LEARNING AND EXPLORING TOGETHER AT THE 36TH EACTS ANNUAL MEETING
year we are thrilled to be joined by colleagues from more than 90 different countries. It is always a pleasure to see so many people interact and embrace the opportunity to learn and build new relationships.
taken back to our home institutions to support our primary goal of improving patient outcomes.
A more dynamic EACTS
Rafa Sádaba EACTS Secretary General
I am delighted to welcome you to the 36th EACTS Annual Meeting. Over the next three days we can look forward to a fantastic programme featuring the latest world-class science and innovation, best evidence and stimulating discussions on the most prevalent issues in cardiothoracic surgery.
The EACTS Annual Meeting is the leading global event for the cardiothoracic community and this

We are constantly thinking about ways to enhance the Annual Meeting experience and deliver more learning opportunities for delegates. This year we are excited to launch EACTS TV, our new premium TV channel and onsite TV studio, which includes daily preview shows focusing on the day’s key topics and big debates with expert panelists. I encourage everyone to visit the onsite TV studio, located in the exhibition hall, to see all the action live.
Although this year is my last Annual Meeting as Secretary General of EACTS my passion and enthusiasm for this important event will continue. This passion is shared by the members of our Domains, Task Forces and Committees who have worked so hard to put together a high-quality and varied scientific programme. Over the next three days we will all gain new knowledge and experiences that can be
As I step down from the role of Secretary General, I am proud to have played a part in the organisation’s achievements in recent times. We have faced some challenges, but we have worked hard to support our members throughout the COVID pandemic, continuing to provide access to first class education and training, to support high standards in patient care.


Over the past few years EACTS has modernised to become a more dynamic and efficient organisation. Even more than ever, we are perceived globally as truly leading in the field, with a membership of over 4,000 surgeons and other professionals from the cardiothoracic community around the world.
A valued team
We are fortunate to have a great team based in Windsor and I am grateful for the support they have given me. They have an excellent understanding of
WELCOME
EACTS and the needs of our members. In recognition of their talents and experience we have devolved more of the day-today running of the organisation to the Windsor-based team, giving them clear responsibilities and areas of work. The team is led by our new CEO, Brendan Eley, who has already made such a positive contribution to our Association, and I know he will work closely with Patrick Myers, our incoming Secretary General, to evolve our offer to the global cardiothoracic surgical community and ensure we are fit for the future.
The way we have organised the Domains and Task Forces has also changed. These groups are critical to driving forward our mission of advancing education and promoting research. We have implemented terms of reference, so Domain and Task Force members have a better understanding of their responsibilities. Importantly, these changes mean that the surgeons who volunteer their time to support EACTS are able to focus on making the strategic decisions that are critical to driving the organisation forward. We have also implemented new recruitment systems to ensure all EACTS members have the opportunity to express their interest in joining these Task Forces.
Delivering high quality education
Education is at the heart of our work and, as Chair of the Education Committee, I am focused on delivering meaningful learning opportunities for our members that enhance skills and expertise and improve clinical practice.
It is important that our courses cover a breadth of experience and knowledge

which is why we have instigated the course levels to allow surgeons to access training at their level of expertise – whether a trainee or an established surgeon. Our prestigious Francis Fontan Fellowship Programme also offers fantastic opportunities for surgeons at different stages of their career. We continue to expand this programme, broadening the range of learning opportunities for our members and building a remarkable global cardiothoracic community.
Members are invited to come forward with ideas for future courses and fellowships and these ideas will be carefully considered and assessed by the Education Committee. We need to be confident that we are making the right investment in education for our members.
Our membership includes surgical communities in more than 100 countries, well beyond Europe, reaching other parts of the world that are less well served in terms of educational opportunities. Of course, there is always much more we can do.
It is often through our close collaborative links with sister organisations, in particular the STS, that we are able to provide unique training opportunities to members across the globe.
Although my time as Secretary General is ending, I am honoured to remain part of EACTS. I will still attend Council meetings and provide advice on education in my role as Chair of the Education Committee. I enjoy being part of the association as it serves such a valuable purpose to so many people, helping the cardiothoracic surgical community continue to improve outcomes for our patients.
I hope you enjoy your time in Milan.
The lightest system with gold standard features and unique advanced technologies for unlimited ECLS clinical applications



REIMAGINE ECLS TREATMENTS. TOGETHER.
The only fully coated and magnetically levitating centrifugal pump designed to optimize blood flow even in the smallest patients

TECHNO COLLEGE
PIONEERING NEW METHODS AND INNOVATIONS
The 36th EACTS Annual Meeting kicked off yesterday with a fascinating Techno-College demonstrating the latest innovations and techniques in cardiovascular and thoracic surgery.

With advances in the field emerging at incredible speed it is critical for surgeons to keep abreast of the latest developments that have great potential to improve patient outcomes. Techno-College, with its unique format of live surgery and live-in-a-box cases, is the perfect forum to help surgeons keep up to date with technological breakthroughs and learn the appropriate use of current and future technologies.
This year EACTS offered two innovative Techno-College programmes featuring emerging trends in cardiovascular and thoracic surgery.
Cardiovascular surgery
The full day cardiovascular programme, developed by the New Technology taskforce, highlighted new surgical, endovascular and interventional techniques in valve intervention and aortic surgery. This included a live demonstration of normothermic arch surgery without circulatory arrest and a new interventional technique for endovascular thoracoabdominal repair.
The first session of the day ‘Aortic Valve, Aorta and Beyond’ featured a number of live-in-a-box presentations such as Minimally Invasive Multi Vessel Coronary Artery Bypass Graft and the transcatheter treatment of a left ventricular assist device induced LVAD induced aortic regurgitation.
There was further live surgery in the session ‘Atrioventricular Valves - Valves’ which focused on the mitral valve including a demonstration of a transapical
beating heart mitral repair procedure and the presentation of a mitral valve prothesis, which is new to the market.
Thoracic surgery
The thoracic surgery programme offered a valuable opportunity for participants to learn the innovative techniques required to perform segmental resections. Sublobar resection is very topical and becoming more prevalent in thoracic surgery.
Participants were able to pick up lots of tips and tricks on performing VATS segmentectomy and robotic segmentectomy and enjoy discussions around the benefits of sublobar resections.
The value of robotic surgery was demonstrated during the afternoon session, with speakers from Europe and the US showcasing the benefits of robotic devices.
Robert Cerfolio from NYU Langone Health in the US discussed how to mitigate and obviate bleeding and other complications during complex robotic pulmonary resections. With experience of undertaking over 2,500 robotic pulmonary operations, Professor Cerfolio and his team are now able to perform every single operation robotically. He demonstrated how to get control of the pulmonary artery intra-pericardial and how to safely dissect the artery after radiation chemotherapy or immunotherapy. Outlining the impact on patient outcomes, he noted that robotic surgery allows surgeons to do sleeves of the bronchus and the pulmonary artery safely and efficiently without blood transfusions and without conversion to thoracotomy in a 2–3-hour operation thus helping to eliminate 30- and 90-day morbidity and mortality risks.
Image-assisted robotic lung segmentectomy
Jean-Marc Baste, MD, PhD, Chief of Thoracic Unit , University Hospital of Rouen, Normandy, France
Lung resection for cancer has moved from open to mainly minimal invasive surgery these past few years.1 Another trend is the development of less aggressive lung resection with lung segmentectomy for early stage lung cancer.2
Since 2012 and the implementation of our robotic programme, we have developed minimal invasive segmentectomy.3,4 The difference between VATS and RATS for segmentectomy showed less bleeding for the robotic group.4
We found during this period that segmentectomy was still a difficult operation despite RATS due to high anatomical variations. We decided to launch a pilot study using 3D CT planning to improve the quality and also the number of segmentectomies.5 This study was very promising but to keep on improving the margins and the number of segmentectomies we added perioperative marking using indocyanine green for tumor and intersegmental plan location.6 This multi-image navigation system allowed us to improve the quality and quantity of segmentectomies.7 Image-assisted surgery is thus a routine procedure in our unit with promising results.8
The robotic approach is helpful to perform segmentectomy but it is only one piece in the whole process. Peri-operative images (pre-operative and peroperative 3D images and marking) are the cornerstone for segmentectomy. We would like to present our comprehensive approach for minimal invasive segmentectomy to treat early stage lung cancer with the highest level of care.
1. Montagne F, Guisier F, Venissac N, Baste JM. The Role of Surgery in Lung Cancer Treatment: Present Indications and Future Perspectives-State of the Art. Cancers (Basel). 2021;13(15).
2. Berg E, Madelaine L, Baste JM, Dahan M, Thomas P, Falcoz PE, et al. Interest of anatomical segmentectomy over lobectomy for lung cancer: a nationwide study. J Thorac Dis. 2021;13(6):3587-96.
AORTIC VALVE, AORTA AND BEYOND
Valve-in-valve with leaflet splitting (live-in-a-box)
Axel Unbehaun, German Heart Center Berlin, GermanyValve-in-valve (ViV) TAVI is an effective treatment for patients with failed bioprosthetic aortic valves. Coronary artery obstruction is a rare but serious complication of ViV TAVI, with an overall incidence of up to 3.5%, with procedural mortality rate approaching 50%.
There are several risk factors that can identify patients at risk for coronary artery obstruction following ViV TAVI procedures, such as supra-annular valve leaflet position, long leaflet profile, externally mounted leaflets, and high device implantation.
Current preventive transcatheter strategies include stenting techniques that are intended to deflect the leaflets away from the coronary ostia or bioprosthetic aortic scallop intentional laceration (BASILICA) to prevent iatrogenic coronary artery occlusion. Although BASILICA is an effective procedure to prevent coronary obstruction, it requires highly skilled and experienced operators utilising this uncommon method, and is performed with off-label tools.
During the annual Techno-College meeting, Dr Unbehaun will be presented a live-in-a-box of ShortCut™, the first dedicated transcatheter device designed to split the leaflets of a degenerated bioprosthetic aortic valve in patients undergoing valve-in-valve (TAVI) procedures who are at risk for TAVI-induced coronary artery obstructions.




Lifetime management for patients with aortic stenosis is an increasingly important consideration, as the use of bioprosthetic valves is rising in younger patients. Therefore, a device such as the ShortCut is necessary to facilitate the treatment of patients requiring multiple valve therapies throughout their lifetime.
The ShortCut device is currently being evaluated globally in a prospective, multi-centre, non-randomised, single-arm, open-label clinical study to demonstrate the safety and effectiveness of the device (The ShortCut Study). ClinicalTrials.gov: NCT04952909.
“Lifetime management for patients with aortic stenosis is an increasingly important consideration as the use of bioprosthetic valves is rising in younger patients.”Richard Milton
AORTIC VALVE, AORTA AND BEYOND


Normothermic frozen elephant trunk without circulatory arrest
Professor Marco Di Eusanio, Lancisi Cardiovascular Center, Politechinic University of Marche, Ancona, Italy


Over the past decade clinical results after Frozen Elephant Trunk (FET) surgery have progressively improved. Nevertheless, death, spinal cord injury and systemic complications remain substantial and, intra-operatively, certainly related to prolonged extra-corporeal circulation (ECC) times and use of hypothermic circulatory arrest (HCA) (D. Tian et al, ACS 2013). Therefore, with the aim of improving our results, we developed a truly hybrid modified FET technique that completely avoids HCA (Di Eusanio ACS 2019). Cornerstones of this truly hybrid approach include a) a combined femoral and innominate artery cannulation for ECC arterial return that allows continuous upper and lower body perfusion, b) antegrade selective cerebral, c) a retrograde trans-femoral stent graft deployment and d) its occlusion with a balloon-catheter following the same route. Main steps of the intervention are indicated in figure 1. After a median sternotomy, both the innominate and the femoral artery are cannulated for ECC arterial inflow. Through a femoral access, an endograft is retrogradely deployed in zone 1 or 2 with appropriate distal sealing. Normothermic ECC is initiated and the left subclavian and carotid artery are cannulated for antegrade selective cerebral perfusion. The ascending aorta is clamped and cardioplegic arrest is obtained. Afterwards, the proximal endograft is retrogradely occluded using a balloon catheter keeping the lower body perfused from the femoral artery; the innominate artery is clamped proximally and the aortic clamp is removed. With a bloodless operative field, the distal anastomosis between a 4-branched vascular graft and the endograft is performed. The vascular graft is clamped, the balloon deflated and the arch reconstruction completed as usual.
Different from other previously reported techniques, this approach completely avoids circulatory arrest and allows a normothermic ECC conduction while providing a perfectly bloodless and maneuverable operative field, as the balloon is retrogradely (and not antegrade) advanced into the stent graft for aortic clamping.

