COLORADO MEDICINE

ADVOCATING EXCELLENCE IN THE PROFESSION OF MEDICINE
Sept. 22-23, 2023
COLORADO MEDICAL SOCIETY
YOU’RE INVITED TO OUR SIGNATURE EVENT CONNECT, LEARN AND RELAX


ADVOCATING EXCELLENCE IN THE PROFESSION OF MEDICINE
Sept. 22-23, 2023
COLORADO MEDICAL SOCIETY
YOU’RE INVITED TO OUR SIGNATURE EVENT CONNECT, LEARN AND RELAX
As your premier medical liability insurance carrier, you can trust us to put our strength, expertise, and agility to work on your behalf. Our claims support includes access to alternative resolution programs designed to help you confidently manage unexpected outcomes and preserve patient relationships. If a claim progresses, we protect and guide you, help you understand your options, and are with you each step of the way That’s Value Beyond Coverage.

Make plans to spend a fall weekend in the mountains with physicians from around the state; register for the signature event of the Colorado Medical Society – our Annual Meeting. There is something for everyone at this family-friendly event: relevant programming, networking opportunities and plenty of time to enjoy Vail.

8 MORAL INJURY IN HEALTH CARE – IT’S NOT JUST BURNOUT

Wendy Dean, MD, and Jeff Cain, MD, illustrate why physicians experiencing exhaustion, cynicism or decreased productivity are not just burned out, they are navigating moral injury due to a broken health care system.
11 MEDICAL MARRIAGE

Physicians face a number of professional challenges, and some of the stress can, in turn, harm a physicians’ marriages. CPHP Medical Director Scott Humphreys, MD, discusses the reasons for this and how to maintain healthy relationships.
12 DR. MICHAEL BESHOER: MORE THAN A PHYSICIAN
CMS member Carl E. Bartecchi, MD, presents an essay on one of the most prominent physicians of the Wild West, Dr. Michael Beshoer, who practiced in Pueblo and Trinidad and did so much more.

13 PHYSICIAN LEADERS REPRESENT COLORADO AT THE AMA ANNUAL MEETING
Your elected delegation to the American Medical Association represented you at the AMA Annual Meeting in Chicago in June.

26 FINAL WORD: COLORADO’S HEALTH CARE AVAILABILITY ACT
COPIC CEO Gerald Zarlengo, MD, explains the history behind the Health Care Availability Act and why this tort reform package has been so crucial to protecting patients and attracting health care providers.
3 PRESIDENT’S LETTER
CMS President Patrick Pevoto, MD, MBA, reflects on his year as president and how his experience relates to the Four Agreements.
22 2023 GILCHRIST SCHOLARS
The Gilchrist Scholarship Committee named two medical students, Neha Lamsal and Courtney Olson, as the recipients of the scholarship named for the former CMS CEO.
21 CMS EDUCATION FOUNDATION
NAMES RURAL TRACK SCHOLARS
The CMS Education Foundation named five recipients of the CMSEF Rural Track Scholarships to assist these students in their pursuit of practice in rural Colorado.
23 2023 RURAL TRACK SCHOLARS
The CMS Education Foundation named five recipients of the CMSEF Rural Track Scholarships to assist these students in their pursuit of practice in rural Colorado.
14 REFLECTIONS: I promise
15 REFLECTIONS:
The landscape within
16 COPIC COMMENT:
COPIC’s Online Resource Center – Tools and materials to support your medical practice
18 INTROSPECTIONS:
Facing fears and looking to the future
20 PARTNER IN MEDICINE SPOTLIGHT: Balancing HIPAA and OSHA compliance in health care practices

24 MEDICAL NEWS
Welcome, Virginia (Ginny) Castleberry, MBA, executive director for Denver Medical Society; NCMS, CMS receive AAMSE awards for excellence
25 MEDICAL NEWS
Young scientists recognized at state science fair
7351 Lowry Boulevard, Suite 110
720.859.1001 • fax 720.859.7509
• Denver, Colorado 80230-6902
• www.cms.org
Patrick Pevoto, MD, MBA President
Omar Mubarak, MD, MBA President-elect
Hap Young, MD Treasurer
Mark Johnson, MD, MPH Immediate Past President
Dean Holzkamp Chief Executive Officer
Brittany Carver, DO
Elizabeth Cruse, MD, MBA
Kamran Dastoury, MD
Amy Duckro, DO
Gabriela Heslop, MD
Enno F. Heuscher, MD, FAAFP, FACS
Dakota Hitchcock, MSS
Rachelle M. Klammer, MD
Marc Labovich, MD
Chris Linares, MD
Michael Moore, MD
Edward Norman, MD
Rhonda Parker, DO
Lynn Parry, MD
Leto Quarles, MD
Hap Young, MD
Dean Holzkamp
Chief Executive Officer
Dean_Holzkamp@cms.org
Kate Alfano Director of Communications and Marketing
Kate_Alfano@cms.org
Jennifer Armstrong
Program Manager, Government Affairs and Communications Jennifer_Armstrong@cms.org
Cindy Austin Director of Membership
Cindy_Austin@cms.org
Virginia "Ginny" Castleberry Executive Director Denver Medical Society Virginia_Castleberry@cms.org
Cecilia Comerford
Executive Director, Boulder County Medical Society Cecilia_Comerford@cms.org
Dorcia Dunn
Program Manager, Membership Dorcia_Dunn@cms.org
Crystal Goodman
Executive Director, Northern Colorado Medical Society Crystal_Goodman@cms.org
Mihal Sabar
Director of Accounting Mihal_Sabar@cms.org
Chet Seward Chief Strategy Officer Chet_Seward@cms.org
AMA DELGATION
David Downs, MD, FACP
Carolynn Francavilla, MD
Mark Johnson, MD, MPH
Jan Kief, MD
Rachelle Klammer, MD
A. "Lee" Morgan, MD
Tamaan Osbourne-Roberts, MD
Lynn Parry, MD
Brigitta J. Robinson, MD
Michael Volz, MD
AMA PAST PRESIDENT
Jeremy A. Lazarus, MD
Kim Vadas Director of Continuing Medical Education and Recognized Accreditor Programs Kim_Vadas@cms.org
Debra Will Director of Business Development Debra_Will@cms.org
Tim Yanetta IT/Membership Manager Tim_Yanetta@cms.org
of the Colorado Medical Society on a space-available basis. Dean Holzkamp, Executive Editor, and Kate Alfano, Managing Editor. Design by Scribner Creative.

My time as your CMS president is ending during the upcoming Annual Meeting in Vail. It has been an honor to serve you this past year and quite a learning experience! Our medical society has been in the midst of many changes, a sort of microcosm of our society today. Our politics continue to be quite divisive, and as servant leaders of Colorado physicians we don’t always represent the individual viewpoints and beliefs of each physician. Many decisions and actions I took could be construed as “right” or “wrong,” but I assure you I always made these decisions with the intention of improving the practice of medicine for physicians and our patients.
I received a letter from a Colorado physician leader that CMS – and particularly me – seemed to insinuate that physicians are their own worst enemies…sort of “victim shaming.” That has never been my intent, especially since things that I have espoused have been directed at me first. As I quoted Dr. Viktor Frankl in my presidential address last September:
“Forces beyond your control can take away everything you possess except for one thing...your freedom to choose how you will respond to the situation. You cannot control what happens to you in life, but you can always control what you will feel and do about what happens to you.”
My goal was to try and provide some tools that might be useful during the weathering of storms and tempests that come our way. We have all suffered from “moral injury” in the practice of medicine; it is hard, painful and at times there seems to be no end in sight. It does follow that finding ways to control our response to moral injury is time well spent, no matter what you use or who you work with in that endeavor.
Many of you have read "The Four Agreements: A Practical Guide to Personal Freedom" (A Toltec Wisdom Book), by Don Miguel Ruiz, MD, a neurosurgeon from Mexico. If you haven’t, I recommend that you do so. The premise of the book is that everything a person does in their lifetime is based on “agreements” they have made with themselves, with others, with God, with society and with life itself (from the source listed above). He outlines four such agreements:
1. Your speech should be impeccable.
2. Don’t take things personally.
3. Don’t make assumptions.
4. Always do your best.
I do not want to rewrite the book in this column. First, I would not do it justice. Second, it is not a long book (less than 170 pages) and can be read in one sitting. I wanted to relate the Four Agreements to my experiences the past year.
During my presidency, I have done my best to make sure my speech has been impeccable. Whether right or wrong, I strived to be transparent and honest. It has always been hard for me not to take things personally. I am a “people-pleaser” and I experience great discomfort when others interpret my speech or actions as offensive. I am the world’s worst at making assumptions as well. An action or decision made by someone, or some group, was being directed at me for nefarious reasons, when that conclusion was far from reality and/or the truth.
The Fourth Agreement is one that I guarantee I worked hard to execute... always do my best! What a realization it was that “my best” does not have to be perfect, does not have to please everyone, does not have to lead to a perfect outcome. I hope that my fellow Colorado physicians know that I was doing my best to represent them, and I will continue to do so when I turn the reins over to Omar Mubarak, MD, MBA, in September.
Thank you so much for giving me the opportunity to serve all of you! ■


