49 minute read
FAKING IT ‘TILL YOU MAKE IT: WHY WE
FAKING IT ‘TILL YOU MAKE IT: WHY WE SHOULD ALL SMILE MORE
by Natalie Pettirossi / art by Allie Verdesca and Mara Russell
Advertisement
We’ve all heard the expression “fake it till you make it.” Whether it’s a friend telling you to be nice to someone who drives you crazy, a teammate encouraging you to play through the pain of an injury, or a parent reminding you to act more confident at school, this phrase might make you roll your eyes. But for all the eye-rolling and annoyance this phrase can bring, there’s actually some truth behind it.
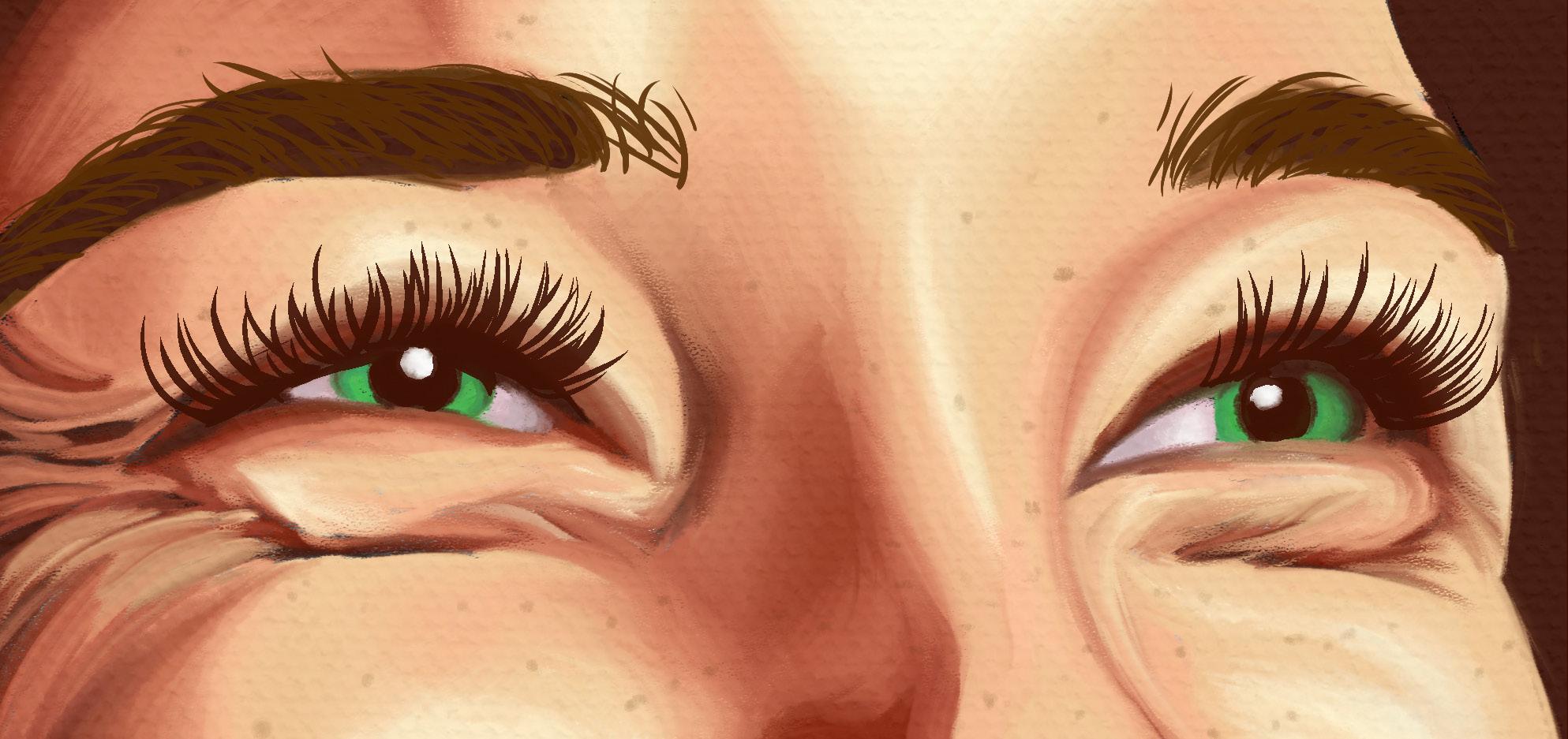
“Fake it till you make it” holds notable merit in the case of faking a smile. Smiles are officially classified into two main categories: the standard smile and the Duchenne, or genuine smile. The standard smile is that small, usually forced expression we offer to someone to be polite or to show that we are paying attention. This smile is representative of the common phrase, “the smile did not reach their eyes,” which is often used to critique ingenuine reactions. While standard smiles merely activate the muscle surrounding the mouth (the zygomaticus muscle), Duchenne smiles activate both the zygomaticus muscle and the muscles surrounding the eyes (orbicularis oculi muscles) [1]. Thus, when you are “smiling with your eyes,” you are actually performing the Duchenne smile. Unlike the standard smile, a Duchenne smile is an unbridled form
of expression that transforms the entire face as both the mouth and the eyes react and change position [2]. Even though both smiles are different, they each trigger the release of beneficial chemicals, improving psychological and physiological body responses.
SMILING ACTIVATES IMPORTANT SUBCORTICAL STRUCTURES
The changing position of facial muscles in both the standard and the Duchenne smile activates the amygdala -- a structure found in the temporal lobes of the brain. The amygdala is responsible for decisionmaking and emotional responses [3]. For example, if you were in the middle of a forest and encountered a bear, your amygdala would trigger the fight or flight response, preparing you to either run away in the opposite direction or stand up to the bear and scream. Your amygdala regulates emotions and behaviors, serving as an alarm to the hypothalamus, another structure in the brain that regulates the release of a variety of chemicals such as neurotransmitters and endorphins [4].
When you smile and your zygomaticus muscle changes position, your amygdala is activated, alerting the hypothalamus to secrete four important moodboosting chemicals: neuropeptides, proteins that combat body stress responses; dopamine, a hormone involved in motivation pathways; endorphins, the body’s natural pain killer; and serotonin, a hormone connected to happiness and mood regulation[5]. These chemicals have many functions in the body, contributing to both physiological and psychological processes. Notably, the release of neuropeptides and endorphins improves the body’s physiological responses. Neuropeptides have a calming effect on the nervous system while endorphins function similarly to opioids, mitigating pain in the body. When neuropeptides and endorphins are released together, the body becomes more relaxed. The release of dopamine and serotonin, on the other hand, play an even larger role in improving the body’s psychological processes. Increasing dopamine levels in the body also increase motivation by heightening reward and pleasure pathways, and raised levels of serotonin increase overall feelings of happiness [5]. Therefore, these “Big Four” components are exactly why we should smile more; the more neuropeptides, dopamine, endorphins, and serotonin our body releases, the better we feel both physically and emotionally.
