

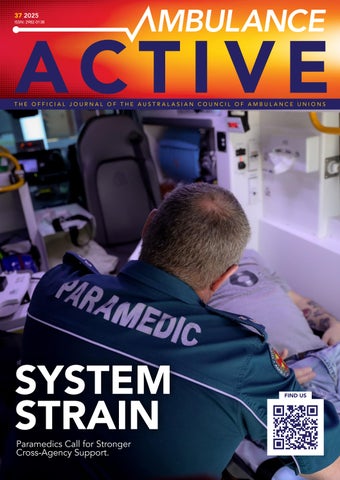


Paramedics Call for Stronger Cross-Agency Support.


















Australasian
PRESIDENT
Tess Oxley (HSU NSW)
VICE PRESIDENT
Faye McCann (First Union NZ)
Alistair Vagg (UWU Qld)
SECRETARY
Josh Karpowicz (AEA SA)
ASSISTANT SECRETARY
Simone Haigh (HACSU TAS)
June Congdon (UWU WA)
TREASURER
Olga Bartesek (VAU VIC)
ASSISTANT TREASURER
Darren Neville (TWU)
AMBULANCE
Craig Berger ( CWA ) 0426 954 744










Membership fees are tax deductible, and we support you with:
advocating for more career opportunities, workforce flexibility, recognition of capabilities, health and wellbeing
free high-quality, industry-informed CPD content
self-paced eLearning, webinars and podcasts
access to College education and research grants
research opportunities and mentoring programs
our FREE CPD tracker
Discounted rates to conferences and events
professional practice programs for continuous training and development
dedicated student study resources
10-12 September 2025 Hotel Grand Chancellor, Brisbane


THERE’S SOMETHING STIRRING IN THE union movement — a renewed fire, a louder voice, and most importantly, a growing one. For the first time in a generation, union membership is rising. And it’s not just legacy numbers or nostalgic returners — it’s young workers, stepping up, showing up, and demanding more.
In ambulance services across Australasia, we’re seeing what every employer fears and every delegate dreams of: workers realising that they are the union. This new wave of unionism is being driven by younger paramedics, call takers, transport officers and dispatchers who are sick of watching the wheels turn while conditions stall. They’re standing up not out of tradition, but out of necessity. And they’re not waiting for permission — they’re organising.
That’s not an accident. It’s the result of deliberate organising, led by our core

belief: members grow members. Across the Council, affiliates are building strength by building each other. We’re investing in delegate development, one-on-one conversations, and member-led campaigns that give people a real say — and a real stake — in the fights that shape their working lives.
We know the old model of servicing unions – waiting for a member to call with a problem and then solving it behind the scenes – doesn’t build power. What builds power is collective action. What inspires new members is seeing their colleagues win. What keeps them is the understanding that the union isn’t just for them — it is them.
That’s why the organising model works. It’s not just about recruitment. It’s about ownership. When a paramedic signs their mate up after a conversation about unsafe rosters, or when a call taker brings their team together to demand air conditioning
that actually works, they’re not just adding names to a list. They’re building strength. They’re building solidarity. They’re building a movement.
But growth without action is just numbers. Real power comes when members move together — in the workplace, in negotiations, and when necessary, on the street. We’ve seen this in every major campaign across our unions: whether it's fighting for professional pay, resisting unsafe roster models, or protecting injured workers. When members take action together, we win.
To the new delegates, the young workers, the future leaders reading this — your voice matters. Your energy matters. And your fight is our fight. Unions aren’t something we inherit; they’re something we build. So let’s build boldly. Let’s organise fiercely. And let’s remind every ambulance employer in the country that this movement is growing — and it’s not going anywhere.

IN MAY, DELEGATES FROM ACROSS Australia and New Zealand came together in Adelaide for the Australasian Council of Ambulance Unions’ (ACAU) 2025 Strategic Planning Day. It marked an important step in setting the strategic priorities facing Paramedics and ambulance professionals across Australasia.
Hosted by the Ambulance Employees Association of South Australia (AEA SA), the Planning Day focused on refining ACAU’s governance, setting our policy direction, and implementing modern communication solutions to enable more effective collaboration across member unions.
A key outcome was the unanimous decision to progress formal incorporation of ACAU—an essential move to strengthen our governance and national identity as we expand our influence across both Australian and New Zealand jurisdictions. It was clear throughout the discussions that ACAU continues to play a vital role in elevating Paramedic and ambulance issues in national forums—spaces from which our voices are too often absent. Paramedics are core members of Australia’s health workforce and must be recognised as such.

Delegates explored how ACAU can foster stronger networks and how to advance our core strategies.
As part of this advocacy, in April, ACAU representatives Tess Oxley (HSU NSW), Olga Bartasek (VAU), Paul Ekkelboom (AEA SA) and I attended the National Forum on Advanced Practice Paramedicine (APP) hosted by the Paramedicine Board of Australia in Sydney. The forum was a significant opportunity for Paramedics to advocate, contribute, and shape the national conversation on APPs. The agenda included presentations on rural health needs, international models, and potential challenges to APP implementation. Interactive roundtables and panels discussed how to align stakeholders, overcome resistance, and develop safe, progressive models of care. It was encouraging to see strong representation from Paramedics across Australia working constructively to advance the APP model. This balance was vitally important to with the many other varied voices of other health professionals, regulators, and jurisdictional ambulance services
A critical part of ACAU’s contribution was our formal submission to the Paramedicine Board. This, along with other stakeholder responses, will soon be published on the Board’s website in full
ACAU fully supports the introduction of a national endorsement for APPs that embeds independent prescribing and recognises advanced practice as a consultant‑level role. Global evidence demonstrates that APPs improve patient access, reduce emergency department presentations and deliver high levels of patient satisfaction. ACAU urges the Board to adopt a regulatory framework that is future‑facing, enabling APPs to practice autonomously across diverse settings, including private and self‑employed models, limited only by their education, training and experience.
From workforce planning and ambulance funding to mental health and occupational violence, ACAU remains best placed to advocate nationally for improved workplace conditions and the health and safety of our members. Together, we are building a united, credible, and industrial voice to shape the future of Paramedicine and ambulance.
My sincere thanks to all who attended the Strategic Planning Day, and to AEA SA for hosting. With our annual conference just around the corner—scheduled for September in Melbourne—we look forward to building on this momentum.
Ambos united will never be defeated.
Josh Karpowicz, a Registered Paramedic with 16 years’ experience, began his career with SA Ambulance Service in 2009. Now an Industrial Officer and Executive Member with AEA SA, Josh has also acted as Secretary, representing members in enterprise bargaining, employment tribunal matters, public campaigns, and policy negotiations. He combines his ongoing frontline paramedic work with strong union advocacy, advanced leadership training, and a drive to improving member conditions across the ambulance industry.










With cyber crimes such as identity theft, malicious attacks, data breaches and phishing still happening through the internet, we continue to do everything we can to keep your ESSSuper account(s) safe online.
We take your online security seriously – using layered protection, strong privacy controls, and constant system checks to stay ahead of threats.
Essential protection at the front door
Two-factor authentication adds an extra layer of security because it requires you to enter a unique, randomly-generated PIN in addition to your login
details. We’ll send the PIN to you in an SMS, so it’s important we have your mobile phone number on file.
Since 2022, we’ve required two-factor authentication either on certain transactions or when you log in to view your account using Members Online. Even if someone manages to guess or steal your password, they still can’t access your account without that one-time PIN which you get on your phone. It’s a simple, powerful way to make it much harder for cyber criminals to get in.
Strong passwords or phrases
Because longer, more complex passwords or phrases are much harder for criminals to crack, we’ve strengthened our password requirements to help protect you better. New passwords must now
have at least 14 characters (previously eight) and include a mix of upper case and lower-case letters, numbers, and special characters (like !, @, #, $).
You should avoid using common, easy-to-guess passwords such as “123456”, “password” and “qwerty123”.
Also, consider changing your Members Online password regularly to keep your account details confidential.
Don’t share your password
Your password is your personal key to your ESSSuper account. Sharing it – even with services you trust to help manage your finances – increases your risk of identity theft and fraud. Once you’ve shared your password, you can’t control how it’s stored, used, or protected.
Beware of fraudulent emails, phone calls and SMSs
ESSSuper will never send you an email or SMS asking you for your personal information or Members Online password. However, fraudsters may call you or send you a fake email or SMS that can be very convincing, in an attempt to steal your personal information.
Contact us
If you have any cyber security queries or concerns, or receive an email, phone call, or SMS you’re unsure about, contact us directly – never use the contact details provided in a suspicious email, phone call or SMS.
This information and more is available on our website at esssuper.com.au/security-privacy