Make plans to spend a fall weekend in the mountains with physicians from around the state; register for the signature event of the Colorado Medical Society – our Annual Meeting. There is something for everyone at this meeting:
• Social time, especially during the Welcome Reception and President’s Reception and Gala
• Great programming with engaging speakers on topics to improve the practice of medicine for physicians and patients
• The chance to present your research or hear the latest research
• A celebration of CMS leaders you have elected: Incoming President Omar Mubarak, MD, MBA; outgoing President Patrick Pevoto, MD; and your newly elected president-elect announced Sept. 1
This is your opportunity to refresh and renew your career, while meeting new contacts in a family-friendly setting.
12-5 p.m. Board of Directors lunch and meeting
This is the third quarterly meeting of the CMS Board of Directors in 2023, and will be offered as a hybrid meeting for in-person or virtual participation. All meetings are open to all CMS members to attend.
6-7:30 p.m. Welcome Reception with Exhibitors
Don’t miss our opening reception to pick
7-8 a.m. Breakfast
8 a.m. - 12 p.m.; 6-10 p.m. Children’s camp ages 2-12
Bring the kids to enjoy arts and crafts, snacks, an evening movie and other activities with professional childcare providers while you participate in the meeting. Advance registration required by Sept. 1.
8-9 a.m. Running on Empty: Physician Stress and Wellbeing

Michael H. Gendel, MD, presents an evidence-based look at physician workstress syndromes of burnout, teaching you methods for managing stress.
9-10 a.m. Failure: How Your Relationship to it Affects Your Patients and You
Aneesh Garg, DO, CAQ, will challenge you to embrace failure as a mechanism of growth rather than something to be feared and avoided.
1 0: 30-11:30 a.m. Recovery Plan for Physicians: Medicare Payment Reform
AMA President-elect Bruce Scott, MD, urges Congress to fix a broken Medicare
up your registration materials, meet and greet old and new friends, and visit with our exhibitors who keep the conference fees low and offer great products and services.
7:30-9:30 p.m. Movie screening: Theatre of Thought with Q&A following CMS has received special permission to screen a film by renowned documentarian Werner Herzog in which he investi -
gates the human brain, looking for clues as to why a hunk of tissue can produce profound thoughts and feelings while considering the philosophical, ethical and social implications of fast-advancing neural technology. Q&A to follow with NeuroRights Foundation Chairman Rafael Yuste, MD, PhD, and Fort Collins neurologist Sean Pazauskie, MD.
payment system that places enormous financial pressure on physicians and threatens the care we provide.
11:30 a.m. - 12:30 p.m. COMPAC Lunch
CMS's Political Action Committee hosts lunch on Saturday featuring state Sen. Kyle Mullica.
12:30-1 p.m. Exhibit break with dessert
1-2:30 p.m. Microaggressions, Allyship and Upstanding
CU Anschutz faculty Rita Lee, MD, presents an interactive session on microaggressions and strategies to be an effective ally. Attendees will also practice upstanding skills to intervene when we experience or witness microaggressions. This session is part three of the Foundations in Equity series, but can also be experienced without the previous two modules.
2:30-3:15 p.m. Exhibit break with raffle drawings
3:15-4:30 p.m. Virtual poster competition presentation
CMS members, especially medical students and residents, will present research in three categories: primary research, case report and evidencebased review. Posters will be projected and presented to a live audience, and awards will be given in various categories during the President's Gala. More information on pg. 6
4:30-6 p.m. Wellness break/free time
Take a break from a busy day to hike, bike or rest, and rejoin the fun for our evening activities.
6-6:45 p.m. President’s Reception
Enjoy a cocktail reception with friends old and new before the President’s Gala.
6:45-10 p.m. President’s Gala
The President’s Gala is the highlight of the weekend, featuring the passing of the gavel from outgoing CMS President Patrick Pevoto, MD, MBA, to incoming CMS President Omar Mubarak, MD, MBA. Dress is semi-formal. Enjoy a buffet dinner, dessert, music and dancing.



CMS will host guests at the Lodge at Vail, a classic icon of the Vail Valley that brings together the authentic character of a grand alpine lodge with a luxury resort. Many award-winning restaurants and high-end and unique shops are within walking distance. CMS negotiated a reduced resort fee of $20 per night (traditionally $40 per night) that grants those staying onsite access to wireless internet throughout the property, in-town transportation, outdoor hot tubs and a heated pool, fitness center, room service and more. CMS also negotiated a reduced valet parking fee of $25 per night (traditionally $50 per night). Pets are allowed for an additional fee.
To make your room reservation , call the reservations department at 855-953-0197 or 1-855-332-1601, select #1 to reach Colorado Resorts, and then option #4 for Vail. Please let the reservations agent know our group name (Colorado Medical Society 2023 Annual Meeting) and group code (BVLCMV23). Group lodging cut-off date: Aug. 31, 2023.


CMS members, especially residents and medical students, are invited to present your research in three categories: primary research, case report and evidence-based review. Awards will be given in various categories at the President’s Gala. Researchers will present their projects live on Saturday, 3:15-4 p.m. Find more information on entering the poster contest or signing up as a judge on the event webpage
The Colorado Medical Society thanks these sponsors and exhibitors for their support of the CMS Annual Meeting: COPIC, Panacea, PatientPop, Cruise Planners, Colorado Physician Health Program (CPHP), Center for Personalized Education for Professionals (CPEP), Dynavax Technologies, ODG and Huntington Bank.
Experienced and licensed childcare professionals from Care 4 Kids in Vail will be provide care for kids ages 2-12 at no cost to meeting attendees. Kids will enjoy arts and crafts, snacks and other activities Saturday morning and dinner and a movie during the President’s Gala. Advance registration is required through the Annual Meeting registration form by Sept. 1
The Colorado Medical Society is accredited by the Accreditation Council for Continuing Medical Education to provide continuing medical education for physicians. Learning objectives can be found on the event webpage. ■




According to the American Medical Association (AMA), physician burnout is an epidemic in the U.S. health care system.1
More than half of physicians report exhaustion, cynicism or decreased productivity. But five years ago, an article in STAT News First Opinion proposed a change in how we talk about, and think about, distress in health care workers, adding “moral injury” to the health care lexicon. It immediately went viral and is excerpted below:
The concept of burnout resonates poorly with physicians: it suggests a failure of resourcefulness and resilience, traits that most physicians have finely honed during decades of intense training and demanding work.
Many well-intentioned wellness initiatives over the past half century have focused on bolstering individual coping strategies, but:
Physicians are smart, tough, durable, resourceful people. If there was a way to MacGyver themselves out of this situation by working harder, smarter or differently, they would have done it already.
We believe that burnout is a symptom of something larger: our broken health care system. The increasingly complex web of providers’ highly conflicted allegiances — to patients, to self and to employers — and its attendant moral injury may be driving the health care ecosystem to a tipping point and causing the collapse of resilience.
The term “moral injury” has traditionally been used to describe soldiers’ responses to their actions in war. It represents “perpetrating, failing to prevent, bearing witness to, or learning about acts that transgress deeply held moral beliefs and expectations.”
The moral injury of health care is not the offense of killing another human in the context of war. It is being unable to provide high-quality care and healing in the context of our current health care system.2
Three years later, in the throes of a global pandemic, which brought the vulnerabilities of our health care systems into stark relief, Ed Yong summarized how many physicians describe their distress in The Atlantic in November 2021:


Health care workers aren’t quitting because they can’t handle their jobs. They’re quitting because they can’t handle being unable to do their jobs. Even before COVID-19, many of them struggled to bridge the gap between the noble ideals of their profession and the realities of its business. The pandemic simply pushed them past the limits of that compromise.3
Moral injury describes the gap between the covenants sworn by healing professionals and the realities of the increasingly corporatized environments in which they work. The concept encapsulates what scores of physicians had described when asked why they felt the term “burnout” did not accurately describe their experience: they were plenty resilient, but they were unable to get patients necessary care because of constraints outside of their control. Moral injury identified elements of distress that seemed distinct from burnout and which spoke to what physicians felt but couldn’t articulate, “…the frustration, anger, and disorientation associated with existential threats to our professional identity as corporate interests undermined the oaths we swore to put our patients’ needs first when we embarked on this path.”
Moral injury belongs alongside burnout, rather than displacing it. Both published and preliminary research has confirmed the initial hypothesis that burnout and moral injury are distinct experiences, which frequently occur together. In other words, distress breaks along not one but two fault lines. First are the operational demands of burnout: clumsy electronic medical records, understaffing, unreasonable scheduling, administrative overburden, and the like. Second are the relational ruptures of moral injury that arise from betrayal, regardless of whether such betrayal was intentional: the expectations of doing yet more with less; misaligned values (i.e., the words on the walls –mission, vision and value statements, for example – don’t match what’s happening in the halls); administrators lacking empathy for frontline challenges or curiosity about clinician perspectives make decisions that unwittingly compromise clinical care as a result. Breaking distress into its two component parts, to address each
with appropriately targeted therapies, will better address the crisis we face.
Researchers have provided countless solutions for physician burnout. Until recently, many of the proposed solutions acknowledged that systems change is difficult, complex and expensive, and advocated for support programs to help physicians better tolerate these difficult systems as individuals. Physician wellbeing programs focus on personal resilience – stress management; yoga; meditation or mindfulness; and optimizing the performance triad of sleep, nutrition and exercise. More recent recommendations have also begun calling for addressing systems issues like excessive documentation, electronic health records without intuitive user interfaces, inflexible scheduling systems, inability to coordinate care within or between systems, poor leadership and short staffing. Resources for tackling burnout are now readily available from the AMA, the Colorado
Medical Society, and physician specialty societies.

