8 minute read
Snakebite: A Neglected Disease of the Poor
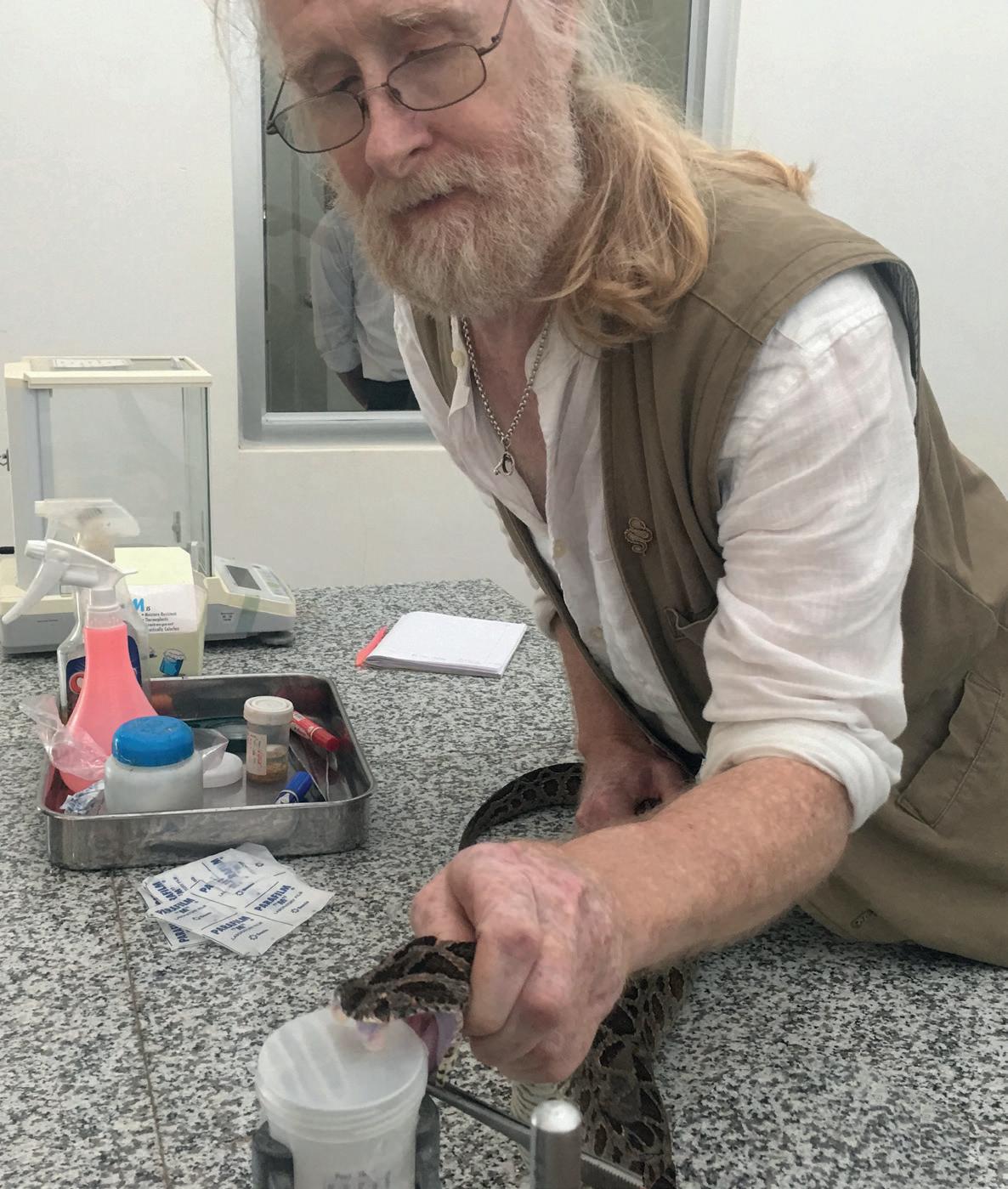
Identifying species
In Australia, members of the public are often advised not to attempt to identify the snake if it means compromising their first aid response or risking another bite. As venom moves through the tissues, blood and lymphatics, the entire limb should be immobilised with a bandage, and the person should avoid unnecessary movement. This is a technique referred to as the “Aussie bandage” and is effective against Australo-Papuan snakebites in that it slows the spread of the venom and enables the victim to get to hospital. In other parts of the world, some venoms cause swelling (such as vipers) the “Aussie bandage” could quickly become a torniquet, which would completely prevent blood circulation and could cause the victim to lose a limb to gangrene. It should only be used when there is a certainty that the snake responsible was an elapid that does not cause swelling. CSL in Australia produces Snake Venom Detection Kits (SVDKs), which allow doctors to use monovalent antivenoms successfully. The kit contains a series of troughs that react by turning blue in reaction to the presence of death adder, brownsnake, blacksnake, tigersnake or taipan venom via a process known as enzyme-linked immunobsorbent assay (ELISA). This is a marvellous method to determine the snake species responsible and target the venom precisely with a monovalent antivenom. Unfortunately, this particular SVDK is only applicable for Australian and Papuan elapids.