Australia’s emergency service workers and volunteers keep our communities safe, but stress and anxiety are often part of the job. Experiencing mental health challenges after a traumatic event is normal and very common — and it’s treatable, too.
Confidential support is available now:
• Take a quick online mental health check and receive a report that identifies your symptoms and provides recommendations for support.
• Book up to 12 sessions with leading, trauma-informed clinicians via telehealth or face-to-face. Free of charge, with no Medicare or GP referral required.
• Access information and resources to help manage your symptoms.
Visit our website nationalemergencyworkersupport.org.au

AS OF WRITING, WE ARE NEARING completion of our process of Enterprise Agreement (EA) variation negotiations. This was an agreed process during our last round of EBA negotiations which were consumed by the finalisation, then implementation of the new 44hr roster and major reform of pay structures for our Communications staff (‘rolled- inrate” for Ambulance workers in ACT who are NOT registered health professionals). We decided to implement these too major reforms as a priority and delay other areas of negotiation so there was no delay to these 2 key reforms.
To do this we inserted a clause in the EA before sign off of an agreed timeline and process of variation to the EA. When such commenced we tabled some 38 points we were seeking either to be inserted or varied in the EA. These included, but were not limited to, pay banding, re-structuring of consultation processes, workforce planning reforms such as agreement on establishment figures, relief factors and unit utilisation rates, insertion and/or referral to spec’s on uniforms, vehicles and station amenities, reviews and agreement on Service Delivery model, WHS reforms which include implementation of Psychosocial hazards inline with new ACT Government policies and various other service wide issues.
Surprisingly we didn’t have a lot of pushback possibly due to most of these
items had little or no cost implications. However, when it came time to actually vary the EA officially via an application to the FWC, suddenly the work was too onerous for ACT Government negotiators to act. However all is not lost as our current EA expires in March 2026 and the ACT Government has proposed to reform the negotiation process so all ACT Government EA’s are negotiated and completed prior to expiry and can then be ready to be signed of and implemented immediately after. Whilst this is quite optimistic optimistic, it gives us a continuity and momentum to continue urther chance to create significant reform and change in our industrial agrrement. We also have like-mindedness from our current team of managers and have permission and agreement to continue commencing some of variations we have proposed prior to them being underwritten in the EA.
On other matters we continue to raise concerns about safety for staff attending dangerous scenes, especially those with forecast risk of Occupational Violence (OV) Several PIN’s remain in place, mainly due to the lack of support provided from the ACT Government in negotiating with the AFP (police) to provide assistance as required. We have also commenced a review of the new 44 roster which has now been in place since April 2024. Whilst it is still proving extremely popular with the
majority of Paramedic members (most who work via such), ongoing lack of ability to recruit experienced staff and all-round staff shortages continue to hamper the full benefits of the new roster being realised. And finally, we have had a changing of the guard with the farewell of our Chief Officer Howard Wren in February 2024. He amassed some 50 years in the ambulance and health industries, a large chunk of that in ACTAS. He trained many of us who started their career in ACTAS prior to the evolution of paramedic degree qualifications becoming the pathway to the commencement of practice in pre-hospital care. And, just recently we have had the commencement of a new Chief Officer, David Dutton who trained as a Paramedic in the ACT mid 90’s (under Howard Wren!) David left ACTAS from a senior management position in early 2013 and worked in NSW for the last 12 years and has now returned as the “prodigal son.” So far, we (the union) have commenced building a very collaborative relationship with him and we remain optimistic of jointly creating important future strategic reform planning for the ACT Ambulance Service. We’ll keep you posted if that continues and builds outcomes. In the meantime we look forward to sharing information and working together to improve our industry as a whole at the annual ACAU Conference in Melbourne in September 2025, see you there!

One of the biggest battles we’re fighting is against the push for single officer responses. Yes, NSW Ambulance is seriously suggesting that it’s safe — and somehow acceptable — to send paramedics alone to emergencies. As workers who deal with life-and-death situations, often in violent or chaotic environments, going solo is dangerous. Both for the paramedic, and the patient they need to treat.
Union members continue to press the case that no emergency worker should be expected to do this job alone.
Violence at work isn’t a risk for us — it’s a reality. Assaults, abuse, threats. And its important to note, its not just aggressive perpetrators. Dementia patients, delirious unwell patients, Traumatic head injuries. There are many factors that lead to occupational violence toward paramedics. NSW Ambulance likes to talk about “zero tolerance,” but what we see is zero follow-through.
In one of the most baffling moves we’ve seen, management floated the idea of holographic partners to accompany solo paramedics. That’s not a joke. They seriously proposed projecting a 3D image of a partner into an ambulance to make us feel supported and maybe deter violent patients. With the assistance of an AI voice in an earpiece and a drone above. A lot of effort and money for things
that are gyuaranteed to fail, instead of agreeing to maintenance of double crewed paramedic rosters!
This is what happens when decisionmakers are completely detached from the work we do. It’s insulting. It’s absurd. And it proves how little value they place on our safety and presence.
NSW Ambulance is touting its On Duty Relief (ODR) model as a success, pointing to metrics like reduced single staff movements and improved crib breaks (They are actually proud of only 20% of staff achieving crib breaks!). But members on the ground have told a different story.
NSW Ambulance claims a reduction in single staff movements and improved response times, but the cost has been shifted to workers. A recent survey of members showed that over 90% do not support this model. Contacting staff out of hours, expecting them to travel to different stations across the metro area in their own time at their own cost, with no additional support or fatigue management.
It’s not ‘relief’ if it leaves staff more fatigued, less in control of their shifts, and having to foot the bill. Relief that isn’t resourced fairly is just exploitation with a glossy name. We need a model that actually supports crews — not one that relies on unpaid labour and hollow statistics to paint a success story that most of us on the ground don’t recognise.
This is what consultation without consent looks like. A top-down model built to serve overtime budgets, not people.
The newest proposed Flexible Work Agreement policy is being dressed up as progress — but in practice, it’s a tool for control. The policy makes it harder for staff, particularly women with caregiving responsibilities, to access or maintain parttime work. It allows managers to reject or review flexible arrangements with little justification, creating instability and pressure.
We’ve seen members pushed out of jobs they love because their part-time hours became “too difficult” to manage. This is a gendered issue. It’s an equity issue. And it’s something every union should be watching closely.
Above all, the clear message from workers is this: NSW Ambulance doesn’t understand us, and worse, doesn’t seem to want to. They’re increasingly removed from the reality of what happens on the road. They make policies in boardrooms that don’t survive five minutes on a job in Western Sydney or the Riverina.
They’ll consult with consultants, but ignore the people wearing the uniform. They’ll talk about “innovation,” but leave real problems unsolved for years. They’ll praise resilience, while creating the very conditions that break us down.
We know our fight isn’t unique. Across the public sector and beyond, frontline workers are being told to do more with less, to bend to systems that ignore our voices, and to stay silent while our safety and conditions erode.
But paramedics don’t stay silent. We organise. We act. And we back each other. breaks on time and we are looking at adjusting this policy to include more crews and hope to see a further increase.
St John agreed to conduct an independent remuneration review as part of the last collective agreement terms of settlement. This review was to include engagement with the unions and their members and the final report was to be made available to the unions. The report is now “complete” with no opportunity for the unions to provide any input or openly review the report. We also note the report did not include any comparison to Queensland Ambulance Service or take in to consideration the total remuneration package of any other service, only base rate pay. This report, which is a very poor reflection on the actual terms and conditions our members have, has now been passed on to the government and will be taken in to consideration for future funding of the service, disadvantaging ambulance officers potential to be appropriately remunerated.
Auckland has been struggling with recruitment and retention for some time now being a higher workload area with a higher cost of living. During Covid St John received funding for an internally run emergency medical technician course so help with nationwide staffing issues. Although that funding stream has now stopped, St John is funding an additional course to train 52 Emergency Medical Technicians specifically for Auckland to help with the current vacancies.
We are seeing an increase in meal breaks being completed within the agreed meal break window with recent data showing this was achieved 66% of the time, up from 60% in the previous quarter. Busier metropolitan areas have an enforced break to assist with getting breaks on time and we are looking at adjusting this policy to include more crews and hope to see a further increase.

