
9 minute read
Customizing myopia treatment
Photo: Silke Sage
Advertisement
Recently, the Global Specialty Lens Symposium (GSLS) was held online with a staggering 4000 delegates registered and with 83 countries represented – truly a ‘global’ symposium. I was put in charge of the myopia session, to be the myopia management moderator, so to speak. The panel was an exhibition of global excellence, with a constant flow around the globe, swinging back and forth from the east coast of Australia (Scott Read from the Queensland University of Technology in Brisbane and Kate Gifford of myopiaprofile.com) to the Netherlands (Jan Roelof Polling from Erasmus MC in Rotterdam) and North America (Langis Michaud, Université de Montréal in Canada). By Eef van der Worp
INSIDE THE BOX
It is no secret that myopia is increasing, quite drastically in fact, worldwide. But what may be new is that during the year 2020, and presumably because of home confinement during the COVID-19 pandemic, concerns have been raised about whether this home confinement may have worsened the burden of myopia owing to both decreased time spent outdoors and increased screen time at home. In short: our kids have been ‘living in a box,’ at least partly, during the last year. A study by Wang et al in JAMA Ophthalmology looked into this and found indeed that in the 123.535 children included in the study, a substantial myopic shift was seen (approximately −0.3D) in the school-based screenings in 2020 compared with previous years (2015-2019) for younger children aged 6 (−0.32 D), 7 (−0.28 D), and 8 (−0.29 D) years. Numerous limitations warrant caution in the interpretation of these associations, including use of non-cycloplegic refraction and lack of orthokeratology history or ocular biometry data. But the authors do conclude
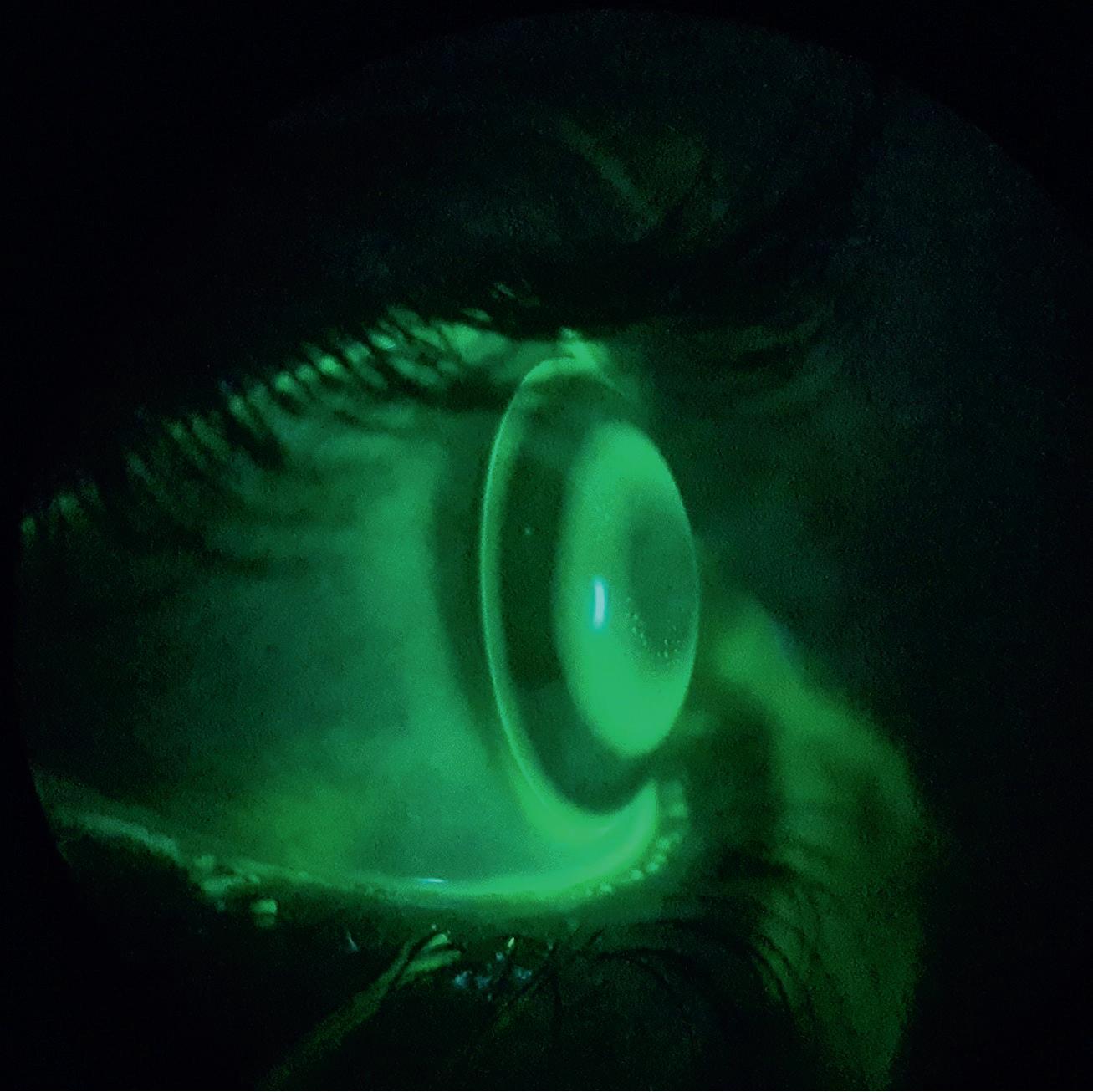
Fig.1: Orthokeratologie. Picture: Massimo Ferrara

that home confinement during the COVID-19 pandemic appears to be associated with a significant myopic shift for children aged 6 to 8 years. And that younger children’s refractive status may be more sensitive to environmental changes than that of older children, given that younger children are in a critical period for the development of myopia.