Advertisement
With high costs associated with producing antivenom, few developing countries even have fully-fledged antivenom programmes. Whilst affluent countries can implement testing procedures, airborne hospital transfers and free healthcare, other countries may not even have access to a single vial of antivenom or the means to keep it cool. This, combined with the fact that every region will have entirely different hazardous animals, means that antivenom research and production are moving at different paces across the world.
Mark explained: “In Africa, things are very variable. South African Vaccine Producers (SAVP) produce a polyvalent that will treat bites from all elapids and viperids in southern Africa, and they also produce two monovalents - one is for boomslang (Dispholidus typus), the other is for carpet vipers (Echis) in North
Africa. Boomslang is not in the polyvalent and last I heard, there was only one horse inoculated with boomslang venom. It is extremely scarce, and I don’t think its available outside South Africa so captive keepers of boomslang beware. But all the southern African adders, cobras, mambas etc, they’re all covered by the polyvalent. One thing keepers may not be aware of – there is no antivenom for twigsnakes (Thelotornis) or bush vipers (Atheris). Boomslang antivenom does not work for twigsnakes and Atheris is not included in the SAVR polyvalent.”
Of course, people do not have to be snake experts to correctly identify the species. Whilst a photograph, or a vague visual description might help assist in correctly identifying the animal, medical professionals can help narrow down the options. “In many cases, you can determine which species is responsible for the bite from the symptoms” added Mark. “If someone is continually bleeding, you know they’ve had either an anticoagulant or a procoagulant venom. In the case of procoagulant, the venom causes lots of microclots that are broken down, until there is no clotting factor left and the venom becomes incoagulable. There are also different types of neurotoxins i.e. pre- and postsynaptic, depending on where the venom attacks the nerve synapse (the junction where two nerves meet).
“Post and pre-synaptic neurotoxins kill through respiratory paralysis but in subtly different ways. You can reverse post-synaptic neurotoxins from a cobra quite late on.
I’ve been bitten by an Egyptian cobra (Naja haje) and antivenom alleviated it very quickly and I sat up in bed with a crossword that evening. If you’ve been bitten by something with a pre-synaptic neurotoxin, like a taipan, once paralysis sets in, you’re down. You’re down for 3–5 days. If someone is in paralysis with pre-synaptic neurotoxin, a bucket full of antivenom is not going to get them breathing again, they need to go on a ventilator. Here is how they differ. Post-synaptic neurotoxins block the receptor sites on the downstream side of the synapse so the message ‘breathe’ does not get across the synaptic gap. However, appropriate antivenom will swiftly clear the blockage and normal service is resumed. Presynaptic neurotoxins act more like cytotoxins, they destroy the transmitter sites on the upstream side of the synapse so the message ‘breathe’ never gets sent, and because this is physical damage the message will not be sent until the transmitter sites have been regenerated, and that takes time. Antivenom will prevent further damage, but it cannot undo damage already done. This is why certain snakes with presynaptic neurotoxins, i.e. black mambas and taipans are so dangerous, they even have their own presynaptic neurotoxins named after them ‘dendrotoxin’ and ‘taipoxin’.”
The economics of snake bite
The high cost of antivenom mean that there are a whole host of social and economic tightropes to navigate to ensure that antivenom is available for those who are bitten. Sadly, those in developing countries are at a much higher risk than those in developed countries. Despite Australia hosting many of the world’s most venomous snakes, only around 2-3 people are killed by snakebites each year.
In countries such as India, where people are generally much more exposed to snakebite and may not receive appropriate treatment, the story is tragically different.
“Snakebite is a disease” added Mark. “When I call it a disease, it is because it has a cure. Now, it is listed officially as one of the Neglected Tropical Diseases (NTDs) of the World Health Organisation (WHO). Hopefully, it’ll stay there because that means it is getting some funding. It is a disease of the poor voiceless people in developing countries, it is not a disease of people in developed countries. Yes, zookeepers get bitten, yes private keepers get bitten, but in very small numbers by comparison. When I used to tell people the figures for deaths and disabilities from snakebite every year they were shocked, but we’ve just had a COVID epidemic that has killed millions, so it’s very difficult to shock people now and it will be for some time. Anywhere between 98,000 and 138,000 people die of snake bites every year around the world. Most of those people are in India, Sri Lanka, Nepal, Myanmar, Mali, Nigeria, Togo, Benin, Senegal, the Gambia and New Guinea. Notice how none of those are Latin American countries. That’s because they have very good antivenom programmes which help alleviate the problem.”