However, a smile does not need to be Duchenne to feel this pleasurable rush. Your amygdala cannot differentiate between a fake or a genuine smile and therefore triggers the same release of neurotransmitters and endorphins regardless if it is “real.” Even when you have to force a smile at someone’s cheesy joke, the zygomaticus muscle changes position, alerting the amygdala to activate the hypothalamus and release the same endorphins and neurotransmitters, regardless of the type of smile [1]. In other words, we no longer need to entertain ourselves with John Mulaney or Trevor Noah to find an excuse to smile; we really can “fake it till we make it,” reaping the same psychological and physiological benefits with an ingenuine smile.
SMILING CAN CHANGE YOUR MOOD
A recent study examined how changing participants’ facial expressions could impact their mood and interpretation of ambiguous stimuli, or stimuli that do not have an explicitly positive or negative connotation [6]. In this experiment, psychology students were shown a slideshow of images and asked to rank each slide as very negative, neutral (ambiguous), or very positive [6]. Electrodes attached to the subject’s facial muscles allowed researchers to control and manipulate these muscles into either a standard smile or a frown as the participants watched the slideshow [6]. The team found that significantly more positive ratings were given to ambiguous stimuli when participants were smiling compared to when they were frowning. This suggests that the activation of the zygomaticus muscle can positively influence how people perceive neutral stimuli [6]. All in all, this study corroborates the point that smiles, even forced ones, can improve your mood, allowing you to view your surroundings and environment in a more positive light [7].
On the other hand, additional studies have shown that the inhibition of facial expressions can actually weaken some emotional experiences [8]. This finding, as well as the one detailed above, prompted researchers to consider the negative consequences of facial muscle activation by looking at the effects of BOTOX injections on decreased amygdala activation and emotional capacity [9]. Botulinum toxin, commonly referred to as BOTOX, is a neurotoxin protein that is used for a variety of medical reasons, though, most notably, by dermatologists to treat wrinkles. BOTOX causes muscle paralysis by blocking the neurotransmitter acetylcholine, which is responsible for smooth muscle contraction [10]. With limited facial muscle movement, fine lines and wrinkles are smoothed out, along with
facial expressions and the corresponding visual cues of mood and emotion. In fact, a study conducted in 2020 found that BOTOX patients experienced a significant decrease in the strength of their emotional experiences, again suggesting that facial expressions may impact emotional experience [11]. Through the inhibition or exhibition of facial expressions, one is able to change one’s own mood.
SMILING MAY IMPROVE STRESS RESPONSES
Not only do facial expressions, such as smiling, make up an integral component of mood and emotional state, but they also impact our physiological health. For example, one of the most important jobs of the smile is to decrease our bodies’ stress response. Stress can be understood as a real or perceived threat to our wellbeing that disrupts homeostasis — our body’s ability to maintain internal stability—and causes our body to react [12]. The stress response is the fight or flight reaction mentioned earlier, like when you encounter a bear in the forest and your body is prompted to decide what to do next. This is an important survival mechanism as the response activates the necessary neuroendocrine systems for a suitable reaction to the threat.
However, the activation of our stress response is not always beneficial. While the acute stress response is evolutionarily necessary, chronic stress is a major physiological problem that affects more and more people at an increasing rate [13]. Chronic stress is characterized by a variety of symptoms, but notable characteristics include high blood pressure, obesity, and brain changes that can contribute to anxiety, depression, and addiction [13]. Some techniques used to counter these responses promote relaxation through visualization and mindfulness practices, deep breathing exercises, and physical activity such as yoga or tai chi [13]. Beyond these, newer research is starting to consider the effects of social support in alleviating bodily stress reactions. So, why not consider the potential benefits of smiling as well?
As such, a recent study looked at how manipulated smiles affected stress recovery and heart rate. Participants were divided into three groups and were trained to hold different facial expressions through the placement of chopsticks in their mouths. The chopstick placement replicated and activated facial muscles responsible for neutral expressions, standard smiles, or Duchenne smiles. After being put through a stressful activity, the participants in both the standard and the Duchenne smile group had lower heart rates than the neutral expression group. While the Duchenne smile group had a trend of lower heart rates than the standard smile group, the difference was not statistically significant, meaning that both types of smiles are considered effective [1]. This goes to show that, just as smiles can increase the secretion of mood-boosting chemicals in the brain and improve positive experiences, they can also alleviate stress responses, therefore improving physiological health.
COMPOUNDING EFFECTS: SMILES AND LAUGHTER
But it doesn’t just stop there: the findings that a smile can improve stress responses bring forth new questions. One research team decided to build off of previous studies of the smile’s impact on stress levels by investigating how both smiling and laughter may affect stress responses. This study was conducted to better understand positive affect, or the state of experiencing pleasure, which typically decreases mental and physiological stress responses [14]. To quantify positive affect, the researchers cited laughter as the highest level or display of pleasure, followed by a Duchenne smile and then no smile at all. The major goal of this study was to determine if laughter
has a stress-buffering effect on participants. Both the frequency and intensity of laughter were studied and it was found that higher frequencies of laughter reduced self-reported stress response symptoms [14]. Interestingly, this study was actually a test of the stress-buffering model of the positive affect hypothesis, which states that positive affect reduces the health-harming effects of physiological stress [15]. A previous study had determined that greater positive affect was found to be associated with lower mortality risk, inspiring the researchers who studied laughter’s effects to build off of this work and determine significant associations between greater positive affect and lower perceived stress. Stress contributes to mortality risk and therefore when positive affect mitigates stress responses, it also mitigates mortality risk too. These studies can be looked at together to understand how smiling and the release of moodboosting chemicals can play a crucial role in mitigating the stress responses that often take a toll on the body. THE POWER OF FAKING IT
In the age of COVID and the heightened stress, worry, and isolation that accompanies this pandemic, it often feels like there is a lot less to smile about. The loss of routine, education, jobs, time with loved ones, and opportunities can be an incredibly challenging weight to bear. However, it’s clear that, now more than ever, it is important to coax those facial muscles to turn on and smile. Doing so will help our brains and bodies stay healthy and prepared to face whatever challenge comes next. Moreover, smiling will set us up for success in other ways, improving our mood and our brain’s chemical balance, therefore decreasing our perception of stress. So now really is the time to fake it till you make it: keep smiling through these challenging times and know that doing so will benefit you both psychologically and physiologically.