The evidence for addressing moral injury in health care is building. From research in military populations and interviews by one author (Wendy Dean, MD), standing up and speaking out against perceived betrayals are important steps to reducing the risk of moral injury. But individual interventions are not the only mainstay of relief. Instead, the key to reducing moral injury is identifying, acknowledging and addressing the regular betrayals – intentional and unintentional – inherent in our current health care systems.
Such betrayal can be as simple and as unintentional as communication that lacks acknowledgement and transparency. In a recent study, nearly one-third of physicians and half of nurses felt administration did not listen or respond to clinicians’ concerns, and in some of

Moral injury describes the gap between the covenants sworn by healing professionals and the realities of the increasingly corporatized environments in which they work.
lacked confidence that hospital management would resolve clinician-identified problems
the hospitals studied, more than half the clinicians felt ignored. Forty-two percent of physicians and 47 percent of nurses in the same study lacked confidence that hospital management would resolve clinician-identified problems in patient care. As any couples therapist knows, relationship repair after a betrayal is impossible if basic communication skills – listening and conveying that you have heard – are lacking. Organizations need to reestablish basics to restore trust with our health care workforce.
A recently completed Delphi survey asked those with academic or clinical competence in moral injury what characteristics health systems with a low likelihood of inflicting moral injury would share. Participants broadly agreed those systems would be wise, learn from their mistakes and challenges; vulnerable; trustworthy – doing what they say, when they say it; mentoring or succession planning with intent; just; and courageous – genuinely welcoming even difficult feedback from the workforce and itself pushing back on requirements that potentially harm the workforce.
First, by incorporating the new language of moral injury alongside “burnout” in our publications and physician education. As one therapist who works with physicians said, “Talking with my clients about moral injury rather than burnout took away their shame and guilt. It wasn’t only about them anymore; it was also about the systems they work in.” The right framing can begin healing.

Second, CMS should advocate for health care systems to treat physicians as respected partners to eliminate the causes of moral injury, training physicians
to become advocates for change, and speaking up to health care systems and the public, so that physicians do not have to walk this path alone.
Third, CMS should advocate for health care system changes to reduce administrative burdens, improve EHR interfaces, reduce unnecessarily restrictive referral and medication guidelines, and the multiple barriers that impede effective patient care and contribute to burnout.
Fourth, CMS should continue to provide and evaluate the effectiveness of programs like their Doc2Doc Wellbeing Consulting program and collaborations with the Colorado Physician Health Program.
The COVID-19 pandemic was not the start of physician distress, but it clarified what many previously suspected – burnout from operational stresses are not the only source of physician suffering. Until we accept that moral injury is a fact of working in human systems, and requires attention and repair, there will never be adequate solutions to physician distress. We have an opportunity to use lessons learned from the pandemic to rebuild stronger, more sustainable institutions for the improved health of physicians and our patients. Let’s not squander it. ■
Wendy Dean, MD, is a psychiatrist, author of “If I Betray These Words,” cohost of the podcast, “Moral Matters,” and co-founder of the Moral Injury of Healthcare. She previously worked for the U.S. Army in medical technology innovation.
Jeffrey Cain, MD, is a family physician, a clinical professor at the University of Colorado School of Medicine, and a past president of the American Academy of Family Physicians.
References:
1. https://www.ama-assn.org/ practice-management/ physician-health/ what-physician-burnout
2. Talbot, S, Dean, W. Physicians aren’t ‘burning out.’ They’re suffering from moral injury. STAT News First Opinion. July 26, 2018.
3. Yong, E. Why Healthcare Workers Are Quitting In Droves. The Atlantic. Nov. 16, 2021.
4. West CP, Dyrbye LN, Sinsky C, et al. Resilience and Burnout Among Physicians and the General US Working Population. JAMA Netw Open. 2020;3(7):e209385. doi:10.1001/ jamanetworkopen.2020.9385
5. Dean W. How the conversation about moral injury in health care is changing. STAT News First Opinion. June 7, 2023.
6. Rosen, A., Cahill, J.M. & Dugdale, L.S. Moral Injury in Health Care: Identification and Repair in the COVID-19 Era. J GEN INTERN MED 37, 3739–3743 (2022). https:// doi.org/10.1007/s11606-022-07761-5
7. Morris, D. Moral Injury and healthcare, Oct 2022: The evidence. Presented at: Erikson Institute Fall Conference on Moral Injury. October 2022.
8. Maslach C. and Leiter M.P. (2016) Burnout. In: Stress: Concepts, Cognition, Emotion, and Behavior, Academic Press, Cambridge, 351-357. https://doi.org/10.1016/ B978-0-12-800951-2.00044-3
9. https://www.ama-assn.org/ practice-management/ physician-health/measuring-andaddressing-physician-burnout
10. https://www.cms.org/articles/ category/physician-wellbeing
11. Dean W, Talbot S. If I Betray These Words: Moral Injury in Medicine and Why It’s So Hard for Clinicians to Put Patients First. Steerforth Press. 2023.
12. Aiken LH, Lasater KB, Sloane DM, et al. Physician and Nurse WellBeing and Preferred Interventions to Address Burnout in Hospital Practice: Factors Associated With Turnover, Outcomes, and Patient Safety. JAMA Health Forum. 2023;4(7):e231809. doi:10.1001/jamahealthforum. 2023.1809
At Colorado Physician Health Program (CPHP), we have evaluated over 6,000 Colorado physicians. Most of these physicians are married and we have noticed some vulnerabilities and areas of strength common in their relationships. I hope you will find these relatable.


First, our marriages (primary relationships) are incredibly important. It is not just the marriage itself. When professional satisfaction has been studied in physicians, hours, paperwork, administrative tasks and pay did not correlate to professional satisfaction as strongly as contentment with their marriage. In other words, being happy in your marriage makes you a more satisfied and, arguably, better doctor.
There are a number of challenges physicians face that are well known. We work long hours and our jobs are stressful. But there are other threats to our marriages that are often unaddressed or just accepted. I will briefly discuss a couple examples here.
The average physician will graduate medical school with over a quarter million dollars in debt. It is not unusual for us to see early physicians with twice that. Whereas many of our friends and colleagues outside of medicine have been working for a decade or more, by the time we finish our education we are in our 30s with no savings and tremendous educational debt. This creates obvious stress on our relationships. This can be compounded by making decisions often pressured by this debt including working in an isolated setting for loan repayment. Most of us have been educated and trained in relatively urban areas and have become used to what these population centers offer. Trying to start a marriage and family in a setting that may seem unfamiliar can further stress a new marriage.
Communication can be a pain point. Medicine is, by necessity, a hierarchy. We deal with life and death. We are taught communication with staff and colleagues should be direct and quick. This style serves its purpose in the hospital but not in the home. Open communication takes
time, a resource all young families lack. It is important to prioritize time for your spouse to feel heard and respected. This requires knowledge many of us don’t have. At CPHP we have found a short course of marital therapy can lead to exponential rewards.
I also want to share some good news. Historically, doctors have had a divorce rate higher than the general population. In the past several years, this has reversed to the point that our divorce rates are now significantly lower. While this trend is positive, we all could use
help now and then. I just want to remind you that CPHP is here for you. CPHP helps not only with health problems but relationship and situational challenges, including marriage difficulties! Give us a

In other words, being happy in your marriage makes you a more satisfied and, arguably, better doctor.
Editor's note: CMS member Carl E. Bartecchi, MD, has written a fascinating essay on one of the most prominent physicians of the Wild West. Michael Beshoar, MD, practiced medicine in Trinidad, Colo., in the latter half of the 19th century, and was in many ways ahead of his time. He was devoted to staying on the forefront of medical technology, improving community health, and educating both doctors and laypersons on best health practices. He also almost certainly crossed paths with some of the most famous figures of the time, such as Doc Holliday and Wyatt Earp. Please enjoy the excerpt below from Dr. Bartecchi’s essay, and visit cms.org to read it in full.
Who would have thought that from Trinidad, Colo., one of the most distinguished and accomplished physicians and entrepreneurs would arise in the latter half of the 19th century? Michael Beshoar, MD, was probably one of the most unrecognized American physicians of that era.
A book; a biography by his grandson Barron Beshoar, “Hippocrates in a Red Vest;” Michael’s own book, “All About Trinidad and Las Animas County Colorado;” and more than eight large boxes (Beshoar Family Papers) donated to the Western History Collection of the Denver

Public Library tell the story of the most prominent physician of the old, Wild West.