On July 16 and 17, 2025, United Workers Union Delegates gathered in Darwin for a two-day meeting to finalise the log of claims for the upcoming enterprise agreement negotiations. The process was shaped by extensive member input, collected through a survey calling for suggestions by July 14.
Delegates representing regions across the Northern Territory—including Katherine, Nhulunbuy, Tennant Creek, and Alice Springs—worked collaboratively to review and incorporate member feedback into the draft. Those unable to attend in person, such as Susan Murray, participated remotely via Teams.
Union representatives expressed their gratitude to members for providing a wealth of suggestions and reaffirmed their commitment to delivering meaningful improvements in the next EBA.


United Workers Union Bargaining Representatives have met with QAS on a number of occasions since mid May 2025. Members claims have all now been tabled and more detailed discussion around key claims related to Finish on Time / End of Shift initiatives. It is clear after the recent State Budget funding announcements that QAS do not have future staffing numbers funded to enable agreement on many of the initiatives.
Make no mistake, your bargaining representatives are very clear that no agreement will be able to be reached on behalf of members unless there is meaningful, enforceable, measures included to address finish on time.
On 12 June 2025, your UWU Bargaining Team wrote to Minister Nicholls to outline:
TAKING OUR MESSAGE PUBLIC UWU issued a media release
“It is clear after the recent State Budget funding announcements that QAS do not have future staffing numbers funded to enable agreement on many of the initiatives.”
• The status of UWU-QAS bargaining,
• The growing need for government investment in additional ambulance resources,
• And a request for a direct meeting to discuss the future of the service and UWU ambitions in this round of enterprise bargaining.
On 24 June, the Queensland Government handed down its 2025–26 State Budget.
ALARM BELLS WERE RINGING across Emergency Departments on Tuesday as the Queensland government handed down a Budget with a gaping hole where funding for ambulance staff and vehicles should be, leaving the critical services that Queenslanders rely on at risk.
With Queensland’s growing population, ambulance services need to keep up or risk putting millions of Queenslanders in danger.
Modelling shows that demand for ambulances in Queensland will grow at least 6% a year. But this Budget’s planned 225 staff per year will only cover a 4% annual increase in demand – meaning an annual 2% net loss of ambulance services.
Ambulance workers are currently bargaining for their terms and conditions for the next three years. Before this budget was handed
down, UWU members reached out to Minister Nicholls about what was needed to reach agreement.
This Minister has provided no reply to this correspondence.
Quotes attributable to Fiona Scalon, Ambulance Coordinator, United Workers Union:
“Queensland is a growing state, and the Government must invest to support that growth, otherwise we’ll fall behind and Queenslanders’ health will suffer.
“Funding for 900 new ambulance staff over 4 years is less than half what the previous ALP Government committed to, and far less staffing than previous budgets.
“For ambulance workers who are already under pressure, that extra annual demand means already lengthy shifts being extended, leave being difficult to get approved, and no respite from a relentless and demanding role.
Disappointingly, this year’s budget included fewer staffing increases than previous years, despite the clear and growing need across the service.
This raises major concerns for both service delivery and the staff welfare claims our members are fighting for in EBA negotiations — especially the critical issue of ending unsafe, excessive shift extensions.
“For Queenslanders, this could mean delays in response time that could have dire patient outcomes.
“Even the funding earmarked for vehicles is laughable. With a fleet of 1600 rapidly aging vehicles, 170 new or replacement vehicles aren’t nearly enough. This budget won’t keep ambulances on the road, and won’t fund enough staff to do the job.
“The Minister’s complete lack of response says it all.
“This Budget is a slap in the face of hard-working and dedicated QLD Ambulance workers who save lives every day, and the Queenslanders who rely on them.”
Quote from Queensland Ambulance worker:
“This Budget will see paramedics continue to be subjected to psychosocially unsafe conditions and will continue to contribute to rising levels of sick leave and burnout. Our paramedics, and our communities, deserve better.”
Highlighting the real risks of underfunding the ambulance service and the toll it's taking on frontline workers. Within hours, Minister Nicholls' office contacted UWU to arrange the meeting we had been requesting — a direct result of our collective voice being heard.
Your UWU Bargaining Team met with Minister Nicholls and advisors on 16th July and are optimistic that these discussions have provided an opportunity for serious consideration by government about what’s at stake this agreement.
Without more FTE, shift extensions will remain the norm — putting your health, your families, and patient safety at risk.
More updates to come as we continue bargaining and push for the investment and respect our members deserve. Stay connected, stay united
In encouraging news, the End of Shift Out of Service process is producing some positive outcomes for United Workers Union members getting to finish closer-to-on-time in Metro South and the Gold Coast where the model has been resourced.
Just over the Easter long weekend, it is reported that between 45 and 65 crews were put OOS in the last 30 mins of their shift in order to make their way back to station to finish on time. On Monday alone, 23 crews were tagged OOS. These are promising figures being seen during these trials. This puts members claims around finish on time in the next EBA in a strong position to fight for.
These EOS models are in their trial phases primarily due to the advocacy of UWU Delegates who have been involved in the Staff Welfare discussions with QAS Executive. UWU Delegates designed a business case and operating model and articulated the benefits to both the Organisation and members convincingly, first on the Gold Coast and then into Metro South. If you get home on time today, thank your UWU Delegate!
After last month’s Member update many members across the state have notified United Workers Union of ongoing increment progression delays and general payroll discrepancies and been allocated through to organisers and Member Rights Team officers to assist to get their matters resolved.
Off the back of UWU Delegate advocacy at RCC and SCC forums, along with engagement with QAS State Executive
around this ongoing and systemic issue, we have seen audits on increment progressions taking place across Regions with hundreds of impacted members having their pay rates adjusted and back pay calculated.
Your State Council met over two days to deep dive into every item in our EBA Log of Claims. Councillors also delivered regional reports to share local wins, raise shared challenges, and plan the next phase of our campaign together.
State Councillors have been setting up regional communication platforms to keep members connected and informed.
Want to stay in the loop? Contact your local State Councillor to get connected — this will be essential as we move deeper into negotiations.
To make sure you're getting updates as the campaign heats up, take a moment to check your contact details: https://forms. office.com/r/SHYbQEjSjy
All members are reminded of their obligation to protect patient and case information in line with their responsibilities as employees of the Queensland Ambulance Service (QAS). This includes how and when you access iROAM
When logging into iROAM, users are presented with the following:
iROAM is a Queensland Ambulance Service (QAS) system and must only be accessed by authorised QAS users. By accessing iROAM, the user agrees to be subject to all relevant QAS policy and procedure, including any information security policy and procedure applicable to QAS personnel. All access and usage of
iROAM may monitored, examined, intercepted, copied, recorded, audited and disclosed to law enforcement personnel for any lawful purpose.
Users must not use or disclose information accessed through iROAM unless authorised to do so.
iROAM contains 'confidential information' as defined by the Ambulance Service Act 1991 (the Act). Unlawful disclosure of that confidential information is an offence under the Act and offenders may be prosecuted.
Unlawful or improper use of iROAM may result in administrative disciplinary action and/or criminal penalty.
By continuing to use iROAM, you acknowledge and agree to comply with the above and any other terms and conditions of use. Do not continue to use iROAM if you are not authorised to access the system or if you do not agree to comply with the above or any other terms and conditions of use.
Recent investigation processes have revealed that iROAM access is routinely audited in disciplinary matters. This includes an examination of:
• Every instance of access,
• What specific information was accessed,
• And whether there is a clear work‑related justification for each instance. (often requiring explanations going back years, numbering in the hundreds), If a member cannot demonstrate a legitimate, work-related reason for accessing a case file, this can and has led to significant disciplinary consequences, including termination.
Members with supervisory or management responsibilities are particularly at risk. As part of your duties, ensure you only access case information directly related to your current role and responsibilities. Never access files “out of interest” or for convenience — the system tracks and timestamps every action.
• Always ask yourself: “Is there a clear operational reason I’m accessing this file right now?”
• If the answer is no — don’t click through.
• If in doubt, seek advice from your UWU delegate or your supervisor.
Your union is here to support you — but proactive caution is your best protection.

