28 minute read
CONTRACEPTION Theresa Lowry Lehnen provides a comprehensive overview of the available methods of contraception for women and men in Ireland
AUTHOR:
Theresa Lowry-Lehnen, RGN, PG Dip Coronary Care, RNP, BSc, MSc, PG Dip Ed (QTS), M Ed, PhD,and Clinical Nurse Practitioner and Associate Lecturer, South East Technological University
A-Z OF CONTRACEPTION
EXAMINING THE VARIETY OF CONTRACEPTION METHODS AVAILABLE IN IRELAND TO HELP YOUR PATIENTS MAKE THE RIGHT DECISIONS FOR THEM
Contraception is the act of preventing pregnancy. Although hormonal contraceptives and intrauterine devices (IUDs) are highly effective at preventing pregnancy, they do not protect against sexually transmitted infections (STIs). The correct and consistent use of condoms, in addition to helping prevent pregnancy, reduces the risk of contracting HIV and other sexually transmitted infections. Condoms offer the best protection from STIs if used correctly, and using dual protection, ie, condoms with another method of contraception, is recommended.1,2
There are many different types of contraception available. Choosing the right method is a personal decision and involves finding what works best for the individual. Contraceptive counselling with a health professional is a marked contributor to the successful use of contraception. When considering contraceptive methods, counselling should include efficiency, safety, acceptability, and availability, including accessibility and affordability.
Some 17-to-25-year-olds can now get free contraception in Ireland. The free scheme is to be extended to 26-yearolds from January 2023, and to 26-to30-year-olds in September 2023. The free contraception scheme covers the full cost of prescription contraception, including the cost of consultations with medical professionals to discuss suitable contraception options and enable prescription of same. The scheme provides a wide range of contraceptive options, including contraceptive injections, implants, IUDs, intrauterine systems (IUSs), the contraceptive patch and ring, and various forms of oral contraceptive pill, including emergency contraception. It also includes fitting and removal of long-acting reversible contraception (LARC), plus any necessary checks by medical professionals certified to insert or remove them. This is a major step forward for sexual and reproductive health in Ireland, and a progressive step towards promoting women’s health.2
Combined hormonal contraceptives (CHCs) containing synthetic oestrogen and progesterone are among the most commonly prescribed and wellresearched types of contraceptive medication in use. CHCs can be delivered through a pill, patch, or vaginal ring. In CHCs, both progestins and oestrogen inhibit the hypothalamic–pituitary–ovarian axis, which controls the reproductive cycle. Progestins prevent pregnancy by inhibiting the luteinising hormone (LH) surge, suppressing ovulation, thickening the cervical mucus, lowering fallopian tube motility, and causing the endometrium to become atrophic. Oestrogens prevent pregnancy by suppressing folliclestimulating hormone (FSH) production, which prevents the development of a dominant follicle. Progesterone is responsible for most contraceptive action and side-effects, and the addition of oestrogen helps prevent irregular or unscheduled bleeding.4
