




An Old Woman With a Newly Discovered Heart Murmur 51 Diagnosis and Management of Growth Hormone Deficiency in Adults 15 A CME Journal for Family Physicians Antibiotic Diabetes Q&A Study In 2 Minutes 23 26 28 Dr Amdekar's Revision Notes UMEM Pearls Spot The Diagnosis 29 33 35 Top Papers Of The Month Nutritional Pearls Legal Pearls 41 54 56 Empowering Your Practice Vol 13 No 11, February 2023 Drugs for GERD and Peptic Ulcer Disease 42 SUBSCRIBER Evidence-Based Consultations In Primary Care 38 ICMR Releases Antimicrobial Guidelines 2022: Update on Doxycycline


2 GP CLINICS Vol 13 No 11, February 2023







4 GP CLINICS Vol 13 No 11, February 2023
GP Clinics® (ISSN 2249-1872), a initiative, is printed and published by Clinics India Press Pvt. Ltd., F-59, Ashtavinayak, Ganesh Chowk, DN Nagar (Upper JUHU), Andheri (W), Mumbai 400 053, India. Printed at Print Bank, Unit No. 141, First Floor, A/1, Shah & Nahar Industrial Estate, Dhanraj Mill compound, Lower Parel, Mumbai - 400 013, India.
Editorial office: GP Clinics®, Clnics India Pres Pvt. Ltd, F-59, Ashtavinayak, Ganesh Chowk, DN Nagar (Upper JUHU), Andheri (W), Mumbai 400053, India. Tel. +91-22- 2624 3979 / 2624 7061. Whatsapp No.: 81049 63608; Email: GPC@gpclinics.in; Website: www.gpclinics.in
No part of this publication may be reproduced or transmitted in any form, by any means, without written permission of the publisher. This publication is for private circulation to a registered medical practitioner or a hospital or a laboratory in India only.

Statements, opinions, and data published in GP Clinics® are those of the authors and do not reflect the policy or position of GP Clinics® or Clinics India Press Pvt. Ltd. The appearance of advertisements in GP Clinics® does not reflect endorsement of the product or service or guarantee of the advertisers' claims by GP Clinics® or Clinics India Press or Authors or Knowledge Sharing Partner Publishers/Associations/Organizations/ Hospitals or Universities.

5 Vol 13 No 11, February 2023 GP CLINICS
FEATURE DIAGNOSIS AND MANAGEMENT OF GROWTH HORMONE DEFICIENCY IN ADULTS ALEXANDRA MARTIROSSIAN, MD and JULIE SILVERSTEIN, MD Washington University School of Medicine in St. Louis, St. Louis, Missouri 15 Empowering Your Practice A CME Journal for Family Physicians Vol 13 No 11, February 2023 Contd. ... Study in 2 minutes, 28 Diabetes Q&A, 26 Feature, 14 DIABETES Q&A An Interaction With Experts WHAT IS HYPOGLYCEMIA UNAWARENESS?
University
of Medicine in
26 Appropriate And Smart Prescribing ACUTE OTITIS MEDIA 23 ANTIBIOTIC
KIM A. CARMICHAEL, MD—SERIES EDITOR Washington
School
St Louis, Missouri.

6 GP CLINICS Vol 13 No 11, February 2023
GP Clinics® is an authoritative source for comprehensive information and education servicing healthcare professionals. GP Clinics® includes peerreviewed and non-peer-reviewed medical information. It is distributed to Family Physicians, GPs, AYUSH Doctors, IMA, GPA and NIMA members, Internal Medicine Practitioners, State Medical Council Members, in clinic- and/or hospital-based general practice, family practice, and internal medicine practice.
Various knowledge sharing partners contribute quality content in GP Clinics® from time to time. GP Clinics® also contains articles under license from various reputed international resources.


The appearance of advertisements in GP Clinics® is not a warranty, endorsement or approval of the products or services advertised or of their effectiveness, quality or safety by GP Clinics® or Clinics India Press or Authors or Knowledge Sharing Partner Publishers/Associations/Organizations/ Hospitals or Universities. GP Clinics® or Clinics India Press is not responsible for accuracy of dosages given in articles printed herein. GP Clinics® or Clinics India Press disclaims responsibility for any injury to persons or property resulting from any ideas or products referred to in the articles or advertisements.

7 Vol 13 No 11, February 2023 GP CLINICS Dr Amdekar's Notes, 29 UNIVERSITY OF MARYLAND SCHOOL OF MEDICINE Emergency Medicine Educational Pearls AN INTRAVENOUS DRUG ABUSER COMPLAINS OF FEVER, CHILLS AND COUGH: What's the Diagnosis? HANEY MALLEMAT, MD 33
Empowering Your Practice A CME Journal for Family Physicians Vol 13 No 11, February 2023 Contd. ...
DR AMDEKAR'S REVISION NOTES A Way To Clinical Perfection TUBERCULOSIS: AN UNCONQUERED DISEASE YESHWANT K. AMDEKAR, MD, DCH, FIAP 29 STUDY IN 2 MINUTES Quick Recap of A Clinical Trial ALCOHOL ABSTINENCE DECREASED ARRHYTHMIA RECURRENCES IN CHRONIC ALCOHOLICS WITH ATRIAL FIBRILLATION 28
UMEM Perarls, 33

8 GP CLINICS Vol 13 No 11, February 2023 Empowering Your Practice A CME Journal for Family Physicians Vol 13 No 11, February 2023 Offices • India: GP Clinics®, F-59, Ashtavinayak, Ganesh Chowk, DN Nagar (Upper JUHU), Andheri (W), Mumbai 400 053. • USA: GP Clinics®, 2160 W 86th Street, #202, Indianapolis, IN, 46260, USA. • Australia: GP Clinics®, 7 Eumina Street, Cameron Park, NSW 2285, Australia. Postmaster • GP Clinics® is sent through registered post service of Indian Postal Department, Mumbai. • GP Clinics® is dispatched in the last week of every month for the issue dated coming month. • It takes around 7 working days for the delivery. Contd. ... ONE MINUTE QUIZ A Breather To Stay Up To Date ACUTE MIGRAINE TREATMENT IN YOUTH 40 mQ1 One Miniute Quiz, 38 NEWS AND PERSPECTIVE Medical Happenings Around the World ICMR RELEASES ANTIMICROBIAL GUIDELINES 2022: UPDATE ON DOXYCYCLINE 38 TOP PAPERS OF THE MONTH Articles You Don’t Want To Miss URINALYSIS HAS PYURIA, LEUCOCYTE ESTERASE —AND IS GROWING BACTERIA; CAN YOU RESIST THE URGE TO TREAT? GREGORY W. RUTECKI, MD 41 Drugs In Practice, 42 SPOT THE DIAGNOSIS Test Your Diagnostic Skills In Dermatology QUIZ #61 35 Spot The Diagnosis, 35


9 Vol 13 No 11, February 2023 GP CLINICS DRUGS IN PRACTICE Critical Review of Drugs Used in Daily Practice DRUGS FOR GERD AND PEPTIC ULCER DISEASE 42 Empowering Your Practice A CME Journal for Family Physicians Vol 13 No 11, February 2023 Change of address • Send address changes to GP Clinics®, F-59, Ashtavinayak, Ganesh Chowk, DN Nagar (Upper JUHU), Andheri (W), Mumbai 400 053, India. • Email your old and new address at GPC@gpclinics.in OR Whatsapp at 81049 63608 Subscriptions • For subscription enquiries visit www.gpclinics.in and click subscription icon on the home page and follow the instructions accordingly. OR • Whatsapp at 81049 63608 OR Call at 81049 63608 or 022-2624 3979 OR • SMS at 81049 63608 OR Email at GPC@gpclinics.in Missing issues/grievance • “Missing issue” complaints should reach us within 30 days of missing an issue. • Whatsapp at 81049 63608 OR Call at 81049 63608 or 022-2624 3979 OR SMS at 81049 63608 • Email at GPC@gpclinics.in WHAT’S THE “TAKE HOME”? Critical Appraisal In Medicine A 78-YEAR-OLD WOMAN WITH A NEWLY DISCOVERED SIGNIFICANT HEART MURMUR RONALD N. RUBIN, MD—SERIES EDITOR 51 NUTRITIONAL PEARLS Nutrition and Health THE BENEFITS OF CYCLING FOR INDIVIDUALS WITH DIABETES TIMOTHY S. HARLAN, MD 54 LEGAL PEARLS Law Prespecitve In Medicine CAN A HOSPITAL BE RESPONSIBLE FOR PATIENT CARE BY AN OUTSOURCED PHYSICIAN? ANN W. LATNER, JD 56 Nutritional Pearls, 54 Legal Pearls, 56
Medical Advisors
DR
DR NH BANKA
MD,
DCH, FIAP Consultant Pediatrician
PROF (DR) DG SAPLE
MD, FCPS (Dermatology)
Fellow of Johns Hopkins University, USA Prof. & Ex-HOD, Dermatology, Grant Medical Collage, Mumbai Consultant in Dermatology, Cosmetology, Trichology & Hair Transplant
DR RAM PRABHOO

MS (Orthopedics), FICS
Medical Director, Mukund Hospital, Andheri HOD, Orthopedics, Wadia Hospital, Parel Orthopedic Consultant, Hiranandani Hospital,Powai, Mumbai IPP, Indian Orthopedic Association
DR UMESH KHANNA
MD, DNB (Nephro) Consultant Nephrologist and Transplant Physician Chairman, Mumbai Kidney Foundation
DR MAKARAND DAMLE
MS (ENT), DNB, FCPS, DORL Ear, Nose, Throat and Head - Neck Surgeon
DR KETAN MEHTA
MD (Medicine), FCPS, FICP, FISE, Consultant Physician, Cardiopulmonologist and Diabetologist
DR SAMEER SHRIVASTAVA MD (Med), DM (Cardiology)





Executive Director, Non-Invasive Cardiology and Head of Research, Fortis Escorts Heart Institute, New Delhi
MD (BOM), FCPS, FACG (USA) Chief, Hepato-Gastroenterologist, Bombay Hospital and Medical Research Centre Fellow American College of Gastroenterology
PROF JC SURI
MD, DNB, FNCCP, FACCP
Chairman, JCS Institute of Pulmonary, Critical Care and Sleep Medicine.
Ex-Prof and HOD, Department of Pulmonary, Critical Care and Sleep Medicine, VM Medical College and Safdarjung Hospital, New Delhi

DR SHASHANK R JOSHI
MD, DM, FICP, FACP (USA), FACE (USA), FRCP (Lon,Glsg & Edin); (Padma Shri Awardee), Endocrinologist, Lilavati Hospital, President, API, 2014-15, Emeritus Editor, JAPI, President, IAD & Hypertension Society of India Chapter Chair India, AACE

DR AGAM VORA
MD (Chest and TB), DETRD, FIAHE, FCCP, FSASMS, Asthma and Allergy Specialist, Consultant Pulmonologist and Chest Physician
PROF (DR) MANOJ SHARMA, MBBS, Ph.D., MCHES Professor & Chair, Department of Social & Behavioral Health, School of Public Health, and Adjunct Professor, Department of Internal Medicine, Kirk Kerkorian School of Medicine at UNLV, University of Nevada, Las Vegas (UNLV)



DR MAHESH C GOEL

MD, MBA, FRCS, MCh Chief, Institute of Urology Advanced Center of Sexual Function Indianapolis, Indiana, USA

10 GP CLINICS Vol 13 No 11, February 2023
YESHWANT K AMDEKAR
Knowledge Sharing Partners


Seventeen speciality departments. One goal. Your well-being.
There’s only one thing that matters at our Centres for Excellence. You. So, whether it’s investing in cutting-edge technology or recruiting the finest medical professionals, we’re willing to go the extra mile to ensure your well-being.

11 Vol 13 No 11, February 2023 GP CLINICS
Room
Deluxe



12 GP CLINICS Vol 13 No 11, February 2023
Vomiting: Look beyond GI system
Abdominal Pain: Beware, it is in a Pandora's Box
Pallor: Bedside Diagnosis Possible


13 Vol 13 No 11, February 2023 GP CLINICS
5
GP Clinics,
20.11.22
Dec ’22
6
GP Clinics,
18.12.22
Jan’23
7
GP
29.01.23
Clinics, Feb’23
Is your phone keeping you up at night? With a few tweaks to your tech habits, you can wake up more refreshed and ready to face the day.
Charge your device as far away from your bed as possible. Added bonus? The distance may help you feel less overwhelmed in general. MOVE IT.

