LYNN CLARK
Nic ole Kofoe d
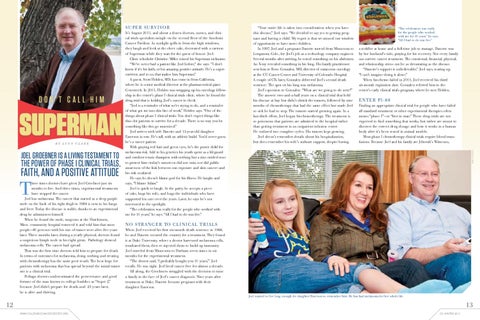
Don’t call him
Superman B y L y nn C l a r k
Joel Groebner is a living testament to
the power of phase I clinical trials,
faith, and a positive attitude
T
hree times doctors have given Joel Groebner just six months to live. And three times, experimental treatments have stopped the cancer. Joel has melanoma. The cancer that started as a deep purple mole on the back of his right thigh in 1988 is now in his lungs and liver. Today the disease is stable, thanks to an experimental drug he administers himself. When he found the mole, surgeons at the Hutchinson, Minn. community hospital removed it and told him that most people—80 percent—with his size of tumor were alive five years later. Three months later, during a yearly physical, doctors found a suspicious lymph node in his right groin. Pathology showed melanoma cells. The cancer had spread. That was the first time doctors told him to prepare for death. In terms of outcomes for melanoma, doing nothing and treating with chemotherapy has the same poor result. The best hope for patients with melanoma that has spread beyond the initial tumor site is a clinical trial. Perhaps doctors underestimated the perseverance and good fortune of the man known to college buddies as “Super J,” because Joel didn’t prepare for death, and 23 years later, he is alive and thriving.
It’s August 2011, and about a dozen doctors, nurses, and clinical trials specialists mingle on the second floor of the Anschutz Cancer Pavilion. As sunlight spills in from the high windows, they laugh and look at the sheet cake, decorated with a cartoon of Superman while they wait for the guest of honor: Joel. Clinic scheduler Christine Miller coined his Superman nickname. “We’ve never had a patient like Joel before,” she says. “I don’t know if it’s his faith, or his amazing positive attitude. He’s a supersurvivor, and to us, that makes him Superman.” A guest, Scott Holden, MD, has come in from California, where he is senior medical director at the pharmaceutical giant Genentech. In 2001, Holden was wrapping up his oncology fellowship in the center’s phase I clinical trials clinic, where he found the drug trial that is holding Joel’s cancer in check. “Joel is a reminder of what we’re trying to do, and a reminder of what got me into this line of work,” Holden says. “One of the things about phase I clinical trials: You don’t expect things like this—for patients to survive for a decade. There is no way you let something like this go unnoticed.” Joel arrives with wife Danette and 13-year-old daughter Emerson in tow. He’s tall, with an athletic build. You’d never guess he’s a cancer patient. With graying red hair and green eyes, he’s the poster child for melanoma risk. Add to his genetics his youth spent as a lifeguard and outdoor tennis champion with nothing but a zinc-oxided nose to protect him—today’s sunscreen did not exist, nor did public awareness of the link between sun exposure and skin cancer—and his risk escalated. He says he doesn’t blame god for his illness. He laughs and says, “I blame Adam.” Joel is quick to laugh. At the party, he accepts a piece of cake, hugs his wife, and hugs the individuals who have supported his care over the years. Later, he says he’s not interested in the spotlight. “The celebration was really for the people who worked with me for 10 years,” he says. “All I had to do was live.”
“Your entire life is taken into consideration when you have this disease,” Joel says. “We decided to say yes to getting pregnant and having a child. My regret is that we missed our window of opportunity to have more children. In 1997, Joel and a pregnant Danette moved from Minnesota to Longmont, Colo., for Joel’s job as a technology company engineer. Several months after arriving, he noted something on his abdomen. An X-ray revealed something in his lung. His family practitioner sent him to Rene Gonzalez, MD, director of cutaneous oncology at the CU Cancer Center and University of Colorado Hospital. A couple of CTs later, Gonzalez delivered Joel’s second death sentence: The spot on his lung was melanoma. Joel’s question to Gonzalez: “What are we going to do next?” The answer: two-and-a-half years on a clinical trial that held his disease at bay but didn’t shrink the tumors, followed by nine months of chemotherapy that had the same effect but made Joel so sick he had to stop. The tumors started growing again. In a last-ditch effort, Joel began biochemotherapy. The treatment is so poisonous that patients are admitted to the hospital rather than getting treatment in an outpatient infusion center. He endured two complete cycles. His tumors kept growing. Joel doesn’t remember details about his hospitalization, but does remember his wife’s stalwart support, despite having
“The celebration was really for the people who worked with me for 10 years,” he says. “All I had to do was live.”
a toddler at home and a full-time job to manage. Danette was by her husband’s side, praying for his recovery. Not every family can survive cancer treatment. The emotional, financial, physical, and relationship stress can be as devastating as the disease. “Danette’s support is unbelievable,” Joel says, tearing up. “I can’t imagine doing it alone.” When biochemo failed in 2001, Joel received his third six-month expiration date. Gonzalez referred him to the center’s early clinical trials program, where he met Holden.
E n t e r PI -8 8 Finding an appropriate clinical trial for people who have failed all standard treatment or other experimental therapies often means “phase I”—or “first in man.” These drug trials are not expected to find something that works, but rather are meant to discover the correct drug dosage and how it works in a human body after it’s been tested in animal models. Most phase I chemotherapy clinical trials require blood trans fusions. Because Joel and his family are Jehovah’s Witnesses, Nicole Kofoed
Su p e r Su rv ivo r
N o stran g e r to c li n i ca l t r ia l s When Joel received his first six-month death sentence in 1988, he and Danette scoured the country for a treatment. They found it at Duke University, where a doctor harvested melanoma cells, irradiated them, then re-injected them to build up immunity. Joel traveled from Minnesota to Durham seven times in six months for the experimental treatment. “The doctor said, ‘I probably bought you 10 years,’” Joel recalls. He was right. Joel lived cancer free for almost a decade. All along, the Groebners struggled with the decision to raise a family in the face of Joel’s cancer diagnosis. Nine years after treatment at Duke, Danette became pregnant with their daughter Emerson. Joel wanted to live long enough for daughter Emerson to remember him. He has had melanoma for her whole life.
12
13 www.coloradocancercenter.org
C3: Winter 2011