Born in a small Pennsylvania town in 1833, Michael went on to graduate from the University of Michigan Medical School in 1853. In 1861, Beshoar, with his friends and neighbors, joined the Confederate Army where he served as a surgeon in the medical corps. He was captured by the Union Army in 1863 and ended up as a prisoner of war. However, after signing an Oath of Amnesty, he was allowed to join the Union Army where he served as an assistant surgeon until the end of the Civil War.
Following his medical career, Beshoar pursued private practice ventures, eventually ending up in Denver, whose population in 1867 was under 4,000. His success in Denver was hindered by the “anti-southern” bias of that community. That encouraged him to look farther to the south, to the town of Pueblo, which was more friendly to southerners and had only one doctor for its population of 400 at that time. Besides initiating a medical practice in Pueblo, he opened the first drug store between Denver and Santa Fe, N.M. In that same year, 1867, he also found his way south to Trinidad, Colo., a town of about 400 inhabitants that also favored southerners. He arrived there just seven years after the first settlers. He started a medical practice there and opened up a pharmacy. In Trinidad, he moved into a boarding house run by the sister of the famous [chief of the Oglala Sioux], Red Cloud. She was also the aunt of the [indigenous American] known as Crazy Horse.
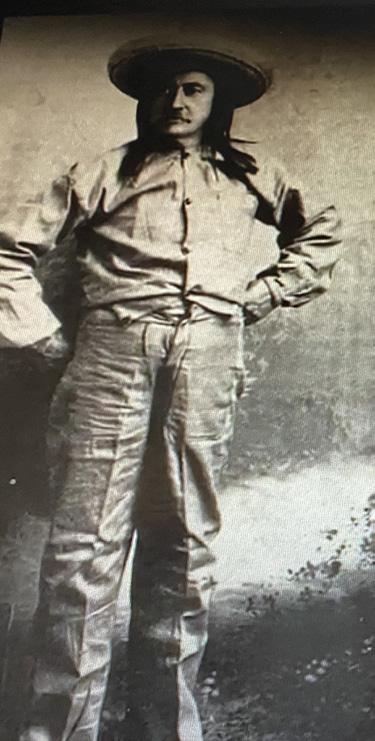
Trinidad, with its gambling halls and popular saloons lent itself to plenty of
drunken brawls between the Americans, Mexicans and the [indigenous Americans] that frequented the town and lived in the surrounding area. This allowed Beshoar the opportunity to utilize the surgical and orthopedic skills that he had acquired during his training and his experience in the Civil War, providing his services to all sides of these conflicts. He was often the only physician available and capable of treating the wounded from these frequent conflicts and the traumatic injuries common in the agricultural, mining and industrial settings of the region. His successful “care of wounds” brought him wide acclaim. He was also one of the only physicians who provided medical care for the local Native American population during his early days in Trinidad, for they were often unable to pay for their care and medications.
A perusal of copies of his billing records indicate a wide range of medical services that he provided. These services included “minor and more important surgical operations, ordinary and difficult obstetric cases and ordinary and acute cases, often including medicines.” He also provided “tooth extractions, bloodletting and cupping, and local and distant house calls.” He proudly noted that his charges were at least one-third lower than those adopted by the Colorado Medical Association.
Read the full version on cms.org for more on Dr. Beshoar: Among his many other accomplishments, he launched a monthly magazine, The Medical Educator; founded the Pueblo Chieftain newspaper, still in print today; was concerned with the health of the community and endorsed school lunches and vaccines; and was county coroner, county clerk and a Colorado state legislator. ■
Your elected delegation to the American Medical Association and Colorado medical student leaders traveled to Chicago in June to represent all physicians in our state at the AMA Annual Meeting. The meeting brings together hundreds of physicians from around the country to consider a wide array of proposals to help fulfill the AMA’s mission of promoting medicine and improving public health.
TOP COLORADO HIGHLIGHTS FROM THE MEETING:
• Tamaan K. Osbourne-Roberts, MD, MBA, FAAFP, DiplABLM, was reelected to the AMA Council on Science & Public Health.
• Jan Kief, MD, was reappointed to the AMA Council on Long Range Planning & Development.

Matthew Wynia, MD, MPH, received the American Medical Association Foundation Award for Leadership in Medical Ethics and Professionalism, which honors people dedicated to the principles of medical ethics and the highest standards of medical practice and who have made an outstanding contribution through active service in medical ethics activities. The award is in partnership with the American Medical Association.
Wynia directs the University of Colorado Center for Bioethics and Humanities. The center runs an annual Aspen Ethical Leadership Program and major commu -
• Matthew Wynia, MD, MPH, received an AMA Foundation 2023 Excellence in Medicine Award; more information below.
The AMA continues to advocate for Medicare physician payment reform, as part of their AMA Recovery Plan for America’s Physicians. Outgoing AMA President Jack Resneck Jr., MD, said “This cannot wait; we are past the breaking point. Our patients are counting on us to deliver the message that access to health care is jeopardized by Medicare’s payment system. Being mad isn’t enough. We will develop a campaign—targeted and grassroots—that will drive home our message.”
Additionally, the AMA installed a new president, Jesse M. Ehrenfeld, MD, MPH, who is a practicing anesthesiologist, senior associate dean, and tenured
nity engagement programs, including the Holocaust Genocide Contemporary Bioethics program and the “Hard Call” podcast series. Earlier in his career, Dr. Wynia spent 18 years at the AMA, where he led the Institute for Ethics and the Center for Patient Safety and was director of patient and physician engagement. He also led the project on the history of African Americans and the medical profession that, in 2008, prompted the AMA’s public apology for a legacy of racial discrimination and exclusion in organized medicine.
Wynia has delivered more than two dozen named lectures and visiting professorships and he is an author of more than 230 academic publications. He is a fellow of The Hastings Center, past president of the American Society for Bioethics and Humanities and past chair of the Ethics Forum of the American Public Health
professor of anesthesiology at the Medical College of Wisconsin. He is the first openly gay person to hold the office of AMA president. And Bruce A. Scott, MD, an otolaryngologist from Kentucky, was elected president-elect of the AMA. Scott will be a special guest at the CMS Annual Meeting in Vail in September.
THANK YOU TO THE COLORADO DELEGATION TO THE AMA:
David Downs, MD, FACP
Carolynn Francavilla, MD
Mark Johnson, MD, MPH
Jan Kief, MD
Rachelle Klammer, MD
A. "Lee" Morgan, MD
Tamaan K. Osbourne-Roberts, MD, MBA, FAAFP, DiplABLM
Lynn Parry MSc, MD
Brigitta Robinson, MD, FACS
Michael Volz, MD ■
Association and the Ethics Committee of the Society for General Internal Medicine.
In his honor, the AMAF awarded a $2,500 grant to the University of Colorado Center for Bioethics and Humanities.

A woman lies in the ED bed: she is cachectic, contracted, barely cognizant. A series of strokes, renal failure and heart attacks have stolen her livelihood. The resident and I are here to discuss code status with the family, in no small part because the futility and agony of cracking this woman’s ribs make our stomachs turn. Her granddaughter, the medical power of attorney, recently transitioned the patient to hospice, which is meant to take effect in two days. With this in mind, we explain the trauma that would result from resuscitative efforts, and we advise a change from Full Code to DNR/DNI. From there, the conversation spirals.
What we do not know is that this transition to hospice care is a direct consequence of her insurance benefits running out: the granddaughter has been robbed of the choice of life-sustaining dialysis. What we do not fully grasp is how her justified distrust – she is an African American woman who has already received subpar care – splits a chasm between us. And most of all, we do not see until far too late the weight of her children’s excruciating hope on her hunched shoulders. I walk out of the room feeling that I failed the patient – who will likely die during this hospitalization and will now have to undergo a full code – and that I failed the family in my communication. One of the
great-granddaughters says, “This is why I hate doctors.” I do not blame her.

Later, I circle back and apologize for not giving them the quality of care they deserved. The family graciously accepts, and the great-granddaughter says, “Thank you. I just want you to do better next time.” I promise them I will.

