Dear Friends,
Welcome! As you flip through our 2024 VISION magazine, we’re excited to show you what’s happening at the Duke Eye Center and in the field of Ophthalmology. This year, we’ve got some truly amazing stories to share about the incredible work our team is doing.
We’re all about turning great ideas from the lab into real treatments that can change lives. Imagine being the first to find a way to treat eye diseases that were once thought untreatable — that’s what we’re working on here at Duke. By working closely with experts in different fields at Duke like engineering and cancer research, we’re creating new ways to help people see better.
One of our impressive projects is finding out more about eye diseases that are passed down in families. Our goal is to understand these diseases better so we can come up with expanded gene therapy treatments, which could one day restore vision to people who have lost it.
We’re also working on a new way to check kids’ eyes to identify problems early, which is super important for keeping their vision sharp for life.

A new program available through our vision rehabilitation division is teaching future occupational therapists how to help people with vision loss — it’s pretty special because it’s not something you can find just anywhere.
Our team is also at the forefront of treating eye tumors with new, less invasive techniques. Thanks to our teamwork with Duke Radiation Oncology and the addition of a new expert in eye cancers, we’re making big strides in this area.
And we are continuing to expand our global efforts. Our Duke Global Ophthalmology program is making a difference in places where eye care is hard to come by. We’re even starting a fellowship to train doctors to work in this important area.
Lastly, our education programs for doctors in training continue to be top-notch, with our residents and fellows doing incredible work in ophthalmology.
Don’t miss the section on awards and honors to see what our faculty, trainees and staff have achieved.
I hope you find these stories as inspiring as I do. It’s the passion and dedication of our team that makes all this possible.
Warmest regards,
Edward G. Buckley, MD Vice Dean for Education, School of Medicine Chair, Department of Ophthalmology Vice Chancellor for Duke-National University Singapore Affairs Gills Professor of Ophthalmology Professor of Pediatrics Duke University School of Medicine
Bringing hope to patients with inherited retinal disease


INHERITED RETINAL DEGENERATIONS are genetic diseases that cause irreversible blindness. Developing treatments for these conditions is a challenging task, particularly because they are caused by mutations in over 300 genes that lead to varying types and severity of vision loss.
Historically there has been no cure for inherited retinal degenerations. Recent innovations in research have provided a promising type of treatment called gene therapy. This approach aims to correct defective genes by replacing them with healthy ones.
The introduction of gene therapy to practical ophthalmology is a remarkable example of how a complex human disease can be addressed by combined efforts of scientists and clinicians. A “bench-to-bedside” approach highlights the tremendous efforts of laboratory research teams behind the development of groundbreaking medications.
One particularly severe type of inherited blindness is Leber’s congenital amaurosis, which impacts children at a young age. The first breakthrough in understanding the cause of blindness for those with Leber’s was in the 1990s, when scientists discovered that the disease arises from an error in the RPE65 gene. This set the stage to take action against this disease.
During the same time another group of scientists found that the same gene, RPE65, is affected in a group of dogs who are blind. This discovery led to an unprecedented opportunity to determine if supplying these dogs with a healthy RPE65 gene would enable them to regain vision.
Left to right front row: Natasha Klementeva, PhD, Lauren Cao, BS, Lin Yu, PhD, Stella Finkelstein, MS, Carson Castillo, MS, Margaux Kreitman, PhD, Vadim Arshavsky, PhD.
A few years later, a dog named Lancelot made an unusual visit to the U.S. Congress. Lancelot had been born blind but could now clearly see the members of the Congress after receiving a revolutionary gene therapy treatment. A collaborative effort by teams of scientists and clinicians
Scientists at Duke Eye Center are working to develop universal therapies that can save sight regardless of which genes are mutated.

Oleg Alekseev, MD, PhD joined Duke Eye Center faculty in 2022, helps translate proteasome enhancement into an effective treatment.

The concept of proteasome enhancement, to assist in clearing of damaged proteins in the retina, was discovered in the laboratory of Vadim Arshavsky, PhD. His laboratory reported promising treatment results in animals with the same mutations as those found in human patients.
made history by showing that replacement of the damaged RPE65 gene with a healthy one could restore vision in animals.
The path to curing blindness in human patients was now in sight. The treatment entered clinical trials, and for the first time, children treated with a healthy replacement gene could see the faces of their parents and siblings. Upon completion of the trial, the drug, voretigene neparvovec-rzyl, known commercially as Luxturna® became the first gene therapy approved by the FDA to treat any blinding genetic condition. The landmark bench-to-bedside development of Luxturna® emphasized just how much science can do to improve the wellbeing of the public; but it also emphasized how many resources are required at every step from scientific discovery to clinical application.
Duke Eye Center is a premier destination for the treatment of vitreoretinal diseases, offering the latest in patient care. As a recently Certified Center of Excellence for Luxturna®, Duke is the only Luxturna® treatment center between Philadelphia and Miami for patients on the East Coast of the U.S. Patients eligible for Luxturna® treatment are cared for by a team of expert clinicians, including specialists in the diagnosis and management of inherited retinal diseases and vitreoretinal surgeons with advanced expertise in delivering gene therapy medications to the retina. The clinical team is supported by a dedicated genetic counselor working with patients and their families to uncover their diagnoses through specialized genetic testing. An important aspect of patient care is a comprehensive retinal electrophysiology facility, where patients undergo sophisticated testing, such as electroretinography (ERG), to measure the ability of the retina to detect light. This detailed testing gives the retina specialist information needed to identify candidates, prepare for and monitor treatment.
The development of Luxturna® is a monumental achievement, but this is just a first step in helping patients suffering from inherited retinal degenerations. Patients eligible for Luxturna® treatment represent less than one in a thousand of all people suffering from these conditions.


Maldonado, MD
This is because there are more than 300 other genes whose defects lead to various forms of this disease, with more still discovered every year and only a handful addressed in ongoing trials. A major challenge with developing new therapies, especially gene therapy, is that it takes a tremendous amount of time and money to bring each treatment to clinic.
To overcome this challenge, scientists at Duke Eye Center are working to develop universal therapies that can save sight regardless of which genes are mutated. The scientific foundation of this pursuit is their discovery that many mutations causing inherited retinal degenerations lead to a buildup of damaged proteins in the retina. As everywhere else in the body, the retina has a built-in system for garbage disposal called proteasomes, which eliminate damaged proteins to keep the retina healthy. In retinas affected by inherited degenerations, proteasomes may be overwhelmed and become unable to keep up with the disposal of damaged proteins. A sound solution would be to bring new proteasomes to the rescue, and this is exactly what Duke scientists strive to bring to degenerating retinas in order to clear proteins damaged by disease-causing mutations.
The concept of proteasome enhancement was discovered in the laboratory of Vadim Arshavsky, PhD, a world-renowned retina scientist and Vice Chair for Basic Science Research at Duke Eye Center. His laboratory reported promising treatment results in animals with the same mutations as those found in human patients.
Much more remains to be done to translate this scientific discovery into an effective treatment. These efforts are spearheaded by Oleg Alekseev, MD, PhD who joined Duke Eye Center faculty in


Lejla Vajzovic, MD, FASRS

Genetic Counselor
2022. Trained as both a scientist and a clinician, he is uniquely qualified to move this program forward. “Learning from my patients in the clinic inspires me to work tirelessly in the laboratory to better understand their conditions and to devise novel treatments to improve the quality of their lives”, said Alekseev.
To integrate, facilitate and expand the audacious efforts of these and other researchers, Duke Eye Center has an exciting plan to establish the Center for Innovative Treatments of Retinal Degenerations. This will establish a robust translational research pipeline, whereby the ideas generated in laboratories and clinics will be converted into novel therapies. In this pipeline, new discoveries will be evaluated in blind animals first, followed by a streamlined process of developing and testing new therapeutics, and subsequently advancing the most promising candidates to clinical trials.
Other scientists at Duke Eye Center engaged in drug discovery and development to cure inherited blindness are Sidney Gospe, MD, PhD, who addresses rare but disastrous and currently incurable blinding conditions affecting the optic nerve, and Jeremy Kay, PhD, who is tackling a severe form of childhood blindness by using gene therapy.
Duke is fortunate to have a broad range of expertise on the same campus, which allows for enhanced collaboration. With the expertise in place, financial resources are needed to continue groundbreaking research that will hopefully one day cure blindness for people with inherited retinal degenerations. 05
Oleg Alekseev, MD, PhD Anna Duemler, MS Xi Chen, MD, PhD Ramiro
Equipping occupational therapists to empower low vision patients
Today, more than seven million Americans suffer from blindness or low vision — defined as the loss of sight unable to be corrected with prescription glasses, contacts, or surgical interventions. Often caused by age-related disorders like macular degeneration or glaucoma, the number of people impacted by low vision is only expected to rise

“Despite the fact that vision impairments are steadily climbing, less than 20 percent of academic occupational therapy training programs include specialized coursework in vision disorders and visual impairments.”
Diane Whitaker, OD Division Chief, Vision Rehabilitation & Performance
as the percentage of the U.S. population over 65 surges in the next 20 years. According to recent data, in North Carolina alone the number of residents who are 85 or older will more than double by 2041.
Unlike complete blindness, individuals with low vision often retain some level of sight and for many, the use of visual aids can help to enhance their remaining vision. Symptoms of the condition vary, ranging from blind spots and poor night vision to glare sensitivity and blurry vision, posing unique challenges to their daily routines and independence. With the exponential growth in the number of older adults affected by low vision, there is an increasing demand for trained professionals to provide care and teach fundamental life skills.
In response, the Duke University Occupational Therapy Doctorate (OTD) Program in cooperation with the Duke Eye Center Vision Rehabilitation and Performance Division has launched a groundbreaking Low Vision Certificate. This certificate program, initiated in the academic year 2022-23, addresses the shortage of experienced practitioners equipped to assist people living with vision impairments.
“Despite the fact that vision impairments are steadily climbing, less than 20 percent of academic occupational therapy training programs include specialized coursework in vision disorders and visual impairments,” said Diane Whitaker, OD, vision rehabilitation division chief at Duke Eye Center “Together our multi-disciplinary team of professionals — with the full support of the Duke University School of Medicine — established this one-of-kind curriculum for training occupational therapy students.”
The Duke OTD vision certificate program is one of only two certificate programs in the nation for entry-level practitioners. This uniquely interconnected training curriculum was developed based on the collaboration and guidance of Whitaker, Tomeico Faison, OTD, OTR/L, Barbara Hooper, PhD, OTR/L, FAOTA and Kimberly Hreha, EdD, OTR/L. As a result of considerable enthusiasm, by its second year the highly sought after program had to establish a competitive application process. Already, nearly
20 students have confirmed their interest in pursuing the Certified Low Vision Therapist (CLVT) certification and recently 12 new participants were accepted into the course of study.
“The success of our inter-departmental collaboration is realized in the hybrid structure and flexibility of this innovative curriculum,” shared Faison. “Through it, occupational therapy students are collaborating with members of the rehab team as well as optometrists and ophthalmologists from the Duke Eye Center Rehabilitation and Performance Division. Together we are equipping the next generation of therapists with the skills required to help patients live fuller lives despite their low vision challenges. It’s inspiring to see the possibilities.”
The comprehensive 14-week course covers essential topics required for the students to earn their CLVT certification, along with specific
occupational therapy proficiencies. Participants are engaged through rigorous training that includes topics such as ocular anatomy, interprofessional teamwork, common eye diseases, assessment processes, interventions, community resources, technology, and research.
“The Duke OTD vision certificate program was a rare opportunity for me to receive high-quality low vision education from the best practitioners in the field,” Stephanie Stellato, program participant. “During my fieldwork at Duke Eye Center I gained valuable patient experience and benefitted from the feedback I received from each practitioner and professor. This training has equipped me with the skills I need to be become an occupational therapist who specializes in Low Vision.”
After completing their coursework, students must complete a 350-hour fieldwork or capstone experience before being eligible to take the credentialing exam. This work takes place