AORTIC
Reverse Frozen Elephant Trunk for Thoracoabdominal Repair
Sabine Helena Wipper, Department of Vascular Surgery, University Hospital Innsbruck
The Thoracoflo® graft is designed for hybrid thoracoabdominal aortic repair, avoiding thoracotomy and extracorporal circulation by using retrograde visceral perfusion via an iliac side branch (SPIDER technique). The graft design is based on the Frozen Elephant Trunk technique and the graft is implanted in a reversed way against the blood flow. The Thoracoflo® graft consists of a proximal stent graft connected to a seven-branched abdominal prosthesis for reattachment of visceral and iliac arteries via a collar. The access branch can be used for reattachment of lumbar arteries. The graft design was modified and re-evaluated in an experimental in-vivo setting to improve graft deployment, fixation and stability, and de-airing as well as enabling reattachment of lumbar arteries and establish over-the-wire implantation.





The technique of graft implantation works as follows:
After retroperitoneal exposure of the infradiaphragmatic aorta, including visceral and renal arteries, one iliac branch is temporarily attached to an iliac artery to maintain retrograde visceral and antegrade iliac perfusion after deployment of the thoracic stentgraft segment (SPIDER-technique). The proximal stent-grafted segment is deployed in the thoracic aorta via direct aortic puncture or an access branch over the wire under transesophageal echocardiography avoiding fluoroscopy. To reduce the risk of bleeding and graft migration this is performed under in-flow occlusion or rapid pacing. After de-airing of the graft via the side branches, flow via the iliac side branch to the visceral and iliac arteries is established avoiding extracorporeal circulation by establishing pulsatile blood flow. Visceral, renal and lumbar arteries are then subsequently sutured to the corresponding side branches of the graft and the collar is attached to the aorta to prevent graft migration and back bleeding from intercostal arteries. If needed, the access branch can be used for reattachment of lumbar arteries.
This technique requires a landing zone in the descending thoracic aorta, which can be realised by an endovascular treatment using TEVAR.


After feasibility testing, including quantitative assessment of organ perfusion, the first implantation in a human was successfully performed. Actually selected patients are treated and evaluated in dedicated centers.


INSPIRIS RESILIA* Aortic Valve The only valve with VFit technology**
Expansion zone designed for potential future valve-in-valve procedures.Figure 1: The Thoracoflo® graft before (top) and after (bottom) deployment
INNOVATION AWARD
WINNER
An innovative approach to improving patient treatment
Francesco Pollari has been awarded the 2022 Techno-College Innovation Award for his innovative MIC Cannula for minimally invasive central aortic perfusion.


The MIC-Cannula, which was recently granted a European patent, is an intravascular cannula for arterial perfusion of the human body allowing a more natural and physiological arterial perfusion of patients needing mechanical circulatory support (CPB, ECMO or ECLS), whilst reducing invasiveness at the same time.
This innovative device could improve the treatment of patients in many
settings such as cardiology, cardiac surgery and ICU, and represents a significant advance towards hybrid cardiac surgery.


Commenting on his win, Francesco said, “I am delighted to win the TechnoCollege Innovation Award. There is no better platform to showcase this device and seek opportunities to collaborate and partner with medical professionals and industry representatives. I am confident that the MIC Cannula has the potential to improve treatment for patients and I am looking forward to progressing this innovation further.”
The Techno-College Innovation Award supports the development of new innovative ideas, techniques and developments in cardiovascular and thoracic surgery. Two recent winners of the Techno-College Innovation Award describe how the award has helped make their dreams become a reality.
ACKNOWLEDGEMENT
DEGREE
Vinayak Bapat, Chief of Cardiothoracic Surgery at Abbott Northwestern Hospital in Minneapolis, won the Techno-College Innovation Award in 2013 for his innovative aortic app platform, one of the first apps to support clinicians involved in complex valve in valve procedures. He outlines how the experience has helped further the development of new innovative apps.
“It was an honour to receive the Techno-College Innovation Award. It is a peer acknowledgment of the highest degree, and it gave us a boost to develop the next two Apps.
“Clinicians involved in Valve in Valve procedure need to access specific information that is easily identifiable, easily accessible and relevant to the clinical scenario. The Valve in Valve app provides the platform to identify, confirm and then narrow down the information to match the clinical scenario.
“The prize money seed funded the development of Mitral VIV app, which launched in 2014. The Mitral VIV app addresses a more complex subject of Mitral VIV, Mitral Valve-in-ring and Tricuspid Valve-in-Ring procedures.


“We continue to update the apps with new content such as new TAVI and surgical valves, new procedural clips and more importantly, inclusion of topics/new concepts in this field. A third app, to be launched in October 2022, will address heart valve space and is aimed at surgeons and echocardiographers.
“These Apps are now downloaded in 156 countries and has over 70,000 users.”
AN EXPERIENCE OF A LIFETIME
Hazem Fallouh, a thoracic surgeon at University Hospitals Birmingham, was awarded the Techno-College Innovation Award in 2021 for his innovative pericardial device to monitor cardiac output and diagnose tamponade in patients undergoing cardiac surgery. He describes the impact of winning the award.

“The impact of the Techno-College Innovation Award has been phenomenal. I have had the patent for the pericardial device for about four years. The idea has always resonated with a lot of my colleagues who agreed that it had the potential to improve patient’s outcome. This device aims to predict the development of cardiac tamponade and monitor cardiac output at no extra cost. Despite its appeal, trying to raise funds to develop the technology was very challenging.
“Winning the award provided a major boost and raised the interest in the device to another level. It is like an objective peer review certificate. Shortly after, I was awarded a grant for £500,000 from Innovate UK to fund the development of the prototype. I am sure the award strengthened the grant application. Since the award and grant, I haven’t stopped”.
“I am now working with the University Hospitals Birmingham and Professor Tom Clutton-Brock, MBE, a retired cardiac anaesthetist and a medical device expert from his work with NICE in the field. We are building the prototype and collaborating with the University of Sheffield to perform the necessary trials. I am hoping to have a functioning prototype in the next 12 months.
“It’s been extremely fulfilling few months. We are now building a team for the project. The Techno-College Innovation Award was the experience of a lifetime. The endorsement and exposure have been invaluable.”
DOMAIN HIGHLIGHTS
EACTS Domains are member led groups working across the four EACTS Domains - Acquired Cardiac, Congenital Heart, Thoracic and Vascular diseases - to drive forward the Association’s mission of advancing education and promoting research. Experts on the Domain Committees play an instrumental role in putting together the Annual Meeting scientific programme. Here, the Domain chairs outline some of the key sessions to look out for this year.
ACQUIRED CARDIAC DISEASE DOMAIN
Critically appraising the evidence
The FAME 3 trial, which was published earlier this year, will be covered extensively during the Annual Meeting, including Saturday’s sessions ‘What should we learn from FAME 3? ’ and ‘Clinical Trials Update’. This trial is important as it demonstrates the value of CABG in triple vessel disease, so I recommend these sessions to delegates interested in learning more about what the trial means for CABG and PCI.
An exciting addition to this year’s programme is a session hosted by ERAS (Enhanced Recovery in Cardiac Surgery). This is a new movement within surgery that is also covering cardiac surgery. The session on Saturday will consider major elements of ERAS for cardiac surgery, including Optimising an ERAS Patient Blood Management Program and Standard of Care for Mechanical Circulatory Support.
And let’s not forget what makes the EACTS Annual meeting so special – the opportunity to reunite with friends and make new connections that will last a lifetime.
The Acquired Cardiac Disease Domain has a great programme at this year’s Annual Meeting featuring many global experts in their field. The 12 task forces that are part of our domain have designed sessions that cover the latest innovations, developments and evidence across their specialties. We have worked hard to find practical topics that are important in everyday practice and represent different challenges across the globe.
We will examine the latest evidence that is presented through trials, studies and published papers. In Thursday’s session ‘Clinical trials in coronary surgery – a look into the future ’ we will examine recent trials that focus on the value of CABG and consider new data which focuses on the enhanced role of CABG in coronary revascularisation.

As well as providing an overview of the FAME 3 trial, the ‘Clinical Trials Update’ session will provide a broader look at conducting clinical trials and using critical analysis to interpret the trial results as well as insights into how clinical trials can influence daily practice.
Last year the ‘TMVI for beginners ’ was a very well received session and, as the number of surgeons involved with the mitral valve will increase, it continues to be a critical session for many delegates. The focus session this year, taking place on Thursday, has a different format which will explore more intricate discoveries about the mitral valve.
Robotics and aviation are two new taskforces to the Acquired Cardiac Disease Domain and this year robotics features in many sessions across the fields of adult cardiac surgery. The session ‘Minimally invasive mitral valve repair: strategies and outcomes’ on Friday will, for example, explore robotic approaches to valvular heart disease.
I would encourage everyone not to miss our honorary guest speaker, retired Lufthansa pilot Manfred Müller who will share his knowledge and insights about flight safety and how to implement safety strategies from the aviation world into the medical world.
Domain Members
Filip Casselman, Chair, Acquired Cardiac Disease Domain
“Robotics and aviation are two new taskforces to the Acquired Cardiac Disease Domain and this year robotics features in many sessions across the fields of adult cardiac surgery.”
“We will examine the latest evidence that is presented through trials, studies and published papers.”
• Filip C asselman
Patrick Myers
Fabio Barili
Manuel Castella
Dahle
Michele De Bonis
Ruggero De Paulis
Gloria Färber
Mario Gaudino
B. Grau
THORACIC DISEASE DOMAIN
Inspiring the next generation
Richard Milton, Chair, Thoracic Disease DomainI feel fortunate to be chair of the Thoracic Disease Domain at such an exciting time as we work to increase our footprint across EACTS and support the next generation of thoracic surgeons.
Yesterday’s Techno-College was a great start to the 36th EACTS Annual Meeting, providing a fantastic platform to showcase the latest technology and innovations in thoracic surgery. Experts in the field demonstrated the latest techniques required to perform segmental resections and delegates saw first-hand the value of robotic surgery during complex thoracic surgery.
Expert speakers
The theme of innovation runs throughout the thoracic programme at this year’s Annual Meeting. Today’s focus session ‘Thoracic innovation’ will include talks on 3D imaging, artificial
intelligence in radiology, and electromagnetic navigation. This is an important session to attend as we continue to explore new ways to improve patient outcomes.
Within thoracic surgery we often work with other specialties and this approach to joint working is evident in the scientific programme. For example, Thursday’s session on ‘Management of early-stage lung cancer ’ features Betty Tong, a surgeon from the States, Kevin Franks, an oncologist from Leeds in the UK, and a radiologist from Oxford, Dr. Anderson. Attracting speakers from different specialties who can provide a different viewpoint is fantastic.
In addition, as a domain, we intentionally chose speakers from around the world who can provide a unique international perspective. In Friday’s session on ‘Quality in Thoracic Surgery ’ we will hear from Doug West who is very active in UK data collection as well as Rene Peterson from Copenhagen who will discuss benchmarking thoracic surgery in Denmark. Unlike most countries, Denmark captures data on all thoracic surgery patients, so the country has a great resource to measure outcomes.
Saturday’s focus session on ‘Drainology ’, which we are running with colleagues from the Acquired Cardiac Disease Domain, will be interesting. It is likely we have only touched the tip of the iceberg in our knowledge on chest drains given the incredible advances in technology. In this session we’ll look at variations in chest drain management between cardiac and thoracic surgery as well as evidence-based chest drain management and the use of digital drains in cardiac surgery.
Training the future of thoracic surgery
I’m proud of how much we’re focused, both within the thoracic domain as well as across the whole association, to involve residents in the scientific programme as much as possible. With thoracic surgery on the rise, residents really are critical to our future and the Annual Meeting is a great forum for residents to start their journey into thoracic surgery.
How we train residents is very important and simulation now plays a huge part of resident training. This year in the thoracic Learning Lab delegates will have an opportunity to train on a VATS simulator in a session led by my domain colleague, Tomaž Štupnik, who designed the VATS simulator model.
The use of simulators highlights the added value of virtual reality for both surgical planning and surgical training/educational purposes. The educational focus of the thoracic Learning Lab will be on pulmonary lobar and segmental bronchovascular anatomy from a surgical perspective. Spaces in the Learning Lab are limited, so anyone interested should register as soon as possible.
This is the first Annual Meeting after all COVID restrictions have been lifted. For me, the meeting is as much social as scientific, so meeting with and making new friends and colleagues from around the world is priceless. I’m really looking forward to it.
Domain Members
• Tim Batchelor• Korkut Bostanci