DON’T BE MEAN
With this in mind, and as a starting point, the panel at GSLS tried to analyse what is the best way in clinical practice to reduce myopia progression to the max, while staying on the safe and ethical side of things. The first appraisal made was a very important and critical one: don’t be mean! We hear all these stories about ‘50%’ or ‘60%’ reduction, also with new spectacle lenses now for myopia management. But what does this really mean? Work by Noel Brennan and Mark Bullimore, originally posted at ARVO 2019, has shown that these numbers are very relative in nature. First and foremost, it is important to realize that these are all average (or ‘mean’) numbers. ECPs can never present, promote or promise this in that way to patients and parents. Furthermore, even if these numbers of reduction are met, it is only the case within a relatively short period of time. Let’s say for convenience and to avoid complex discussion about that (hot) topic that the bulk of the treatment in myopic children needs to take place between the ages of 8 and 12 years. That is a pretty narrow window of opportunity.
What this also means is that we need to do everything we can to get as much treatment in during that limited time frame. Depending on the child and the situation, this could mean that we need to combine treatments if/where possible to get the most out of it in terms of efficiency. The session at GSLS showed that not only do we need to customize the treatment for each child, we also need to customize the intervention method – optical or not – to the max. ATROPINE
What this means for pharmaceutical intervention (basically atropine drops currently) is to look at the optimal concentration. Kate Giffford and Jan Roelof Polling shed some light on this. The latest research shows that higher concentrations of atropine seem to be the most effective (and less rebound effect after treatment is tapered), at the cost, of course, of more side effects including reduced accommodation, pupil size enlargement (hence photophobia), irritation and possibly headaches. And a low 0,01% concentration may unfortunately not meet the expectations we have of it.
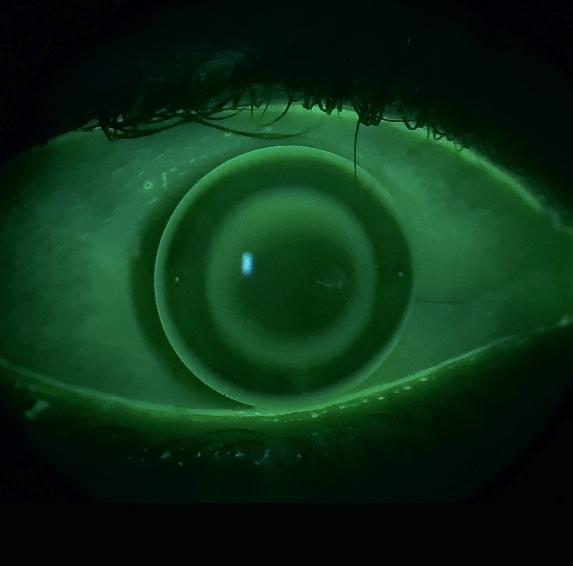
How effective a certain concentration of atropine is for a given child can be best monitored by following the axial length growth charts, almost like what we have for children’s height every time we visit the paediatrician (see figure 2). Basically, if the child is diverting from the designated path or line ‘upward,’ it is time to upgrade the atropine concentration; but if the kid is ‘lower’ than the designated line – then it is time to decrease atropine concentration and/or to add additional intervention methods such as optical intervention. This is a really nice way of following and monitoring myopia progression, with at least some kind of apparent control over the potential outcome.
OPTICAL INTERVENTION
In this category, our number one ‘champion’ is still orthokeratology, which has the longest track record and good evidence in the literature. However, here too, customization to optimize the outcome seems warranted. The myopia-reducing effect of orthokeratology was pretty much found by accident using standard orthokeratology lenses. We can most probably ‘upgrade’ the effectiveness of the modality by first looking at the optical zone treatment diameter on the cornea and the power profiles achieved. Langis Michaud and Kate Gifford explored ways of doing this. First, optical zone diameters should

Fig. 1: Axial length growth chart. Source: Erasmus MC, Rotterdam
not be too large to be effective; ideally, they should be limited and customized to roughly the pupil zone area. But the optical treatment zone shouldn’t be too small either: there is a small sweet spot between being too small and too large.