Occupational Therapy Doctorate candidate Stephanie Stellato during her clinical rotation learns how Omar Mohiuddin, OTR/L, MS, MPH, CLVT adapts diabetes self-management tasks to train a client with low vision check their blood glucose level.
at leading institutions across the country — including Duke Eye Center — with additional sites under consideration to accommodate the growing number of students pursuing the certificate.
“For decades eye care providers have been anticipating the needs of aging baby boomers and growing concern over the paucity of resources to meet those needs,” said Whitaker. “This certificate program pairs the expertise of Duke Ophthalmology with the benchmark therapies provided by Duke OTD, equipping specialists to help bridge that gap.”
Still in its infancy, Duke OTD is leading the way, becoming a model for the formation of similar courses at other institutions. By cultivating robust partnerships with national organizations such as the American Academy of Ophthalmology, the Academy for Certification of Vision Rehabilitation
“At Duke, we attract and train the best and the brightest. We’re confident that our OTD graduates will be equipped to excel, drive advancements in world of vision rehabilitation and help low vision patients thrive.”
Barbara Hooper, PhD, OTR/L, FAOTA Founding Program Director, Duke Occupational Therapy Doctorate
& Education Professionals and other leaders in optometry and occupational therapy, Hooper, Faison, Hreha and Whitaker hope to see this and other programs grow.
“At Duke, we attract and train the best and the brightest. We’re confident that our OTD graduates will be equipped to excel, drive advancements in world of vision rehabilitation and help low vision patients thrive,” said Hooper.

Ocular Oncology is a distinct subspecialty of ophthalmology which focuses on the diagnosis and treatment of cancers that impact the eye, orbit (eye socket) and eyelids. The Division of Ocular Oncology was formally established at Duke Eye Center in Fall 2023 after more than 20 years of providing treatment for eye cancer. Under the leadership of Miguel Materin, MD, professor of ophthalmology and professor of radiation oncology, the Division of Ocular Oncology is dedicated to providing full time specialized care for children and adults battling benign and malignant tumors of the eye.
Originally part of the retina division, the demand for treatment has only increased over the past several years. Steadily expanding to more than 500 patients visiting Duke Eye Center each month for ocular oncology support, the need for a division solely devoted to eye cancer was clear.
“More than 90% of our patients are referred to us from other specialties within ophthalmology or from caregivers in other fields including melanoma, breast cancer, neuro-oncology, radiation oncology and pediatric oncology,” said Materin. “Our ocular oncology patients come from North Carolina, South Carolina, Virginia, Georgia, Tennessee and other states and countries. We also treat patients from other departments within Duke.”
In June 2023, Duke became one of only three treatment sites in the U.S. certified to utilize the novel high dose-rate (HDR) yttrium-90 (Y-90) brachytherapy procedure.

The Y-90 procedure, cleared by the Food and Drug Administration for episcleral brachytherapy of ocular tumors and benign growths, involves placing an applicator with a Yttrium-90 disc directly over the surface of eye for treatment. This approach effectively treats small lesions from a variety of conditions, including ocular surface tumors and posterior (intraocular) tumors. Remarkably, most procedures are completed in less than 10 minutes.
“We’re honored to have been chosen as one of the first centers in the country to offer this innovation in patient care,” said Materin. “Y-90 is an incredibly less-invasive procedure that replaces traditional therapy and will positively contribute to the evolution of ocular oncology on a national scale.”
“We’re honored to have been chosen as one of the first centers in the country to offer this innovation in patient care. Y-90 is an incredibly lessinvasive procedure that replaces traditional therapy and will positively contribute to the evolution of ocular oncology on a national scale.”
Miguel Materin, MD
“All brachytherapy is a team sport. None of this happens without a high degree of collaboration between the surgeon, the radiation oncologist, a dedicated physics team, as well as the nurses, surgical coordinators, recovery staff and assistants in the operating room.”
Junzo Chino, MD
In collaboration with the Department of Radiation Oncology at Duke, Junzo Chino, MD, associate professor of radiation oncology and director of brachytherapy, has worked with Materin to successfully perform the Y-90 procedure.
During the initial consult, the patient is evaluated to determine if they are a good fit for the Y-90 procedure. If so, using tumor measurements, the team calculates the time to the appropriate depth and then provides quality assurance during preplanning. In the operating room, Chino attaches the Y-90 disc to the wand, then ophthalmologist delivers the treatment to the patient. Physicists monitor the time as the source is applied. The
procedure is over in a matter of minutes.
“All brachytherapy is a team sport,” said Chino.
“None of this happens without a high degree of collaboration between the surgeon, the radiation oncologist, a dedicated physics team, as well as the nurses, surgical coordinators, recovery staff and assistants in the operating room. Every role in this group is absolutely critical to ensure we’re on top of our game and each procedure is done as safely and effectively as possible.”
The collaborative team in ophthalmology and radiation oncology continue to pave the way for advancements that not only improve patient outcomes but also set new standards of

OR Team for Y-90 procedure. Materin, Chino, physics team, anesthesiology, and nursing staff.
excellence, positioning Duke as a pioneering force in the development of eye cancer treatments.
In response to the growing need for ocular oncology care at Duke Eye Center, the division is host to a thriving training ground, including a one-year Ophthalmic Oncology and Pathology Fellowship program. The fellowship embraces a multidisciplinary approach to medical and surgical management of a wide range of ophthalmic cancers, along with a robust research component. Since 2017, six ocular oncology fellows have trained with Materin. These physicians have hailed from outside institutions around the globe.
Upon completion of the program, the most recent fellow, Arpita Maniar, MBBD, MD — also a skilled oculofacial plastic surgeon and ophthalmologist — became a full-time member of the Ocular Oncology division and is now working alongside Materin, as an attending physician and Duke faculty member. Together, the two are helping train ophthalmology residents, providing hands-
on patient care and contributing to research. “The Duke Ocular Oncology fellowship was a tremendous opportunity for me to gain specialized skills and cultivate a deep knowledge of this rare field of cancer,” shared Maniar, associate professor of ophthalmology. “The support of the Duke Ophthalmology team and the collaboration with oncologists from other cancerrelated disciplines makes this fellowship impactful, and allows us to provide our patients with the highest level of care.”
Essential to the ability of the Ocular Oncology division to train the next generation of practitioners and deliver much-needed care to patients, is the cooperation and teamwork they enjoy with the Duke Cancer Center and other nationally-recognized treatment facilities. Together with renowned cancer specialists from areas such as pediatrics, neurosurgery, radiation oncology, breast cancer and others, they are able to provide the highest level of care to patients battling the spread of disease.
Building a program with the power to transform people’s lives and economies worldwide.
BY VICKIE FRYE PHOTOGRAPHS BY CHRIS HILDRETH/ROOSTER MEDIA
Recent statistics on global blindness are dramatic and tell a complex story. A story that begins with 36 million; the number of people around the world who are living with blindness. Most of these individuals — nearly 90 percent — reside in low resource countries where corrective medical treatments are not readily available.
Collectively, the most common causes of vision impairment and blindness in emerging nations are conditions familiar to patients in developed countries; issues such as cataracts, glaucoma, corneal trauma and uncorrected refractive errors like astigmatism or myopia. Regrettably, when they go untreated, these disorders often have devastating effects on a person’s overall
health and wellness, as well as on the social and economic circumstances of their family and community. In short, sight loss and the lack of accessible eye care contribute to a cycle of poverty and the potential onset of other debilitating health conditions.
Fortunately, the story doesn’t have to end here. There is hope. Over half of those 36 million people could have their sight completely restored through procedures that can be performed for less than $100 (the average American’s monthly coffee allowance). What’s more, according to the World Health Organization, for an estimated $15 billion, needless blindness worldwide could be solved and glasses provided to the nearly 371 million people whose vision is impaired.
36 million people are blind
217 million people are MSVI
253 million people are visually impaired
References: Ackland P, Resnikoff S, Bourne R. World blindness and visual impairment: despite many successes, the problem is growing. Community Eye Health. 2017;30(100):71-73. PMID: 29483748; PMCID: PMC5820628. World report on vision. Geneva: World Health Organization; 2019. Licence: CC BY-NC-SA 3.0 IGO. Adelson, J., Bourne, R. R. A., Briant, P. S., Flaxman, S., Taylor, H., Jonas, J.B., et al., Causes of blindness and vision impairment in 2020 and trends over 30 years, and prevalence of avoidable blindness in relation to VISION 2020: the Right to Sight: an analysis for the Global Burden of Disease Study, Lancet Global Health. 2020. Accessed via the IAPB Vision Atlas (https://iapb.org/learn/vision-atlas).
In response to this large-scale need for skilled ophthalmologists and transformative care, the Duke Eye Center has launched Duke GO — the Division of Duke Global Ophthalmology. Led by corneal specialist, Lloyd Williams, MD, PhD, Duke GO is aiming to make a positive and lasting impact on eye health worldwide, bridging the
gap by offering essential treatments and training doctors to become warriors in the fight against preventable blindness.
At the forefront of this progressive initiative are distinguished doctors whose vision and
Balu Sesay was the first person in Sierra Leone to receive a cornea transplant in 2021, restoring her sight after 29 years of blindness. She was able to see her children for the first time ever after the surgery. Her daughter is on the left.

commitment are helping shape the future of global ophthalmology. Williams — with support from Duke Eye Center and in partnership with passionate colleagues including glaucoma specialist, Leon W. Herndon Jr, MD, and cataract surgeon Anupama Horne, MD, — is spearheading Duke GO. This extraordinary team is dedicated to building a program that transcends borders and delivers solutions to the problem of preventable blindness through direct patient care, formal education and training and a sustainable infrastructure.
From Honduras and South Sudan to Sierra Leone and Nepal, hands-on patient care is of utmost importance in countries where there is a lack of skilled ophthalmologists.
“On my first trip to Honduras, we conducted surgeries, provided clinical care to patients in need of basic eye health screenings and offered much-needed medicines that are otherwise not readily available,” shared Horne. “This year
I am excited to return — leading a talented and committed team comprised of two fellow surgeons, three technicians and three O.R. nurses. Together, we’ll conduct operations and routine treatments that will make a huge difference in the lives of individuals with emerging conditions that may not have otherwise been detected or addressed.”
Duke GO is helping bring the joy of vision to thousands suffering unnecessarily with diminishing eyesight made worse by the lack of diagnosis or available treatments. Despite challenging conditions, intricate surgical procedures including corneal transplants, cataract surgeries and glaucoma therapies are delivering extraordinary results — restoring vision and the hope of a bright future to patients and their families.
The mission of Duke Ophthalmology is “curing eye diseases worldwide through excellence in research, training and patient care.” Through Duke GO, the opportunity to fulfill this commitment has never been greater.
“Our objective is to enable local doctors with the knowledge and skills to make a real difference in the lives of fellow citizens who are suffering from treatable eye conditions.”
Lloyd Williams, MD, PhD



By way of regular face-to-face training and partnering with incountry physicians and institutions in locations like South Sudan, Roatan and Sierra Leone, Williams and other Duke GO leaders are changing patient outcomes today and for the future.

