahead to make sure gifts are appropriate or allowed under clinic policies. Often, a plate of cookies for the office staff or a bouquet for the front desk brightens everyone’s day and lets them know their kindness hasn’t gone unnoticed.
The truth is, health care can be a demanding and emotionally intense field. Providers carry so much on their shoulders, often beyond what patients can see. A few moments of acknowledgment, a thoughtful word, or a public vote of confidence can offer real encouragement. You don’t need to wait for a major occasion— sometimes the best thank-you is the one given in the quiet after a routine visit or a follow-up call that reminded you someone’s looking out for you.
If there’s a doctor, nurse, or care provider who has supported you with skill, compassion, and grace, don’t keep it to yourself. Say thank you—and let the world know how much that care meant to you.

By RAYMOND “BUZZ” HARPER
Aging is a strange little trick the universe plays on us. One day you’re sleeping like a baby, waking up bright-eyed and dewyskinned. The next, you sprain something putting on socks and your back makes noises like a microwave popcorn bag. It’s nature’s way of saying, “Surprise! You’re now creaky and mysterious.” But before you start investing in orthopedic flip-flops and buying bananas for their fiber instead of their flavor, let’s talk about the secret weapon that makes this whole wild ride not just tolerable—but downright funny.
Humor. It’s not just a coping mechanism; it’s the duct tape holding the whole operation together.
Let’s be honest: aging comes with a parade of indignities that nobody warned us about. Yes, we expected to get a little gray around the edges. We might’ve even braced for a little sagging here or there. But did anyone mention the rogue eyebrow hair that’s now long enough to braid? Or the fact that your knees audibly negotiate before stand-
ing up? And let’s not even start on the reading glasses situation. Every room now has at least three pairs, none of which are ever where you actually need them.
You don’t fid humor in these moments—you need it. Otherwise, you’re just sitting in a waiting room holding a Ziploc full of pills, wondering if your doctor’s old enough to drive.
Science backs up the value of a good chuckle. According to the Mayo Clinic, laughter stimulates your organs, improves your immune system, relieves pain, and increases personal satisfaction. So essentially, it’s nature’s multivitamin—minus the fish oil aftertaste. Also, it’s free. Try saying that about hearing aids or progressive lenses.
There’s something beautifully rebellious about laughing in the face of aging. It’s like flipping off the Grim Reaper with jazz hands. Because while your body may be muttering things like “we don’t bend that way anymore,” your humor gets sharper, bolder, and—let’s admit it—weird-
You don’t find humor in these moments— you need it. Otherwise, you’re just sitting in a waiting room holding a Ziploc full of pills, wondering if your doctor’s old enough to drive.
er. Suddenly, it’s completely normal to spend 20 minutes talking with friends about the metaphysical horror of Tupperware lids. (“Why do they multiply? Where is the lid for this one? Did it run off with my youth?”)
The joy of growing older is that you finally get the full absurdity of life. You start noticing things younger folks miss, like the fact that every new medical procedure sounds like the name of a 1970s rock band. (“What did the doctor say?” “Oh, just a mild case of Frozen Shoulder. Opening for Steely Dan this weekend.”)
You also develop a curious relationship with technology, which is the source of at least half your daily laughs. There’s nothing like trying to update your phone and accidentally turning on voice dictation while muttering curse words under your breath. And the moment you finally master your smart TV remote, the manufacturer releases a new version with fewer buttons and more confusion. You don’t just laugh at technology—you laugh to keep from hurling it into the fireplace.
And then there’s fashion. Remember when clothing was an exciting form of self-expression? Now, if it has an elastic waistband and doesn’t itch, it’s couture. Forget heels and skinny jeans—give us memory foam shoes and pants that forgive. The pinnacle of style is now the holy trifecta: stretch, softness, and the ability to get them off quickly in case of a bathroom emergency.
Speaking of which, bathrooms now get a lot more airtime in your conversations. There’s a kind of camaraderie in sharing the truth that your bladder now keeps a more demanding schedule than your toddler grandchild ever did. And no one tells you that aging means you can pull a muscle sneezing. That’s not even fair. That’s not even a sport. But laughing about these things doesn’t diminish them—it takes their power away. It turns them from medical complaints into party anecdotes. “I fell off the curb the other day. Not because I was drunk. Because I forgot how curbs work.” That’s funny. That’s human. That’s healing.
The real magic of humor, though, is what it does for relationships. The shared laughter with friends over lunch when someone forgets what story they were telling mid-sentence. The knowing chuckle when someone walks into the room and announces, “I don’t remem-
ber why I came in here, but I’m committing to the experience.” Humor connects us, reminds us we’re not alone, and makes even the weirdest symptoms feel a little less scary.
You begin to develop a healthy irreverence. You realize the world is full of too many serious people and not enough people who will put googly eyes on their vitamins just to make the mornings more entertaining. And while some might be chasing youth through expensive serums and kale smoothies, the rest of us are putting bubble wrap on our garden kneelers and calling it “joint protection with flair.”
Some of the funniest people you’ll ever meet are the ones who’ve been around long enough to know better. They’ve survived decades of hairstyles, heartbreaks, questionable casseroles, and the agony of dial-up internet. They’ve had kids, or raised plants, or both, and lived to laugh about it. They’ve learned that if you don’t find humor in a lost car key or a misplaced bra (which was eventually discovered in the freezer), you’re going to spend way too much time frowning—and nobody looks good with frown lines.
The truth is, aging can be hilarious if you let it. There’s a moment of pure comedy when you put your car keys in the fridge, your sandwich in your purse, and your glasses on top of your head (while asking your spouse where your glasses are). And while yes, some days are harder than others, the moments where you can step back and laugh—those are the moments that keep you going.
So maybe we don’t bounce back as quickly, maybe we forget why we walked into a room, maybe we now describe the weather based on what body part hurts. But we also laugh harder, longer, and with deeper appreciation than ever before.
Let’s face it: if life is a sitcom, we’ve made it to the good seasons. The characters are well-developed, the plot twists are more dramatic, and the jokes? Chef’s kiss.
And if you’re still worried about aging, just remember this: every laugh line is a souvenir from a moment that made you giggle until you snorted. Every gray hair is a tiny lightning bolt of wisdom. And every joke you tell is proof that time may be marching on—but you’ve still got the best punchlines.
Now go find your glasses. They’re probably in the laundry basket again.
“Where we are committed to excellence”


