12 minute read
Safety in sclerals – Part 2
Overnight orthokeratology
A trilogy on specialty contact lens safety – part 2
Advertisement
A pleonasm: The term ‘overnight orthokeratology’ (ortho-k) can be seen to a large degree as a pleonasm, derived from the ancient Greek word pleonasmós – pleon, or 'to be in excess' – which means a redundancy in linguistic expression. In this case, the ‘overnight’ would be the redundant part, as there is hardly a situation thinkable in which ortho-k lenses are worn during the daytime hours; there is not a need to reshape the cornea for a corrected corneal surface during the sleeping hours. Ortho-k lenses in some parts of the world are called ‘night-lenses’: that is, worn during the night for vision during the day. Originally started as a clever management term, it is now the leading nomenclature to describe ortho-k in a generic way in the Netherlands, for instance, and has even been adopted by professional organizations. The ‘overnight’ part of this modality though, carries most of the weight regarding ‘safety’ issues. So, let’s circle back to the title and assess the special circumstances surrounding this overnight modality. By Eef van der Worp
WITH CONFIDENCE
Back to basics regarding contact lens safety: according to a study by Stapleton et al,1 the incidence of a microbial keratitis (MK) with loss of visual acuity in daily wear with soft lenses (silicone hydrogels) is 0.00011%. This is more easily interpreted as a chance of 1.1 per 10,000 patient years. The 95% confidence interval (CI) with these lenses is between 0.9 and 1.4. What does this tell us? The interval of confidence basically suggests that if this study were to be repeated 100 times, then the outcome in 95% of the cases would be between these values (0.9 and 1.4 here). The smaller this range, the more certainty there is regarding the outcome numbers. Comparing the relative risk of MK (not per se leading to vision loss) by lens modality, the annualized incidence per 10,000 wearers was determined to be 1.2 (CI 1.1-1.5) for daily wear rigid corneal lenses; 1.9 (CI 1.8-2.0) for daily wear soft; 2.0 (CI 1.7-2.4) for daily disposable; 11.9 (CI 10.0-14.6) for silicone hydrogel soft; 19.5 (CI 14.6-29.5) for overnight wear soft; and 25.4 (CI 21.2-31.5) for overnight wear silicone hydrogel. No real data regarding overnight rigid lens wear is available. From this data, a couple of things become clear: corneal rigid lenses are the gold standard and are by far the safest contact lens modality out there. Period. The data further clearly shows

that daily wear is the safest lens wear modality, occasional overnight wear increases the risk, and regular overnight wear further increases that risk.
In ortho-k the lenses are only worn during the night, and the wearer is lens-free during the day. What are the risks, considering this? Bullimore et al (2013)2 reported a survey involving 1,317 patients (640 adults and 677 children) that resulted in 2,599 patient years of data (1,164 in adults, 1,435 in children). Fifty cases of painful red eye were reported, eight cases of corneal infiltrates, and two cases of microbial keratitis (MK). They reported an incidence, per 10,000 years of wear, of 7.7. The confidence interval here was 0.9 to 28. Note that the CI here is larger; hence, there is less certainty, or confidence, that the absolute number of 7.7 is correct, it is roughly somewhere between one and 30. The latter is most probably the preferred estimate to use toward patients, not the absolute 7.7 number. For children, the MK risk was found to be 13.9 per 10,000 patient-years, again with a large CI of 1.7 to 50.4, while for adults the estimated incidence was zero per 10,000 patient-years (with a CI of zero to 31.7).
In essence, there is a higher risk of MK with ortho-k, but it’s not from the lens or the material; ortho-k lenses are not substantially thicker (as is the case with scleral lenses, as described in the previous paper in this GlobalCONTACT trilogy) or made in any different materials (if anything, the Dk is higher in ortho-k lenses). It is the ‘overnight’ part that is different in ortho-k. MYOPIA MANAGEMENT
Ophthalmologists are advising against using this modality in children for myopia control in some parts of the world, for instance in the Netherlands – hence putting an important pillar in myopia management partly ‘off-side’, in football terms, for eye care practitioners. There are a few complicating factors when discussing this topic. The first problem is that large sample sizes are needed to be able to present confirmatory results on the risk of infection. If the incidence of a corneal infection is one in 100,000, then information from hundreds of thousands of lens wearers, ideally under controlled conditions, is needed. This is problematic for specialty lens modalities, including for ortho-k. Chance plays an important role in any numbers that are generated if sample size numbers are smaller.