“The theme of innovation runs throughout the thoracic programme at this year’s Annual Meeting. Today’s focus session ‘Thoracic innovation’ will include talks on 3D imaging, artificial intelligence in radiology, and electromagnetic navigation.”
• Richard Milton
• Fabian Dörr
• Marion Durand
• Vincent Fang
• Jari Räsänen
• Tomaž Štupnik
VASCULAR DISEASE DOMAIN
Stimulating and lively debates
We’re looking forward to some stimulating and perhaps controversial debates as we discuss prevalent topics in our field – such as the risks and decisions around Acute Type A Aortic Dissection and the advantages and disadvantages of different treatment options for thoracic vascular disease, including endovascular and open surgery.

The aortic arch features strongly in the Vascular Disease Domain programme this year. This includes two focus sessions on Saturday: ‘Aortic arch treatment – a balancing act between risks and benefits’ which explores the surgical management of the complex aortic arch disease and ‘Neurological outcome in aortic arch surgery – Opening the Pandora´s box ’ which focuses on neurological complications and protection strategies in any kind of aortic arch treatment.
This year we have also put together two fantastic Learning Lab sessions. On Thursday morning in the ‘AV Repair’ Learning Lab delegates can learn about the two main techniques for valve sparing aortic root surgery: reimplantation and remodelling, and there is a fantastic opportunity on Friday to practice skills with our hands-on training on endovascular stent graft thoracic aortic treatment in the TEVAR simulation Learning Lab.
Domain Members
• Konstantinos

Tsagakis
• Martin Czerny
• Nimesh Desai
The Vascular Disease Domain has worked hard to prepare an interesting programme for the 36th EACTS Annual Meeting, which covers all fields of aortic disease including open surgery and vascular treatment.
We’re delighted to once again host a joint focus session with STS. Taking place today, ‘Connecting to connective tissue aortic disease ’, considers the management and treatment of the aorta in connective tissue disorder. This includes a presentation on the lifelong management of genetic aortic syndromes that present with acute aortic dissection.
• Davide Pacini
• Florian Schoenhoff
• Andreas Zierer
WE TAKE LI F E TO HEA RT
CONGENITAL HEART DISEASE DOMAIN
Cutting-edge innovations
As surgeons it is important that we keep an eye on new trends that may outperform our classic surgical approach. In a joint session with AEPC on Thursday – ‘The Cyanotic Newborn – Surgery or Intervention for Palliation’ – we will cover new developments for the management of cyanotic newborns. Given the shift from surgery to intervention with, to date, an unknown impact on patient outcomes, we can look forward to a fascinating discussion of the pros and cons with our friends in paediatric cardiology.
Challenges in developing countries
comparison. In the session ‘Database and machine learning ’, which is run jointly with ECHSA, CHSS, STS, WSPCHS and ASCVTS, we will consider the role of new technologies in analysing big data and the benefits of databases.
Jürgen Hörer, Chair, Congenital Heart Disease Domain
Cutting-edge new technologies will feature strongly in this year’s Congenital Heart Disease Domain programme, showcasing exciting new innovations that have game-changing potential for our patients.



In the session ‘New Technologies ’ on Saturday we will explore the surgical options for pulmonary vein stenosis, highlighting innovative techniques such as xenotransplantation, which could be a promising technique for congenital heart disease in the future, as well as robotic surgery and mitochondrial transplantation.
More fascinating new technology will be discussed during Saturday’s session ‘Strengths and weaknesses of diagnostic modalities ’. As the preferred diagnostic tools continue to change with the availability of 3D visualisation, printing and virtual reality, we will discuss the advantages and disadvantages of the different diagnostic tests available for evaluating congenital heart disease.
This year the Congenital Heart Disease Domain has included a number of topics in the scientific programme that haven’t featured for several years. Thursday’s session on ‘Late presentation’ run jointly with Global Heart Care PASCaTS will focus on congenital heart surgery in developing countries, mostly in Africa.


“After many years of data collection, we have big data, sufficient enough to use artificial intelligence and machine learning for outcome prognosis and comparison.”
EACTS is a global organisation, and a lot of our colleagues come to the Annual Meeting from around the world, including developing countries. It is therefore important that we provide a forum to discuss some of the specific challenges they face in daily practice. This is an opportunity to learn from colleagues who treat these patients on a daily basis and discuss the differences in surgical strategy for repair of congenital heart disease in patients who are referred late for treatment.
After many years of data collection, we have big data, sufficient enough to use artificial intelligence and machine learning for outcome prognosis and
EACTS
“EACTS is a global organisation, and a lot of our colleagues come to the Annual Meeting from around the world, including developing countries. It is therefore important that we provide a forum to discuss some of the specific challenges they face in daily practice.”
The EACTS Annual Meeting always provides great opportunities to gain hands-on experience from expert surgeons. The Congenital Heart Disease Domain is running a very interesting Learning Lab this year focused on surgical strategy in complex congenital heart disease. During this two-hour session we will be discussing alternatives for biventricular repair with left systemic ventricle and using 3D printing models to understand complex cardiac malformations and plan surgical strategies.
Domain Members
• Jürgen Hörer
• Amir-Reza Hosseinpour
• Kirolos Jacob
• Matej Nosal
• Caner Salih
• Eva Sames-Dolzer
• Luca Vricella
New for 2022
Our new EACTS premium TV channel and onsite TV studio will broadcast a mixture of live and recorded content.
Highlights include:
Daily preview shows
on the day’s key topics
The big debates with our expert panellists
In Focus sessions with key opinion leaders
keynote sessions broadcast live from the session rooms in Milan
Daily review shows summarising and debating the day’s programme
Get closer to the action and visit the EACTS TV studio located in the exhibition hall. View the full daily schedule on page 22.
ARE DELIGHTED TO WELCOME RETIRED PILOT AND HEAD OF FLIGHT SAFETY AT LUFTHANSA HG, MR MANFRED MÜLLER, AS OUR HONOURED GUEST SPEAKER AT THIS YEAR’S ANNUAL MEETING.
While both Professor Troidl and Manfred agree that highly sophisticated technologies are needed to prevent catastrophes within the aviation and medical industry, what is equally, if not more essential, is the way employees work together as a team in handling safety critical situations.
 Manfred Müller
Manfred Müller
When Manfred observed how hospitals operate, he noticed that the main difference between the aviation and medical industries was the way that failures are analysed. In the aviation industry, every accident is documented perfectly; all switch positions, communications and perimeters of flights are monitored to get a clear picture of what has gone wrong. A significant number of catastrophes occured because errors or unclear concern was not addressed by the co-pilot and communicated clearly with the pilot. This cooperation and support from fellow colleagues is key to mitigating risk situations.
With more than 40 years’ experience working as a pilot for Lufthansa, Manfred dedicates his time to sharing his knowledge and insights about flight safety and how to implement safety strategies from the aviation world into the medical world.
For almost two decades, Manfred has lectured on risk management at the University of Bremen and the Technical University of Munich. He has supported the European Commission in organising projects to improve flight safety within the EU and has been awarded the Federal Cross of Merit for diverse commitment in the field of risk management.

His collaborations with Professor Troidl, a highly respected surgeon and passionate advocate of patient safety, have solidified Manfred’s approach to implementing specific safety strategies. Combining their aviation and medical expertise, they discovered that almost identical strategies are required to increase passenger and/or patient safety.
Over the years they spent doing failure analysis and sharing knowledge of their respective industries, they learned that the root cause of more than 70 per cent of all mishaps was human error. After carrying out studies and experiments with the goal of reducing human error, the conclusion was unanimous: the quality of team interaction is a key factor in reducing the risk level.
When Manfred observed how hospitals operate,
noticed that the main difference
When it comes to the medical industry, Manfred observed a steep hierarchy that hinders some colleagues’ ability to “speak up”, afraid of ruining their careers if they do. Manfred concludes that the leading doctor and pilot must be supported, corrected and assisted by the rest of the team if mishaps, failures and accidents are to be minimised. Being assertive and speaking up is a main key to risk reduction.
Manfred believes that these basic principles of teamwork organisation from the aviation world should be applied to the medical world in order to significantly increase patient safety.
Hear more about Manfred’s unique perspective on risk management today at 12:00.
THREE DAYS OF WORLD-CLASS SCIENCE
This year's
scientific
latest
Today's abstract and focus sessions
Thoracic Non-Oncology
A 20 Year Analysis Comparing Predictors of Abdominal Organ and Lung Procurement in DCD Donors Reveals Stricture Donor and Organ Function Criteria Required for Lung Transplantation
In the US today, controlled DCD is the primary mechanism of DCD procurement in order to reduce warm ischemic times, and multicenter-large-cohort studies continue to show comparable survival outcomes between these DCD organs and DBD organs. Yet, despite these favorable outcomes, it is possible that various institutional and ethical barriers, as well as unfamiliarity of surgeons with DCD practices, have led to their underutilisation. In this study, we looked to analyse patterns in clinical practice that differentiate non-use in DCD abdominal organs versus DCD lungs to identify potential subjectivity and ultimately promote utilisation.
Our data revealed that transplantation teams applied more rigorous criteria when evaluating many donor characteristics for procurement of DCD lungs compared to DCD abdominal organs and recorded these decisions in the OPTN. These discrepancies in what transplant teams deemed acceptable were evident in both the lifestyle and clinical characteristics of these donors, including history of smoking, diabetes, insulin dependence, hypertension, duration of resuscitation, LVEF, and P/F ratio.


Our research shows that while DCD organ procurement is on the rise in the US, the percentage of procured lungs from potential donors is significantly lower in DCD patients compared to DBD patients despite similar post-transplant survival. The ambiguous reason for DCD lung discard demonstrates that DCD lung transplantation is still not the standard of care, likely related due to surgeons’ apprehensiveness and discomfort in transplanting these lungs. Hopefully, as trends of DCD lung use continue to rise, the recovery rate will grow in turn as surgeons become accustomed to these procurement practices. Studies like these and exercises to build consensus can help accelerate these efforts.
2 3
scientific insights,
part
J.Sam Meyer / Rabin Medical Center, IsraelQ. Where did you carry out your training?
I carried out my training under at the Rabin Medical Center in Israel the mentorship of Prof. Yaron Barac MD, PhD, Director of the Heart and Lung Transplant and Mechanical Circulatory Support Programme. I am an MD-PhD student at Tel Aviv University and Ben Gurion University of the Negev.