The combined pill is more than 99 per cent effective with perfect use and 91 per cent effective with ‘typical use’. Advantages are that it does not interrupt sex, often reduces bleeding and period pain, and may help with premenstrual symptoms. Disadvantages are that it can be less effective if a pill is missed, if there is vomiting or severe diarrhoea, or by taking certain medications. It is not suitable for smokers over 35 years of age or those who are obese. It may not be suitable for women who are breastfeeding and medical advice should be obtained. The combined pill may not be suitable for women with hypertension, circulatory disease, blood clots, breast cancer (current or within
mycontraception.ie (2022)
the past five years), migraine with aura, gallbladder or liver disease, or diabetes with complications.5 On commencing the combined pill, some women may experience breast tenderness, skin irritation, mild headaches, a bloated feeling, or have some breakthrough bleeding between periods. These symptoms should settle within the first few months of using the combined pill. In healthy women who do not smoke, the combined pill can be used up to menopause. However, as the risks of cardiovascular disease increase with age, doctors often recommend changing after the age of 40. Long-term use of the combined contraceptive pill does not affect fertility, but once stopped, it may take some time for the body's natural hormones to go back to their normal levels.2,3,5
The CHC transdermal patch is a thin adhesive square about 4-5cm wide, containing synthetic oestrogen and progesterone. It can be placed on the stomach, upper arm, buttock, or back, and must be completely attached to the skin to be effective. The patch is replaced every week for three weeks. During the fourth week, no patch is worn and a withdrawal bleed occurs. It is over 99 per cent effective with perfect use, and 91 per cent effective if not always used correctly.2,4 Advantages are that it does not interrupt sex and may be easier to remember than taking a pill every day. Unlike the pill, the CHC patch is not affected by vomiting or diarrhoea. It may protect against cancer of the ovaries and the uterus.5 Effectiveness may be reduced by taking certain medications. It is not suitable for people who are obese, or for smokers over the age of 35. It may not be suitable for women who are breastfeeding, and
medical advice should be sought.2,3 It is a very effective method when used correctly, however, pregnancy can occur if an error is made using the patch, especially if it becomes loose or falls off for more than 24 hours, or the same patch is left on the skin for more than one week.5
The CHC vaginal ring (NuvaRing) is a clear, flexible ring about two inches in diameter containing synthetic oestrogen and progesterone that is placed in the vagina for 21 days, and removed for seven days to allow for withdrawal bleeding. It is replaced monthly. Users can place the ring in the vaginal canal themselves. As with the patch, the less frequent applications can be appealing and can lead to increased adherence. The ring’s internal placement ensures the steady delivery of hormones, which allows for lower serum concentrations than occur with either the patch or pills. As a result, the ring generally has milder side effects than seen with other CHC delivery methods. Some users may experience increased vaginal irritation and discharge. There is also some evidence of reduced vaginal dryness, which may appeal to perimenopausal women and others who tend to experience such dryness.4 It is over 99 per cent effective with perfect use, and 91 per cent effective if not always used correctly. Advantages are that it can be self-inserted, does not interrupt sex, and stays in place for 21 days before removal. Its effectiveness may be reduced by taking certain medications, and it is not suitable for people who are obese or smokers over 35. It may also be unsuitable if breastfeeding and medical advice should be sought for same.2,3