Dim your screen or use a red filter app at night. The bright blue light of most devices can mess with your circadian rhythm and melatonin production. DIM IT.
Alarms aren’t just for waking up –set a bedtime alarm to remind you that it’s time to wrap it up for the night. SET IT.
If you’ve got a scrolling habit you need to kick, try an app-blocking app that makes it impossible to get lost in after-hours emails, social media or gaming. LOCK IT.
BLOCK IT.
Tell notifications to buzz off if they’re waking you up at night. Put your phone on “do not disturb” mode to block it all out when you’re trying to sleep.
You may cut this poster and paste it in your clinic for patients' education and information
EAT SMART. MOVE MORE. BE WELL.
©2020 American Heart Association, Inc., a 501(c)(3) not-for-profit. All rights reserved. Unauthorized use prohibited. DS16479 8/20 HEART.ORG/HEALTHYFORGOOD GET MORE WELLNESS TIPS AT
CUT HERE CUT HERE Reprinted with permission Healthy for Good™ ©American Heart Association, Inc. https://www.heart.org/en/healthy-living/healthy-living-infographics
Diagnosis and Management of Growth Hormone Deficiency in Adults
Alexandra Martirossian, MD1 • Julie Silverstein, MD2
Growth hormone deficiency (GHD) is a clinical syndrome caused by decreased production of or decreased tissue responsiveness to growth hormone. The most common cause of GHD in adults is pituitary tumors and their associated treatments of surgery or radiotherapy. Clinical manifestations of adult-onset GHD are nonspecific and include central obesity, loss of lean muscle mass, decreased bone density, insulin resistance, cardiovascular disease, hyperlipidemia, decreased exercise tolerance, and decreased quality of life. Diagnosis of GHD is confirmed by stimulatory testing or a low insulin-like growth factor 1 (IGF-1) level in the setting of multiple pituitary hormone deficiencies and organic pituitary disease. Treatment involves replacement with recombinant human growth hormone, and goals of therapy include clinical improvement, avoidance of adverse effects, and normalization of IGF-1 levels. Recombinant human growth hormone should only be prescribed for its approved clinical uses by an endocrinologist, and the risks and
AFFILIATIONS:
benefits of therapy should be weighed on a case-by-case basis.1,2
Physiology
Growth hormone (GH) is a polypeptide hormone secreted by somatotroph cells in the anterior pituitary that exerts several anabolic effects throughout the body. The GH receptor is expressed in multiple tissues including the liver, cartilage, muscle, fat, and kidneys.1 Activation of the GH receptor in the liver leads to hepatic production of insulin-like growth factor 1 (IGF-1), a peptide important for mediating many of GH’s effects. In children, GH and IGF-1 are required for chondrocyte proliferation and linear growth. In adults, GH promotes several primarily anabolic effects including breakdown of fat, muscle growth, hepatic glucose production, and bone formation.1,3 Growth hormone secretion is regulated by a complex mixture of signals from the hypothalamus, gut, liver, and gonads, with production stimulated by growth hormone-releasing hormone (GHRH) from the hypothalamus and inhibited by somatostatin, which is
1Fellow, Division of Endocrinology, Metabolism, & Lipid Research, Washington University School of Medicine in St. Louis, St. Louis, Missouri
2Associate Professor of Medicine and Neurological Surgery, Division of Endocrinology, Metabolism, & Lipid Research, Washington University School of Medicine in St. Louis, St. Louis, Missouri
CITATION:
Martirossian A, Silverstein J. Diagnosis and management of growth hormone deficiency in adults. Published online October 14, 2021. Received July 25, 2021. Accepted August 27, 2021.
DISCLOSURES:
The authors report no relevant financial relationships.
CORRESPONDENCE:
Julie Silverstein, MD, Washington University School of Medicine in St. Louis, 660 South Euclid Avenue, St. Louis, MO 63110.
primarily secreted in the brain and gastrointestinal tract. Factors that stimulate GH secretion include deep sleep, fasting, hypoglycemia, α-adrenergic pathways, ghrelin, sex steroids, stress, and amino acids (eg, arginine, leucine).3 Factors that suppress GH secretion include obesity, glucocorticoids, glucose, hypothyroidism, IGF-1 (negative feedback), α-adrenergic pathways, and free fatty acids. GH secretion is episodic and exhibits a diurnal rhythm with approximately two-thirds of the total daily GH secretion produced at night triggered by the onset of slow-wave sleep.3 GH levels reach a nadir during the day and may be undetectable, especially in obese or elderly persons. Over the course of a lifetime, GH secretion gradually rises during childhood, peaks during puberty, then gradually declines through adulthood. The phenomenon of agerelated decline in GH levels is sometimes referred to as “somatopause.”4
Causes of Growth Hormone Deficiency
GHD can occur at any age and results from both congenital and acquired disorders (Table 1). Congenital causes include gene mutations and structural defects. Mutations in the genes encoding GH, GH receptor, GHRH receptor, and various transcription factors can cause GHD.
Structural defects include empty sella syndrome, septo optic dysplasia, hydrocele, and pituitary hypoplasia. 2 Acquired causes include intracranial tumors (eg, pituitary adenoma, craniopharyngioma, Rathke cleft cyst, glioma/astrocytoma, metastasis), head trauma, central nervous system infection, infarction (Sheehan syndrome), and infiltrative/granuloma-
15 Vol 13 No 11, February 2023 GP CLINICS
Feature
Diagnosis and Management of Growth Hormone Deficiency in Adults
Table 1. Causes of Growth Hormone Deficiency in Adults2,14
Intracranial tumors
Pituitary adenoma
Craniopharyngioma
Rathke cleft cyst
Meningioma
Glioma/Astrocytoma
Skull-base lesions
Chordoma
Hamartoma
Lymphoma
Metastases
Traumatic brain injury
Surgery in the sella, suprasellar, and parasellar regions
Cranial irradiation
Infiltrative/granulomatous disease
Sarcoidosis
Amyloidosis
Langerhans cell histiocytosis
Autoimmune hypophysitis (primary, secondary)
Central nervous system infections
Infarction/hemorrhage
Apoplexy
Sheehan syndrome
Subarachnoid hemorrhage
Ischemic stroke
Congenital
Genetic mutations (GH, GH receptor, transcription factors)
Structural defects (septo-optic, dysplasia, empty sella syndrome)
Hydrocephalus
Idiopathic
tous disease (eg, sarcoidosis, Langerhans cell histiocytosis, tuberculosis). GHD can also result from treatments for some of the aforementioned conditions, particularly cranial surgery or irradiation. In adults, the most common cause of GHD is a pituitary adenoma or treatment of the adenoma with pituitary surgery and/or
radiotherapy, with the risk of deficiency proportional to the size of the tumor and extent of treatment. 2
Benefits of Growth Hormone Deficiency
Manifestations of GHD in adults may include central obesity, loss of lean muscle mass, decreased bone mass, insulin resistance, cardiovascular disease, hyperlipidemia, and decreased quality of life.1 Data supporting the benefits of GH replacement are mixed, with much of the data showing benefit coming from retrospective and open-label observational studies. Some, but not all, studies show that GH replacement is associated with an increase in strength and exercise capacity2 and is associated with an increase in bone mineral density5,6 and decreased fracture risk.7 In terms of cardiovascular disease, a metanalysis of randomized, blinded, placebo-controlled trials suggests that GH replacement increases lean body mass and decreases fat mass, has a beneficial effect on low-density lipoprotein cholesterol, and lowers diastolic blood pressure8, but there is no evidence that these changes are associated with measurable changes in cardiovascular function.9
The effect of GH replacement on glucose metabolism is complex. GH antagonizes the action of insulin, and evidence suggests that GH replacement may lead to a transient increase in fasting glucose10 but not necessarily an increased incidence of diabetes.11 Long-term observational studies of patients with adult GHD also suggest that GH replacement is associated with an improvement in quality of life when assessing parameters such as memory and concentration, fatigue, tenseness, socializing, and self-confidence.12,13
Diagnosing Growth Hormone Deficiency
Making the diagnosis of GHD is generally easier in children because the outcome of short stature is readily apparent. The task is more difficult in those with adult-onset deficiency because the
symptoms are generally nonspecific, so a higher index of suspicion is required.
Because of the high financial cost of recombinant human growth hormone (rhGH) and possibility of adverse effects, it is crucial that the correct diagnosis is made and that treatment is only pursued in those adults who are truly GH deficient. This shrewdness is important for prevention of inappropriate treatment that is sometimes seen in nonmedical conditions such as aging and sports. In deciding who to screen, a clinical history guides the extent of required testing (Figure)
In adults with a history of organic hypothalamic-pituitary disease (eg, pituitary mass with previous surgery and cranial irradiation) with at least 3 hormone deficiencies (eg, hypothyroidism, adrenal insufficiency, and hypogonadism) and a low serum IGF-1 level (< –2.0 standard deviation score, also reported as a Z-score), no further testing is required, and treatment can be initiated.14 This also applies to adults who have congenital structural defects or genetic mutations affecting the hypothalamic-pituitary axes who have at least 3 other hormone deficiencies and low serum IGF-1 level. In adults who have a history of organic hypothalamic-pituitary disease with 2 or fewer hormone deficiencies, high clinical suspicion, and a low IGF-1 level (< 0 standard deviation score), provocative testing for GHD is indicated.14
In the absence of any of these risk factors, testing is not advised. It should be noted that 30% to 40% of patients with adult-onset GHD may have normal IGF-1 levels, so if clinical suspicion remains high, diagnostic testing should be pursued.15 In adults with idiopathic GHD in childhood, retesting should be performed because a significant proportion of this population may have normal GH secretion as adults.16-19
Measurement of random GH levels for the purpose of diagnosing GHD is not reliable for multiple reasons. First, GH has a short circulating half-life of only 10 to 20 minutes, and the pulsatility of GH
16 GP CLINICS Vol 13 No 11, February 2023
secretion makes interpretation of single measurements difficult. 20 Second, GH secretion is suppressed in the postprandial state, so timing of food consumption is important to know. Other factors associated with decreased IGF-1 levels that should be taken into consideration when interpreting laboratory test results include advanced age, obesity, poorly controlled diabetes, liver disease, renal failure, oral estrogen use, hypothyroidism, and critical illness. 21 Additionally, assays for GH and IGF-1 have not been rigorously standardized, and “normal” baseline values for adults are often inadequate. To circumvent these diagnostic issues, GH stimulation tests are used. There are several GH provocative tests available in clinical practice (Table 2), each with its own advantages and disadvantages.
The insulin tolerance test (ITT), although not commonly used in the United States, is considered the gold standard for diagnosis of GHD.4,14,22 Insulin-induced hypoglycemia stimulates the release of GH. The ITT is performed by having
the patient fast for at least 8 hours and then intravenous insulin is administered at a dose of 0.05 to 0.15 U/kg. Blood is drawn fasting and then 20, 30, 40, and 60 minutes after adequate hypoglycemia is achieved (blood glucose, < 40 mg/ dL). 22,23 The diagnostic cutoff for GHD is a GH level 5 µg/L or lower after hypoglycemia is achieved. The positive predictive value is 93%, sensitivity is 96%, and specificity is 92%. 22 Several drawbacks of the ITT—including the requirement for close medical supervision by a physician throughout the test, the possibility of inducing severe life-threatening hypoglycemia, and the risk of causing seizures and altered consciousness in certain susceptible populations—limit its use. The ITT is contraindicated in individuals aged older than 65 years, those who are pregnant, and those who have a history of or are at risk for seizures and cardiovascular disease. Moreover, normoglycemic or hyperglycemic patients with obesity and insulin resistance may require higher doses of insulin (0.15-0.2 U/kg) to achieve
target hypoglycemia, thus increasing their risk for delayed hypoglycemia.
Finding an alternative to the ITT for the diagnosis of GHD has been challenging. The GHRH-arginine stimulation test showed favor for some time because of its convenience, reproducibility, and discriminatory power. However, in 2008, the recombinant GHRH (ie, injectable sermorelin) was removed from the market, so the test could no longer be performed in the United States.14,22 Since then, the glucagon stimulation test (GST) has become a preferred alternative diagnostic test for GHD in the United States. The exact mechanism for how glucagon stimulates GH secretion is poorly understood, but it has been shown to be a more-potent stimulator of GH secretion than other agents, including arginine and clonidine. 24,25 Glucagon is more effective at stimulating GH secretion when administered intramuscularly compared with intravenously. 26 The GST is performed by first having the patient fast for 8 to 10 hours, and then intramuscular glucagon