ENCOUNTERS WITH THE THIRD KIND: THE MEMORY TWILIGHT ZONE

by Zoe Curran / art by Naomi Tomlin
SOMETHING IN THE SKY
Your car careens around sharp turns as you make your way home on a dark, forested highway. You drive through unfamiliar territory tonight, far from streetlights and neighbors. Even the trees look different out here. You’re passing a road sign when you first hear it: a high-pitched whine infiltrating the car through the cracked windows. The whine ascends to a scream. You notice a spotlight piercing through the darkness, cutting across the treetops, shining through your windshield. In a moment of panic, you crash into the highway barrier. Suddenly, the spotlight is on you. You finally see the source of the sound and light: a wide, chrome saucer hovering 50 feet above you, beaming you up! A door begins to open, tall grey figures illuminated within. You wake up the next morning in your own bed. Outside your window, your car is intact. And yet, your body is covered in scratches and you can’t shake the image of the saucer and the tall grey figures. Who took you that night, and where did you go? THE ORIGIN OF THE EXTRATERRESTRIAL
When reading the story above, could you see the bright saucer lights and hear the crunching car metal as you collided with the highway barrier? What features can render a false memory easy to believe? To begin untangling the neural complexity of false memory formation, we must first understand how memory salience can change how, and what, we remember. Salience is defined as being particularly noticeable or prominent; therefore, a salient memory is one that readily comes to mind out of a sea of surrounding memories.
Cultural relevance plays a key role in the salience of a memory. For example, iterations of the alien abduction narrative have invaded popular culture since the early 1960s. The true origin of this narrative actually belongs to the Puritan fisherman James Everell [1, 2]. As documented by John Winthrop, governor of the mid1600s Massachusetts Bay Colony, Everell claimed he saw a mysterious light that “ran as swift as an arrow” darting across the marshland of “Muddy River.” Future fishermen described seeing the same unexplained
light appearing on the marsh. Some heard voices or commands. Everell even claimed that the light had carried his boat a mile upstream [2]. Flashing lights, strange beings, and lost time – sound familiar? The details of the Puritans’ experiences echo elements of another Encounter with the Third kind: Betty and Barney Hill’s 1961 tale of an extraterrestrial encounter deep in New Hampshire’s White Mountains. Their story begins with Betty and Barney in the final stretch of their late- night drive home; a sleepy Barney was behind the wheel when he first saw the lights of a strange object flying overhead, following the movement of their car and growing brighter with each passing mile [1]. The extraterrestrial powers of their abductors rendered the couple paralyzed and unconscious. When they awoke two hours later, they realized that they had traveled 35 miles down the road.
Before the story’s publication, the Hills lived a quiet suburban life, untouched by extraterrestrials or media frenzy. However, their story forever changed how alien abduction accounts were both told and understood. In the years after their alleged encounter, the couple developed severe psychosomatic symptoms: crippling anxiety, disturbing dreams, and even stomach ulcers. Plagued by their physical and mental ailments, the couple sought out a hypnotherapist to determine if there was a relationship between that fateful encounter and the onset of their suffering. It took weeks of hypnosis for the ulcers to heal and the anxiety to diminish, and as their mental health began to recover, the Hills felt compelled to tell their curious tale [1].
Three key characteristics of this encounter are worth examining. First, prior to the Hills’ experience, extraterrestrial encounters were painted as friendly, albeit strange. The fact that the Hills were attacked challenged this notion, explaining why their narrative made for such great storytelling. Second, the Hills provided an incredible amount of detail when presenting their encounter. The couple could remember how many miles away from a rest stop they had traveled, the structure of the tailing UFO, and the color of the lights on the spacecraft. Lastly, the recollections only emerged after the couple had been placed in a hypnotic trance and asked a series of leading questions by their psychiatrist. In this hypnosis-induced state of heightened susceptibility,
the Hills could have been led to believe that anything had happened to them. In a sense, their own memories

were up for grabs, ripe for manipulation. In addition to sparking an American fascination with saucers in the night sky, Betty and Barney revealed a crucial paradox of memory: humans often believe irrational things for rational reasons. For example, encoding a salient memory after being attacked by a terrifying figure is rational, but improperly encoding the figure as an alien is irrational. Moreover, being “rational” does not exempt someone from forming false memories. False memory formation can occur in all of us.
HOW A FALSITY BECOMES A TRUTH: THE FORMATION OF FALSE MEMORIES
The human brain can form memories fairly easily, even ones involving aliens. But how, exactly, do these memories form? Think of an equation you are trying to memorize for a class. You begin by looking at your notes, taking in the details, the length, the meaning of each variable, and its application. Your notes and the elements of the equation serve as sensory input: the initial stage of memory formation. This information is then stored in a temporary memory bank. While the equation waits patiently in this bank, you repeat the information by rewriting the equation over and over. This process is called rehearsal. As you rehearse the equation, it leaves the sensory memory bank and travels to a new storage location: your short-term memory. From here, the information will be encoded and remembered for the long haul and is said to be a component of your long-term memory, divided into two subsets: explicit and implicit memory. Learning a math equation is a form of explicit memory, requiring conscious effort to recall. Remembering your mother’s name is an example of implicit memory, or something that is recalled effortlessly.
Many tend to incorrectly assume that these memory processes all occur in one location: the famed hippocampus. Although peripherally involved in a number of memory processes, the hippocampus is primarily involved in the storage of episodic memory, or autobiographical accounts of specific life events [3]. The formation of long-term memories, however, requires the simultaneous engagement of multiple neural pathways outside of the hippocampus [3]. Auditory sensory input undergoes initial processing in a different location of the brain than visual sensory input. To encode and store this sensory information, additional structures are needed. This neural process of memory formation seems nearly as intricate as Betty and Barney’s tale! However, it doesn’t just stop there; several other brain structures are also involved in memory formation, such as the neocortex and amygdala. The neocortex is the largest part of the cerebral cortex, characterized by the wrinkly layer of tissue that covers the surface of the brain. It is responsible for sensory perception, motor commands, spatial reasoning, and elements of language. Sensory perception is defined as the processing of an element in the environment, while spatial reasoning refers to an individual’s capacity to picture objects in 3-dimensional space and draw conclusions about them based on limited information. Interestingly, the neocortex also acts as a storage unit; memories that were temporarily stored in the hippocampus can also be stored in the neocortex as everyday knowledge. The amygdala, on the other hand, is responsible for attaching emotional significance to memories. Memories with strong emotional ties are the hardest to forget, regardless if the memory formation was accurate or falsely conceived. For example, because fear is a particularly powerful emotion, overpowering other strong emotions like joy or shame, memories associated with fear are more likely to be ingrained in our long-term memory. Thus, the stability, or propensity for the long-term duration, of a memory is largely determined by interactions between the hippocampus, neocortex, and amygdala.