Ring users may have concerns about their risk for pregnancy if the ring is removed intentionally or accidentally. The ring can be removed for up to three hours without diminishing its contraceptive effect. The manufacturer recommends rinsing the device in cool or lukewarm water prior to reinsertion. If the ring is out for more than three hours, users should take extra steps to protect (condoms or abstinence from sex) against pregnancy. As with any device, users should consult the package insert for more specific instructions.4
Progesterone-only pill (POP)
POPs are generally made with firstgeneration progestins and dosage amounts are substantially lower than those found in any CHC. POPs must be taken at the same time every day. They are used continuously, with no hormone-free interval.4 Progestogenonly pills are considered safe in many clinical scenarios where CHCs are contraindicated. Progestogen-only
pills, however, have a higher failure rate when not taken at the same time every day because effective drug levels are only maintained in the bloodstream for 22 hours. The progestogen-only pill may be commenced at any time. Another method of contraception should be used if vaginal intercourse takes place during the first 48 hours of pill use. Protection will begin after two days.5 The most common side-effects of POPs are unscheduled bleeding and spotting, likely due to the shorter daily window of efficacy and the absence of oestrogen. Its effectiveness may also be reduced by taking certain medications, missing a pill, or having vomiting or severe diarrhoea. Advantages are that it does not interrupt sex and can be used by smokers over the age of 35. It can also be used while breast feeding.2,3 The progestogen-only pill may not be suitable for women with liver, heart disease or stroke, breast cancer (current or in the past), systemic lupus erythematosus (SLE) or lupus, or irregular vaginal bleeding. However, in healthy women with no medical conditions that make it unsuitable, it can be taken until menopause or age 55.5
There are two types of progestogenonly pills available in Ireland, Noriday and Cerazette, which differ in the way they work and instructions for what to do if a pill is missed. If a pill is forgotten, it should be taken as soon as remembered, and the next one at the correct time. This may mean taking two pills in one day. If the Noriday
pill is taken more than three hours late, the woman is not protected. She should continue to take the pill as soon as possible and will be protected again after two days of taking the pill normally. Until then, using condoms or abstinence from sex is required. If the Cerazette pill is more than 12 hours late the woman is not protected against pregnancy. Protection against pregnancy will return after two days of taking the pill normally. Until then using condoms or abstinence from sex is required.5 It is unlikely that taking the pill during early pregnancy will increase the risk of defects in the foetus. However, although it is rare, the likelihood of ectopic pregnancy is greater if pregnancy occurs while taking the progestogen-only pill.5
Long-acting reversible contraception (LARC)
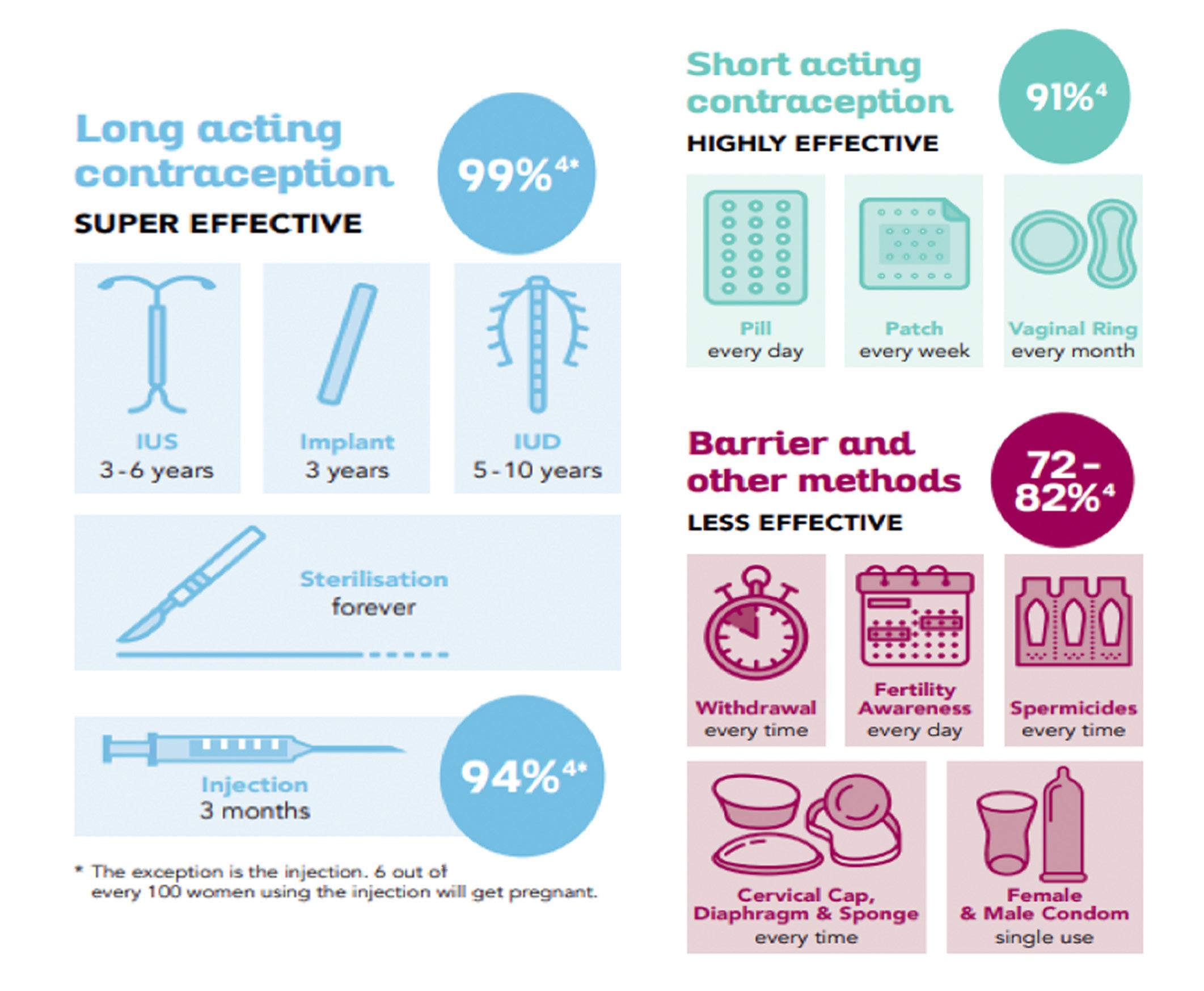
LARCs are a group of contraception methods that provide very effective contraception, are long-acting, and reversible when removed or stopped. They include injections, IUDs, IUSs, copper coils (IUCDs), and subdermal contraceptive implants. LARC are the most effective reversible methods of contraception because their efficacy is not reliant on patient compliance.
