
22 minute read
HEALTH & FITNESS
HEALTH
& FITNESS
– Everything you need to keep fit, healthy, and happy –
Sleep Better this Summer with Pillowsprays

As the weather warms up, sleep quality often suffers. Broken sleep isn’t inevitable however and a new range of pillow sprays is helping to tackle those sleepless nights. The creator of the brand, who has a background in Sleep Psychology, shares his tips.
Not Just Lavender
The range of natural sleep aids, available from www.pillowsprays.co.uk includes both Lavender and Non-Lavender scents which means there really is something for everyone. The beautiful, floral scents include; • Bergamot and Frankincense • Lavender and Mandarin • Sweet Orange, Ylang Ylang, Patchouli and Lime • Neroli, Rose Geranium and Frankincense • Lavender and Rose Geranium Simply spray a fine mist over your bedding and/or pillow a few minutes before you’re ready to sleep, breathe in and prepare for a deep sleep.
Sleep Psychology meets Aromatherapy
Pillow Sprays is a coming together of two strands of study; Psychology and Aromatherapy. The company was started by Steven Crumblehulme who is based in the Cotswolds.
Steven received a Masters in Cognitive Therapies and Sleep Psychology and, after a period working as a Psychology teacher, now runs a successful Reflexology practice.
Over several years Steven has used his knowledge of Psychology and Aromatherapy to help many of his existing clients. With a belief that a sound sleep is the foundation of a healthy body and mind, Pillow Sprays was set up to bring high quality natural sleep aids to the market.
pillowsprays.co.uk
Sleep Tips to help you Sleep Better in Summer


• Aim for your bedroom to be approximately 18°C. Too warm and you’ll struggle to fall asleep, too cold and you’ll likely wake around 5am when body temperatures are at their lowest. Avoid eating too late as this will raise your body temperature as you digest food. • Get plenty of morning daylight. Outdoor light - even on a cloudy day - is many times brighter than artificial light. This brighter light increases alertness and resets our Circadian Rhythms (our sleep/wake cycles). • Avoid caffeine after midday. The ‘half-life’ of caffeine in adults is about 5-6 hours. By drinking caffeine after midday you risk disrupting your sleep pattern and your sleep quality. • Limit device use before bed. Many studies suggest that blue light in the evening disrupts your brain’s natural sleep-wake cycles, which are crucial for optimal health. • Find a relaxing night-time routine. Whether it is reading or listening to soft music, keeping a routine before bed tells your brain that it is time for sleep. This repetition is a form of ‘Classical Conditioning’ or ‘learning through association’. • Deep breathing before bedtime. The rest and digest system is another name for the Parasympathetic nervous system, which is associated with repair, relaxation and rest. The opposite is the Sympathetic system, which is our ‘fight or flight’ response. By deep breathing before bed, and focussing on your breathing, you help kickstart your ‘rest and digest’ system and sleep better. • Write down your worries. Keep a notepad to record your worries, or simply use it to record the key tasks you need to accomplish in the coming days. By commiting these thoughts to paper you externalise them. This is turn leaves you less prone to lay awake pondering on them if you wake in the night.



THE KENSINGTON WING

The Kensington Wing is the dedicated private maternity unit at Chelsea and Westminster Hospital, providing women with around-the-clock clinical care, comfortable en-suite private rooms and hospitality services.
Being located in the heart of Chelsea and Westminster Hospital - one of the UK’s safest hospitals - the safety and wellbeing of mother and baby are reassuringly supported at all times. The Kensington Wing is immediately located next to the hospital’s outstanding and newly expanded Neonatal Intensive Care Unit (NICU) and a consultant anaesthetist remains on site at all times, 24/7, dedicated to the needs of women on the Kensington Wing.
In these uncertain times, expectant parents can have additional anxieties or concerns about childbirth or going into a hospital. To ensure the safety of women and their birth partners, The Kensington Wing have important infection control procedures for staff and visitors to adhere to, but remain welcoming to your chosen birth partner for all stages of your pregnancy, birth and postnatal stay. Your individual room and en-suite facilities are a haven in these times and the catering and hospitality team ensures your stay is relaxing as well as safe.
On the Kensington Wing the consultant obstetricians, midwives, nurses and maternity support workers provide care as a team. And are delighted to offer both consultant-led and midwife-led maternity packages.
The Kensington Wing’s highly experienced team of midwives welcome enquiries from prospective women and the opportunity to discuss midwifeled care in more detail. These ‘meet the midwife’ sessions are always a relaxed and special time to talk and discover more without any obligation. For those women who are appropriate for midwife-led care, the team provide full support throughout your pregnancy and the midwifery team are available 24 hours seven days a week for advice or concerns throughout your pregnancy, birth and postnatal stay.
The consultant-led care package allows you the choice of one of our experienced consultant obstetricians to personally guide you through your pregnancy and birth. Your consultant provides continuity and individualised expertise throughout your journey. They build a relationship with you and your partner through the antenatal period to give you confidence to birth safely with them in line with your birth preferences. They remain to support you through the postnatal period including your 6 week postnatal check. All consultants are available to meet you and your birth partner without any obligation.
The Kensington Wing enquiry team are always happy to support with these arrangements and answer any questions.
If you would like to talk to one of the team email kensington@chelwest.nhs.uk or visit our website thekensingtonwing.co.uk