“Our objective is to enable local doctors with the knowledge and skills to make a real difference in the lives of fellow citizens who are suffering from treatable eye conditions,” said Williams. “Through collaboration and education, we are creating a powerful network of global ophthalmologists dedicated to combating preventable blindness.”
By way of regular face-to-face training and partnering with in-country physicians and institutions in locations like South Sudan, Roatan and Sierra Leone, Williams and other Duke GO leaders are changing patient outcomes today and for the future. For example, Herndon, who currently serves as the president of the American Glaucoma Society, has teamed up with experts nationwide to teach surgical techniques — virtually — to ophthalmologists in Nigeria who are treating glaucoma patients.
“The need for adequate eye care is everywhere, and through our teaching we are creating access to proper diagnoses and treatment which will close the gap between the haves and have nots,” shared Herndon. “For nearly 30 years, I’ve been privileged to take an active role in preparing the next generation of physicians — I’m thrilled to be

part of a passionate team who’s helping to change lives through empowerment.”
A robust infrastructure is crucial for the success of the Duke GO division. Active participation by Duke Eye Center specialists in pediatrics, corneal disease, glaucoma and retinal disease, the addition of a program coordinator and the potential for a formal fellowship program is providing the fuel necessary to power the global ophthalmology program for years to come.
“As we generously invest in Duke GO and the division continues to evolve and thrive, I envision a future where preventable blindness is minimized, if not eliminated,” shared Williams. “Through ongoing research, partnerships and outreach, we can impact lives and become a catalyst for positive change on a global scale.”
WATCH: NBC News report where Lloyd Williams, MD, PhD discusses global blindness and restoring sight during a recent trip to South Sudan.


In pediatric ophthalmology, early detection of retina-related disorders is the key to unlocking a future full of possibility for young patients. Yet, all too often children do not recognize, or are unable to, articulate their vision problems and our current screening methods may not recognize retinal issues.

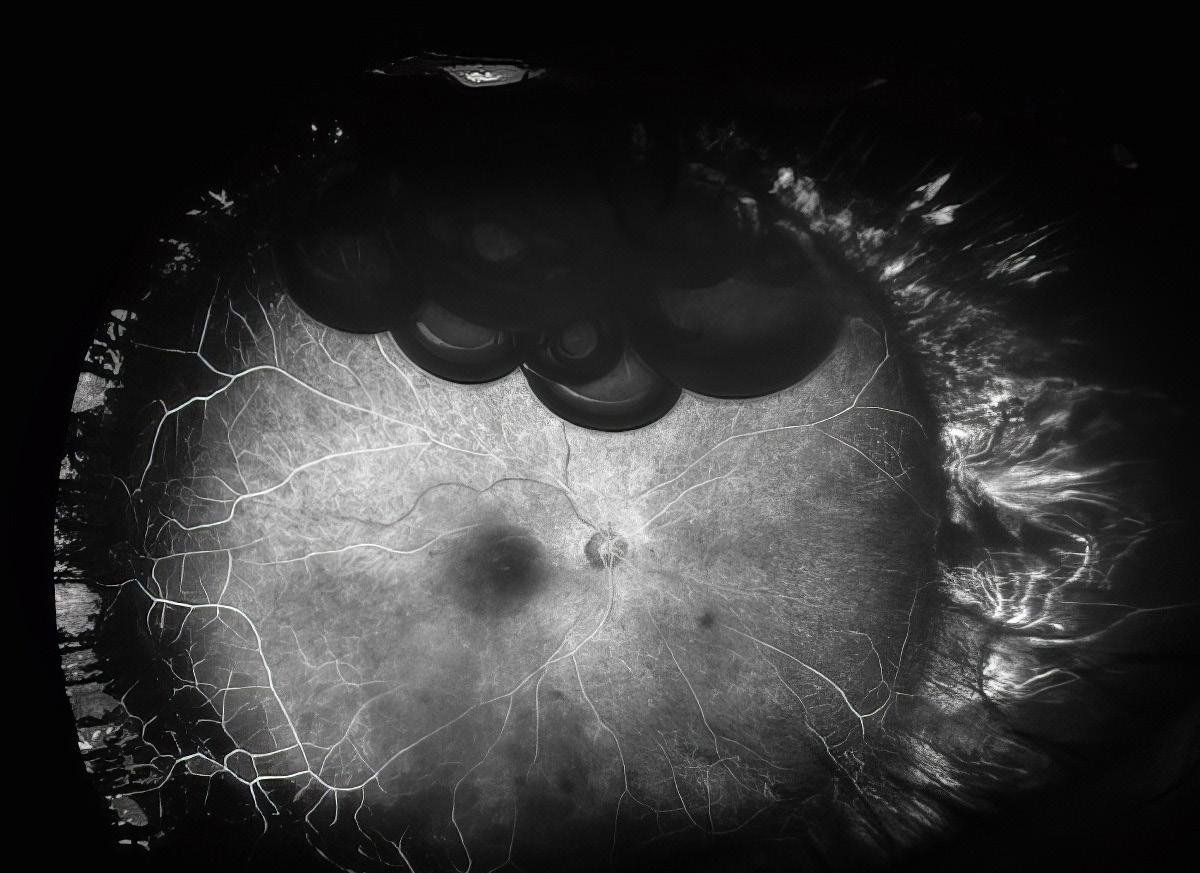
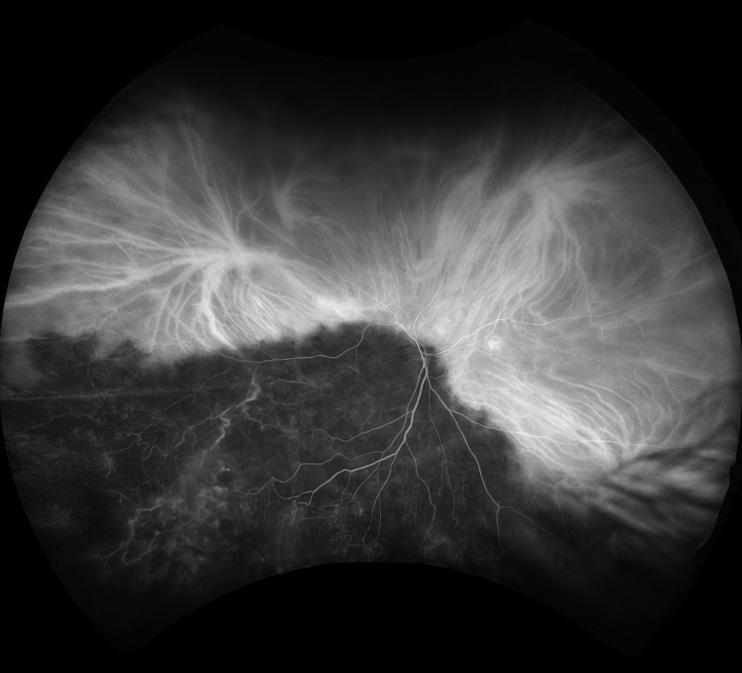
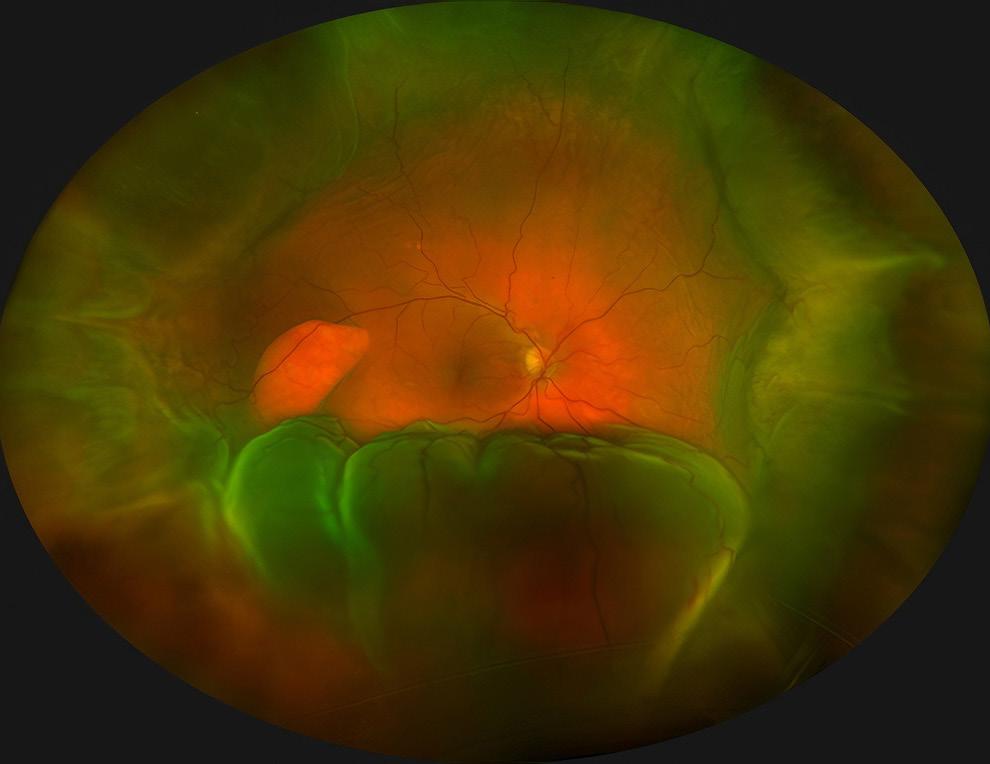
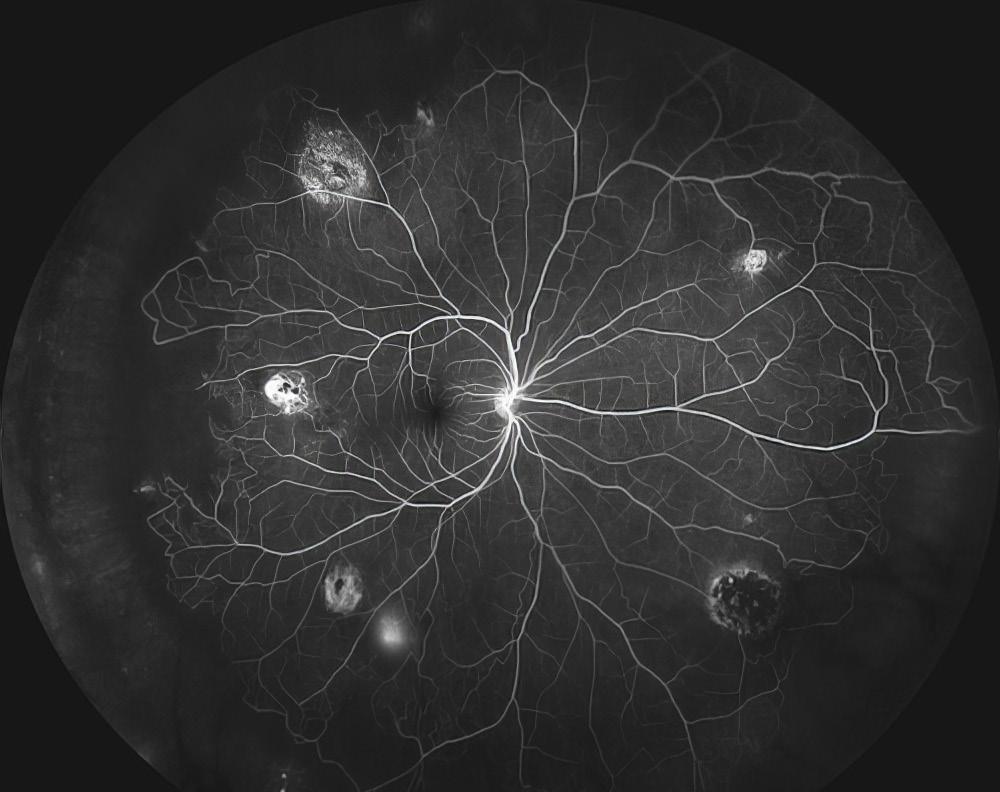
This leads to delayed diagnoses and longterm negative impacts on their eyesight. However, a groundbreaking study — Pediatric Retina Artificial Intelligence System Evaluation (PRAISE) — is under way at Duke Eye Center and holds the potential to transform routine childhood eye exams. By adding the use of wide field fundus photography to the standard eye chart and red reflex testing, the intent is to advance the discovery of retinal detachment and other retinal problems.
Still in its initial phases, the PRAISE study shows how the laser-assisted tele-screening technology, called an optomap, is enabling ophthalmologists, optometrists, pediatricians and other professionals to capture ultra-widefield, detailed images of the fundus — the back of a child’s eye — without the discomfort of traditional methods involving bright lights, dilating drops or more involved procedures that require sedation. Lejla Vajzovic, MD, FASRS, the pioneering force leading the study emphasizes the transformative power of this innovative approach to pediatric eye care especially as