LARC needs to be inserted and removed by a specially trained doctor or nurse. Most are more than 99 per cent effective. An exception is the injection, which can have lower efficacy. LARC can be used by most women of any age, including those who cannot use contraception containing oestrogen; experience side-effects with oestrogen, such as nausea or breast tenderness; have migraines; smoke; have never had a baby; are breastfeeding or have recently had a baby; have recently had a termination of pregnancy; are overweight; have diabetes or epilepsy; are living with HIV; or have inflammatory bowel disease. Different LARC work in different ways.6
Implant (Implanon)
The contraceptive implant is a small flexible plastic rod, which is implanted by minor surgery under the skin in the inner part of the upper arm. Local anaesthetic is used to numb the skin before insertion. The implant slowly releases progesterone hormone and gives contraceptive protection for three years. It can be removed at any time with minor surgery, and it can be used by women of all ages, whether they have had children or not. A pregnancy test will be performed before insertion to confirm the woman is not pregnant. The implant is suitable for women who are breast-feeding or who do not tolerate oestrogen. Fertility returns to normal once the implant is removed. In the first three-to-six months of use, many women have irregular bleeding. After this, most women will have lighter or less frequent periods. Some will have regular monthly periods and some will not bleed at all.3,7
The implant will begin to work within one week. If there are no medical problems, the implant can be used as a method of contraception until menopause. Each implant will have to be changed every three years, but there is no limit to the number of implants that can be fitted. Removal may leave a small scar. The implant is not affected by common antibiotics, but is affected by enzyme-inducing medication, such as HIV treatments or epilepsy medication.7,8
An implant can be inserted three weeks (21 days) after giving birth. If the implant is inserted on or before day 21, the woman will be protected from pregnancy immediately. If the implant is put in later than day 21, an extra method of contraception is required for seven days. The implant can also be used immediately after a miscarriage or termination of pregnancy.7,8 There is no evidence that there is a delay in return to fertility after the removal of an implant. Over 90 per cent of women will have returned to a normal cycle within three-to-four weeks.7
IUS hormonal coil
The hormonal coil, also called an IUS, is a small, T-shaped device that is placed in a woman’s uterus. It is made of flexible plastic, which contains a slow-releasing hormone called levonorgestrel. It has two soft threads on the end that hang through the opening at the entrance of the cervix into the top of the vagina. An IUS works by changing the conditions in the uterus and cervix. These changes prevent sperm fertilising an egg and may also prevent a fertilised egg implanting in the womb.9
There are three types of IUS available; the Mirena, which lasts for eight years Kyleena for five years, and Jaydess for three years.2,9 An IUS can be fitted at any time during the menstrual cycle, once it is confirmed that the woman is not pregnant. An internal examination is carried out before the IUS is inserted and the insertion visit takes approximately 15-to-20 minutes. Insertion can be uncomfortable and some women experience a periodtype pain and light bleeding for a few days afterwards. Some women may experience common hormonal sideeffects, such as headaches, breast tenderness, and abdominal discomfort. There is a small risk of infection and of expulsion. The risk of perforation is very low when the IUS is fitted by an experienced healthcare provider.