However, while the brain has developed these complex processes for memory formation and storage, it still lacks a foolproof mechanism for differentiating between real and false encoded information. This means that false memories can be remembered as real ones, though these are typically only constructed in a susceptible state of mind when information is suggested as real, or when a prior experience is confused with a new one [4]. The incorporation of this information resembles the slow addition of small strokes to a painting of a village; a dash of green on a villager’s arm, a splotch of purple on a cloud, a tinge of red on a building. Each revisit to that same memory will lead to more and more strokes of paint added onto the original painting, until the villagers’ skin is green and the sky is purple: a completely changed scene.
Memories characterized by something fearful, such as being experimented on by unfamiliar beings, are particularly memorable. The sensory system, hit with flashy, fresh stimuli, desires to learn every detail it can about this incoming information. Simultaneously, parallel neurological processes work to determine the importance of retaining these details. While visual features of the stimuli are processed in the visual
brain region, the auditory and tactile features are synchronously processed elsewhere.
But how does the brain decide whether or not this potential memory should take precedence over other incoming stimuli? New stimuli, referred to as novel stimuli, have high salience (prominence of a stimuli and the likelihood it will be remembered) when compared to repeating stimuli [3]. Earlier, we also examined the importance of cultural relevance in salience. The UFO and the extraterrestrial figures offer a double punch of both cultural relevance and novelty, making them fantastic candidates for encoding. Further, emotion inhabits another key role in memory, with memories generated on the basis of the valence, or the attractiveness or aversiveness, of the emotion [4]. An attractive emotion, such as excitement, has “positive valence,” whereas an aversive emotion, such as fear, has “negative valence.” Emotions that lie on either end of this scale, such as highly positive or negative ones, are more likely to be remembered. In the Hills’ case, fear of the alien lifeforms provided negative valence, while the overall traumatic experience created high arousal, as the situation contained many novel stimuli. These, combined with the physical and psychosomatic trauma the Hills allegedly endured while aboard the saucer, created the perfect memoryencoding storm. So, their brains went to work on the long-term neocortex storage of their Encounter with the Third Kind.
It’s important to note, though, that many experiences may be encoded even without the salient features present in the Hills’ alleged abduction. The brain subconsciously notices countless stimuli in our environment, leading to some passive integration of stimuli into memory. Aside from this small bit of subconscious encoding, most of the information we recall best, or is stored in long-term memory the longest, is the result of conscious processing. Conscious processing occurs when an individual is aware and in control. In this way, we do have some autonomous control over what we remember vividly. Of course, there are exceptions to this, such as the impact of emotions and stimulus novelty on the stickiness of a memory. There are also many situations that can disrupt the typical memory processing chain, generating mild to severe encoding failures. One example is being in an altered state of consciousness, such as sleep or hallucination, both of which are capable of reducing one’s ability to consciously evaluate the accuracy of the “memory.” Thus, memory processing is highly dependent on the situation at hand and the state of the individual’s brain. SLEEP DEPRIVATION AND HYPNOSIS: WHEN ARE YOU SUSCEPTIBLE TO SUGGESTION?
The Hills’ journey home was fueled by black coffee purchased from a diner and chugged quickly before hitting the road around 10:30 pm. Given the long days of travel before and the hours of driving ahead, one can assume that Barney was partially sleep deprived at the wheel. Sleep is heavily involved in the process of translating memories from the short-term bank into a long-term savings facility [6]. In addition to memory translation, sleep is also responsible for replenishing your ability to encode details more accurately. Sleep deprivation, then, runs the risk of increasing inconsistencies when encoding memories and recalling personal events.
But can sleep deprivation also lead to false memory formation? In 2016, researchers investigated this proposed link using two memory tasks: learning a list of semantically related words, and “misleading” the subject before asking them to recall a memory. The tasks were both designed to determine if, and how much of, the false information was encoded while playing with the same key memory salience characteristics mentioned earlier: stimulus novelty and emotional valence. Researchers found that partial sleep deprivation significantly elevated faulty encoding while having a smaller impact memory recall [6]. The prevalence of memory encoding failures may help to provide a potential explanation for why the Hills encoded the wrong story but remembered it in fantastic detail. The ability to provide such detail is oddly striking; wouldn’t more details make the abduction harder to recall? Interestingly, perhaps not. Another study found that certain types of details can be stored in large amounts, actually enhancing these memories [7]. Any detail an individual sees as relevant to themselves is associated with stronger memories. Cultural context is critical, as you’re more likely to falsely remember an event that somehow makes sense; are there contextual details that would further suggest this particular detail is likely? Have you seen these details or images around you [7]? From the Hills onward, alien abductions were marked by the deeply personal trauma abductees endured. The attacks harmed the body, and were therefore inherently personal. And although most people would probably not jump to “alien abduction” to explain the development of their bumps and bruises, the prevalence of these narratives provides a tantalizing explanation for otherwise unexplained trauma. The
usage of an abduction narrative is typically presented under a semi-specific set of factors, but nonetheless, they remain omnipresent in the cultural fabric of American mythos.
When the Hills began attending hypnosis sessions with Simon, they were initially seen separately for confidentiality reasons. Simon claims that the abduction claims appeared fast and furious; Barney’s retelling was riddled with frequent emotional outbursts, and Betty had been dreaming of the events for months so her final account mimicked the dreams closely. According to Barney, Betty would often cry out in the night and experience periods of intense sleep paralysis and hallucinations. Despite being separated for the majority of sessions, Betty and Barney produced similar narratives while in hypnotic regression. Simon chose to dig deeper into these claims, interfering very little during the sessions and instead opting to listen and provide occasional guidance. Hypnosis is defined as a “waking state of consciousness,” in which an individual is detached from the outer world and fully absorbed in internal experiences. It is particularly useful for increasing susceptibility to suggestion and heightening the mind-body link [8]. In hypnosis, words are used to evoke specific imagery, calling events lodged deep in the subconscious mind to the forefront. For Barney and Betty, Simon may have asked them to return to the darkness of that New Hampshire night and tell him everything they knew. Being in a hypnotic state of detachment can allow an individual to perceive a memory using their right hemisphere of the brain more than their left hemisphere. The right hemisphere is involved in symbol and image production (among many, many other tasks – it is a whole hemisphere after all!) and shows an increase in activity when we are relaxed or deeply involved in an activity. Thus, when the right hemisphere is highly active in this detached state, images can be more easily accessed from the unconscious mind and brought into the conscious mind [8]. It’s impossible to know if Simon asked leading questions directly related to extraterrestrial encounters, or if the Hills truly produced those ideas entirely on their own. Still, knowing that the Hills were entering his office with severe trauma produced under strange circumstances would motivate anyone to uncover the root cause.