Physiotherapy and Breast Cancer

1 in 7 women in the UK will develop breast cancer during their lifetime and around 150 people are diagnosed every day in the UK. However, studies suggest that if you make changes to your lifestyle, your risk of getting breast cancer could be reduced.
Breast cancer is the abnormal growth of the cells lining the breast lobules or ducts. These abnormal cells divide in an uncontrolled way and may eventually spread into other tissues. Though breast cancer can affect both men and women, it is uncommon in men. Your risk of getting cancer is determined by many factors. 4 in 10 cancers in the UK are potentially preventable. Cancer Research has a quiz on its website to measure your risk and find out how to reduce it. (cancerresearchuk.org/ about-cancer/causes-of-cancer/cancer-risk-healthquiz )
The treatment you need depends on the type of breast cancer you have, as well as your general health. Treatments may include surgery, chemotherapy, radiotherapy and hormone therapy. When diagnosed at its earliest stage, 98% of people with breast cancer will survive the disease for five years or more, compared with 26% of people when diagnosed at the latest stage. Breast screening in the UK is available for women between the ages of 50 and 70. Regardless of your age, it is important to check your breasts monthly. If you notice any unusual changes or feel something is not right, it is important to seek medical help. Breast Cancer UK hosts a video on how to check your breasts properly. (vimeo. com/461308095)
Following surgery and treatment for breast cancer, you may encounter a few complications which can be alleviated with specialist physiotherapy. Therapy may include joint mobilisations, myofascial release, massage, stretches and mobility exercises, pilates and a functional rehabilitation program to get you back to your normal daily activities and sports.
A specialist oncology physiotherapist, such as there is at RRMG, can assist you with the following post-operative complications: • Cording • Scar Tissue • Joint and muscular pain and stiffness • General deconditioning • Rehabilitation following reconstructive surgery About the Author Fara Sonday is a specialist oncology, pelvic health and musculoskeletal physiotherapist at RRMG.
rrmg.com



The Harley Street ENT Clinic

The Harley Street ENT Clinic is UK’s foremost private medical centre dedicated to providing high quality care for all ear, nose, throat, head & neck and balance related disorders. It was set up in 2004 by leading ENT surgeons Dr Gerald Brookes and his partner Dr Natalie Brookes, to create a onestop ENT Clinic.
Over the years, the clinic has developed inhouse, a state-of-the-art diagnostic laboratory capable of carrying out comprehensive and specialised hearing, balance, facial, voice, laryngeal, nasal, olfactory, airway, allergy and sleep investigations, endoscopy, and vestibular tests.
An experienced team of ENT specialists can diagnose and treat all kinds of ear, nose and throat problems as well as balance and sleep disorders. Whether you need an ear specialist to help with your child’s recurring infections or a nose specialist who can tackle your snoring, The Harley Street ENT Clinic can help. The Harley Hearing Centre within the ENT clinic is the place to get help with your hearing aids.
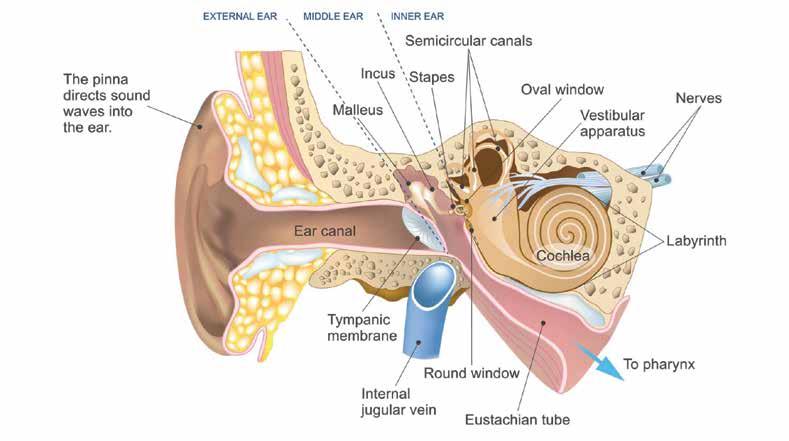
Ear Blockage
Ear blockage can be due to conditions of the outer, middle or inner ears. Obstructions in the external canal can be caused by impacted wax or swelling of the skin lining due to infection (otitis externa). Middle ear infections (otitis media) with fluid (effusion) cause blockage and hearing loss.
Eustachian tube blockage (dysfunction)