•Private and semi-private studios, some with kitchen elements and/or Frenchdoor courtyard patios
•Flat-Screen televisions
•32 channels of satellite television service
•Wi-Fi internet access
•Electric beds for easy comfort adjustments
•Living room with fireplace and player piano
The Cantex Advantage
Cantex Continuing Care Network has been performing the highest standards of transitional healthcare and long-term residential services for more than 30 years. Ask anyone who knows. Cantex stands for quality.

•Library with computer stations and complimentary internet access
•Chapel
•Neighborhood cafes with complimentary premium beverages and snacks
•Restaurant-Style dining room
•Beauty/barber shop with full-time beautician
•Activity program with community outings
•Sedan and van for resident transportation



•Around-the-clock skilled nursing
•Physical, Occupational, and Speech Therapies
•Wound Management
•Intravenous Therapy
•Tracheotomy Care
•Physician Services
•Medication Administration
•Enteral/Parenteral Therapy
•X-Ray Services
•Laboratory Services

DFW Wound Care Center is a group of wound care specialists in all of the DFW area. They are fellow trained surgeons, and board certified in wound care and reconstructive surgery. All physicians have also completed an intense residency and fellowship in the area of limb salvage, and foot and ankle surgery. When it comes to wound care and limb salvage, DFW Wound Care Center has the knowledge and experience to successfully treat your condition. As a result, patients from all over the country seek to be treated by DFW Wound Care Center.