The AEA SA continues to raise serious concerns about an escalating safety risk for our members: the expectation that paramedics and ambulance officers attend welfare checks either in lieu of, or without the presence of, police. This follows South Australia Police’s (SAPOL) rollout of its new “THRIVE” model, which has seen a withdrawal from duties that have traditionally been police-led.
Under this model, SAAS crews are increasingly dispatched alone to welfare checks—often with unclear risk levels. These incidents can involve mental health crises, aggressive individuals, drug or alcohol-affected persons, or hazardous environments. Paramedics are not trained, resourced, or empowered to safely manage these situations without police support.
The AEA SA has not agreed to any operational change that places the responsibility for these high-risk responses onto ambulance personnel. We have formally escalated the issue to the Minister for Health and Wellbeing and are preparing direct correspondence to the Commissioner of Police.
For union colleagues across jurisdictions, this sets a dangerous precedent. It highlights how the shifting of operational responsibilities between agencies—without consultation, adequate training, or formal risk assessment—can erode workforce safety. Alarmingly, this is not isolated to South Australia: recent media reports across Australasia have documented assaults on paramedics following welfare check responses.
We urge ambulance unions nationally to monitor for similar encroachments, and to hold the line in preserving inter-agency boundaries that protect the safety of frontline workers.
The AEA SA is actively encouraging members to report all incidents and concerns—whether through our internal Issue Report tool or through SAAS channels such as SLS, WHSIR, or IRQA. Member safety is not negotiable. These changes must be reversed so that paramedics and ambulance officers can focus on their core clinical role— and police can fulfil theirs.
One of the most important industrial protections secured by AEA SA has been the strengthening of end-of-shift relief provisions to reduce unreasonable postshift overtime.
Key entitlements include:
• Crews must not be tasked during the last hour of their rostered shift, except for Priority 1 emergencies (e.g. cardiac arrest).
• Once a shift ends, no further taskings may occur unless explicitly agreed to by the crew.
• If ramped at hospital at the end of shift, the crew must be relieved— even if Priority 2 incidents are active in the community.
These protections were secured by raising safety concerns under the Work Health and Safety Act 2012 (SA) via Right of Entry powers, and ultimately through intervention by SafeWork SA.
While these gains have created essential protections, many members still report routine post-shift overtime due to persistent ramping and excessive demand. The AEA is now advocating to expand relief processes so that replacement crews are dispatched before shift end—eliminating the “builtin” overtime currently required just to access relief.
We continue to monitor compliance and encourage members to document breaches, notify the AEA, and stand firm on these entitlements.
GROWING OUR SAFETY NETWORK: HEALTH AND SAFETY REPRESENTATIVES (HSRS)
In response to mounting health and safety issues, AEA SA is prioritising the development of a more active, well-supported network of Health and Safety Representatives (HSRs).
Our strategy includes:
• Identifying WHS gaps and high-risk locations
• Rebuilding underrepresented work groups
• Providing direct support and mentoring to active HSRs
With increased psychosocial risks and new SafeWork Australia Codes of Practice now in effect, this work is more important than ever. We are equipping HSRs to play a stronger role in enforcing member safety rights and creating workplace accountability.
After years of advocacy, AEA SA has secured a significant win: the reintroduction of dedicated transit wards at both the Royal Adelaide Hospital (RAH) and The Queen Elizabeth Hospital (TQEH), under the Central Adelaide Local Health Network (CALHN).
Transit wards provide short-stay spaces to facilitate structured patient flow— both incoming and outgoing—and were notably excluded when the RAH was redeveloped in 2017. Their absence contributed significantly to ramping and internal delays.
These new wards allow for the;
• Improve predictability of patient movement
• Reduce offload delays for paramedic crews
• Ease bottlenecks that delay ED throughput
Importantly, these wards are integrated with on-site pharmacy services, enabling medication management and earlier discharge clearance—freeing up inpatient capacity sooner.
This outcome is the result of targeted union consultation, sustained pressure, and evidence-based advocacy. It represents a practical model that could benefit hospital networks across the country facing similar congestion and flow issues.
The AEA SA remains alarmed at the steadily increasing ramping figures, despite State Government investments in hospital capacity and ambulance resourcing. This clearly demonstrates that the root causes of hospital ramping go far deeper than resourcing alone.
Concerningly, recent public data from SA Health indicates that ambulance response times are once again declining. This is a direct consequence of sustained and worsening ramping. The issue is no longer being offset by additional ambulance crews, as the final tranche of new crews from the 2022 election commitments commenced in July. With ramping hours exceeding 5,000 in June—and early reports from members indicating even worse conditions in July— we are gravely concerned that a new and unwanted record will be set this winter.
In response, the AEA SA has renewed its calls for:
• Expansion of rapid offload and transit beds to relieve pressure on emergency departments
• Extended operating hours for Virtual Care Services (VCS), including evenings and weekends
• Improved inter-LHN coordination and communication to divert low-acuity patients from emergency departments
• Investment in system-wide reforms that address unnecessary presentations, not just ambulance flow
• Additional crewing to meet seasonal winter demand
The AEA SA is actively pursuing these initiatives however we remain concerned that few levers remain to be pulled ahead of the peak winter period. Sustainable, long-term improvements to system flow and resourcing are needed to ensure the ambulance service can meet growing demand—and is not left, unable to respond from hospital ramps.
Total Hours Lost
Following a comprehensive consultation and development process with regard to the log of claims, negotiations have now commenced for the next Ambulance enterprise bargaining round. We have now met twice with Ambulance Tasmania and Central Government negotiators.
Our claim is comprehensive and deals with matters relating to rosters, salaries, classifications, safety and a raft of other pressing industrial matters.
However, if you’ve been watching the news Tasmanians are now back to the polling booth again (just over 12 months since the last State Election)
Sadly, as a result of the “Caretaker conventions” now in place the negotiators are unable to commit any incoming government to an outcome. However, the news is not all bad in that agreement has been reached to continue discussions and work on matters where there may be common interests until the election has been concluded and a new Government is formed.
We are deeply concerned that the election will impact on our ability to achieve an outcome prior to the 1 December deadline (when the next wage increase is due for members). We made it clear that that date is nonnegotiable and that backpay would have to be paid if the Government (whichever colour they are) fail to meet that deadline!
We have a clear objective to achieve a positive result for our members that will ensure we are paid decent wages, can work in a safe environment and that Ambulance Tasmania is equipped to provide the best possible service to the Tasmanian community.
Watch this space!!
Most members have now received their back pay arising from the Classification Structure increases; however, a number of members remain unpaid as we enter the seventh month since the Enterprise Agreement (EA) came into effect.
The VAU is currently in dispute with TZV regarding the calculation of back pay under the new Classification Structure. TZV has failed to recognise months of service already accrued within an acquired
In our last report we referred to a review of the Transfer of Care Procedure implemented across all Tasmanian Hospitals in April 2024. We were awaiting the release of the review findings and being provided with a copy of the final report.
In May the report was finally released.
The review highlighted that whilst there are still problems with the ongoing implementation of the procedure it had successfully achieved a significant reduction in ramping and that there were further changes that can be made to make the protocol even more effective.
Of significant importance highlighted in the report (amongst other things) was the need for the hospitals to develop “appropriate action plans ….. that outline escalation pathways and key responsibilities of Nurse Unit Managers, the Integrated Operations Centre and the (Hospital) Executive Director of Operations to address TOC delays.”
In simple terms what is suggested is that each of the four main hospitals develop their own “local workplace instructions or action plans” that reflect local responses and workflows that align with the Ambulance Policy. This recommendation is strongly supported by HACSU.
The review recommends that key stakeholders (including HACSU) be engaged in the implementation of the recommendations.
If you are keen to read the report and all of the recommendations, you can access the report here: https://www.health. tas.gov.au/sites/default/files/2025-05/ download_the_transfer_of_care_ procedure_review_pdf.pdf
Ambulance Tasmania has agreed to settle a dispute regarding salary and classification matters relating to the above groups. A formal offer was ultimately put to us by Departmental representatives which was ultimately accepted by members.
The agreement includes an interim, More Responsible Duties payment for all staff whilst the substantive classification is resolved and a substantial back pay offer. At the time of writing members were still waiting for the backpay to arrive in their bank accounts.
Over a decade of inaction in addressing the need for additional staff to support the ever-increasing numbers of operational paramedics has in northern Tasmania has led to industrial action to address the enormous workload being placed on Operational Supervisor members. By way of background, they had attempted on several occasions over recent years to have Ambulance Tasmania senior management address their concerns but discussions never went anywhere.
Only a few weeks ago, the OS group stood together and in a united way decided to take the matter into their own hands. Their industrial action, essentially removes a significant number of low level (but onerous) duties to create the capacity for them to do their actual job, that is supervise and support their staff.
At the time of writing, Ambulance Tasmania Management has put in place contingencies to ensure that the banned work is done but we are waiting for a more concrete offer of additional resources. Discussions on these matters will occur over coming weeks.
classification, instead resetting employees to the start of the classification year and applying the EA implementation date as the commencement of service. This has effectively erased prior service credit.
Alongside other unions at TZV, we have pursued the internal dispute resolution process and are now preparing to lodge an F10 application to escalate the matter to the Fair Work Commission (FWC).
There are several ongoing issues with the implementation of the EA, and the
VAU continues to meet regularly with TZV in an effort to resolve them. Despite this, we remain in dispute over multiple clauses within the Agreement.
Separately, the VAU and CWU have received the decision from the Federal Court regarding the matter of Workplace Trainers not receiving the Mentoring Allowance. Unfortunately, the Court found against us. After careful consideration, the parties have agreed not to appeal the decision.
The VAU continues to engage in enterprise bargaining with Health Select in pursuit of a new Enterprise Agreement. To date, there has been no agreement on several key claims, including recognition of Years of Service, the introduction of a Student Observer Allowance, provision of Paid Meal Breaks, and the application of indexation to wages and allowances.
While there has been some progress on minor claims, Health Select’s overall position on wages and allowances remains unsatisfactory. Prior to the 1 July Fair Work Commission minimum wage increase announcement, Health Select put forward two inadequate wage offers of 2% per year, the 2.5%. Following the FWC announcement, their revised offer stands at 3.5% in the first year, 3% in the second, and 2.75% in the final year—none of which are indexed.
Given Health Select’s failure to address any of the major monetary claims, members are unlikely to accept a wage offer that lacks indexation and falls short of reflecting the rising cost of living.

