8 minute read
Dear diary…A day in the life of someone with a birth injury
Julianne ran athletics at state level, but after giving birth she couldn’t run, jump, cough, or even sneeze without experiencing leakage. She eventually went on to have surgery to repair the injuries she sustained during childbirth. This is her story.
NAME: Julianne
FAMILY: Husband in the military and two young children. I have an au pair who helps to look after my youngest while I am at work.
OCCUPATION: Former military, now senior program management role for a major consultancy firm.
CONDITION: Prolapse resulting from a birth injury.
SYMPTOMS: Constipation, diarrhoea, urinary leakage.
TREATMENT: Pelvic health physiotherapy, surgery.
Before kids...
Prior to childbirth, I would exercise most days, regularly running 5km with bursts of sprinting. I also worked out at the gym focusing on building strength and enjoyed landscaping my garden—often lifting bags of soil as needed. Prior to joining the Army, I was in the best fitness of my life—doing stair runs, sit-ups and push-ups to meet the basic entry standards.
Pregnancy...
During my pregnancy, I attended bi-weekly specialist pregnancy fitness classes with a pelvic health physiotherapist in Brisbane, which focused on our core and pelvic floor strength. Throughout my life, my mother had regularly described the prolapse issues she faced after delivering me and how it had impacted her. I shared these concerns with my obstetrician who dismissed them.
Birth injury...
I was induced for the birth of my first child. I received an epidural after around 4 hours. After a relatively short first stage of labour (8 hours for a first-time mother), I was instructed to start pushing. I didn’t get much guidance from either the midwives or the doctor on pushing and breathing (something I learnt about from my very different second birth experience). After 45-minutes of pushing, my obstetrician declared that my daughter was stuck and in distress, and that they needed to use the vacuum to extract her. The doctor said they would need to perform an episiotomy (a cut to the perineum—the area between the vaginal opening and the anus—to allow them to insert the vacuum). Three pulls of the vacuum were used on me before my healthy daughter was born with an initial AGPAR (birth score out of 10) of 8, which increased to 9 at the five-minute interval. She certainly didn’t exhibit any signs of having been in distress. Following her delivery, I suffered a significant haemorrhage. The quantities were not recorded, but it was enough for me to go into a state of shock and required medication to help stop my bleeding. There were no details recorded in my post birth report—but I believe I had a third-degree tear from the vaccum (tear that involves a partial tear of the muscles around the anus that control when you do a poo), which was stitched in the birth suite. I struggled to walk for around 24-30 hours following the birth and couldn’t sit comfortably for around 4 weeks.
Around 4 weeks after the birth, I felt significant ‘heaviness’ above my vagina and inside my pelvis which I reported to my obstetrician. She dismissed it as ‘still healing and recovering’ and didn’t conduct an internal assessment to determine if there were any issues. Again—I didn’t realise this should have been routinely performed until the birth of my second child. Currently, there is no Australian guideline requiring an internal assessment following a vaginal delivery—however ‘best practice’ recommends it. When I was 6-weeks post-partum I saw a pelvic health physiotherapist who cleared me for exercise, and suggested I continue my pelvic floor exercises.
ON THE OUTSIDE I WAS A FIT, HEALTHY YOUNG WOMAN—BUT MY INSIDES WERE BETRAYING ME. I NEVER EXPECTED THAT GIVING BIRTH WOULD IMPACT MY ABILITY TO REGULARLY EXERCISE.
Incontinence...
When I eventually felt like I had recovered enough to go for a run, I leaked with every step I took. I tried stopping and starting again, but the leaking continued. The next time I went to the bathroom before I left, but I had the same result. I increased my pelvic floor exercises but it made no difference. I had also noticed if I sneezed or coughed I would leak. I didn’t really talk to anyone about it because I assumed it was normal, especially as I was still less than 12-months post-partum.
When my daughter was 2, we took her to a trampoline centre. With every bounce I took, I leaked. I spent more time in the bathroom than with my daughter that day. I eventually sat on the side watching her, and realised my problem was more severe than I wanted to live with.

Seeking treatment...
I spoke to my GP and he referred me to a pelvic health physiotherapist. There, they gave me an internal assessment and informed me that I had a prolapse with 2 options—wear a pessary (supportive device inserted into the vagina) and/or more pelvic floor exercises. I opted for more exercises, but I knew they weren’t making a difference.
Fast forward another 2 years and we were being sent to the USA for my husband’s work. Whilst there, I gave birth to my second, and last, child. My birth was a breeze compared to my first, with no tears. My doctor gave me clear direction on how to correlate my pushes with my breathing, and I was in control of my epidural through a button—I could still feel my legs and walked from the birth suite to my room after delivery.
At my 6-week check up my doctor did a full internal exam and identified a ‘cystocele’ and ‘rectocele’–terms I had never even heard before. Which meant I had a prolapse of the bladder into the vagina and prolapse of the rectum (or lower bowel) into the vagina. It was the first time I had been diagnosed with a rectocele and it made so much sense—it explained why I had constantly struggled with either diarrhoea or constipation. She referred me to a urogynaecologist who did a range of internal assessments as well as advanced 3D imaging. He was able to show me that my muscles had torn from the pelvis and were struggling to hold up my internal organs. I was shocked; partially because of the severity of the diagnosis but also that this hadn’t been detected or even examined before. Why hadn’t this been checked in Australia? Why didn’t the doctor check this before my second delivery?