It’s particularly interesting to consider how Betty’s narrative developed, as well as how this may have significantly impacted Barney’s account. As mentioned earlier, Betty had experienced a series of extraterrestrial-infused night terrors accompanied by sleep-talking, shouting, and occasional bouts of sleep paralysis. Disrupted sleep is a common somatic symptom of trauma, particularly repressed trauma, even if the memories are different from the events themselves. Disrupted sleep as a result of trauma can be infused with sleep paralysis and hallucinations. Paralysis occurs when an individual awakens from Rapid-Eye-Movement, or REM sleep, and is often accompanied by tactile and visual hallucinations [9]. These hallucinations can be mistakenly viewed as a “reliving” of past experiences or encoded as entirely new memories [9]. Of course, hallucinations and memories differ, but sleep, and REM sleep in particular, is an altered state of consciousness where
one’s ability to accurately differentiate between reality and falsity is diminished. Did Betty and Barney have an alien-themed film playing before they went to sleep? Was the theme of abduction prevalent in the Hills’ childhoods or adulthoods? Were they perhaps

attacked by a group of people, and in an effort to contend with the pain of being attacked, framed it as something non-human entirely? Speculation alone is worth little, but it is worth considering the impact and influence of these different elements on the final stored memories. Just like with hypnosis, a sleeping individual is in a vulnerable state, and any of these variables could have affected the contents of the night terror.
THE IMPORTANCE OF RECOGNIZING AND TREATING TRAUMA, REGARDLESS OF ORIGIN
Simon ultimately argued that Barney borrowed his narrative from snippets overheard from Betty, and Betty had misremembered her night terrors for reality [1]. It was a logician’s attempt to explain the impossible. Although Simon’s analysis provided a rationale for both the matching narratives and the extremity of the experience, it fails to negate that the Hills did, in fact, encounter something in the woods that night. That particular something was also deeply distorted and responsible for the development of severe psychological perturbations.
Repressed memories, now also referred to as dissociative amnesia, are frequently mischaracterized as “materializing out of nowhere” or “appearing purely because of suggestions.” These memories remain a hotly contested topic in psychological research for neuroscientists and psychologists, with their reputation being born out of early therapeutic techniques used to examine childhood sexual trauma. More extensive cross-examination of these techniques revealed frequent instances of reinterpretation and misassigned meaning, often crossing the line into the formation of entirely false memories. These techniques were phased out as our understanding of human memory and memory formation improved. Psychologists learned that often certain aspects of trauma are relatively well-remembered, flashbacks and intrusive memories are relatively common, and complete memory loss is rare [10]. In addition, it was discovered that traumatic memories can be painted as entirely different events, with the original details being temporarily replaced by more salient details [10]. The core components of the traumatic event typically remain the same, however. The Hills did not display severe repression per say; there was a lapse in time between the beginning and end of their abduction, but their reaction and investigation of the events began relatively quickly. As we have uncovered through an admittedly brief exploration into false memories, memories are remembered for a reason. Sometimes, the details that provide a memory’s backbone and flesh are falsified, eventually appearing twisted, deformed, even alien-like. Sometimes it isn’t this dramatic. But even an illogical narrative sticks as a memory because it is somehow salient. Repressed memories are referenced most frequently within the realm of trauma [10]. A traumatic event occurs and is characterized by extremely aversive emotions, which are difficult for an individual to bear; the memory is almost too sticky, like molasses. Its presence gums up the neurological workings of the brain, oozing out in unexpected ways. With the Hills, this dark ooze was anxiety, panic attacks, night terrors. It looks different for everyone, but it is nearly always disrupting the system, and takes time and care to be treated effectively and empathetically. Recognizing the validity of the Hills’ trauma is critical; though their experience may be labeled as “false,” “whacky,” or “unsettling,” the couple still experienced life-altering consequences, both in

the context of their personal battles and in the larger lens of their cultural impact.
However, within this recognition a key question still remains: did the abduction really occur? The painstakingly detailed accounts, the night terrors, and the public frenzy would certainly suggest a high degree of believability. Yet, only the Hills will ever truly know. That’s the core reality to keep in mind; their memory of that night is inevitably subjective, ever-shifting, and fallible. Our interpretation of their experience is just as fallible because sometimes, memories just aren’t correct, no matter how much we believe (or want to believe) them.
With difficult or traumatic memories, whether they are false or true can have significant implications. With the story of the Hills, their impact was both individual and collective. That fateful night drive through the White Mountains blew their understanding of life to pieces, literally. Earth was no longer the only place home to life, and not all other life forms were friendly. It rendered them psychologically disturbed, desperate for an explanation for their suffering. In the 1960s, their trauma, their healing, and their story resonated with millions. This tale of the extraterrestrial continues to have a profound impact on us all. Seeking answers to impossible questions is part of being human. Is there a God? Where do I go after I die? If I drove 76 miles unconsciously and woke up bruised and scratched, who took me and where did I go? Perhaps we don’t all turn to aliens and saucers to quell our thirst for explaining life’s uncertainties, but we all surely turn to something.

BEWARE THE POST-VACCINE BLUES
by Brenna McMannon art by Darling Garcia
Have you ever had the post-vaccine blues? It’s hard to imagine that such a minor experience could manage to impact your mental health. However, in recent years, evidence has emerged supporting a possible link between bodily inflammation and depression. This idea — that inflammation, the body’s natural response to injury, can have a psychological impact — has expanded our perception of mental health, adding to the enigma of the human brain. The mystery of the brain has made mental health, and depression specifically, incredibly hard to study and even harder to treat. This is mainly due to the fact that no one brain region or molecule has been identified as the sole cause of major depressive disorder (MDD), despite the fact that about 21% of women and 12% of men in the United States alone will experience depressive symptoms at some point in their lives [5]. This gap in understanding poses a real threat to people suffering from MDD across the world. However, recent research suggests a link between bodily inflammation and depression, expanding our understanding of the many causes of depression and aiding in the development of treatments. Before we get into that, let’s explore our existing knowledge of depression.
DEPRESSION: WHAT WE KNOW
Many of the key players in depression are concentrated in the limbic system: the set of brain structures involved in emotion and memory. Despite this knowledge of where depression occurs in the brain, the treatment of depression doesn’t focus on these brain regions; rather, it targets the tiny chemicals that send messages between them. Yes, I’m talking about neurotransmitters, the famous chemical messengers of the brain. Brain cells called neurons send signals to one another via neurotransmitters. Therefore, the amount of neurotransmitters being produced are important to their functionality, because having too little or too many can cause problems.