Whether caused by diabetes, infection or disease, any wound that will not heal can be very serious. If you are experiencing a wound or ulcer that will not properly heal, our wound care center can provide a range of expert treatment options best in each case. We offer non-surgical and surgical treatments for:
Diabetic Wounds & Ulcers
Arterial Ulcers
Infected Wounds
Open Wounds
Pressure Ulcers
Vascular Wounds
Acute Wounds
Non-Healing Wounds
Chronic Wounds
Surgical Wounds
Traumatic Wounds




PLANO CLINIC 5804 Coit Road, Ste. 100 Plano, TX 75023
LEWISVILLE CLINIC 502 N. Valley Pkwy., #2 Lewisville, TX 75067
IRVING CLINIC
6161 N. State Hwy. 161, Ste. 320 Irving, TX 75038
DESOTO CLINIC 714 N. Hampton Rd. DeSoto, TX 75115
Josh Creel, DC is a chiropractor with Airrosti, a healthcare group that specializes in rapid recovery for soft tissue injuries by utilizing manual therapy—a hands-on treatment used to alleviate pain, improve mobility, and promote overall physical well-being. In nearly all cases, this allows for rapid recovery, complete injury resolution, and lasting results. In-clinic patients should expect to see dramatic improvement after the first visit, and most patients experience complete injury resolution in as few as three visits (based on in-clinic and Remote Recovery patientreported outcomes).
Dr. Creel has been serving the McKinney/Prosper area for 10 years and provides patients with an individualized treatment plan, and uses a variety of techniques, including joint mobilization, soft tissue manipulation, and muscle energy techniques to address specific musculoskeletal issues and promote recovery.
Dr. Creel graduated with honors from Mississippi State University. Soon after, he received his Doctor of Chiropractic degree from Parker University in Dallas, Texas. In Dr. Creel’s free time, he enjoys all types of fitness activities and spending time with his wife and three children. Dr. Creel is an active member of Lighthouse Church in Prosper, TX.


OLIVIA ROGERS , RN, BSN, CHPN, CHPO, MBA,
Dear Olivia,
I’ve been caring for my mother since her health started declining, and I’m feeling completely overwhelmed. At her last doctor’s appointment, they mentioned palliative care, home health services, private duty nursing, and hospice as options, and now I’m confused about what would actually help Mom the most. I don’t understand the differences between these services or when each one would be appropriate for her situation. Can you please help me make sense of all these care options so I can make the best decision for my mother? I’m exhausted and feeling lost about what to do next.
~Care Option Overload
Dear Care Option Overload,
Care options have indeed become very complicated! The Visiting Nurse Association is here to help. Here is a brief summary of each one. Home health is appropriate for rehabilitative services when someone is too ill, has just had surgery or a procedure, or has another disability that does not allow them to leave home for therapy. The goal here is to improve their







health and function. Private duty services, delivered through a nurse or home health aide, are appropriate when a person needs help with activities of daily living such as bathing, dressing, medication management, housekeeping, or other personal care services. Palliative care, or what VNA calls Supportive Palliative Care, is needed when a person has a serious or complex illness that requires symptom management. The person may or may not be at the end of life, but they need help to alleviate suffering. This care is delivered by a comprehensive team; VNA’s Supportive Palliative Program is called Care Choices. Likewise, hospice services are delivered by a comprehensive team to alleviate suffering. Hospice Care is specifically for those nearing the end of life. Hospice provides support to not only the patient but the entire family. The goal of hospice is symptom management and holistic, patient-centered care that meets the needs of the whole person at the end of life. I hope this very brief summary helps!
~Olivia