A check-up is required four-to-six weeks after insertion, to check the strings, make sure the device is properly in place, and that there are no problems. The woman is taught to feel for the strings and should check them monthly to make sure the IUS is in place. Normal fertility returns as soon as the IUS is removed. Another IUS can be inserted directly after the old IUS has been removed. If the woman is not going to have another IUS inserted, is sexually active and does not want to become pregnant, an extra contraceptive method, such as condoms, should be used for seven days once the IUS is removed. An IUS can be put in within 48 hours of giving birth, but fitting of an IUS is usually deferred until at least eight-to-12 weeks after the birth. Another contraceptive method will need to be used until then. An IUS can be used safely while breastfeeding and does not affect milk supply.9
IUCD- copper coil
An IUCD, also known as the IUD, loop, or copper coil, is a small T-shaped contraceptive device that is placed in a woman’s uterus. It is made of flexible plastic with a coating of thin copper wire. It has one or two soft threads on the end, which hang through the opening at the cervix into the top of the vagina. An IUCD works by preventing
sperm from surviving in the cervix, uterus, or fallopian tubes. It may also work by stopping a fertilised egg from implanting in the uterus.10
The IUCD acts as an effective method of contraception for five-to-10 years, depending on the device used. There are several different types of IUCDs. The newer devices contain more copper and are more than 99 per cent effective. Older IUCDs have less copper and are less effective. An IUCD can be fitted at any time during the menstrual cycle, once it is confirmed that the woman is not pregnant. An internal examination is carried out before the IUCD is inserted. Insertion can be uncomfortable and some women may experience a periodtype pain and light bleeding for a few days after insertion.10 There is a slight risk that an IUCD might perforate the uterus or cervix during insertion. This may cause pain, but there are often no symptoms. If this happens the IUCD may have to be surgically removed. The risk of perforation is very low when the IUCD is fitted by an experienced practitioner. There is also a small risk of pelvic infection in the first three weeks after insertion.10
An IUCD can be inserted within 48 hours of giving birth, but fitting is usually deferred until at least eightto-12 weeks after the birth. Another contraceptive method will need to be used until then. An IUCD can be used safely while breastfeeding.10
If another IUCD is not being inserted following removal of a device, and the woman does not want to become pregnant, an extra contraceptive method, such as condoms should be used for seven days before the IUCD is removed. Sperm can survive for up to seven days inside the body and could cause pregnancy once the IUCD is removed.10 If a woman becomes pregnant with an IUCD in place, the doctor will usually remove the device, if possible. While there is a risk of miscarriage following removal of the device, leaving it in could cause miscarriage later in the pregnancy. If the woman does not have a miscarriage, the IUCD will not harm the baby. An IUCD can be put in immediately after a miscarriage or termination of pregnancy if the woman was pregnant for less than 24 weeks. The IUCD is also a very effective form of emergency contraception used after unprotected sex or contraceptive failure.10
Injection (Depo-Provera)
The contraceptive injection, DepoProvera, contains the hormone progestogen. It is effective for 12 weeks. The hormone is injected into a muscle, initially during the first five days of a woman’s period, and further injections are required every 12 weeks. The injection acts primarily by preventing ovulation. Less often, it works by thickening cervical mucus to prevent sperm from fertilising an egg, or by altering the lining of the uterus, which may prevent implantation of a fertilised egg. The contraceptive injection may be associated with weight gain and other side-effects, such as acne, breast tenderness, bloating, and changes in mood. For some women, use of DepoProvera may be associated with an increase in weight of up to two-to-three kilograms over a one-year period.11,12
Some medical conditions may make the injectable contraceptive unsuitable. These can include breast cancer; unexplained vaginal bleeding; thrombosis; heart attack or stroke; diabetes with complications or for more than 20 years; active liver disease; and risk factors for osteoporosis. As with any injection, there is a risk of a small infection at the site of the injection. Prolonged Depo-Provera use for more than three-to-four years is associated with a small loss of bone mineral density, which is largely recovered when the contraceptive injection is stopped.11,12
The injection can be started immediately after a termination of pregnancy or miscarriage if the woman was pregnant for less than 24 weeks. Protection against pregnancy is immediate. If a woman has just had a baby, delaying the injection for six weeks often makes irregular bleeding less likely. Contraceptive injections can be used while breastfeeding. A small amount of hormone enters the milk, but is not harmful for the baby. There could be a delay of up to one year in the return of fertility after discontinuing the use of injectable contraceptives, so this method of contraception may not be suitable for women who are planning on conceiving a baby within the next year.11
Emergency contraception
Emergency contraception is a safe, effective, and responsible method of preventing pregnancy when regular contraception has failed, no contraception was used, and in the event of sexual assault. Emergency contraception will usually prevent pregnancy if taken on time.13
Emergency contraception, also known as post-coital contraception, is available in two forms, the emergency contraceptive pills (ECPs) progesterone (taken within three days of unprotected sex) and ulipristal (taken within five days of unprotected sex), or insertion of an IUCD.
The progesterone ECP is available from pharmacies without a prescription, and from a doctor or family planning clinic. It must be taken within 72 hours of unprotected sex, but is most effective the sooner it is taken.
