7 minute read
The Power of Measuring Light in the Field
from Aug 2025
By Mariana G. Figueiro, PHD - Light and Health Research Center at Mount Sinai
The hallmark of the Lighting Research Center (LRC) and the Light and Health Research Center (LHRC) at Mount Sinai has been our commitment to the measurement and characterization of light.
Our commitment draws inspiration from H. James Harrington’s observation that “measurement is the first step that leads to control and eventually to improvement. If you can’t measure something, you can’t understand it. If you can’t understand it, you can’t control it. If you can’t control it, you can’t improve it.”
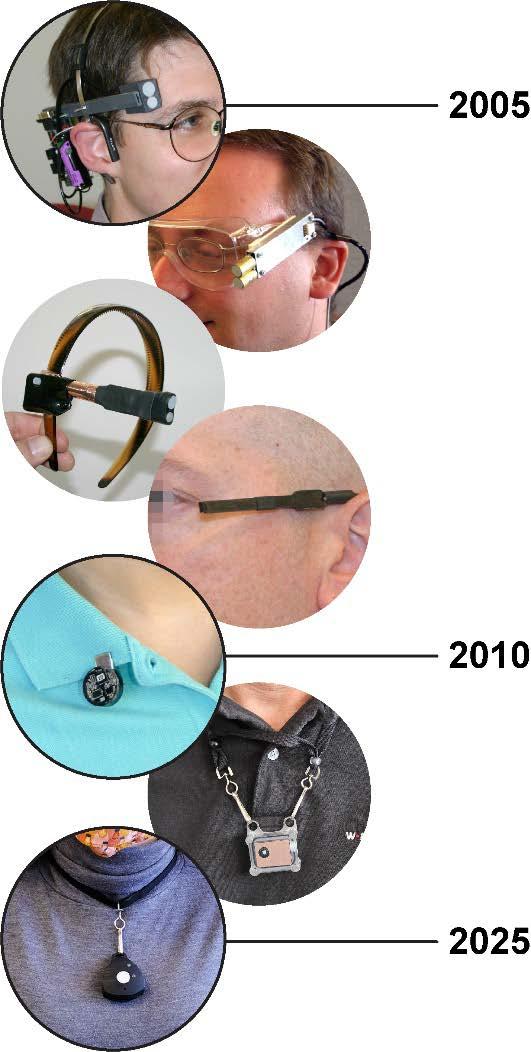
In the early 2000s, when the topic of light and health was still in its infancy, the LRC was the first research group to develop a personal light meter that was calibrated to measure circadian-effective light. However, the project’s funder, the U.S. Department of Energy (USDOE), was not willing to fund the development of technology related to health because it was outside their agency’s mandate.
The USDOE was, however, very interested in understanding the benefits of daylight, both for energy savings and for providing satisfaction to building occupants. Because daylight is a powerful regulator of the circadian system, we named our device the “Daysimeter” as a playful nod to the similarly named dosimeter developed by the USDOE at its Hanford Site in 1944. [1]
Our early field studies using the Daysimeter taught us that while measuring light at the plane of the cornea (rather than the wrist) was important, research subjects showed little willingness to comply with a device attached to their head.
Soon thereafter, we were awarded a multi-year, multimillion-dollar research grant from the National Institute on Aging to develop the Dimesimeter, a smaller version of the Daysimeter that would be more appropriate for collecting light data in people living with Alzheimer’s disease and related dementias (ADRD). Measuring roughly the size of a dime (hence the name), the Dimesimeter was a tremendous success, winning a place among the The Scientist magazine’s Top 10 Innovations in Science in 2011. [3]
Our research with the new device showed that the Dimesimeter worn as a pin or a pendant provided light measurements comparable to those obtained at the plane of the cornea, but with much greater subject compliance than the device’s predecessor.
Despite this considerable advantage, we realized the Dimesimeter was not sustainable because it could not be reused when its battery died. We therefore developed a version with a replaceable battery, named the Daysimeter-D, also funded by the National Institute on Aging.

The Daysimeter-D has been used to collect data in probably over 1000 individuals, including schoolchildren, office workers, cancer patients, ADRD patients, Parkinson’s disease patients, shift-working nurses, and even cows and lemurs (Figure 1)! This newer device allowed us to further the work with ADRD and lies at the core of the technology we have continued to develop and use to this day (Figure 2).
My long-time colleague Mark Rea once said that the Daysimeter was like a telescope: “You don’t know what’s out there until you start using one.” And he was correct, because we have indeed learned so many things over the years, some that we hypothesized and others we did not expect. Here are some of our key findings:
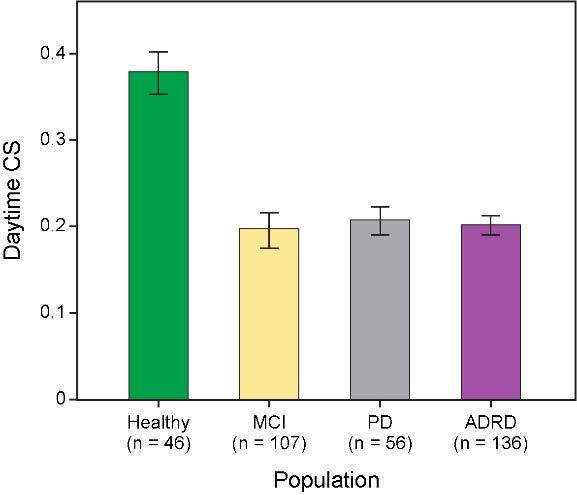
1. Healthy adults receive much more circadian-effective light (measured by our lab as circadian stimulus or CS) than people living with neurodegenerative diseases (Figure 3).