Another paper by Bullimore et al reported on a retrospective study of the safety of ortho-k.3 All episodes of infiltrative keratitis from a children's hospital in Moscow were recorded and adjudicated by three ophthalmologists, which resulted in 139 cases of infiltrative keratitis in children, of which 45 were MK (32%). Five of them were overnight ortho-k wearers. The annual incidence thus reported was about 5.0 (CI, 2.1 to 12.4). One of the findings of the Bullimore studies is that the group with the biggest risk of MK was not the younger age group (8- 12-year-olds) but rather the 13- to17-year-olds, and the highest risk was in the 18- to 25-year-old group.
It appears, according to experts in the field – although anecdotally and not evidence based – that practices that fit the most ortho-k take the care that the modality requires very seriously. Informed consents are obtained, for parents and for the children, and hygiene and compliance protocols are reconfirmed on all follow-up visits, and it is made very clear to exclude any tap water from the care regimen. Practices that ‘do ortho-k on the side’ may be less ‘on-top-of-things’ and may not always have the same rigor in their protocols and regulations follow up. In some of the larger ortho-k practices, for instance, patients are told that if they do not return for follow-up care, they are excluded from further lens purchases and eye care in order to show the seriousness of eye and lens assessment. Here is an important task, for the industry and profession, to work on together.
BALANCING THINGS OUT
To summarize, the risk with overnight ortho-k is increased compared to with daily wear of contact lenses, and certainly if compared to daily rigid corneal lens wear – but the risk does not seem to exceed that of extended wear of soft lenses. Early detection and referral are key, as only a small portion of MK cases actually lead to permanent vision loss when managed in an adequate way.
The fact that ortho-k lenses are not worn during the day may be a plus in theory. In addition, intact immune systems result in normal healthy eyes (as opposed to in patients who require regular scleral lens or bandage soft lens wear, for instance). Corneas of ortho-k wearers have been reported to show small amounts of corneal staining, which may or may not pose a minor increased risk for corneal infection, although in rigid corneal lens wear – which has the lowest rates of corneal infection – corneal staining (especially three- and nine o’clock staining) is not uncommon either.4 In conclusion, the overnight part of the modality poses the biggest risks, it seems.
The unavoidable overnight component of ortho-k and the associated higher risk of an MK need to be balanced against the benefits that ortho-k can provide in terms of myopia progression reduction. Work by Gifford et al 5 showed that this balance can be favorable for lens wear if myopic retinal pathology is considered, and a recent paper by Bullimore et al also reported the potential benefits of myopia control to outweigh the risks.6 High-Dk materials are needed for ortho-k; without them, no safe ortho-k lens wear is possible. But apart from that, it seems that the biggest risk factors regarding safety are lens care and hygiene, for which the eye care practitioner together with the patient could play a crucial role. A notable consideration is that when an ortho-k lens is placed on the eye, whatever is ‘trapped’ behind the lens stays behind the lens. There is arguably almost no tear film exchange in ortho-k after the lens is placed on the eye, and the eyelid is closed – so removal of debris and of potential micro-organisms will not take place. This puts lens hygiene, especially upon lens application, on a higher rung of
the ladder of importance than in other lens modalities. This is a very important task, for the industry and the ECP alike, to focus on in the interest of both ocular health and the future of the modality.
In the next ‘episode’ of this trilogy on specialty lens safety, soft specialty lens wear will be placed under the magnifying glass. What are the special considerations for that modality? Stay tuned. Stay safe. n
Parts of this publication appeared in a Contact Lens Spectrum article (April 2022) that summarized a 2022 Global Specialty Lens Symposium session devoted to contact lens safety featuring Mark Bullimore, Melissa Barnett, Gloria Chiu and Pauline Cho.
References
[1] Stapleton F, Keay L, Edwards K, Naduvilath T, Dart JK, Brian G, Holden
BA. The incidence of contact lens-related MK in Australia. Ophthalmology. 2008 Oct;115(10):1655-62. doi: 10.1016/j.ophtha.2008.04.002. Epub 2008 Jun 5. PMID: 18538404. [2] Bullimore MA, Sinnott LT, Jones-Jordan LA. The risk of MK with overnight corneal reshaping lenses. Optom Vis Sci. 2013 Sep;90(9):937-44. doi: 10.1097/OPX.0b013e31829cac92. PMID: 23892491. [3] Bullimore MA, Mirsayafov DS, Khurai AR, Kononov LB, Asatrian SP,
Shmakov AN, Richdale K, Gorev VV. Pediatric Microbial Keratitis With
Overnight Ortho-k in Russia. Eye Contact Lens. 2021 Jul 1;47(7):420-425. [4] van der Worp E, De Brabander J, Swarbrick H, Nuijts R, Hendrikse F.