Furthermore, in essence orthokeratology converts peripheral hyperopia into relative peripheral myopia for low to average myopic eyes. The degree of relative peripheral myopia increases with the magnitude of central myopia that is corrected, Langis Michaud explained. Kate Gifford warned against not correcting low myopes with orthokeratology though, as there is not enough evidence to say that it would be less effective in low myopia.
What seemed relatively new to many delegates was the optics side of things and how important spherical aberrations and other higher-order aberration measurements are and their implementation in myopia management. The good thing is that it is all optics, which is (or should be) our core business. With respect to slowing myopia progression, the most important advantage of orthokeratology over either spectacles or soft contact lenses is that orthokeratology can induce very large optical effects in moderate to high myopes. But there is a need to customise orthokeratology fitting, according to Langis Michaud, to optimise the outcome. The optical profile and the treatment zone diameter can be altered, and back-toric lens design can be used to optimize the result.
A POSITIVE NOTE ON NEGATIVE LEVELS OF SPHERICAL ABERRATION
distances in the lens: a primary focal distance for far vision (i.e., the myopia correction) and a secondary plus power to slow eye growth (either a concentric design, aspheric design or Fresnel design). These designs aim to introduce positive/ myopic defocus to the retinal image. Optically, most lens designs tend to introduce increased levels of positive spherical aberration. This is pretty complex, however, and the amount of defocus induced will depend on a range of factors, including lens design, interactions with the eye’s natural optics, pupil size and accommodation and, lastly, lens (de-)centration.
Natural accommodation of the human eye alters the eye’s normal optics and introduces negative spherical aberration. This would reduce the amount of peripheral myopic defocus. Accommodation through the lens influences the myopic vs. hyperopic stimulus to human eye growth. This is where ‘Zernike polynomials’ come in, which describe complex aberrations of the eye. According to Scott Read, optimising soft contact lens designs for increased myopia control efficacy may be possible if these lenses are customized to the individual child. Langis Michaud took it ‘one step up’ from here by looking at choroidal thickness in the human retina in response to different optical profiles provided by soft lenses for myopia management. He coined the term ‘dose response’ in this regard: by varying the amount of peripheral ‘plus,’ the myopia reduction effect can be optimized. The newest BLINK study results show that with higher add power, typically a more significant rate of myopia progression reduction can be achieved. Studies at the Université de Montréal also show the same results as well as that the
treatment zone diameter can significantly influence the choroidal thickness (larger treatment zones result in reduced choroidal volume – which means longer eyes). They even found quadrant-specific differences in this regard, with a high inter-subject variability (threshold). This screams for customized designs to be developed.
CUSTOMISING TREATMENT
If this session made one thing clear, it is that we not only need to customise the treatment for myopia (chosing the right option in the right situation) but also that we will need to further customise the treatment (e.g. increase efficiency by looking at concentrations of atropine and/or optimize optical profiles). In other words: it starts with the children and their individual needs and circumstances. Within that frame, and within a narrow window of time, we need to carefully chose the myopia management method for the individual. And within each category, it seems like we’ll have to customize the treatment itself as well – in atropine concentration and in terms of aberrations corrected and applied. Especially within the optical intervention methods, there is a lot to gain in that regard within our industry.
References: [1] Brennan NA, Toubouti YM, Cheng X, Bullimore MA. Efficacy in myopia control. Prog Retin Eye Res. 2020 Nov 27:100923. [2] Tideman JWL, Polling JR, Vingerling JR, Jaddoe VWV, Williams
C, Guggenheim JA, Klaver CCW. Axial length growth and the risk of developing myopia in European children. Acta Ophthalmol. 2018 May;96(3):301-309. [3] Wang J, Li Y, Musch DC, Wei N, Qi X, Ding G, Li X, Li J, Song L,
Zhang Y, Ning Y, Zeng X, Hua N, Li S, Qian X. Progression of
Myopia in School-Aged Children After COVID-19 Home
Confinement. JAMA Ophthalmol. 2021 Jan 14: e206239.
Eef van der Worp, BOptom, PhD, FAAO, FIACLE, FBCLA, FSLS is an educator and researcher. He received his optometry degree from the Hogeschool van Utrecht in the Netherlands (NL) and has served as a head of the contact lens department at the school for over eight years. He received his PhD from the University of Maastricht (NL) in 2008. He is a fellow of the AAO, IACLE, BCLA and the SLS. He is currently adjunct Professor at the University of Montreal University College of Optometry (CA) and adjunct assistant Professor at Pacific University College of Optometry (Oregon, USA). He lectures extensively worldwide and is a guest lecturer at a number of Universities in the US and Europe.
Advertisement
Fast, reliable and objective measurement of contact lenses!
Refractive data
Power map with 0.040mm physical resolution
Multifunctional cuvette
Easy and fast loading of CL Temperature control to ±0.1 °C
High quality imaging system
Lens diameter, sag, haptic recognition Visualisation of defects
Made in Germany. Tel. +49 9131 69 15 00 email sales@optocraft.de