Duke pediatrician and study collaborator May Slowik, MD potential to transform routine childhood eye exams.
a screening tool in pediatrician and
other primary care offices.
“Employing this technology as a screening tool in pediatric and primary care offices will be a game changer, giving us the ability to detect retina issues early on and prevent the need for invasive procedures,” said Vajzovic. “Through this technology, doctors are equipped to capture thorough imagery of the eye and able to make informed treatment decisions that will result in positive outcomes and better quality of life down the road for countless children.”
What sets the PRAISE study apart is its ambition to integrate tele-screening technology into primary care practices and school settings. The ongoing study, conducted in collaboration with May Slowik, MD, a board-certified pediatrician in Durham, NC, has already imaged an estimated 150 children, with results revealing that nearly 5 percent of the patients may have undetected issues that
could benefit from corrective treatment.
“It is a privilege for our primary care clinic to partner with pediatric ophthalmology to share the common goal of early childhood eye disease detection and prevention,” shared Slowik.” From toddlers to teenagers, our patients and their families have been excited to see their retinal images and to contribute to advancements in pediatric vision screening.”
“We are excited to pave the way for this technology to be used to revolutionize vision screenings, progress pediatric eye care and improve outcomes for children everywhere.”
Lejla Vajzovic
In addition to the study, Vajzovic and her team are working in
partnership with Duke Biomedical Engineering in the development of technology that will read the exam images and automatically deliver a pathology report. Ultimately, the hope is that by pairing the use of wide field fundus photography with artificial intelligence for automatic analysis, testing facilities of all types will be capable of providing quick assessments and facilitating timely referrals to eye specialists.
Beyond its applications in pediatric care, this telescreening technology has already been proven successful in the care and diagnosis of patients with diabetes and among endocrinologists, showcasing its versatility and effectiveness in a variety of medical fields. The prospect of identifying retinal issues such as retinal detachment or Coats’ disease early on, opens doors for more positive outcomes and brighter futures for children.
“We are excited to pave the way for this technology to be used to revolutionize vision screenings, progress pediatric eye care and improve outcomes for children everywhere,” shared Vajzovic.
Less than three years ago, Daryl Johnson was diagnosed with eye cancer that threatened not just his eyesight, but potentially his life. Thanks to the expertise of Jason Liss, MD, his oculofacial plastic surgeon at Duke Health, today Johnson enjoys spending peaceful afternoons on his back porch in La Grange, NC. He credits the care he received at Duke for allowing him to see the world clearly, cancer-free.
In spring of 2021, Daryl Johnson, now age 83, noticed a growth in the corner of his left eye. While it did not interfere with his vision, his eye was irritated and uncomfortable, so he made an appointment with a local ophthalmologist. After examining Johnson’s eye, the doctor referred him to a larger practice in Greenville, NC. By that time, the growth had spread to his lower eyelid. The doctor in Greenville knew that Mr. Johnson needed specialized care. “He took one look and said that I needed to go to Duke,” recalled Johnson.
In March, he met with Jason Liss, MD, an oculofacial plastic surgeon — an ophthalmologist with specialized training in the treatment of eyelid, eye socket, and tear duct diseases — at the Duke Eye Center. Dr. Liss was immediately concerned with Johnson’s condition. “The mass was unusual, and right away I was afraid for his ability


Duke Health, to have the mass in front of the ear removed.
to keep his eye, and depending on what type of tumor it was, his life could be at risk too.” Dr. Liss recommended surgery to remove as much of it as possible. A biopsy would also be performed to identify the tumor type.
During Johnson’s surgery, Dr. Liss took out most of the mass, which was identified as squamous cell carcinoma, a type of skin cancer, while leaving Johnson’s eye intact. “The good news was that we were able to separate it from the eye. The bad news was we had not removed all of it,” Dr. Liss said. That meant a second eye surgery was needed.
In a follow-up visit, Dr. Liss noticed another growth in front of Johnson’s left ear. It’s not uncommon for cancer in or near the eye socket to spread to lymph nodes in front of the ear, he explained. Dr. Liss referred Johnson to Russel Kahmke, MD, a head and neck surgeon at
Then, Dr. Liss presented Johnson with two options for his final eye surgery. The first was to take out the rest of the tumor without disrupting the eye. Dr. Liss explained that this approach might mean that some of the cancer would be left behind, and that due to scarring, the eye might not function properly after surgery. The second choice was to remove the eye and surrounding tissues to better ensure that that the entire tumor was eliminated. This would mean the loss of Johnson’s left eye. Johnson did not want to sacrifice his eye and chose the first option. “Thankfully, the surgery went really, really well,” Dr. Liss said. Johnson, who is now in remission, agrees. His vision was unaffected by the cancer and the surgeries. Today he relishes spending time with his three grown children, who live nearby, and is grateful to Dr. Liss for his compassionate care and expertise. “Dr. Liss is on my list of some of the greatest people on earth,” said Johnson. “He is the man.”
Duke University researchers created a computer program that determines, with 94% accuracy, if a person’s age-related macular degeneration will worsen within a year.
The deep learning algorithm, featured in an Oct. 19 study in JAMA Ophthalmology, analyzes detailed eye scans to predict if the common eye condition will progress to a more severe stage known as geographic atrophy (GA).
This faster foresight could streamline clinical trial recruitment and aid rollout of targeted treatments designed to preserve the vision of older adults.
“Being able to predict disease progression means we can be proactive, potentially halting its progression and improving patient outcomes,” said senior study author Eleonora Lad, MD, PhD, vice chair of clinical research and associate professor at the Duke Eye Center.
Eye doctors at Duke Eye Center collaborated with Duke AI Health, the Duke Department of Electrical and Computer Engineering and global experts on the recent study of the algorithm known as DeepGAze.
“This predictive tool could transform how we screen for the disease, how often we see patients, and even when to start treatments,” Lad said. Progression from intermediate AMD to geographic atrophy represents a transition from a largely asymptomatic condition to one that may devastate central vision, which is needed to read, drive and see pictures and faces.
The U.S. Food and Drug Administration recently approved medications that can offer a reprieve for the 1.5 million Americans diagnosed with geography atrophy. Izervay can slow GA’s progression and Ladd led clinical trials for Pegcetacoplan, the first FDA-approved medication for GA.
The Lancet recently highlighted Phase 3 clinical trial results confirming the ability of Pegcetacoplan to curb GA lesion growth with monthly or bimonthly injections.
Algorithms such as DeepGAze, like other technology used to track diabetic retinopathy, are poised to refine the diagnostic process and
BY SHANTELL M. KIRKENDOLL
help doctors figure out who’ll benefit most from maintenance and treatment.
In JAMA Ophthalmology, researchers detail how the DeepGAze algorithm sorted through volumes of spectral-domain optical coherence tomography scans of the retina to spot which eyes would progress from intermediate stage AMD to geographic atrophy within a year.
The program used data from several U.S. centers and the Age-Related Eye Disease Study (AREDS2). In all, 417 patients were involved in the study. The ability of DeepGAze to predict progression to GA within a year had a true positive rate of .94. In other words, it was right 94% of the time.
Even when experts added annotations, a timeconsuming and expensive task, to the model, it didn’t get significantly better than when it was working on its own.
Additional Authors: Co-first authors, Eliot R. Dow, MD, PhD and Hyeon Ki Jeong, PhD; Ella Arnon Katz, MD; Cynthia A. Toth, MD; Dong Wang, PhD; Terry Lee, MD; David Kuo, MD; Michael J. Allingham, MD, PhD; Majda Hadziahmetovic, MD; Priyatham S. Mettu, MD, PhD; Stefanie Schuman, MD; Lawrence Carin, PhD; Pearse A. Keane, MD; and Ricardo Henao, PhD.
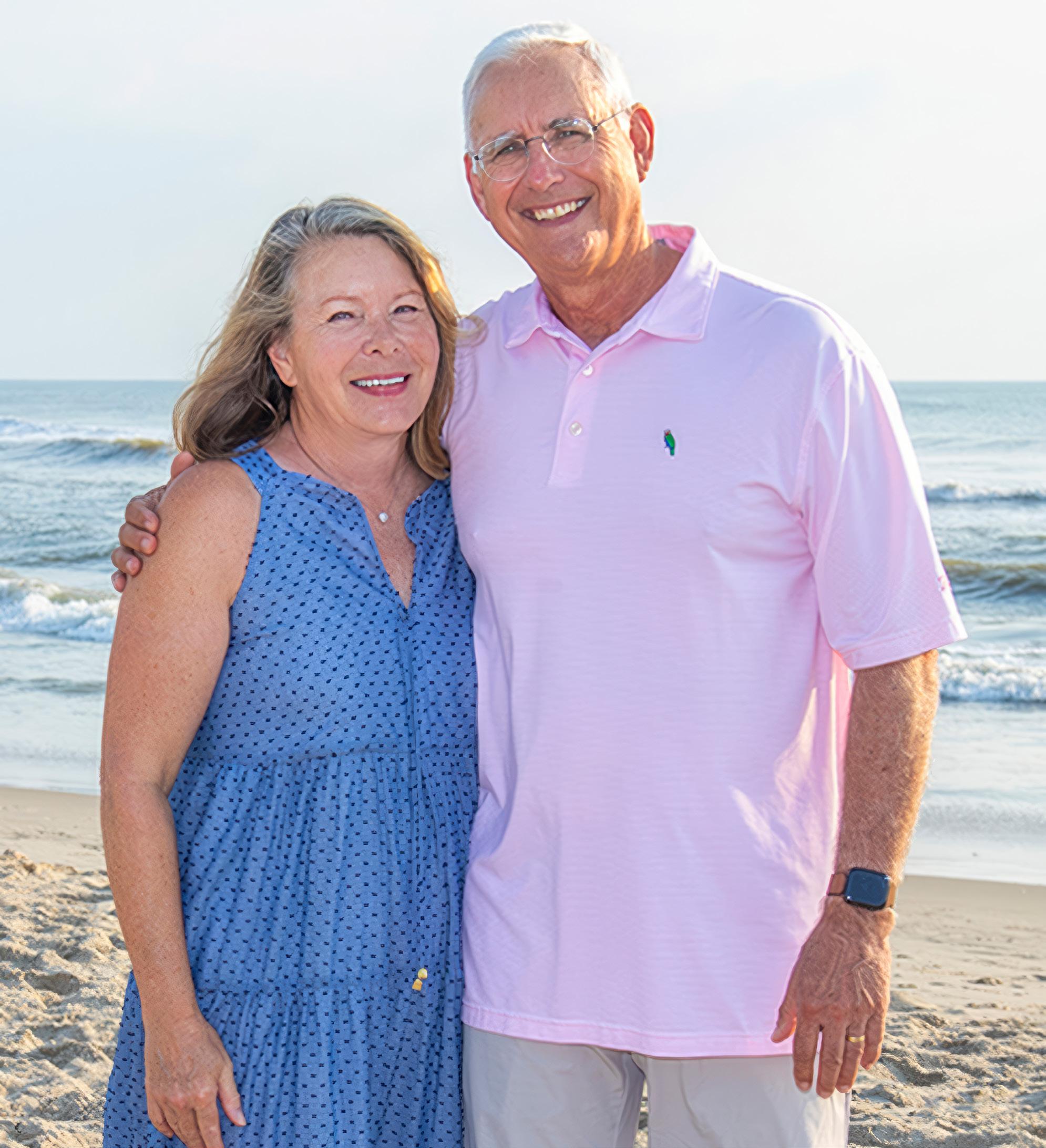
Looking back, Mark Stavish knows how fortunate he was.
Just as Mark and Wendy Stavish moved into their new home in Raleigh in the summer of 2022, the vision in Mark’s right eye began fading in and out. As someone with a history of benign floaters, he initially didn’t think much of it, but did seek out an ophthalmology recommendation from one of his new neighbors who happened to be a Duke primary care physician.
By the time Mark made it to his appointment three days later, he knew something was seriously wrong. The diagnosis confirmed it: he had a severe detachment of his retina.
BY WENDY GRABERThe couple were so impressed with Vajzovic’s skill as a surgeon and clinician that when they learned of her research to address retinal issues in children, they wanted to help. Toward that goal, they recently made a $1 million gift to support Vajzovic’s research to use state-of-the-art imaging with machine learning analysis for early diagnosis and treatment of pediatric retinal disease.
“Gifts like this one from the Stavishes allow our outstanding faculty to take on innovative projects to advance research and patient care. These gifts are crucial to Duke Eye Center’s sustained excellence.”Edward Buckley, MD
“It was a bad way to get introduced to Duke,” recalled Mark with humor. “But clinically it was just an amazing experience because everybody handled it so well. Everyone was so professional and Dr. Vajzovic really was amazing.”
Lejla Vajzovic, MD, FASRS, an ophthalmologist and vitreoretinal surgeon, was the surgeon on duty who performed the emergency surgery to reattach Mark’s retina. That surgery, and two follow-up surgeries for scarring and cataracts related to the reattachment, restored Mark’s vision to close to 20/20. He says every experience he had with Duke Eye Center was phenomenal.
“The people, obviously the clinical outcomes, clinical skill, the care, it was just great,” he recalled. “Every resident and fellow that I met was just terrific. And you could tell these are really committed, very, very, very bright young people. And that’s what you attract when you’re Duke. You get the cream of the crop, and I think that makes the attendings better. It makes all the clinical professionals around them better. And I think it’s kind of one of these self-referential loops. It just elevates the clinical skills.”
The challenge with diagnosing retinal disease in children is that by the time they are noticeably symptomatic they are often in danger of permanent vision impairment, or worse, loss of sight.
“My research aim is to identify concerns in the back of the eye, including any type of retinal, optic nerve, or blood vessel issue, before progression. Early diagnosis is key to saving a child’s vision,” said Vajzovic. “And because technology has evolved tremendously in ophthalmology, we now have the capability to identify areas of concern early on through images without having to do an in-depth examination. Not having to touch the eye or use bright lights helps when trying to diagnose infants and young children.”
The gift provides two years of research support. “This generous donation has ignited our research,” Vajzovic said. “We have launched a pilot program to assess the efficacy of using images from the back of the eye and algorithmic analysis for ocular screening in a pediatrician’s office. Our main goal is to ascertain the method’s ability to accurately detect retinal impairments. Furthermore, we seek to evaluate patient benefits, particularly in terms of early identification of conditions and the prevention of vision loss. Our efforts are focused on these fundamental questions and gathering the essential data to strengthen future applications for federal funding.”
Gifts for early-stage or high-impact research can leverage much larger follow-on funding capable of propelling preliminary discoveries into exciting new therapies.
“Dr. Vajzovic is an exceptional clinician, surgeon, and researcher,” said Edward Buckley, MD, chair of the Department of Ophthalmology and vice dean for education at Duke University School of Medicine. “Gifts like this one from the Stavishes allow our outstanding faculty to take on innovative projects to advance research and patient care. These gifts are crucial to Duke Eye Center’s sustained excellence. The flexibility of philanthropic funds allows our researchers
freedom to be ingenious and pursue new lines of inquiry.”
The long-term goal of this project is to combine access to new technology with artificial intelligence to determine in real-time whether patients should be referred to a pediatric retinal specialist for further evaluation, expediting early evaluation and treatment of possible disease.
“Dr. Vajzovic is just amazing,” said Mark. “She is a tremendous researcher, in addition to an outstanding clinician. And we’re really excited for her research because we know that the funds are in really good hands.”