Q. What are your main areas of interest within cardiothoracic surgery?
Transplantation and specifically increasing donor pools through large-scale retrospective analyses of the UNOS database to promote DCD donation and optimise donor criteria. Additionally, as part of my PhD I am exploring various surgical technologies surrounding pointof-care 3D printing and personalised medicine in cardiothoracic surgery.
Q. What are your interests outside of your work?
I received my bachelor’s degree in Comparative English Literature and outside my work I enjoy spending time with my wife and son reading Shakespeare and Tolstoy at the beach!
“Hopefully, as trends of DCD lung use continue to rise, the recovery rate will grow in turn as surgeons become accustomed to these procurement practices.”
Aortic Expedition beyond the left subclavian artery - Light or Shadows
Brown 3
-
Practice of Neuromonitoring in thoracoabdominal aortic surgery –An international expert based Delphi consensus Study
T. Schachner, Innsbruck, R. Gottardi, Freiburg, J. Schmidli, Berne, J. Van Den Berg, Lugano, T. Wyss, Winterthur, M. Czerny, Freiburg
We conducted an international survey on the practice of thoracoabdominal aortic aneurysm (TAAA) surgery. Forty-six participating centres were located in 18 countries (Australia, Austria, Belgium, China, Finland, France, Germany, Hungary, Italy, Japan, South Korea, Netherlands, Norway, Poland, Portugal, Switzerland, United Kingdom, USA). There is still a great variability of technical details in this type of surgery. However, we found several aspects that were performed similar by a majority of participants. For example: the use of cerebrospinal fluid (CSF) drainage and cerebral near infrared spectrometry (NIRS). On the other hand, Motor Evoked Potentials (MEP), Somatosensory Evoked Potentials (SEP), and
Aortic Expedition beyond the left subclavian artery – Light or Shadows
Brown 3 08:15 - 09:45
Thomas Schachner / Innsbruck Medical University, Austria
Q. Where did you carry out your training?
Medical School at University of Vienna, Vienna, Austria. Training in Cardiac Surgery and Thoracic Surgery at Innsbruck Medical University.
paravertebral NIRS were used less frequently. We found different patterns of use with regard to the Crawford type of TAAA. We also saw variations within the management of the CSF drain: When is the CSF drain inserted? What is done in the case of a bloody puncture? What are the upper pressure limits of the CSF drain tolerated intraoperatively? When should we remove the CSF drain in the absence or presence of symptomatic spinal cord injury? Which professions are involved for monitoring and interpretations of MEP/SEPs?

We are looking forward to an interesting discussion on this topic.
Q. What are your main areas of interest within cardiothoracic surgery?
Aortic surgery, coronary surgery, heart valves.
Q. What are your interests outside of your work?
Health promotion for the general population, physical activity and training.
I finished my residency in cardiac surgery at the German Heart Center Berlin. And, I am currently undergoing further training as a vascular and endovascular surgeon.

Q. What are your main areas of interest within cardiothoracic surgery?
I am very interested in the open surgical and endovascular therapy of aortic diseases and work in this field at my clinic. Especially in the endovascular area, new treatment options are opening up for segments of the aorta that have traditionally been treated with open surgery. It is an exciting field that will offer further endovascular innovations over the coming years.

Single-centre experience with novel E-nside™ multibranched stent graft for thoracoabdominal aneurysms E-nside™ prosthesis (Jotec GmbH, Germany) is a novel pre-cannulated, inner branch based, off-the-shelf stent graft for repair of thoracoabdominal aneurysms.
It is a multibranched endograft with four antegrade oriented inner branches for the renovisceral vessels. It is designed to treat both elective and emergency cases with a consistent approach. Patient factors and comorbidities often make open surgery unattractive, leading to increased interest in endovascular solutions. However, only limited experience has been published so far.
We evaluated the use of the multibranched endograft in 13 patients in elective and emergency/ urgent admissions between December 2020 and April 2022. Mean age ± SD 71.9 ± 8,05 yrs, 8 female patients (61.5%).
Prior to E-nside™ implantation, 8 patients had undergone TEVAR of the descending aorta, 1 patient TEVAR of the aortic arch and 2 patients open “Frozen Elephant trunk” procedure.
During E-nside™ implantation, 8 patients needed extension of the proximally descending stents with endografts to ensure sufficient proximal stability.
E-nside™ implantation was successfully performed in 12 patients in a single-stage procedure. One E-nside™ implantation had to be completed in a two-staged fashion due to complex renovascular anatomy and prolonged fluoroscopy time.
An “all femoral” access with retrograde branch cannulation was performed in 7 patients. Axillary access was selected for branch cannulation in 5 patients. Conversion to axillary access occurred in 1 patient.
The inner branch for truncus coeliacus had to be closed with an Amplatzer II 12mm plug due to chronic occluded TC ostium in 3 patients.
Femoral access site complications with lower limb ischemia and operative revision appeared in 2 cases.


2 patients needed endovascular revision for type 2 and type 3 endoleak, respectively.
None of the 13 patients showed any signs of paraplegia postoperatively. Postoperative survival rate was 100%.
In conclusion, complex endovascular repair of thoracoabdominal aneurysms can be challenging. We implanted successfully the novel off-the-shelf, multibranched E-nside™ endograft in 13 patients in elective and emergency/urgent admissions.
Initial results look promising with 100% survival rate and no case of postoperative paraplegia.

Dr. med. Adam Penkalla / German Heart Center Berlin
Q. Where did you carry out your training?
TMVI for Beginners
(Vahanian A, Eur J Cardiothorac Surg 2021). However, adequate allocation of secondary MR patients to TEER remains controversial due to conflicting data of recent randomised trials (Stone GW, N Engl J Med 2018; Obadia JF, N Engl J Med 2018) and should be restricted to those patients who fulfil established “criteria suggesting an increased chance of responding to the treatment”.
to the notion that a rather large-bore TA device might represent a challenge for procedural safety especially since it is being used in more often than not thin-walled, hypokinetic MR ventricles, this TMVI system has demonstrated excellent procedural safety with an implant success rate of 97%, an apical access complication rate of only 1% and procedural mortality rate of 0% in an early series of 100 high-risk patients (Sorajja P, J Am Coll Cardiol 2019). This is most likely due to the tethered design, which allows for disintegration of annular sealing and apical fixation. The latter is achieved by an apical fixation pad which is firmly opposed onto the epimyocardial surface and acts like an additional hemostatant.
Transcatheter mitral valve implantation: transapical access and devices
During the past decades the therapeutic landscape has witnessed important additions to the armamentarium for treatment of mitral regurgitation (MR). Besides reconstructive mitral valve surgery, which continues to be the well established main stay for both primary as well as selected cases of secondary MR and which should preferably be performed in a minimally-invasive, endoscopic fashion, transcatheter therapies have gained ground for specific subsets of MR patients. Transcatheter edge-to-edge repair (TEER) has achieved widespread acceptance for high-risk patients ineligible for surgery and has received an upgraded recommendation for secondary MR in the recently updated ESC / EACTS guidelines for the management of valvular heart disease
The potential role of transcatheter mitral valve implantation (TMVI) is less established but holds the promise of combining decreased invasiveness of an off-pump approach with the effectiveness of surgery in complete resolution of MR. At present by far the most experience has been gathered using transapical (TA) TMVI devices and here, the Tendyne TMVI device (Abbott, Santa Clara, CA, USA; figure 1A) is clearly in the lead with > 1.200 patients treated to date worldwide. Contrary
Another system is the Tiara device (Neovasc, Richmond, BC, Canada; figure 1B) which is currently filing for CE mark. This device is available in two sizes and has three tabs for annular anchoring. In total, 83 patients have been treated mostly at North American and European sites. In an overall high-risk patient population with predominantly secondary MR, procedural safety has been excellent with 0% acute mortality. Complete resolution of MR was achieved in the vast majority of patients and only 2.5% of moderate MR at discharge.


The current bottleneck of TMVI appears to be the identification of anatomically suitable patients and most series are afflicted by a poor screen-toimplant ratio. This issue, as well as the desired transition from the more invasive TA to a fully endovascular transseptal delivery route, is among the most pressing future tasks.

Q. Where did you carry out your training?
I completed my training as a cardiovascular surgeon at the Italian Hospital of Buenos Aires.

Q. What are your main areas of interest within cardiothoracic surgery?
Heart transplant surgery and minimally invasive surgery.
Q. What are your interests outside of your work?
Swimming and oenology.
Hybrid approach treatment of arch aortic aneurysm in a high-risk patient: a two staged case report using Tevar after carotid-carotid and left subclavian-carotid bypass

Estrada Ronald MD; Posatini Ricardo MD; Raffaelli Pablo MD; Chas Jose MD; Rabellino Martin MD ; Kotowicz Vadim MD
In recent decades, hybrid arch repair has become an established treatment modality
among surgeons. This combined approach is a therapeutic alternative in high-risk patients with Thoracic Aorthic Aneuryms (TAA) and provides a less invasive and safer strategy, with a shorter convalescence, and minimal neurologic deficits. This treatment in separated stages is proposed to solve an unfavourable anatomy, and an inadequate proximal or distal landing zone (LZ).
The aim of this case report is to show a two staged treatment in a 66-year-old female with a diagnosis of Aortic Isthmus Aneurysm (AIA) and a previous history of Autoimmune Hepatitis, Scleroderma, STS score: 7.2 . Stages : a) carotid-carotid and left subclavian-left carotid bypass b) TEVAR in zone 1 of the aortic arch.
The Echocardiogram shows : LVSF was preserved without signs of pulmonary hypertension. AngioCT : AIA 72.4 x 57.3 mm in maximum diameter associated with a component of ulcerous and mural thrombus. (Fig. 1)
First stage: Side-to-side bypass with a 6 mm polytetrafluoroethylene (PTFE) graft passed through retropharingeous space between common carotíd rigth (RC) - carotid left (LC). (Fig. 2) Another 6 mm PTFE graft was passed through the lateral neck area avoiding the nerves (cevical plexus and frenic nerve) after opening scalen muscle. A side to side bypass between the left common carotid artery (LA) and left sublclavian artery (LSA) was performed. It provides an uncomplicated LZ of the TEVAR in zone 1 of the aortic arch. We preserved the vertebral artery and excluded a proximal LSA and LC to avoid posterior leaks.
Second stage: five days later, a 40x40x200 mm CTAG Active Control endoprosthesis was placed, released behind the emergence of the innominate trunk excluding the ulcerated lesion at the level of the aortic arch.