This was a moment that exemplified humanism in medicine: It included the vigilant practice of empathy, careful listening and recognition of the power of forgiveness – critical intangibles that push us to become better stewards for our patients and for each other. I see it in my colleagues who settle personal differences with respect and understanding. I see it in my residents who own their guilt
and pain after patient deaths. I see it in my attendings who acknowledge their shortcomings in treating patients who are racial minorities or speak a different language (somehow, the interpreter line for Chuukese is never available). And I see it in my patients, who greet me with a smile each day despite being wrapped in gauze from head to toe. We are all doing the best we can with what we have. Some days, that will be enough. Other days, we will lean on our ingenuity and self-reflection to figure out how we can be enough in the future. ■
Later, I circle back and apologize for not giving them the quality of care they deserved. The family graciously accepts, and the great-granddaughter says, “Thank you. I just want you to do better next time.” I promise them I will.
 Amira Otmane
Amira Otmane

“The most peaceful people that I know and the wisest people that I know are the ones who have created enough internal space to allow all parts of themselves to coexist despite the contradictions, so they have room for their creativity but also room for their fear, they have room for their dignity, and they also have room for their shame…they create this big huge auditorium of a landscape inside themselves.”
This quote from Elizbeth Gilbert, author of “Eat, Pray, Love,” embodies the beauty of being human, and each time I think about it, I think of how leaning in and making space can allow us to be better – for ourselves, our colleagues and our patients.
During my clinical year, I had the privilege of working with one of the most compassionate physicians I have ever met. She was beloved by all; everyone walking down the halls of the hospital would stop for a quick chat with her. Her patients probably loved her the most. They had developed deep connections with her, discussing their medical problems while also updating her on other parts of their lives. She was always such a bright light in every one of her interactions.
I remember one day, right before we were set to begin a scheduled procedure, she received a phone call that was quite distressing. She disappeared for a moment and when she returned it was clear that she was upset – her cheeks were flushed and her eyes were puffy. But she took a deep breath, stepped into the room and carried on with the procedure. After we were done, she followed her patient out of the procedure room, made sure she was recovering well, finished her notes and asked me if I wanted to take a walk with her before our next case. We proceeded to discuss a little bit of the difficult news she received this morning and how it would impact her life.
What struck me about this particular instance was my preceptor’s ability to honor her own humanity. Though she clearly embodies and practices humanism in medicine when it comes to her practice of patient care, it was her willingness to extend this to herself that served as a powerful reminder.
We often forget that humanism does, and should, extend to ourselves as physicians. Seeing her take just 10 mins to address her phone call, calm herself down, and get in the headspace to treat her patient was incredible. She didn’t silence herself, didn’t take out her emotions on her staff or colleagues, or completely disappear
and not finish the rest of her work. Instead, she chose to hold space for all her emotions – her concern about her phone call, her compassion towards her patient waiting for her, her love of her craft, and her fears about what was to come given the news she received in the morning. Her willingness to debrief with me and not ignore how she reacted earlier also allowed me to see her as a human and was a testament to her own humility.
How we show up for our patients and for ourselves is the best way we can nurture our humanity. In expanding our own auditorium to make space for all our emotions, we invite our patients to do the same. When our patients step into our office, they should be able to discuss all their fears, hopes, goals, and frustrations, and we need to take this all in and validate them in doing so. But how do we expect to understand the range of emotions our patients feel if we do not let ourselves have the same luxury? How can we empathize with patients about their nuanced feelings if we don’t explore them within ourselves? After all, with our growing diversity and multicultural communities, we might not be able to understand one another’s exact experiences, but we can always be sure of our ability to connect with the same emotions that make us all human. ■

A key aspect of COPIC’s commitment to patient safety and risk management is developing resources that inform and support physicians and the health care community. We continue to invest in a library of materials that are developed based on feedback from our insureds, experiences from occurrences and claims, and medical and patient safety research. This library can be accessed via a Resource Center on our website at callcopic.com/resource-center Some examples of the available materials include:
• A list of “latest updates” that highlight our newest resources including upcoming education seminars and current articles on risk topics.
• Sample informed refusal or other procedure-specific consent forms that you can easily edit and use at your practice.
• An archive of past Copiscope newsletters that provide guidance on key medical liability trends and risks.
In addition, there are specific resources to help physicians navigate the ever-changing legal, regulatory, and medical environments in Colorado.

• Opioid Continuing Education Requirements (by State) for Physicians
• CME Opioid Education Resource List —Information on national organizations that offer CME education to meet newly enacted DEA requirements. Please note: a) many of the CME courses provided by these organizations are free; and b) these courses are from organizations outside of COPIC and do not qualify for COPIC points.
Medical providers who prescribe opioids are required to complete certain training requirements on both a state and federal level. To assist with understanding and meeting these requirements, COPIC has developed an Opioid Education Resources atcallcopic. com/resource-center/guidelines-tools/ opioid-resources with the following materials:
• Links to COPIC On-Demand Courses that include:
• COPIC’S Three-Hour Opioids Review (Education for DEA Training Requirements)
• Opioid Management: A Practical Approach to a National Crisis (Opioids I)
• Opioid Crisis: Strategies for Reducing the Burden (Opioids II)
The Colorado Candor Act is a bipartisan effort that establishes a voluntary framework for health care providers and facilities to offer compassionate, honest, timely, and thorough responses to patients who experience an adverse health care incident. It went into effect in 2019 and is designed to benefit patients, their families, clinicians, and health care systems by formalizing a non-adversarial process where there can be open communication about what happened, why it happened, and what can be done to prevent this in the future. This section includes resources that provide details about the Act, the Candor process, as well as sample templates of required forms.
FOR THOSE INSURED BY COPIC: We will walk you through the Candor process and answer any questions you may have. As with all incidents, COPIC insureds should call a COPIC occurrence specialist nurse during business hours, 8 a.m.-5 p.m. (Mountain Time), Monday through Friday,

by calling (720) 858-6395. The occurrence specialist nurse will evaluate the incident with our internal team to determine if it is appropriate to utilize the Colorado Candor Act.
Many physician groups discuss adverse events, patient complaints, challenging cases, or concerns about a colleague, but aren’t aware that these communications can be protected under the peer review privilege if a practice has peer review policies and procedures in place. To support this, COPIC’s Legal Department has developed the below state-specific peer review toolkits that contain:
COPIC promotes peer (or "professional") review to improve medicine in the communities we serve. We have been a strong advocate of using this process as a tool for improving patient safety.
It's important for making sure a provider is qualified and safe to practice.
It's a way to learn from case reviews to avoid preventable harm for patients going forward.
Most physicians are aware of confidential peer review in the hospital setting but aren’t aware that their state law also protects peer review communications in the clinic and physician practice setting.
• A Colorado-specific article explaining the legal protections for peer review and its practical application for physician practices and clinics
• A Peer Review Checklis t of what’s required (consistent with state and federal peer review laws)
• A Confidentiality Agreement for peer review participants
• Peer Review Policy templates that a practice can tailor to meet its needs
PLEASE NOTE: COPIC advises practices to have their own attorney review these materials. ■
https://coloradopainsociety.org/annual-meeting-2023-2/

Critical reflective writing holds a prominent place in the Medical Humanities curriculum at Rocky Vista University College of Osteopathic Medicine. Beginning in the first semester of Medical Ethics, students engage in critical reflection to explore their own assumptions and biases and how their values impact their practice. This submission is selected and edited by Nicole Michels, PhD, chair of the Department of Medical Humanities, and Alexis Horst, MA, writing center instructor.
Scarlett Kass is a third-year medical student at Rocky Vista University School of Osteopathic Medicine in Colorado. She grew up in Aiken, S.C., and later got her B.S in exercise science at the University of South Carolina. Prior to medical school, she attended Rocky Vista for her M.S. in biomedical science. She is interested in pursuing a career as an emergency medicine and sports medicine physician.

There is nothing more daunting than sitting in an MRI machine with a cage around your head at one of the top medical facilities in the world with your mind racing about what could be going on –the unknown. Those 45 minutes were the most trapped I have felt in my entire life. I had no option but to sit there as still as possible with the loud machine whirring in my ears thinking about my inevitable fate. Why me? Why now?
In March 2020, I, like so many others, contracted COVID-19. I was in the middle of my master’s program, so I refused to be taken down by a viral illness. I had a moderate case of the virus, but my recovery took a little longer and also had some unexpected turns.
At that time there was no diagnostic test or treatment for COVID-19. I was treated using supportive care that managed my symptoms at the time. No one knew what to expect during or afterwards. What was
normal? What was abnormal? What are red flags that I need to be aware of and looking out for?
I remember my first episode of neurologic symptoms. I got the worst headache of my life and then proceeded to have leftside motor and sensory weakness with changes in vision, nausea and slurred speech. My first thought was that I was having a stroke, but I didn’t know what to do because I could not move. I felt alone, helpless and terrified in that moment. Is this how I go? Who is going to find me? I eventually lost consciousness in what I had accepted could be the end for me. I woke up hours later, my dog whining next to me, with resolution of symptoms.
Over the next few months, I had repeat episodes. I saw my primary care physician and she suspected I had multiple sclerosis (MS), so she ordered the full workup. The brain scan showed “nonspecific brain inflammation,” and I didn’t know what that