Diane S. Litke, MD Diplomate American Board of Orthopaedic Surgery
Dr. Litke is a passionate artist, both in her spare time and as an orthopaedic surgeon. At L&W Orthopaedics, she approaches every orthopaedic problem with an eye toward restoration of function and mobility. With a deep knowledge of the inner workings of the body’s most active and important joints, Dr. Litke is able to repair most hip, knee, and shoulder problems, giving her patients the freedom to move again. Assisting her skilled hands, she uses the latest state-of-the-art robotic equipment for accuracy and precision, delivering a powerful combination of experience and technology to all of her patients.
Dr. Litke earned her medical degree at the University of North Carolina Chapel Hill. She went on to complete her orthopaedic residency at the University of South Carolina in Columbia South Carolina. She is certi ed by the American Board of Orthopaedic Surgery, and is a Fellow of American Academy of Orthopaedic Surgery and a Fellow of the American Associaion of Hip and Knee Surgeons. Dr. Litke is the medical director of the Orthopedic Department for Methodist Health System and is a liated with the Methodist Richardson Medical Center, where she is the director of the joint program. When she’s not working, Dr. Litke enjoys photography and cycling.
Please call 972.498.4791 to schedule an appointment.

Orthopaedic Surgeons located in Richardson, TX

www.LWOrthopaedics.com


By CARRIE UMSTEAD
Colon cancer, or colorectal cancer, is a type of cancer that starts in the colon or rectum. It is one of the most common types of cancer, but when detected early, it can be treated effectively. The disease often begins as non-cancerous growths known as polyps, which can develop into cancer over time if left untreated. Understanding the signs and symptoms play a crucial role in early detection and prevention.

tional modifiable risk factors that can elevate the likelihood of developing colorectal cancer.
In its early stages, colon cancer may not cause noticeable symptoms, which is why regular screening is essential, especially for those over the age of 50 or with risk factors. However, as the cancer progresses, it can produce a range of symptoms that affect digestion and bowel habits.
One of the most common signs is a change in bowel habits that lasts for several weeks. This could include persistent diarrhea or constipation, or a noticeable difference in the consistency of stools. These changes often occur without any apparent cause and may be accompanied by a feeling that the bowel does not completely empty.
Another potential sign is the presence of blood in the stool, which may appear bright red or dark, making the stool look almost black. Blood in the stool may be accompanied by rectal bleeding. While not always indicative of colon cancer—conditions such as hemorrhoids or anal fissures can also cause bleeding—persistent or unexplained bleeding should always be checked by a healthcare professional.
Unexplained weight loss and fatigue can also be early signs of colon cancer. Weight loss occurs as the body uses more energy to fight the cancer, and fatigue may develop due to anemia from blood loss in the digestive tract. This can leave individuals feeling unusually tired even after adequate rest.
Abdominal discomfort, such as cramping, bloating, or pain, may develop as the tumor grows, obstructing the passage of stool. This can lead to a feeling of fullness, even after a small meal. In some cases, advanced colon cancer can cause nausea or vomiting if a bowel obstruction occurs.
While the exact cause of colon cancer is not fully understood, several risk factors can increase the likelihood of developing the disease. Age is a significant factor, with most cases occurring in people over 50. A family history of colon cancer or certain genetic conditions, such as Lynch syndrome or familial adenomatous polyposis, further elevates the risk.
Lifestyle choices also play a role. A diet high in red or processed meats has been linked to an increased risk of colon cancer, as has a sedentary lifestyle. Obesity, smoking, and heavy alcohol use are addi-
Preventing colon cancer involves a combination of regular screening, healthy lifestyle choices, and sometimes medical interventions for those at high risk. Screening is the most effective way to detect colon cancer early or even prevent it by identifying and removing precancerous polyps. The American Cancer Society recommends that individuals at average risk start screening at age 45, while those with a family history or other risk factors may need to begin earlier.
Colonoscopy is the most commonly recommended screening test because it allows for the direct visualization and removal of polyps during the procedure. Other screening options include stool-based tests, which check for hidden blood or abnormal DNA in the stool, and flexible sigmoidoscopy, which examines the lower part of the colon.
Diet plays an essential role in reducing the risk of colon cancer. A diet rich in fruits, vegetables, and whole grains provides fiber, vitamins, and antioxidants, which help protect against cancer. Fiber, in particular, promotes healthy digestion and helps reduce the time that waste spends in the digestive tract, potentially limiting exposure to harmful substances. Consuming less red and processed meat, along with avoiding excessive alcohol, further contributes to a lower risk. Incorporating fish, lean poultry, and plant-based protein sources can be beneficial.
Regular physical activity has been shown to decrease the risk of cancer as exercise helps maintain a healthy weight and regulate hormone levels that may contribute to cancer growth. Even moderate activities such as walking can make a significant difference in overall health.
Smoking cessation is another crucial preventive measure. Tobacco use is not only linked to lung cancer but also increases the risk of many other cancers, including colon cancer.
For individuals with a high genetic risk of colon cancer, medical interventions may be necessary. Preventive surgeries may be considered in those with inherited conditions like Lynch syndrome. Genetic counseling can help assess risk and guide these decisions.
Colon cancer is highly treatable when detected early, with survival rates significantly higher for cancers caught before they spread. That’s why it’s important to not ignore symptoms or delay routine screenings. Seeking medical advice without hesitation can be life-saving.