17 Vol 13 No 11, February 2023 GP CLINICS Feature
Diagnosis and Management of Growth Hormone Deficiency in Adults
Figure. Algorithm for Stimulation Testing and Treatment in Adults With Suspected Growth Hormone Deficiency14
Table 2. Provocative Tests for the Diagnosis of Growth Hormone Deficiency in Adults1,22,29
Insulin tolerance
Fast at least 8 h
Unpleasant hypoglycemic symptoms may occur
IV insulin, 0.05-0.15 U/kg Requires close medical supervision
Record neuroglycopenic symptoms
Blood sampling at fasting and 2, 30, 40, and 60 min after hypoglycemia (blood glucose, < 40 mg/dL) is achieved
Glucagon Fast at least 8 h
IM glucagon, 1 mg (1.5 mg if > 90 kg)
Measure GH every 30 min for 4 h
Macimorelin Fast at least 8 h
0.5 mg/kg oral solution
Measure GH at 30, 45, 60, and 90 min
is administered (1 mg if weight is ≤ 90 kg, 1.5 mg if weight is > 90 kg). Serum GH and blood glucose levels are measured at 0, 30, 60, 90, 120, 150, 180, 210, and 240 minutes after glucagon is administered. A GH cutoff of 3 µg/L has been shown to have sensitivity and specificity of up to 100% in lean subjects (body mass index, ≤ 25 kg/m2). 22 However, because obesity blunts the GH secretion response to glucagon, a lower cutoff of 1 µg/L is recommended in individuals who are overweight or obese (body mass index, > 25 kg/m2). 22 Advantages of the GST include its availability, reproducibility, safety, lack of influence by gender and hypothalamic cause of GHD, and relatively few contraindications. Disadvantages include its long duration, the need for intramuscular administration and multiple blood draws, and gastrointestinal adverse effects. The
if BMI is ≤ 25 kg/m2
if BMI is > 25 kg/m2
Contraindications: epilepsy, cardiovascular disease, age > 65 years, pregnancy
Nausea, vomiting, and delayed hypoglycemia may occur
Contraindications: Malnourished patients, fasting > 48 h, severe fasting hyperglycemia > 180 mg/dL
Avoid concomitant use with medications known to cause QTC prolongation
Safety and diagnostic performance not established for BMI of > 40 kg/m2
High cost
test is contraindicated in malnourished individuals or individuals who have not eaten for more than 48 hours, as well as those with severe fasting hyperglycemia (> 180 mg/dL). 22,23 Because late hypoglycemia may occur, individuals should be advised to eat small and frequent meals after completion of the test.
In 2017, the US Food and Drug Administration (FDA) granted approval for the use of macimorelin for diagnosing adult GHD. 27 Macimorelin acetate is an oral ghrelin receptor agonist with GH secretagogue activity that is readily absorbed and effectively stimulates endogenous GH secretion in healthy volunteers with good tolerability. 28 To validate the efficacy and safety of macimorelin in the diagnosis of adult GHD, Garcia and colleagues performed an open-label, randomized, multicenter, 2-way cross-
over study of the macimorelin test vs the ITT. 29 Participants with high (n = 38), intermediate (n = 37), and low (n = 39) likelihood for adult GHD and healthy, matched controls (n = 25) were included in the efficacy analysis. The macimorelin oral solution was prepared at a dose of 0.5 mg/kg of body weight. Blood samples for GH serum levels were collected before and at 30, 45, 60, and 90 minutes after administration of macimorelin. Using a GH cutoff of 2.8 ng/ mL for the macimorelin test and 5.1 ng/ mL for the ITT, the sensitivity was 87% and specificity was 96%. In post-hoc analyses, increasing the GH cutoff for the macimorelin test to 5.1 ng/mL while maintaining the GH cutoff of 5.1 ng/mL for the ITT resulted in a sensitivity of 92% and specificity of 96%. A greater peak GH level was seen in all groups
18 GP CLINICS Vol 13 No 11, February 2023 Feature
Diagnosis and Management of Growth Hormone Deficiency in Adults
TEST PROTOCOL GH CUTOFF COMMENTS
test
≤ 5 µg/L
≤
µg/L
3
≤
µg/L
1
≤ 2.8 µg/L
Diagnosis and Management of Growth Hormone Deficiency in Adults
with the macimorelin test compared with the ITT. Reproducibility for macimorelin was high at 97%. The macimorelin test was well tolerated with no serious or frequent adverse effects reported. The most common adverse effect was mild and transient dysgeusia. Garcia and colleagues later performed post-hoc analyses to determine whether macimorelin performance was affected by age, body mass index, or sex and evaluated its performance vs ITT over a range of GH cutoffs.30 They found that macimorelin performance was not meaningfully affected by age, body mass index, or sex. Caution should be used in generalizing these results in pediatric, elderly, and severely obese patients, since the study population age range was 18 to 66, and the highest recorded baseline body mass index was 36.6 kg/m2, with most participants having a body mass index of less than 30 kg/m2. Of the 4 GH cutoffs evaluated (2.8 ng/mL, 4.0 ng/mL, 5.1 ng/ mL, and 6.5 ng/mL), the cutoff of 5.1 ng/ mL provided maximal specificity (96%) and high sensitivity (92%) and was in good overall agreement with the ITT at the same cutoff (87%). At present, the approved FDA cutoff is the lower value of 2.8 ng/mL. 29 Compared with the ITT and GST, the macimorelin stimulation test has the advantages of being safer, well tolerated, easier to perform, and is less influenced by body weight, so its use in clinical practice may increase in coming years. A major factor currently limiting its widespread use is high financial cost.14
Treatment of Growth Hormone Deficiency
Once the diagnosis of GHD has been made, treatment is initiated with rhGH, which contains the identical sequence of amino acids found in HGH. For many years, the only rhGH product on the US market was somatropin, a once-daily injection. In September 2020, the FDA approved once-weekly somapacitan for the treatment of adult GHD, but it is not yet available on the market.31,32 It is hoped
that the decreased frequency of injections should lower the burden of treatment and improve treatment adherence. Multiple brands of somatropin are available, and there is no evidence that one commercial product is different or more advantageous than another, apart from differences in pen devices, electronic autoinjector devices that are user-friendly, dose per milligram adjustments, and whether the product requires refrigeration.14
In adults, the typical dose of somatropin ranges from 0.1 to 0.4 mg/d and is influenced by age, sex, comorbidities, and concomitant medications. Per the 2019 guidelines published by the American Association of Clinical Endocrinologists (AACE), the recommended starting dose for patients aged younger than 30 years is 0.4 to 0.5 mg/d, aged between 30 to 60 years is 0.2 to 0.3 mg/d, and aged older than 60 years is 0.1 to 0.2 mg/d. In patients transitioning from pediatric to adult care, rhGH should be continued at 50% of the dose used in childhood and then gradually adjusted. In patients with concurrent type 2 diabetes, previous gestational diabetes, and obesity, lower doses of 0.1 to 0.2 mg/d are recommended. Women tend to require higher doses than men to achieve the same IGF-1 level, especially if they are taking oral estrogen.33,34 Approximately 85% of circulating IGF-I is liver derived, and oral estrogen, which undergoes first pass metabolism, suppresses hepatic production of IGF-1. rhGH dose reduction is often necessary when oral estrogen is stopped or switched to transdermal. Most adverse effects of treatment are dose related. The most common adverse effects are related to insulin resistance and fluid retention and include hyperglycemia, paresthesias, joint stiffness, peripheral edema, arthralgias, myalgias, and carpal tunnel syndrome. 2 Contraindications to treatment include active malignancy and active proliferative or severe nonproliferative diabetic retinopathy.
After GH replacement therapy is initiated, it is recommended that patients follow-up in 1- or 2-month intervals at
first, which can later be spaced out to 6or 12-month intervals once a stable dose has been reached.14 Determination of the appropriate dose is influenced by multiple factors, including clinical improvement in symptoms, avoidance of adverse effects, and IGF-1 level. Assessment of fasting glucose, hemoglobin A1c, fasting lipids, body mass index, waist circumference, waist-to-hip ratio, and quality of life should be performed at least once per year. Assessment of other pituitary hormone deficiencies and structural pituitary lesions with laboratory and imaging studies, respectively, should be performed as clinically indicated. If the initial bone density scan is abnormal, repeat evaluations at 2- to 3-year intervals are recommended. IGF-1 levels are commonly used to guide the adequacy of rhGH dosing, and the general recommendation is to target a level within age-adjusted reference ranges (standard deviation score, –2 and +2). However, studies have shown varying benefits and drawbacks to targeting IGF1 levels in the upper or lower half of this range. Targeting IGF-1 levels in the upper range of normal (standard deviation score, 1-2) has shown benefits in body fat composition, waist circumference, and microcirculatory function but at the expense of increased insulin resistance and myalgias.35,36 Targeting IGF-1 levels in the lower range of normal (standard deviation score, –2 to –1) is more often associated with fatigue. Women may have a narrower therapeutic dose window than men. In a study by van Bunderen and colleagues, a high-normal IGF-1 target level in female study participants was associated with impaired prefrontal cognitive functioning, whereas a low-normal target IGF-1 level was associated with decreased vigor.37
The question of how long to continue GH replacement therapy is frequently debated. If clinical benefits have resulted from treatment (eg, improved quality of life, body composition, cardiovascular health, bone density), rhGH can be continued indefinitely presuming there are no contraindications. If there are neither subjective nor objective benefits after at
19 Vol 13 No 11, February 2023 GP CLINICS Feature
Diagnosis and Management of Growth Hormone Deficiency in Adults
least 12 to 18 months of treatment, the option of discontinuing GH replacement should be discussed with the patient. 2,14 Since GH promotes cellular proliferation and tissue growth, there has been a longstanding theoretical concern that rhGH leads to increased risk of malignancy. Although studies show no increased risk of malignancy in hypopituitary patients on long-term growth hormone treatment, an abundance of caution should be exercised when deciding whether to start rhGH in patients with GHD and a history of or genetic predisposition to malignancy.38 It has been suggested that in adult patients with a history of cancer, low-dose rhGH should only be initiated 5 years after cancer remission is achieved.14,39 The patient’s oncologist should be in agreement and closely involved in follow-up care while the patient is taking therapy. In all patients, regardless of cancer risk, cancer screening guidelines should be followed. A topic that has gained much attention in our culture is the use of GH for antiaging, with some citing it as a “fountain of youth.”40 Despite the popularity of this idea, no studies have assessed long-term (> 6 months) efficacy or safety of rhGH administration for this purpose in humans.14 Paradoxically, studies performed in mice have shown that mice with isolated GHD caused by GHRH or GHRH receptor mutations, combined deficiency of GH, prolactin, and thyroid-stimulating hormone, or global deletion of GH receptors live longer than their normal siblings and exhibit multiple features of delayed and/or slower aging.41-43 Liu and colleagues performed a meta-analysis of 31 studies describing the use of GH in healthy elderly adults and found that GH use was associated with small changes in body composition but increased rates of adverse events.44 In the United States, off-label distribution or marketing of rhGH to treat aging or aging-related conditions and for the enhancement of athletic performance is illegal. Given the clinical concerns and legal issues involved, it is strongly recommended that rhGH only be
prescribed for the well-defined approved uses of the medication, which are GHD and HIV-associated lipodystrophy.14,45,46
Conclusions
Growth hormone replacement therapy in adults with confirmed GHD has been shown to be associated with improvement in multiple aspects of health, including body composition, muscle mass, cardiovascular health, bone density, and quality of life. The clinical manifestations of GHD in adults are often nonspecific, so diligence to confirm an accurate diagnosis is essential for avoiding the costs and ethical dilemmas of inappropriate treatment. There are multiple GH stimulatory tests available, each with its own benefits and caveats. Once the diagnosis of adult GHD is established, rhGH should be initiated at low doses and uptitrated based on IGF-1 levels and symptoms, while avoiding adverse effects. Research into longer-acting rhGH formulations and enhanced diagnostic testing is ongoing and will be essential for guiding the management of adult GHD.
REFERENCES
1. Melmed S. Pathogenesis and diagnosis of growth hormone deficiency in adults. N Engl J Med. 2019;380(26):2551-2562. https://doi.org/10.1056/nejmra1817346
2. Molitch ME, Clemmons DR, Malozowski S, et al. Evaluation and treatment of adult growth hormone deficiency: an Endocrine Society Clinical Practice Guideline. J Clin Endocrinol Metab. 2006;91(5):1621-1634. https://doi.org/10.1210/jc.2005-2227
3. Kaiser U, Ho K. Pituitary physiology and diagnostic evaluation. In: Melmed S, Koenig R, Rosen C, Auchus R, Goldfine A, eds. Williams Textbook of Endocrinology. 14th ed. Elsevier; 2020:184-235.e14.
4. Van Den Beld AW, Lamberts SWJ. Endocrinology and aging. In: Melmed S, Koenig R, Rosen C, Auchus R, Goldfine A, eds. Williams Textbook of Endocrinology. 14th ed. Elsevier; 2020:1179-1194.
5. Barake M, Klibanski A, Tritos NA. Effects of recombinant human growth hormone therapy on bone mineral density in adults with
growth hormone deficiency: a meta-analysis. J Clin Endocrinol Metab. 2014;99(3):852860. https://doi.org/10.1210/jc.2013-3921
6. Elbornsson M, Götherström G, Bosæus I, Bengtsson BÅ, Johannsson G, Svensson J. Fifteen years of GH replacement increases bone mineral density in hypopituitary patients with adult-onset GH deficiency. Eur J Endocrinol. 2012;166(5):787-795. https:// doi.org/10.1530/eje-11-1072
7. Mazziotti G, Bianchi A, Bonadonna S, et al. Increased prevalence of radiological spinal deformities in adult patients with GH deficiency: influence of GH replacement therapy. J Bone Miner Res. 2006;21(4):520528. https://doi.org/10.1359/jbmr.060112
8. Maison P, Griffin S, Nicoue-Beglah M, et al. Impact of growth hormone (GH) treatment on cardiovascular risk factors in GH-deficient adults: a metaanalysis of blinded, randomized, placebo-controlled trials. J Clin Endocrinol Metab. 2004;89(5):2192-2199. https://doi.org/10.1210/jc.2003-030840
9. He X, Barkan AL. Growth hormone therapy in adults with growth hormone deficiency: a critical assessment of the literature. Pituitary. 2020;23(3):294-306. https://doi. org/10.1007/s11102-020-01031-5
10. Woodmansee WW, Hartman ML, Lamberts SW, Zagar AJ, Clemmons DR; International HypoCCS Advisory Board. Occurrence of impaired fasting glucose in GH-deficient adults receiving GH replacement compared with untreated subjects. Clin Endocrinol (Oxf). 2010;72(1):59-69. https://doi. org/10.1111/j.1365-2265.2009.03612.x
11. Attanasio AF, Jung H, Mo D, et al. Prevalence and incidence of diabetes mellitus in adult patients on growth hormone replacement for growth hormone deficiency: a surveillance database analysis. J Clin Endocrinol Metab. 2011;96(7):2255-2261. https://doi.org/10.1210/jc.2011-0448
12. Mo D, Blum WF, Rosilio M, Webb SM, Qi R, Strasburger CJ. Ten-year change in quality of life in adults on growth hormone replacement for growth hormone deficiency: an analysis of the hypopituitary control and complications study. J Clin Endocrinol Metab. 2014;99(12):4581-4588. https://doi. org/10.1210/jc.2014-2892
13. Koltowska-Häggström M, Mattsson AF,
20 GP CLINICS Vol 13 No 11, February 2023
Feature
Diagnosis and Management of Growth Hormone Deficiency in Adults
Shalet SM. Assessment of quality of life in adult patients with GH deficiency: KIMS contribution to clinical practice and pharmacoeconomic evaluations. Eur J Endocrinol. 2009;161 Suppl 1:S51-S64. https:// doi.org/10.1530/eje-09-0266
14. Yuen KCJ, Biller BMK, Radovick S, et al. American Association of Clinical Endocrinologists and American College of Endocrinology guidelines for management of growth hormone deficiency in adults and patients transitioning from pediatric to adult care. Endocr Pract. 2019;25(11):1191-1232.
https://doi.org/10.4158/gl-2019-0405
15. Hilding A, Hall K, Wivall-Helleryd IL, Sääf M, Melin AL, Thorén M. Serum levels of insulin-like growth factor I in 152 patients with growth hormone deficiency, aged 19-82 years, in relation to those in healthy subjects. J Clin Endocrinol Metab. 1999;84(6):2013-2019. https://doi. org/10.1210/jcem.84.6.5793
16. Maghnie M, Strigazzi C, Tinelli C, et al. Growth hormone (GH) deficiency (GHD) of childhood onset: reassessment of GH status and evaluation of the predictive criteria for permanent GHD in young adults. J Clin Endocrinol Metab. 1999;84(4):1324-1328.
https://doi.org/10.1210/jcem.84.4.5614
17. Wacharasindhu S, Cotterill AM, Camacho-Hübner C, Besser GM, Savage MO. Normal growth hormone secretion in growth hormone insufficient children retested after completion of linear growth. Clin Endocrinol (Oxf). 1996;45(5):553556. https://doi.org/10.1046/j.1365-
2265.1996.00850.x
18. Longobardi S, Merola B, Pivonello R, et al. Reevaluation of growth hormone (GH) secretion in 69 adults diagnosed as GH-deficient patients during childhood. J Clin Endocrinol Metab. 1996;81(3):1244-1247. https://doi.org/10.1210/jcem.81.3.8772606
19. Nicolson A, Toogood AA, Rahim A, Shalet SM. The prevalence of severe growth hormone deficiency in adults who received growth hormone replacement in childhood. Clin Endocrinol (Oxf). 1996;44(3):311316. https://doi.org/10.1046/j.1365-
2265.1996.671492.x
20. Iranmanesh A, Lizarralde G, Veldhuis JD. Age and relative adiposity are specific
negative determinants of the frequency and amplitude of growth hormone (GH) secretory bursts and the half-life of endogenous GH in healthy men. J Clin Endocrinol Metab. 1991;73(5):1081-1088. https://doi. org/10.1210/jcem-73-5-1081
21. Kwan AY, Hartman ML. IGF-I measurements in the diagnosis of adult growth hormone deficiency. Pituitary. 2007;10(2):151-157. https://doi.org/10.1007/s11102-007-0028-8
22. Yuen KC, Tritos NA, Samson SL, Hoffman AR, Katznelson L. American Association of Clinical Endocrinologists and American College of Endocrinology disease state clinical review: update on growth hormone stimulation testing and proposed revised cut-point for the glucagon stimulation test in the diagnosis of adult growth hormone deficiency. Endocr Pract. 2016;22(10):12351244. https://doi.org/10.4158/ep161407.dscr
23. Yuen KCJ. Growth hormone stimulation tests in assessing adult growth hormone deficiency. In: Feingold KR, Anawalt B, Boyce A, et al., eds. Endotext. MDText.com, Inc.; November 1, 2019. http://www.ncbi. nlm.nih.gov/books/nbk395585/
24. Rahim A, Toogood AA, Shalet SM. The assessment of growth hormone status in normal young adult males using a variety of provocative agents. Clin Endocrinol (Oxf) 1996;45(5):557-562. https://doi.org/10.1046/ j.1365-2265.1996.00855.x
25. Aimaretti G, Baffoni C, DiVito L, et al. Comparisons among old and new provocative tests of GH secretion in 178 normal adults. Eur J Endocrinol. 2000;142(4):347-352. https://doi.org/10.1530/eje.0.1420347
26. Ghigo E, Bartolotta E, Imperiale E, et al. Glucagon stimulates GH secretion after intramuscular but not intravenous administration. Evidence against the assumption that glucagon per se has a GH-releasing activity. J Endocrinol Invest. 1994;17(11):849854. https://doi.org/10.1007/bf03347790
27. Macrilen (macimorelin) for Oral Solution. US Food & Drug Administration. Published January 31, 2018. Accessed March 14, 2021. https://www.accessdata.fda.gov/drugsatfda_docs/nda/2017/205598Orig1s000TOC. cfm
28. Piccoli F, Degen L, MacLean C, et al. Pharmacokinetics and pharmacody-
namic effects of an oral ghrelin agonist in healthy subjects. J Clin Endocrinol Metab. 2007;92(5):1814-1820. https://doi. org/10.1210/jc.2006-2160
29. Garcia JM, Biller BMK, Korbonits M, et al. Macimorelin as a diagnostic test for adult GH deficiency. J Clin Endocrinol Metab. 2018;103(8):3083-3093. https://doi. org/10.1210/jc.2018-00665
30. Garcia JM, Biller BMK, Korbonits M, et al. Sensitivity and specificity of the macimorelin test for diagnosis of AGHD. Endocr Connect. 2021;10(1):76-83. https://doi. org/10.1530/ec-20-0491
31. FDA approves weekly therapy for adult growth hormone deficiency. News Release. US Food & Drug Administration. Published September 1, 2020. Accessed March 27, 2021. https://www.fda.gov/ drugs/drug-safety-and-availability/fda-approves-weekly-therapy-adult-growth-hormone-deficiency
32. Johannsson G, Gordon MB, Højby Rasmussen M, et al. Once-weekly somapacitan is effective and well tolerated in adults with GH deficiency: a randomized phase 3 trial. J Clin Endocrinol Metab 2020;105(4):e1358-e1376. https://doi. org/10.1210/clinem/dgaa049
33. Burman P, Johansson AG, Siegbahn A, Vessby B, Karlsson FA. Growth hormone (GH)-deficient men are more responsive to GH replacement therapy than women. J Clin Endocrinol Metab. 1997;82(2):550-555. https://doi.org/10.1210/jcem.82.2.3776
34. Cook DM, Ludlam WH, Cook MB. Route of estrogen administration helps to determine growth hormone (GH) replacement dose in GH-deficient adults. J Clin Endocrinol Metab. 1999;84(11):3956-3960. https://doi. org/10.1210/jcem.84.11.6113
35. van Bunderen CC, Lips P, Kramer MH, Drent ML. Comparison of low-normal and high-normal IGF-1 target levels during growth hormone replacement therapy: a randomized clinical trial in adult growth hormone deficiency. Eur J Intern Med 2016;31:88-93. https://doi.org/10.1016/j. ejim.2016.03.026
36. van Bunderen CC, Meijer RI, Lips P, Kramer MH, Serné EH, Drent ML. Titrating growth hormone dose to high-normal IGF-1 levels
21 Vol 13 No 11, February 2023 GP CLINICS Feature
Diagnosis and Management of Growth Hormone Deficiency in Adults
has beneficial effects on body fat distribution and microcirculatory function despite causing insulin resistance. Front Endocrinol (Lausanne). 2021;11:619173. https://doi. org/10.3389/fendo.2020.619173
37. van Bunderen CC, Deijen JB, Drent ML. Effect of low-normal and high-normal IGF-1 levels on memory and wellbeing during growth hormone replacement therapy: a randomized clinical trial in adult growth hormone deficiency. Health Qual Life Outcomes. 2018;16(1):135. https://doi. org/10.1186/s12955-018-0963-2
38. Child CJ, Conroy D, Zimmermann AG, Woodmansee WW, Erfurth EM, Robison LL. Incidence of primary cancers and intracranial tumour recurrences in GH-treated and untreated adult hypopituitary patients: analyses from the Hypopituitary Control and Complications Study. Eur J Endocrinol. 2015;172(6):779-790. https://doi.
TRACK FAST
org/10.1530/eje-14-1123
39. Yuen KC, Heaney AP, Popovic V. Considering GH replacement for GH-deficient adults with a previous history of cancer: a conundrum for the clinician. Endocrine 2016;52(2):194-205. https://doi.org/10.1007/ s12020-015-0840-2
40. DiGiorgio L, Sadeghi-Nejad H. Growth hormone and the fountain of youth. J Sex Med. 2018;15(9):1208-1211. https://doi. org/10.1016/j.jsxm.2018.04.647
41. Bartke A, Darcy J. GH and ageing: pitfalls and new insights. Best Pract Res Clin Endocrinol Metab. 2017;31(1):113-125. https://doi. org/10.1016/j.beem.2017.02.005
42. Aguiar-Oliveira MH, Bartke A. Growth hormone deficiency: health and longevity. Endocr Rev. 2019;40(2):575-601. https://doi. org/10.1210/er.2018-00216
43. Flurkey K, Papaconstantinou J, Miller RA, Harrison DE. Lifespan extension
and delayed immune and collagen aging in mutant mice with defects in growth hormone production. Proc Natl Acad Sci U S A. 2001;98(12):6736-6741. https://doi. org/10.1073/pnas.111158898
44. Liu H, Bravata DM, Olkin I, et al. Systematic review: the safety and efficacy of growth hormone in the healthy elderly. Ann Intern Med. 2007;146(2):104-115. https://doi. org/10.7326/0003-4819-146-2-20070116000005
45. Clemmons DR, Molitch M, Hoffman AR, et al. Growth hormone should be used only for approved indications. J Clin Endocrinol Metab. 2014;99(2):409-411. https://doi. org/10.1210/jc.2013-4187
46. Burgess E, Wanke C. Use of recombinant human growth hormone in HIV-associated lipodystrophy. Curr Opin Infect Dis. 2005;18(1):17-24. https://doi. org/10.1097/00001432-200502000-00004
... page 42
22 GP CLINICS Vol 13 No 11, February 2023
Feature
Lifestyle modifications, such as not lying down for at least 2 hours after eating or drinking, elevating the head of the bed, and weight loss in patients who are overweight or have recently gained weight, should be a component of management.
23 Vol 13 No 11, February 2023 GP CLINICS Appropriate And Smart Prescribing Antibiotic Acute otitis media 23 GP CLINICS Contd. ...
Acute otitis media
24 GP CLINICS Vol 13 No 11, February 2023 Acute otitis media Antibiotic Contd. ...
24
Antibiotic
Acute otitis media
Citation and disclaimer: Web Annex. Infographics. In: The WHO AWaRe (Access, Watch, Reserve) antibiotic book. Geneva: World Health Organization; 2022 (WHO/MHP/HPS/EML/2022.02). Licence: CC BYNC-SA 3.0 IGO. This limited and part material has been reproduced from the above source without any change and for educational purpose only for registered medical practitioners. The objective and intent behind this reproduction is for larger good and is solely to disseminate, update and educate the largest population of practicing Primary Care Doctors (i.e., in India compared in anywhere in the world) to use antibiotics appropriately to help curb the problem of antimicrobial resistance, which is a threat to global health. This piece of reproduction has no commercial interest attached.
25 Vol 13 No 11, February 2023 GP CLINICS
Acute otitis media
25
An Interaction With Experts
What Is Hypoglycemia Unawareness?
Kim A. Carmichael, MD—Series Editor Associate professor of medicine in the Department of Medicine, Division of Endocrinology, Metabolism, and Lipid Research at Washington University School of Medicine in St Louis, Missouri.
Q:How does one diagnose hypoglycemia unawareness?
The phenomenon of hypoglycemia unawareness (which is an impaired sympathoadrenal response) in persons with diabetes mellitus most often is determined by a patient’s history of very low blood glucose levels without immediate clinical symptoms or warning. This may be manifested by bizarre behavior, erratic motor vehicle driving or activities, loss of consciousness, seizures, or even death. The first symptom, often noticed by others, usually is confusion.1 Clinicians, therefore, should question patients about symptoms in conjunction with low recorded glucose numbers, because this is a dangerous condition. When hypoglycemia unawareness occurs during sleep, patients may notice only elevated morning blood glucose levels (the Somogyi effect) due to enhanced counterregulatory effects
to correct for the overnight low levels.
Q:What are the risk factors for hypoglycemia unawareness?
The most common risk factor for hypoglycemia unawareness is hypoglycemia-associated autonomic failure (HAAF), which is a generally reversible metabolic adaptation to frequent hypoglycemia.1,2 HAAF often occurs due to overzealous treatment of hyperglycemia by patients and/or clinicians in an attempt to improve hemoglobin A1c (HbA1c) levels. This adaptation may develop rapidly and has been shown to occur after as few as three 2-hour periods of hypoglycemia within 30 hours.3
Generalized autonomic neuropathy, which may or may not be reversible, also may manifest similarly to HAAF
26 GP CLINICS Vol 13 No 11, February 2023 Diabetes Q&A
but often is accompanied by other autonomic dysfunction symptoms (e.g., gastroparesis, orthostatic hypotension, bladder dysfunction). Inaccurate glucose sampling or determination also may cause erroneous or inaccurate diagnosis (pseudohypoglycemia).
Q:
What conditions may worsen hypoglycemia unawareness?
Hypoglycemia unawareness is more prevalent during sleep and with exercise.2 Patients need to check glucose levels more carefully during these times in order to determine their risk. This may necessitate setting the alarm clock during the sleep interval, which is particularly important if the later morning glucose levels are inexplicably high.
Patients with type 1 diabetes or advanced type 2 diabetes not only may have attenuated hypoglycemia awareness, but also are at risk of having a diminished counterregulatory capacity to correct the hypoglycemia.2
Q:
How does one manage hypoglycemia unawareness?
Like all persons with diabetes, persons with hypoglycemia unawareness should carry a medical alert ID, as well as glucose replacement and injectable glucagon. They should be instructed to always check glucose levels before operating a motor vehicle, maintaining a level greater than 100 mg/dL, and should follow the recommendations by authorities.4,5
The most important part of the long-term management of HAAF is to avoid hypoglycemia, allowing the natural compensatory mechanisms (such as the epinephrine and glucagon responses) to recover. This may take up to 2 weeks for initial responsiveness and 3 months for full recovery.1
What Is Hypoglycemia Unawareness?
In the case of generalized autonomic dysfunction, the target glucose level and HbA1c levels should be increased to a point at which patients are far less likely to become hypoglycemic.
In the event of high morning glucose levels that are rebound effects of overnight low levels, the treatment may be to decrease nocturnal insulin or to change the timing of long-acting basal insulin.
Q:How does one prevent hypoglycemia unawareness?
The first interventions to prevent hypoglycemia unawareness include patient education and dietary intervention.1 Patients should carefully monitor blood glucose levels during exercise and soon after. Medication adjustments may include discontinuation of sulfonylureas or glinides and changing basal and/or mealtime insulins. Insulin pump therapy may be appropriate for some individuals. Many patients also benefit from continuous glucose monitoring, with alarms set to warn for low glucose levels and trends before confusion and other hypoglycemic events occur.
REFERENCES:
1. Seaquist ER, Anderson J, Childs B, et al. Hypoglycemia and diabetes: a report of a workgroup of the American Diabetes Association and the Endocrine Society. J Clin Endocrinol Metab. 2013;98(5): 1845-1859.
2. Cryer PE. Mechanisms of hypoglycemia-associated autonomic failure in diabetes. N Engl J Med. 2013;369(4):362-372.
3. Moheet A, Kumar A, Eberly LE, Kim J, Roberts R, Seaquist ER. Hypoglycemiaassociated autonomic failure in healthy humans: comparison of two vs three periods of hypoglycemia on hypoglycemia-induced counterregulatory and symptom response 5 days later. J Clin Endocrinol Metab. 2014;99(2):664-670.
4. National Highway Traffic Safety Administration. Driver Fitness Medical Guidelines. Publication HS 811 210. http://www.nhtsa.gov/DOT/NHTSA/ Traffic%20Injury%20Control/Articles/Associated%20Files/811210.pdf. Published September 2009. Accessed December 7, 2015.
5. Carmichael KA. What do doctors need to teach their patients with diabetes about driving their vehicles? Consultant. 2014;54(4):271-272.
... page 42
DIABETES Q&A
PPIs are more effective than H2RAs in relieving chronic heartburn and regurgitation and in healing erosive esophagitis. Addition of an H2RA as needed may be beneficial for patients who have symptoms despite twice-daily PPI treatment.
TRACK FAST
Study In 2 Minutes
Alcohol abstinence decreased arrhythmia recurrences in chronic alcoholics with atrial fibrillation
Alcohol abstinence to improve atrial fibrillation