His explanations were detailed, but also simple. I had 2 options, a pessary or surgery. If I didn't have surgery, I would likely have a complete prolapse within 10 years and my symptoms would increase. He explained that the surgery was still relatively new—he had pioneered it and had been performing it for several years—but because of this there was no data to indicate long-term success. The process of repairing and restitching my muscles would be performed robotically and laparoscopically (through small incisions with cameras to guide the surgeon), the most minimally invasive. However, it was considered major surgery and initial recovery would require 6-8 weeks of rest and support, and full healing would take 6 to 9 months. We carefully reviewed the risks and benefits. I did as much research as possible—joining various forums of women that had undergone similar pelvic floor repair or removal of their uterus. Some of the posts were worrying. Some surgeries had failed. Others complained of extreme tightness at the vaginal entrance, making intimacy more challenging. All wrote how difficult the recovery was, it was certainly daunting. As the surgery date crept closer, I began to prepare myself as much as possible.

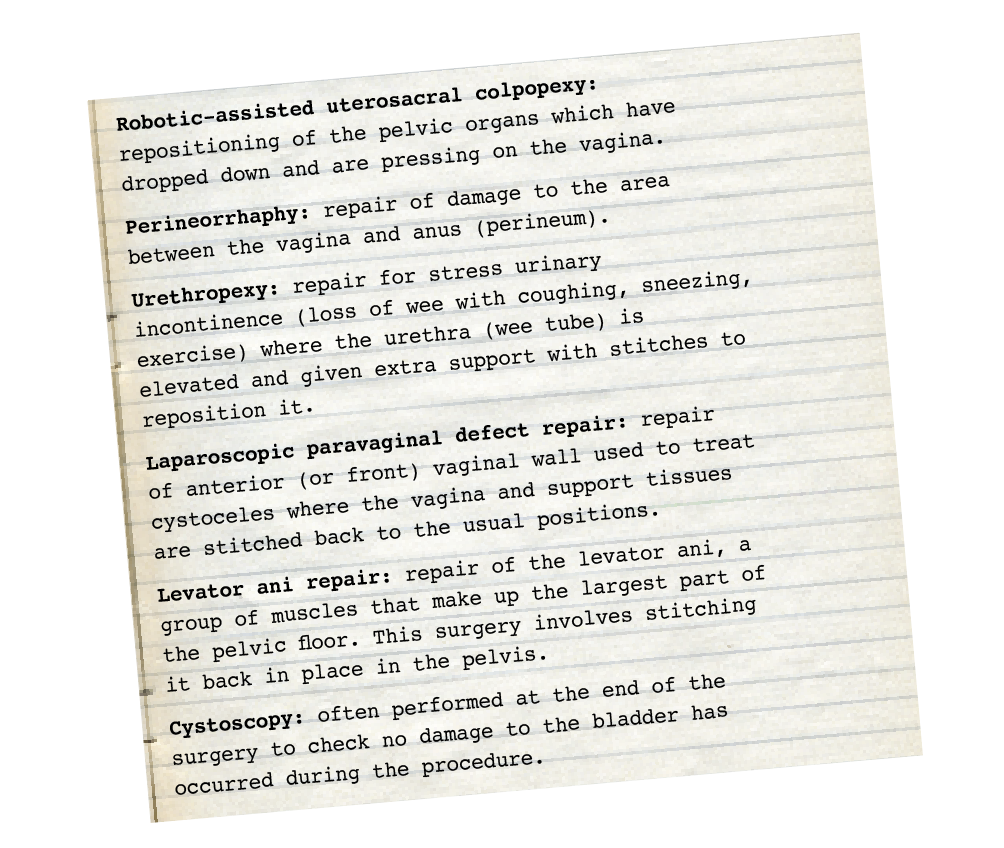
Julianne’s surgery
There are many treatments for prolapse and incontinence, of which surgery is one. The technology has come a long way and is now able to be performed through small skin incisions with robotics which makes it less invasive with a shorter healing time.
The future...
It has now been 9 months since my surgery and I am just beginning to get back into exercise. So far I don’t experience any leakage when I run. I am probably being overly cautious, but want to give my body adequate time to heal internally.
Because prolapse and incontinence involve sharing such personal information, women haven’t discussed it in the past and medical professionals don’t seem to have a full awareness or regard for it. Until now, it has essentially been a ‘silent’ issue. One of the most positive outcomes of the internet and low-cost connectivity around the world is the connection of women of all ages and nationalities in online forums. Being able to type and share our experiences provides some aspect of anonymity, and with that, less shame. It is allowing women from Europe, Australia, Asia and the Americas to connect, question and understand their births and birthing injuries. I strongly feel that women should be given information at the time of their birth, or upon discharge, of their right to make an official complaint. I hope that through advocacy and awareness, that others can better learn and prepare and hopefully avoid some of the issues I have faced.
In sharing the intimate details of my experience I hope to provide other women with the courage and insight to question more and expect more from their medical treatment, especially before and after giving birth.
For more information on incontinence and prolapse after birth, call the National Continence Helpline for a free and confidential chat with a nurse continence specialist. 1800 33 00 66 Mon-Fri 8am-8pm AEST.