3 minute read
Snakebite: A Neglected Disease of the Poor
Every year, up to 138,000 people die and a further 400,000 are permanently disabled because of snake envenoming. Whilst it’s easy to adopt a romanticised love of snakes from the comfortable position of a developed country with an effective healthcare system, those at risk of snakebite mortality must face a very different reality. Professor Mark O’Shea has been involved in snakebite research since the 1990s. Over that time, advancements in antivenom production have seen treatments become far more successful. Yet, there is still a majority population across the globe that cannot access these life-saving resources. Exotics Keeper Magazine caught up with Mark to discuss the problem.
Antivenom explained
Advertisement
Antivenom was first developed in the late 19th Century. It is sometimes referred to as ‘antivenin’ or ‘venom antiserum’ and is composed of various antibodies that are designed to treat the effects of envenoming. Antivenoms bind to and neutralise the venom to halt further damage, which in some cases allows the body to recover. Although it should only be used in the most serious cases, antivenom remains the primary method of treating snake and spider bites, as well as fish and scorpion stings.
Professor Mark O’Shea has been working with venomous snakes for over forty years, catching and milking a plethora of species across the world to support the work of Oxford University, the Liverpool School of Tropical Medicine, the Australian Venom Research Unit at the University of Melbourne, and the University of Adelaide, most recently in Myanmar. The bulk of this research was based in Papua New Guinea (PNG) – a region where snake envenoming is likely to lead to death. Mark is also a Professor of Herpetology at the University of Wolverhampton and teaches students about reptile and amphibian behaviour and conservation. “There are two different ways of looking at snake antivenom” explained Mark. “First, is it liquid or is it lyophalized antivenom (freeze-dried)? In the case of freeze-dried, you need to add sterile water for injection, to bring it back to a liquid. Freeze-dried is a bit more stable temperature-wise, but both need to be kept cool in a process called the ‘cold chain’. If the antivenom becomes warmer than 8°C, the chain is broken, and it shouldn’t be used. However, the powder is more useful in tropical countries.”
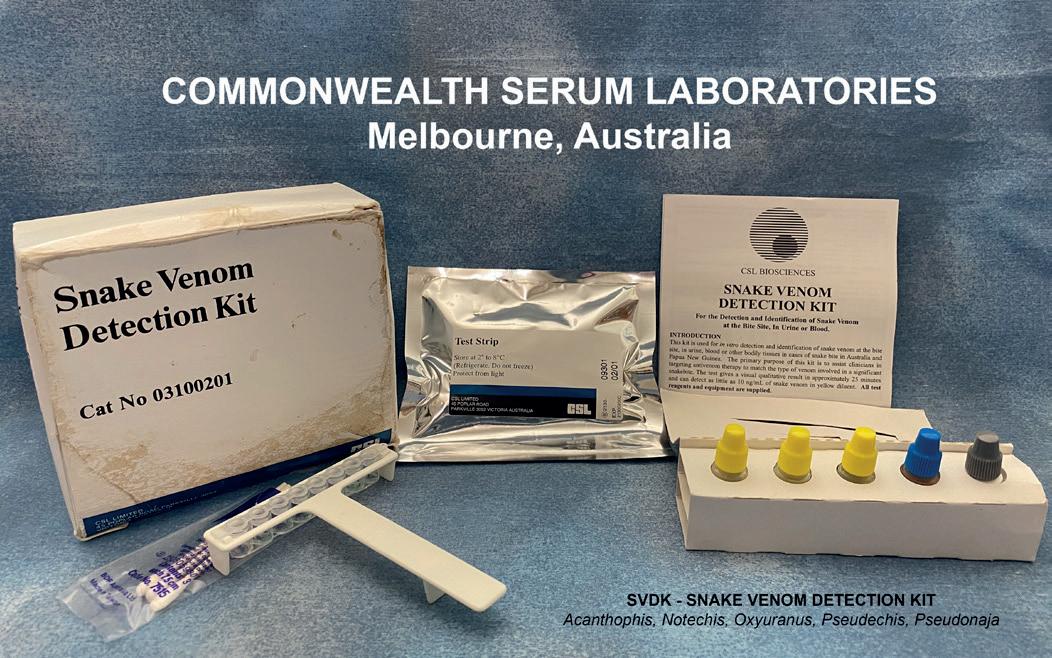
“The other way you divide antivenom is monovalent or polyvalent. Polyvalent antivenom is made from the antibodies of horses inoculated against all snakes in a particular area. The Australian polyvalent antivenom is produced at the Commonwealth Serum Laboratories (CSL) in Melbourne. The horses are inoculated against taipans (Oxyuranus spp. ) , blacksnakes (Pseudechis spp. ) , brownsnakes (Pseudonaja spp. ) , death adders (Acanthophis spp. ) and tigersnake (Notechis scutatus) . You end up with a BIG vial. That’s going to be more expensive for a start, but you’re also giving the patient a lot that they don’t need. They have only been bitten by one of those species. Having a greater volume of antivenom administered increases the chance of an adverse reaction. However, it should treat the envenoming and is therefore a better choice if the species of snake responsible is unknown.”
It isn’t just the likelihood of an allergic reaction preventing the widespread use of polyvalent antivenoms. These types of antivenom can be extremely expensive. For example, the Australian polyvalent antivenom, which is frequently shipped to PNG (a country which shares some of the biodiversity of Australia), costs around $2,500 for one treatment. In Papua New Guinea patients do not have to pay for their
Snakebite: A Neglected Disease of the Poor
treatment, but the sheer cost of the antivenom means PNG can afford less and less antivenom each year.
Mark continued: “A monovalent is produced for only one specific snake species. The Australian CSL also produce monovalent taipan, monovalent death adder, monovalent blacksnake, etc. In most cases, they’re much smaller vials of antivenom (except the taipan monovalent which is quite large). If you know what the patient has been bitten by it is a better idea to avoid the higher risk of negative reactions and economise by giving them the antivenom of the snake they have been bitten by. That’s if they are available and licensed to be used in that country – which is not always the case in Papua New Guinea.”


“An example of this are tigersnakes, which do not occur in New Guinea but the CSL tigersnake monovalent antivenom has been proven to work against the venom of the New Guinea small-eyed snake (Micropechis ikaheka). However, it is not licensed for use to treat bites from that species so CSL Polyvalent must be used.”
As the highly expensive polyvalent is the only choice in Papua New Guinea, there is a severe shortage of treatments. This has led to situations where doctors have felt obliged to share a single vial of antivenom (used to treat one snakebite), between three people because they could not face having to choose a single patient to treat, but now none of the three will receive a therapeutic dose.