Randomised trial in 140 patients who consumed ≥10 standard drinks per week# and who had paroxysmal or persistent atrial fibrillation in sinus rhythm.
Clinical end points evaluated during the study:
The overall atrial fibrillation burden over 6 months of follow-up was significantly lower in the abstinence group than in the control group (0.5%) (1.2%).
According to the findings of the trial, a substantial reduction in alcohol intake by patients with symptomatic atrial fibrillation was linked with a reduction in the recurrence of atrial fibrillation and a reduction in the percentage of time spent in atrial fibrillation.

Primary end point





Recurrences of atrial fibrillation of more than 30 seconds’ duration (after a 2-week blanking period)
Secondary end point Atrial fibrillation-related hospital admission

% of patients with an atrial fibrillation burden in the abstinence and control groups.
Regular alcohol use is a risk factor for atrial fibrillation that may be controllable. In this study of regular alcohol drinkers with atrial fibrillation, patients randomly assigned to the abstinence group reduced their alcohol consumption from approximately 17 drinks per week to 2 drinks per week and experienced a reduction in both the burden and risk of atrial fibrillation recurrence.
#Standard drink containing approximately 12 g of pure alcohol.
28 GP CLINICS Vol 13 No 11, February 2023
Reference: NEJM 2020;382:20-8.
Abstinence Group Control Group 60 50 40 30 20 10 0 0 0-5 >5
Abstinence
group Control group 50% 50%
Abstinence Group Control Group 53% 73% 9% 20%
Q: Can abstinence from alcohol reduce the incidence and overall burden of atrial fibrillation?
Quick Recap of A Clinical Trial
Dr Amdekar's Revision Notes
Tuberculosis: An Unconquered Disease
Yeshwant K Amdekar, MD, DCH, FIAP* Consultant Pediatrician, Jaslok Hospital and Research Center and Breach Candy Hospital, Mumbai.

*Dr Amdekar is a practicing pediatrician for 50 years and a visiting consultant at SRCC Hospital, Mumbai. He has been a teaching faculty at the Institute of Child Health, Grant Medical College and JJ Group of Hospitals, Mumbai. He has also been the past President of Indian Academy of Pediatrics (IAP) and a member of editorial committee of Indian Pediatrics–the official journal of IAP
ABSTRACT: Robert Koch discovered TB bacillus more than 100 years ago and first anti-TB drug became available more than 60 years ago; but even then tuberculosis has remained unconquered in spite of the advances in diagnostic techniques and drug therapy. This is largely because of failure of rational diagnosis and non-standard therapy on the part of physicians and poor compliance on part of patients. This has resulted in increasing prevalence of MDRTB–multidrug resistant TB. HIV infection has added further threat to control of tuberculosis. Standard protocols for diagnosis are available and so also standard therapeutic regimes. It is the duty of every physician to follow these protocols strictly and ensure compliance on the part of patients.
Key words: childhood tuberculosis, TB diagnosis and therapy
Tuberculosis (TB) is a chronic communicable disease that continues to be a major health problem in India. It is estimated that 5 in 1000 people are infected with Mycobacterium tuberculosis, of which half will present as smear positive. With such a high incidence of TB, it is not surprising that most children acquire the infection from adults in their surroundings. That is why the epidemiology of childhood TB follows that in adults. Consequently, early diagnosis and prompt standardized treatment of childhood TB is very important. Depending on the age at presentation, the symptoms and severity of TB vary, making diagnosis challenging. A proper understanding of the diagnosis and treatment of childhood TB by physicians is essential to limit the spread of the disease.
combination of clinical features has its drawbacks. Fever is often not documented and hence unreliable. Loss of appetite is non-specific and weight records are usually not available to confirm recent weight loss. In addition, a positive contact history is often not available. Besides, TB may present with variable degrees of fever and cough that may be different from the standard presentation. Such atypical presentations are fairly common and merit further discussion. Extrapulmonary TB is more difficult to suspect.
YK Amdekar
STANDARD PRESENTATION OF CHILDHOOD TB
Children can present with TB at any age, but the most common vulnerable age is between 1 and 4 years where serious forms of tuberculosis are more likely including TB meningitis and miliary TB. This is also an age where early diagnosis is a bigger challenge. Unexplained fever and/or cough for 2 weeks or more is highly suggestive of TB (Table 1) especially if it is accompanied by loss of appetite, weight loss and a positive contact history. In addition, failure to respond to broad-spectrum antibiotics and poor nutritional state make a diagnosis of TB even more likely. However, the
THE HOST DECIDES THE PATHOLOGY AND THEREFORE THE CLINICAL PRESENTATION OF TB
Fever in childhood TB varies in acuity, severity and duration. Night fever accompanied by night sweats is typically seen in a malnourished child with an impaired immune response and the fever presents intermittently. An acute onset of high fever that lasts for a few days is a classical presentation in an older child with good nutrition and good immune function. An older child with localized destructive disease or a young child with military disease may present with moderately high continuous fever. Thus, the type of fever relates to the pathology and is suggestive of a particular type of TB.
Cough is an airway disease and depending upon the pathology, the severity of cough varies. A mild, dry cough is characteristic of TB as well as other kinds of upper airway disease. A severe cough suggests significant endobronchial lesion or airway compression by mediastinal lymph nodes. Cough with expectoration is classically seen in chronic cavitary lesions and bronchiectasis in older children. Thus, the severity of cough correlates with the pathology and one can suspect a
29 Vol 13 No 11, February 2023 GP CLINICS
A Way To Clinical Perfection
Table 1 – Algorithm for the diagnosis of childhood tuberculosis
abnormality on physical examination and should be suspected based on history as mentioned above. Fibrocaseous cavitary lesions on physical examination are quite pathognomonic of TB in India although they can be mimicked by fungal infection as well. Similarly, the acute onset of pleural effusion in a healthy older child is highly suggestive of TB in our epidemiology as are miliary lesions with hepatosplenomegaly.
Enlarged peripheral lymph nodes are often found in pulmonary TB in children and are useful clinical correlates to substantiate the diagnosis. However, insignificant cervical lymph nodes are so common and should not be considered in favor of TB. It is the size (often >1-1.5 cm), consistency (firm or matted) and progressive enlargement that suggests diseased lymph nodes.
INVESTIGATIONS
type of disease based on the cough. Other symptoms are very nonspecific and do not help a great deal in the diagnosis of TB. Recent weight loss is only significant if weight records are maintained. Thus, a growth chart is an excellent tool for monitoring general health and the presence of disease. In acute disease of any kind, body weight is lost but quickly regained when the body is back to normal. In contrast, in chronic disease, growth falters over weeks or months and serves as an early indicator of evolving disease even before symptoms develop. Childhood being a growing period, what better way to monitor a
child’s health than by maintaining a growth chart! It is indicative of health and picks up early disease.
PHYSICAL EXAMINATION
Abnormalities in physical examination relate to pathology and not etiology. Thus, there are no classical clinical features of childhood TB. Pneumonia is characteristically the same irrespective of etiology, although chronic persistent pneumonia in spite of treatment with broadspectrum antibiotics raises the strong possibility of it being TB. Pulmonary primary complex is often devoid of any
The gold standard of diagnosis of TB is demonstration of acid-fast bacilli (AFB) in bronchial secretions, sputum or tissue obtained by biopsy such as a lymph node. It is now established that it is possible to confirm bacteriological diagnosis in childhood TB even in the early stage of the disease. Gastric aspirate collected early morning on an empty stomach on three consecutive days offers an easy way to demonstrate AFB. Older children may be able to produce a small sample of sputum for examination under the microscope. However, smears are often negative, as a higher number of bacilli are required to be present in a sample for positive detection. Standard
30 GP CLINICS Vol 13 No 11, February 2023 Tuberculosis: An Unconquered Disease Dr Amdekar's Revision Notes
Table 3 – Disease categories practiced
Category of TB patients Treatment protocol Cat 1 newly diagnosed sputum +ve cases, sputum –ve serious and extensive cases 2HRZE/4HR Cat 2 relapser, defaulter, treatment failure 2HRZES/1HRZE/5HRE Cat 3 Sputum –ve less severe cases, pulmonary primary complex, isolated lymphadenitis, unilateral pleural effusion 2HRZ/4HR H, isoniazid; R, rifampicin; Z, pyrazinamide; E, ethambutol; S, streptomycin. Table 2 – Risk of active disease after natural infection Age group Risk (%) < 1 year 30% - 40% 1-2 years 10% - 20% 2-5 years 5% 5 yearspreadolescent 2% Adolescent 10% - 20%
earlier
Fever and/or cough >2 weeks Look for contact with open case and other factors If +ve, suspect TB If –ve, look for alternate diagnosis Mt test /chest X-ray/gastric aspirate No diagnosis Alternate diagnosis +ve –ve Antibiotic trial for 7-10 days ATT per protocol Treat accordingly Failed trial Consider ATT Observe Better
Dr Amdekar's Revision Notes
Tuberculosis: An Unconquered Disease
bacteriological culture takes a few weeks but faster methods are now available including the BACTEC system that offers results in a few days, especially in the diagnosis of smear-negative TB. Ideally, every attempt should be made to diagnose TB by bacteriology because it is possible and multi-drug resistant TB (MDR-TB) is a threat in every case today. Molecular diagnosis is now available in the form of GeneXpert test that gives results in a few hours, is fairly sensitive and specific and also defines
Clinical highlights
rifampicin sensitivity or resistance. However, it is ideal to order both culture and molecular tests as one of them may be false -ve. Newer tests are now being invented with the idea of improving bacteriological diagnosis.
Supportive evidence is important as bacteriological proof is not possible in every case of childhood TB although an attempt must be made, as mentioned above. The Mantoux tuberculin skin test (TST) suggests whether a person has been infected with TB bacilli but
• It is estimated that 5 in 1000 people are infected with Mycobacterium tuberculosis, of which half will present as smear positive.
• Children can present with TB at any age, but the most common age is between 1 and 4 years.
• Unexplained fever and/or cough for 2 weeks or more is highly suggestive of TB especially if it is accompanied by loss of appetite, weight loss and a positive contact history.
• Fibrocaseous cavitary lesions on physical examination are quite pathognomonic of TB in India though they can be mimicked by fungal infection as well.
• The acute onset of pleural effusion in a healthy older child is highly suggestive of TB in our epidemiology as are miliary lesions with hepatosplenomegaly.
• Enlarged peripheral lymph nodes are often found in pulmonary TB in children and are a useful clinical finding to substantiate diagnosis.
• It is the size (often >1-1.5 cm), consistency (firm or matted) and progressive enlargement that suggests diseased lymph nodes.
• The gold standard of TB diagnosis is demonstration of acid-fast bacilli in bronchial secretions, sputum or tissue obtained by biopsy such as a lymph node by using liquid culture medium as well as GeneXpert PCR test.
• Mantoux tuberculin skin test (TST) is not recommended in the diagnosis of tuberculosis.
• CT scan of the chest is unnecessary, as it does not add any more information than conventional chest X-ray except for localizing necrotic lymph nodes that may be indicative of TB.
• CBC and ESR are not useful either. ESR can be used for monitoring. Serological tests such as TB antibodies (TB IgG, TB IgA) are not dependable and are not recommended for use.
• The RNTCP in India, had recommended a standard protocol of treatment based on three categories that should be followed universally even in children. However, it is no longer recommended and has been replaced with National TB elimination program with simplified treatment approach.
• MDR-TB should be suspected if there is evidence of contact with a known case of MDR-TB or if there is a past history of anti-tuberculosis treatment and should be referred to experts for further treatment.

