NURSING
Fall 2017
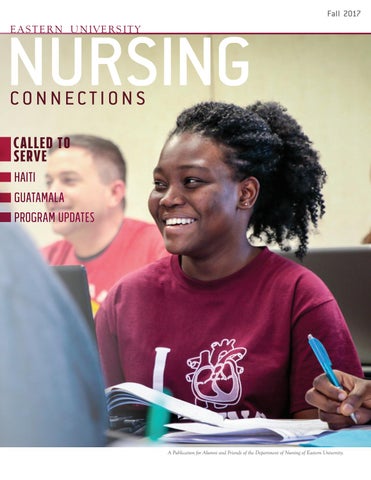
CONNECTIONS Called to serve Haiti Guatamala Program Updates
A Publication for Alumni and Friends of the Department of Nursing of Eastern University.
NURSING
Fall 2017
CONNECTIONS Called to serve Haiti Guatamala Program Updates
A Publication for Alumni and Friends of the Department of Nursing of Eastern University.