Brian Nwannunu, MD, MS, is an orthopedic surgeon specializing in hip and knee replacement. He care for patients at Texas Joint Institute in Allen and in McKinney, Texas.
Dr. Nwannunu, a native of Dallas, graduated Valedictorian from the High School for Health Professions at Townview Magnet Center in DISD. He then earned his bachelor’s degree in Biology at Morehouse College in Atlanta, Georgia, where he was part of the Morehouse College Honors Program. Upon graduation, he completed his master’s degree in Physiology at Georgetown University in Washington, D.C., with a concentration on complementary and alternative medicine. Dr. Nwannunu then graduated with his medical degree from Howard University College of Medicine in Washington, D.C., where he was inducted into the Alpha Omega Alpha Honor Medical Society.
Dr. Nwannunu completed his residency in orthopedic surgery at the John Peter Smith Health Network in Fort Worth, Texas, before pursuing additional training with a fellowship in adult reconstruction at Baylor College of Medicine in Houston, Texas. In addition to his clinical training, Dr. Nwannunu enjoys mission work abroad, providing medical care and health education to populations in need. He is also one of the few official Jiffy Knee™ surgeons in the North Texas area.
He is a member of the American Medical Association, National Medical Association, American Academy of Orthopaedic Surgeons and the American Association of Hip and Knee Surgeons.
When not working, Dr. Nwannunu enjoys basketball, weight training, outdoor activities, attending art and music festivals, traveling, world news, and reading.


At KoonsFuller, we only practice family law. Which means we’re fully dedicated to serving Dallas area families and their unique legal needs. From informal negotiations to mediations, collaborative law to court proceedings, our thirty plus attorneys across four offices provide an unmatched network of expertise. Working together as a fully integrated team, KoonsFuller’s attorneys are equipped to handle estates of all sizes, cases of all complexities, and custody issues of any kind.
See what KoonsFuller can do for your family.Working together, as a fully integrated team, there is no case too large or complex for us to manage. To learn more about KoonsFuller, visit koonsfuller.com.
TX 75202 (214) 871-2727 (Principal Office)

» Staffed by 2 Licensed, Doctors of Audiology
» Hearing Aid Fittings, Maintenance and Repairs
» Invisible Fittings/Open Fittings
» Evaluation Period On All Hearing Aids
» Hearing Evaluations For All Ages
» Wireless/Connectivity Hearing Solutions
» Battery Purchase Programs
» Custom Ear Protection
» Assistive Devices