Corneal desiccation in rigid contact lens wear: 3- and 9-o'clock staining.
Optom Vis Sci. 2003 Apr;80(4):280-90. doi: 10.1097/00006324200304000-00005. PMID: 12692484. [5] Gifford KL. Childhood and lifetime risk comparison of myopia control with contact lenses. Cont Lens Anterior Eye. 2020 Feb;43(1):26-32. doi: 10.1016/j.clae.2019.11.007. Epub 2019 Nov 30. PMID: 31796370. [6] Bullimore MA, Ritchey ER, Shah S, Leveziel N, Bourne RRA, Flitcroft DI.
The Risks and Benefits of Myopia Control. Ophthalmology. 2021
Nov;128(11):1561-1579. doi: 10.1016/j.ophtha.2021.04.032. Epub 2021 May 4. PMID: 33961969.
Eef van der Worp, BOptom, PhD, FAAO, FIACLE, FBCLA, FSLS is an educator and researcher. He received his optometry degree from the Hogeschool van Utrecht in the Netherlands (NL) and has served as a head of the contact lens department at the school for over eight years. He received his PhD from the University of Maastricht (NL) in 2008. He is a fellow of the AAO, IACLE, BCLA and the SLS. He is currently adjunct Professor at the University of Montreal University College of Optometry (CA) and adjunct assistant Professor at Pacific University College of Optometry (Oregon, USA). He lectures extensively worldwide and is a guest lecturer at a number of Universities in the US and Europe.
Blocking Without Compromise
When planning a new manufacturing facility or optimizing an existing operation, it’s easy to focus on the lathe and neglect the role played by support processes such as material handling. While the lathe is arguably the single most important piece of equipment in a contact lens or IOL manufacturing laboratory, its precision can be easily undermined by underperforming equipment elsewhere in the process, most notably blocking. Today’s CNC lathes and lens design software combine to offer unprecedented options for meeting the needs of patients through precise control of lens geometry and sub-micron level surface accuracy, yet this can be easily undone by misaligned surfaces or unintended prism.
“If back and front [surfaces] are not perfectly aligned, you can get decentered optics, prism and poorly formed edges.”, says Manoel Carvalho, Director of Lab Operations and fitting consultant for BostonSight in Needham, Massachusetts. “All lenses need to have perfect optics. However, when dealing with multifocal or HOA correction, that becomes even more critical.”
DAC International has addressed these concerns by re-imaging the blocker from the ground up. The DAC Precision Blocker is a ‘no-compromise’ solution for RGP, Soft and IOL blocking that was developed to maximize the full potential of the DAC lathe’s edge contouring capability and form accuracy. Back or front surfaces are blocked with a high degree of accuracy and repeatability, and a minimum of time and operator attention.
The DAC Precision Blocker offers fast, reliable calibration, easy and intuitive initial setup, and stable, accurate and repeatable blocking. Additionally, the rigid, ½” steel construction and a design that manages ambient heat in the machine frame means that the DAC blocker holds calibration reliably over time, without the need to re-calibrate during the workday.
A blocker that holds calibration yields better lenses, but it also saves time and money. Greg Wicker, Maintenance Manager for X-Cel Specialty Contacts in Duluth, Georgia, has worked out the numbers: “Based on the average maintenance tech spending about 15 minutes setting a traditional blocker twice a day, [that’s] 30 minutes a day times 255 working days per year - 7,650 minutes total, or 127.5 hours per year”. Greg continues “Although more expensive than traditional blockers, I feel that it pays for itself with the reduction of prism related rejects and downtime for setting blockers.”
While accuracy and reliability are important, an ideal blocker also needs the versatility to handle the wide range of specialty products manufactured by a modern laboratory. Safe, consistent wax dosing, interchangeable waxpots and a fully programmable interface ensure that the DAC Precision Blocker has the flexibility to cover the full gamut of RGP, soft and IOL lenses currently in production.
Drop size is fully adjustable from zero to 2.5ml, and multiple drops can be programmed. Wax pots are hot-swappable with no down-time required to rapidly switch between waxes for different applications. Additionally, an on-board timer for wax pot warm-up lets lab managers start their morning without any waiting time; different start times may be set for each workday.