2. The mathematics of light and sleep is simple—the more CS one gets during the day, the better one sleeps at night (in the dark) (Figure 4).
3. Daytime light levels in offices, nursing homes, and hospitals generally fall below the threshold for activation of the circadian system.
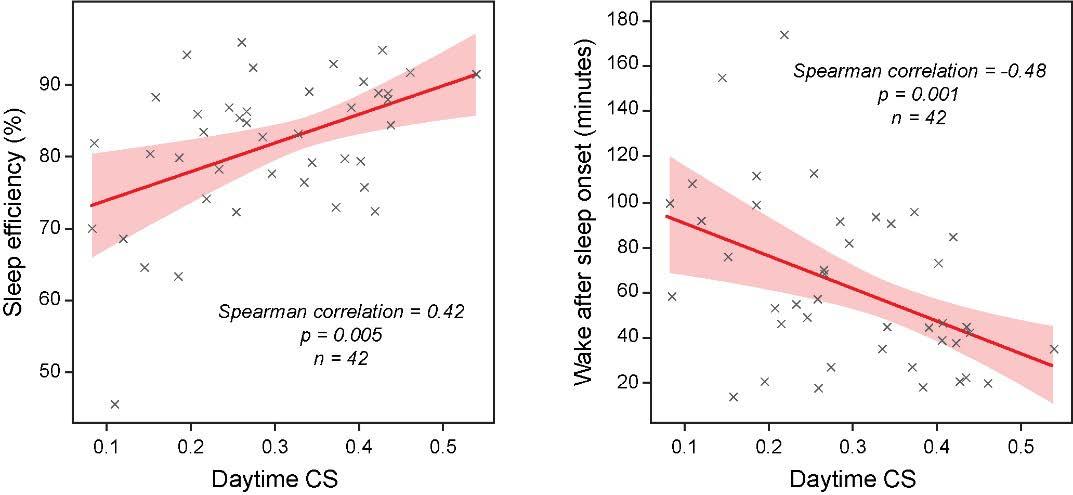
4. Exposure to a CS ≥ 0.3 during the daytime and ≤ 0.1 in the evening improved sleep, mood, and behavior in various populations. We have used that knowledge as the basis for lighting recommendations in the built environment.
5. The benefits of circadian-effective light are more pronounced in more controlled environments, such as nursing homes, hospital rooms, and submarines, which are typically poorly lit and do not promote circadian health and well-being.
6. Daylight that extends into the evening during the summer may delay the release of the sleep hormone melatonin, and consequently sleep onset, especially in children.
7. Nurses working nights do not always get sufficient light to lower their melatonin levels (the suppression of which has been linked to serious health risks). But that does not mean their circadian systems are not disrupted.
8. Outdoor electric lighting is often below the threshold for circadian activation and is certainly ineffective for stimulating the human circadian system in urban settings where window shades are used.
9. When US Navy submariners changed their watch schedules from an 18-hour cycle to a 24-hour cycle, the change in their light exposures led to better circadian alignment.
In 2018, the LHRC transferred this technology through a Small Business Innovation Research grant from the National Institute on Aging to Blue Iris Labs, whose founder and CEO Erik Page has been marketing newer and more advanced versions of the Daysimeter (called the Speck) to researchers around the world.
Although going by a different name, the Speck’s technology is still based on the LRC/LHRC calibration methods that made the Daysimeter such a unique research device. (To be clear, we do not have any commercial interest and do not receive any royalties from his business.) But far from simply reaching the research community, our ultimate goal is for everyone to use this technology as a tool in their everyday lives, allowing them to tailor their lighted environment (among various other integrated systems) for better health and well-being.
But potential obstacles to that goal are beginning to appear. Underlying all the knowledge we have gained, as well as the technology’s formidable potential, is the US federal government’s massive contribution to our own research and the broader field of lighting research.
Plaudits must be given to sponsors like the USDOE, National Institute on Aging, National Cancer Institute, National Institute of Neurological Disorders and Stroke, General Services Administration, Office of Naval Research, and National Institute of Occupational Safety and Health, among others. Without their generous support over the past 30 years, we would have been in the dark regarding the measurement of light in the built environment, left with unanswered questions about how light affects health and well-being.
But times have changed, and there is great and growing uncertainty surrounding the future of federal funding for biomedical research. Barring a change of the present course, it is our community’s ardent hope that others will step up to support the continued exploration of light’s impact on our lives. ■
References
1) Wilson R. H. Historical Review of Personnel Dosimetry Development and Its Use in Radiation Protection Programs·at Hanford, 1944 to the 1980s. Report # PNL-6125, UC-41. Richland, Washington: Pacific Northwest Laboratory, 1987. Available at https://www.osti.gov/servlets/purl/6696446
2) Rea M. S., Figueiro M. G., Jones G. E., Glander K. E. (2014). Daily activity and light exposure levels for five species of lemurs at the Duke Lemur Center. American Journal of Physical Anthropology, 153, 68-77. doi: 10.1002/ajpa.22409
3) The Scientist. Top Ten Innovations 2011. The Scientist, January 2012. Midland, Ontario, Canada: LabX Media Group, 2012. Available at https://www.the-scientist.com/ top-ten-innovations-2011-41527