
3 minute read
Springtime and tick prevention go HAND-IN- HAND
BY KASHA STOLL
It is springtime in the Twin Ports. Bring on the warmer weather, longer days, green grass, flowers and tick protection.
“Most veterinary clinics in the area recommend (tick) preventatives March through November,” said Justin Dahl, owner and veterinarian at Happy Tails Animal Hospital in Superior. “The risk is especially high up here, and it changes with the weather pattern. Warmer winters mean more ticks.”
The Minnesota Department of Health and the Wisconsin Department of Health Services classify the Twin Ports and all surrounding areas as high risk for tick-borne diseases. The ticks become active as soon as the weather warms and most of the snow has melted.
Blacklegged ticks, also known as deer ticks or bear ticks, are the most common type of tick found in the area and are the most likely to carry and spread Lyme disease. That is a potentially serious bacterial infection that can cause flu-like symptoms, such as fever, chills, headache, fatigue, and muscle and joint pain. Over time, Lyme disease can lead to joint swelling, problems with the nervous system and persistent weakness and fatigue.
“Ticks can carry more than one disease at a time,” Dahl said. “It’s not just Lyme disease. They might also carry anaplasmosis or babesiosis. That is a recipe for disaster, and these pets live in our houses. They sleep on our beds. People don’t think about it because it is their cute little pet, but tick diseases are nasty and scary.”
Dahl answered some common questions about keeping pets and their owners safe from tick-borne diseases.
What can pet owners do to keep their pets safe from ticks?
All dogs “need some sort of tick prevention,” he said. “The most popular products are chewable pills rather than topical medicine. People like how effective they are and how quickly they kill ticks.”
Dogs that have a higher risk of exposure can also receive a vaccination for Lyme disease. These dogs might live in the woods, run through tall grass, or go hunting or hiking with their owners. Dahl said indoor dogs may be at high risk if they live with another dog that goes outside and can bring ticks back into the house.
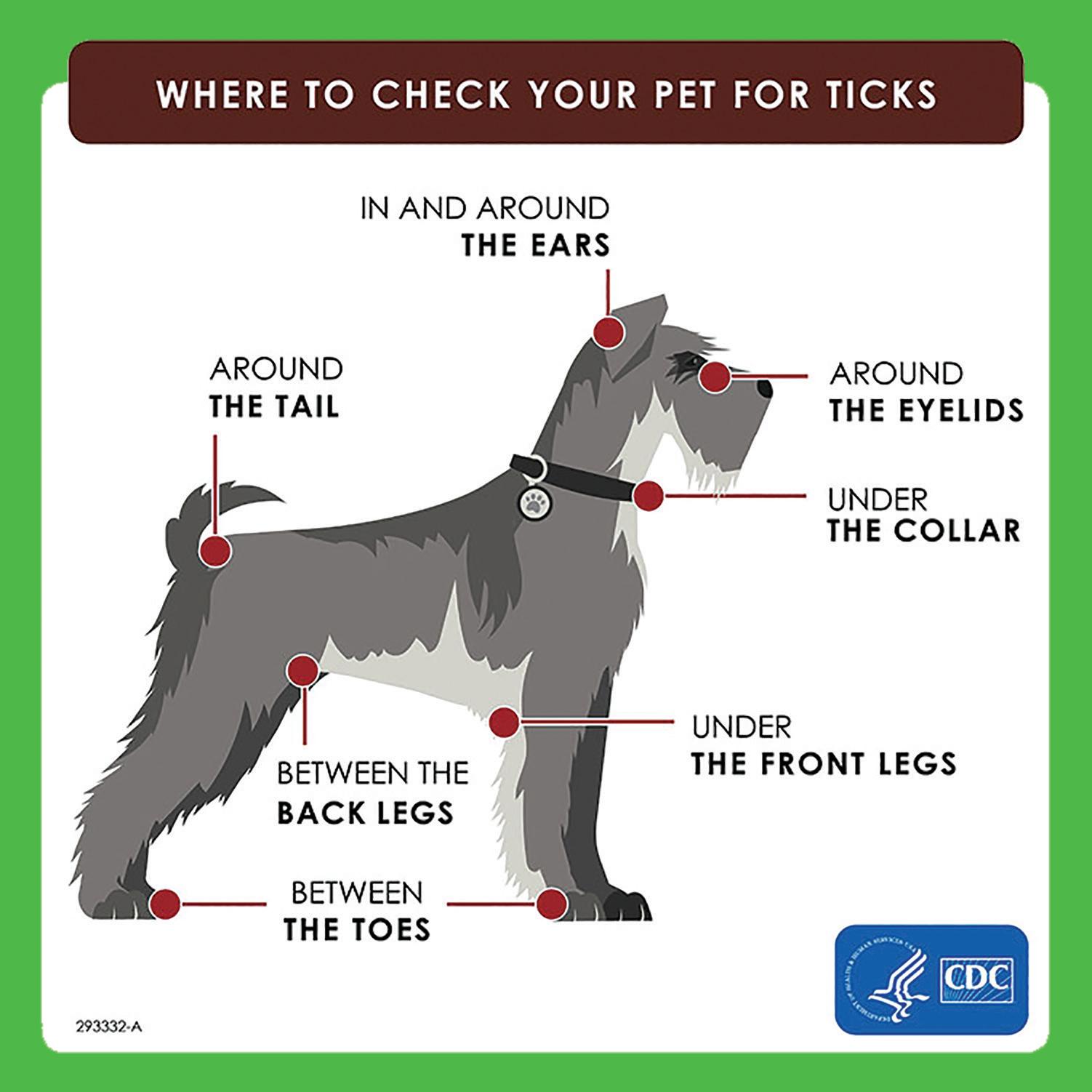
Dahl also recommends pet owners do a visual inspection of their dogs’ skin if they spend a lot of time in the woods.
“The idea is, ‘can I kill the ticks before I bring them into the house,’” Dahl said. “Dogs often sleep on our beds. Ticks don’t care who they bite; they just want warm blood. They will bite a person just like a dog.”