Courtesy HEARING SERVICES OF McKINNEY

Summer is a time for new sights, new experiences, and wellearned vacations. But for those who live with tinnitus—a condition marked by ringing, buzzing, or humming in the ears— air travel can introduce more than excitement. The stress of flying, coupled with noise and pressure changes in the cabin, can make tinnitus symptoms feel louder or more intrusive. The good news is that with a little preparation, you can manage these challenges and enjoy your journey with greater comfort.
Tinnitus is the internal perception of sound when no external noise is present. It might sound like a whistle, static, rushing air, or even a faint tone. Often, it’s linked to inner ear damage, chronic exposure to loud noise, infections, or side effects from certain medications. Though not a disease in itself, it is frequently a sign of an underlying issue. The American Tinnitus Association reports that nearly 25 million people in the U.S. experience tinnitus to some degree— making it a common, yet uniquely frustrating, condition.
While tinnitus can persist on a daily basis for some, air travel has a way of making it worse. This often happens due to changes in air pressure as the plane ascends and descends. Normally, small passageways called eustachian tubes help equalize pressure between the inner ear and the environment. But if these tubes struggle to adjust during flight, it can cause pressure imbalances that affect hearing— and in turn, make tinnitus seem louder or more bothersome.
Another factor is noise exposure inside the plane itself. Aircraft engines generate high levels of continuous noise, which can reach up to 100 decibels depending on your seat location. That kind of sound environment can fatigue the auditory system, especially for someone already dealing with sensitive ears. Add in the stress of travel, disrupted sleep, or dehydration, and it’s easy to see why tinnitus symptoms may spike midair.
The first and best defense against in-flight discomfort is a solid strategy. One smart investment is a pair of noise-canceling headphones. These reduce the hum of the plane and let you play soft background sounds or music, which can help mask your tinnitus and make the flight more pleasant. Calming playlists, ambient sounds, or even white noise apps can shift your focus away from the internal ringing.
Seat selection may also play a role. If you can, choose a spot toward the front of the plane—areas farther from the engines tend to be quieter. It’s also a good idea to skip standard foam earplugs, which may worsen pressure issues. Instead, look for pressure-regulating earplugs that are designed specifically for air travel. These help your ears adjust to altitude changes more gradually and reduce strain on the eustachian tubes.
During takeoff and landing—when the most pressure changes occur—it helps to stay awake and engaged. Actions like chewing gum, yawning, swallowing, or sipping water encourage the eustachian tubes to open, allowing pressure to equalize more effectively. If you’re prone to nasal congestion or seasonal allergies, consider asking your doctor if a decongestant is appropriate to use before your flight.
Keeping your brain occupied is another helpful tool. Distraction can lower the intensity of tinnitus simply by redirecting your focus. Bring along a few favorite audiobooks, light movies, puzzles, or games. You might also try breathing exercises or guided meditation through an app to keep your mind calm and grounded. Anxiety tends to make tinnitus worse, so anything that helps you stay relaxed will pay off in the air.
It’s also important to prepare your body for the trip. Get a good night’s rest before travel, stay hydrated, and skip caffeine and alcohol on flight day. These small habits can reduce the chances of a flare-up. And if you use hearing aids, don’t hesitate to wear them on the plane. Some models offer features that help reduce internal noise perception and support more natural hearing in loud environments.
If flying consistently brings on tinnitus flare-ups or makes travel stressful, it may be time to talk with a hearing care professional. A full hearing evaluation can help identify contributing factors and provide tailored recommendations—from sound therapy tools to pressure management techniques—that make flying more comfortable.
If your travel plans are being overshadowed by ear discomfort, the team at Hearing Services of McKinney is ready to help. From personalized evaluations to travel-friendly hearing solutions, their experienced professionals can guide you toward relief. Call today to schedule a consultation and take the first step toward quieter skies.