Over the past half century, psychiatrists have prescribed depressed patients with drugs that aim to correct a chemical imbalance in the brain, usually involving a reduction in the neurotransmitter serotonin. Enter: Prozac. Also known as fluoxetine, this drug is currently the most commonly prescribed antidepressant and is classified as a selective serotonin reuptake inhibitor (SSRI). The drug functions to correct serotonin imbalances in the brain by allowing more serotonin to accumulate in the spaces between neurons, called synapses, through which neurotransmitters travel from one neuron to another. Then, neurotransmitters bind to the receiving cell and convey their signal. SSRIs work to keep serotonin from being recycled back into the neuron that released it, leading to an accumulation of serotonin in the synapse. When the concentration of serotonin in the synapse increases, the neuron receiving the signal can be activated more frequently.
SSRIs work for many people with depression, boosting their mood and stripping them of their depressive symptoms. However, the causal link between serotonin and depression is still widely unknown. While a serotonin imbalance may play an important role in some patients’ depression, this is not the case for every person with MDD. Unfortunately, SSRIs and other antidepressants don’t work for everyone suffering from depressive symptoms. In fact, about 30% of people with depression do not respond to any antidepressant treatments [1]. These patients suffer from treatment resistant depression (TRD) and end up trying every kind of treatment you can imagine (meditation, talk therapy, medication, and medical procedures), often to no avail.
Depression research is ongoing and consistently funded, so why don’t we know more about its cause, especially in people with treatment resistant depression? Because most people suffering from MDD display such a wide array of responses to different treatments, its root cause remains elusive. Many people with TRD resort to electroconvulsive therapy (ECT) — one of the most effective TRD treatments, with a response rate of 50%-70% [3]. ECT uses electrodes to send an electric current through the brain, inducing a brief seizure. But here’s the kicker: nobody really knows how or why ECT is an effective treatment for TRD. This common theme in the study of MDD makes it difficult to formulate consistently effective solutions. Treatments like SSRIs and ECT reveal the high degree of variation among MDD patients, signaling how important it is to examine each case individually and treat the patient based on the suspected cause rather than employing a universal approach. This is where the immune hypothesis comes in as another potential cause of depression.
THE IMMUNE HYPOTHESIS
The immune hypothesis proposes a possible link between inflammation in the body and depression in the brain. However, the existence of an important brain structure, called the blood brain barrier (BBB), has made it hard for scientists to causally link bodily inflammation with depression. The BBB is a filtration mechanism built into the endothelial cells that surround the brain. These cells form an important layer within blood vessels that regulate the exchange of materials. The primary function of the BBB is to prevent toxins and other potentially harmful substances from entering the central nervous system (i.e. the brain and spinal cord). The filter also blocks out large molecules, cells, and other structures, meaning that many substances — like immune cells — circulating in the periphery of our bodies are not able to enter and affect the brain. For example, when you stub your toe, it usually becomes inflamed. However, scientists never thought that this simple inflammatory response could reach the brain because the immune cells are too big to cross the BBB. Now, we know that this is far from the whole story.
In order to fully understand the connection between inflammation and depression, we must first familiarize ourselves with some important members of the immune system. Inflammation is the body’s natural reaction to injuries or viruses. When you sprain your ankle or get a root canal, your body generates a cytokine storm. Cytokines, the messenger cells of the immune system, are released from immune cells and sent out to promote inflammation and protect affected areas. In other words, your body starts vigorously pumping out cytokines to spread the word that there is an injury or foreign invader. This maelstrom of angry cytokines arrives on the scene and removes damaged tissue so that the healing process can begin. The main player in inflammation is a proinflammatory cytokine called tumor necrosis factor (TNF). While TNF is too big to cross the BBB, in the past few decades, scientists have discovered a correlation between increased blood levels of proinflammatory cytokines, like TNF, and depressive symptoms [4]. But, how is this possible if cytokines can’t cross the BBB?
This is where we find out that stubbing your toe can
actually affect your mental health, bringing a mindbody connection into play. Pathogens, like influenza or Salmonella virus, have previously been associated with depressive symptoms, such as feelings of sadness or apathy [14]. Interestingly, these pathogens have the ability to cause the release of cytokines and the consequent activation of microglial cells in the brain [12]. Microglia are the first line of immune defense for the central nervous system, as the immune cells of the brain. Inflammatory cytokines are able to get their message across the BBB and to the microglia without actually entering the brain, by binding to receptors within the endothelial cells. When microglia pick up the signal that there is inflammation in the body, they start pumping out their own cytokine storm into the brain. The involvement and function of cytokines in the brain is still poorly understood, but we do know that it is the brain’s response to receiving an inflammatory message. Although this is a natural biological response, microglial activation can be harmful, especially in the context of depression.
When these angry microglia activate cytokines in the brain, they often impact serotonin production. Normally, cells in the brain produce serotonin from an amino acid called tryptophan. But when cytokines are released into the brain and start causing trouble, they can potentially instruct cells to use tryptophan to create other products in place of serotonin. Not only are these new products toxic to other cells in the brain, but they also decrease levels of serotonin. In this sense, it is no surprise that depressive symptoms tend to correlate with an increase in nonserotonin, tryptophan-derived molecules, resulting in a decrease of serotonin in the brain [9]. Decreased serotonin levels may also render some SSRIs ineffective, which may help explain why some people don’t respond to them. SSRIs work to inhibit the reuptake of serotonin, so if there is not enough serotonin being produced to begin with, they would have no effect. In fact, one study found that MDD patients who don’t respond well to SSRIs and other antidepressants are more likely to already have some sort of inflammation present in their body [8]. INFLAMMATION: WHERE DO WE GO FROM HERE?
There are so many ways for the body to become inflamed— it’s downright unavoidable. For instance, simply being female puts you at higher risk of inflammation due to factors such as childhood adversity, obesity, and interpersonal stressors, all of which disproportionately affect women [2]. Coincidentally, women also experience depression at a higher rate than men [5]. However, one of the most common causes of inflammation is psychological stress, as sustained feelings of stress can result in the chronic release of pro-inflammatory cytokines in the brain [6]. What’s more, chronic stress can lead to severe conditions like coronary heart disease (CHD) [13]. Even episodes of short-term stress can induce CHD in a more vulnerable subset of people [13]. This subset of patients has one thing in common: all are inflamed. Furthermore, the events of your childhood can affect levels of inflammation during adulthood [7]. Recent studies have found that experiencing some kind of childhood adversity (e.g. parental separation,

low socioeconomic status, or familial mental illness/ disorders) is often coupled with both inflammation and depression later on in life [7].
