8 minute read
Ultrasound Zoom
Point-of-Care Ultrasound in Pulmonary Embolism
By Andrea Alvarado, MD, PGY-2
Advertisement
Jackson Memorial Hospital
Edited by Leila Posaw, MD, MPH
Emergency Ultrasound Director, Jackson Memorial visualization of a clot in transit is
Are you concerned about your patient who is short of breath? Is your patient hypotensive, tachycardic and too unstable for the “donut of truth” (also known as the CT scanner)? I know—I have been there. Identifying the etiology of shock can be nerve-racking in unstable patients, and when it is pulmonary embolism (PE), it can be scary as a large percentage of patients end in sudden death. We as emergency physicians need to be empowered to diagnose and manage such patients at bedside in the emergency department, and one of the best ways to do that is with point-of-care ultrasound. Our strategy needs to be directed towards examining the heart, lungs and lower extremity veins. Read on for my technique and tips!
TECHNIQUE A. Cardiac
Probe: Phased array probe
Fig. 1: Summary of sensitivities and specificities
Sign Sensitivity Specificity
RV Dilatation 80% 80%
McConnell
D-Sign 22% 26% 64% 97% 95% 61% Pre-set: Cardiac Patient position: Supine position with left arm over the head; left lateral decubitus may help bring the heart closer to the chest wall in order to achieve a better apical four-chamber (AP4C) view. Technique: If the display marker is on the left, the probe marker will point to the left hip for the parasternal long axis view (PSLAX), the right hip for the parasternal short axis view (PSSAX), and the right flank for the sub-xiphoid (SX) and AP4C.
B. Lung
Probe: Curvilinear probe or Linear probe Pre-set: Thoracic (Lung) Patient position: Sitting upright or lying supine with elevated torso. Technique: The probe is placed perpendicular to the ribs in order to acquire a view of the pleural space between two rib shadows. The 12-view examination is performed bilaterally at the anterior thorax mid-clavicular line, lateral thorax at the mid-axillary line, and posterior thorax, with a close inspection of the costophrenic angles for pleural effusion.
C. Lower Extremity Veins
Probe: Linear probe Pre-set: DVT Patient position: Reverse Trendelenburg with external hip rotation and approximately 30 Technique: Compression is applied at the common femoral vein (sapheno-femoral junction), the superficial femoral vein, and the popliteal vein. Lack of compression (with pressure sufficient to cause tenting of the artery) is indicative of thrombosis.
POCUS SIGNS A. Cardiac
Based on a meta-analysis published by Fields et al. in 2017, undefined right heart strain is a common ultrasound finding in PE with a sensitivity of 53% (95% CI, 45%-61%) and a specificity of 83% (95% CI, 74%-90%). Multiple other ultrasonographic signs, including ventricle size ratio, paradoxical septal motion, tricuspid regurgitation, 60/60 sign, McConnell’s sign, right heart thrombus, right ventricle (RV) hypokinesis, pulmonary hypertension, RV end-diastolic diameter, tricuspid annular plane systolic excursion, RV systolic pressure, and early systolic notching, have been identified. Due to variable specificities and sensitivities (Fig. 1), no single sign is sufficient to exclude PE. Although, degrees of knee flexion.
the most specific sign. The following six signs (three related to size and three related to function) are simple to perform and suggest acute right heart strain.
Size: (1) RV dilatation, (2) McConnell’s sign, and (3) D-Sign Function: (4) TAPSE, (5) S’, and (6) FAC
1. Right Ventricular Dilatation
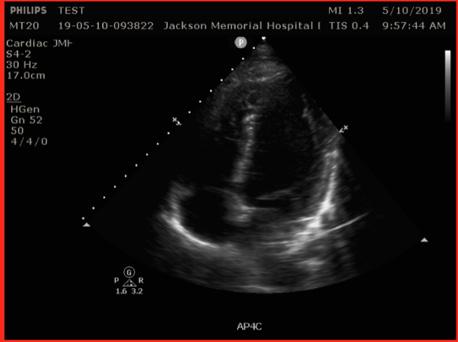
Significance: RV dilatation is suggestive of acute RV strain. Technique: RV end diastolic diameter should be measured at the midlevel in the AP4C view. A diameter greater than 35mm is suggestive of RV dilatation. Alternatively, obtaining a ratio of RV to LV enddiastolic diameter greater than 0.6 is considered abnormal.
2. McConnell’s Sign
Significance: McConnell et al. compared RV dysfunction in patients with acute PE with patients with chronic pulmonary hypertension, and found that the cardiac echocardiogram in patients with acute RV strain had an akinetic RV free wall while the apex had normal contractions. McConnell’s sign is 94% sensitive for acute right heart strain. In subsequent studies, this sign has been found in patients with acute RV infarct and 17% of chronic pulmonary hypertension,
1

2
and thus is far from definitive proof of PE. Technique: McConnell’s sign is visualized best in the AP4C view.
3. Paradoxical Septal Motion (D-sign)
Significance: Septal wall flattening or deviation toward the left ventricle (LV) is another marker of RV dysfunction that can clue us into identifying the presence of right heart strain. D-sign is suggestive of elevated RV pressure. Technique: Paradoxical septal motion is assessed in the PSSAX view. Abnormal septal motion is characterized by flattening of the septum and deviation towards the LV during diastole.
3