commonly occurs with an upper respiratory tract infection or sudden changes of the environmental pressure, such as landing in an aeroplane or scuba diving. Stress related jaw spasms (Temporomandibular joint -TMJ dysfunction) can also result in tension of the Eustachian Tube muscles. Conditions with an increase in the inner ear fluid pressure, such as Meniere’s disease and acoustic neuroma, cause ear blockage which may resemble the features of Eustachian tube dysfunction. Conditions with an increase in the inner ear fluid pressure (endolymphatic hydrops), such as Meniere’s disease and acoustic neuroma, cause ear blockage which may closely resemble the clinical features of Eustachian tube dysfunction. Sometimes, patients complain of ear blockage when they mean that they cannot hear properly. be able to assess, diagnose and treat the causes of your ear blockage.
The Harley Street ENT Clinic medical team includes some of the most well-respected consultants and therapists, highly qualified audiologists and scientists and caring ENT practice nurses, co-ordinated by a very experienced Clinical Services Manager. They are supported by a fully trained and extremely capable administrative team, supervised by an exceptionally knowledgeable Head of Operations and guided by a very strong Board of Directors.
During a 2019 Care Quality Commission inspection the Harley Street ENT Clinic received an overall rating of GOOD with exceptional feedback on the services provided and the standard of care they provide to patients.
Diagnostics
Because of the wide spectrum of possible causes, an extensive range of audiological investigations may be necessary to make an accurate diagnosis.
Thorough clinical examination can often, but not always, identify the problem. Basic audiological tests, such as Pure tone audiometry, Tympanometry and Stapedial reflexes, can usually indicate the source of the symptom. However, more detailed audiological investigations, such as Eustachian tube function testing, Otoacoustic emissions or Electrocochleography may be necessary to make an accurate diagnosis. At the Harley Street ENT Clinic our experienced ENT Consultants and Audio-Vestibular Scientists will THE DETAILS
Open Monday to Friday 8.30am - 6.00pm for face to face and video consultations.
The Clinic has remained open throughout the Covid-19 pandemic with patient safety their primary concern - a secure environment, following a very strict Infection Control protocol for the safety of patients and staff including rigorous antiseptic cleaning, social distancing and Personal Protective Equipment.
109 Harley Street, W1G 6AN
Telephone number: 0207 224 2350
Email: info@harleystreetent.com
Website: harleystreetent.com
Linkedin: The Harley Street Ent Clinic
Twitter: @HarleySt_Ent


THE AESTHETICS CENTRE
Do you have the post-COVID blues? Was that video call image the real you?
Zoom Dysmorphia’ or Zoom Face is a growing phenomenon and not many of us feel confident or good about our appearance over the last year of lockdown. This may become all too apparent as we appear much more frequently on the computer screens of family, friends and work associates all over the world. Our faces are magnified and scrutinised in more detail than ever before.
For most of us it is important to look good and above all feel good about ourselves. Might it be time to restore, rejuvenate and reverse the biological clock? Why not press the pause button and feel younger at The Aesthetics Centre, Harley Street. Looking fresh and radiant has never been safer or more comfortable than in the expert hands of Dr Max Malik, our internationally renowned leading Aesthetics Specialist Doctor.
Dr Max Malik MB ChB, PG Derm, MBCAM, MRCPsych. is an Aesthetics Doctor, Aesthetic Dermatologist and a Hair Restoration Surgeon. In addition, he is a trainer and teacher of other doctors in this field and a Key Opinion Leader for some of the top international companies in Aesthetic Medicine. Bespoke procedure combinations are expertly planned and performed.
As well as non-surgical facelift procedures, Dr Max also uses many other treatment modalities, such as lasers, PRP (Platelet Rich Plasma), Soft Surgery, supplemented by other types of aesthetic treatments, including topical prescription systems to enhance the facial structure, symmetry and balance, whilst always providing natural results
The improved skin quality makes the face look younger, fresher and glowing. All areas of the face and neck, including body areas, can be treated as appropriate, with various highly advanced techniques, using state of the art equipment and products under highly effective local anaesthetic. There is no ‘surgical cutting’ involved at all.
So why not call and Dr Max’s team will be happy to help you onwards on your rejuvenation journey. A no-obligation initial consultation, by remote video link or face to face, is a great first step, to discuss and demonstrate what is possible and what may be helpful. Currently, a range of introductory packages are available. THE DETAILS
For more details visit harleystreetent.com/About-Us/ Team/Dr-Max-Malik or call 020 3909 8729 The Aesthetics Centre, 109 Harley Street, W1G 6AN info@aestheticscentreharleyst.com
Your questions about bowel cancer, answered
Bowel cancer is one of the most commonly diagnosed cancers in the UK. Treatment can be faster, safer and more precise if you’re diagnosed early. This Bowel Cancer Awareness Month, we asked the team at King Edward VII’s Hospital’s Colorectal Robotics Service to answer some common questions you may have about bowel cancer.
Mr Alex von Roon Mr Charles Evans Mr Danilo Miskovic Mr James Kinross