There’s a good chance that you will experience some level of inflammation-linked depression at some point in your life. So, how can you get ahead of it? There is compelling evidence that exercise can have a protective effect against the danger of stress, specifically chronic stress [11]. Of course, exercise is not going to be the perfect solution for everyone. What about people with chronic inflammation that isn’t caused by psychological stress, like rheumatoid arthritis? Conditions like these are considered to be autoimmune, meaning the immune system is overactive and producing inflammation where it isn’t needed. Scientists have started to develop experiments to invent drugs targeting this inflammatory response, though very few studies in the past decade have rendered promising results. One study conducted in 2013 included 60 people with MDD, half of which were taking antidepressants and half of which were resistant to treatments (moderate TRD). They were given either a placebo drug or a drug that contained a TNF antagonist, which worked to block the binding of TNF and prevent an inflammatory response. Over a 12 week period of drug administration, they found no overall differences in depressive symptoms between the placebo group and the antagonist group. However, when they reexamined the data, researchers found that when they took into account baseline inflammation, the drug had a significant effect. In other words, the participants that had a higher baseline level of inflammation at the start of the study experienced significantly more antidepressant effects than those who had less inflammation, suggesting that inflammation may have greatly contributed to their symptoms of depression [10].
This brings us back to the importance of individual differences and creating treatments based on the individual rather than the condition they suffer from. It’s clear that various risk factors, including childhood adversity, biological sex, and disease, produce different experiences of depression. In the same way that SSRIs may not work for those who are struggling with a serotonin imbalance, TNF antagonist drugs may be ineffective in treating those without inflammation. Eventually, there needs to be a comprehensive diagnostic test to determine the cause of a patient’s symptoms. Then, an individualized treatment plan could be developed to target that cause. But don’t hold your breath — these kinds of things take time. Depression research is constantly evolving, and this new link between inflammation and depression is simply the beginning of another chapter in understanding the complexities of the brain.
Only when future developments enable us to look past the diagnosis of MDD and determine the specific causes for each person, will relief be an option for everyone. For now, this developing link between inflammation and depression may clear the way for the development of new and effective treatments. And it may explain why you feel a little down in the dumps after getting your COVID-19 vaccine.
by Benjamin Kheyfets, Daniella Lorman, and Clem Doucette / art by Phoebe Kinder
RNA: A NEW FACE IN THE FIGHT AGAINST NEURODEGENERATION
In the time it takes for you to read this sentence, over seven million cells in your body have died. And by this same time tomorrow, an unfathomable 1011 more of your cells will have died and been replaced by new cells [1]. As alarming as this fact may sound, cell death, known as apoptosis, is an essential process to biological life. Apoptosis is critical in regulating a number of different bodily functions, ranging from the shapes of our organs to the amount of neurons in our nervous system [1]. However, certain conditions, like neurodegenerative diseases (NDDs), can cause apoptosis to go haywire, and when unplanned apoptosis occurs in the brain, it can result in catastrophic effects [2].
Right now, nearly 6.5 million Americans are suffering from some form of neurodegenerative disease, and estimates show that by 2030, as many as 12 million Americans may suffer from a NDD [3]. NDDs occur when the cells of the nervous system — including those of the brain, spinal cord, and nerves — function abnormally. Symptoms may be mild at first; short-term memory loss or coordination issues are common early indications of NDDs. However, as cells continue to deteriorate, symptoms such as loss of communication, seizures, and skin infections gradually increase in severity until they become fatal [4]. Unfortunately, no NDD is currently curable [5]. While some treatments do exist, such as medications and therapies, these interventions can only slow disease progression and manage symptoms. Given the ever-increasing urgency to find cures and treatments for NDDs, biotech and pharmaceutical companies have been heavily investing into research endeavors. A growing body of new research shows that genetic regulation, specifically via RNA, may play a huge role in the development of these diseases [6]. With this new and extensive research, RNA and its role in NDD development and progression has garnered a considerable spike in interest. This review will explore the role of RNA in neurodegenerative disease, with the goal of illuminating potential options for future treatments or cures.
RNA: MORE THAN A MESSENGER
In order to explore how RNA is involved in NDDs, it is essential to first understand RNA’s relationship to DNA. Imagine that you are in charge of developing a standardized cookbook for a nationwide fast food chain. Each restaurant receives the same cookbook, which has specific information about the ingredients needed to make each meal and exactly how to prepare it. Our DNA, found in the nuclei of most of our cells, is just like this cookbook.
A DNA molecule consists of alternating sugars and phosphate groups; these components create DNA’s famous double helix structure. The “steps” of DNA’s ladder-like structure are made up of four different molecules called nucleotides: adenine, thymine, guanine, and cytosine, abbreviated with the letters A, T, G, and C [7]. A group of three letters (i.e. CCG, ATG, and ACT) is called a codon, which codes for an amino acid — the building blocks of proteins, and the ingredients in our recipes. Like recipes in a cookbook, these unique orderings of nucleotides provide the blueprints for creating different amino acids, and subsequently proteins. Just like cooking, where the ingredients you use determine the dish you end up with, the order of the amino acids in a protein determines the identity and function of that protein, and the order of the letters of DNA determine the genetic code of the individual.
But how are these DNA recipes then turned into proteins? Enter: RNA. If DNA is a cookbook with recipes, then RNA is a copy of one recipe, containing the same information. However, RNA doesn’t write this recipe in the exact same code. Unlike DNA, RNA is a single stranded molecule with a slightly different chemical composition; in place of the DNA’s T, RNA uses a different nucleotide, uracil, abbreviated U [8]. Like in DNA, the order of nucleotides in RNA is critical. While the order of nucleotides in DNA determines an individual’s genetic code, the order of nucleotides of RNA determines the RNA’s function or the corresponding protein that will be made.
RNA’s most well-known role is that of the messenger RNA (mRNA) molecule. Messenger RNA serves as the genetic intermediary between DNA and ribosomes, or the organelles that manufacture proteins in our cells. Ribosomes are the chefs of our restaurant analogy. This process of creating mRNA from DNA is known as transcription, where, after being created, the mRNA recipe copy is brought to the ribosome (i.e. the chef). The ribosome then uses the mRNA recipe to create proteins; this process is known as translation. Because both transcription and translation are essential to cell functioning, they are regulated very closely to minimize the potential for missteps or errors.