does not equate to diagnosis of TB disease. The test should be performed with 2 or 5 TU of PPD. An induration of 10 or more millimeters is considered positive and suggests infection but not necessarily disease. Hence, Mt test is not recommended for the diagnosis of TB disease. However, the younger the age and positive tuberculin reaction, the more likely it is active disease (see Table 2). Chest X-ray may be supportive although it is not pathognomonic of TB. However, in our epidemiology, fibrocaceous lesion, miliary shadows, mediastinal enlarged lymph nodes and pleural effusion in a healthy older child are most likely indicative of TB. When in doubt, lateral chest X-ray may help localize the lesion. Decubitus film can confirm the presence of pleural fluid. CT scan of the chest is unnecessary, as it does not add any more information than a conventional chest X-ray except for localizing necrotic lymph nodes that may be indicative of TB. CBC and ESR are not useful either. ESR can be used for monitoring; however, there are better parameters available to judge progress. Serological tests such as TB antibodies (TB IgG, TB IgA) are not dependable and are not recommended for use.
NEWER LABORATORY TESTS FOR DIAGNOSIS
Polymerase chain reaction (PCR) is a highly sensitive method to confirm a clinical diagnosis of TB. However, the high number of false-positives that were found suggests that results obtained should be confirmed with BACTEC, which considerably reduces the time required for identification, and makes it possible to carry out an antibiotic assay rapidly. Moreover, it is positive in 95% of culture +ve cases but only 50% of culture –ve cases. In addition, As mentioned above, GeneXpert test is now readily available so it is routinely employed in the diagnosis of TB. Interferon gamma release assays are not recommended as the sensitivity and specificity of QuantiFERON, QuantiFERON-TB Gold, the T-spot TB test and ELISpot TB test have not been determined in children. Instead of trying newer tests, maybe one should
31 Vol 13 No 11, February 2023 GP CLINICS
Dr
Amdekar's Revision Notes
seek expert advice in difficult cases.
DISEASE CATAGORIES RECOMMENDED NOW
Rifampicin sensitive TB / newly diagnosed TB 2HRZE/4HRE (for neuro and spine TB 2HRZE/8HRE rifampicin resistant TB is suspected in case of relapse, treatment defaulter and one in contact with rifampicin resistant TB such a patient must be referred to an expert as treatment demands use of many more new drugs that are also toxic.
TREATMENT
The Revised National Tuberculosis Control Program (RNTCP) in India, had recommended a standard protocol of treatment based on three categories (Table 3) that should be followed universally even in children. According to the Directly Observed Therapy-short course strategy (DOTS) strategy it is essential to monitor patient compliance to the treatment, as non-adherence is the major factor responsible for the development of MDR-TB. In addition,
patients should receive careful clinical follow-up for two years after completion of a treatment regimen so that any indication of relapse can be diagnosed early and treated promptly. RNTCP has been replaced with NTEP – a national TB elimination program.
Recent National Tuberculosis Elimination Programme recommends only two categories for treatment as mentioned above – RS-TB (Rifampicin sensitive) and RR-TB (Rifampicin resistant TB)
Combination therapy is recommended though ethambutol has to be given separately but the other three drugs are used in fixed drug combination that is available in dispersible tablet form though Ethambutol tablet is not dispersible Drug treatment is available free of charge at the government centers.
MDR-TB should be suspected if there is evidence of contact with a known case of MDR-TB or if there is a past history of anti-tuberculosis
treatment (ATT). An adolescent with cavitary fibrocaseous TB is at a high risk of developing MDR-TB.
HIV testing is not routinely performed in childhood TB except if clinical markers of HIV infection are present, there is a history of HIV in parents or there is a history of blood transfusion. In summary, the diagnosis and treatment of TB should be made according to protocol and compliance must be ensured to prevent the development of MDR-TB.
SUGGESTED READING:
• Arora, VK. Issues in pediatric tuberculosis under DOTS strategy. Indian Pediatr 2004;41:891-893.
• Chauhan LS, Arora VK. Management of pediatric tuberculosis under the revised national tuberculosis control program (RNTCP). Indian Pediatr 2004;41:901-905.
• Kabra SK, Lodha R, Sheth V. Category based treatment of tuberculosis in children. Indian Pediatr 2004;41:927-937.
• Shaheb T, Zoha MS, Malik A, Malik A, Afzal K. Prevalence of human immuno-deficiency virus infection in children with tuberculosis. Indian Pediatr 2004;41:595-599.
• Kabra SK, Lodha R. DOTS in pediatric tuberculosis. Indian Pediatr 2006; 43: 276-278.
CME questions on: Tuberculosis: An Unconquered Disease
Fever in childhood tuberculosis may be:
a) Intermittent
b) High grade
c) Absent
d) All of the above
e) None of the above
Which of the following does not always indicate tuberculosis?
a) Unilateral pleural effusion
b) Fibrocaseous tuberculosis
c) Miliary tuberculosis
d) Pneumonia
e) All of the above
Which of the following tests should be routinely performed?
a) CT scan of chest
b) PCR
c) Gastric aspirate
d) QuantiFERON TB test
e) None of the above
5
Risk of active disease in an asymptomatic Mantoux +ve child is lowest in:
a) Adolescence
b) 2-5 years
c) 5 years to preadolescence
d) 1-2 years
MDR-TB should not be suspected in:
a) HIV +ve
b) Contact with MDR-TB individual
c) Past history of ATT
d) Failure of compliant therapy
1 4 2 3 Scan this QR code for explanatory answers

32 GP CLINICS Vol 13 No 11, February 2023
e) None of the above
Tuberculosis: An Unconquered Disease
An Intravenous Drug Abuser Complains
of Fever, Chills and Cough:
What's the Diagnosis?
Haney Mallemat, MD
Question
A 34 year old male with history of IVDA (intravenous drug abuse) complains of fever, chills and cough. What is your diagnosis?

What's the Diagnosis?
Diagnosis and discussion on the next page
The views expressed in this pearl(s) represent the opinions of the authors. They are provided here for medical education purposes to be used by the registered medical practitioners only. Although the authors have made every effort to provide the most up-to-date evidence-based medical information, these pearl(s) should not necessarily be considered the standard of care and may not reflect individual practices in respective geographic locations. Picture used is for representation purpose only.
The opinions presented in this pearl(s) do not represent the views of the University of Maryland School of Medicine or the Department of Emergency Medicine at the University of Maryland School of Medicine. Though we make every attempt to be accurate in the information we provide, application of this information to any particular clinical scenario is the responsibility of the practitioner.

33 Vol 13 No 11, February 2023 GP CLINICS
Emergency Medicine Educational Pearls
UMEM Pearls
What's the Diagnosis?
Answer
Lung Abscess (from septic pulmonary emboli)

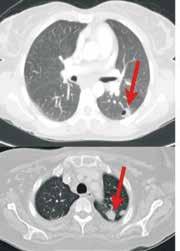

Discussion
• Lung abscess is necrosis of lung parenchyma with pus and debris-filled cavities.
• It is caused by direct injury (e.g., aspiration pneumonia) or secondary causes (e.g., tricuspid endocarditis, bacteremia, etc.).
• Suspect with:
o Loss of airway reflexes (e.g., CVA, seizures, alcohol / narcotic abuse, etc.)
o Poor dentition
o Immunosuppression
o IVDA
• Gram positives, negatives and anaerobic bacteria have all been implicated.
• Chest X-ray may suggest diagnosis, but CT scan better identifies abscess, necrotic tissue, empyema, or other pathology (see image above).
• After drawing blood cultures, broad-spectrum antibiotics should be started and narrowed once culture data is available; address underlying cause (e.g., valve replacement for endocarditis).
• Prognosis is generally good with normal immune function and antibiotics, but mortality sharply increases with immunocompromise and treatment delay.
REFERENCE:
• Mansharamani N, et al. Lung abscess in adults: clinical comparison of immunocompromised to non-immunocompromised patients. Respiratory Medicine. Mar 2002;96(3):178-85
34 GP CLINICS Vol 13 No 11, February 2023
Spot The Diagnosis
Test Your Diagnostic Skills In Dermatology
Quiz # 61 Question
A 56-year-old man has had progressive, erythematous plaques across the forehead and temples for the past few weeks. He describes these areas as “a little itchy and a little tender.” The patient is otherwise healthy and takes no medications.

Which of the following is the most likely cause?
A. Rosacea
B. Seborrheic dermatitis
C. Contact dermatitis
D. Cutaneous lupus
E. Photodermatitis
See answer and discussion on page No 53
35 Vol 13 No 11, February 2023 GP CLINICS






36 GP CLINICS Vol 13 No 11, February 2023




37 Vol 13 No 11, February 2023 GP CLINICS
News and Perspective
Medical Happenings Around the World
ICMR Releases Antimicrobial Guidelines 2022: Update on Doxycycline
The Indian Council of Medical Research (ICMR), one of the oldest medical research bodies in the world, has recently released a revised, updated version of guidelines for antimicrobial treatment in India in the year 2022. The goal of the guideline is to provide medical personnel with a practical guide for treating patients and using antimicrobial agents appropriately.
These 2022 ICMR Guidelines focus on the antibiotic use in common ailments and infections such as acute fever, sepsis, respiratory tract infections, urinary tract infections, central nervous system infections, skin and soft tissue infections, etc. The guidelines recommend the use of doxycycline in various disease conditions. The recommendations on the use of doxycycline are given below.
Acute undifferentiated fever
Empirical treatment with doxycycline for patients with
undifferentiated fever and negative rapid diagnostic tests for malaria and dengue is an option for the clinician.
Short-term prophylaxis of malaria
Doxycycline 100 mg daily in adults and 1.5 mg/kg for children more than 8 years old can be given for short-term prophylaxis of malaria. The drug should be started 2 days before travel and continued for 4 weeks after leaving the malarious area.
38 GP CLINICS Vol 13 No 11, February 2023
ICMR Recommended
Doxycycline as an empirical choice in acute undifferentiated fever
Rickettsial infections and leptospirosis
• Doxycycline is the preferred treatment for rickettsial infections for a duration of 7 days.
• It is also used as a treatment for leptospirosis, for a period of 7 days.
Skin and soft-tissue infections (SSTIs)
Doxycycline, in combination with ciprofloxacin, is the preferred antibiotic for the treatment of necrotizing fasciitis occurred by Aeromonas/V. vulnificus.
Acute febrile encephalopathy (AFE)/ acute encephalitis syndrome (AES)
Initial management includes resuscitation and stabilization based on the clinical condition, followed by clinical evaluation, imaging, and investigations to establish the diagnosis. Empiric therapy (may include ceftriaxone, acyclovir, doxycycline, and artesunate) should be started immediately after drawing blood cultures, pending the results of tests. Supportive care should be continued, and then therapy should be narrowed based on the results of investigations.
Community-acquired pneumonia (CAP)
Doxycycline is the choice of empiric antimicrobial therapy in adult
CAP. It is the preferred drug for:
• Outpatients with co-morbidities* or use of antimicrobial in 3 months
• Inpatient, non-ICU
• Inpatient ICU
• Inpatient ICU with risk factors for Pseudomonas aeruginosa/other enteric gram-negative bacteria.
Urinary tract infections (when culture results are awaited) Doxycycline is a drug of choice for the treatment of epididymo-
orchitis (high risk of being sexually transmitted) in combination with ceftriaxone.
Obstetrics and gynecology
Doxycycline in combination with other antimicrobial agents (AMAs) is preferred for the treatment of:
• Hysterosalpingography (HSG)
• Pelvic inflammatory disease (mild to moderate)
• Pelvic inflammatory disease (severe) e.g., turbo-ovarian abscess, pelvic abscess
Diarrhea
Doxycycline is used to treat diarrhea [300mg (not recommended in children and pregnant women)] for treating V. cholerae.