The angiography control shows a good permeability and the absence of leaks. (Fig. 2) Postoperative course was uneventful and the patient was discharged on the sixth postoperative.
Hybrid procedures for treatment of TAA are a promising alternative and a feasible option to open surgery especially in high-risk patients, with lower early morbidity and mortality rates.
Estrada Ronald Manuel / Italian Hospital of Buenos Aires
Gvido Janis Bergs / Hospital Clinic de Barcelona
Q. Where did you carry out your training?
I trained in cardiac surgery in Pauls Stradins Clinical University Hospital, in Riga, Latvia. This year, as the Francis Fontan Fellowship Fellow in Advanced Intensive Postoperative Care, I had the chance to train for four months in Hospital Clinic de Barcelona under the supervision of a great cardiac surgeon and fantastic person, Dr. Eduard Quintana. He also supported me throughout the process of creating the abstract for the EACTS Annual Meeting.
Q. What are your main areas of interest within cardiothoracic surgery?
It's early in my career as a cardiac surgeon, so I’m still in the process of formulating my main areas of interests in cardiac surgery. For now, I can say, that I’m more interested into aortic valve surgery, aorta surgery and congenital heart defect surgery in children and adults. Also, the time I spent in Barcelona has added surgical management of HOCM to my field of interests.
Q. What are your interests outside of your work?
Outside my work I try to be as physically active as I can. I enjoy running, cycling, playing tennis. During warmer months I often go kitesurfing and in winter I really like to go mountain skiing or snowboarding. I’m also a hunter. Hunting gives me a chance to spend time away from the crowd and noise, to be closer to nature.
Facing Challenges of Aortic Graft Infection
 Gvido Janis Bergs and Eduard Quintana Hospital Clínic – University of Barcelona
Gvido Janis Bergs and Eduard Quintana Hospital Clínic – University of Barcelona
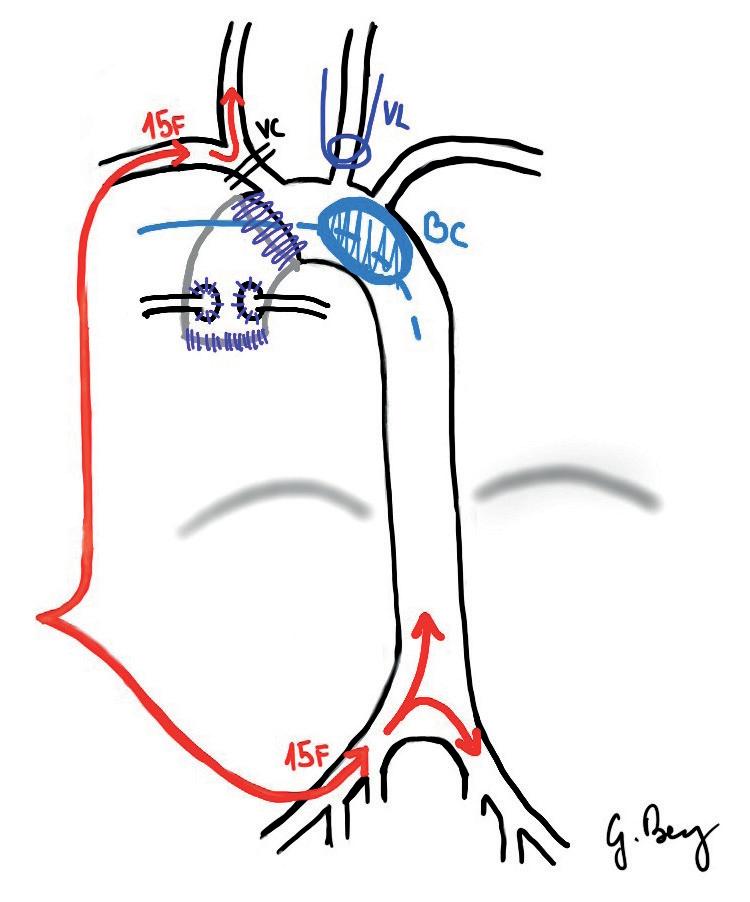
Thoracic aortic graft infection is rare but potentially a catastrophic complication after aortic surgery and there is no consensus regarding many aspects of management. When planning such reoperations there are several questions that need to be formulated. What is the best canulation strategy based on individual anatomy to institute CPB and maintain cerebral perfusion? What degree of hypothermia should be used to safely perform the procedure based on extend of aorta involvement? Is there a way to minimise visceral ischemia, duration of circulatory arrest and cardiopulmonary bypass times?
CT SURGERY RESIDENT
Figure 1: The drawing of whole body perfusion strategy: separate head and visceral-distal body perfusion instituted via two15F arterial cannulas inserted into axillary and femoral arteries. Separate circulation is accomplished via clamping the brachiocephalic trunk and left carotid artery, and occluding distal aortic arch with a balloon catheter to create bloodless operating field without interrupting visceral-distal body circulation.
Removal of all infected and suspicious tissue has always been the cornerstone of treatment. However, the best substitute material for vascular reconstruction is still a matter of debate, leading to institutional differences in practice. There are more unsolved questions related to the next phase of treatment: should patients be left with open
chest for multiple debridements/washouts or be primarily closed? Is there a real need for prolonged antibiotic regimes?
Herein we present a case of late mediastinitis after proximal aorta repair, highlighting a reproducible whole body perfusion strategy (see Fig 1), which may minimise end-organ injury, vasoplegia and coagulopathy usually seen in cases where moderate-to-deep hypothermia and interruption of lower body perfusion is applied to reconstruct the aortic arch. To maintain perfusion to the entire body and avoid long use of hypothermia, two separate 15F arterial cannulas – right axillary and right femoral artery – were used. After the management of aortic valve prosthesis and aortic root, the brachiocephalic trunk and left carotid artery were clamped and axillary perfusion initiated. A brief period of less than 5 min of lower body perfusion interruption of flow to explore the aortic arch was followed with positioning of a 40mm Reliant® stent graft balloon catheter in the distal aortic arch (zone 3). Visceral-distal body perfusion was reinstituted via femoral perfusion and immediate rewarming started. Resection of infected aortic prosthesis and surrounding tissue was performed afterwards. Subsequently, a distal anasthamosis (hemiarch-type) was created and stent graft balloon catheter was removed, reestablishing perfusion to the remaining epiaortic vessels. The patient had normal lactate levels throughout the entire operation and was transferred to cardiac ICU with open chest for mediastinal washouts and had a delayed sternal closure.
We believe that this perfusion strategy can minimise biological derangements caused by long periods of moderate-to-deep hypothermia, visceral circulatory ischemia and extended CPB in septic patients, therefore potentially improving outcomes. Equivalent strategies could be utilised in selected patients requiring different extends of arch replacement based on endovascular occlusion feasibility.
Get ready for a Jeopardy-style competition of cognitive skills. Two-person teams of residents will face off against one another in a test of knowledge in five cardiothoracic surgery categories – cardiac, congenital, thoracic, history of the specialty, and decision making.
Come and support this year’s teams, including:
• Henri Haapanen and Tommi Järvinen, Helsinki University Hospital
• Konstantinos Papakonstantinou and Filippos-Paschalis Rorris, Evangelismos General Hospital
• Alissa Florian and Polina Mantaj, Medical University of Graz
• Sam Heuts and Jules Olsthoorn, Maastricht University Medical Center+

• Carolina Mayor Deniz and Consuela María Sisinni Ganly, Álvaro Cunqueiro University Hospital
• Nebil Ajmi and Abdulrahman Aljuayli, Toulouse University Hospital
Q. Where did you carry out your training?
I trained in cardiac surgery at the Cardiac Surgery School of the Second University of Naples, Italy

Q. What are your main areas of interest within cardiothoracic surgery?
Surgery of the aorta and aortic valve, including aortic arch procedures, aortic repair and valve sparing operations, aortic valve replacement with minimally invasive access. Although I like performing every kind of surgical procedure in this discipline, I am particularly interested in surgery for the chronic and acute diseases of the aorta, which are also the main focus of my research and teaching work.
Q. What are your interests outside of your work?
I like travelling. In my spare time I love reading, listening to music and playing the piano – and when I am home I also enjoy cooking for friends, family and loved ones.
How aortic geometry can predict the evolution of the aortopathy in bicuspid and tricuspid aortic valve patients: a multi-centre study
Elective aortic surgery aims to prevent acute complications of aortopathies, namely rupture and dissection. Prophylactic aortic replacement is indicated on the basis of dimensional criteria, i.e. the maximal diameter and growth rate. However, most acute type A aortic dissections (ATAADs) occur with a diameter smaller than the recommended cut-off of 55mm. Therefore, further candidate criteria for risk estimation of AAEs have been focused on, also including the elongation and angulation of the aorta (from the valvular plane to the brachio-cephalic trunk origin).
In a previous study, recently published in the EJCTS, we have highlighted that although elongation accompanies both aneurysms and ATAADs, an associated narrowing of the ascending-arch angle is uniquely observed in ATAADs. In that pilot study, an ascending-arch angle <130° was present in all ATAAD patients.
Since bicuspid aortic valve (BAV) is a known risk factor for ATAAD, as a follow-up to that study, we collected 354 angio-CT scans of the aorta from three Italian cardiac surgery Centres (including 97 non-aneurysmal aortas, 100 aneurysms and 157 dissections), now focusing on differences between BAV and tricuspid aortic valve (TAV) patients. When comparing the two groups in terms of clinical characteristics and geometry of the aorta, we found that the ascending tubular tract diameter and length were significantly greater in BAV non-ATAAD patients vs TAV nonATAAD patients, whereas they were similar in BAV+ATAAD as TAV+ATAAD. The length of the
root tract was significantly greater in BAV than in TAV patients only in the ATAAD group (p=0.009), consistent with a significant clustering of root phenotype in the BAV+ATAAD subgroup. This configuration of the aorta was typically associated with narrower ascending-arch angle even in nonATAAD patients. In TAV non-ATAAD patients, the ascending-arch angle was significantly correlated with the length of the root tract (r=-0.39; p<0.001), less robustly with the diameter at sinuses and sino-tubular junction and with the total length of the aorta. In BAV non-ATAAD patients, the only significant correlation was with the length of the root (r=-0.39; p=0.008).


While elongation of the aorta may be a nonspecific marker of aortopathy, the narrowing of the ascending-arch angle (and the root-phenotype with BAV) seem to have a potential as risk markers for ATAAD.
“In a previous study, recently published in the EJCTS, we have highlighted that although elongation accompanies both aneurysms and ATAADs, an associated narrowing of the ascending-arch angle is uniquely observed in ATAADs.”
this the best
Alessandro Della Corte / University of Campania “Luigi Vanvitelli”Figure
Brown
20-year follow-up of Aortic Valve
Reimplantation using the Valsalva graft
Ilaria Chirichilliab, Raffaele Scaffaa, Francesco Giosuè Iraceab,c, Andrea Salicaa, Luca Paolo Weltertad, Salvatore D’Aleoa , Luigi Chiariellof, Ruggero De Paulisa,g
a Department of Cardiac Surgery, European Hospital, Rome, Italy
b Department of Cardiac Surgery and Heart Transplantation, San Camillo Forlanini Hospital, Rome, Italy
c Department of General and Specialized Surgery “Paride Stefanini”, Sapienza University, Rome, Italy
d Department of Statistics, UniCamillus International University of Health Sciences, Rome, Italy
f Cardiac Surgery Unit, Mediterranean Clinic, Naples, Italy g Chair of Cardiac Surgery, UniCamillus, International University of Health Sciences, Rome, Italy
Over the past 20 years valve-sparing root replacement has aroused increasing interest because of a progressive attitude towards the preservation of natural tissue. Aortic Reimplantation is the most used technique to spare the valve, allowing simultaneously aortic root replacement and aortic annular stabilisation. The Reimplantation into a graft with sinuses guarantees an optimal anatomic and functional reconstruction with established good results at 15 years. The aim of this study is to report the world's longest follow-up (20-years) of aortic valve Reimplantation using the Valsalva graft.
From February 2000 to December 2021, 265 consecutive patients with aortic root aneurysm received Reimplantation using the Valsalva graft. The mean age was 52.9 ± 13.4; 18.9% had a bicuspid aortic valve and 55.9% an aortic regurgitation ≥2+. From 2016 leaflet plication with the routinary use of Caliper was performed. The mean follow-up was 85 ± 63 months.
Overall survival was 83.7 ± 5.1, freedom from cardiac death 99.6 ± 0.4, freedom from recurrent AR ≥ 3+ and reoperation was 91.9 ± 2.3 and 95.5 ± 1.9, respectively. At 20 years, reoperation-free survival was 79.6%. There was a minimal incidence of infective endocarditis, thromboembolism and hemorrhage. All patients requiring reoperation had surgery within the first period of experience. At multivariate analysis, an early sub-optimal result and an associated leaflet repair before the introduction of a routinary use of a Caliper, had a negative effect on residual aortic regurgitation.
In conclusion, the first 20-year follow-up of aortic Reimplantation using the Valsalva graft demonstrated excellent results in terms of recurrent aortic regurgitation, reoperation and cardiac death, and a minimal incidence of infective endocarditis, thromboembolism and hemorrhage.
Long-term results, already improved according to the learning curve, have further improved after the routinary use of a Caliper. Indeed, we found a significant stability of the aortic valve competence when the eH was ≥ 9 mm. Even if the aortic Reimplantation was born as a complex procedure, its standardisation over the years and the use of objective parameters, have allowed it to be simplified, making it a routine operation in experienced hands with excellent and durable long-term results.
Figure 1: 2a (left): Schematic drawing of aortic valve
Reimplantation using the Valsalva graft. 2b (right): Intraoperative picture of aortic valve Reimplantation of a Tricuspid Aortic Valve.