While bringing a copy of a recipe to the cook is the most common job of RNA, recent research has found that RNA does far more than just carry messages. Researchers have identified different classes of RNAs based on their length and function [9]. One such class is microRNA (miRNA); these mainly bind to mRNA molecules in order to block the ribosome from producing the mRNA’s encoded protein. If you are the ribosomal chef, this is like trying to read a smudged or water-stained copy of the recipe. While some portions of it may be legible, using it to prepare a meal would be virtually impossible. Another class of RNA is small interfering RNA (siRNA); these are short RNA molecules that bind to certain other RNA molecules, triggering their destruction. Cells can use siRNAs as a defense mechanism, protecting themselves from viruses and other foreign entities by destroying foreign nucleic acids [10]. In our restaurant analogy, siRNA would be a health inspector stopping by a restaurant where a number of customers have suffered severe food poisoning. To prevent further illnesses, the health inspector throws out the restaurant’s recipes causing sickness. Additionally, long noncoding RNAs (lncRNAs) are lengthy RNA molecules that, like siRNAs and miRNAs, do not actually code for proteins. Because of their length, they can take on many different shapes, and, depending on the specific characteristics of the RNA, can aid in the regulation of many different genes [9].
A KEY PLAYER IN NDD ONSET
Abnormalities in certain processes involving RNAs have been increasingly implicated in neurodegenerative diseases [11]. For example, a recent study suggested that flaws within proteins that bind to RNA, termed toxic aggregates, are a potential cause of certain NDDs [12]. Additionally, recent research has shown that NDDs can also be caused in part by the presence of too many RNA protein aggregates, which influence how mRNA is processed after it is formed. The role of RNA in NDDs is thought to be due to its self-assembling

nature: certain RNAs can spontaneously assemble without the need for any energy or assistance from the cell [13].
One mechanism related to RNA that may contribute to the cell degradation characteristic of NDDs can be found in the functioning of lncRNAs [14]. LncRNAs are highly expressed in our central nervous system, and their expression is regulated so that they are only present in certain regions of the cell at certain times. This selective expression allows the cell to respond efficiently to environmental changes. In patients suffering from several NDDs, lncRNAs have been demonstrated to dysregulate proteins throughout the
central nervous system, interfering with how certain proteins bind to other classes of proteins. For example, lncRNAs in Parkinson’s disease patients increase the rate at which ribosomes create certain proteins from RNA. Several types of lncRNAs have also been found to be dysregulated in patients with Huntington’s disease, becoming either over- or under-produced [15]. More specifically, researchers have found that certain lncRNAs play a role in the development and onset of Alzheimer’s. One known connection between RNA and Alzheimer’s disease includes the lncRNA BACE1-AS, which protects certain mRNAs from being degraded by certain miRNAs. This process can lead to the buildup of the plaques that contribute to Alzheimer’s. Another lncRNA named 51A leads to the formation of compounds that are involved in the onset of Alzheimer’s [16]. These molecules play an intricate role in NDDs and regulating neurons, and researching their dysregulation may be the key to improved treatments, and perhaps even cures [14].

RNA DRUGS IN NDD TREATMENTS
In light of our new understanding of RNA’s role in NDDs, researchers have explored the efficacy of RNAtargeted drugs to address problems created by the dysregulation of proteins. In 2018, two new drugs, inotersen and patisiran, were approved in the United States and Europe to treat hereditary transthyretin (hATTR) amyloidosis [17]. This disease is caused by a mutated form of the gene that codes for transthyretin, a blood protein made in the liver. This mutation makes transthyretin dissolve less easily, so instead of freely traveling throughout the blood as it should, the protein clumps up around nerves and destroys neuronal tissue function. To treat this, inotersen and patisiran bind to the mRNA that encodes for the mutated form of transthyretin, blocking the ribosome from using this mRNA, preventing the clumps of mutant protein from forming. The drug inotersen, a modified form of DNA, accomplishes this by binding to the transthyretin mRNA and blocking it from producing mutated transthyretin proteins. Meanwhile, when patisiran (an siRNA drug) binds to the mutated transthyretin mRNA molecule, the cell destroys the mRNA strand [17]. Thinking back to our cookbook, the functioning of patisiran is like having your recipe copy come out either smudged and unclear, making it unreadable, or having the copy torn up, making it unusable. In either case, the meal doesn’t get made.
Even though these drugs show enormous potential for NDD treatments, there is still a long way to go
until such medicines can become commonplace. First, RNA tends to degrade in a cell relatively quickly [17, 18]. A drug made of RNA must be able to survive in the body long enough to enter the cells or organs of interest and interact with other molecules. To combat this degradation, the RNA is often packaged in lipid nanoparticles, which are spheres made of lipids (a type of fat molecule). Second, these treatments are somewhat invasive. RNA-based medicine cannot be taken orally; the technology still hasn’t developed to that point of convenience. For treatment to be effective, it needs to be injected either subcutaneously (under the skin) or intravenously (into the bloodstream). Third, there are potential side effects of RNA medicines, many of which we may not know of yet. For example, intotersen can lower one’s blood platelet count, potentially leading to difficulty in clot formation and, therefore, severe bleeding. Additionally, patients who receive patisiran also need to receive steroids to suppress other unwanted infusion-related reactions [17]. As such, researchers are still trying to uncover the consequences of, or risks associated with, RNAbased medicines.
RNA: THE FUTURE OF MEDICINE?

RNA may be useful in the treatment of NDDs and other physiological diseases. In fact, the COVID-19 pandemic may be accelerating RNA-based research, as both the Pfizer and Moderna vaccines are mRNA vaccines [19]. When you get either vaccine, you are injected with mRNA that codes for all or part of the spike protein found on the surface of SARSCoV-2 (i.e. the virus that causes COVID-19) [20]. Your immune cells then manufacture that very protein, and its presence triggers an immune response. Then, if you are infected with SARS-CoV-2 following your vaccination, the immune system will already be equipped with the ability to handle the virus quickly before it can cause any serious damage [20]. Arming the immune system with preemptive knowledge of a disease is the basic premise of vaccines. However, some vaccines accomplish this using a different strategy. The Sinopharm vaccine created by the Beijing Institute of Biological Products, for example, uses a handicapped version of the actual SARS-CoV-2 virus to reach immunity [21]. NDDs are very different from viral infections, but the success of these RNA vaccines coupled with increased research behind RNA’s roles in NDDs still may lead researchers to develop RNAbased medicines for NDDs [22]. Despite expectations of RNA acting solely as a messenger (or a copier of recipes), recent research has proven it to be a molecule of many trades. With its diverse classes and forms, RNA is a multifaceted player in many essential neural processes. Considering the increasing prevalence of NDDs, discoveries of neurodegenerative implications associated with RNAmediated protein production are more imperative than ever. While we still have a lot to learn about RNA’s role in the process of neurodegeneration, RNA-based medications offer a promising new treatment option to the millions of people suffering from NDDs and may be the first step taken toward finding a cure.