What are the signs of bowel cancer?
Danilo Miskovic: The most common symptoms of bowel cancer are a change in bowel habits (such as going to the toilet more often), bleeding from the bottom and pain or bloating brought on by eating.
These symptoms are often caused by other factors, so most people with these symptoms won’t have bowel cancer, but it’s useful to keep an eye on them and see if they resolve on their own.
If your symptoms last longer than three weeks, make an appointment with your doctor.
What are some less common symptoms?
Alex von Roon: Some people with bowel cancer may notice that they feel extremely tired for no obvious reason, or are losing weight without trying, though this is less common.
Some people may also have pain or a lump in their stomach or back passage - this could be a sign to see your GP.
What other conditions can also cause these symptoms?
James Kinross: Bowel cancer symptoms can be caused by a range of other conditions. These include haemorrhoids, sometimes known as piles, which are lumps inside and around your bottom that can also cause bleeding when you go to the toilet.
A change in bowel habits is often caused by something you’ve eaten, or you may have a gastrointestinal issue such as irritable bowel syndrome, ulcerative colitis or diverticulitis.
Although your symptoms will often be caused by something other than bowel cancer it is still important to seek medical advice if you’re worried.
What are the risk factors for bowel cancer?
Charles Evans: Having a close family member who has been diagnosed with bowel cancer can increase your risk of developing it yourself. Other cancers can sometimes be linked to your risk of developing bowel cancer - such as if you or a close family member has had ovarian, womb, stomach or pancreatic cancer - but not in every case.
If you’re concerned about your family history and being at higher risk of developing cancer, it’s a good idea to speak to your GP, who might refer you for further testing.

The other risk factors for bowel cancer include age (it is most common in people over the age of 50), a diet that’s high in red or processed meat, smoking, drinking alcohol (particularly to excess), and being obese (especially in men).
How can I lower my risk?
DM: There are lots of things you can do to help lower your risk of developing bowel cancer. Eating healthily and losing weight if you’re overweight can help, and there’s some evidence that a diet high in fibre could also help.
Cutting down on smoking and drinking alcohol will help reduce the risk of bowel cancer as well as several other cancers.
And getting enough exercise is a good idea for your general health, but it can also help lower your risk of developing bowel cancer. It’s recommended that most people aim for at least 150 minutes of moderate exercise per week, or 75 minutes of vigorous exercise.
How do you test for bowel cancer?
AvR: Usually your GP will carry out an examination of your bottom and your abdomen to see if they can feel any lumps, and you may have a blood test to test for anaemia.
If you need to be referred on for more tests,


