9 minute read
Ask A Health Care Prefessional
Wei-Ann Bay, M.D., Chief Medical Officer, Blue Cross and Blue Shield of New Mexico
No matter how old we are, we are always adapting to change. Older adults face lots of changes — medical problems, retirement, death of loved ones, stressful life events, and now the COVID-19 pandemic. It is normal to have feelings of stress, anxiety and sadness about changes, but after a bit of time and adjusting, most can move on and feel well again. However, if the negative feelings persist and interfere with activities of daily living and normal functioning, it may mean depression.
Advertisement
What is the difference between grief and depression?
Grief after loss of a loved one is a normal reaction to loss and generally does not require mental health treatment. However, grief that lasts a very long time or is unusually severe following a loss may result in depression and require treatment.
Depression is not a normal part of aging. It is not a weakness nor a personal flaw. It is an actual medical condition — just like diabetes, hypertension and heart disease are medical conditions.
What are the risk factors and signs of depression?
Depression is often underdiagnosed. Underdiagnosis can result in an unnecessary move to a nursing home, an uncontrolled chronic medical condition resulting in a hospitalization, or loss of independence.
Those who experience their first episode of depression later in life are less likely to have a family history of depression or other mental disorders than those whose first episode occurred earlier in life. Risk factors include social isolation, lower socioeconomic status, comorbid medical conditions, uncontrolled pain, insomnia, and functional or cognitive impairment. Females and people who are widowed, divorced or separated are also at higher risk for depression.
Common signs and symptoms of depression for all ages include persistent sadness, feelings of hopelessness or helplessness, loss of interest in activities that used to be pleasurable, decreased energy, difficulty concentrating and making decisions, difficulty with sleep, eating more or less than usual, thoughts of suicide, and frequent crying. Older adults may not have the more obvious signs, such as sadness or crying. Instead they may be less likely to talk about it and more likely to present with somatic complaints (e.g., tiredness, heart palpitations, shortness of breath, body aches, restlessness, nausea or vomiting), irritability, confusion, or attention or memory problems, which can look like dementia.
Finally, it is important to consider medication side effects, which can sometimes contribute to depressive symptoms.
What are the types of depression that can occur late in life?
Major depression: severe symptoms that interfere with daily activities; a subtype of this can present with delusions or hallucinations.
Persistent depressive disorder (also known as dysthymia): depressive symptoms that are less severe than major depression but last a long time, at least two years.
Minor depression: depressive symptoms that are less severe than major depression or dysthymia and do not last long.
Depression related to stroke and vascular changes in the brain is becoming more recognized. This is called “vascular depression.” Depression can also be a complication of Alzheimer’s disease and other dementias. Presentation and treatment differ from the more common types of depression.
How do I get help?
If you think that you have depression, or if you think your loved one has depression, it is important to seek help immediately. Don’t wait it out or deal with it on your own. Untreated depression can lead to serious outcomes, such as other serious physical illnesses or suicide. A health care provider will review your medical history, medications and do testing to rule out other conditions that may be contributing to the depressive symptoms. Remember to be open and honest because this will help the health care provider find the right path forward. There are many effective treatments, such as medications and behavior therapy; and sometimes just talking with a counselor can be a huge benefit. If you or your loved is in a crisis, please immediately call 911 or visit the emergency room. The National Suicide Prevention Lifeline is 1-800-273-TALK (1-800-273- 8255). The New Mexico Crisis Line is 1-855-NMCRISIS (1-855-662-7474).
If you have a health question that you would like to be considered in Ask a Health Care Professional, please email AskHealthcareProfessional@ bcsbsnm.com. BCBSNM will select questions that may appear. Questions will not be personally answered. The opinions expressed in this column are solely those of the author and not necessarily those of BCBSNM. This column is not intended to be a substitute for professional medical care.
• SAFE • RELIABLE • AFFORDABLE
Professional Non-Emergency Medical transportation We travel throughout the state and treat you and your
loved ones with the same care we give our families.
Call 505 681-2128 Accepts Medicaid, Private Pay
Peace of mind for you, a future filled with love for them.

This is what Animal Humane New Mexico can ensure when you plan now for your pets.
Prime Time Publishing, LLC
Home of Prime Time Monthly News Family Caregivers Resource Guide 50+ EXPO
Publisher/Editor David C. Rivord primetime@swcp.com Sr. Advertising Executive Joe A. Herrera primesales@swcp.com Art Director Ashley Conner primeart@swcp.com Graphic Designer/ House Photographer Dana Benjamin Webmaster Gary Rivord webmaster@primetimenm.com Copy Editor Autumn Gray Calendar Editor Liz Otero Contributing Writers Dr. Wei-Ann Bay Richard Fagerlund Autumn Gray Jim Miller Dr. Gerard Muraida Dr. Barry Ramo Dr. Shellie Rosen, D.O.M. Charles Schlesinger DDS, FICOI Shannon Wagers
Get news and see event pictures on our new Facebook page at facebook.com/primetimepublishing!
Visit us at ptpubco.com
P.O. Box 67560 Albuquerque, NM 87193 505.880.0470
The Publisher does not take responsibility for the accuracy or legitimacy of the advertiser’s message or that of the guest writer/columnists or any aspect of the business operation or conduct of the advertisers in the paper.
