ALUMNINOTES
I N T E R V I E W with
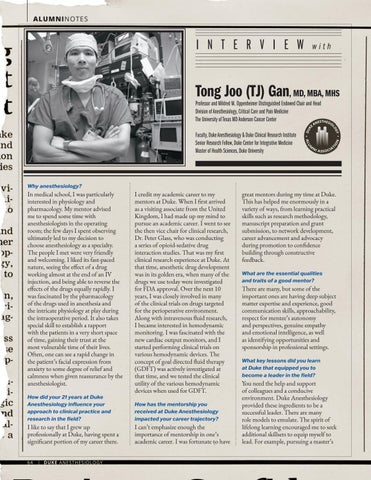
Tong Joo (TJ) Gan, MD, MBA, MHS Professor and Mildred M. Oppenheimer Distinguished Endowed Chair and Head Division of Anesthesiology, Critical Care and Pain Medicine The University of Texas MD Anderson Cancer Center Faculty, Duke Anesthesiology & Duke Clinical Research Institute Senior Research Fellow, Duke Center for Integrative Medicine Master of Health Sciences, Duke University
Why anesthesiology?
In medical school, I was particularly interested in physiology and pharmacology. My mentor advised me to spend some time with anesthesiologists in the operating room; the few days I spent observing ultimately led to my decision to choose anesthesiology as a specialty. The people I met were very friendly and welcoming. I liked its fast-paced nature, seeing the effect of a drug working almost at the end of an IV injection, and being able to reverse the effects of the drugs equally rapidly. I was fascinated by the pharmacology of the drugs used in anesthesia and the intricate physiology at play during the intraoperative period. It also takes special skill to establish a rapport with the patients in a very short space of time, gaining their trust at the most vulnerable time of their lives. Often, one can see a rapid change in the patient’s facial expression from anxiety to some degree of relief and calmness when given reassurance by the anesthesiologist. How did your 21 years at Duke Anesthesiology influence your approach to clinical practice and research in the field?
I like to say that I grew up professionally at Duke, having spent a significant portion of my career there. 64
| DUKE ANESTHESIOLOGY
I credit my academic career to my mentors at Duke. When I first arrived as a visiting associate from the United Kingdom, I had made up my mind to pursue an academic career. I went to see the then vice chair for clinical research, Dr. Peter Glass, who was conducting a series of opioid-sedative drug interaction studies. That was my first clinical research experience at Duke. At that time, anesthetic drug development was in its golden era, when many of the drugs we use today were investigated for FDA approval. Over the next 10 years, I was closely involved in many of the clinical trials on drugs targeted for the perioperative environment. Along with intravenous fluid research, I became interested in hemodynamic monitoring. I was fascinated with the new cardiac output monitors, and I started performing clinical trials on various hemodynamic devices. The concept of goal directed fluid therapy (GDFT) was actively investigated at that time, and we tested the clinical utility of the various hemodynamic devices when used for GDFT. How has the mentorship you received at Duke Anesthesiology impacted your career trajectory?
I can’t emphasize enough the importance of mentorship in one’s academic career. I was fortunate to have
great mentors during my time at Duke. This has helped me enormously in a variety of ways, from learning practical skills such as research methodology, manuscript preparation and grant submission, to network development, career advancement and advocacy during promotion to confidence building through constructive feedback. What are the essential qualities and traits of a good mentor?
There are many, but some of the important ones are having deep subject matter expertise and experience, good communication skills, approachability, respect for mentee’s autonomy and perspectives, genuine empathy and emotional intelligence, as well as identifying opportunities and sponsorship in professional settings. What key lessons did you learn at Duke that equipped you to become a leader in the field?
You need the help and support of colleagues and a conducive environment. Duke Anesthesiology provided these ingredients to be a successful leader. There are many role models to emulate. The spirit of lifelong learning encouraged me to seek additional skillsets to equip myself to lead. For example, pursuing a master’s