Christopher Dermarkarian, MD, assistant professor of ophthalmology, joined Duke Eye Center as a member of the Oculofacial and Orbital Surgery Division.
His clinical interests are wide-ranging and include the following: management of eyelid disorders, “droopy eyelids” and eyelid malposition (dermatochalasis, ptosis, entropion, ectropion, etc.), management of eyelid tumors and cancer, reconstruction of the face or eyelids following traumatic injuries or Mohs surgery, brow lifts, cosmetic upper and lower eyelid surgery, medical and surgical management of thyroid eye disease, orbital inflammation and orbital tumors, management of anophthalmic sockets, and management of lacrimal drainage dysfunction.
Dermarkarian completed a prestigious ASOPRS fellowship at the University of California, Irvine after completing his residency training in ophthalmology at Baylor College of Medicine. Dermarkarian received his medical degree from the University of Miami Miller School of Medicine. He received his undergraduate degree from Duke University.
Dermarkarian’s research interests include eyelid and orbital cancers as well as improving treatments outcomes for the most common
oculoplastic procedures.
Outside of work, he enjoys fitness classes, sporting events, cooking, visiting new restaurants and spending time with his family and wife.

Michelle Go, MD, assistant professor of ophthalmology, joined Duke Eye Center Pediatric Ophthalmolgy and Strabismus divsion faculty. She completed a research fellowship, and a pediatric ophthalmology and strabismus surgery fellowship at Duke. Prior to coming back to Duke as faculty, she was an Assistant Professor of Ophthalmology at University of North Carolina..
Go provides specialized medical and surgical treatment for conditions such as tearing, amblyopia, strabismus, pediatric cataract, and childhood glaucoma. Her research interests include home tonometry and OCT imaging in children with glaucoma. She received her BA in Biochemistry and MS in Chemistry from the University of Pennsylvania, PA, and her medical degree from the University of Illinois at Peoria. After an Internal Medicine internship, she completed an Ophthalmology residency and served as Chief Resident at the University of North Carolina School of Medicine.

Arpita Maniar, MD, assistant professor of ophthalmology, joined the newly established Ocular Oncology Division after completing an ocular oncology fellowship at Duke in 2023. She also completed a fellowship in oculoplastics, ocular oncology, orbit and reconstructive surgery at the LV Prasad Eye Institute. Maniar provides comprehensive care for a wide variety of benign and malignant tumors affecting the eye and its surrounding structures, across all age groups. This includes common ocular tumors like melanoma, lymphoma, ocular metastasis and retinoblastoma to eyelid tumors like squamous cell carcinoma and basal cell carcinoma, to less common and rare orbital and ocular surface tumors. She also manages ocular side-effects from systemic chemotherapeutic drugs. She often collaborates with other specialists from radiation oncology, interventional radiology, medical oncology, ENT and neurosurgery to deliver comprehensive cancer care. Her research interests lay in studying ocular melanomas and retinoblastomas. She has published several peer-reviewed journal articles and book chapters on these conditions, and has delivered talks at regional, national and international conferences.
Qiaohui Wei
White, OD, MS, joined Duke Eye Center as Medical Instructor after completing a residency in Pediatric Optometry and Ocular Disease at Duke in 2023. White specializes in myopia management and specialty contact lenses including scleral lenses, aphakic contact lens fitting, and orthokeratology. She also specializes in amblyopia, strabismus, and co-management of pediatric ocular diseases with pediatric eye surgeons.
White earned her Bachelor of Medicine degree in China before completing her Standard Ophthalmology Residency Training in China from 2015–2018. Following that, she obtained her doctorate degree in Optometry in a joint MS/OD program at the New England College of Optometry in Boston, Massachusetts.

Sharon Fekrat, MD, FACS, FASRS, professor of ophthalmology and neurology, has been appointed Vice Chair for Faculty Affairs. She is a distinguished retina specialist, and an accomplished educator and clinical researcher with broad administrative and leadership experience. Fekrat has a proven record of faculty support, mentoring, and faculty development. At Duke, she has held several leadership positions including Vice Chair of the School of Medicine Clinical Sciences Appointments, Promotions, and Tenure Committee, Co-Chair of the 5-year review of department of anesthesiology, Director of Ophthalmology Faculty Mentoring and Career Development, Director of the Vitreoretinal Surgery Fellowship, and she is founder and Director of the iMIND Research Group. She founded and spearheaded Duke Eye Center’s All About Your Eyes for patients, The Duke Manuals of Ophthalmic Surgery for eye surgeons, and Duke Journal of Case Reports in Ophthalmology for ophthalmologists. At Duke’s VA affiliate (Durham VA Health Care System), she has been Chief of Ophthalmology, Interim Chief of Surgery, and is currently Associate Chief of Staff.

Amy Fowler, MD, associate professor of ophthalmology, brings a wealth of experience to the Vice Chair for Clinical Operations. An avid Duke alumna (BS ’93, HS ’02), as a Duke resident she was an inaugural recipient of the K. Alexander Dastgheib Resident Surgery Award. In 2020, she joined the Duke Eye Center oculofacial plastic surgery division. Previously, she served 12 years as the ophthalmology residency director and served as Vice Chair for the UNC department of ophthalmology. During that time, she led the Faculty Compensation Committee and participated in the Outpatient Task Force Committee, which managed clinical operations. She has had extensive experience in a variety of clinical settings including both Duke and UNC hospitals, CMC hospitals, VA Hospitals, community and hospital based ambulatory surgery centers, and private practice clinics. Dr. Fowler has always valued the comradery and world class patient care the Duke Eye Center provides and is excited to support and help further the department’s mission of excellence in her new role.




Catherine Bowes Rickman, PhD, George and Geneva Boguslavsky Distinguished Professor of Eye Research, was honored at the 2023 Future Vision Foundation Award Gala with the Laureate Award for her outstanding research efforts focused on molecular/cell biology and pathobiology of age-related macular degeneration. The foundation showcased Bowes-Rickman’s work with an inspirational film tribute that debuted during the Gala on November 11, 2023 at the Cleveland Institute of Art. Scan the QR Code to view the film.
Oleg Aleskeev, MD, PhD
1 of 4 Duke School of Medicine faculty to receive the 2023 Physician-Scientist Strong Start Award.
Sanjay Asrani, MD Keynote speaker at the Latin American Glaucoma Society Annual Meeting and North Carolina Optometric Society Annual Meeting.
Invited lecturer at the Pan American Ophthalmology Association Annual Meeting, Asia Pacific Ophthalmology Association Annual Meeting, Nordic Glaucoma Society Annual Meeting and World Glaucoma Congress.