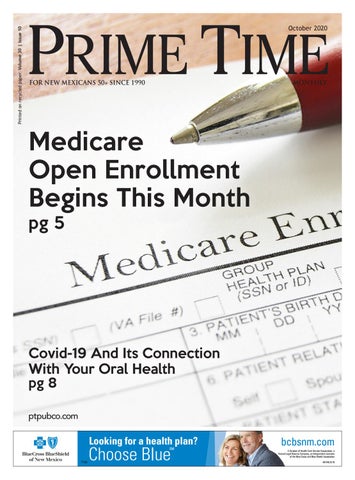
By Autumn Gray
Times may never have been more challenging than they are now for seniors needing access to health care and trying to navigate their options for how to receive it. As the open enrollment period for Medicare recipients approaches this month, so does the onset of flu season, coupled with the continued threat of the novel coronavirus. Typically, local health care providers would be ramping up for a flurry of in-person educational seminars to help beneficiaries make informed choices about their medical insurance plans for the coming year. Not so this fall.
About the only thing that’s business as usual is the enrollment period itself: Oct. 15-Dec. 7. During that time, anyone who is Medicare eligible (generally age 65, or any age and with some level of disability) may join, drop or switch plans, with coverage taking effect Jan. 1. Except for this constant, providers have made changes to their enrollment processes, plan pricing and benefits, and even to physician appointment options to ensure all are safe, accessible, and responsive to what their members have been requesting.
Blue Cross and Blue Shield of New Mexico (BCBSNM), Presbyterian Healthcare Services and Humana, for example, are all offering enrollment, workshops, and/or general open enrollment information virtually or over the phone.
“We’re doing everything we can to meet seniors in a space that they’re comfortable with because this is such an important decision,” said Janice Torrez, BCBSNM’s incoming president. “Even if they’re not shopping (for a Medicare health or prescription drug plan), it’s important to make sure to understand changes to their existing plan because they don’t want to be surprised later when it’s time to receive services.”
It’s advisable for newly eligible or current Medicare recipients to compare Medicare basic plans with Medicare Advantage, for example. Medicare Advantage provides everything that basic Medicare does but may also provide prescription drug coverage and a number of additional providerdependent perks. Extra benefits may include gym memberships, transportation assistance to doctor appointments, vision and dental care, and even chiropractic and acupuncture visits in some cases.
For example, BCBSNM Medicare Advantage members have access to its popular SilverSneakers wellbeing program that provides avenues for physical activity, education, social interaction and a fitness center membership at no extra cost. BCBSNM’s Advantage plan also provides a quarterly over-the-counter stipend and various rewards for taking preventive health care measures such as getting a flu shot, having an annua physical exam, or getting a mammogram or colonoscopy.
Mark Iorio, regional president of senior products for Humana’s Central West Region, emphasized Humana’s benefits around Covid-19: “Humana is continuing to waive all member costs related to COVID-19 testing and treatment, and you’ll also get 14 days of home-delivered meals if you’re diagnosed with Covid.” In addition to expanded telehealth services for members, Humana is making novel coronavirus testing easier with inhome Covid-19 testing, he said.
Iorio also praised Humana’s “award


winning mail order pharmacy,” transportation benefits, plans for veterans and over-the-counter health essentials kit.
Many Advantage plans also have some dental, hearing and vision coverage, but costs and extent of coverage vary by provider. Fewer offer broad alternative medicine coverage such as acupuncture and chiropractic services.
Jim Decker, director of sales for Presbyterian’s Medicare Advantage plans, said the network’s physicians and patients have requested a high degree of alternative therapy benefits, especially to help patients avoid pain medications like opioids.
“Our very own Presbyterian Medical Group doctors are saying we want that covered,” Decker said.
In addition, he said, “We learned that a prescription drug deductible is a hindrance to patients getting prescription drugs filled, so we lowered the cost to zero. … There’s no deductible for generic or brand name drugs.”
The most significant nationwide Medicare coverage change impacts renal patients. Before 2021, patients with end-stage renal disease were unable to enroll in Medicare Advantage plans unless there was a Medicare Special Needs plan available in their area for ESRD patients. But that is changing for 2021, under the terms of the 21st Century Cures Act.
Not everyone will want or need to make adjustments to their plans, but people in a Medicare health or prescription drug plan should nevertheless review them to ensure their plans will continue to meet their needs in the next year. Providers say that when shopping for coverage or conducting research to ensure the plan you have remains the best for you, there are some fundamental questions to consider: • Look for a plan that includes your preferred physicians and hospitals • Compare out-of-pocket maximums • Ensure a plan covers your prescriptions, and look for one that has low or zero deductibles for prescriptions, both generic and brand name (The simplest way to check formularies is by visiting medicare.gov and filling out an online form.) • Confirm that the pharmacies you are accustomed to working with are available • Check dental, vision, hearing, and/or mental health benefits • Find out if telehealth is covered and to what degree
For more information about any of the insurers mentioned in this article and for general information, visit Presbyterian at Phs.org/medicare or 923.8458; Blue Cross and Blue Shield at Bcbsnm.com/medicare or 866- 286-6159, Humana at Humana.com/ medicare or 800.213.5286, and for the official U.S. government website for Medicare, visit medicare.gov.