meant, so I called my father, who is an internal medicine physician, and told him what was going on.
He advised me to see a neurologist as soon as possible. I called every office in Denver, and because of COVID-19, I couldn’t get in anywhere for six to nine months. In that moment, I felt unheard and unseen, like no one was listening to me or could help me. I never want patients to feel like I did when I called begging to be seen.
I have never been more scared in my life – paranoid of getting an attack and wondering how long it would last, how much pain I would be in, the lasting side effects, and if it could be potentially fatal. I wanted to know what was wrong with me so that it could be treated because I wanted to get back to my life. On the other hand, I was frozen with fear with what that diagnosis was and what it entailed.
My father had a connection at Mayo Clinic Florida, and I was scheduled to see the head of neurology within a month. Once at Mayo Clinic, the workup began. There was an eerie feeling in the waiting room. It was full of people from all across the world with severe or rare medical conditions, but I could see the hope in their eyes because they were at Mayo Clinic seeing the best of the best – if they had a chance, it was here.
After the MRI results came back, I was diagnosed with hemiplegic migraines, a rare disorder in which individuals experience a migraine headache along with weakness on one side of the body.
What does that mean? How is this going to affect my quality of life? Can my body and mind still handle medical school? There was no cure, no definitive treatment, and no real consistent data on how it affects people. There were some off-label medications that I could try, but there was no guarantee because every case was different.
This continues to be a part of my everyday life, and I have reflected a lot over the past few years. I have learned so many things both personally and professionally that I choose to use to shape me to be a better human and a better health care provider in the future.
I have learned the value of trusting your patient whether that be their story, symptoms or especially their instinct because it is usually right. They know their body best; listen to them, and we may be surprised at how integral patients can be to their diagnosis and care. Nothing compares to not feeling heard, and I never want my patients to feel the way I did.




Something I didn’t anticipate was the level of personal growth that this diagnosis would bring me. I have learned far more than I can write in this reflection and continue to learn and grow each day as life gives me new challenges. I have gained a new level of resilience. It took some creativity, adjustment and flexibility but I am doing it.
Being flexible has been a major adjustment. I have to really listen to my body, and there are many factors that I have to consider when choosing how to spend my time and energy. I also can’t anticipate when I will feel sick or have a bad day, and I have to adjust to that in real time, which has forced me to practice healthy life balance. I have no other choice other than to make sure that I am well taken care of mentally, emotionally, spiritually, physically and academically if I am going to make it. I check in with myself throughout the day, really tune in to what my body needs, and then do that.
Finally, I have learned and better appreciate that life is short. I know it is cliché but it’s true. We never know what is going to happen, and life is chaotic and so out of our control. But we can choose to control our response. I choose to still pursue my personal and professional aspirations and embrace all the good and the bad in the hopes that it will continue to shape me into a better human as well as a more well-rounded health care provider. ■

Abyde
Compliance requirements can sometimes feel like a dance routine, and for health care practices, the choreography involves the overlapping steps of HIPAA and OSHA. Striking the right balance between protecting patient privacy and ensuring employee safety can be challenging but crucial. Here are some practical steps health care practices can take to navigate the convergence of HIPAA and OSHA compliance without drama or theatrics.
UNDERSTANDING HIPAA AND OSHA:
1. HIPAA COMPLIANCE:
HIPAA stands as the guardian of patient privacy and data security. It sets the standards for electronic transactions, privacy rules, and security measures. Health care providers, health plans, and clearinghouses are obligated to implement safeguards to protect sensitive health information.
2. OSHA COMPLIANCE: OSHA is responsible for maintaining a safe and healthy working environment for employees across all industries, including health care. It focuses on identifying workplace hazards, providing safety training, and ensuring proper record-keeping for occupational injuries and illnesses.
MANAGING THE OVERLAP:
1. ASSESS RISKS: Begin by conducting a thorough risk assessment considering HIPAA and OSHA requirements. Identify potential areas where these compliance realms intersect, such as situations where employee safety might come into contact with patient information.
2. DEVELOP POLICIES AND PROCEDURES: Craft policies and procedures that encompass both HIPAA and OSHA compliance.
Ensure they address privacy, security, patient safety, employee training and hazard prevention. Strive for clear and concise guidelines that are easily understood by staff.
3. EMPLOYEE EDUCATION AND TRAINING:
Educate and train your employees on both HIPAA and OSHA regulations. Empower them with the knowledge to protect patient privacy and maintain a safe workplace. Integrate training sessions that highlight the areas of overlap, emphasizing the importance of handling sensitive data in a secure manner.
4. SAFEGUARDING PATIENT PRIVACY: Implement measures to protect patient privacy while maintaining a safe work environment. Establish designated areas for confidential discussions and restrict access to authorized personnel only. Remember, the aim is to achieve a balance that safeguards patient information without compromising employee safety.
5. WORKPLACE SAFETY:
Regularly assess the physical environment for potential hazards and implement protocols to address them promptly. Focus on proper storage and disposal of hazardous materials, ergonomics and infection control practices. Encourage a safety culture that promotes vigilance and preventative measures.
6. INCIDENT REPORTING AND DOCUMENTATION:
Establish a streamlined process for reporting incidents that may involve both patient information and employee safety. Emphasize the importance of accurate documentation while maintaining patient confidentiality. Clear reporting procedures help identify areas for improvement and drive proactive safety measures.
7. IT SECURITY:
Maintain robust IT security measures to protect electronic patient health records from unauthorized access or breaches. Stay vigilant with software updates, conduct regular risk assessments, and educate employees on best practices for data security and privacy.
8. COMPLIANCE AUDITS AND MONITORING:
Regularly conduct compliance audits to ensure adherence to both HIPAA and OSHA requirements. Monitor compliance, review incident reports and identify areas that need improvement. Assign designated staff members to oversee compliance efforts and keep the focus on continuous improvement.
Finding a rhythm between HIPAA and OSHA compliance is essential for health care practices striving to protect patient privacy while maintaining a safe working environment. By assessing risks, developing comprehensive policies, and providing education and training, health care organizations can achieve the delicate balance required.
Compliance doesn’t need to be a stressful rehearsal for things to go wrong. It's a practical endeavor that protects both patients and employees alike. At Abyde, we strive for a harmonious dance where patient privacy and workplace safety are the show’s stars. Our revolutionary software bundles HIPAA and OSHA compliance for health care, making the balancing act of compliance easy for practices.
For more information, visit abyde.com ■


The Gilchrist Scholarship Committee has named two scholars, Neha Lamsal and Courtney Olson, for 2023. In recognition of their extraordinary achievements, both scholars received monetary awards to aid them in their medical education. Each of this year’s recipients showed exceptional dedication to leadership and advocacy in organized medicine.
NEHA LAMSAL is a thirdyear medical student at Rocky Vista University College of Osteopathic Medicine. She was the Community Outreach chair for the RVU CMS chapter, and in this position was able to bolster their partnership with the Well Clinic – a free clinic working with diabetic foot care and other patient needs. Through this partnership, medical students volunteered under the supervision of physicians, providing direct care and diabetes education to patients. These students were able to help improve access to care for this population, as well as provide information that would help patients advocate for themselves in the future.
Neha wrote in her application, “I consider the partnership between RVU CMS and the Well Clinic to be my most meaningful accomplishment in my tenure as Community Outreach chair. This experience brought me into contact with physicians who were passionate about promoting health care for vulnerable populations and were looking for partners in that effort. I see CMS as a partner in realizing these visions are shared by many physicians.”
COURTNEY OLSON is a fourth-year medical student at the University of Colorado School of Medicine. She has held leadership positions with both the CMS Medical Student Component (representing both UCSOM and RVU) and with the American Medical Association. In these positions, she learned how to mobilize and organize with her medical school peers to ensure their voices are heard at the legislative level. Courtney has co-authored a resolution to integrate Holocaust Remembrance Day into medical education, as well as provided testimony at legislative
sessions. As a physician, Courtney would like to use her voice to advocate for marginalized communities in medical education and in medicine and intends to stay involved with organized medicine in order to make her voice heard.
“Throughout my career, I want to practice being a physician-citizen through leadership in state and national societies. I am incredibly grateful for the opportunities I have had in organized medicine thus far and am committed to continue advocating for equitable and accessible healthcare.”

The Alfred D. Gilchrist Student Leader Scholarship Foundation was established in 2020 to honor former CMS CEO Alfred Gilchrist’s 40-year career of physician advocacy. It is open to third- and fourth-year medical students who have demonstrated a significant leadership contribution to organized medicine. Preference is given to students who are active with CMS or a CMS component medical society. Contribute to the Alfred D. Gilchrist Student Leader Scholarship at cms.org/contribute ■
TO ALL COLORADO PHYSICIANS WHO HAVE INVESTED IN MEMBERSHIP IN THE COLORADO MEDICAL SOCIETY. WE COULDN’T DO OUR WORK ON YOUR BEHALF WITHOUT YOUR SUPPORT.
DUES NOTICES FOR 2024 MEMBERSHIP WILL GO OUT IN SEPTEMBER. We urge individual physicians and groups to return these invoices as soon as possible to prevent any disruption in your membership benefits.

