3 minute read
Should we talk about maternal health? - Thor Nissen
No doubt our knowledge about health conditions and associated pathologies around pregnancy, childbirth, and the postnatal period has progressed greatly along with medical and technological advances. Research on maternal-fetal medicine in the past decades helped to advance our understanding of the field. Examples of such findings are1:
• Routine magnesium sulfate administration for women who are at risk of preterm delivery within 7 days to prevent cerebral palsy in their children.
Advertisement
• Guidelines on the safety of vaginal birth after cesarean section.
• Proper treatment of mild gestational diabetes and high-normal blood sugar levels during pregnancy reducing complications for the mother and baby.
• Steroids given to women at risk for preterm birth improve survival and limit brain injury in infants. •
Changes to how healthcare providers categorize births. •
Progesterone for preventing preterm birth.
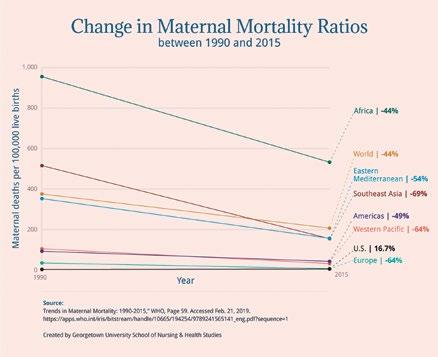
The impact of these and other significant discoveries in the field has had different results in different geographical regions. The following figure shows the change in maternal mortality ratios seen between 1990 and 2015 in different regions, compared to the world average2 .

The highest declines occurred in the least developed regions. A surprising increase was reported in the United States. And it is clear that the starting point for each region is very different, with ratios of maternal deaths per 100,000 live births ranging from less than 20 to over 900.
Reasons for these disparities are complex and involve social, financial, cultural, and other non-medical fields. Common factors may include delays in deciding to seek appropriate medical help, availability of appropriate obstetric facilities, and receiving adequate care when a facility is reached. Cultural factors also influence the outcome of pregnancy. A study demonstrated significant associations between male partners’ involvement in maternal health care and utilization of some maternal health care services by female partners.4
Opportunities remain to reduce maternal mortality and severe maternal morbidity. Data quality and measurement are crucial. Research relies largely on community participation.5
The World Health Organization launched a strategy describing the vision for improving the health of every woman and every child, everywhere, between 2016 and 20306. The Guiding Principles for this program named Ending Preventable Maternal Mortality are:
• Empower women, girls, and communities.
• Protect and support the mother-baby dyad.
• Ensure country ownership, leadership, and supportive legal, technical and financial frameworks.
To achieve its goals inequities must be addressed, universal health coverage should be ensured, and health systems have to be strengthened to improve quality of care and equity.
• Apply a human rights framework to ensure that high-quality reproductive, maternal, and newborn health care is available, accessible, and acceptable to all who need it.
So, the answer to the question in the title is certainly, yes. Much can still be done and needs to be achieved in the medical area and contributing fields.
Thor Nissen

Doctor, graduate in Clinical Pharmacology and MBA in Quality Management. He has managed to collaborate for the development of medicines in world leading pharmaceutical companies both in medical matters and in clinical research in new drugs, regulation, marketing and sales departments.
1. Building the Maternal Health Research Field. https://www.nichd.nih.gov/newsroom/news/051619-maternal-health-researchadvances/slide1
2. Georgetown University. School of Nursing & Health Studies. Maternal Health Around the World, April 2, 2019 https://online. nursing.georgetown.edu/blog/maternal-health-around-the-world/#:~:text=The%20World%20Health%20Organization%20 quantifies,for%20every%20100%2C000%20live%20births.&text=Globally%2C%20maternal%20deaths%20decreased%20 44,they%20increased%20almost%2017%20percent.
3. Barnes-Josiah D, Myntti C, Augustin A. The "three delays" as a framework for examining maternal mortality in Haiti. Soc Sci Med. 1998 Apr;46(8):981-93. doi: 10.1016/s0277-9536(97)10018-1. PMID: 9579750.
4. Mohammed, B.H., Johnston, J.M., Vackova, D. et al. The role of male partner in utilization of maternal health care services in Ethiopia: a community-based couple study. BMC Pregnancy Childbirth 19, 28 (2019). https://doi.org/10.1186/s12884-019-2176-z
5. Chinn JJ, Eisenberg E, Artis Dickerson S, King RB, Chakhtoura N, Lim IAL, Grantz KL, Lamar C, Bianchi DW. Maternal mortality in the United States: research gaps, opportunities, and priorities. Am J Obstet Gynecol. 2020 Oct;223(4):486-492.e6. doi: 10.1016/j. ajog.2020.07.021. Epub 2020 Jul 17. PMID: 32682858; PMCID: PMC7564012.
6. Maternal mortality: Levels and trends 2000 to 2017. https://www.who.int/reproductivehealth/publications/maternalmortality-2000-2017/en/