you might have a flexible sigmoidoscopy or colonoscopy, which are procedures that use a tube with a light and camera at the end to examine your bowel. These procedures are carried out in a hospital.
For people aged 60 to 74, the NHS offers a particular type of bowel cancer screening test called a faecal occult blood (FOB) test, every two years.
King Edward VII’s Hospital also offers FIT testing, a newer, more advanced type of screening for bowel cancer that can be carried out at home.
How is bowel cancer treated?
JK: Treatment for bowel cancer may include chemotherapy, radiotherapy or surgery (often keyhole surgery). Using robotic surgery can improve surgical precision and limit surgical trauma. It is very safe and can ultimately lead to a faster recovery, less time in hospital and reduce the risk of complications after surgery. Hospital are training more and more surgeons to carry out surgery in this way. And advancements in imaging will help us to pinpoint the exact location of the cancer, so we can be even more precise with the surgery.
Ideally, we will also get to a point where we are diagnosing bowel cancer earlier, so in many cases surgery will not be needed.
To help diagnose cancer earlier, it’s really important to be aware of what’s normal for you, and to seek help if you’re worried.
Is it still possible to get medical help during lockdown?
DM: If you have symptoms that you’re worried about, it’s important to still seek help. Lots of doctors are now conducting appointments over the phone or over video call, so it might be possible to reassure you without having to go to a GP surgery or hospital in person. If a physical examination is necessary, medical staff have taken every precaution to keep patients safe. There might be some new rules to follow when you attend your appointment, so make sure you read any letters or correspondence carefully.
What’s the future of treatment?
CE: I expect that in the future more and more procedures will be carried out by robot-assisted surgery, I and the team at King Edward VII’s
About the Colorectal Robotics Service
What’s your advice for people who might be embarrassed to seek help?
AvR: It’s perfectly natural to be embarrassed to go to the doctor, especially if your concern is about a more private area! However, there’s no reason to be embarrassed and medical staff will do everything to make you feel comfortable. If you suspect there may be a problem, I’d really urge you to seek medical help. It’s probably nothing and we’re always more than happy to rule something serious out. On the off chance it is a serious issue, the sooner we catch it, the better the treatment options will be. King Edward VII’s Hospital Colorectal Robotics Service is the UK’s premier clinic for robotic colorectal and general surgery.
The team are specialists in robotic gastrointestinal and general surgery and deliver ultra-precise, minimally invasive robotic surgeries for those with bowel cancer, using our Da Vinci XI robot.
Working at London teaching hospitals and operating busy NHS clinics, the collective experience and expertise of the team is unrivalled anywhere in the UK.
They have performed more than 500 major robotic procedures between them and are supported by highly skilled surgical and specialist nursing teams.
If you’re concerned about bowel cancer symptoms, call a member of our dedicated patient services team at King Edward Hospital to discuss your options: 020 7467 4344, Mon – Fri, 9am – 5pm.
kingedwardvii.co.uk


Prevention is better than cure
Tena Walters, Consultant Breast Surgeon MBBS, FRCS, MS
Astudy at the Royal Marsden Hospital in 1940 first suggested that breast cancer could run in families, but it wasn’t until 1994 that the first genetic abnormality, which caused breast cancer was identified.
Approximately 5% to 10% of the 4 million breast cancers diagnosed in the world, per year are due to genetic mutations. Approximately 1:400 people in the population carry the abnormal gene.
More than half of all women with breast cancer, who are found to have an abnormal gene do not have a family history of breast cancer, but currently only patients with breast cancer who are considered to have a greater than 10% risk of carrying one of the abnormal genes is offered testing. This is based on their age, type of cancer and family history.
Patients are offer testing if they have one of the following criteria:
• One first degree relative with breast cancer younger than 40 years of age • One first degree male relative at any age • One first degree relative with bilateral breast cancer, when the first was diagnosed younger than 50 years old • Two first degree relatives or one first degree and one second degree relative with breast cancer at any age
However, a recent study has suggested that it would be more cost effective to offer testing to all women with breast cancer, which would identify more gene carriers and their relatives, who would benefit from preventative therapy.
Testing patients with a family history only means that 50% of gene carriers are missed. This is because there may be a lack of awareness of the significance of family history by patients and clinicians leading to restricted access, and underuse of genetic testing services with only 20-30% of eligible patients tested. This means that 97% of carriers of an abnormal gene in the population remain unidentified.
If patients are known to have an abnormal gene then they may, like Angelina Jolie opt to have a risk reducing mastectomy with reconstruction. Patients who have breast cancer may opt to have a mastectomy instead of lump removal and a risk reducing mastectomy on the other side with breast reconstruction. This may also reduce the need for radiotherapy following lumpectomy. They may be also eligible for different, new preventative drugs. Most importantly, it is now possible to test embryos for the genetic mutation and this could prevent the gene from being passed on the future generations.
Identification of gene carrying relatives could allow those individuals to have selective and advanced screening techniques with MRI and tomo synthesis mammography or risk reducing surgery.
Prevention is better than cure and patients with breast cancer should discuss genetic testing with their clinicians.
For appointments please call 01622 873058. For more details call Tena’s PA Helen on 07982 249612.Or email tenakerrywalters@gmail.com


www.bearrene.com @bearrene