Ilaria Chirichilli / Department of Cardiac Surgery and Heart Transplantation, San Camillo Forlanini Hospital, Rome, Italy and Department of Cardiac Surgery, European Hospital, Rome, Italy

Q. Where did you carry out your training?
While undertaking my medical studies in Rome, I had two foreign experiences: the former in Lugano-Switzerland with Prof. F. Siclari at the Cardiocentro Ticino, the latter in the Research Laboratory for the Study of Grafts and Cardiac Prostheses of the Broussais Hospital of Paris with Prof. Alain Carpentier and Prof. J.C.Chachques. I graduated and completed my residency at the “University of Rome La Sapienza”. In 2014 I joined a team directed by Prof. Ruggero De Paulis, focusing on aortic valve-sparing procedures, aortic arch surgery and aortic valve repair. Since October 2019 I have been working in the Department of Cardiac Surgery and Transplantation of S. Camillo Hospital of Rome, directed by Prof. Francesco Musumeci, particularly focused on minimally invasive programmes for valve surgery and transcatheter procedures.
Q. What are your main areas of interest within cardiothoracic surgery?
My area of interest is represented by aortic valve including aortic valve repair (EACTS Task Force Member since 2020), ascending aorta and aortic arch surgery.
Q. What are your interests outside of your work?
Classical and modern dance, and foreign languages. I love travelling.
Figure 2: 2a (left): Freedom from reoperation. 2b (right): Freedom from recurrent aortic regurgitation ≥ 3+.
Figure 3: Aortic valve reoperation-free survival and the competing risk (cumulative incidence function) for reoperation on the aortic valve and death (without reoperation) in the overall cohort.


Francesco 'Giosuè' Irace / Department of Cardiac Surgery and Heart Transplantation, San Camillo Forlanini Hospital, Rome, Italy and Department of Cardiac Surgery, European Hospital, Rome, Italy
Q. Where did you carry out your training?
I graduated in 2012 as a medical doctor at the Sapienza University of Rome. In 2013 I started the Cardiac Surgery residency, working at the Policlinico Umberto I of Rome (Sapienza University), Salam Center for Cardiac Surgery of Khartoum (Emergency ONG) and European Hospital of Rome. In 2018 I graduated as a Cardiac Surgeon; after finishing my residency I completed my training focused on aortic valve repair and aortic root valve sparing procedures at the European Hospital of Rome. In 2022 I obtained a PhD in Angio-Cardio-Thoracic Pathophysiology and Imaging. Currently, I am staff surgeon at Department of Cardiac Surgery and Heart Transplantation of San Camillo-Forlanini Hospital of Rome.

Q. What are your main areas of interest within cardiothoracic surgery?
My areas of interest are heart valve surgery and aortic reconstructive surgery.
Q. What are your interests outside of your work?
Skiing and travelling.
FRIDAY
R. Milton, Leeds, J. Hörer, München, N. Hussein,


J. Bavaria,
B. Keogh,
E.

P. Sardari
J. Kluin, Amsterdam, M. Grabenwöger, Wien, F. Melfi, Pisa, A. Zientara,

N.

EACTS LEARNING
GET ‘HANDS-ON’ IN THE EACTS LEARNING LAB

Learn specialist techniques and draw on the knowledge of some of the world’s most experienced and expert surgeons with the EACTS Learning Lab training sessions. These ‘hands-on’ workshops include wet and dry labs and other small practice sessions. These can only be purchased upon registering for the 36th EACTS Annual Meeting and are available to book now.
THURSDAY 6 OCTOBER
AV Repair
Learn about the two main techniques for valve sparing aortic root surgery: reimplantation and remodelling. You will have the opportunity to learn the pitfalls of this technique on a model, ask questions and seek advice from our experienced faculty. Please note that delegates must choose either reimplantation OR remodelling – both sessions will run concurrently.
Surgical strategy in complex congenital heart disease
Understand complex cardiac malformations with the use of 3D printed models. Develop surgical strategy for repair of complex cardiac malformations.
Discuss alternatives for biventricular repair with left systemic ventricle.
Mitral Valve
Receive basic training on mitral and tricuspid valve access, repair and replacement.
FRIDAY 7 OCTOBER
TAVI/TMVR Simulator Session
Touch and play with guidewires, valves, delivery systems and simulators and take a fascinating journey through the latest transcatheter valve devices and technologies.
TEVAR Simulator Session
Come and practise your skills with our hands-on training on endovascular stent graft thoracic aortic treatment.
Thoracic Surgery
Learn how exponential technologies (including artificial intelligence, virtual reality and computational modelling) contribute to surgical planning and intraoperative image-guidance of anatomical (sub)lobar resections. In addition, patient-specific virtual reality (VR) simulators will be used to highlight the added value of VR for both surgical planning and surgical training/educational purposes. The educational focus will be on pulmonary lobar and segmental bronchovascular anatomy from a surgical perspective.
SATURDAY 8 OCTOBER
Coronary Surgery
Learn how to perform coronary anastomoses and the techniques for proximal and distal anastomoses, sequential and composite grafts. Techniques and devices for conduit harvesting and
will also be presented.
09:00 – 11:00
12:30 – 14:30
15:30 – 17:30
09:00
12:30
15:30
09:00
OPTIMISING PERIOPERATIVE CARE
Eighty per cent of cardiac surgical morbidity occurs outside of the operating room, according to figures from the Cardiac ERAS (Enhanced Recovery After Surgery) Society. Many of the complications that can impact on a cardiac patient’s quality of life, such as anemia or wound infection, occur following discharge or in the later days of their recovery.
ERAS is a multidisciplinary approach to optimising perioperative care through an evidence-based protocol in order to deliver improved patient safety, sustained quality of life and better longterm outcomes.
Marjan Jahangiri, Professor of Cardiac Surgery at St George’s Healthcare NHS Trust and Vera von Dossow, Professor of Anesthesiology and Critical Care Medicine at the Heart and Diabetes Center Bad Oeynhausen, Ruhr-University Bochum discuss the impact of Cardiac ERAS strategies on patient care.

What are some of the key strategies that should be implemented by heart teams in order to optimise the perioperative pathway for cardiac patients?
Professor Jahangiri - The ERAS perioperative care bundle is organised into the three phases of care – pre-, operative and post-operative. During all these phases there are steps we can take to optimise patient care. For example, in the preoperative period patients who are chronic smokers will benefit from a few days of nebulisation in order to optimise the pulmonary function.
There are also strategies we can implement in the operating theatre to optimise patient care such as keeping operations shorter, ensuring the patient’s body temperature is not too low, and maintaining hemoglobin and acid base with the help of perfusion scientists. We also need to pay attention to good neurological recovery using infrared spectroscopy and keeping good perfusion pressure. Making sure the hemodynamic monitoring is accurate will help.
Prof. Dr. med von Dossow – The ERAS concept in cardiac surgery is still very young. In order to implement an ERAS programme several steps are required. The first step is to define outcome measures such as length of hospital stay, or more patient-related outcomes measures such as quality of life. It is then important to achieve interdisciplinary consensus between all participating professionals in the hospital in cooperation with general practitioners.
The third step is to build a core team and to define and determine evidence-based strategies such as risk stratification, which includes frailty assessment, nutrition assessment and delirium screening in the pre-operative period. This approach allows us to plan a strategy for the whole perioperative setting so cardiac patients receive a co-management approach. It is also important to include patients in the shared decision-making process.
For anesthesiologists the major proven goals to optimise perioperative care include early extubation, less sedation after surgery and multi model pain therapy. These goals are easy to implement in a cardiac surgical setting.
How can surgeons and anesthesiologists work together to help improve the care and recovery of cardiac patients?
Professor Jahangiri - The evolution of cardiac intensive care means that there is now a whole specialty team, and this has encouraged shared responsibilities. We have learnt the importance of collaboration. Although a lot of our working practices have already been established, the ERAS model has put it in writing by providing well defined evidence-based bundle of care for the whole team to follow.
Prof. Dr. med von Dossow – Cardiac surgeons and cardiac anesthesiologists have worked closely together for many years, so cooperation is already very good. Surgeons and anesthesiologists should discuss their patients in more detail prior surgery and should involve patients in the shared decisionmaking process, not only one day prior to surgery when patients are admitted to the hospital. It is important that the multidisciplinary team actively participates in the ERAS programme and team members have defined roles in order to effectively implement the different ERAS strategies and process steps.
What are the main success factors in the perioperative period to consider when starting a Cardiac ERAS programme?
Professor Jahangiri - Early extubation is really important. It immediately reduces the hemodynamic requirement and that can be assisted by the new and novel optimum hemodynamic monitoring. The management of anemia and renal dysfunction are also important factors.
Prof. Dr. med von Dossow – Post-operative complications can only be prevented if dependent steps are in place. The first step is risk stratification and then putting in place prevention strategies. Monitoring is important for patient safety, for example monitoring cerebral function and hemodynamic function and then have a plan of intervention in place.
Why is it important for heart teams to deliver more individualised patient care?
Professor Jahangiri – Providing individualised patient care reduces complications. For older patients an assessment of frailty is important and a consideration of other factors such as whether the patients live alone or have support at home. Patients who don’t live alone tend to do better post-operatively.

Prof. Dr. med von Dossow - Patients are becoming more complex due to demographic changes and co-morbidities. In addition, older patients have heart insufficiencies, so we have to consider hemodynamic instabilities throughout the whole perioperative pathway. It is important to have an individualised hemodynamic protocol for every patient. The means that risk stratification includes not only a cognitive and functional assessment but also a hemodynamic profile of the patient.
What role can innovative technology and techniques play in driving improvements to patient safety and improving outcomes for patients?
Professor Jahangiri – Advances in monitoring in the operating theatre are supporting improvements in patient safety, for example the newer perfusion monitoring and the neuromonitoring to keep adequate oxygenation. The most important technological contribution in the operating theatre is the minimal hemodynamic monitoring which is less invasive than the swan pulmonary artery catheter, which was previously used.
Prof. Dr. med von Dossow - Artificial intelligence and early risk alarming systems are of major importance in the future. Patients are becoming older and more complex, therefore AI systems such as delirium risk or renal dysfunction risk assessment systems can help to preassess the patients a status. Early warning systems like predictive hemodynamic monitoring support us to take the right clinical decision in the perioperative phase and are of crucial importance for a stable intraoperatively blood pressure management.
AI alarm systems to monitor blood pressure alterations can help and support a more proactive strategy. This is especially useful for healthcare professionals such as nurses and younger doctors who are yet to develop a feeling for deterioration of patients. The Hypotension Prediction Index™ software might be a helpful tool, not only for patient safety but also for professionals who are not familiar with hemodynamic instabilities such as in cardiac surgery.
SATELLITE SYMPOSIA
Satellite symposia, organised by some of our industry partners,
an opportunity to learn more about new-to-market

state-of-the-art products, innovations and developments in the cardiothoracic market.







sponsored
THURSDAY
OCTOBER
not form
of
scientific
of
Room: Amber 5 Innovative strategies for superior outcome in Cardiac Surgery including pMCS support
therapy
Room: Botticelli Beyond the hemiarch: a simple therapy for Acute Type A Dissections
Room: Amber 4 A patient-centric approach for AF treatment
Room: Amber 1 & 2 Surgical Site Infections in cardiac surgery: optimizing prevention
Room: Brown 3
12:45-14:00
18:00-19:15
FRIDAY 7TH OCTOBER
12:45-14:00
of the art in the treatment of aortic valve regurgitation in young patients
Room: Amber 3 Mission (Im)Possible – Four Cornerstones for Success in Cardiac Surgery