“5000 people die a year in all of Latin America, 20,000 in Africa, 100,000 in Asia – and that’s just the deaths. A lot of snake venoms from snakes like puff adders (Bitis arietans) and spitting cobras (Naja spp.), the bites of which might not kill, cause tissue destruction and people lose parts of their bodies. Similarly, lanceheads (Bothrops) in South America causes limb loss, disfigurations, effects on central nervous systems and even on people’s cognitive abilities. It is estimated that 400,000 people are permanently disabled by snake bites, many more than are maimed by land mines. These people are often the breadwinners of the family or the children. The family inevitably must spend money to get the loved one to the hospital or pay for treatment. This means selling all their goats and everything they have. Even then, it’s like putting your house on a lottery ticket. It might work but it might not. People could end up with their family member dying or becoming permanently disabled with no social security AND now have lost their livelihoods. It pushes people into poverty beyond that which anyone in the West could imagine.”
Despite the horrific repercussions of snake bites in developing countries, social and political discourse has placed snakebite on the fringe of global aid priorities. Snakebite is not infectious and therefore it holds much less fear in the West than other tropical diseases. Someone cannot ‘catch’ snakebite and transmit it to other people. Ebola, on the other hand, was much better funded based largely on its threat to developed countries. Despite the immense number of snakebite victims and mortalities across the world, antivenom research gets just a fraction of the funding that malaria research does, though malaria still kills upwards of 600,000 per year, people can catch it and have it treated by their country’s healthcare system upon returning home. “There are heroes in antivenom” Mark stated. “They are the Costa Ricans that work in the Instituto Clodomiro Picado at the Universidad de Costa Rica in San José. They’re not a big bio-pharma company, but they are doing amazing work to help provide antivenom to the most impoverished countries. They started producing antivenom for the snakes in Costa Rica, then in Latin America, and now they produce antivenom for taipans in New Guinea, Russell’s vipers in Sri Lanka and various African antivenoms too. Their taipan product was just as efficacious as the CSL but because they are not a bio-pharma company, instead of $2,500 their antivenom was $250.”
The future of antivenom research
Over recent decades, the availability of antivenoms has shifted the way we look at the most dangerous species of snakes. Moreover, the most dangerous are not always the most venomous. Species which are widespread or inhabit urban environments in developing countries are often far more dangerous than Australia’s highly venomous taipans because humans encounter them on a much more regular basis. Arguably, at the top of the list of dangerous snakes causing large numbers of bites are the Russell’s vipers (Daboia russelii, D. siamensis) and the North African carpet vipers (Echis ocellatus, E. jogeri, E. romani), whereas the inland taipan (Oxyuranus microlepidotus), often trumpeted as the world’s most dangerous snake, has not yet caused a single fatality.
Mark explained: “Both Russell's vipers and three West African Echis species are particularly dangerous. Sometimes they can be thick on the ground and people collecting firewood get bitten. Although Daboia russelii in Sri Lanka is considered the same species as Daboia russelii in India, its venom is different. This is because snake venom is adapted to the prey. If you’ve got snakes that feed on different prey in different areas, over a fairly short time the venom will begin to adapt, it is a predatorprey arms race. When you’ve got juvenile snakes feeding on lizards and adults eating mammals, again, they go through an ontogenetic change as they get older. This has been proven in puff adders (Bitis arietans) and in Western diamondback rattlesnakes (Crotalus atrox).”
There is still much to learn about the way venom works. Whilst protecting the hundreds of thousands of lives affected by snake bites each year would be a very commendable aim, many of the countries able to finance this kind of project are far removed from the devastating reality of snakebite. However, other (slightly more selfish) motivations are continuing to push venom research in a positive direction. “Snake venoms are such amazing compounds, there’s a lot of hidden uses” added Mark. “The things that snake venom can do to you can be beneficial. There has been some work in the past to see if neurotoxic venoms can be used therapeutically for MS. A venom that can cause prolonged bleeding could be used in a drug to prevent blood clot forming, this would be really useful to someone that, for example, has recently had heart surgery. There used to be a drug (Arvin) produced from Malayan pit vipers (Calloselasma rhodostoma) for that purpose. After all, a lot of the excellent medicines we use today came from nature.”

Venom research is a broad and fascinating subject. Nowadays, the success rate of antivenom treatments is extremely high. Not only does venom research save lives but ongoing research is likely to uncover myriad applications to treat health defects and improve the health of citizens in the most affluent countries. However, with over 100,000 preventable deaths occurring in impoverished areas across the world each year, we are still a very long way away from medical equality.
More information on the World Health Organisation’s ‘Road to 2030’ strategy and regular reports on snakebite envenoming can be found on their website: www.who.int.
A powerful film on the issue of snakebite in impoverished countries can be watched by visiting: https://minutestodie.com










