
11 minute read
Projections for the decade ahead
As we enter 2020, we’re asking what the next ten years might hold for social care. Nuno Almeida of Nourish shares the three key areas that he thinks will change the face of the sector in the decade to come.
We are now in the year that so many governments and institutions used as a signifier of the ‘distant future’ in the early years of the millennium. Let’s all prepare for events called ‘2020 Vision’, and for lots of promises and attempts to set lofty, ambitious goals for 2030 and 2040.
Advertisement
The Prime Minister’s promise of a plan for social care has already been kicked into the long grass – again – but what does the next decade hold for social care?
I believe that, on the cusp of this new decade, there are three key areas that will shape the evolution of health and social care, regardless of what governments do (or don’t do, as seems to be more often the case).

AGEISM – AN OPEN DEBATE AROUND HEALTHY AGEING
‘We live in a world where people age 60 and over will soon outnumber children aged five and under.’ (World Health Organisation, 2019)
At the World Economic Forum this year, it is as important that we discuss ageing as it is that we discuss global warming and economic growth.
This is the decade when society will have to address its perceptions of ageing. It has become clear that our collective attitudes are themselves a leading cause for loss of quality of life. A person who believes the negative stereotypes associated with ageing will shorten their life by seven and a half years, compared to a person who manages to focus on staying active and living with purpose.
This is the decade when the exponential growth of the population aged 60 and over, seen by many as a threat to our economies and a burden, will evolve to be seen as another, different, driver for growth.
The transition towards seeing this part of the population as a diverse group of individuals with strengths, rather than simply ‘pensioners’, is already taking place as people start realising that age and health are different matters – and that it’s possible to live healthily for longer. But this can only continue if each and every one of us avoids fitting our own existence into the traditional narrative of what it looks like to get older.
'“Old” is a meaningless social construct that boxes an amazingly diverse array of people. Might as well try to group horses, oranges and orangutans. Problem is it drives social policy and, worse, we can internalise the expectations that come with the label.’ (John Beard, Former Director of Ageing and Life Course, WHO)
Businesses will have a role to play – over 60s are consumers, after all – but health systems and governments need to increase awareness of the importance of living a healthy, active and engaged life as we get older. This may well be the lever that determines whether >
our older people are drivers of economic growth or a cost and a burden.
It seems the solutions we need for this growing new segment of our population are therefore not always ‘more hospitals’ or ‘more care homes’. We will realise in time that building communities is just as important, and the solutions may end up being more green parks, flexible employment for older people, or nurseries and care homes built next to one another, which can all lead to greater overall happiness and more vibrant economies.
Alongside existing care homes, I foresee a surge of activity in creation of communities. Both existing care homes opening up to communities around them, and an increase in extra care or housing with care schemes. Some of our neighbours may live with learning difficulties, some of our neighbours may have nursing needs – but they will all be valued parts of the community.
Maybe this sounds like ‘Vision 2030’ territory, but I think this is on the cusp of happening, and not a long way away. >
INTEGRATION: THE LAST MILE CHALLENGE
The second area I think will change in the next ten years is integration of health and social care. Integration is still as urgent as ever, but all attempts to accelerate it tend to grind to a halt under the weight of complexity.
A person receiving care in the community, moving between a care home, hospital and back, or someone managing the care of a relative in their own home, still has to deal with services and systems that make their lives a lot harder than they should be, often resulting in degradation of quality of care. And although budgets for health and social care are often a factor, they are not the only factor.
We have learnt that integration is not achieved in isolation by the NHS, or by local authorities. The terms ‘co-design’ and ‘cocreation’ have become part of the vocabulary in recent years and, where these are done well, we see people’s experiences of care improving significantly.
Saying this, the moment integration started being discussed, everyone rushed to make their area the ‘hub’ for aggregation of patient data. GPs felt they were the natural hub. Local authorities felt they were the natural hub. District nurses felt they were the natural hub. And yet, people kept experiencing clunky journeys of care, assessments by different entities, contradictory advice and signposting. However, there clearly is progress being made in the creation of shared data within health and social care. Local Health and Care Records (LHCRs) are a significant advance – now, when healthcare teams and local authorities interact with a person, they are doing so whilst holding the same data about this individual. This is a seismic improvement compared to siloed organisations with the person being completely in charge of coordinating multiple entities.
