7 minute read
Trauma: The Pandemic of the Mind - Anjli Garg, Diya Marwah
Trauma: The Pandemic of the Mind
Anjli Garg, Diya Marwah, Mariam Usmani, Zoya Asim
Advertisement
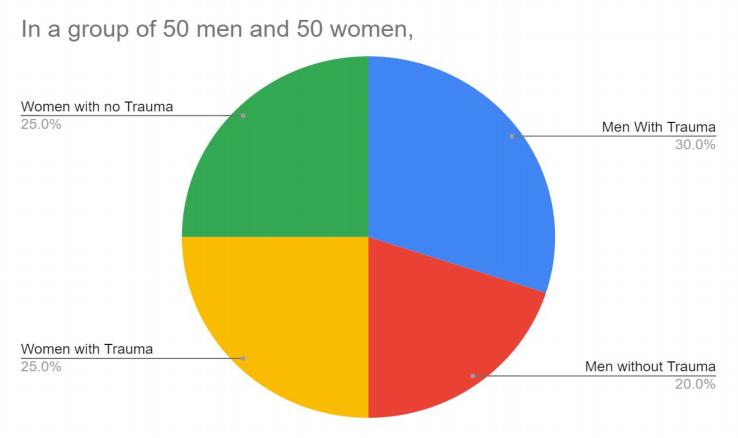
“Through the words of Gilbert Parker, the once prominent novelist and politician, “Memory is man’s greatest friend and worst enemy ” . From a statistical perspective, 60% of men and 50% of women experience trauma. Trauma is common; it is the psychological injury and consequence of experiencing one or more distressing incidents. But how does our trauma affect us, our brain and our memory?
Acute trauma is a result of suffering from a single traumatic event occurring, such as an accident, being a victim of a crime, or even due to a natural disaster. However, if the trauma is repeated and prolonged for more than six months, for example relapsed traumatic episodes of highly stressful events, it can be classed as chronic trauma. Chronic trauma often emerges when the perpetrator is a known individual to the victim, and the event exhibits a behavioural pattern. Living with chronic trauma tends to be overwhelming and enervating; in a report published by Paper Dolls Research Group, survivors were seen to liken the feeling to “bruises, ” “ walls, ” “bullets, ” “a nightmare” and “the inability to see” - with the word “pain” arising frequently. It often has lasting effects on both a person’s physical and mental health, and on one’s sense of identity. Due to the erosive and long-term nature of chronic trauma, where survivors perceive things to be getting worse before they get better, survivors may not recognise the full extent of the abuse that occurred and may also face isolation and a lack of support from others.
Acute trauma can cause permanent brain damage by affecting your ability to process and store information, a fundamental function of memory (the inability to do so could ultimately lead to memory loss). Additionally, it has been scientifically evident that patients with a history of trauma, depression, or even stress are more likely to form false memories - fabricated memories of events that did not take place. Traumatic incidents negatively impact your psyche and daily life, however, resolving trauma is not an easy task and if left ‘ignored’ it can do more harm than good. Over time, our memory works to delete information, and as a result we lose certain memories, forget details of those we do retain, and alter aspects of other memories as the result of our constant retrievals numerically, 15% to 38% of known trauma survivors fail to recall their experiences. Memories of trauma have important characteristics that make them appear different from normal, everyday memories. After experiencing a traumatizing event,
several studies have shown that it may be remembered forever and this is an adaptive outcome as the brain responds by clutching onto the memory in hopes of confronting it later.
The brain has been able to learn that “this is important, remember this because it could later save your life. ” However, the more the trauma is ignored, the more your body will hold onto it; it needs to be processed consciously and in a professional manner in order for the trauma to be overcome.
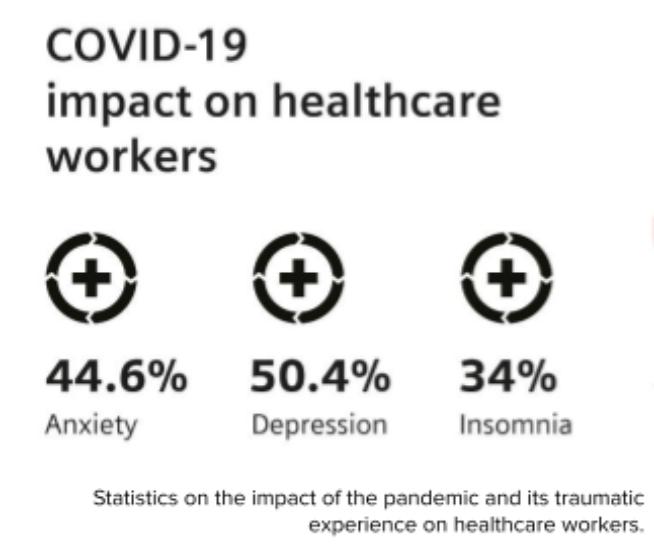
Complex trauma is when a lifetime of distressing and shocking events accumulate over a long-term period. It is the result of exposure to multiple traumatic events that often leaves many individuals to believe life is nothing more than their trauma. This arises from situations like an unsolved kidnapping or children who are given a lack of warmth and praise in their childhood. A notable example of complex trauma is Post-Traumatic Stress Disorder, which can be developed after an individual experiences or witnesses a shocking or distressing incident and its aftermath, such as natural disasters, war or combat, etc. Covid19 has brought about huge numbers of distressing incidents around the world, most obviously, death and prolonged illness of loved ones. Others have witnessed friends and close relatives being made unemployed and forced to relocate with their survival being under threat. Covid-19 has and is still creating unknown levels of complex trauma with potentially permanent effects on the generations of people involved. Complex trauma can lead to significant effects like constant stress and negative thoughts, emotions and beliefs about yourself or the world. Complex traumas can disrupt healthy development and increase the risk of many other mental health issues. This is unlimited to depression, anxiety, eating disorders, suicidal thoughts, as well as drug and alcohol abuse, although time may have passed from the occurrence of the event - this does not bode well for people in the years following Covid19. If the trauma is not overcome, it can often lead to shame and disappointment that only worsens the condition. Overall, there are many long-term effects that can cause significant deteriorations in the day-to-day lives of those struggling with the disorder.