The main brand of the ulipristal ECP in Ireland is ellaOne. It is also available from pharmacies without a prescription, GPs, and family planning clinics. It must be taken within 120 hours of unprotected sex, but is more effective the sooner it is taken. Evidence suggests that the ulipristal ECP (ellaOne) is more effective than the progesterone ECP. Both methods of the ECP work by preventing or delaying ovulation, thereby preventing
fertilisation. There are no long-term side-effects from using the ECP.13
It is important to take the ECP as soon as possible after unprotected sex, and the doctor or pharmacist should be informed if the woman is taking any other medication. A small number of medications may reduce the effectiveness of the ECP, and the woman may need a different dosage or an IUCD. If vomiting occurs within three hours of taking the ECP, it is important that patients return to their healthcare provider as soon as possible for a second dose or further advice. Taking different kinds of the ECP during the same cycle is not recommended as they work in different ways. If a second dose is required during the cycle, the same ECP must be used as the first dosage. Other methods of contraception are recommended after taking the ECP as it does not provide contraception for the remainder of the cycle. There is a small risk of failure with the ECP and the woman may still become pregnant. The ECP does not work if a woman is already pregnant.13
Barrier methods of contraception Condoms
Condoms are a barrier method of contraception which work by preventing semen from entering the vagina. A male condom is made from very thin, natural latex rubber, which is soft and stretchy. It is closed at one end, with a teat to collect sperm, and fits over an erect penis. A female condom is made of very thin polyurethane plastic. It is closed at one end, and designed to form a loose lining to a woman’s vagina with two flexible rings, one at each end, to keep it in place.14
Advantages are that condoms help prevent the spread of HIV and STIs, are easily accessible, only need to be used when having sex, and have very few or no side-effects. Male condoms come in a variety of shapes and sizes. A female condom can be put in any time before sex. Disadvantages are that the male condom can sometimes slip off or split. Some people are sensitive to latex, though this is rare. Female condoms may be noisy and may slip during sex. Female condoms are not suitable for women who have an infection in their vagina or cervix.14
Male condoms are 98 per cent effective with perfect use every time, but 82 per cent effective when the method is not used correctly every time. Using condoms correctly requires practice. They can get damaged if handled roughly or used with an oilbased lubricant. They too must be
used before the expiry date on the packet. Female condoms are 95 per cent effective with perfect use every time, and 79 per cent effective when not always used correctly.15
Using condoms every time during sex reduces the risk of getting an STI. Condoms offer the best protection from sexually transmitted infections if used correctly. Using dual protection, ie, condoms with another method of contraception is recommended.2
Diaphragm
A vaginal diaphragm is a barrier method of contraception that fits into the woman’s vagina. Vaginal diaphragms are domes made of thin, soft silicone with a flexible rim. The diaphragm covers the woman’s cervix and prevents the sperm from reaching the egg. To be effective, diaphragms need to be used with a contraceptive gel to inactivate any sperm that are present. If used according to instructions and with the gel, latex diaphragms are 92-to-96 per cent effective. They are only 71-to-88 per cent effective if not always used correctly, and it is important that patients are made aware of this. They should receive an examination for the initial fitting and correct sizing, as well as education regarding correct insertion.17,18
Advantages are that the diaphragm can be put in place anytime before sex, reused after careful washing and drying, and it is a useful method if the woman wants to avoid taking hormonal contraception.18
Disadvantages are that it can disrupt sex; may not be suitable for people
who are sensitive to the chemicals in contraceptive gel; annual checks are required to make sure it still fits; a different size may be needed if more than three kilograms of body weight has been gained or lost; it must be left in place for at least six hours after sex, but not longer than 24 hours; extra spermicide must be used if sex occurs more than once; and it does not protect against STIs. Cystitis can also be a problem for some women who use a diaphragm. It may not be a suitable method of contraception for women with weak vaginal muscles, an unusual shaped cervix, repeated urinary tract infections, or a history of toxic shock syndrome.17,18
Other methods of contraception Spermicides
Spermicides are not very effective when used on their own and are best combined with a barrier method, such as a condom or a diaphragm. There are many different types available,
from foams to creams and gels, but they all work in similar ways. Spermicide needs to be applied prior to intercourse, every time.22
Chemicals in spermicides make it difficult for sperm to move in the vagina. Since spermicides are best used with another form of contraception, the directions on how to use them will depend on the barrier method they are applied to. Spermicides must be left in the vagina for at least six hours after sex. Close attention must be paid to the spermicide's expiry date. Some people experience allergic reactions or irritation caused by the chemicals in spermicide products. They do not protect against sexually transmitted infections.22
The withdrawal method
The withdrawal method pre-dates science and is not a reliable method of contraception. It involves the man removing his penis from the vagina before ejaculation. It requires a lot of self-control and it can be a very undependable method of contraception. Withdrawal does not protect against sexually transmitted infections.23
Natural planning
Natural planning, sometimes referred to as fertility awareness, is a technique of tracking exactly which stage of the menstrual cycle the woman is at, and only having sex on non-fertile days. Natural planning methods vary in terms of how much attention they need, but it’s important to be aware of fertile days and to use additional contraception on these days. It is about 76 per cent effective with typical use.24
Permanent methods of contraception Vasectomy - male sterilisation
Vasectomy (male sterilisation) offers a safe, convenient, and effective permanent method of family planning for men (or couples) who are certain that their family is complete and/or who do not want (any more) children. Before carrying out the procedure counselling is recommended to ensure it is the best method of family planning for them. The operation is a minor procedure carried out under local anaesthetic and involves cutting and sealing the spermatic tubes. The doctor will make either a small cut or puncture in the scrotum. The tubes will be cut and re-joined by tying the ends together or sealing them with heat. The opening in the scrotum is very small and sutures may not be needed. If sutures are required, dissolvable stitches or surgical tape will be used.