Durga Borkar, MD, MMCi
Named Director of Clinical Data Science.
Retina Today’s “One to Watch” in the May/ June Issue.
Inducted into the Retina Society.
Received Women in Ophthalmology Emerging Leader Award.

Catherine Bowes Rickman, PhD
Honored at the 2023 Future Vision Foundation Award
Gala with the Laureate Award.
Delivered the Friedman Lecture at the Harvard Symposium on Age Related Macular Degeneration.



Xi Chen, MD, PhD Inducted into the prestigious Macula Society.

Sharon Fekrat, MD, FACS, FASRS
Newsweek ’s America’s Best Eye Doctors of 2023.
Appointed Vice Chair for Faculty.
Sidney Gospe, MD, PhD
2023 North American NeuroOphthalmology Society Pilot Grant Award for his presentation: “Reducing neuro-inflammation in a mouse model of mitochondrial optic neuropathy.”
Laura Enyedi, MD
Honored with Secretariat Award at American Acadamy of Ophthalmology Annual Meeting.
Sina Farsiu, PhD 2023 Duke Bass Chair, for achieving true excellence in both research and teaching.

Majda
Hadziahmetovic, MD
Retina Today’s One to Watch, August Issue.Received a National Institute of Health R21 grant for her research, “Learning-based 3D modeling of AMD to assess disease progression and response to treatment.” This is a collaboration with Pratt School of Engineering. Co-Investigators include Miroslav Pajic, PhD (Pratt), Anthony Kuo, MD and Glenn Jaffe, MD.
Leon W. Herndon Jr, MD
American Glaucoma Society president.
Named on “The Ophthalmologist” 2023 Power List.
Newsweek ’s America’s Best Eye Doctors of 2023.



Kourtney Houser, MD
Received the Achievement Award at the American Acadamy of Ophthalmology Annual Meeting.
Glenn Jaffe, MD
Newsweek ’s America’s Best Eye Doctors of 2023.
for GA that led to approval of first drug for GA secondary to AMD (Apellis).
Author of Lancet manuscript on pegcetacoplan for treatment of GA.


Katy Liu, MD, PhD
Received the American Glaucoma Society MAPS Award.
Jullia Rosdahl, MD, PhD
Promoted to Associate Professor of Ophthalmology with Tenure. She was elected to serve as a Treasurer of Women in Ophthalmology and will continue to serve on WIO Board of Directors and direct the WIO Clinical Trials Training Program.
Terry Kim, MD
Newsweek ’s America’s Best Eye Doctors of 2023.
Rupalatha Maddala, PhD BrightFocus Foundation National Glaucoma Research Award for her research, “Role of Septin Cytoskeleton in Trabecular Meshwork, IOP and Glaucoma,” with Vasantha Rao, PhD and Pratap Challa, MD as Co-Principal Investigators.
Anthony Kuo, MD
RPB PhysicianScientist Award for his research to extend the capabilities of the ophthalmology imaging system, “Robotically Assisted Anterior Eye Examinations for Acute Eye Care.”

Eleonora Lad, MD, PhD
Named Vice Chair of Clinical Research.
Keynote speaker at the Barkan Day Research Symposium, San Francisco, CA. Faculty leader during Heed resident retreat, and Gifford Lecturer at the Illinois Society of Eye Physicians and Surgeons and the Chicago Ophthalmological Society and 2024 Helen Keller Lecturer at the University of Alabama at Birmingham Department of Ophthalmology and Visual Sciences Annual Symposium.
Primary investigator for first successful registration phase 3 trial
Ramiro Maldonado, MD
Individual Investigator Award from the Foundation for Fighting Blindness, to propel research efforts and advance the field of inherited retinal diseases (IRD) in children.

Goldis Malek, PhD
Recipient of the Rosalind Franklin Society Award in Science for Journal of Ocular Pharmacology and Therapeutics, recognizing outstanding published peer-reviewed research by women and underrepresented minorities in science. She presented the award lecture at the 2023 Association for Ocular Pharmacology and Therapeutics meeting.

Yos Priestley, OD
Received Kids Care Grant of $7,000 in support of patients and families.
Nathan Cheung, OD and Qiaohui “Vivi” Wei White, OD will collaborate on the project.

Daniel Saban, PhD 2024 Cogan Award recipient, presented by the Association for Research in Vision and Ophthalmology. This prestigious award recognizes young researchers that have made significant contributions to research in ophthalmology or visual science, and that show substantial promise for future contributions in this field.

Stefanie Schuman, MD
Promoted to Associate Professor of Ophthalmology.
Daniel Stamer, PhD Honored at the 2023 Association for Research in Vision and Ophthalmology Foundation Gala in recognition of his extraordinary efforts to develop the EyeFind Research Grant and his generous philanthropic support of the Foundation.

Sandra Stinnett, DrPH
Presented with the Distinguished Contributor Award by the American Society of Retina Specialists for outstanding contributions to the Journal of Vitreoretinal Diseases.

Cynthia Toth, MD Lawrence A. Yannuzzi Award, presented by the International Retinal Imaging Society. This award recognizes significant scientific accomplishments in the field of retinal imaging.
Lifetime achievement award at the American Academy of Ophthalmology Annual Meeting.
Delivered the Gisbert Richard Keynote Lecture at the EURETINA 2023 annual meeting on October 7, 2023 in Amsterdam.

Lejla Vajzovic, MD, FASRS
Appointed to serve as Treasurer and Executive Board Member of Women in Ophthalmology, as Director of Women in Ophthalmology Clinical Trial Training Program, as Retina Society AAO Council Representative, as Course co-director for Advances in Pediatric Retina, as Program Committee Member for AAO Eyecelerator Meeting and Hawaiian Eye and Retina Meeting. She was also invited to serve as section editor for the Eye and to serve on editorial boards for Journal of VitreoRetinal Diseases and Retina Today. Several of her mentees have received research awards including VitreoRetinal Surgery Foundation Research Fellowship, VitreoRetinal Surgery Foundation Research Awards, Jack McGovern Coats’ Disease Foundation Travel Grants, and Advances in Pediatric Retina Course NIH Travel Awards.

Lloyd Williams, MD, PhD
Serves as the Secretary and Treasurer for the North Carolina Society of Eye Physicians and Surgeons, and will be inducted as President for 2024-2025 at the upcoming annual meeting.

S. Madison Duff, MD
Best in show award for poster presentation at the American Association for Pediatric Ophthalmology and Strabismus Annual Meeting.
Jullia A. Rosdahl, MD, PhD Associate Professor of Ophthalmology, with tenure
Stephanie Schuman, MD Associate Professor of Ophthalmology
Xi Chen, MD, PhD Associate Professor of Ophthalmology
Kevin Jackson, MD
Best Paper of Session, Surgical Complications, “Comparing IOL Formula Prediction Error after SK/PTK and CEIOL Based on Ablation Pattern” at the American Society of Cataract and Refractive Surgery Annual Meeting.

Vahid Ownagh, MD North Carolina Society of Eye Physicians and Surgeons first place research presentation winner.
Modupe Adetunji, MD
Best in Sub-Specialty Poster Award for her presentation, “Ophthalmic Findings in Pediatric Neuromyelitis Spectrum Disorder” at the Women In Ophthalmology Conference.


Alice Choi, MD 2023-2024 Heed Fellow. Kelly Donovan, MD, PhD 2023 Technician Support award from the Duke Office of Physician Scientist Development.
Rami Gabriel, MD
2022–2023
Machemer Resident Research award for his project “A Novel Approach for Glaucoma Tube Closure”.
Tammy Hsu, MD
Jack McGovern Coats Disease Foundation 2022 Educational Grant.
Meghana Konda, MD
American Society of Cataract and Refractive Surgery Excellence Award for exhibiting exemplary performance in research, patient care, leadership, and education. Women in Retina Grant to attend the American Society of Retina Specialists Annual meeting.

Angela Li, MD and Tammy Hsu, MD
National Eye Institute and National Institute of Heath travel grant to present at the International Advances in Pediatric Retina 2023 conference.
Cason Robbins, MD Best Paper of Session in Surgical Outcomes Category, 2nd Place in the Glaucoma/Retina/ Pediatrics Poster Category, and Honorable Mention in Cataract Poster Category.
Vit-Buckle Society Academic Grant Award for, “Evaluating the retinal architecture and microvasculature in traumatic brain injury using optical coherence tomography angiography,” mentor Sharon Fekrat, MD, FACS, FASRS.
James Tian, MD American Society of Cataract and Refractive Surgery Excellence Award for exhibiting exemplary performance in research, patient care, leadership, and education. He also received the Best Paper of Session Preoperative Tests and IOL Paper Calculations III Category at the 2023 Annual Meeting.
Yuxi Zheng, MD Bulldogger award for best poster presentation at the Vit Buckle Society Annual Meeting. She also received an academic grant. Women in Retina Grant to attend the American Society of Retina Specialists annual meeting for her research, “Myopia is associated with release of vitreomacular traction after cataract surgery” (mentored by Sharon Fekrat MD, FACS, FASRS).

Samuel Alvarez, PhD
Best in show award for poster presentations at 2023 American Association of Pediatric Ophthalmology and Strabismus Meeting.
Third Year Residents (PGY4)
Rami Gabriel, MD
Lucy Hui, MD
Sri Meghana (Meg) Konda, MD
Richmond Woodward, MD
Yuxi Zheng, MD
Second Year Residents (PGY3)
Modupe Adetunji, MD
Kelly Donovan, MD, PhD
Angela Li, MD
Aaron Lindeke-Myers, MD
Richard Morgan, MD, PhD
Cason Robbins, MD
First Year Residents (PGY2)
Juno Cho, MD
Jinwon (Terry) Lee, MD
Keke Liu, MD
Gregory McElroy, MD, PhD
Esteban Peralta Chacon, MD
James Robbins, MD
Interns (PGY1)
Jean Adomfeh, MD
Nicholas Johnson, MD
Emily Jung, MD
Hazem Mousa, MD
Naveen Karthik, MD
Ailin (Irene) Song, MD

Cole Beatty PhD candidate in the Saban Lab, honored with the Cora Verhagen Award for having the best ocular immunology poster or paper presented by a graduate student or post-doctoral fellow at the 2023 Association for Research in Vision and Ophthalmology meeting.
Sahil Aggarwal, MD Glaucoma
Rolake Alabi, MD, PhD V-Retina
Eun Young (Alice) Choi, MD Glaucoma
Elsayed Elbasiony, MD, MSc Ocular Oncology
Alexandra Castillejos Ellenthal,MD Glaucoma
Nickolas Garson, MD Cornea
Alden Gregston, MD Pediatrics
Andrew Gross, MD Glaucoma
Stephanie (Tammy) Hsu, MD
V-Retina
Mustafa Iftikhar, MBBS V-Retina
Olivia Killeen, MD, MS Pediatrics
Gunay Kirimli, MD M-Retina
David Kuo, MD M-Retina
Irene Lee, MD Plastics
Tali Okrent, MD Neuro
Kubra Sarici, MD Retinal Genetics
Rohini Sigireddi, MD Pediatrics
Bonnie Sklar, MD Cornea
Sudip Thakar, MD Plastics
Yunbo (James) Tian, MD Cornea
Ramyar Torabi, MD Plastics
Christopher Turski, MD M-Retina
Heidi Volos, MD Pediatric Optometry
Stephen Yoon, MD Glaucoma
Xiao (Ellie) Zhou, MD V-Retina