Since July 2024, the VAU and ANMF have continued enterprise bargaining with RFDS for a new Enterprise Agreement. The parties have made significant progress, reaching agreement on the majority of claims, and the drafting process is now nearing completion.
UWU DELEGATES ACROSS WA HAVE been ensuring SJA members entitlements are upheld and improved via multiple consultation processes and issue by issue enforcement.
The end of 2024 and the first half of 2025 has revolved around winning outcomes in the Paramedic EBA.
This has been a long and hard fought bargaining campaign. UWU members should be proud of being the first to lodge and vote to take action, thereby leading the charge for better pay and conditions for all St John paramedics.
The significant elements of the offer are:
• Pay increase of 7%, 5% and 5% with no limit on back pay, reached by making savings through:
A Reducing ambulance cleaning time from 30 minutes to 15 minutes;
B Reverting to a flat rate for night shift payments for all classifications equivalent to the current rate for AP3 classification (plus annual indexation);
C Reverting to the existing flat rate structure for the on-road tutor allowance and the working with volunteer allowance (plus annual indexation); and
D Reducing the allowances for a CPHC Trainer and CPHC Training Coordinator from 8% and 10% of rolled-in rate to 5% and 7% respectively.
• Increase in minimum breaks on the 224 roster to 11 hours between days and 10 hours between nights. The minimum break will be 10.5 hours for the day van roster.
• Implementation of block out periods at the end of shifts (P0 and P1 only in last 15 minutes and no transfers greater than 35km in last 90 minutes of shift, unless P1).
• Escalating penalties for consecutive missed or broken meal breaks over a set.
• Greater flexibility in taking long service leave entitlements.
• Strengthened consultation clauses to improve our ability to engage with SJA prior to organisational change.
Agreement has recently been reached on the final outstanding matters related to meal break amenities, dispute resolution, and the Occupational Health and Safety clause. The only remaining item to be resolved is the Part-Time Employment clause, which is currently under discussion.
Between record ramping leading into the winter surge and WA hospitals continuing to struggle this has inevitable consequences for the delivery of ambulance services.
In a shock announcement SJA chose this time to Axe up to 90 operatives across the organisation.
See statement from UWU regarding this cut in investment in ambulance services.
“The people of Western Australia deserve an ambulance service with motivated, committed workers who have job certainty and security.
We understand the potential job losses aren’t directed paramedics and frontline staff, but cuts to support services have flow-on effects and will impact not only our paramedic members, but the people of Western Australia who rely on St John’s during emergencies.
Support workers are an important part of a functioning, fit-for-purpose ambulance service that can meet the needs of the Western Australian community.
Investing in all workers should be a key priority for St John, one of the largest ambulance services in Australia.”

Paramedics Call for Stronger Cross-Agency Support.
Kieran Hitchenson found himself defending against a violent patient outside a Canberra police station. After pressing his duress alarm and receiving no assistance, he made the decision to drive to the nearest station himself. Still, no one came - until officers noticed the altercation on CCTV and rushed outside.
The event, first reported by The Canberra Times, is just one of many that Hitchenson and other ACT Ambulance Service delegates say illustrates a growing crisis on the frontline.
“We’re often left without support when we need it most,” Hitchenson said. “We’re told to ‘just run away’ or find our own way out. Once I had to climb out a window because a patient became aggressive and there was no other exit.”
The delegates - representing members of the Transport Workers Uniondescribe a system where support from police is inconsistent, communication is poor, and workloads are unsustainable. They claim there’s a worrying disconnect between emergency service leadership and frontline realities.
“There are times when we’re left waiting with multiple crews held off scene,” Hitchenson said. “And if something goes wrong while we’re standing by, who carries the risk? Us.”
Industrial relations liaison officer Simon Gallagher noted that all emergency services are stretched thin. That shortfall, he said, often leaves paramedics exposed when incidents escalate and police support is unavailable.
Communication centre clinician Darren Neville echoed the concern, stating: “It’s not about blaming police, but there’s a lack of two-way communication. We feed them information, but rarely get anything back.”
He added that a traditionally strong working relationship between services is beginning to erode. “Frontline crews are starting to question who’s in charge of a scene, and why we’re there without backup.”
Paramedics say they’re increasingly unable to make patient-focused decisions due to external delays and a lack of realtime support. “We’re all here to help the community,” Hitchenson said. “But that means we need to support each other, too.”
Union delegates also raised alarm about reports that police are looking to reduce involvement in mental health-related incidents. While paramedics agree that

policing isn’t always appropriate for these calls, they stress the importance of backup when needed.
Bryan Woodford, a PACER paramedic educator, noted: “Many people in crisis don’t need a law enforcement responsebut until we assess the situation, we don’t know if it’s a mental health issue, substance use, or a medical emergency. Either way, we can’t do our job if it’s unsafe.”
Neville also pointed to concerns about a broader national shift. “We’ve heard suggestions from the Australian Federal Police Association (AFPA) that police are moving away from mental health jobs,” he said. “But if that’s the direction, where are the resources to fill the gap?”
In response to these concerns, an ACT Policing spokesperson told The Canberra Times that police prioritise responses based on risk and urgency. “The safety of individuals and the protection of life remain our top priorities.”
They rejected claims of withdrawing from joint models like PACER and highlighted that an independent 2023 review found it to be effective in reducing the use of restrictive practices.
The spokesperson added: “Where incidents involve health or mental health issues, our aim is always to provide support that’s least restrictive, least intrusive, and centred on care - not criminalisation.”
AFPA spokesman Troy Roberts also pushed back on the idea of a national
agenda to withdraw from mental health calls, calling it “an overstatement.” However, he acknowledged that ongoing resourcing challenges raise valid questions about the best role for police in nonviolent, health-centric situations.
Union officials also flagged a steep rise in Triple Zero calls, stretching paramedic capacity further. Ben Sweaney from the Transport Workers Union said there had been a 15% increase in demand over the past year - well beyond the usual 8-10% annual rise.
“We’re being called to non-urgent situations far too often. One case involved a blood nose after a basketball game. That’s not a life-threatening emergency,” Sweaney said.
Gallagher added that ACTAS is severely under-resourced: “On any given night, we’ve only got about 17 paramedics covering the entire Canberra region. That’s not enough.”
This article was adapted from an exclusive report by The Canberra Times and shaped by the voices of paramedics and union delegates who are standing up for a safer, more supported frontline.