REFERENCE:
• Treatment guidelines for antimicrobial use in common syndromes 2022. ICMR guidelines.
39 Vol 13 No 11, February 2023 GP CLINICS ICMR Antimicrobial Guidelines 2022: Updates on Doxycycline News and Perspective
Doxycycline is the preferred treatment for rickettsial infections for a duration of 7 days
Doxycycline is the choice of empiric antimicrobial therapy in adult CAP
One Minute Quiz
A Breather To Stay Up To Date
Acute Migraine Treatment in Youth
Q:According to the AAN/AHS guideline on the Acute Treatment of Migraine in Children and Adolescents, during which phase of a migraine attack is acute migraine treatment most effective?
Prodrome A
Aura B
Headache C
Postdrome D
A:Correct answers: A. Prodrome
The guideline states:
1. "Clinicians should counsel that acute migraine treatments are more likely to be effective when used earlier in the migraine attack, when pain is still mild."
2. “Clinicians should prescribe ibuprofen oral solution (OS) (10 mg/kg) as an initial treatment option to reduce pain in children and adolescents with migraine.”
3. “For adolescents with migraine, clinicians should prescribe sumatriptan/naproxen oral tablet (OT) (10/60 mg, 30/180 mg, 85/500 mg), zolmitriptan nasal spray (NS) (5 mg), sumatriptan NS (20 mg), rizatriptan oral disintegrating tablet (ODT) (5 mg or 10 mg), or almotriptan OT (6.25 mg or 12.5 mg) to reduce headache pain.”
Reference:
• AAN/AHS guideline on the Acute Treatment of Migraine in Children and Adolescents, 2019.
40 GP CLINICS Vol 13 No 11, February 2023
mQ1
Top Papers Of The Month
Articles You Don’t Want To Miss
Urinalysis has Pyuria, Leucocyte Esterase—and is Growing Bacteria; Can You Resist the Urge to Treat?
Gregory W. Rutecki, MD
The medical community has repeatedly been cautioned about the negative impact of unrestrained script-writing, particularly when it comes to antibiotics. Yet over and over again, stories surface about too hasty and too generous antibiotic dispensing. A notoriously egregious clinical example is in the treatment of asymptomatic bacteriuria. In 68% of diagnosed cases, patients are inappropriately prescribed antimicrobials. This very high percentage is concerning for (what should be) a very straightforward reason: If a person is without symptoms of a urinary tract infection (asymptomatic means that they are experiencing no frequency, dysuria, urgency, hematuria) the individual should not be screened (urinalysis and additional studies) unless pregnant or about to undergo a urologic procedure with mucosal disruption.1,2
These are the only 2 cohorts who benefit from antibiotic therapy for asymptomatic bacteriuria.
Furthermore, if asymptomatic patients are screened inappropriately and have bacteriuria and pyuria, they should not be treated with antibiotics. This month’s featured “Top Paper” 1 begins with a patient who has neither of the indications for screening and is asymptomatic in regard to his urinary tract. He has pyuria and leucocyte esterase without
symptoms.The patient was chosen wisely by the authors, since he is in his 80s and therapeutically anticoagulated with warfarin. Inappropriate antibiotic(s) administration exposes him to many risks, including bleeding because he is anticoagulated with a Vitamin K antagonist.
Here are the authors’ most salient points:
• Studies performed in nonpregnant women, the elderly, and institutionalized persons without catheters have not demonstrated any benefit of antibiotics in the setting of asymptomatic bacteriuria.
• Treatment of asymptomatic bacteriuria does not decrease the risk of symptomatic infections. In fact, the risk of a symptomatic infection in these folks is slight at most anyway.
• There is no association between asymptomatic carriage of bacteria and kidney function, malignancy, blood pressure, or mortality.
• Treating inappropriately with antibiotics increases the risk of resistant infections or Clostridium difficile later.
• One study suggested that asymptomatic bacteriuria in sexually active young women may be protective in that it decreases colonization by more virulent strains of bacteria.
• In a matter of weeks, I have seen multiple people without urinary tract symptoms treated with antibiotics for any of the following: pyuria, positive urine cultures (significant colonies or not), microscopic hematuria, or a positive leucocyte esterase. I also continue to witness simple, uncomplicated cystitis treated for a week to 10 days with antibiotics when guidelines recommend 3 days only! The costs in terms of money and complications should lead us to a change in this practice. It is high time we listen and learn. ■
Gregory W Rutecki, MD, is a physician at the National Consult Service at the Cleveland Clinic. Dr Rutecki reports that he has no relevant financial relationships to disclose.
REFERENCES:
1.Weiskopf J, Scott S. Asymptomatic bacteriuria, what are you treating? JAMA Intern Med. 2015;175(3):344-345.
2.Lin K, and Fajardo K. US Preventive Services Task Force. Screening for asymptomatic bacteruria in adults: Evidence for the US preventive services task force reaffirmation recommendation statement. An Intern Med. 2008;149:W20-24.
41 Vol 13 No 11, February 2023 GP CLINICS
Drugs In Practice
Critical Review of Drugs Used in Daily Practice
This column carries evidence-based, peer-reviewed evaluations of new FDA-approved drugs with conclusions reached by a consensus of experts, and new information on previously approved drugs including pivotal clinical trials, new indications, and safety warnings. Also, will carry, from time to time, the comparative reviews of drugs for a given indication with particular attention to clinical efficacy, adverse effects and drug interactions.
Drugs for GERD and Peptic Ulcer Disease
GASTROESOPHAGEAL REFLUX DISEASE
Gastroesophageal reflux disease (GERD) is the most common GI condition encountered in the outpatient setting; it affects about 20% of people.
DIAGNOSIS
Heartburn and regurgitation are the clas sic symptoms of GERD. Other symptoms include dyspepsia, chest pain, belching, and chronic cough. Endoscopy is recommended to evaluate alarm signs and symptoms such as dysphagia, GI bleeding, anemia, weight loss, and persistent vomiting. It is also recommended for patients at high risk for complications, including those whose symptoms do not respond adequately to acid suppression, and for those with multiple risk factors for Barrett’s esophagus.1,2
LIFESTYLE MODIFICATION
Lifestyle modifications, such as tobacco cessation, not lying down for at least 2 hours after eating or drinking, and elevating the head of the bed, should be a component of GERD management.3 Weight loss can improve symptoms in patients who are overweight or have recently gained weight.4,5 Routine avoidance of foods that have been associated with reflux, such as chocolate, caffeine, alcohol, and spicy foods, may be helpful, especially for nocturnal symptoms, but is generally not necessary.2
CHOICE OF DRUGS
Drugs that suppress gastric acid are the standard treatment for GERD (see Table 2). The choice of drug depends on the frequency and severity of symptoms and the presence or absence of erosive esophagitis. Patients with infrequent or mild symptoms can be treated with an antacid or H2-receptor antagonist (H2RA) as needed. For patients whose symptoms are inadequately controlled on these agents and those with more frequent or severe symptoms or erosive esophagitis, a proton pump inhibitor (PPI) is recommended.
Key points: drugs for GERD and PUD
GERD
• Lifestyle modifications, such as not lying down for at least 2 hours after eating or drinking, elevating the head of the bed, and weight loss in patients who are overweight or have recently gained weight, should be a component of management.
• As-needed use of an antacid or H2-receptor antagonist (H2RA) is recommended for patients with infrequent or mild symptoms.
• Daily use of a proton pump inhibitor (PPI) is recommended for patients with more frequent or severe symptoms or erosive esophagitis.
• PPIs are more effective than H2RAs in relieving chronic heartburn and regurgitation and in healing erosive esophagitis.
• Addition of an H2RA as needed may be beneficial for patients who have symptoms despite twice-daily PPI treatment.
PUD
• Helicobacter pylori infection and use of nonsteroidal antiinflammatory drugs cause most cases of PUD.
• All patients with PUD should be tested for H. pylori.
• All patients with PUD should be treated with a PPI.
• If the underlying cause of PUD can be identified and eliminated, long-term PPI therapy may not be needed.
• Bismuth quadruple therapy is recommended for first-line treatment of H. pylori infection; rifabutin triple therapy is an alternative.
• Clarithromycin-based therapy should only be used when antimicrobial susceptibility tests have shown that H. pylori is susceptible to clarithromycin or in areas where H. pylori resistance to clarithromycin is known to be <15%.
• All patients should be tested for eradication of H. pylori ≥4 weeks after completion of therapy.
PPIs decrease GERD symptoms and heal esophagitis more effectively than H2RAs and are generally preferred.
ANTACIDS
Antacids containing aluminum, magnesium, and/or calcium carbonate can provide rapid but transient relief of GERD symptoms.
42 GP CLINICS Vol 13 No 11, February 2023
Adverse Effects
Aluminum and calcium carbonate can cause constipation, and magnesium-based antacids can cause diarrhea.
Drug Interactions
Antacids can decrease the absorption of some other drugs (e.g., tetracyclines, levofloxacin) by altering gastric acidity or by binding to other drugs in the GI tract.
Pregnancy
Heartburn occurs commonly during pregnancy; it is largely attributed to a progesterone-mediated decrease in lower esophageal sphincter tone. Antacids can be tried for symptomatic relief, but products containing sodium bicarbonate (may cause metabolic alkalosis and fluid overload) or magnesium trisilicate (long-term use of high doses has been associated with nephrolithiasis, hypotonia, and respiratory distress in the fetus) should be avoided.6
H2-RECEPTOR ANTAGONISTS
H2RAs inhibit the action of histamine at H2 receptors on parietal cells, decreasing basal acid secretion and, to a much lesser extent, food-stimulated acid secretion. H2RAs have a faster onset of action than PPIs, but they are less effective in relieving chronic heartburn and regurgitation and in healing erosive esophagitis,2 and tolerance can develop quickly with continuous use.
Drugs In Practice
Drugs for GERD and Peptic Ulcer Disease
Adverse Effects
Severe adverse effects are uncommon with H2RAs. Hepatic enzyme elevations, hematologic toxicity, and CNS effects such as headache, lethargy, depression, and cognitive impairment have occurred. Cimetidine is weakly antiandrogenic; chronic use may rarely cause reversible impotence and gynecomastia. The FDA has withdrawn all prescription and OTC formulations of ranitidine because they may contain the carcinogen N-nitrosodimethylamine (NDMA).
Drug Omeprazole Equivalent
Pantoprazole 20 mg 4.5 mg
Lansoprazole 15 mg 13.5 mg
Omeprazole 20 mg 20 mg
Esomeprazole 20 mg 32 mg
Rabeprazole 20 mg 36 mg
Dexlansoprazole 30 mg2 50-60 mg
1. Based on the percentage time gastric pH is >4 over a 24-hour period with once-daily dosing. Adapted from DY Graham and A Tansel. Clin Gastroenterol Hepatol 2018; 16:800.
2. Compared to twice-daily use of other PPIs, once-daily dexlansoprazole is less "potent".
43 Vol 13 No 11, February 2023 GP CLINICS
Table 1 – Relative Potency of PPIs1
Drugs In Practice
Drugs for GERD and Peptic Ulcer Disease
Table 2 – Some oral drugs for GERD and PUD
ODTs = orally disintegrating tablets; OTC = over the counter; soln = solution; susp = suspension
1 The lower end of the range is generally used for initial treatment of GERD. Higher or more frequent doses may be needed for patients with erosive esophagitis, peptic ulcer disease, hypersecretory conditions such as Zollinger-Ellison syndrome, or for treatment of H. pylori infection. Dosage adjustments may be needed for renal or hepatic impairment.
2. In April 2020, the FDA requested that all OTC and prescription ranitidine products be removed from the market because they may contain the carcinogen N-nitrosodimethylamine (NDMA).
3. Taking the total daily dose in the evening may also be effective.
4. Also available in combination with ibuprofen.
5. PPIs are generally taken 30-60 minutes before the first meal of the day. Taking one dose before the evening meal or taking the drug twice daily may be more effective for nocturnal acid control. PPIs should generally be swallowed whole and should not be crushed or chewed. Dexlansoprazole can be taken with or without food. Omeprazole/sodium bicarbonate should be taken on an empty stomach at least 1 hour before a meal.
6. Capsules can be opened and their contents sprinkled on soft food such as applesauce and consumed immediately.
7. Also available in combination with naproxen.
8. Also available in combination with amoxicillin/clarithromycin.
9. Immediate-release formulation of omeprazole. Should be used with caution in patients on a low-sodium diet.
10. Since each capsule contains 1.1 g of sodium bicarbonate, two 20-mg capsules are not equivalent to one 40-mg capsule.
11. FDA-approved only for prevention of NSAID-induced gastric ulcers.
12. Also available in combination with diclofenac (Arthrotec, and generics).
13. FDA-approved only for short-term treatment and maintenance therapy of duodenal ulcers.
14. Should be taken on an empty stomach.
Drug Interactions
H2RAs can decrease serum concentrations of drugs that require gastric acidity for absorption, such as itraconazole and the antiretroviral drugs rilpivirine and atazanavir. Cimetidine is a moderate inhibitor of CYP1A2, 2C19, and 2D6; it can increase serum concentrations of drugs that are metabolized by these enzymes, such warfarin and fluoxetine.7 Famotidine and nizatidine are less likely to affect the hepatic metabolism of other drugs.
Pregnancy
H2RAs are generally considered safe for use during pregnancy, but adequate studies are lacking.
PROTON PUMP INHIBITORS
PPIs bind to the activated proton pump on the apical membrane of parietal cells, resulting in variably potent inhibition of acid secretion into the gastric lumen (see Table 1). They are more effective than H2RAs in relieving
44 GP CLINICS Vol 13 No 11, February 2023
Drug Some Available Oral Formulations Usual Adult Dosage1 H2-Receptor Antagonists (H2RAs)2 Cimetidine – generic 200, 300, 400, 800 mg tabs; 300 mg/5 mL soln 200-400 mg PO bid3 Famotidine4 – generic 20, 40 mg tabs; 40 mg/5 mL susp 20-40 mg PO bid3 Nizatidine – generic 150, 300 mg caps; 15 mg/mL soln 150 mg PO bid3 Proton Pump Inhibitors (PPIs)5 Dexlansoprazole – generic 30, 60 mg delayed-release caps6 30-60 mg PO once/day Esomeprazole magnesium7 – generic 20, 40 mg delayed-release caps6 20-40 mg PO once/day Lansoprazole – generic 15, 30 mg delayed-release caps6; 15, 30 mg ODTs 15-30 mg PO once/day Omeprazole8 – generic 10, 20, 40 mg delayed-release caps6 20-40 mg PO once/day Omeprazole/sodium bicarbonate9 – generic 20/1680, 40/1680 mg/packets for susp; 20 mg/1.1 g, 40 mg/1.1 g caps10 20-40 mg PO once/day Pantoprazole – generic 20, 40 mg delayed-release tabs 20-40 mg PO once/day Rabeprazole – generic 20 mg delayed-release tabs 10-20 mg PO once/day Others Misoprostol11,12 – generic 100, 200 mcg tabs 200 mcg PO bid, tid, or qid Sucralfate13 – generic Carafate 1 g tabs; 1 g/10 mL susp 1 g PO qid14
chronic heartburn and regurgitation and in healing erosive esophagitis. Treatment with a PPI for 8 weeks is recommended for healing of erosive esophagitis.2 Almost all patients with erosive esophagitis will have a relapse of symptoms within 6 months of stopping the PPI and most will require long-term maintenance therapy.
PPIs have short serum half-lives, but their duration of action is longer than that of H2RAs, allowing for oncedaily dosing in most patients with GERD. For patients who continue to have symptoms, switching to twice-daily dosing is more effective than increasing the dose.8 Addition of an H2RA as needed may be helpful for patients who still have symptoms despite twice-daily PPI treatment.
PPIs generally are most effective when taken on an empty stomach, 30-60 minutes before a meal. Dexlansoprazole can be taken without regard to meals. Other antisecretory drugs such as H2RAs should not be taken at the same time as a PPI. Unlike H2RAs, tolerance to PPIs does not develop with continuous use.
Adverse Effects
Short-term use of PPIs is generally well tolerated. Headache, nausea, abdominal pain, constipation, flatulence, and diarrhea can occur. Gynecomastia, hepatic failure, subacute myopathy, arthralgia, severe rash, lupus erythematosus, and acute interstitial nephritis have been reported.
In observational studies, long-term PPI use has been associated with a number of safety concerns, including dementia, vitamin B12 deficiency, chronic kidney disease, and increased all-cause mortality.9,10 Most of these concerns are not supported by a causal mechanism or consistent data. The FDA has issued safety warnings about an association between long-term PPI use and hypomagnesemia, increased fracture risk, and Clostridioides difficile infection. In a population-based cohort study in new users of PPIs and H2RAs, use of PPIs was associated with a 45% greater risk of gastric cancer, but the absolute risk was low.11 The benefits of PPI treatment generally outweigh the risks in patients with a clear indication for long-term treatment.12
Drug Interactions
PPIs may decrease serum concentrations of drugs that require gastric acidity for absorption, such as itraconazole and the antiretroviral drugs rilpivirine and atazanavir.
Most PPIs are metabolized primarily by CYP2C19. Patients who are CYP2C19 ultra-rapid metabolizers may have a decreased response to PPI treatment, and poor metabolizers (many Asian patients) may have higher PPI serum concentrations.13 Lansoprazole and dexlansoprazole are metabolized primarily by CYP3A4. Omeprazole and esomeprazole are moderate inhibitors of CYP2C19 and could increase serum concentrations of drugs metabolized by this pathway, such as warfarin and phenytoin.7,14
The antiplatelet drug clopidogrel is converted to its active form by CYP2C19; inhibition of CYP2C19 may interfere
Drugs In Practice
Drugs for GERD and Peptic Ulcer Disease
with its activation. Whether concurrent use of clopidogrel and a PPI results in clinically significant adverse cardiovascular outcomes is not clear.15,16 Since omeprazole and esomeprazole appear to be most likely to reduce the antiplatelet activity of clopidogrel and the FDA specifically warns against their concomitant use, it would be prudent to choose another PPI in patients taking clopidogrel.17
Pregnancy
PPIs are generally considered safe for use during pregnancy, but clinical data are limited. In a metaanalysis of 7 observational studies, first trimester PPI use (predominantly omeprazole) was not associated with an increased risk of congenital malformations.18 A cohort study produced similar findings.19
ALGINATE
A polysaccharide derived from brown algae, alginate forms a floating foam/gel that acts as a physical barrier between gastric contents and the lower esophagus. In one randomized, placebocontrolled trial, addition of an alginate-based product improved symptoms in patients who had heartburn or regurgitation despite standard-dose PPI treatment.20 Alginatebased products contain aluminum hydroxide and magnesium carbonate. Alginate-based and other products available in many countries contain larger amounts of alginate.
ANTIREFLUX SURGERY
In patients with PPIrefractory and reflux-related chronic heartburn, antireflux surgery is an effective alternative to long-term pharmacologic treatment.21
PEPTIC ULCER DISEASE
Peptic ulcer disease (PUD) is most commonly caused by Helicobacter pylori infection. Use of nonsteroidal antiinflammatory drugs (NSAIDs), including aspirin, is another common cause. Eradication of H. pylori can promote ulcer healing and prevent recurrence of gastric and duodenal ulcers.22 It may also reduce the risk of gastric cancer in those who have a family history of the disease.23
PPI Treatment
All patients with PUD should be treated with a PPI for ulcer healing. If the underlying cause of PUD is identified and addressed (stopping the NSAID or eradicating H. pylori), long-term PPI treatment may not be needed. Long-term PPI treatment is recommended for patients with NSAIDinduced PUD who are unable to stop taking NSAIDs (fixed-dose NSAID/PPI combinations are available for such patients) and for those whose PUD is not caused by H. pylori or NSAIDs.12
DIAGNOSIS OF H. pylori
Many diagnostic tests are available to identify H. pylori infection.24, 25
45 Vol 13 No 11, February 2023 GP CLINICS
Drugs In Practice
Table 3 – Preferred regimens for Helicobacter pylori infection1
Drug Usual Adult Dosage2 Comments
Empiric Treatment
Bismuth Quadruple Therapy3
Bismuth subsalicylate4 + metronidazole + tetracycline5 + a PPI
Rifabutin Triple Therapy7
Rifabutin + amoxicillin + esomeprazole or rabeprazole
Susceptibility-Based Treatment
Clarithromycin Triple Therapy
Clarithromycin8 + amoxicillin + a PPI
Levofloxacin Triple Therapy
Levofloxacin + amoxicillin + a PPI
Metronidazole Triple Therapy
Metronidazole + amoxicillin + a PPI
PPI = proton pump inhibitor
262 or 525 mg PO qid
500 mg PO qid
500 mg PO bid or qid
See footnote6
150 mg bid
1 g tid 40 mg bid
• Preferred first-line option
• Alternative first-line option
• Can be used in treatment-naive patients or for salvage treatment
500 mg PO bid
1 g PO bid
See footnote6
500 mg PO once/day
1 g PO bid
See footnote6
500 mg PO once/day
1 g PO bid
See footnote6
1. Adapted from Y-C Lee et al. Annu Rev Med 2022; 73:183.
2. The optimal duration of treatment is 14 days.
• Should only be used in patients who reside in areas where clarithromycin resistance is <15% and in patients with no prior macrolide exposure for any indication9
• Levofloxacin resistance is a concern
• Metronidazole resistance is a concern
3. The fixed-dose combination of bismuth subcitrate 140 mg, metronidazole 125 mg, and tetracycline 125 mg can be used, but it is only packaged as a 10-day supply; dosage is 3 capsules qid.
4. Or bismuth subcitrate 120-300 mg.
5. Generic tetracycline may not be available.
6. Esomeprazole 20 mg bid, lansoprazole 45 mg bid, omeprazole 40 mg bid, pantoprazole 40 mg bid, or rabeprazole 20 mg bid.
7. A fixed-dose combination of rifabutin 12.5 mg, omeprazole 10 mg, and amoxicillin 250 mg is available.
8. Clarithromycin may increase the risk of cardiac adverse effects and death in patients with coronary artery disease (FDA Drug Safety Communication, February 2018).
9. Clarithromycin resistance rates are considered to be ≥15% unless local resistance patterns that show otherwise are available.
Urea Breath Tests
A urea breath test can be used for clinic-based diagnosis of active infection and confirmation of eradication. These tests typically have >90% sensitivity and specificity, and results are available within 10-20 minutes, but they require use of a mass spectrophotometer.
Stool Antigen Tests
Stool antigen enzyme immunoassay (EIA) testing also has >90% sensitivity and specificity and can test for active infection and eradication. It does not require special equipment and may be less expensive than urea breath tests. Stool samples can be used for molecular testing to determine antimicrobial susceptibility.
Serology
Serologic antibody tests for H. pylori lack sensitivity and specificity and do not differentiate between active and past infection. They cannot be used to confirm H. pylori eradication.
Endoscopy with Biopsy
H. pylori can be diagnosed from endoscopic biopsies using urease testing, histopathology, or culture. Urease testing of biopsy specimens has >90% sensitivity and specificity. Rapid tests are available that provide results in one hour. Histologic diagnosis from biopsy specimens has >95% sensitivity and specificity, but it takes longer and is more expensive than urease testing. Culture permits
46 GP CLINICS Vol 13 No 11, February 2023
Drugs for GERD and Peptic Ulcer Disease
testing for antimicrobial susceptibility.
Drug Interference
The sensitivity of urea breath tests, stool antigen tests, and urease testing of biopsy specimens for H. pylori is reduced by use of PPIs, bismuth-containing products, and antibiotics. Patients should not take a PPI for at least 1-2 weeks or a bismuth-containing product or antibiotics for at least 4 weeks before these tests.
ERADICATION OF H. pylori
Preferred regimens for eradication of H. pylori infection are listed in Table 3.
In clinical trials, combinations of antibacterial drugs have been successful in eradicating H. pylori , but in clinical practice, eradication rates have been lower because of bacterial resistance and poor patient adherence to multidrug regimens. Local resistance patterns and antimicrobial susceptibility testing should guide the selection of antibacterial drugs, but they are not readily available.
Bismuth quadruple therapy (bismuth, metronidazole, tetracycline, and a PPI) is recommended for first-line treatment of H. pylori infection. 26 H. pylori resistance to tetracycline is rare, and adequate dosing of metronidazole can be effective even in the presence of in vitro resistance. 27
