4 minute read
Q&A: Artificial Urinary Sphincters
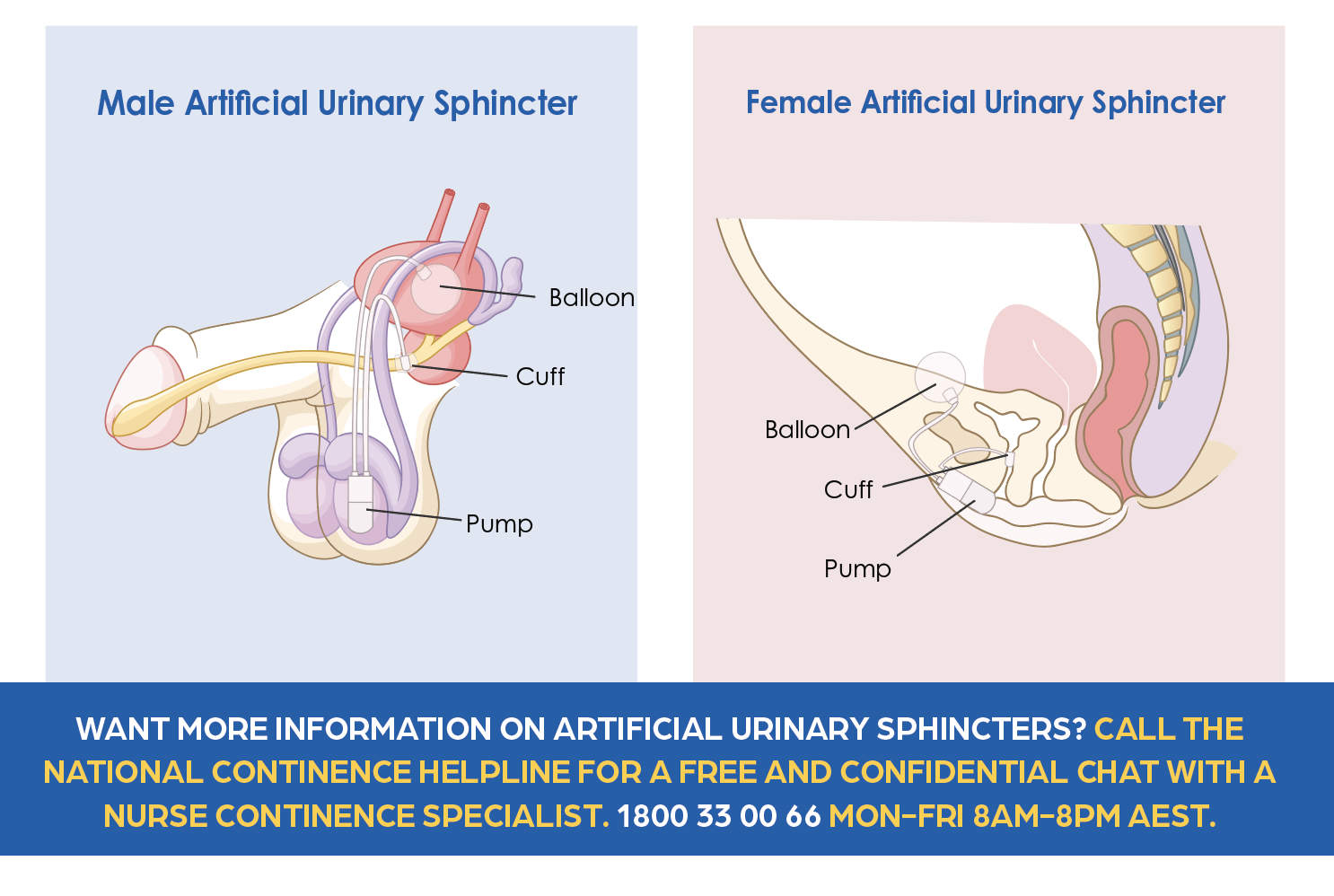
We talk to urologist, Professor Eric Chung, about innovation and technology in continence health. He specialises in the artificial urinary sphincter which can help both men and women experiencing trouble controlling their urine (wee). It involves a surgical procedure to implant the device and can be life changing for people with severe bladder symptoms.
Q: WHAT IS AN ARTIFICIAL URINARY SPHINCTER (AUS) AND WHICH SYMPTOMS CAN IT TREAT?
A: An artificial urinary sphincter is a device that mimics the natural urinary sphincter (muscles in the body that control the flow of urine) to provide urinary continence. It is offered for those with moderate to severe urinary incontinence (more than 4-5 pads per day or greater than 500 ml/24hr pad when weighed). It is considered the gold standard treatment for male stress urinary incontinence, radiation-induced incontinence, and those who have persistent or recurrent incontinence following male sling surgery (insertion of mesh-like surgical tape to reinforce your bladder where it joins the urethra which is the tube that allows urine to exit out of your penis). Although more common in men, these devices can also be used in women.

Q: HOW DOES AUS WORK?
A: When working well, your urinary natural sphincter is closed tight most of the time, and you relax it to urinate. The AUS works in the same way, the cuff part of the device is tight around your urethra until you want to go to the toilet, then you use a pump in your scrotum or labia to relax the cuff and let the wee out. It prevents leaks and accidents in your day-to-day life.
Q: WHAT ARE THE RISKS, BENEFITS AND ALTERNATIVES?
A: The benefit is that the patient will be dry and is able to resume and enjoy day-to-day activities without wearing a continence pad. Any surgery can have risks and these include cuff erosion or movement, recurrence of incontinence and damage to other surrounding structures (such as the urethra where your wee comes out). The male sling is effective for those with mild to moderate incontinence and those without radiation damage. Otherwise, the patient would have to consider continence pads, a penile clamp or an indwelling urinary catheter into the bladder.
Q: HOW HAS THE AUS CHANGED SINCE IT WAS INTRODUCED 50 YEARS AGO?
A: The device is more robust now with higher durability and mechanical reliability. Advances in scientific technology and surgical techniques have enhanced the clinical outcomes and patient satisfaction rates. The usual mechanical life span is around 7-10 years.
Q: HOW HAS THE SURGICAL PROCEDURE AND AFTER-CARE CHANGED?
A: We see streamlining of the surgery and enhanced postoperative care. The patient usually stays 1 night (instead of 2 nights) in the hospital, and the device can be activated ready to use after 4 weeks (previously 6 weeks postoperatively). There are new surgical techniques to deal with complex patients such as those with radiation-related incontinence, existing penile prosthesis implant, redo incontinent surgery cases, patients who need to perform self-catheterisation (regularly insert a catheter to empty their bladder), and females with stress urinary incontinence.
Q: WHAT QUESTIONS SHOULD PATIENTS ASK THEIR UROLOGISTS WHEN CONSIDERING AN AUS?
A: Patients should choose a urologist who has completed formal training in prosthetic urology and can handle complex reconstructive cases. It is important to find a urologist who is regarded as an expert surgeon in this field. Remember, the first operation is the most critical to ensure success and avoid complications.
Q: ARE THERE ANY INNOVATIONS AND NEW TREATMENTS BEING DEVELOPED IN UROLOGY?
A: Yes, there are other novel AUS-like devices in the market now, with research into the role of an electronic AUS device. As we learn more about male incontinence, we realise quality of life is important for these patients, and that wearing a pad is not the solution. Patients should be encouraged to seek an effective (and more permanent) solution and strive to be pad-free!