Union says Ambulance NSW service has lost sight of its priorities when it comes to paramedic staffing.
UNION SLAMS “CRISIS LEVEL”
Staffing at Goulburn Ambulance Station
The Health Services Union is calling on the NSW Government to urgently boost paramedic staffing at Goulburn’s under-resourced ambulance station, warning that ongoing shortages are putting lives at risk.
As part of the campaign, ambulances marked with the slogan “Labor Government Abandons Goulburn” have been seen across the city, highlighting frustration among local paramedics and residents alike.
Local HSU delegate and intensive care paramedic Paul Taylor said the Goulburn station is operating with just 24 paramedics -12 short of what’s needed to safely meet demand.
“Goulburn’s staffing is dangerously low. That means crews from Bowral, Yass, Crookwell, and Queanbeyan are constantly being pulled in to cover,” Mr Taylor said. “But those towns need their own paramedics too. It’s robbing Peter to pay Paul.”
While NSW Ambulance has defended the approach, calling it part of a “mobile workforce,” Taylor says this misses the point. “They know the workload for each town. Rostering should reflect that, not shuffle people around and hope for the best.”
HSU Secretary Gerard Hayes added that the rostering practices were not only inefficient but insulting. “If a crew is funded for a town, that’s where they should stay. Rural areas already face a lack of healthcare access -taking away paramedics to support bigger towns is a direct risk to patient safety.”
The issue came to a head last year when a dementia patient at a Goulburn aged care facility waited five hours for an ambulancedispatched from Queanbeyan.
The union argues that understaffing is exacerbated by NSW Ambulance’s failure to replace paramedics who are unavailable for shifts. “These aren’t optional extras,” Hayes said. “They’re vital frontline workers. You don’t just skip a shift because someone calls in sick.”
In 2023, Goulburn gained five new paramedics - its first increase in 30 yearspart of a statewide commitment to recruit 500 new regional paramedics. Still, Taylor says it’s not enough to match the area’s growing demand.
NSW Ambulance Commissioner Dr Dominic Morgan told a February expenditure hearing that Goulburn operates as a “hub,” supported by nearby stations.
But Taylor says that’s misleading. “Crookwell is close - but everything else is an hour away. When it comes to heart attacks or trauma, that’s the difference between life and death.”
An Ambulance NSW spokesperson said emergency calls would be responded to and that consultation with staff and unions continues. They would not confirm whether Goulburn would receive more paramedics.
Mr Taylor is also pressing for greater transparency around staffing numbers.

“If it’s just data and modelling, then why does Lithgow -servicing 60% of Goulburn’s workload - have 36 paramedics compared to our 24? Why does Bowral get 36 with fewer call-outs?”
Together with co delegate Jock Cartwright, Taylor pushed for roster reform to match peak demand periods -proposing an additional afternoon shift to address the surge in afternoon emergencies. Instead, NSW Ambulance introduced a two-day, two-night rotating roster from March 22.
“That’s basically what we had 30 years ago,” Taylor said. “It’s not reflective of today’s call volumes or community needs.”
Dr Morgan defended the decision, stating that the alternative would have left Goulburn without 24/7 coverage. NSW Ambulance also cited the need to reduce fatigue and eliminate overnight on-call shifts.
Although the union withdrew its Industrial Relations Commission case, the fight continues.
“We’re turning to local MPs and targeting Goulburn’s marginal seat status to push for reform,” Taylor said. “Response times won’t improve with the current plan.”
He pointed to the South Coast where, despite a doubling of staff, emergency response times remain above the state average.
“It’s disgraceful,” Taylor said. “We’ve got specialty units up north for the floods, but in Goulburn, someone’s grandma waits an hour with a fractured femur. It’s not just bad policy - it’s a moral failure.”


“IT’S A DISGRACE. WE’RE STILL FIGHTING AND EXPOSING THE ENORMOUS WASTE OF TAXPAYER FUNDS...”
AFAC25 powered by INTERSCHUTZ Conference & Exhibition returns to Western Australia, delivering products, services, and solutions for all emergency management and rst responder sectors.
Ambulance Fleet requirements, asset management, dispatch systems and t out, PPE, equipment, workforce learning and development, community risk reduction strategies and systems, emerging response operations communication technology, and so much more.
A world class showcase of international and national brands with best practice solutions for all rst responder sectors.

















Delivering solutions to these industry groups:
Fire First Responders / Police / Ambulance
/ Recovery Mining / Gas & Petroleum




Northern Territory’s ambulance service contract faces first tender in over 50 years following St John procedure ban.

FOR THE FIRST TIME IN MORE THAN half a century, the Northern Territory’s ambulance service contract will be open to competitive tender after St John Ambulance was prohibited from performing two critical, high-risk life-saving procedures.
NT Health Minister Steve Edgington confirmed that the existing St John contract is set to expire in early 2026, with preparations underway to commence a procurement process for a new contract.
A spokesperson for NT Health also revealed the department is reviewing service requirements to renew patient transport contracts starting in 2026.
“Procurement strategies for both emergency and patient transport services are being finalised,” the spokesperson said. “Upcoming tender opportunities and industry briefings will be announced soon.”
United Workers Union NT secretary Erina Early described the announcement as historic, marking a significant shift in the management of the Territory’s ambulance services.
“Since 1974, the St John Ambulance contract has simply been rolled over every five years,” Ms Early explained. “Despite numerous reviews highlighting issues, St John NT has consistently held the contract. This will be the first time a tender process is held for ambulance services in the Northern Territory.”
While the union continues to advocate for the ambulance service to be brought under direct government control, Ms Early noted the tender could attract bids from other private providers such as CareFlight, the Royal Flying Doctor Service, and Falck.
“There may also be interest from other government ambulance services,” she added.
Given the ongoing turmoil within St John NT, Ms Early expressed confidence that a change in provider would not cause major disruption.
“Our paramedics, patient transport teams, and communications officers are highly professional,” she said.
“Considering the current clinical governance challenges and recent vote of no confidence, a transition could even stabilise the service.”
Minister Edgington’s announcement followed St John NT’s immediate suspension last Friday of two “High Acuity, Low Occurrence” (HALO) procedures: finger thoracostomy and pre-hospital emergency anaesthesia.
Andrew Thomas, Director of Ambulance Services at St John NT, informed staff that these procedures were halted due to concerns raised by the Road Ambulance Services Clinical Governance Committee.
“This suspension will remain until governance and oversight requirements - particularly the appointment of an Ambulance Service Medical Officerare fully met,” Mr Thomas said.
Mr Edgington emphasised the suspension was a “proactive safety measure,” noting that concerns about these HALO procedures and gaps in clinical governance had previously been highlighted in a leaked independent Clinical Governance Review from December.
Mr Thomas confirmed on Tuesday that St John NT is actively working with NT Health to implement the report’s recommendations.

“We are currently recruiting a medical director,” he said.
The HALO procedures had been introduced three years ago under a former chief medical officer, with nine Intensive Care Paramedics trained and qualified to perform them.
“St John NT remains committed to the health and wellbeing of our community. Our crews are dedicated professionals managing some of the nation’s most complex medical emergencies,” Mr Thomas said.
NT Health stated that St John NT was notified of the suspension on Friday, June 6, following a thorough review of clinical governance and procedural compliance.
“This action is part of due diligence and a proactive commitment to safetynot in response to any specific incident,” a department spokeswoman said.
“NT Health will continue to work closely with St John Ambulance to reach a satisfactory resolution, including the timely appointment of a medical director to oversee patient safety and quality improvements. This appointment is expected in the coming weeks.”



Ambulance officers with Hato Hone St John call for real funding in the Budget to improve pay and conditions, warning the Government of the risk of losing experienced paramedics offshore or into further industrial action.
AMBULANCE DELEGATES FROM across Aotearoa gathered in Auckland for a Workers First conference (photo above) as the group prepares to enter bargaining again with the partially charity-funded ambulance provider. They also discussed their growing concerns about a workforce crisis that is being made worse by insufficient public health funding.
Faye McCann, Workers First National Ambulance Coordinator, said that this year’s Budget marks the final year of a four-year ambulance funding agreement, and last year’s negotiations had failed to substantially lift wages, address penal rates that are significantly lower than comparable health professions, or deliver
the infrastructure needed to keep the service functioning successfully while meeting growing patient demand.
"We can’t keep plugging holes with goodwill and expecting ambulance officers to carry the cost of a broken system," said Ms McCann.
"Ambulance staff are already burnt out, understaffed, and responding to more mental health and high-risk incidents than ever before. It’s getting worse, especially in Auckland, where short staffing is at crisis levels even as the population grows and demand rises."
"Officers are leaving for Australia because the pay is better, the infrastructure is better, and the workload is safer.
We’re losing people we can’t afford to lose."
Ms McCann said ambulance officers were dismayed that last year’s Budget failed to fulfil the National Party and New Zealand First’s coalition promise to increase the proportion of Government funding for the country’s ambulance services.
"When it comes to the Treaty Principles Bill or other dodgy political priorities, the coalition agreement framework between parties is treated like it’s enshrined in law - but when it comes to funding emergency services, that promise is suddenly a 'nice-to-have'," said Ms McCann.
She warned that unless this Budget delivers real improvements, ambulance officers could be forced back into the same impossible bargaining position as last year, when St John repeated that they couldn’t improve wages and conditions without additional Government funding.
"Some funding eventually came, but only after a national strike and a drawn-out, behind-closed-doors process that no one wants to repeat," said Ms McCann.
"We’re calling on the Government to fund ambulance services properly so that St John can offer decent wages, fair conditions, and a service that New Zealanders can actually rely on."
"Cuts to the broader health budget, or a failure to meet growing cost pressures and rising demand, will mean ambulance officers are the ones bearing the brunt of underfunding, and patients will be worse off for it."
"Ambulance services cannot be the casualty of another austerity Budget from this Government."
Ms McCann said that Workers First ambulance officers’ ultimate goal remained the full operational funding of emergency health services, and she believed that services like St John and Wellington Free fully supported that aim.