The operation takes approximately 10to-15 minutes to complete.19
There is a small risk that the procedure may not be successful. Semen tests should be performed 16 and 18 weeks after the vasectomy to ensure there is no sperm left in the tubes and that the operation has been successful. Until two negative semen tests have been confirmed, another method of contraception should be used. More than two semen tests may be required. There is also a very small risk, (one-in-2,000) of late failure.19
Vasectomy is a minor procedure with very little risk involved. However, a small number of men can experience bleeding, swelling, or infection, and occasionally sperm can leak out of the tube and collect in the surrounding tissue causing inflammation and pain. Vasectomy should not affect the man’s libido or sex life.19
Female sterilisation (tubal occlusion)
Female sterilisation, or tubal occlusion, is a surgical procedure carried out under anaesthetic to permanently prevent pregnancy. The fallopian tubes are blocked or sealed to prevent the sperm from reaching the egg and becoming fertilised.20 Sterilisation is for people who have completed their families or who are sure that they never want to have children. It should not be undertaken at a time of stress or crisis, and consideration should be given to alternative forms of long-term contraception during the decision-making process. Counselling will be recommended before the procedure. Female sterilisation cannot be easily reversed.21
A pregnancy test will be taken to confirm the woman is not pregnant before the procedure. There is a slight risk that the operation will not work. Although it is rare for fertility to return, the tubes do sometimes re-join. The risk of failure is about three-in-1,000, depending on the procedure used. All operations carry some risk, including the risk of wound and other infections, but the risk of serious complications with tubal occlusion is low. Wound sutures will need to be removed at a follow-up appointment, unless dissolvable sutures were used.20,21
It is very unlikely that pregnancy will occur after a tubal occlusion. If pregnancy does occur, there is a chance that the pregnancy will develop in the fallopian tube (ectopic pregnancy) rather than in the uterus. Contraception will need to be continued for four weeks after the operation or until the woman’s next period after the procedure. Sex can resume as soon as it feels comfortable. Sterilisation should not affect the woman’s libido or sex drive. The woman can usually return to work after five days, but this will depend on her general health and type of work. Heavy lifting should be avoided for a week.20,21

Outlook
Effective contraception provides social and health benefits by reducing unplanned pregnancies, termination of pregnancies, and facilitating family planning. Optimal contraceptive selection incorporates safety, efficiency, reliability, availability, accessibility and affordability, and should include the individuals’ preferences and values. Oral contraceptive pills are the most commonly used form of reversible female contraception. LARCs, including intrauterine devices and subdermal implants, have the highest levels of effectiveness. Progestin-only and nonhormonal methods carry the lowest risks. LARCs, which include IUDs, IUS-hormonal coils and IUCD-non-hormonal coils, and implants, offer women a safe, long-lasting choice for preventing pregnancy. They are highly reliable and more effective than birth control pills, the patch, or the vaginal ring. The injection is also a reliable method of LARC for many women, but can be less effective than other LARC methods, and is not suitable for all.2,25