Despite the advancements, as ever in very large and complex projects, this journey is suffering from a ‘last mile’ challenge. I say ‘last mile’ as I see it as being similar to the challenge telecoms operators faced when bringing highspeed internet to every home. This does not diminish the value of the work done so far in implementing LHCRs – they are an essential building block for integration – but we need to bring the benefits to the care teams supporting each person receiving care.
THE ROLE OF NURSES
There is little doubt that nursing professionals, alongside skilled care workers and healthcare assistants, hold the key to enabling the health and social care sector to meet increased demand. But for this workforce to be effective, roles need to be questioned. In 2020, we mark Florence Nightingale’s 200th birthday – 110 years after her death, how we can reinvent nursing and the part that nurses play?
In my opinion, nurses will become even more important sources of knowledge, mentors and leaders in the upskilling of the workforce over the next ten years, whether as part of teams in care homes, or as district nurses working in a co-ordinated fashion with care workers – the role will become one of defining the correct protocols for a care team, ensuring everyone has the skills they need and can confidently use them, and ensuring everyone then monitors the quality of care, and how outcomes are being met.
This vision for a future of nursing where care protocols are set and monitored by nurses allows a nurse to deliver a much greater impact – in such a structure, with digital monitoring of risk and adherence to prescribed practice, each trained nurse can oversee far higher numbers of people; but to achieve this, we need to give nurses the tools, including: • A mandate to train others, and teach skills and protocols to healthcare assistants and care workers. • The right digital tools to monitor risk, and mechanisms for escalation that allow nurses to get involved when they can make a real difference – either in upskilling others, or in dealing with acute cases. • Nursing schools that encourage continuous professional development fit for different approaches to the role of nursing – including encouraging a larger number of nurses to become clinical leads of multiple care worker teams.
It is also easy to see that there is an opportunity to do more regarding nurses having a full picture of the person they are caring for, which means that, over the next decade, we need to find and implement the right systems for information sharing, leading to natural coordination of care around each person.
DIGITAL TRANSFORMATION
As mentioned above, digital is an essential part of enabling roles to change shape and will continue to enable true integration between health and care teams.
What providers are increasingly demonstrating is that digital transformation focused on recording the interactions between care workers and people receiving support is far more effective in monitoring and encouraging improvements in care quality than some other systems focused on time and attendance.
Care management teams are also starting to use data analytics to improve their ability to audit at scale, and to develop strategies for monitoring and mitigating key risks in their services. Analytics are enabling providers to think proactively in defining what needs to be managed and rolling out business intelligence and dashboards to empower teams to focus on those key aspects.
I believe that over the next ten years there is unique potential for digital to deliver a transformation to the sector. Where in other sectors this means consumers now deal with smartphones rather than people, what it will mean for social care is very different: we can maximise the eye-to-eye and skin-to-skin contact between care services and people receiving support, while ensuring that care is safe, and enabling care teams to act in a co-ordinated fashion.
We must create safe services with the right quality and capacity, fit for the demands of the next decade – managers as always will either drive this change or be driven by it. Embracing this change and steering it is invariably the attitude that leads to the best outcomes. CMM
What do you think social care will look like in ten years’ time? Do you agree with Nuno? Share your insights on the CMM website where you can comment on this article, www.caremanagementmatters.co.uk Nuno Almeida is Founder and Chief Executive of Nourish. Email: getintouch@nourishcare.co.uk Twitter: @nourishcare
specialist healthcare business agents
Independent expertise Nationwide knowledge
It has been a month to celebrate as DC Care ‘came of age’ with its 18th Birthday, whilst Regional Directors Alison Willoughby and Andy Sandel celebrated their 10th Anniversaries since joining us!
The dawn of a new decade often brings about new goals and objectives for businesses and people alike across the world. In our 18th year, nothing changes as we continue discreetly selling care businesses UK-wide, here’s just a small selection of successful sales so far in 2020...




SOLD
When industry knowledge and wisdom are needed, when a discreet sale is desired, our clients choose DC Care to sell their healthcare business.
SALES | ACQUISITIONS | APPRAISALS | CONSULTANCY
CareTutor Video-based eLearning
Skills for Care Endorsed CPD Accredited Best quality eLearning Free trial Interactive Content






















Care Certiicate Training Matrix 60+ Courses Video-based NOT text-based like others
Unlimited Use from 45p per user per month
Pay As You Go
from 95p per course
We will NOT be beaten on quality orprice! Call 0345 644 2866 now www.caretutor.org | info@caretutor.org
WIRELESS NURSE CALL TECHNOLOGY LET LOOSE

No matter where the action takes place, you’ll know if there’s a call or a fall
IN ASSOCIATION WITH
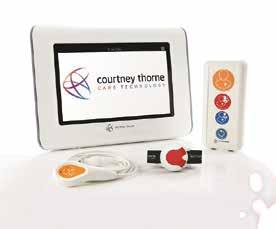
WANT TO TRY? CALL 0800 0862483