Rifabutin triple therapy (rifabutin, amoxicillin, and a PPI) is an alternative option for empiric treatment of H. pylori infection. A fixed-dose combination of omeprazole, amoxicillin, and rifabutin eradicated H. pylori in about 80% of treatmentnaive patients in two small clinical trials and is FDA-approved for treatment of H. pylori infection in adults.28 Rifabutin-based triple therapy has not been compared directly to other regimens for firstline treatment of H. pylori infection in adults. Rates of H. pylori resistance to rifabutin have been low; whether more widespread use as part of a first-line regimen would increase resistance rates remains to be determined.
The efficacy of clarithromycin against H. pylori has been diminished by increasing antimicrobial resistance. Regimens containing clarithromycin should be used for first-line treatment only when antimicrobial susceptibility tests have shown that H. pylori is susceptible to the drug or in patients who have no history of macrolide use for any indication and reside in areas where H. pylori resistance to clarithromycin is known to be <15%. Limited data are available on H. pylori resistance rates; they should be assumed to be ≥15% unless local resistance patterns show otherwise.
Adequate acid suppression with a PPI is associated with higher H. pylori cure rates. A higher intragastric pH improves antibiotic stability and bioavailability, resulting in higher drug concentrations. It also promotes H. pylori replication, making it more susceptible to antibiotic treatment. The potency of PPIs in maintaining a higher
Drugs In Practice
Drugs for GERD and Peptic Ulcer Disease
gastric pH varies from drug to drug (see Table 1). 8 PPIs should be given twice daily (30-60 minutes before breakfast and dinner) for treatment of H. pylori infection. Dexlansoprazole can be given without regard to meals. Some experts recommend using high PPI doses (e.g., omeprazole 40 mg bid) for H. pylori eradication, especially in patients who are CYP2C19 ultra-rapid metabolizers. 29
TREATMENT FAILURE
Testing for eradication of H. pylori should be performed at least 4 weeks after completion of therapy. Patients who are still infected should be treated with a different regimen. Bismuth quadruple therapy can be used in patients who initially received a regimen containing clarithromycin. Those who were initially treated with bismuth quadruple therapy can receive rifabutin triple therapy.
OTHER DRUGS
Sucralfate, an aluminum hydroxide complex of sucrose thought to act locally to protect ulcers from exposure to pepsin and gastric acid, has been used to heal peptic ulcers and as maintenance treatment to prevent recurrence. It may not be effective in relieving ulcer pain, must be taken multiple times per day, and can reduce the absorption of drugs taken concomitantly.
Misoprostol, a prostaglandin E1 analog, can prevent and heal gastroduodenal ulcers in patients taking NSAIDs chronically, but it requires multiple daily doses and is not well tolerated.
Vonoprazan, a potassium-competitive acid blocker that has not been approved by the FDA to date, but has been available in Japan since 2014 for treatment of gastric and duodenal ulcers and eradication of H. pylori . It is more rapidly absorbed, achieves a higher intragastric pH, and has a substantially longer duration of action (half-life 7.7 hours) than conventional PPIs.30 It appears to be more effective than conventional PPIs in eradicating H. pylori , with similar adverse effects. 31
ADVERSE EFFECTS
The most common adverse effects associated with use of antibacterial drugs for treatment of H. pylori are diarrhea, nausea, vomiting, anorexia, and abdominal pain.
Bismuth subsalicylate can temporarily turn the tongue and stool black and can cause tinnitus. Metronidazole frequently causes a metallic taste and might cause a disulfiram-like reaction to alcohol; neurologic adverse effects, including seizures and neuropathy, have also been reported, particularly at high doses. Tetracyclines can cause GI adverse effects, vaginal candidiasis, photosensitivity, intracranial hypertension, and hyperpigmentation. Use of tetracyclines during tooth development (second and third trimesters of pregnancy, children ≤8 years old) can result in permanent discoloration of teeth. Because of their adverse effects on tooth and bone development,
47 Vol 13 No 11, February 2023 GP CLINICS
Drugs In Practice
Drugs for GERD and Peptic Ulcer Disease
tetracyclines should not be used during pregnancy or in children ≤8 years old. Levofloxacin can cause severe hypoglycemia, delirium, agitation, nervousness, and disturbances in attention, memory, and orientation. It can also cause persistent or permanent peripheral neuropathy and an increased risk of pseudotumor cerebri syndrome. Tendinitis, tendon rupture, exacerbation of myasthenia gravis, C. difficile infection, and QT-interval prolongation and torsades de pointes can also occur. Rifabutin can cause brown-orange discoloration of urine, feces, saliva, sputum, perspiration, tears, and skin. It can rarely cause myelotoxicity (generally with higherthanrecommended doses or prolonged use) and uveitis. Serious, sometimes fatal, hypersensitivity reactions and C. difficile infection has been reported with use of rifabutin. Clarithromycin commonly causes taste disturbances that some patients find intolerable, and it can cause QT-interval prolongation. 32 The labeling of clarithromycin contains a warning about an increased risk of cardiac adverse events and death in patients with coronary artery disease.33
Sucralfate is generally well tolerated, but patients often complain about its metallic taste. It can cause constipation and, particularly in patients with renal impairment, aluminum toxicity. Abdominal pain and dose-related diarrhea, which can be severe, are the most common adverse effects of misoprostol. Severe nausea, dyspepsia, and flatulence can also occur.
DRUG INTERACTIONS
Metronidazole is an inhibitor of CYP2C9 and may increase serum concentrations of drugs metabolized by this isozyme, including warfarin. Coadministration of products containing calcium, magnesium, or iron can decrease absorption of tetracycline and levofloxacin; either should be taken 2 hours before or 6 hours after these products. Rifabutin is an inducer of CYP3A4, 2C8 and 2C9 and can reduce serum concentrations of drugs that are metabolized by these isozymes. Clarithromycin is a strong inhibitor of CYP3A4 and P-glycoprotein (P-gp) and may increase serum concentrations of drugs that are CYP3A4 or P-gp substrates. 7 Taking clarithromycin with other drugs that prolong the QT interval, especially those metabolized by CYP3A4, can increase the risk of QTinterval prolongation and torsades de pointes. 33 Sucralfate decreases the absorption of many other drugs, including fluoroquinolones, tetracyclines, and levothyroxine; administration should be separated by at least 2 hours.
PREGNANCY
Bismuth subsalicylate is converted to bismuth and salicylic acid in the GI tract. Bismuth is minimally absorbed. The FDA has required new warnings in the labels of NSAIDs, including aspirin, advising against their use during pregnancy beginning at 20 weeks’ gestation because of a risk of fetal renal dysfunction that
could lead to low amniotic fluid levels and neonatal renal impairment. NSAIDs can cause premature closure of the ductus arteriosus and persistent neonatal pulmonary hypertension when used after 30 weeks’ gestation.34 Metronidazole is generally considered safe for use during pregnancy. An association between metronidazole exposure in utero and development of cleft lip was observed in one case-control study, but this finding has not been replicated in numerous other observational studies and meta-analyses. 35 Tetracyclines can cause fetal harm and reversible inhibition of bone growth when taken during pregnancy. Levofloxacin also should generally be avoided during pregnancy if possible. Fluoroquinolones have caused arthropathy in animal studies, but observational data in pregnant women suggest that teratogenic effects are unlikely to occur at therapeutic doses. Rifabutin and clarithromycin are generally not recommended for use during pregnancy. Sucralfate is minimally absorbed and does not appear to be associated with adverse fetal outcomes. Misoprostol is an abortifacient and should not be used in women who are or could become pregnant.
REFERENCES:
1. J Maret-Ouda et al. Gastroesophageal reflux disease: a review. JAMA 2020;324:2536.
2. PO Katz et al. ACG clinical guideline for the diagnosis and management of gastroesophageal reflux disease. Am J Gastroenterol 2022;117:27.
3. E Ness-Jensen et al. Lifestyle intervention in gastroesophageal reflux disease. Clin Gastroenterol Hepatol 2016;14:175.
4. M Singh et al. Weight loss can lead to resolution of gastroesophageal reflux disease symptoms: a prospective intervention trial. Obesity (Silver Spring) 2013;21:284.
5. E Ness-Jensen et al. Weight loss and reduction in gastroesophageal reflux. A prospective population-based cohort study: the HUNT study. Am J Gastroenterol 2013;108:376.
6. C Body and JA Christie. Gastrointestinal disease in pregnancy: nausea, vomiting, hyperemesis gravidarum, gastroesophageal reflux disease, constipation, and diarrhea. Gastroenterol Clin North Am 2016;45:267.
7. Inhibitors and inducers of CYP enzymes, P-glycoprotein, and other transporters. Med Lett Drugs Ther 2021 October 20 (epub). Available at: http://secure.medicalletter.org/downloads/CYP_PGP_Tables.pdf.
8. DY Graham and A Tansel. Interchangeable use of proton pump inhibitors based on relative potency. Clin Gastroenterol Hepatol 2018;16:800.
9. Safety of long-term PPI use. Med Lett Drugs Ther 2017;59:131.
10. MF Vaezi et al. Complications of proton pump inhibitor therapy. Gastroenterology 2017;153:35.
11. D Abrahami et al. Proton pump inhibitors and risk of gastric cancer: population-based cohort study. Gut 2022;71:16.
12. DE Freedberg et al. The risks and benefits of long-term use of proton pump inhibitors: expert review and best practice advice from the American Gastroenterological Association. Gastroenterology 2017;152:706.
13. T Furuta et al. Influence of CYP2C19 pharmacogenetic polymorphism on proton pump inhibitor-based therapies. Drug Metab Pharmacokinet 2005; 20:153.
14. RS Wedemeyer and H Blume. Pharmacokinetic drug interaction profiles of proton pump inhibitors: an update. Drug Saf 2014;37:201.
15. SA Scott et al. Antiplatelet drug interactions with proton pump inhibitors. Expert Opin Drug Metab Toxicol 2014;10:175.
16. SD Bouziana and K Tziomalos. Clinical relevance of clopidogrel-proton pump inhibitors interaction. World J Gastrointest Pharmacol Ther 2015;6:17.
17. Drug interaction: clopidogrel and PPIs. Med Lett Drugs Ther 2017;59:39.
18. SK Gill et al. The safety of proton pump inhibitors (PPIs) in pregnancy: a meta-analysis. Am J Gastroenterol 2009;104:1541.
19. B Pasternak and A Hviid. Use of proton-pump inhibitors in early pregnancy
48 GP CLINICS Vol 13 No 11, February 2023
and the risk of birth defects. N Engl J Med 2010;363:2114.
20. C Reimer et al. Randomised clinical trial: alginate (Gaviscon Advance) vs. placebo as add-on therapy in reflux patients with inadequate response to a once daily proton pump inhibitor. Aliment Pharmacol Ther 2016;43:899.
21. SJ Spechler et al. Randomized trial of medical versus surgical therapy for refractory heartburn. N Engl J Med 2019;381:1513.
22. AC Ford et al. Eradication therapy for peptic ulcer disease in Helicobacter pylori-positive people. Cochrane Database Syst Rev 2016;4:CD003840.
23. IJ Choi et al. Family history of gastric cancer and Helicobacter pylori treatment. N Engl J Med 2020;382:427.
24. MP Dore et al. Dyspepsia: when and how to test for Helicobacter pylori infection. Gastroenterol Res Pract 2016;2016:8463614.
25. 25. Y-C Lee et al. Diagnosis and treatment of Helicobacter pylori infection. Annu Rev Med 2022;73:183.
26. WD Chey et al. ACG clinical guideline: treatment of Helicobacter pylori infection. Am J Gastroenterol 2017;112:212.
27. SC Shah et al. AGA clinical practice update on the management of refractory Helicobacter pylori infection:expert review. Gastroenterology 2021;160:1831.
Drugs In Practice
Drugs for GERD and Peptic Ulcer Disease
28. Talicia – a 3-drug combination for Helicobacter pylori infection. Med Lett Drugs Ther 2020;62:83.
29. P Malfertheiner et al. Management of Helicobacter pylori infection–the Maastricht V/Florence consensus report. Gut 2017;66:6.
30. DY Graham and MP Dore. Update on the use of vonoprazan: a competitive acid blocker. Gastroenterology 2018;154:462.
31. S Shinozaki et al. Effectiveness and safety of vonoprazan versus proton pump inhibitors for second-line Helicobacter pylori eradication therapy: systematic review and meta-analysis. Digestion 2021;102:319.
32. RL Woosley et al. QT drugs list. Available at: www. crediblemeds.org. Accessed March 17, 2022.
33. FDA Drug Safety Communication: FDA review finds additional data supports the potential for increased long-term risks with antibiotic clarithromycin (Biaxin) in patients with heart disease. February 22, 2018. Available at: https://bit.ly/35m8rBk. Accessed March 17, 2022.
34. In brief: New warnings on NSAID use in pregnancy. Med Lett Drugs Ther 2020;62:175.
35. O Sheehy et al. The use of metronidazole during pregnancy: a review of evidence. Curr Drug Saf 2015;10:170.
TRACK FAST
49 Vol 13 No 11, February 2023 GP CLINICS
If a person is without symptoms of a urinary tract infection (asymptomatic means that they are experiencing no frequency, dysuria, urgency, hematuria) the individual should not be screened (urinalysis and additional studies) unless pregnant or about to undergo a urologic procedure with mucosal disruption.
... page 41
Drugs In Practice
Drugs for GERD and Peptic Ulcer Disease
QUICK RECAP: CME QUESTIONS ON "DRUGS IN PRACTICE" IN THIS ISSUE
1. Lifestyle modifications for treatment of gastroesophageal reflux disease (GERD) include:
a. weight loss in patients who are overweight
b. not lying down for at least 2 hours after eating or drinking
c. elevating the head of the bed
d. all of the above
2. Which of the following is generally preferred for treatment of erosive esophagitis in GERD?
a. an H2-receptor antagonist (H2RA)
b. a proton pump inhibitor (PPI)
c. a magnesium-based antacid
d. a calcium carbonate-based antacid
3. Compared to PPIs, H2RAs:
a. have a faster onset of action
b. have a longer duration of action
c. are less likely to lose efficacy because of development of tolerance
d. all of the above
4. A 36-year-old woman with erosive esophagitis taking a standard dose of a PPI once daily for the past 4 weeks still has symptoms. Which of the following should you recommend first?
a. switch to twice-daily dosing of the PPI
b. switch to an H2RA
c. add an H2RA
d. add sucralfate
5. A 20-mg dose of rabeprazole is equivalent to what dose of omeprazole?
a. 15 mg
b. 20 mg
c. 36 mg
d. 60 mg
6. The FDA has issued safety warnings about an association between long-term PPI use and:
a. hypomagnesemia
b. vitamin B12 deficiency
c. all-cause mortality
d. all of the above
7. All patients with peptic ulcer disease should be treated with:
a. an antacid
b. an H2RA
c. a PPI
d. sucralfate
8. Which of the following regimens is preferred for empiric treatment of Helicobacter pylori infection?
a. clarithromycin triple therapy
b. bismuth quadruple therapy
c. levofloxacin triple therapy
d. metronidazole triple therapy
9. Which of the following statements about the use of clarithromycin is true?
a. its efficacy in eradicating H. pylori has been diminished by increasing antimicrobial resistance
b. it has been associated with an increased risk of adverse cardiac effects in patients with coronary artery disease
c. it can increase serum concentrations of drugs metabolized by CYP3A4
d. all of the above
10. Misoprostol can prevent and heal gastroduodenal ulcers in patients who must take NSAIDs chronically, but it:
a. requires multiple daily doses
b. can cause severe GI toxicity
c. is an abortifacient
d. all of the above
50 GP CLINICS Vol 13 No 11, February 2023
1. d. all of the above 2. b. a proton pump inhibitor (PPI) 3. a. have a faster onset of action 4. a. switch to twice-daily dosing of the PPI 5. c. 36 mg 6. a. hypomagnesemia 7. c. a PPI 8. b. bismuth quadruple therapy 9. d. all of the above 10. d. all of the above
Answers:
What’s The “Take Home”?®
A 78-Year-Old Woman With a Newly Discovered Significant Heart Murmur
Ronald Rubin, MD—Series Editor
A78-year-old woman has moved to your area in order to be closer to her children, and she presents as a new patient to your practice.
HISTORY
She has been quite healthy all of her life, without significant major medical diagnoses. Specifically, she has no history of diabetes, hypertension, or chronic obstructive pulmonary disease. She has never smoked. Her most recent interaction with the health system was an uneventful hip replacement 5 years ago. She uses nonsteroidal antiinflammatory drugs sporadically for joint soreness.
Review of systems is negative for chest pain, dyspnea on exertion, paroxysmal nocturnal dyspnea, or edema. She is active and can easily climb 2 flights of steps without symptoms. She does report being told of a heart murmur years ago that “could just be monitored.”
PHYSICAL EXAMINATION
Physical examination reveals a healthy-appearing woman with a pulse of 84 beats/min and a blood pressure of 114/75 mm Hg. Findings of examination of the head, eyes, ears, nose, and throat are unremarkable. Her chest is clear to percussion and auscultation. A coarse, holosystolic, rasping murmur is loudest at the cardiac base and radiates into the neck. There is delay and blunting of the carotid pulsations. There is no gallop rhythm. Her joints are normal, and she has no pedal edema.
Correct Answer: D
This case is an entry into the clinical presentation, diagnostic evaluation, and management of valvular aortic stenosis (AS), a very important and common condition today.
VALVULAR AORTIC STENOSIS
Valvular AS is a progressive disease wherein obstruction of left ventricular outflow eventually causes inadequate cardiac output (syncope), left ventricular hypertrophy with relative ischemia with effort (angina), and congestive heart failure (CHF). Those 3 clinical findings are the cardinal symptoms of advanced AS, but the murmur may be discovered before any symptoms develop, as in the case of the patient presented here. AS is quite common and surely will become more so as the
WHICH ONE OF THE FOLLOWING IS THE CORRECT STATEMENT ABOUT HER MANAGEMENT?
A. Genetic analysis seeking the specific gene abnormality responsible for her heart murmur is an important initial component of her evaluation.
B. If her echocardiogram reveals evidence of severe disease and a preserved, normal ejection fraction (EF), prompt valve replacement is required.
C. Despite her being asymptomatic, her mortality risk will increase by 20% per year.
D. If her echocardiogram reveals evidence of severe disease and a preserved, normal EF, frequent clinical and echocardiographic monitoring is appropriate.
LABORATORY TESTS
Laboratory evaluation reveals a normal complete blood count and normal levels of blood glucose, hemoglobin A1C, and creatinine. She is scheduled for an echocardiography study.
population ages. The prevalence increases from 0.2% in adults aged 50 to 59 years to 2.8% in adults older than 75, to 9.8% in octogenarians.1
Much basic research is ongoing exploring the complex deranged biochemistry and biophysics interacting at the aortic valve, causing progressive AS. Less-complex is the list of known causative and associated lesions, including (the less common in the United States today) rheumatic heart disease and the presence of a bicuspid aortic valve. Of note, unlike hypertrophic cardiomyopathy, which can cause left ventricular outflow obstruction usually in a younger population, no specific gene cluster or abnormality has been identified for valvular AS.1 Thus, Answer A is incorrect.
As in this case, the initial presentation of AS is the presence of a characteristic heart murmur. The murmur typically is
51 Vol 13 No 11, February 2023 GP CLINICS Critical Appraisal In Medicine
TAKE-HOME MESSAGE
Valvular aortic stenosis is quite common in the elderly, and its prevalence will increase as the population ages. The natural history is well known, with no increased mortality in asymptomatic patients, but a 50% 2-year mortality rate once the classic symptoms of congestive heart failure, angina, or syncope develop. No effective medical therapy exists, and proper management involves careful, educated monitoring utilizing clinical findings, echocardiography for assessing and monitoring severity and progression, and ensuring appropriate timing of aortic valve replacement.
holosystolic and has a crescendo-decrescendo, “diamondshaped” character. The murmur usually is loudest at the base and radiates into the neck. Refined auscultation skills may detect an absence of S2 sounds. More easily detected is a delay and blunting of the carotid pulsations. Having said all this, the refined technology of echocardiography is required (1) to confirm that the murmur indeed is AS rather than another lesion; (2) to assess whether the AS is the sole abnormality or whether other lesions also are present, and which one is the hemodynamically significant one (eg, in rheumatic multiple valvular situations); and (3) to assess the severity of the AS using long established anatomic and hemodynamic parameters.2
ECHOCARDIOGRAPHY
The specifics of a detailed echocardiographic study include quantitation of calcification and leaflet motion of the aortic valve, maximum flow velocity (Vmax), Vmax through the valve (mild, < 2.0 m/s; moderate, 2.0-3.9 m/s; severe, ≥ 4.0 m/s), and mean transaortic pressure gradient (mild to moderate, 20-39 mm Hg; severe, > 49 mm Hg). The echocardiogram also will establish the functional capacity of the left ventricle with an EF measurement, normal being ≥ 50%.3
The above measurements then must be coupled with clinical findings—symptoms or no symptoms, comorbid diseases, and general prognosis. This is because regardless of echo findings (there are complex exceptions beyond the scope of this vignette), mortality essentially is not increased when AS is asymptomatic. And conversely, when symptoms are present, pathophysiologic changes can alter echocardiogram numbers, but the AS must be addressed, because as a broad statement, symptomatic AS has a 50% 2-year mortality rate unless the valve is replaced.1-4 These facts make Answer C incorrect. She is asymptomatic, and the stated mortality risk in this setting is too high.
Similarly, Answer B is incorrect in that even severe disease as demonstrated by echocardiography does not require urgent valve replacement so long as the patient is asymptomatic. This is the case for now, in part because the mortality of a surgical
procedure to correct AS still exceeds the mortality curve of an asymptomatic AS population. 1,4 This patient can be safely and carefully monitored, clinically for symptom changes and hemodynamically for echocardiographic deterioration, with the most specific finding being a decrement in EF to < 50%, which would prompt aortic valve replacement to preserve left ventricular function. 1,3,5 Thus, Answer D is the best choice here.
OUTCOME OF THE CASE
The clinical findings strongly suggested hemodynamically significant AS. This was confirmed by echocardiography, which revealed severe calcification with reduced leaflet motion, Vmax of 4.2 m/s, a mean transvalvular pressure of 46 mm Hg, and an EF of 55%.
The history was reviewed again with the patient, and she truly was asymptomatic, confirming the diagnosis of stage C1 severe AS.1 The plan was to monitor the patient clinically in the office at 3-month intervals and perform echocardiogram monitoring at 6-month intervals. She understands that aortic valve surgery is very likely in the future. She knows to promptly report any symptoms of angina, CHF, or syncope. n
Ronald Rubin, MD, is a professor of medicine at Temple University School of Medicine and chief of clinical hematology in the Department of Medicine at Temple University Hospital, both in Philadelphia, PA.
REFERENCES:
1. Otto CM, Prendergast B. Aortic-valve stenosis—from patients at risk to severe valve obstruction. N Engl J Med. 2014;371(8):744-756.
2. Rosenhek R, Binder T, Porenta G, et al. Predictors of outcome in severe, asymptomatic aortic stenosis. N Engl J Med. 2000;343(9):611-617.
3. Nishimura RA, Otto CM, Bonow RO, et al. 2014 AHA/ACC guideline for the management of patients with valvular heart disease: executive summary: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol. 2014;63(22):2438-2488.
4. Iung B, Vahanian A. Degenerative calcific aortic stenosis: a natural history. Heart. 2012;98(suppl 4):IV7-IV13.
5. Kodali SK, Williams MR, Smith CR, et al; PARTNER Trial Investigators. Twoyear outcomes after transcatheter or surgical aortic-valve replacement. N Engl J Med. 2012;366(18):1686-1695.
A 78-Year-Old Woman With a Newly Discovered Significant Heart Murmur What’s The “Take Home”?
Test Your Diagnostic Skills In Dermatology
Quiz # 61 Answer Spot The Diagnosis
B. Cutaneous lupus
(Quiz # 61 Question is published in this issue on page 35)
DISCUSSION
A skin biopsy confirmed the diagnosis of cutaneous lupus, D; subsequent blood test results, including an antinuclear antibody assay, were normal. Rosacea commonly involves the central face but is in the differential. Seborrheic and contact dermatitides typically show more scaling and are not tender. Photodermatitis usually occurs following use of a systemic or a topical agent; this patient had no such history.
The best management option for this patient is a sunscreen that blocks the UV-A spectrum, which aggravates cutaneous lupus.