Dahl said cats should receive tick protection if they go outside. However, there is no pill version for cats. They're only option is a topical medicine.
What are the symptoms of tick-borne diseases in pets?
Dahl said symptoms can be classified into three groups:
CLASSICAL: Pets may exhibit the same type of symptoms that humans do. They may be stiff, sore or achy.
NOT CLASSICAL: Pets may throw up or not want to eat.
ADR (AIN’T DOING RIGHT): Dahl said ADR is a common term used by veterinarians in the area. Pet owners know their pet is sick, but they don’t know why. The pets may have one or several symptoms. “It’s not just one presentation,” Dahl said. “But people know something is wrong.”
According to the Centers for Disease Control and Prevention, dogs may exhibit signs of tick-borne diseases anywhere from one week to three weeks after being bit.
Pet owners should watch their dog closely for changes in behavior or appetite if they suspect their pet was bitten by a tick.
What should pet owners know about tickborne diseases?
“The more protection, the better,” Dahl said. “Vaccine alone is not enough. Tic protection alone, if you are high risk, it is not enough. They work in conjunction.
“Lyme disease is really a scary thing. There are dogs who die. We can diagnose early on and treat it appropriately, and they still develop kidney failure and die. It’s not common to die from one of these tick issues, but it can happen.” —
MDT
How to remove a TICK
1. Use fine-tipped tweezers to grasp the tick as close to the skin’s surface as possible.
2. Pull upward with steady, even pressure. Don’t twist or jerk the tick; this can cause the mouth-parts to break off and remain in the skin. If this happens, remove the mouthparts with tweezers. If you are unable to remove the mouth easily with clean tweezers, leave it alone and let the skin heal.

3. After removing the tick, thoroughly clean the bite area and your hands with rubbing alcohol or soap and water.



4. Never crush a tick with your fingers. Dispose of a live tick by putting it in alcohol, placing it in a sealed bag/container, wrapping it tightly in tape, or flushing it down the toilet.
5. Avoid folklore remedies such as “painting” the tick with nail polish or petroleum jelly, or using heat to make the tick detach from the skin. Your goal is to remove the tick as quickly as possible, not wait for it to detach.
SOURCE: cdc.gov
DEER TICK CREDIT: USDA