SCHOLARSHIP HELPS FIRST-YEAR MEDICAL STUDENTS PURSUE RURAL MEDICINE




 Erin Arcand, contributing writer
Erin Arcand, contributing writer
Congratulations to first-year students from the University of Colorado School of Medicine and Rocky Vista University College of Osteopathic Medicine who were each awarded $4,000 scholarships from the Colorado Medical Society Education Foundation (CMS EF). Awardees are Aidan Sokup, Cooper Sclar and Brandon Middlemist. Mariah Werner is the recipient of the Maribeth and Jack Berry Scholarship and Timothy Ghan is the recipient of the William Gerald Rainer Scholarship.
MARIAH WERNER is in the rural training track at CUSOM, and intends to practice in rural northeastern Colorado, where she grew up on a ranch. Mariah will be completing a rural clerkship in Sterling, Colo., this upcoming school year, and is looking forward to learning in her own community and other rural areas. Mariah also hopes to bring education and mentoring opportunities to rural youth who aspire to careers in health care. She wrote in her application, “I believe that providing information and mentorship to students in rural areas about healthcare careers is vital to securing future generations of providers who will stay in the community.”
AIDAN SOKUP is also in the rural training track at CUSOM. He grew up on the Western Slope of Colorado, and stated in his application essay “my connection to the area is deep, inseverable, and intertwined with my passion for rural medicine – I feel the duty to give back to the communities of western Colorado.–” Aidan feels strongly about mentorship for rural youth as well. He says, “Since getting accepted to medical
school, I’ve made it my mission to not only become a great physician, but also to become a role model and mentor for rural students who want to become health care professionals. As someone with such a similar background, I hope to serve as proof that they can pursue their dreams and serve their community, and this further deepens my desire to return to practice in rural Colorado.”
COOPER SCLAR is in the rural and wilderness medicine track at RVU, and grew up in a small mountain town, where he observed his parents – both physician assistants –provide medical care to the community. In Cooper’s words, “Colorado rural care is adaptive and personal. In these settings, patients are proud of where they are from.” Being a part of the community he serves, as well as building deep and meaningful relationships with his patients is something Cooper is passionate about, and what he believes will enable him to provide the highest level of care for those in the community.
BRANDON MIDDLEMIST is in the rural track at CUSOM. His upbringing included working on his family’s farm, which taught him how to problem-solve using available supplies in creative solutions; a skill that has served him well in helping patients with limited resources. Brandon wrote in his application essay, “I am drawn to rural medicine due to its global nature: from bringing newborns into the world, to treating their grandparents. Just as my doctor growing up cared for multiple generations of my family, I hope to offer continuity of care to my patients, form -
ing relationships, and getting to know them beyond a case in front of me.” He also believes that rural family physicians have the opportunity to help improve the health of the whole community by addressing the unique medical issues of that specific population.
TIMOTHY GHAN is in the rural track at CUSOM and grew up in rural western Colorado. Before beginning medical school, he returned to his hometown and spent time working both in behavioral health and hospital settings. Timothy said in his application essay, “My family has personally struggled with the healthcare deficit that is present in many of the rural areas across Colorado, and my time during my gap year began to show me the impact I could have in counteracting these disparities. For this reason, after medical school I hope to return to rural Colorado to continue to work against the health care disparities that are present in much of our state.”
CMS EF, a 501(c)(3) private foundation, has a mission to render financial support to select first-year medical students at UCSOM and RVU. Student scholarships are based on criteria such as the student’s financial status, academic achievement and desire to practice in rural or underserved areas upon graduation.
The CMS EF Board is thankful for the generous financial contributions and support from CMS members and others who make these education scholarships possible. You can contribute to the CMS Education Foundation at cms.org/contribute ■
Virginia (Ginny) Castleberry, MBA, has been hired as the new Denver Medical Society (DMS) executive director. Ginny brings an entrepreneurial spirit to all she does, whether it’s attracting new clients and partners, or starting a new program. She believes it comes down to listening well, moving boldly, then learning from feedback to continuously improve. She has a BS in Finance and an MBA with a specialization in Entrepreneurship from CU Denver.
Ginny has more than 20 years of experience working in for-profit and nonprofit
organizations, and spent 16 years with medical professional liability provider, COPIC. The experience gave her a deeper understanding of the challenges that face health care professionals and health care organizations today. Ginny has worked for a variety of companies, from Fortune 10 to a small but mighty health education nonprofit, from a startup whiskey distillery to a school of theology. These diverse experiences have allowed her to learn the importance of staying innovative, fostering partnerships across communities, and focusing on the needs of clients.
Ginny is excited to get out and meet the members of the Denver Medical Society and the greater health care community in Colorado. She will be reaching out to members and partners to listen to their ideas, challenges, and concerns. ■
The Northern Colorado Medical Society was awarded an AAMSE 2023 Profiles in Excellence Award for Membership Engagement . NCMS Executive Director Crystal Goodman attended the AAMSE Annual Meeting in Phoenix July 19-21 and accepted the award. NCMS was recognized for their partnerships with community organizations, local events, their stethoSCOPE podcast, e-newsletter
campaigns, and strategic plan to increase membership engagement.
The Colorado Medical Society was awarded an AAMSE 2023 Profiles in Excellence Award for Excellence in Diversity, Equity and Inclusion . BCMS Executive Director Cecilia Comerford accepted the award on behalf of CMS at the AAMSE Annual Meeting. CMS was

recognized for building a foundation for DEI at CMS, which began with Colorado physicians volunteering to serve on the CMS DEI Committee. Led by Chair Phyllis Bergeron, MD, the committee then proposed a five-year strategy focused on communication, education and organizational change; and coordinated education for the CMS Board of Directors, CMS staff and all CMS members. ■