53 Vol 13 No 11, February 2023 GP CLINICS
The Benefits of Cycling for Individuals With Diabetes
Timothy S. Harlan, MD, FACP, CCMS
Your patient is a 55-year-old man with type 2 diabetes who is worried about his health as he ages. He asks you if there are any recommended forms of exercise that can help him feel better about his health
HOW DO YOU ADVISE YOUR PATIENT?
(Answer and discussion as under)
Discussion
A study that suggests that exercise can help reduce the risk of developing diabetes1 in those who are overweight or obese. In fact, "for every additional 17 minutes of brisk daily walking, the participants saw a 6% reduction in their risk of developing diabetes." Yet exercise is also important for those who already have diabetes; it helps improve glucose control and cardiovascular fitness and reduces the risk of overall mortality as well as mortality due to heart disease.2

54 GP CLINICS Vol 13 No 11, February 2023
Nutritional Pearls Nutrition and Health
Timothy S. Harlan, MD, is a board-certified internist and professional chef who translates the Mediterranean diet for the kitchen with familiar, healthy recipes. He is an assistant dean for clinical services, executive director of The Goldring Center for Culinary Medicine, associate professor of medicine at Tulane University in New Orleans.
Nutritional Pearls
The Benefits of Cycling for Individuals With Diabetes
An international team of researchers noted that one of the greatest barriers to regular exercise is time.3 What if people with diabetes started using a bicycle for regular short-to-medium trips, such as commuting? What impact might that have on their risk of mortality?
The Research. The European Prospective Investigation into Cancer and Nutrition (EPIC) is an ongoing study that began recruiting participants in 10 Western European countries. Over 500,000 men and women are included, but for today’s research, the authors focused on the over 7400 people who had been diagnosed with diabetes (any type) before the study began.
Upon recruitment, the participants responded to a detailed lifestyle survey that allowed the researchers to assess the participants' levels and types of physical activity, from the nature of their work to any leisure time exercise as well as activities of daily life.
Additionally, the participants completed a detailed dietary questionnaire as well as demographic and medical history surveys. Their height, weight, and waist circumference were recorded along with their medical history. Five years later, the surviving participants again responded to a lifestyle questionnaire.
After an average of 10 years of follow-up, the authors compared the amount of cycling the surviving participants reported at the start of the study with that of those participants who passed away.
The Results. After considering several variables—from
WHAT’S THE “TAKE HOME”?
Mediterranean diet score to other health conditions such as high blood pressure—the authors found that compared to those who did not bicycle at the start of the study, those who averaged less than one hour of cycling per week were 22% less likely to die of any cause. Those who cycled between 60 and 149 minutes per week reduced their risk of death by 24%, and those who bicycled between 150 and 299 minutes per week were 32% less likely to die of any cause.
With the results from the follow-up survey, the authors could also look at those who started cycling after the initial survey, those who stopped cycling, and those who reported cycling at both surveys.
Individuals who maintained their cycling habit enjoyed the lowest risk of mortality from heart disease or any other cause—a drop of about 36%. But those who did not initially bicycle but reported any amount of cycling at the second survey still saw their overall risk of death fall by 34%. Similar results held for risk of death from heart disease.
REFERENCE:
1. Harlan TS. Exercise more effective than medication in preventing diabetes. Dr. Gourmet. Published April 14, 2021. Accessed January 3, 2023. https://www.drgourmet.com/bites/2021/041421.shtml
2. Colberg SR, Sigal RJ, Yardley JE, et al. Physical activity/exercise and diabetes: a position statement of the American Diabetes Association. Diabetes Care. 2016;39(11):2065-2079. doi:10.2337/dc16-1728
3. Ried-Larsen, M, Rasmussen MG, Blond K, et al. Association of cycling with all-cause and cardiovascular disease mortality among persons with diabetes. JAMA Intern Med. 2021;181(9):1196-1205. doi:10.1001/jamainternmed.2021.3836
55 Vol 13 No 11, February 2023 GP CLINICS
Certainly, there are plenty of barriers to cycling: first, you need a bicycle, then you need somewhere safe to ride it.
What I take from this study is that cycling is great exercise, but any moderately intense exercise that you can do consistently will help those with diabetes reduce their risk of mortality. Aim for at least 150 minutes of exercise per week, which breaks down to 30 minutes per day, 5 days per week.
Can a Hospital be Responsible for Patient Care by an Outsourced Physician?

Q:A patient went into cardiac arrest in her home and was transported by ambulance to a local medical center where she was in a coma. After some hours in the emergency department (ED), the treating physician arranged for a transfer to another hospital with a Level II trauma center because it was better equipped to provide appropriate care. Once the patient arrived at the second hospital, still in a coma, the treating physician in the hospital’s ED decided against inducing therapeutic hypothermia. The patient was left with permanent brain damage and complete disability. Her family sued the second hospital, alleging negligence and harm caused by the ED physician’s decision not to induce hypothermia.
A Court of Appeals was asked to dismiss a case against a hospital because the hospital’s ED was operated by an independent contractor physician group, and the doctor who treated the patient was employed by the independent contractor. Thus, the hospital claimed it was not responsible for the harm to a patient.
IS THE HOSPITAL AT FAULT?
(Answer and discussion on the next page)
56 GP CLINICS Vol 13 No 11, February 2023
Legal Pearls
Law Prespecitve In Medicine
Ann W. Latner, JD, is a freelance writer and attorney based in New York. She was formerly the director of periodicals at the American Pharmacists Association and editor of Pharmacy Times.
Ann W. Latner, JD
The Background
The hospital asked that the case be dismissed, claiming that its agreement with the group that provided emergency services clearly stated that the ED would be run as an independent contractor with no employer/employee relationships created between the hospital and the physicians employed by the company. Thus, the hospital argued, only the independent contractor and its physicians could be held liable for negligence arising from treatment decisions in the emergency department. The trial court agreed and dismissed the case. The plaintiff appealed, and the case went to the Court of Appeals.
The Case
The Court of Appeals noted that the contract between the hospital and the physician group running the ED cut both ways. On the one hand, it did state that no employer/employee relationship is created and that the physician group—not the hospital—is responsible for the acts of its employees. But on the other hand, the agreement gave the hospital ultimate control of
ED personnel and the methods and practices of the emergency physicians. The agreement stated that “the overall authority and responsibility for policy, administration and executive control matters relating to the operation of the Emergency Department” shall remain with the hospital. The Court noted that the agreement repeatedly sets forth the hospital’s ultimate control over the ED and places final physician-hiring authority with the hospital.
The Decision
Based on this, the Court concluded that there is a genuine dispute about the hospital’s supervision and control of the ED physician, and thus the Court reversed the trial court’s dismissal of the case.
REFERENCE:
• Latisha A. Gradia, individually, and Latisha A. Gradia, as Next Friend of BXG and BNG, minor children vs Baptist Hospital, Inc. Justia. Accessed December 13, 2022. https://law.justia.com/cases/florida/first-districtcourt-of-appeal/2022/21-1560.html
TRACK FAST
• Helicobacter pylori infection and use of nonsteroidal antiinflammatory drugs cause most cases of PUD.
• All patients with PUD should be tested for H. pylori .
• All patients with PUD should be treated with a PPI.
... page 42
57 Vol 13 No 11, February 2023 GP CLINICS
Can a Hospital be Responsible for Patient Care by an Outsourced Physician?
Legal Pearls
BOTTOM LINE—The hospital argued that it had no employer/employee relationship with the ED physicians, but it was not acting that way.

58 GP CLINICS Vol 13 No 11, February 2023






59 Vol 13 No 11, February 2023 GP CLINICS
Date of Publishing: 27th of previous month
Total pages: 60
If undelivered, please return to GP Clinics, F-59, Ashtavinayak, Ganesh Chowk, DN Nagar (Upper JUHU), Andheri (W), Mumbai 400053
 RNI No. MAHENG/2010/34121
RNI No. MAHENG/2010/34121























































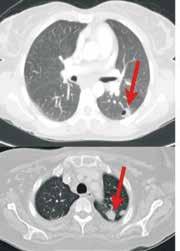


















 RNI No. MAHENG/2010/34121
RNI No. MAHENG/2010/34121