Room: Michelangelo Cardiac Surgery time machine: get ready for the future!
Room: Brown 1 Routine Quality Assessment in CABG and Aortic surgery
Room: Brown 2 CARL. Controlled Automated Reperfusion of the whoLe body – A new concept treating patients with cardiac arrest



Room: Amber 4 Bright future for vein grafts: techniques and technologies to improve the clinical outcome of CABG
Room: Brown 2 From Established to Advanced Heart Failure Therapies and Technologies that Change Lives
Room: Amber 3 Choosing the most appropriate treatment option for arch pathologies
Room: Amber 4 Hemoadsorption with CytoSorb in high-risk cardiac surgery indications – new data


Room: Brown 3 Aortic valve disease: Patient centric management in elderly population
Room: Michelangelo TOP secrets you need to know for Your Success in SAVR
Room: Amber 1 & 2 Thoraflex Hybrid: Gold Standard
SATURDAY 8TH OCTOBER
12:45-14:00
WOMEN
Room: Raphael EBCP Annual Meeting / 22nd EcOPEaT / Milan
CARDIOTHORACIC SURGERY
Open to all who support
advancement of
in cardiothoracic

3-D Matrix A04 Abbott B12
ABIOMED B10
Advancis Surgical C06
American Association for Thoracic Surgery (AATS) A30
AMT Medical B.V. C32
Andocor NV B24
AngioDynamics A16
Artivion EMEA GmbH B14
Artivion EMEA GmbH - Learning Lab C03a
Asanus Medizintechnik GmbH C13
AtriCure Europe B.V. B16
AtriCure Europe B.V. - Learning Lab B02
BD Interventional - Becton Dickinson A09 & A11
BioCer Entwicklungs-GmbH C18
Bio Sud Medical Systems Srl A03bis
Cardia Innovation AB A23
Cardio Medical GmbH C20
CARL. B20
CARMAT A10
Chalice Medical Ltd B26
Cook Medical Europe LTD B07
Corcym S.r.l. B08
CTSNet.org A28
CUI INTERNATIONAL LIMTED A06
CytoSorbents Europe GmbH B21 & B23 & B25
Delacroix-Chevalier C22&C24
Dendrite Clinical Systems Ltd A25
Dr. Franz Koehler Chemie GmbH C15 & C28
EACTS - The European Association For Cardio-Thoracic Surgery C13
EACTS - Learning Lab C01
EACTS - TV Studio A17
Edwards Lifesciences C09
EpiHeart Oy C34
Eurosets s.r.l. C07
Exstent Limited B31
Fehling Instruments GmbH & Co KG C21 & C23
FIAB Spa B27 & B29
Foldax, Inc. A21
GEISTER Medizintechnik GmbH B06
Genesee BioMedical Inc A15
HAART- Aortic Valve Repair Technologies by BioStable Science & Engineering C17 Hemonart Medikal Sistemler Sanayi Ticaret A.S. A12
ISMICS/HVS (International Society for Minimally Invasive Cardiothoracic Surgery & Heart Valve Society) A01 & A03 Jafron Biomedical Co., Ltd. A07BIS Jarvik Heart Inc C19
Johnson & Johnson Medical Devices Companies A14 Kapp Surgical Instrument, Inc. A05bis KLS Martin Group A08 & B09 LifeTec Group A19 LSI Solutions A18 & A20 Medela AG B05 Medistim ASA B04
Medtronic International Trading SÁRL C05 Medtronic International Trading SÁRL - Learning Lab C03 Meril Endo Surgery Pvt Ltd C02 & C04
NEOS SURGERY C30
Osypka AG B03
Oxford University Press B33 Peters Surgical B04a PHOENIX s.r.l. B11
POSTHORAX ltd. B01 Qualiteam s.r.l. B19
REDAX Spa B15 & B17
Scanlan International, Inc C08 & C10 & C12 & C14
STS-The Society Of Thoracic Surgeons A27 Sunoptic Technologies A02
Terumo Aortic & Terumo Europe N.V. B18 Thompson Surgical Instruments, Inc.
tisgenx, Inc.
Systems, Inc.
EMPOWERING WOMEN SURGEONS
Women in Cardiothoracic Surgery Committee
Join the Women in Cardiothoracic Surgery (WiCTS) Committee for the workshop ‘Embodied Leadership: The Hidden Dimension’ taking place today at 18.00.

The empowering workshop, which is inclusive to both men and women surgeons, will examine what defines impact, particularly in leadership, and explore gender bias in cardiothoracic surgery. Introduced by incoming EACTS Secretary General, Patrick Myers, and hosted by leadership and diversity expert, Dr. Mira Vasic, participants will have an opportunity to take part in practical exercises to practise presence and calm for more confidence and resilience.
Professor Jolanda Kluin, Chair of the WiCTS Committee, said, “It can be easy to judge people’s abilities based on how they present themselves but in doing so there is a risk that we will miss very talented people who are highly capable of taking leadership positions. This session is beneficial for both men and women surgeons; it will encourage participants to consider how bias may impact our relationships with others, but also help us examine how the way in which we present ourselves can exacerbate such bias. The bottom
line is recognising how different personalities can become impactful leaders.”

The workshop will be followed by a networking session. Professor Kluin says, “As women surgeons we must not underestimate the importance of building a network. A good network not only supports career progression, but it can help you learn more about surgical techniques or advice about leadership positions. It’s also fun to meet and talk to people."
The WiCTS committee recently launched a new thought-provoking webinar series “the changing face of leadership: moving from diversity to inclusion” which blends theory with practical information from experts and guest speakers with discussions on the changing face of leadership and women’s challenges and roles in the current landscape. The series offers tools to gain and maintain influence and leadership as a cardiothoracic surgeon.
For more information about the webinar series go to www.eacts.org/resources/women-in-cardiothoracic-surgery/



Thoracic innovation
Brown 1
10:15 - 11:45
Introduction of Artisential Surgeonpowered robotics in video-assisted thoracoscopic surgery (VATS): Experiences, indications and techniques.
Robotic Assisted Thoracic Surgery (RATS) offers outstanding precision via robotic wristed instruments, but robotic platforms are expensive and are not accessible to every surgeon and every patient at all times; moreover, the surgeon is unscrubbed away from the patient’s side without haptic feedback. With the new Artisential instruments, the most important feature of roboticassisted surgery – the free articulation of the instrument tip – has been successfully incorporated into a purely mechanical cost-effective instrument.
Through the double-joint structure of the end effector, these hand-held instruments offer a 360 degree of freedom and an articulation and dexterity comparable to a daVinci robotic platform while preserving tactile feedback directly by the patient’s side.
Here, we report our recent experiences with these articulating instruments in video-assisted thoracic surgery (VATS) during the first 16 months of use. Indications and benefits are highlighted and technical features of the application such as the trocar positions as well as practical issues for training with these instruments are discussed.
From April 2021 – August 2022, more than 100 minimally invasive procedures have been
Thoracic Innovation
Brown 1 10:15 - 11:45
PulmoVR: leveraging virtual reality and artificial intelligence for advanced surgical planning.
Traditionally, management of patients with earlystage non-small cell lung cancer (NSCLC) consisted of a lobectomy. However, over the past few years, there has been an increasing interest and shift towards lung-sparing segmentectomy procedures.
On top of that, segmentectomy for small (<2cm) stage I NSCLC has been proposed by various groups and the results of a phase III randomised controlled trial (JCOG0802, comparing lobectomy versus segmentectomy) showed a better 5-year overall survival1. Pulmonary segmentectomies are generally more challenging for surgeons, as a thorough and deep understanding of the segmental anatomy is necessary for identification, isolation, and division of the segmental vessels and bronchi. Patient-specific bronchovascular variations increase complexity even further.
Identifying intersegmental divisions and reviewing (segmental) branches of pulmonary arteries, veins, and bronchi on two-dimensional (2D) computed tomography (CT) can be difficult. Immersive virtual reality (VR) could contribute to a better understanding of patient-specific CTscans, by enabling an in-depth and 3D view of the intrathoracic anatomy by using head mounted displays. Several articles in other fields of surgery have already shown the added value of VR in pre-operative planning 2. In 2019, we have codeveloped (together with MedicalVR, Amsterdam) a VR and artificial intelligence (AI)-platform (PulmoVR) to facilitate on-site pre-operative

Dr Alexander Kern / Department of Thoracic Surgery, Fachkrankenhaus Coswig, University Hospital Dresden, Germany

Q. Where did you carry out your training?
• Department of General, Visceral and Transplantation Surgery, University Hospital Jena, Friedrich-Schiller University Jena, Germany
• University of the Witwatersrand, Johannesburg, South Africa
• Department of Visceral, Thoracic and Vascular Surgery, University Hospital Dresden, Germany
performed in our department using the wristed instruments through a duo/triportal approach. We have analysed early outcomes of Artisentialassisted anatomic lung resections, thymectomies and diaphragm plications. Thanks to the articulation, especially lymphadenectomy and dissection during mediastinal resections could be carried out much more precisely, more completely and more clearly compared to conventional VATS with straight and rigid instruments.

Multiportal VATS with articulating instruments is a safe procedure with good perioperative results. Especially the ability to angle the instruments to 90 degrees in all directions with improved ergonomics enabled accurate dissection of the
• Department of Thoracic Surgery, Fachkrankenhaus Coswig, Germany
Q. What are your main areas of interest within cardiothoracic surgery?
Lung cancer: minimally invasive anatomic lung resections, bronchoplastic/angioplastic lung resections, mediastinal tumors; minimally invasive mediastinal resections, laser resection of metastases
Q. What are your interests outside of your work?
Family, my sons. I like hiking and endurance sports, Kung Fu, yoga and meditation. I also enjoy travelling and reading.
lymph nodes and mediastinal tumors, with clear superiority to standard VATS instruments.
Amir H. Sadeghi / Thoraxcenter, Department of Cardiothoracic Surgery, Erasmus University Medical Center, Rotterdam, The Netherlands