Michael De Leso, PhD
2nd Place Research Poster at the International Society of Eye Research.
Ekta Mayur Dembla, PhD Postdoc in Kay Lab received the Ruth K. Broad Foundation Postdoctoral Fellowship for the academic year 2024.
 Leon W. Herndon Jr, MD Professor of Ophthalmology
Leon W. Herndon Jr, MD
Leon W. Herndon Jr, MD Professor of Ophthalmology
Leon W. Herndon Jr, MD
I have been honored to serve as the 21st president of the American Glaucoma Society (AGS). I first became a member of AGS in the year 2000 and have been amazed to witness the growth of the organization which now represents over 1,600 glaucoma specialists in the country.
I served on the AGS Board several years ago, then again more recently, and was nominated and elected by my peers to serve as PresidentElect, then President. My term as President concluded at the end of our annual meeting in Huntington Beach early March 2024.
As a young glaucoma specialist, I never envisioned the day that I would become President of our organization…did not think I had the “smarts” to lead such a highly regarded society. I just kept busy in my clinical practice, and in my educational responsibilities, and saw that I could help to make a difference in the care of glaucoma patients.
“We have been successful in our efforts to increase public awareness of glaucoma, and I am proud that I was a driving force to form a coalition of like-minded organizations to establish programs to bring glaucoma to the forefront.”
I am passionate about spreading the word about the importance of glaucoma screening, as half the patients who have glaucoma don’t know they have it. We have been successful in our efforts to increase public awareness of glaucoma, and I am proud that I was a driving force to form a coalition of like-minded organizations to establish programs to bring glaucoma to the forefront. We have also worked on a program to increase efforts to screen family members of those with glaucoma, as we know the greatest risk of being diagnosed with glaucoma is if one has a family member with glaucoma.
Advocacy for our profession is a big part of my job, and we worked with sister organizations to push back efforts from Medicare carriers to halt the coverage of certain glaucoma procedures. Now patients and their glaucoma surgeons have a choice in their glaucoma surgical care.
I have also been proud that we took our diversity, equity, and inclusion task force to full committee status to ensure that all voices of our membership are heard.
Serving as the President of AGS has been the honor of a lifetime, and I hope that our administration has created programs that will have a lasting impact on the lives of our glaucoma patients.

Sarah Hadyniak, PhD
Kay Lab postdoc received the Hartwell Foundation postdoctoral fellowship, supporting her research for the next two years.


Sejal Patel Undergraduate Research Support Assistantship Funding (mentor Sharon Fekrat MD, FACS, FASRS).
Maria Fernanda Suarez, PhD Stamer Lab research associate, received outstanding poster presentation by American Society for Matrix Biology at the Biennal Joint Meeting (ASMB, ASIP and HCS) for the poster titled: LOXL1 deficiency reduces TGFß1induced fibrosis in Trabecular Meshwwork cells/tissues.

Juan Valdez-Lopez, PhD
Kay Lab postdoc awarded a F32 NRSA postdoctoral fellowship from the National Eye Institute, supporting his research over the next three years.


Isabel Hugar, CRA ASCRS OPS exhibit, honorable mention.

Christopher Keth, BA, CRA
ASCRS OPS exhibit, honorable mention.
OPS exhibit at AAO, Second Place in Stereo Wide Angle Fundus Photo Division.

Christiaan Lopez-Miro, BA Haag-Streit Slit Lamp Imaging Competition.
ASCRS OPS exhibit, honorable mention.
OPS Exhibit at AAO, First Place in the Video Category: Giant Cell Arteritis, Second Place in the Fluorescein Angiography Category: Unknown Third Place in the Fluorescein Angiography Category: Sickle Cell Retinopathy, Honorable Mention in Gonio Photography: Unknown, Honorable Mention in Ultra-Widefield Imaging: Choroidal Detachment with Retinal Tear.

Brian Lutman, CRA ASCRS OPS exhibit, 2nd place in the ICG Anagram category.

Kathleen Warren, CPT, OCT-C Haag-Streit Slit Lamp Imaging Competition, 3rd place for “Epithelial ingrowth.”
ASCRS OPS exhibit, honorable mention.
OPS Exhibit at AAO, Third Place in Eye as Art: Cue the Eye Ball, Honorable Mention in the Fluorescein Angiography Category: Scleral Buckle with Silicone Oil.
Veronica Jones, BA ASCRS OPS exhibit, received first place in two categories, Eye of Art and Gonio Photography.
The VRSF Awards fund early-stage investigators who are conducting relevant research projects in macular and retinal disease, and to encourage a career devoted to retinal disease and research.

Vahid Ownagh, MD 2024 Vitreoretinal Surgery Foundation Research Fellowship, a prestigious award that includes a $10,000 grant in support of his research. He is the first Duke Trainee to receive this award. Optimizing vitrectomy technique and parameters for subretinal gene therapy: An intraoperative OCT based volumetric study (mentored by Lejla Vajzovic, MD, FASRS).
Kelly R. Donovan, MD, PhD
Elucidating the role of EYS in the pathogenesis of retinitis pigmentosa (mentored by Vadim Y. Arshavsky, PhD).
Lindsey A. Chew
Applying artificial intelligence to pediatric retinal screening based on ultra-widefield fundus imaging (mentored by Lejla Vajzovic, MD, FASRS).

Nikhil V. Gadiraju Implementation of ultra-wide field fundus photography for pediatric retinal screening within a primary care setting (mentored by Lejla Vajzovic, MD, FASRS).

Jamie J. Karl
Longitudinal analysis of optical coherence tomography (OCT) and OCT angiography in patients with multiple sclerosis (mentored by Sharon Fekrat, MD, FACS, FASRS).
Jinwon (Terry) Lee, MD
Predicting early hydroxychloroquine retinopathy using deep learning (mentored by Eleonora G. Lad, MD, PhD).
>
Katy Liu, MD, PhD Received the Career Development Grant, this grant provides outstanding earlycareer vision scientists with significant support over 4 years, as a means to start and sustain an independent research program.

Jeremy Kay, PhD Received the Stein Innovation Award that provides funds to proposed high-risk / high-gain vision science research.
Yuxi Zheng, MD and Kelly Donovan, MD, PhD Each received a Small Pilot Research Award, which is supported by the Duke Eye Center’s Unrestricted Annual Research to Prevent Blindness Grant.

Select Photography Award Images, clockwise from top left: Posterior Uveitis by Christopher Keth, BA, CRA; Santos Klimt by Veronica Jones, BA; Sickle Cell Retinopathy by Christiaan Lopez-Miro; Choroidal Detachment with Retinal Tear by Christiaan Lopez-Miro.

The Duke Journal of Case Reports in Ophthalmology (DJCRO) is an open access, fully online, digital international journal. All submissions must be original, previously unpublished, within the scope of the journal, of good quality, and presented in an educational format with a clear, concise structure. Submissions must adhere to the DJCRO rules and guidelines herein or they will be returned to the author before review. There are no fees for submitting, publishing, viewing, or downloading DJCRO articles. Follow us on social media:




The Duke Ophthalmic Technician Program is a 1-year allied health certificate program that prepares students for the certified ophthalmic technician exam and an excellent career in eye care.
Offered by the Duke School of Medicine for almost 40 years, Duke Ophthalmic Technician Program includes interactive classroom work and wet labs for the first three months and nine months of hands-on clinical rotations that take place at Duke Eye Center clinics.
Benefits of the Duke Ophthalmic Technician Program
Students may begin the program after earning a high school diploma
No college degree or prerequisites required
Earn a certificate in one year with eligibility to take the certification exam
Nine months spent getting hands on experience in clinical rotations at Duke Eye Center
Starting pay $22–$24/hr
90% employment rate after program completion
Affordable tuition and financial aid is available

Learn more about the program and access the application.

Fellows Advanced Vitreous Surgery Course
March 22–23
Lecures by Distinguished Guest Faculty and Duke Eye Center
Medical and Surgical Vitreoretinal Faculty; Comprehensive and innovative wetlab for fellows who attend
Visiting Science Lecture
April 11
Valeria Canto-Soler, PhD
Doni Solich Family Chair in Ocular Stem Cell Research Director of CellSight
University of Colorado School of Medicine
Visiting Science Lecture
April 24
Joshua Stein, MD
Frederick G. L. Huetwell Professor of Ophthalmology and Visual Sciences
University of Michigan Institute for Healthcare Policy and Innovation
Stephen and Frances Foster Lecture
May 14
Eric Pearlman, PhD
Director, Institute for Immunology Professor, Physiology and Biophysics Professor, Ophthalmology
University of California, Irvine School of Medicine
Joseph M. Bryan Lecture
May 20
Arlene Drack, MD
Professor of Ophthalmology and Visual Sciences
Professor of Pediatrics
Ronald V. Keech, MD, Professor of Pediatric Genetic Eye Disease Research
Director of the Kolder Electrophysiology Service
Trainee Day Scientific Sessions
June 21
Keynote: Kathryn Colby, MD, PhD
Elisabeth J Cohen Professor and Department Chairman
NYU Grossman School of Medicine
Department of Ophthalmology
*Eligible for 6 hours of CME credit
Dastgheib Pioneer Award in Ocular Innovation Lecture
September 25
Joseph Carroll, PhD
Richard O. Schultz, MD
Ruth Works Professor of Ophthalmology
Professor of Ophthalmology & Visual Sciences, Biophysics, and Cell Biology, Neurobiology
Anatomy Director, Advanced Ocular Imaging Program
Medical College of Wisconsin
Duke Glaucoma Symposium and Fellows Course
October 5–6
Keynote Speakers from Duke, UNC and Wake Forest Universities
*Eligible for 6 hours of CME credit
2024 Duke Eye Center Alumni Reception
October 19
Renaissance Chicago Downtown Chicago, IL
Benign Essential Blepharospasm Research Foundation (BEBRF) Symposium
November 2
Program Director: Julie Woodward, MD
Mittra Family Foundation Lecture
November 12
Prithvi Mruthyunjaya, MD
Professor of Ophthalmology and Radiation Oncology
Stanford Byers Eye Institute
Joseph M. Bryan Lecture
December 12
Lois E. H. Smith, MD, PhD
Professor of Ophthalmology
Harvard Medical School
2024 Grand Rounds
April 23
May 29
September 10
October 8
November 22
December 6
*Eligible for 1 hour of CME credit
Duke Eye on Education Series
May 6
November 4
*Eligible for 2 hours of CME credit
Visit our website for events listings and more information.
The Duke Fellows Advanced Surgery Course (fAVS) will marked its 10th year in 2024. One of the first vitreoretinal surgery courses for fellows, it is now led by Lejla Vajzovic, MD, FASRS, Duke vitreoretinal surgery fellowship director. Duke fAVS has become the premier educational course for retina fellows across the world, attracting more than 90 fellows each year.
Duke fAVS is based on the Duke Advanced Vitreoretinal Surgery Course (AVS) which was established more than 40 years ago by Robert Machemer, MD, “father of retina surgery” and former chair of Duke Ophthalmology. The first of its type in the world at that time, Duke AVS has served as the model for subsequent national and international vitreoretinal courses. Duke AVS is held bi-annually and intended for retina specialists already in practice.
The annual Duke fAVS meeting is a practical course geared toward first-year vitreoretinal fellows, medical retina fellows, and uveitis fellows, training primarily in North America, with a limited number of international fellows accepted.
Packed with extensive educational content, Duke fAVS participants learn from medical and surgical panel discussions, surgical video tricks and tips, and an unparalleled wet lab experience with access to some of the latest technology and cutting-edge procedures with one-on-one faculty/fellow interaction.
The course provides an opportunity for fellows to connect with worldrenowned faculty, industry representatives, and senior colleagues in the field of retina. All fellows have a unique opportunity to directly compare sustained release technology, implants, 3D visualization systems, microscopes, intraoperative OCT machines, vitrectomy machines, forceps, laser probes, subretinal delivery devices, and a range of other tools across manufacturers.
We are proud of this milestone anniversary and look forward to many years of training the next generation of retina experts.
The annual Duke fAVS meeting is a practical course geared toward first-year vitreoretinal fellows, medical retina fellows, and uveitis fellows training primarily in North America, with a limited number of international fellows accepted.