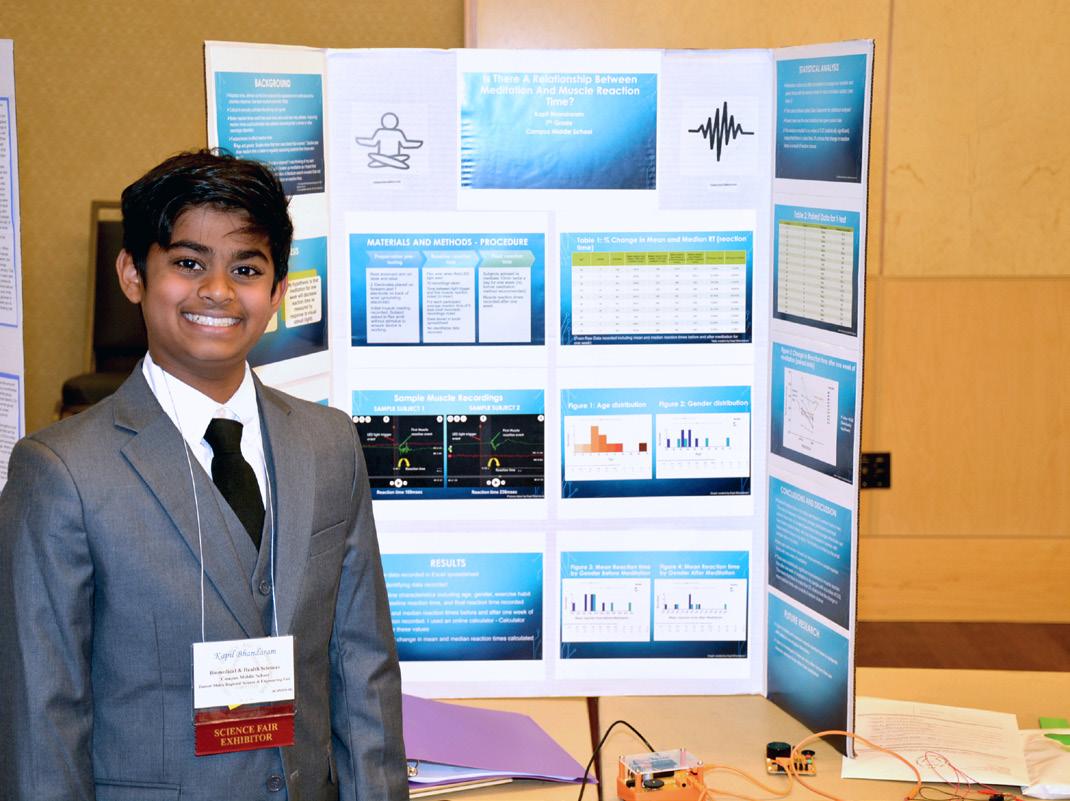
Aditi Avinash and Kapil Bhandaram won the Colorado Medical Society Awards for Excellence at the 2023 Colorado State Science and Engineering Fair held on April 13, 2023, at Colorado State University in Fort Collins.
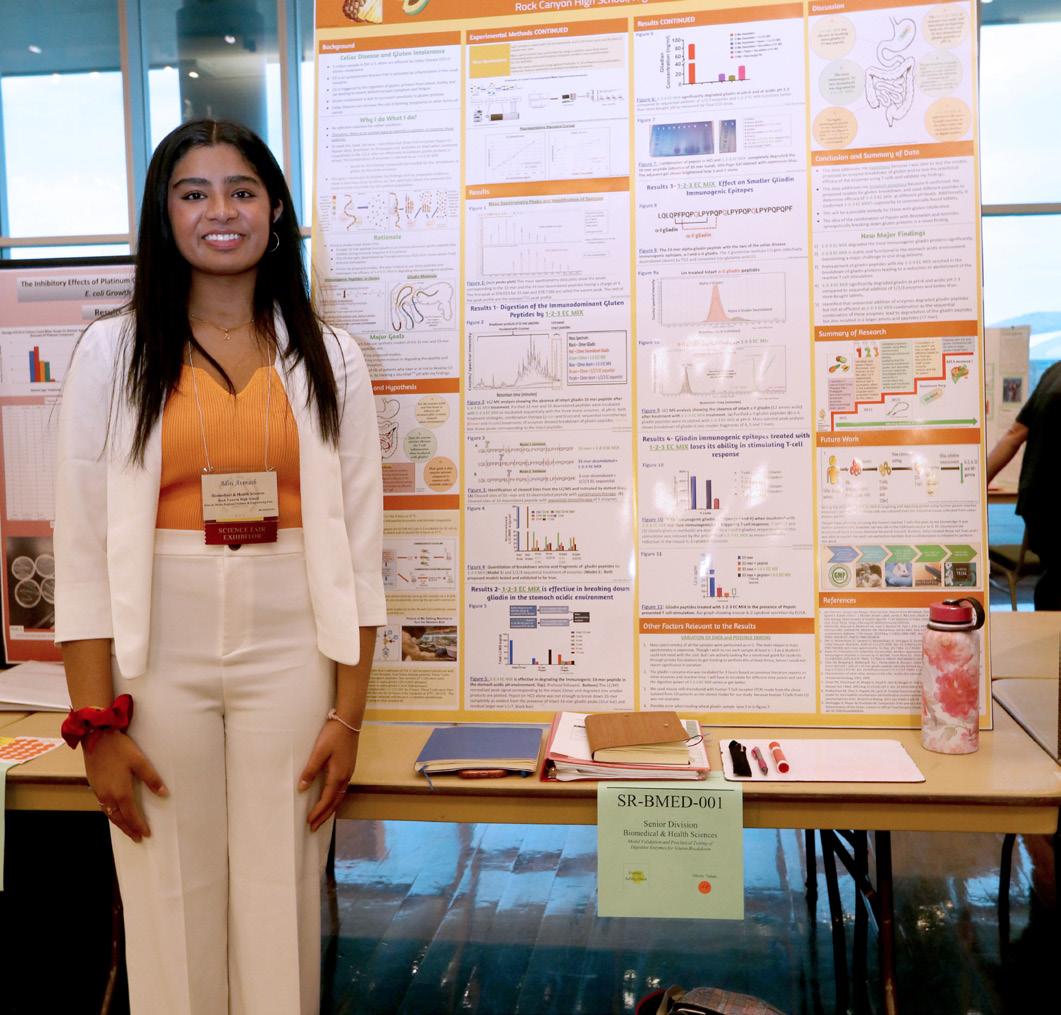
A longtime supporter of the state science fair, each year the CMS Education Foundation presents an award to one student in the junior high division and one student in the senior high division for the Biomedical and Health Sciences category. These students receive $100 and an invitation to the CMS Annual Meeting to display their project and attend the President’s Gala.
Northern Colorado Medical Society leaders Sean Pauzauskie, MD, Cory Carroll, MD, and Donna Sullivan, MD, served as the official Colorado Medical Society judges at this year’s fair.

The junior division winner, Kapil Bhandaram, a seventh grader at Campus Middle School in Greenwood Village, presented his project, “Is there a relationship between meditation and muscle reaction time?” Given that reaction time is critical in everyday activities such as driving and sports, he measured baseline muscle reaction times before meditation in his study group – noting age, gender and exercise habit – then final muscle reaction times after one week of twice-a-day meditation. He found that meditation can improve reaction times in his small sample size.
The senior division winner, Aditi Avinash, an 11th grader at Rock Canyon High School in Littleton, presented her project, “Model validation and preclinical testing of digestive enzymes for gluten breakdown.” She aims to develop a medication for people living with gluten intolerance or celiac disease. She identified three fruit enzymes that synergistically break down gluten when combined and proposed two models of how the enzymes act together to degrade the gluten molecule. She then performed studies to validate the models and felt the results provide her a path to move ahead to formulation.
The judges praised both winners for following a thoughtful and scientific process, and fully grasping their experiments – especially given their young age. They show great promise for future careers in science and, hopefully, medicine. ■
Top: Kapil Bhandaram was awarded CMS’s Award of Excellence in the junior category for his project, “Is there a relationship between meditation and muscle reaction time?”
Bottom: Aditi Avinash was awarded CMS’s Award of Excellence in the senior category for her project, “Model validation and preclinical testing of digestive enzymes for gluten breakdown.”


Editor’s note: Recent changes to medical liability laws in other states underscore a movement of change. The Colorado Medical Society is aware, engaged and actively working to ensure Colorado’s stable medical liability climate remains. CMS and key partners like COPIC will continue to promote patient safety and the importance of liability protections. Physicians should be aware of what current protections are and how they came to be. If you have questions, please do not hesitate to contact Chet Seward, CMS Chief Strategy Officer, at chet_ seward@cms.org or 720-739-5456
The Health Care Availability Act (HCAA) was a major tort reform package passed by the state legislature in 1988 with bipartisan support. These reforms struck a balance to ensure Colorado citizens have access to both high quality health care providers as well as fair compensation if they are harmed due to negligence. The HCAA was crafted after years of a
destabilized, under-regulated tort environment that caused Colorado’s health care providers to experience unpredictably large awards resulting in skyrocketing, unsustainable medical liability insurance premiums in the early 1980s. This resulted in providers being forced to either leave the state and practice medicine elsewhere, eliminate high-risk services from their practice, or fight for reforms to protect their ability to provide needed care to the patients of Colorado. They chose to fight.
The HCAA established a key statutory structure to govern medical malpractice litigation. While the HCAA was modeled after other states also responding to a similar crisis, the brain-trust behind HCAA baked in many reforms that are unique to Colorado. It is due to this thoughtful, multi-pronged reform package that Colorado’s tort environment has been able to withstand legislative and legal attacks over the last 35 years. Several major
pillars of tort reform within the HCAA that are most familiar include:
• Financial liability requirements (e.g. mandating medical liability insurance coverage);

• Limitations on damages (e.g. caps on non-economic damages);
• Establishing judicial procedure (e.g. expert witness standards, disclosure of evidence and judgements, and peer review protections); and
• Limitations on actions (e.g. statutes of limitation, corporate practice of medicine, governmental immunity).
Health care professionals consider a state’s medical liability environment when considering where to practice. Maintaining a stable, balanced tort environment is crucial to the recruitment and retention of quality physicians and to provide accountability and protection for patients who are injured during the course of care. Having fewer health care providers practicing in Colorado means longer wait times, greater distances traveled to reach providers, fewer specialist providers, and higher costs.
Medical liability reforms such as the HCAA help protect patients and the medical community from increasing health care expenses, which is particularly important in underserved communities where quality, affordable health care is at a premium and providers operate on narrow margins. The reforms not only give providers a sense of stability in their practice, but they also allow the medical community to focus their attention and resources on delivering quality care to their patients.
COPIC’s founders helped fight for the HCAA alongside the Colorado Medical Society and have worked to uphold these important reforms over the last 35 years. History has demonstrated that reasonable, thoughtful tort reforms create balance between protecting patients and attracting health care providers. ■

COPIC Financial Service Group’s team of specialists will partner with you to identify your personal goals and navigate your financial path. We’ll help you determine the best option for everything from paying off student loans to retirement planning. We are here for the long haul for each stage of your career, offering insurance and financial solutions at every step. That’s Value Beyond Coverage.

COLORADO PHYSICIAN OR MEDICAL STUDENT CALLS 720-810-9131.
24/7 line answered by a Masters-Level Licensed Clinician (LCSW, LPC) to assess the clinical need of the caller, including life-threatening situations.
CONFIDENTIALITY IS REVIEWED AND PEER SUPPORT SERVICES ARE INITIATED.
Only in circumstances where an individual is a threat to self or others or as outlined in the Medical Practice Act would confidentiality be breached. Doc2Doc Wellbeing Consulting has the same reporting obligation as all licensed Colorado physicians.
PHYSICIAN CALLER RECEIVES WELLBEING SUPPORT FROM A PEER PHYSICIAN.
If Doc2Doc Wellbeing Consulting is the best fit based upon the caller’s presentation, a physician will return the physician’s call for the first of three free peer consultations.
If CPHP traditional comprehensive evaluation services are a best fit based upon caller’s presentation OR if more help is needed at the end of three free Doc2Doc Wellbeing Consulting sessions, CPHP’s process will commence to ensure client has appropriate treatment supports in place.