Q. Where did you carry out your training?
Currently, I am the chief resident of cardiothoracic surgery at the Erasmus University Medical Center, in Rotterdam, the Netherlands.
planning in 3D. We have already published the results of our clinical feasibility study, in which we demonstrated a 40% change in surgical plan, when comparing conventional CT-guided planning of a segmentectomy vs. immersive VR-guided planning3.
More recently, we have also analysed the results of our first consecutive 50 patients undergoing PulmoVR-guided VATS segmentectomy. Moreover, we have trained a deep learning algorithm to be able to perform automated segmentations of the pulmonary arteries, veins, and bronchi.
During this thoracic innovation session, I will share the results of our follow-up clinical studies and will present the AI-based developments that allow us to perform on-site 3D analyses (segmentations) of patient-specific CT-scans. In addition to that, I will present how we leverage VR and stereoscopic 3D technology in daily practice. Finally, I will present some preliminary results of our recently developed PulmoSR (simulated reality) platform
Q. What are your main areas of interest within cardiothoracic surgery?
I did a PhD on the applications of virtual reality in the field of cardiothoracic surgery. Currently, my focus of research is on advanced surgical planning strategies and surgical simulations by using virtual reality, artificial intelligence, and stereoscopic 3D technology.
Q. What are your interests outside of your work?
I have a passion for innovation, technology, and I am interested in entrepreneurship. Besides my professional activities, I like to travel, watch movies, and be around friends and family.
which enables interactive, dynamic, soft-tissue simulation of patient-specific virtual lungs.
Transcatheter tricuspid valve intervention: all you need to know
Amber 1 & 2
10:15 - 11:45
Interventional Imaging of the tricuspid valve: patient selection and procedural guidance
The recent advancement of transcatheter tricuspid valve interventions (TTVI) present several anatomical (wide anatomical variability, large coaptation gaps, difficult visualisation) and physiological challenges (mechanism and definition of tricuspid regurgitation [TR] severity, consequences on right heart chambers).
Characterising morphologic and/or functional abnormalities that result in TR is an essential aspect of appropriate TTVI device selection, and a standardised approach using 3D transthoracic or transesophageal echocardiography (TEE) is required in all cases. TTVI techniques not involving leaflet approximation (annuloplasty, orthotopic and heterotopic transcatheter valve implantation) require additional pre-procedural cardiac computerised tomography (CCT) assessment of TV annular/subvalvular anatomy and right atrial/caval dimensions.
Q. Where did you carry out your training?
Q. What are your main areas of interest within cardiothoracic surgery?
ABSTRACT SESSION
Single Ventricle and Fontan Circulation
Long-term survival is superior in patients with pulsatile pulmonary blood flow after the Fontan-Björk procedure
Lukas Klemm1, Paul Philipp Heinisch1, Helena Staehler1, Christoph Röhlig 2 , Christian Meierhofer2 , Alfred Hager2 , Peter Ewert 2 , Jürgen Hörer1, Masamichi Ono1
1. Department of Congenital and Pediatric Heart Surgery, German Heart Center Munich, Technische Universität München, Munich Germany, Division of Congenital and Pediatric Heart Surgery, University Hospital of Munich, Ludwig-Maximilians-Universität, Munich, Germany
Department of Congenital Heart Disease and Pediatric Cardiology, German Heart Center Munich at the Technical University of Munich, Munich, Germany
The Fontan-Björk procedure is a unique modification of the classic Fontan procedure, which includes the right ventricle (RV) into the pulmonary circulation and is mainly performed on patients with tricuspid atresia. In some patients, the RV grew over the follow-ups, providing a RV-dependent pulmonary circulation. This study aims to evaluate the clinical outcomes and haemodynamic variables late after the Fontan-Björk procedure, regarding their pulmonary flow pattern. According to the pulmonary flow pattern by pulsed-wave Doppler assessment of echocardiography, 43 patients who survived more than 15 years after the Fontan-Björk procedure were divided into two groups: patients with pulsatile systolic pulmonary flow (Group P, n=13), and those without (Group N, n=30). Main diagnosis included 41 tricuspid atresia/stenosis and two double inlet left ventricles. Median age at Fontan-Björk procedure was 5.7 (2.1-7.3) years
• Medical School at St. Bartholomew’s Hospital London
• Cardiology at The Royal Brompton Hospital London
• Echo training (transthoracic, stress, TOE) at The Royal Brompton Hospital London.
Dr. Alison Duncan / The Royal Brompton Hospital, London Masamichi Ono / Department of Congenital and Pediatric Heart Surgery, German Heart Center Munich, Germany


• Procedural image guidance for surgical mitral valve repair (pre- , peri-, and post)
• Image guidance for transcatheter valvular heart disease, initially TAVI, now mitral edge-toedge repair, transventricular neochord repair, transcatheter mitral valve implantation (transapical and trans-septal), tricuspid edge-to-edge repair, transcatheter tricuspid valve implantation.
Q. What are your interests outside of your work?
All things Irish ! My parents were Irish, and I love Irish music, culture, and stores, Irish dancing, and Irish rugby. And I am learning to speak French so I can converse with my French nephews.
Peri-procedurally, the key to successful TTVI is excellent communication and understanding between TV interventional echocardiographer and interventionalist. This requires mutual knowledge on imaging, devices, and procedural steps. Standardisation of right chamber views using the “attitudinal” orientation and nomenclature (whereby the display and relationships of the TV leaflets with adjacent cardiac structures remain identical irrespective of the imaging modality)
provide the basis for a common language within the peri-procedural heart team. In patients with insufficient imaging quality, the use of intracardiac echocardiography (ICE) is helpful and will increase as novel 4D catheters allowing for 3D imaging and multiplanar reconstruction become broadly available. Current and future tools to fuse CCT, fluoroscopy and echocardiographic imaging modalities in real-time may assist some procedures.
Lukas Klemm / Department of Congenital and Pediatric Heart Surgery, German Heart Center Munich, Germany

and median follow-up was 32 (28-36) years. In 43 patients who survived 15 years or more, survival thereafter was higher in Group P, compared with Group N (100 vs. 76 % at 30 years, p=0.045). Cardiac catheterization data demonstrated higher Cardiac Index in Group P patients compared with Group N patients (3.5 vs. 2.8 L/m2, p=0.014). Cardiac magnetic resonance imaging study revealed that Group P patients had higher right ventricular enddiastolic volume index (96 vs. 57 ml/m2, p=0.005), higher end-systolic volume index (49 vs. 30 ml/m2, p=0.013) and higher right ventricular stroke volume index (48 vs. 25 ml/m2, p<0.001), compared with Group N. Exercise capacity tests demonstrated that Group P patients showed a higher percentage of peak oxygen consumption, compared with Group N patients (73 vs. 58%, p<0.001). In conclusion, patients who presented with a pulsatile systolic pulmonary blood flow demonstrated a better survival, larger right ventricular volume, and better exercise capacity, compared with those without pulsatile systolic pulmonary blood flow in the cohort of long-term survivors more than 15 years after the Fontan-Björk procedure. A sufficient volume of the RV seems to be a prerequisite to create pulsatile pulmonary flow.
Figure 1: Survival at 15 years follow-up and later in patients after Fontan-Björk modification.

Figure 1: Changes in peak VO2 over time in Fontan-Björk patients according to the presence (blue circle) or absence (red circle) of pulsatile pulmonary blood flow.

Matching patients and conduits
a patient-centered approach to conduit selection
The second and third conduit choice in coronary surgery – an unresolved challenge



Q. Where did you carry out your training?
Turin – Italy, then I specialised in Genova, Italy, then at the European Hospital in Rome.


Q. What are your main areas of interest within cardiothoracic surgery?
CABG, Conservative Aortic Valve surgery, Blood Management.
Q. What are your interests outside of your work?
Sailing and piloting planes.
When you are asked to present at an International Meeting twice regarding different aspects of the same problem it is probably a good hint at the fact that the problem in question contains some unresolved challenges. And it is true indeed that coronary surgery, despite being in its mature age, is still lacking a few crucial answers guiding the surgeons to proper choices. Most uncertainties pertain to the selection of the second conduit, after having beautifully anastomosed the left mammary artery to the anterior interventricular artery. And it's even worse if we consider the third conduit. The ROMA trial is still recruiting and will hopefully someday soon give a conclusive answer to the question regarding using the second arterial conduit, mostly the second mammary. But the safein vein is still used on thousands of cases every day. When choosing between a second artery and a vein the real world problem to answer is if the extra effort is worthwhile. And the intrinsic problem to coronary surgery is that most answers can only be seen after years. Or, in other terms, you can get happily out of the operation with patent grafts no matter what your strategy is. In my first presentation here at EACTS I try to compare the known literature and personal experience trying to outline the potential benefit of spending more time, skill, and material to harvest the radial instead of the vein.
And in my second presentation I share my experience with veins reinforced with external
metallic elastic mesh, considering as well endothelial biochemical protection products and the no touch technique as a purely technical and non-technological alternative, with the precise perception that if so many tools are gaining traction the old style naked vein is probably coming to an end. Early and midterm results clearly show, in personal experience and in literature, that either choosing a radial artery or adding some protection to the vein reduces graft intimal hyperplasia and ultimately graft occlusion and ischemia drive rerevascularisation. This, by the way, is the only end point that matters to us as surgeons – and most of all to our patients.
Transcatheter edge-to-edge repair in heart transplant patients: a single-centre experience of a novel therapy Tillmann Kerbel1†, Keziban Üyanik-Ünal1†, Markus Mach1, Anna Bartunek 2 , Philipp Bartko3, Andreas Zuckermann1, Martin Andreas1
Isolated tricuspid valve surgery in patients who underwent heart transplantation may impose a higher risk of surgical and postoperative complications compared to nontransplanted patients, which might be reduced by an interventional treatment, namely tricuspid clipping. We established this technology early at the Department of Cardiac Surgery and were therefore able to offer it to patients who previously underwent heart transplantation.
All patients with prior heart transplantation undergoing transcatheter edge-to-edge repair in tricuspid position after thorough heart team discussion were prospectively enrolled in an institutional registry. All patients were clipped by one operator and results were reported in a prospective registry. A specific combination of a tri-clip steerable guiding catheter and a mitra-clip was used (Figure 1). Seven patients (71% female) – all showing a symptomatic tricuspid regurgitation (TR) ≥ IV
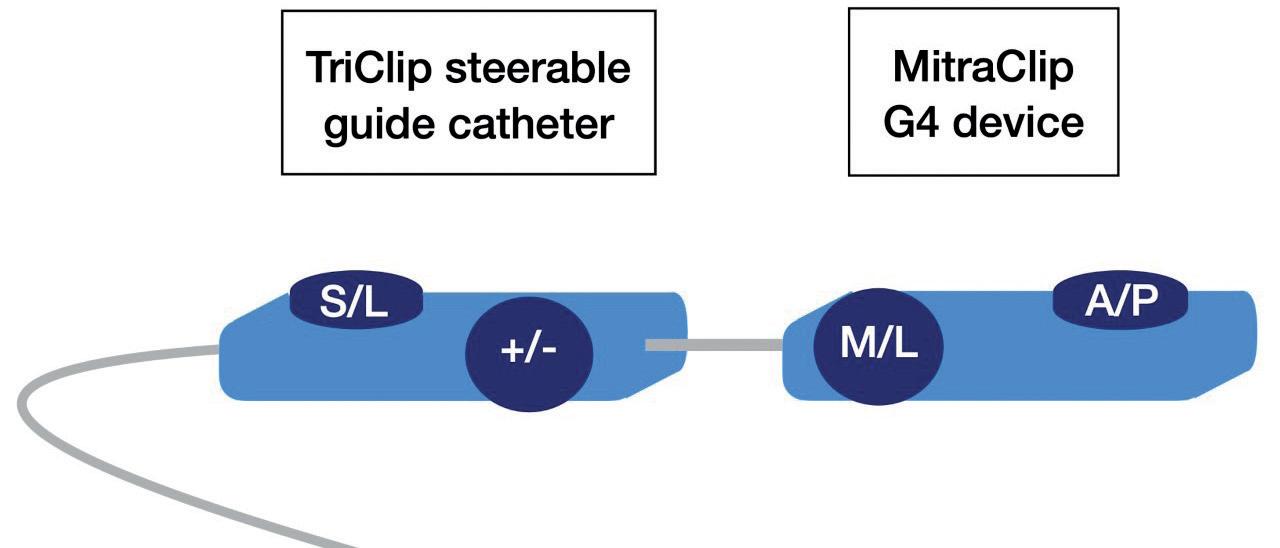
with overt clinical signs of right heart failure –at a median age of 53 [48; 64] years and median EuroSCORE II of 6.8% [5; 8.6] were included. Median time from transplantation to edge-to-edge repair was 13 years. A total of 2 (n=4) and 3 (n=3) clips were implanted with a technical success of 86% (one single device detachment). A significant TR reduction of ≥ 2 level was achieved in all patients directly after the procedure (p=0.016) and at discharge (p=0.016) (Figure 2). Patients treated in an elective setting (n=6) were discharged – without any in-hospital adverse event – after a median postoperative stay of 2.5 [2; 3] days. A significant symptomatic improvement with a NYHA class reduction of ≥ 1 was present in 86% of the patients at 30-day follow-up (p<0.02).
Therefore, we consider transcatheter edge-to-edge repair after transplantation to be safe and effective regarding TR reduction in this early analysis. The initial results may pave the way of a novel approach in TR management in HTX patients.
Figure
Luca Weltert / European Hospital, San Camillus International University of Health and Medical Sciences, Rome, ItalyFigure 1: VEST supported vein
Edwards Lifesciences Lunch Symposiums