Finally, the DAC Precision Blocker is fully programable, with an LCD touch screen providing an intuitive interface that allows the user to optimize blocking variables to suit individual process needs. Key parameters such as drop count, temperature, and air-cooling controls can be accessed, configured and saved to any of six independently configurable blocking tables.
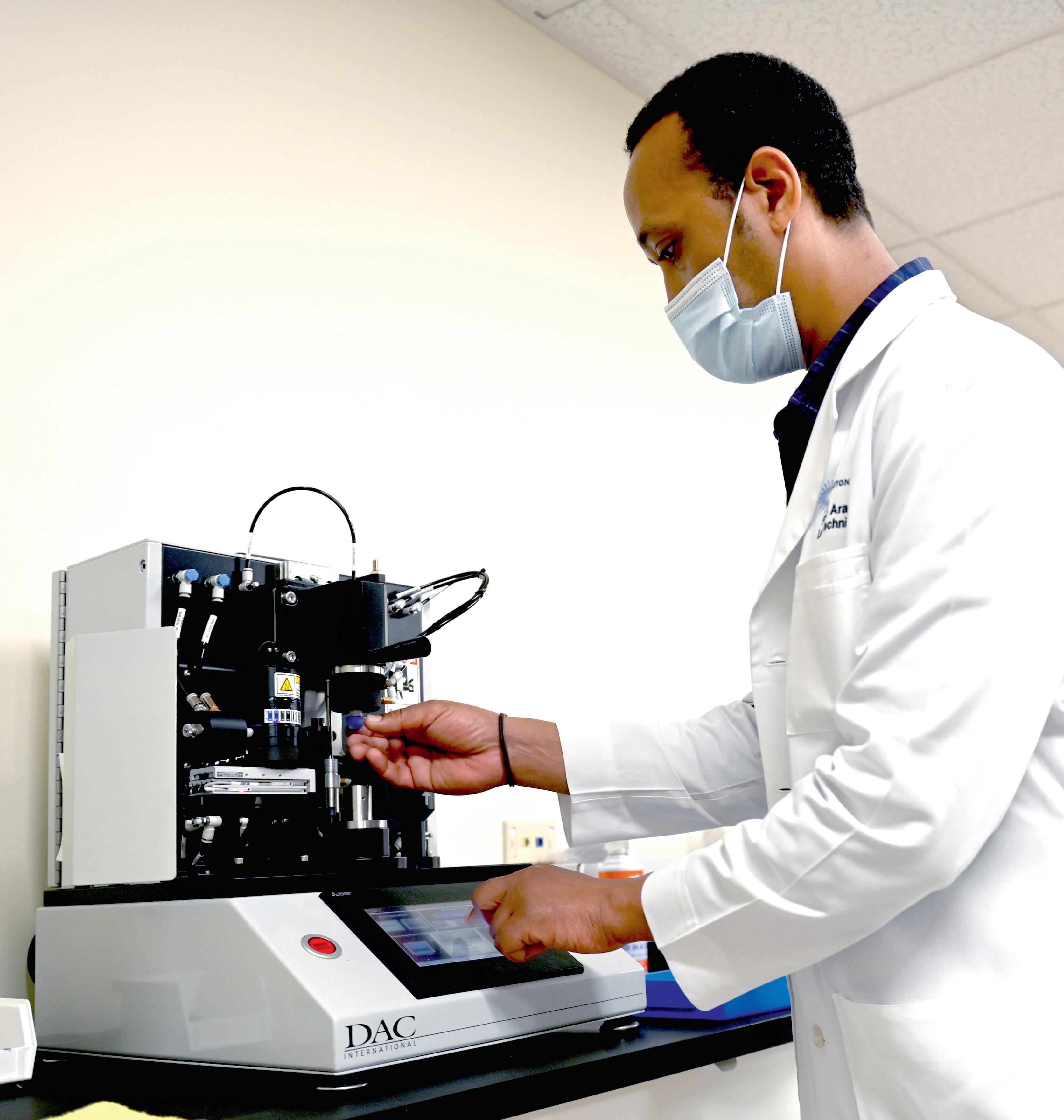
Pedro Araujo of BostonSight working with the DAC Precision Blocker
Treating blocking like the mission critical process that it is means looking seriously at the needs of a rapidly evolving industry and providing a robust and flexible solution that takes no shortcuts in design, materials or construction. To DAC International, this is the meaning of blocking without compromise. n