There are currently no approved contraceptive options for men, except condoms and vasectomy. Research exists on hormonal forms of birth control for men, including a daily pill, however, no male birth control pill is currently available. Ongoing research is exploring further safe and effective contraceptive options for men. The two main areas of research are hormonal contraception using synthetic hormones to block the effect of testosterone on sperm development; and non-hormonal contraception using other techniques to prevent sperm from entering the vagina, such as injections into the vas deferens. Current male contraceptive methods under evaluation attempt to supress sperm count to <1 million/ml and include a testosterone plus progestin topical gel.25
REFERENCES
1. Bansode O, Sarao M. (2022). Contraception. In Statpearls publishing. Available at: www.statpearls.com/ ArticleLibrary/viewarticle/19940. 2. HSE Sexualwelbeing.ie (2022). Contraception. Available at: www. sexualwellbeing.ie/sexual-health/ contraception/free-contraception/. 3. Mycontraception.ie (2022). Smart alternatives to taking the pill every day. Available at: www.mycontraception.ie/ sites/g/files/vrxlpx28156/files/2021-11/ ie_wh_ius_2019_larc_smart_ alternatives_to_the_pill_-_design_ changed.pdf. 4. Britton L, Alspaugh A, Greene M, McLemore M. (2020). An evidencebased update on contraception. Am J Nurs. 2020 Feb;120(2):22-33. Available at: www.ncbi.nlm.nih.gov/pmc/articles/ PMC7533104/. 5. IFPA. (2021). The combined pill. Irish Family Planning Association. Available at: www.ifpa.ie/factsheets/ combined-pill/. 6. FPNSW (2022). Long-acting reversible contraception. Available at: www. fpnsw.org.au/factsheets/individuals/ contraception/long-acting-reversiblecontraception-larc. 7. Irish Family Planning Association (2021). Contraceptive implant. Available at: www.ifpa.ie/factsheets/implant/ 8. Implanon NXT Summary of Product Characteristics. Available at: www.medicines.ie. 9. Irish Family Planning Association (2021). IUS hormonal coil. Available at: www.ifpa.ie/factsheets/hormonal-coil/. 10. IFPA (2021). IUCD Copper Coil. Irish Family Planning Association. Available at: www.ifpa.ie/factsheets/copper-coil/. 11. IFPA (2021). Injectable contraception. Irish Family Planning Association. Available at: www.ifpa.ie/ factsheets/injection/. 12. Depo-provera Summary of Product Characteristics. Available at: www.medicines.ie. 13. IFPA. (2021). Emergency contraception. Irish Family Planning Association. Available at: www.ifpa.ie/ factsheets/emergency-contraception/. 14. IFPA (2021). Condoms. Irish Family Planning Association. Available at: www. ifpa.ie/factsheets/condoms/. 15. Sexualwellbeing.ie (2022). Male condom. Available at: www. sexualwellbeing.ie/sexual-health/ contraception/your-choices/condoms/ male-external-condom.html. 16. Sexualwellbeing.ie (2022). Female internal condom. Available at: www. sexualwellbeing.ie/sexual-health/ contraception/your-choices/condoms/ female-internal-condom.html. 17. IFPA (2021). Diaphragm. Irish Family Planning Association. Available at: www. ifpa.ie/factsheets/diaphragm/. 18. Sexualwellbeing.ie (2022). Diaphragm. Available at: www. sexualwellbeing.ie/sexual-health/ contraception/your-choices/diaphragm/. 19. IFPA (2021). Vasectomy. Irish Family Planning Association. Available at: www. ifpa.ie/factsheets/vasectomy/. 20. HSE (2021). Female sterilisation. Health Service Executive. Available at: www2.hse.ie/conditions/femalesterilisation/. 21. IFPA (2021). Tubal occlusion. Irish Family Planning Association. Available at: www.ifpa.ie/factsheets/ female-sterilisation/. 22. Mycontraception.ie (2022). Spermicides. Available at: www. mycontraception.ie/contraceptionmethods/the-spermicide. 23. Mycontraception.ie (2022). Withdrawal method. Available at: www. mycontraception.ie/contraceptionmethods/withdrawal. 24. Mycontraception.ie (2022). Natural planning. Available at: www. mycontraception.ie/contraceptionmethods/natural-planning. 25. Teal S, Edelman A. (2021). Contraception selection, effectiveness, and adverse effects. A review. JAMA. 2021;326(24):2507-2518. doi: 10.1001/ jama.2021.21392.