Emergency Operations Centre Construction Site.
THE AMBULANCE EMPLOYEES ASSOCIATION (AEA) recently had the opportunity to tour the construction site of the new South Australian Ambulance Service (SAAS) Emergency Operations Centre (EOC) at Mile End Southand the progress is impressive.
This state-of-the-art facility will soon be home to over 200 AEA members, including critical roles such as triple zero (000) call takers, ambulance dispatchers, operational leadership teams, clinicians, rostering staff, and MedStar personnel. Together, these dedicated professionals form the backbone of SAAS’s emergency response system, working tirelessly to ensure help reaches South Australians when they need it most.
The project also includes the construction of a brand-new ambulance station, designed to house four 24/7 ambulance crews and solo responders. Additionally, the site will feature enhanced training facilities aimed at supporting and developing the next generation of paramedics - ensuring a skilled workforce for years to come.
Construction began in 2023, with completion expected later this year. The AEA extends its sincere gratitude to all members who have fought relentlessly for improved resources, making this vital upgrade possible and helping to keep the South Australian community safe.






A review into ambulance ramping at Tasmanian hospitals has revealed an improvement in patient handover times, with transfers completed within the target timeframe jumping from 67% to 82% over the past nine months.
THE TRANSFER OF CARE REVIEW found all four major public hospitals across the state have made progress since the government’s 60-minute ‘ramping ban’ came into effect in April 2024.
Health Minister Jacquie Petrusma welcomed the findings, noting ambulances spent 21,504 fewer hours ramped compared to the previous year, a 67% reduction.
“This is an outstanding improvement and means ambulances are being released from hospitals back into the community and helping Tasmanians sooner,” Petrusma said.
“The amount of time that paramedics are spending at hospitals has also significantly reduced, from an average of 52.5 minutes in April 2024, to just 36.3 minutes in April 2025.”
“I want to thank our dedicated healthcare staff who are making this possible and I am grateful for the contributions of all stakeholders.”
But medical experts warn that while ambulances are moving on quicker, the deeper issue of hospital overcrowding still hasn’t been resolved.
Dr Michael Lumsden-Steel, president of the Australian Medical Association’s Tasmanian branch, said the improvements have simply shifted pressure points elsewhere in the system.
“We’ve been able to get the patients out of the ambulances quicker, but our EDs aren’t really achieving much greater flow out
of the emergency departments into the hospitals,” he told Local Radio.
The review singled out Launceston General Hospital as continuing to struggle with patient movement, with Dr LumsdenSteel calling it “one of the worst” in the country for transfer rates out of the ED.
The Royal Hobart Hospital achieved a 14% improvement in transfer rates despite increasing patient acuity, while North West Regional Hospital and Mersey Community Hospital performed best with 92% and 96% rates respectively.
The report made four key recommendations, including that each hospital develop its own action plan to tackle delays and that data reporting systems be improved.
Dr Lumsden-Steel identified a critical shortage of subacute beds as a major contributing factor to ongoing congestion.
“I think we’ve maximised with this little project the maximum efficiencies we can get. But now we need to increase capacity,” he said.
“I think there’s a lot of effort and money being spent to try and improve the capacity. We’ve got a long way to go.”
The Department of Health says it will now work with staff and unions to implement the review’s recommendations, with consultations to begin in the coming weeks.






A tragic incident has raised fresh concerns about hospital ramping after an elderly man died waiting for help.
AN ELDERLY MAN IN BLACKBURN tragically died from severe bleeding despite making two emergency calls to triple-0, while multiple ambulances remained nearby but were unable to respond.
The man contacted emergency services just before 11:30 pm on June 5 after a fall that caused a serious head injury. Nearly five hours passed before paramedics arrived, only to find he had already passed away. Before his death, he had made a second urgent call for help.
Reports indicate that up to five ambulance crews were delayed at Box Hill Hospital, unable to leave as they awaited clearance to hand over their patients. Paramedics reportedly asked hospital staff to expedite their release but were told they must remain until beds were available.
Danny Hill, secretary of the Victorian Ambulance Union, said the
paramedics who finally reached the man around 4 am - after firefighters gained forced entry - were deeply affected by what they encountered.
“They were shocked by the extent of his injuries and the fact that he was able to call for help in such a condition,” Hill said. “It was a very distressing situation for them.”
The incident has triggered an internal review by Ambulance Victoria, and the matter will also be referred to the state Coroner for further investigation.
An Ambulance Victoria representative said the organisation is committed to delivering excellent patient care and is thoroughly examining the case to understand what occurred. They added that further comments are limited due to the ongoing Coroner’s inquiry.
This tragedy comes as a parliamentary inquiry into Ambulance Victoria continues, focusing on challenges such as ambulance

ramping, paramedic workloads, internal misconduct, and workplace culture.
Evidence presented to the inquiry has revealed that systemic issues have led to lives being lost and others being placed at risk, amid reports of burnout, poor management, and harassment.
When asked about delays in releasing ambulance crews, a spokesperson for Eastern Health, which manages Box Hill Hospital, acknowledged the significant pressure on emergency departments due to an influx of severe cases and limited bed availability.
They expressed condolences to the family of the deceased and noted ongoing efforts to collaborate with Ambulance Victoria to reduce ambulance wait times.
A government spokesperson highlighted that unprecedented demand on paramedics and hospitals has led to a historic $31 billion investment in health services in the recent budget.














The Victorian Ambulance Union (VAU) welcomes additional spending in the Victorian healthcare system.
IN PARTICULAR WE ARE PLEASED TO see further investment in hospitals and urgent care clinics. Investment in the Victorian Virtual Emergency Department (VVED) is also welcome as it prevents unnecessary transports of nonemergency patients.
However, we are disappointed that long overdue election commitments have not been delivered in this budget.
In 2022, the VAU had discussions with the Victorian Government regarding improvements to the Non Emergency Patient Transport (NEPT) sector who play a vital role in transporting patients and freeing up Ambulance Victoria (AV) emergency paramedics to respond to time critical emergencies.
Over 20,000 non-emergency cases each year are unable to be attended to by the private NEPT contractors and are subsequently handed to emergency paramedic crews, preventing them from responding to emergency cases. Private NEPT providers in rural areas
have pulled out of contracts, leaving local AV paramedics overwhelmed with both emergency and non-emergency caseload.
In 2022, the VAU received commitments from the Victorian Government to strengthen the NEPT sector, improve working conditions for Patient Transport Officers and Ambulance Transport Attendants by reducing casualisation, standardising pay and enabling portability of entitlements across employers.
The Government also committed to a review into the outsourcing of NEPT to private contractors with a view to bringing patient transport back into AV.
That review ran throughout 2023 and made several recommendations to improve the sector for both patients and staff. Two years after the review, our members and the industry are still awaiting answers, and there has been no investment or improvements in the privately run NEPT sector.
NEPT is a vital component of the healthcare system and is responsible for
the movement of hundreds of patients every day to appropriate care. Our NEPT sector needs reform and investment to run efficiently and safely as recommended in the Government’s own review. It is disappointing that the Government hasn’t delivered on this commitment.
Quotes attributable to Danny Hill Secretary of the Victorian Ambulance Union
“The Government made commitments to our members to reform the NEPT sector, improve their conditions and free up paramedics from unplanned nonemergency cases so they can respond to emergencies. Three years later we are still waiting for the Government to deliver on its promise.”
“We shouldn’t be surprised that one in three emergency patients are still not getting an ambulance on time. There are over 20,000 NEPT cases each year, that can be resourced by the private contractors. Paramedics end up doing patient transport cases instead of responding to emergencies”.