By RICK ALLEN
It’s something most of us don’t like to think about, much less talk about. Death, and everything that comes after, tends to linger in the background of life—uncomfortable, unknown, and easily pushed aside for another day. But there’s a quiet kind of grace in facing it head-on, especially when it comes to planning your own farewell.
Funeral pre-planning may not be a topic that comes up over coffee with friends, but for many, it becomes one of the most meaningful gestures they leave behind. Not because it’s about choosing caskets or selecting hymns, but because it’s an act of love, of intentionality, and of easing the emotional and logistical weight from those we leave behind.
When a death occurs, especially if it’s unexpected, families are often thrust into a whirlwind of decisions at a time when clarity is in short supply. Grief has a way of distorting time, scrambling priorities, and making even the simplest tasks feel monumental. In the midst of mourning, loved ones are asked to make dozens of decisions quickly: burial or cremation, type of service, location, music, readings, obituary details, and more. Each choice can carry emotional weight, and without guidance, families may struggle with second-guessing what their loved one would have wanted.
That’s where pre-planning becomes a deeply human act and a thoughtful gift to your loved ones. It’s not about morbid obsession or controlling details from beyond the grave—it’s about clarity. It’s about answering questions in advance so that those left grieving can focus on remembering and healing, rather than coordinating logistics.
Pre-planning can be as simple or detailed as you choose. Some of the people I’ve worked with outlined not just what kind of service they’d like, but included the stories or memories they hope will be shared. These gestures can feel like a roadmap, or even a final conversation—a way of saying, “I thought about you.”
One of the most overlooked parts of funeral pre-planning is the emotional relief it offers. It transforms an experience that can feel overwhelming into one rooted in intention. Families who have a clear plan to follow often speak of the peace it brings. They’re not left debating what to do; they’re carrying out a final act of care that was already put into motion.
There are also financial considerations. Funerals can be costly, and making decisions in the fog of grief often leads to overspending out of guilt or urgency. When a plan is in place—especially one that includes prepaid arrangements—it removes the pressure to make fast financial choices. It also minimizes the chance of family disagreements, which can surface when siblings or spouses have different ideas of what a loved one would have wanted.
Some may worry that making plans now feels premature or unnecessary, especially when in good health. But planning a funeral isn’t about predicting when the end will come. It’s about recognizing that, whenever it does, the people we love will be the ones left to navigate the moment. Leaving them with direction is one final way of showing we care.
What surprises many people as they go through this process is how comforting it becomes. Thinking about death often invites reflection on life—on what’s mattered, what kind of legacy one wants to leave, and how they hope to be remembered. Choosing a reading, a song, or even a poem for a future service can become a personal meditation on meaning. In that way, pre-planning is as much for the living as it is for the departed.
In the end, pre-planning a funeral isn’t about death. It’s about easing the path for those who will one day say goodbye. It’s about transforming one of life’s hardest moments into one marked by clarity, calm, and love.
There’s no perfect time to start thinking about these things, but there is always value in beginning. You don’t need all the answers. If you’re ready to take the first step or simply want to explore your options, Allen Family Funeral is here to help with care, clarity, and compassion. Our experienced team can guide you through every aspect of pre-planning—at your pace and on your terms—so you can create a service that truly reflects your life and values. Reach out today to begin a conversation that offers peace of mind for tomorrow.
If we can leave behind a map, even a simple one, it becomes easier for those we love to find their way through the fog. And that may be one of the most generous things we ever do.




VUDHI SLABISAK, MD OrthopaedicSpineSurgeon





BRUCE MARKMAN, MD OrthopaedicSurgeon&Sports MedicineSpecialist


JAMES STANLEY, MD OrthopaedicSpineSurgeon







STEVE HONG, MD Interventional Pain ManagementSpecialist








RAHUL BANERJEE, MD OrthopaedicSurgeon

GEOFFREY G. GLIDDEN, MD OrthopaedicSurgeon










AMIR MALIK, MD Neurosurgeon





KHAWAJA IKRAM, DO OrthopaedicSurgeon


BRIANA HODGSON, PA-C OrthopaedicSurgery PhysicianAssistant

CHARLES MARDER, DPM Podiatrist,Foot&AnkleSurgeon
If you’re suffering from pain or an athletic injury, schedule an appointment with your preferred NTOS location for effective, compassionate treatment.