Edward G. Buckley, MD Chair, Department of Ophthalmology
Vice Dean of Medical Education
Duke University School of Medicine
Vice Chancellor Duke-NUS Affairs
Vadim Arshavsky, PhD Co-Vice Chair, Basic Science Research Scientific Director of Research
Sharon Fekrat, MD, FASRS Vice Chair, Faculty Associate Chief of Staff Durham Veterans Affairs Health Care System
Amy M. Fowler, MD Vice Chair, Clinical Affairs Director of Ambulatory Surgery for Ophthalmology, Medical Director of Hudson
Anthony Kuo, MD Vice Chair, Technology Director of Research Data
Eleonora Lad, MD, PhD Vice Chair, Clinical and Translational Research Research Quality Officer
Goldis Malek, PhD Vice Chair, Diversity Equity and Inclusion
Daniel W. Stamer, PhD Co-Vice Chair, Basic Science Research
Sanjay Asrani, MD Medical Director
Duke Eye Center, Cary
Christopher S. Boehlke, MD Medical Director
Duke Eye Center, Raleigh
Laura Enyedi, MD Medical Director
Duke Eye Center, South Durham
Frank J. Moya, MD Medical Director
Duke Eye Center, Winston Salem
Robin R. Vann, MD Medical Director
Duke Eye Center, Arringdon Perioperative Services
Prithu Mettu, MD Medical Director, Retina Injections
Miguel Materin, MD Medical Director, Duke Eye Center OR Director, Ophthalmic Imaging Director, Ophthalmic Oncology
Julie Woodward, MD Medical Director, Duke Oculofacial Plastic Surgery and Director, Faculty Mentoring and Career Development
Glenn J. Jaffe, MD Director, Duke Reading Center
Durga Borkar, MD, MMCi Director, Clinical Data Science
P. Vasantha Rao, PhD Chair, Department APT Committee
Lloyd Williams, MD, PhD Director of Global Health Director of Refractive Surgery Service
Kelly Muir, MD, MHSc Chief, Division of Ophthalmology, Durham Veterans Affairs Medical Center
Divakar Gupta, MD Access Champion
Stefanie G. Schuman, MD Patient Experience Representative
Nicola (Nicky) Kim, MD Committee Chair for Credentialing and QI/ QA for the department
Division Leadership Melissa Daluvoy, MD – Interim Cornea, External Disease and Refractive Surgery Division
Sharon F. Freedman, MD – Pediatric Ophthalmology and Strabismus Division
Leon W. Herndon, MD – Glaucoma Division
Anupama Horne, MD – Comprehensive
Division
Glenn J. Jaffe, MD – Vitreoretinal Division
N. Troy Tagg, MD – Neuro Ophthalmology
Diane Whitaker, OD – Vision Rehabilitation and Performance Division
Julie A. Woodward, MD – Oculofacial Division
Catherine Bowes Rickman, PhD Director, Third-Year Medical Student Program
Pratap Challa, MD Director, Residency Program
Nathan Cheung, OD Director, Optometry Education
Kourtney Houser, MD Director, Cornea, External Disease and Refractive Surgery Fellowship
Medical Director, Ophthalmic Technician Program
Sharon F. Freedman, MD Director, Pediatric Ophthalmology Fellowship
Miguel Materin, MD Director, Ophthalmic Oncology and Pathology Fellowship
Prithu Mettu, MD Director, Medical Retina Fellowship
Kelly Muir, MD, MHSc Director, Ophthalmology Fellowship Program
Director, Glaucoma Fellowship
Jullia A. Rosdahl, MD, PhD Director, Medical Student Education Director, Patient Education Chief Wellness Officer
Lejla Vajzovic, MD, FASRS Director, Ophthalmology Continuing Medical Education Program
Director, Vitreoretinal Surgery Fellowship
Julie A. Woodward, MD Director, Oculofacial and Orbital Surgery Fellowship
Elizabeth Hunter, MHA, CFM Chief Administrator
Jessica Habecker, MBA Director of Finance
Martha Dellinger, MHA Division Administrator
Tammy Clay, MHA Division Administrator
Heidi Campbell, COT Director of Clinical Operations
George Toutloff, MBA Grants and Contracts Manager
Sarah Jones, MS, CCRC Research Practice Manager
COMPREHENSIVE OPHTHALMOLOGY
Rabia Ali, OD Assistant Professor of Ophthalmology
Melissa Barbour, OD Assistant Professor of Ophthalmology
Anna Bordelon, MD Assistant Professor of Ophthalmology
Thomas S. Devetski, OD Assistant Professor of Ophthalmology
Anupama Horne, MD Assistant Professor of Ophthalmology
Thomas Hunter, MD Assistant Professor of Ophthalmology
Charlene James, OD Assistant Professor of Ophthalmology
Nicola (Nicky) Kim, MD Associate Professor of Ophthalmology
Jeffrey Kozlowski, OD Medical Instructor
Tina K. Singh, MD Assistant Professor of Ophthalmology
Robin R. Vann, MD Associate Professor of Ophthalmology
Christopher S. Boehlke, MD Assistant Professor of Ophthalmology
Corina Busuioc, OD Medical Instructor in the Department of Ophthalmology
Alan N. Carlson, MD Professor of Ophthalmology
Melissa Daluvoy, MD Associate Professor of Ophthalmology
Amber Hoang, MD Medical Instructor in the Department of Ophthalmology
Kourtney Houser, MD Assistant Professor of Ophthalmology
Terry Kim, MD Professor of Ophthalmology
Anthony Kuo, MD Associate Professor of Ophthalmology Assistant Professor in Biomedical Engineering ++
Terry Semchyshyn, MD Assistant Professor of Ophthalmology
Amol Sura, MD Medical Instructor in the Department of Ophthalmology
Lloyd Williams, MD, PhD Assistant Professor of Ophthalmology
C. Ellis Wisely, MD, MBA Assistant Professor of Ophthalmology
GLAUCOMA
Sanjay Asrani, MD Professor of Ophthalmology
Pratap Challa, MD Professor of Ophthalmology
Divakar Gupta, MD Associate Professor of Ophthalmology
Leon W. Herndon, MD Professor of Ophthalmology
Katy Liu, MD, PhD Medical Instructor in the Department of Ophthalmology
Stuart J. McKinnon, MD, PhD Associate Professor of Ophthalmology
Associate Professor in Neurobiology ++
Frank J. Moya, MD Assistant Professor of Ophthalmology
Kelly W. Muir, MD, MHSc Associate Professor of Ophthalmology
Jullia Rosdahl, MD, PhD Associate Professor of Ophthalmology
Henry Tseng, MD, PhD Associate Professor of Ophthalmology
Joanne Wen, MD Associate Professor of Ophthalmology
VISION REHABILITATION AND PERFORMANCE
Diane Whitaker, OD Assistant Professor of Ophthalmology
Madison Dunning, OD Medical Instructor in the Department of Ophthalmology
NEURO-OPHTHALMOLOGY
Mays Dairi, MD Associate Professor of Ophthalmology
Sidney Gospe III, MD, PhD Assistant Professor of Ophthalmology
N. Troy Tagg, MD Associate Professor of Ophthalmology
OCULOPLASTICS
Christopher Dermarkarian, MD Assistant Professor of Ophthalmology
Amy M. Fowler, MD Associate Professor of Ophthalmology
Jason Liss, MD Assistant Professor of Ophthalmology
Julie A. Woodward, MD Professor of Ophthalmology Professor in Dermatology ++
PEDIATRIC OPHTHALMOLOGY AND STRABISMUS
Edward G. Buckley, MD Gills Professor of Ophthalmology Professor in Pediatrics ++
Nathan Cheung, OD Assistant Professor of Ophthalmology
Laura B. Enyedi, MD Professor of Ophthalmology Associate Professor in Pediatrics ++
Sharon F. Freedman, MD Professor of Ophthalmology Professor in Pediatrics ++
S. Grace Prakalapakorn, Associate Professor of Ophthalmology
MD, MPH Associate Professor in Pediatrics ++
Michelle Go, MD Assistant Professor of Ophthalmology
Qiaohui Wei White, OD Medical Instructor in the Department of Ophthalmology
Yos Priestley, OD, FAAO Assistant Professor of Ophthalmology
Secondary appointment
OCULAR ONCOLOGY
Miguel Materin, MD Professor of Ophthalmology Professor of Radiation Oncology++
Arpita Maniar, MBBS, MD Assistant Professor of Ophthalmology
Oleg Alekseev, MD, PhD Medical Instructor in the Department of Ophthalmology
Michael Allingham, MD, PhD Assistant Professor of Ophthalmology
Durga Borkar, MD Assistant Professor of Ophthalmology
Xi Chen, MD, PhD Associate Professor of Ophthalmology
Scott W. Cousins, MD Robert Machemer, MD Professor of Ophthalmology
Professor in Immunology ++
Sharon Fekrat, MD, FACS, FASRS Professor of Ophthalmology
Associate Professor of Surgery
Dilraj Grewal, MD Associate Professor of Ophthalmology
Majda Hadziahmetovic, MD Assistant Professor of Ophthalmology
Glenn J. Jaffe, MD Robert Machemer, MD Professor of Ophthalmology
Eleonora Lad, MD, PhD Associate Professor of Ophthalmology
Stuart McKinnon, MD, PhD Associate Professor of Ophthalmology
Prithu Mettu, MD Assistant Professor of Ophthalmology
Stefanie G. Schuman, MD Associate Professor of Ophthalmology
Cynthia A. Toth, MD Joseph A.C. Wadsworth Professor of Ophthalmology
Professor in Biomedical Engineering++
Lejla Vajzovic, MD Associate Professor of Ophthalmology
Vadim Arshavsky, PhD Helena Rubinstein Foundation Professor of Ophthalmology
Professor in Pharmacology & Cancer Biology ++
Catherine Bowes Rickman, PhD George and Geneva Boguslavsky Professor of Eye Research
Professor in Cell Biology
Sina Farsiu, PhD Professor of Biomedical Engineering and Ophthalmology
Associate Professor in Electrical and Computer Engineering++, Professor in Computer Science++
Paulo Ferreira, PhD Associate Professor of Ophthalmology
Associate Professor in Pathology ++
Jeremy Kay, PhD Associate Professor of Neurobiology
Associate Professor of Ophthalmology, Associate Professor in Cell Biology ++
Paloma Liton, PhD Professor of Ophthalmology
Associate Professor in Pathology ++
Goldis Malek, PhD Associate Professor of Ophthalmology
Associate Professor in Pathology
P. Vasantha Rao, PhD Richard and Kit Barkhouser Professor of Ophthalmology
Professor in Pharmacology & Cancer Biology
Daniel R. Saban, PhD, MS Associate Professor of Ophthalmology
Associate Professor in Immunology ++
Nikolai Skiba, PhD Associate Professor of Ophthalmology
W. Daniel Stamer, PhD Joseph A.C. Wadsworth Professor of Ophthalmology
Professor in Biomedical Engineering++
Sandra Stinnett, DrPH Associate Professor of Biostatistics & Bioinformatics
Associate Professor in Ophthalmology ++
Fulton Wong, PhD Professor Emeritus of Ophthalmology
Professor in Neurobiology and Pathology ++, Assistant Professor in Pathology ++