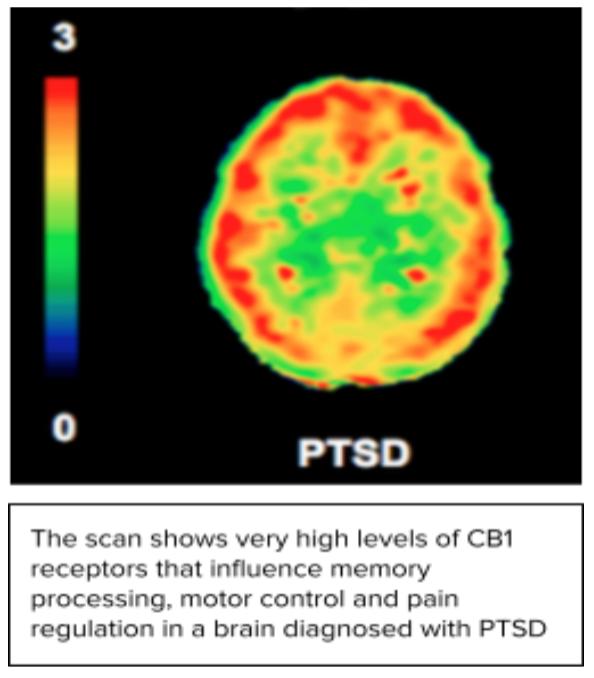
It has been proven that complex traumas can often lead to structural changes in the brain including the enlargement of the amygdala (the alarm center of the brain) and the shrinkage of the hippocampus (the part critical to remembering the event that happened). These structural changes can lead to altered brain activity such as an increase in stress hormones; this can ultimately result in other psychiatric disorders. The shrinkage of the hippocampus impairs an individual's ability to experience and regulate a healthy range of emotions and prevents the consolidation of memories that allow an individual to move on from the trauma. The amygdala contains implicit and fragile memories of the trauma, and this ability is heightened and therefore triggers often lead to the arousal of fragmented memories of a traumatic event.
This can be seen in Ehlers’ and Clark’s cognitive model of Post-Traumatic Stress Disorder where the nature of traumatic memory is depicted to be “fragmented, readily primed and triggered, and poorly contextualized into memory. ” As a result, memories of traumatic events, for example an instance of sexual assault, can be disjointed and difficult to recollect in a complete or linear way. Nevertheless, the effect on memory differs from person to person, as some are able to recall the traumatic incident clearly (depicted through flashbulb memories), whilst others suffer from amnesia with regards to major parts of their memories.
Trauma survivors might be in a constant state of stress and fear; they perceive life for all its negativity and may not recognise the full extent of their abuse. Since your body holds on to your trauma in hopes of addressing it in the future, if left untreated, it can result in a psychological chain reaction of illnesses like depression. Therapy is usually the first response for treatment, possibly in the form of somatic experiencing and psychotherapy. Somatic experiencing therapy utilises mind and body exercises to release repressed trauma from the victim’s subconscious and conscious self. Aside from that, psychotherapy, or talk therapy, helps people achieve a deeper understanding of what triggers their symptoms by encouraging them to open up and explore their thoughts. Overall, therapy allows victims to identify safer coping mechanisms to confront their trauma and progress onwards from their psychological distress. Considering this and our desire to recover from our current, trauma-inducing time period, we should as a society make therapy more readily available for those who are suffering.
While therapy is usually effective for most, individuals may need to resort to medications. Trauma patients respond to ‘threat’ differently and their ‘fight or flight’ response is easily triggered; they have an abnormal release of neurotransmitters in the brain and may be easily susceptible to depression and anxiety. Hence, medications like Selective Serotonin Reuptake Inhibitors (SSRI) and SerotoninNorepinephrine Reuptake Inhibitors (SNRI) are used. SSRIs include Fluoxetine, Paroxetine and Sertraline; these drugs increase levels of serotonin by preventing its re-absorption into neurons. SNRIs include Venlafaxine, these medications regulate the balance of serotonin and norepinephrine. Both SSRI and SNRI drugs improve mood stabilisation, feelings of wellbeing, happiness and the ability to cope.
Trauma can take control of a person’s entire mind and body; it can change your brain’s structural features, which results in incoherent and implicative memories. These memories aren’t perfectly recalled, can be reconstructed and forgotten. For example, many victims suffer from amnesia and forget major parts of their trauma; in a study investigating the memories of adult survivors of sexual abuse, psychologists found that 31% of participants reported no memories of their abuse and were unable to recall the incidents. However, in some cases
trauma can augment memories as ‘flashbulb memories’ - they are extremely vivid and comprehensive memories of shocking or traumatic events that are retained for a lifetime and continue to trigger emotions and feelings. Therefore, different victims remember their traumas differently memories can be fragmented and forgotten or remembered as graphically as a screenshot. Ultimately, this may even affect how an individual copes and approaches their traumatic experiences. Nevertheless, as Peter A. Levine remarks, “Trauma is a fact of life. It does not, however, have to be a life sentence” .