By MICHAEL TURNER
At some point in midlife, it hits you. Maybe it’s the fourth set of wine glasses that doesn’t fit in the cabinet, or the box of gadgets in the garage labeled “Just in Case.” Maybe it’s the antique bread machine you never used but moved three times. Whatever the trigger, the realization is universal: we’re full. Full of stuff, full of storage bins, full of “what was I thinking?” purchases.
And yet, what do most of us never regret? That impromptu weekend road trip to the coast. The concert under the stars. The cooking class where you and your partner discovered both a new pasta recipe and the joy of laughing at each other in aprons. These moments don’t collect dust—they collect value.
The idea of investing in experiences over things isn’t just a whimsical Pinterest quote or a minimalist’s manifesto. It’s backed by research. A 2014 study published in the Journal of Positive Psychology found that people reported greater happiness from experiential purchases—such as vacations, concerts, or special meals—than from material ones. In fact, the anticipation of an experience alone can produce more happiness than the actual purchase of an item.
It makes sense when you think about it. Stuff depreciates. That designer handbag? Out of fashion next season. The latest tech gadget? Replaced by something shinier before you’ve even memorized your password. But memories have a sneaky way of gaining value over


time. That sunset you watched on a mountainside, breathless and content? It doesn’t go obsolete. If anything, it becomes richer, funnier, more meaningful in the retelling.
Of course, this isn’t to say there’s anything wrong with loving beautiful things. A cozy reading chair or a treasured family heirloom absolutely has its place. But many of us are drowning in more than our fair share of “might-need-this” clutter. And midlife offers a unique opportunity—a kind of emotional inventory—to reassess what we really need.
If you’re ready to shift from collecting things to collecting memories, you don’t have to travel far. Denton County is filled with opportunities to enjoy meaningful experiences—many of them right in your own neighborhood.
Start with local event calendars like DiscoverDenton.com, DentonMainStreet.org, and city websites for Lewisville, Highland Village, and Flower Mound. From music festivals and art walks to food truck nights and downtown movie screenings, there’s always something to do just around the corner.
Want something more hands-on? Take a pottery class at the Visual Arts Society of Texas in Denton, explore your creative side at Painting with a Twist in Flower Mound, or sharpen your culinary chops with a cooking class at Market Street. These experiences go beyond a finished product—they offer laughter,
learning, and maybe even a new favorite hobby.
Don’t underestimate the simple joy of the great outdoors. Spend a sunny afternoon walking the trails at Lewisville Lake Environmental Learning Area, enjoy a picnic at North Lakes Park, or explore the unique blend of art and nature along the murals and public sculptures scattered across downtown Denton.
Need inspiration at your fingertips? Download apps like Eventbrite, Meetup, or Airbnb Experiences. They’re full of local outings, group activities, and creative events hosted by passionate community members eager to share what they love.
And for those looking to build community, there are plenty of local clubs and social groups to join. Whether it’s a running group in Corinth, a book club in Denton, or a wine tasting event in Argyle, meaningful experiences often begin with simply showing up.
Investing in experiences doesn’t have to mean jet-setting around the globe. Local concerts, weekend getaways, a class at the community center, or even planning a family “staycation” with themed dinners and board games can all offer meaningful returns on your investment. What matters is the intention behind it: the choice to be present, engaged, and curious.
And if you need one more nudge: experiences are notoriously hard to re-gift.

Florian F. Dibra, MD is a board-certified, orthopedic surgeon located in Frisco, Texas who has extensive knowledge in hip and knee orthopedics and treats operative and non-operative hip and knee arthritis. He focuses on minimally invasive muscle-sparing total hip and knee replacement, anterior hip replacement, partial knee replacement, robotic joint replacement and complex hip and knee replacement revisions. Dr. Dibra is specialized in MagicKnee and MagicHip, muscle-sparing techniques with robotic technology.
Dr. Dibra graduated with honors from Villanova University in Pennsylvania. Soon after, he received his medical degree, with cum laude honors from the esteemed Jefferson Medical College in Philadelphia, Pennsylvania. He completed his orthopedic surgery training at the University of Florida. He continued at the University of Florida Health Hospital to complete his fellowship in Adult Arthroplasty with an emphasis in hip and knee reconstruction. During Dr. Dibra’s surgical training, he accomplished several publications, book chapters, and poster presentations.
Dr. Dibra’s family consists of his wife and two children. In addition to English, he is fluent in Albanian, Italian, and proficient in Spanish.