IN ST JOHN AMBULANCE WESTERN Australia Ltd T/A St John Ambulance WA and United Workers’ Union [2025] FWC 1375, Commissioner Lim of the Fair Work Commission made recommendations aimed at resolving an ongoing dispute between St John Ambulance (WA) and its staff.
The dispute concerned the terms of a new enterprise agreement intended to replace the expired St John Ambulance Western Australia Ltd Ambulance Officers’ / Paramedics Enterprise Agreement 2021. That agreement expired in June 2024, and negotiations had been underway since December 2023. A draft agreement was presented to the workforce on 14 March 2025 but was rejected. Following this, the union sought and gained member approval to undertake protected industrial action.
On 24 March, St John Ambulance requested the Commission’s involvement to help resolve outstanding issues.
At that time, unresolved matters included:
• Rates of pay
• Breaks between shifts for employees working the 2/2/4 and 4×4 roster patterns
• The block-out period relating to shift conclusion work allocation
• Duration and extension periods for Community Paramedic secondments
• Introduction of a new day, early, late, and night roster pattern
• Rates of pay for the CCP/ECP classification
• The manner in which overtime is allocated
• A framework for managing performance and conduct issues

• Introduction of a new classification level, AP4
• Methods for addressing long service leave
• Updates to consultation committee processes and outcomes
• Developing back-to-back community paramedic coverage over time The parties engaged in further negotiations and on Wednesday, 14 May 2025, St John Ambulance presented its best and final offer to the bargaining representatives. (This detailed offer can be reviewed in full within the Commission’s decision.)
The offer will be presented to the workforce as a Proposed Agreement for their vote, with voting access starting no later than Wednesday, 28 May 2025. Employees will have the opportunity
to review the terms and decide whether to accept them.
Commissioner Lim issued a cautious assessment:
“It is my view that any further protected industrial action will not achieve a better bargaining outcome. Even if union members were to take additional industrial action, St John Ambulance is constrained by its contract with the WA State Government and current financial losses, limiting its ability to improve the offer. Simply put, members risk further industrial pain and wage loss for no better result.”
“There is also a significant risk that continued or escalated industrial action will lead to protracted litigation before the Commission or Courts, benefiting neither the workforce nor the negotiations.”
“I also note that if no enterprise agreement is reached, there is a real possibility that one party will apply for an Intractable Bargaining Declaration (IBD). While I do not predict the outcome of such proceedings, I observe that IBD processes tend to be lengthy and resource-intensive. Ultimately, this could result in the Commission determining the terms of a replacement enterprise agreement, rather than the parties themselves.”
Commissioner Lim recommended the workforce vote to accept the proposed agreement, noting she understood the union would be advising its members to support it. It remains to be seen whether the St John workforce will accept the current offer.

WESTERN AUSTRALIAN AMBULANCE workers entered their third week of protected industrial action on May 14 against their employer St John Ambulance, the principal provider of ambulance transport.
Union members have chalked campaign messages on the windows of their vehicles, highlighting the inadequate pay and conditions paramedics face.
“Ambos=Saving Lives, WA Health=Saving $’s” highlights the levels of exploitation frontline workers face to cover for WA Labor’s failure to properly fund the health system.
Others, such as, “13 hour night shifts … no break. Are you safe? We aren’t” and “‘No more money left’... said 3000 managers” point to St John’s disregard for workers’ safety and wellbeing and perceptions that resources are being erroneously directed to excessive bureaucracy while frontline services suffer.
The United Workers Union (UWU), which covers ambulance workers across the country, overwhelmingly rejected St John’s recent proposal in April to settle. Enterprise agreement negotiations have gone on for months.
A majority of UWU members supported protected industrial actions in their April 14 ballot. They include: an unlimited number of stoppages for 10 minutes; employees putting themselves first in relation to fatigue management and only accepting overtime shifts of their choosing;
employees not performing work unless wearing union T-shirts or black T-shirts; and stoppages to write campaign messages on the outside of vehicles.
Members also approved periodic or indefinite bans on a number of aspects of work including: training/tutoring employees on the road; using the St Johncontrolled Yammer and WhatsApp groups; responding to or acting upon contact from St John’s outside of normal work hours; starting vehicle and equipment checks outside work hours; using the calendar to indicate overtime availability; and accepting emergency calls outside of work hours.
The UWU has ruled out strike action beyond minor stoppages due to a commitment to patients. They stress people should still call 000 and services will not be interrupted.
Beyond a compound raise of 21.6% over the new three-year agreement, unionists are demanding strong measures to stop them being forced to do hundreds of hours of overtime.
The UWU emphasises their members’ serious concerns with how spiralling hospital emergency room wait times are negatively affecting the quality of care residents receive, and the availability of ambulance response services.
The ramping crisis was described on April 29, where paramedics are forced to spend hours providing treatment to
patients in ambulances, outside hospitals, while waiting for a bed to become available. It means that ambulances are not being used to transport patients.
“In 2017, ambulances were ramped for an average of 819 hours per month. By 2025, that figure has surged to over 5100 hours each month - a staggering increase. To put it in perspective, former Health Minister Roger Cook labelled it a ‘crisis’ back in 2015, when ramping was just onefifth of what it is today.”
WA Premier Roger Cook has offered glib praise for paramedics, but said little about the dispute besides urging St John’s and the union to resolve differences so the health sector is not impacted. However, the critical shortage of ambulance workers and the ramping crisis, caused by a shortage of emergency room beds, are problems that only the government can resolve.
St John’s Ambulance WA, a registered charity, received the greatest slice of its funding which contributed to its $2.8 million surplus last year, from userpay services and first aid training. It also received 44.8% of its funding from government contracts.
The UWU has submitted multiple Freedom of Information requests to examine the Labor contract with St John’s for ambulance services. These requests were denied on the basis that the contracts are “commercial in confidence.”

We’re always t he re to help. Let ’s m a ke su re we help eac h ot he r a n d a sk R U O K?

08 9325 2424 • www.easternguruma.com.au
Eastern Guruma has been in operation for 20 years and is a 100% owned Indigenous company providing services in rehabilitation, landscaping, facilities management, traffic management, road works, drilling and more. Eastern Guruma is owned by members of the language group Muntulgura Guruma, the lands of which surround Tom Price in the Pilbara Region of WA the team has delivered services to Australia’s largest mining companies, Rio Tinto, BHP and Fortescue Metals Group.
Eastern Guruma is exploring the expansion into the building services industry. Leveraging its strong and reliable reputation; the aim is to extend our expertise into residential & construction maintenance including the refurbishment of houses and related projects in the Pilbara and Kimberly regions. Recognised as the ‘one stop shop’ for all maintenance and building services, Eastern Guruma will provide electrical, HVAC, plumbing, instrumentation and building services as it expands its platform into construction.

Eastern Guruma recently celebrated its 20th anniversary. Held at Frasers, Kings Park - it was the perfect venue for such a milestone occasion. Staff and VIP guests honoured the co-owners’ and directors’, Tania Stevens and Samantha Connors and all their accomplishments. All were incredibly proud of the journey and achievements over the past two decades. The milestone marked two decades of growth and achievements since its inception in 2004. The celebration highlighted significant milestones, including the rapid expansion from 2009 through to 2023 which saw Eastern Guruma receive prestigious awards such as the Business News 2023 RISE Business Award and the Rio Tinto 2023 Local Engagement Award. The 20-year celebration was a chance for all to celebrate and a testament to Eastern Guruma’s vision, dedication and hard work.
The company has recently invested in significant capital expenditures to its fleet, including the purchase of a CAPEX D9 100T float Liebherr Dozer, Excavator, Digger, and over 40 light vehicles. The acquisition of the Cat D9 Dozer comes with customizable blade options, efficient boosters, integrated components, advanced technology and cost-effective performance this empowers the team to deliver results that exceed client expectations. With this powerful tool at their disposal, the team is ready to achieve new heights in the industry. The dedication and expertise of the Eastern Guruma team have played a pivotal role in facilitating the purchase of new equipment on Site for our team.



Additionally, Eastern Guruma’s landscaping and maintenance contract with Fortescue Solomon’s Kangi Camp has been renewed for another five years. The contract ensures continued collaboration and service excellence whilst working towards a carbon neutral supply of plant & equipment by transitioning from diesel to electric. Eastern Guruma’s ongoing growth and success is a testament to its commitment to community development, industry excellence, and the empowerment of Indigenous people.

Eastern Guruma has been fortunate enough to acquire its own business premises in Perth. Located on the corner of Bulwer Street and Fitzgerald Street, Perth settlement was in July. The new premises has undergone a recent extensive refurbishment upgrade and includes open plan seating, 15 offices, five meeting rooms and one boardroom.
Eastern Guruma is proud to announce we have more than 30% of our 300 staff employed as First Nations People working full time in the mining industry. This is an outstanding result of focus and dedication from our HR and Indigenous Employment, Engagement and Development teams. Great efforts from the road shows, screening of candidates and assisting those who need a hand to get through the process. The milestone reflects the company’s dedication to providing employment opportunities for First Nations People.