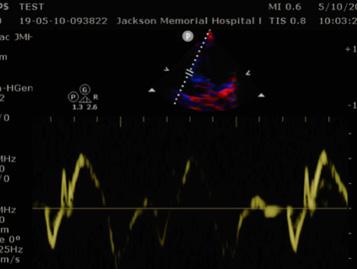
4. Tricuspid Annular Plane Systolic Excursion (TAPSE) (Fig. 2)
Significance: RV function has been shown to correlate with the RV free wall excursion, or TAPSE. Preliminary studies also suggest that the use of TAPSE in tachycardic and hypotensive patients increases the sensitivity for identifying acute PE. A normal value is >20 mm, and excursion of less than 16mm is considered abnormal, and suggestive of RV systolic dysfunction and, consequently, RV strain. Technique: The goal is to measure the movement of the tricuspid annulus from the end of diastole to the end of systole using M-mode. Step 1: Obtain the A4C view. Step 2: Place the M-mode marker through the lateral tricuspid annulus. Step 3: Measure the distance from the peak to the valley.
POCUS-PE.to.go
• Cut along the dotted border of the table below, fold along the bold line and stick in your wallet to reference onthe-go. Courtesy of authors Leila PoSaw, MD and Andrea Alvarado, MD, PGY-2
POCUSPE
Cardiac probe
Curvilinear probe
Linear probe Is there RV dilatation?
POCUS -PE

Figure on PPT Is there a D-sign? Is the TAPSE < 17 mm? Is there a McConnell’s sign? Are there A-lines?
Are there sub-pleural consolidations? Is there a DVT?
Figure on PPT

Figure on PPT

Figure on PPT Figure on PPT
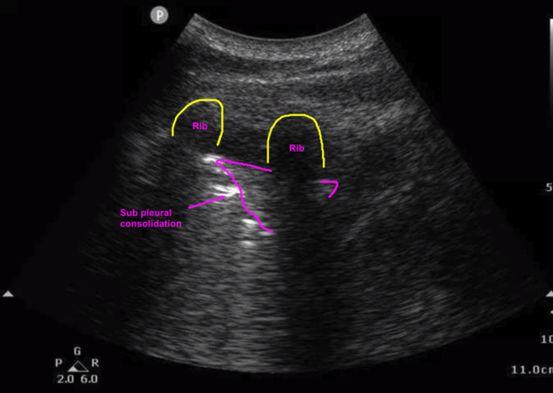

Figure on PPT
1

2
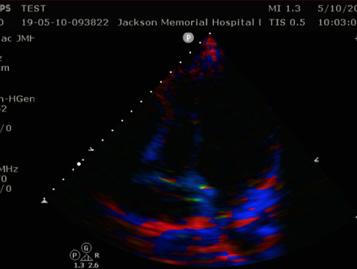
5. Systolic Excursion Velocity (S’) (Fig. 3)
Significance: The S’ is a measure of RV systolic function, and a velocity less than 10 cm/s is suggestive of depressed RV function. Technique: Step 1: Obtain the A4C view. Step 2: Turn on the TDI mode. Step 3: Place the PW Doppler on the lateral free wall near the tricuspid annulus. Step 4: Measure the velocity of the S’ wave.
6. Fractional Area Change (FAC) (Fig. 4)
Significance: FAC is another measure of RV systolic function. Values greater than 32% of change are indicative of normal RV systolic function. FAC <30% is mild, <24% is moderate and <17% is severe depression of the RV systolic function. Technique: This is performed in the A4C view by tracing the RV cavity to calculate the area at the end of diastole and at the end of systole. FAC is a function of the change in area divided by the end-diastolic area.
B. Lung (Fig 5)
The thoracic ultrasound is not the single best imaging modality especially if used alone. However, if abnormal or when used in conjunction with the cardiac or lower extremity (LE) venous ultrasound, the lung ultrasound may be extremely helpful. The association of a normal (A-profile) lung POCUS with a positive LE venous scan has been shown to favor the diagnosis of PE. Recently, several lung abnormalities have been described for PE, including the (1) presence of multiple lesions, (2) rounded, polygonal or wedge shaped lesions, (3)
3

4
Fig. 4 FAC. Courtesy of Brittney Giuffre, MD
1

2
(DA - SA)/DA %

Fig. 5: Normal lung and sub-pleural consolidation
Normal lung


Sub-pleural consolidation
associated pleural effusions, (4) right lung affectation more than left, (5) and posterior lower lung findings. In patients presenting with dyspnea, thoracic ultrasound can help rule out other etiologies of respiratory distress such as pneumonia, pulmonary edema, pneumothorax, or COPD/asthma.
Sub-pleural consolidations Thoracic ultrasound seeks to evaluate the pleural line for subpleural consolidations that may be representative of pulmonary infarction. The majority of findings occur in the posterior and inferior areas of the lung. Some studies suggest that pleural lesions between 0.5cm to 3cm are more indicative of PE.
C. Lower Extremity Veins
In patients undergoing clinical evaluation for PE, a LE ultrasound with positive findings for deep venous thrombosis increases the pre-test probability of the patient having a PE.
In the right clinical context, POCUS has the power to quickly raise or lower clinical suspicion for PE. It is important to keep in mind that POCUS is a rule-in test for PE. While the specificities of these exam findings are high and help us rule in the diagnosis, these findings have poor sensitivities and cannot be used to rule out the










