
15 minute read
Effect of Irrigants on Dislodgement Resistance of Two Root Repair Materials in Furcation Perforations
An In Vitro Study
Ruchi Agrawal, M.D.S.; Tina P. Purayil, M.D.S.; Kishore Ginjupalli, M.Sc., Ph.D.; Nidambur V. Ballal, M.D.S., Ph.D.
A B S T R A C T
Aim: To evaluate the effect of 2.5% sodium hypochlorite (NaOCl) and 2% chlorhexidine (CHX) irrigants on dislodgement resistance of EndoSequence Root Repair Material Fast Set Putty (ERRMF) and Endocem MTA in furcation perforations.
Materials and Methods: Sixty mandibular molars were decoronated, and perforation was carried out by using a #1.2 bur perpendicular to the furcal floor and was further enlarged by #4 Peeso reamer. The specimens were divided into two groups (n=30) and the furcal perforations were restored with ERRMF and Endocem MTA.Then the specimens of each material were further divided into three subgroups (n=10) according to irrigation solution used (2.5% NaOCl, 2.0% CHX and distilled water control group). Later, push-out bond strength was measured using universal testing machine.
Statistical Analysis: The data was analysed using oneway ANOVA and independent t-test. Results: Results showed that ERRMF had higher pushout bond strength than Endocem MTA (p<0.05). However, none of the root canal irrigants had significant influence on the bond strength of ERRMF and Endocem MTA.
Conclusion: ERRMF as a root perforation material exhibited superior push-out bond strength compared to Endocem MTA. Use of NaOCl and CHX did not affect the push-out bond strength of these materials.
Endodontic therapy aims to maintain the integrity of the natural dentition, to achieve proper form, function and esthetics. Root perforation is one of the most common mishaps during endodontic tooth preparation. A perforation is any communication between the root canal space and the periradicular tissues which may be iatrogenic or pathological in nature. 1 Perforations that are present in the pulp chamber floors and cervical third of the root have a poor prognosis compared to those present in the middle or apical third of the root. It has been suggested that furcation perforations be repaired immediately with a suitable material, to reduce contamination with bacteria and infection of periodontal tissues. 2
An ideal material for perforation should have adequate sealing ability, dimensional stability, insolubility, biocompatibility and radiopacity. 3 It should also not dislodge under mechanical stresses of occlusion or from forces used for condensing permanent restorative materials. 4
To date, many materials have been used to repair perforation defects, including amalgam, composite resin, glass ionomer cement, intermediate restorative material, super EBA and mineral trioxide aggregate (MTA). Leakage, solubility, handling properties— especially longer setting times—biocompatibility and moisture incompatibility are some of the problems encountered with the use of these materials. 5
More recently, two fast-setting cements, namely, pozzolanbased MTA (Endocem, Maruchi, Wonju, Korea) and EndoSequence Root Repair Material Fast Set Putty (ERRMF) (Brasseler USA, Savannah, GA) were introduced to overcome the drawbacks of longer clinical setting times. Pozzolan MTA consists of pozzolan particles, which increase the surface area on mixing with liquid, whereas ERRMF is a calcium silicate–based material and consists of calcium silicates, zirconium oxide, tantalum oxide, monobasic calcium phosphate and fillers.
After furcal perforation repair, routine endodontic treatment is performed with various irrigants, like 2% chlorhexidine gluconate (CHX) and sodium hypochlorite (NaOCl). 6 However, this can cause unavoidable interaction between irrigants and repair materials.

Guneser et al. have shown that NaOCl and CHX have no significant effect on the dislodgement resistance of Biodentine, Dyract AP, IRM and amalgam. However, CHX was shown to decrease the microhardness and alter the surface morphology of ProRoot MTA, thereby reducing its push-out bond strength. 7 Kogan et al. found that NaOCl gel decreased the setting time of ProRoot MTA, improved its strength and hence push-out bond strength. 8
There has been increased acceptance of Endocem MTA and ERRMF for endodontic applications. Jang et al. 9 demonstrated that irrigation protocol significantly influences the washout resistance of Endocem, whereas Alsubait et al. showed that NaOCl irrigation increased the push-out bond strength of ERRMF to the tooth. 10 The existing literature lacks sufficient evidence to suggest the effect of irrigants on the performance of these materials as root furcation perforation repair materials. Hence, the purpose of this study was to evaluate and compare the effect of various endodontic irrigants (ie, 2.5% NaOCl, 2% CHX, distilled water) on the dislodgement resistance of ERRMF and Endocem MTA in furcation perforations.
Materials and Methods
Ethical clearance was obtained from Institutional Ethical Committee (IEC 647/2015). Sixty human mandibular molar teeth with divergent roots and completely formed apex were selected. Teeth with carious lesions, development defects, fused roots, fractured or cracked teeth and endodontically treated teeth were excluded.
After surface debridement with the scaler, the samples were stored in 0.2% sodium azide (Sigma-Aldrich, Germany) until the experiment at 4˚C. Teeth were decoronated using diamond disk (Horico, Germany) at cementoenamel junction, and a perforation was created perpendicular to the furcal floor and parallel to the long axis of the teeth by using round bur (#1.2) (SS White Burs, Inc, USA). Further, the dimension of the perforation was increased to a diameter of 1.3 mm using #4 peeso reamer (Mani, Tochigi-ken, Japan). The height of the perforated area was measured using a periodontal probe (Hu-Friedy Mfg. Co. UK) for all the samples to standardize the height to 2 mm. The samples having less than or more than 2 mm dentin height were excluded. Subsequently, samples were mounted in acrylic molds (DPI-RR Cold Cure, DPI, India) such that clearance between the furcal area and the acrylic mold was 3 mm. Space was left to place Gelatamp (Roeko-Coltene, Germany), which would act as a matrix to pack materials.
Teeth were then randomly divided into two groups based on root repair material used: in Group I, the perforation site was repaired with ERRMF; in Group II, it was restored with Endocem MTA. ERRMF, the premixed paste, was injected into the perforation site completely and any excess material was removed using a moist cotton pellet. Endocem MTA was mixed, as per the manufacturer’s instructions, and was placed incrementally in the perforation site and condensed using a hand plugger (Manipal Acharya, Manipal, India). A wet cotton plug was placed in contact with both of the materials to allow the material to completely set.
The samples in both groups were placed in an incubator at 37°C and 100% relative humidity. After the materials were set, each group was further subdivided into three groups (n=10) based on irrigation solution used over the perforation site: Group A-2.5% NaOCl; Group B-2% CHX; and Group C-distilled water (control group).
Each sample was irrigated using 20 mL of test irrigant to the perforation repair site from a disposable syringe with 27-gauge Monoject needle (Ultradent Products Inc., USA) for five minutes. Then the perforation site in all samples was finally irrigated with 5mL of distilled water to counteract the prolonged effect of irrigants. Samples were stored for 24 hours at 37°C and 100% humidity.
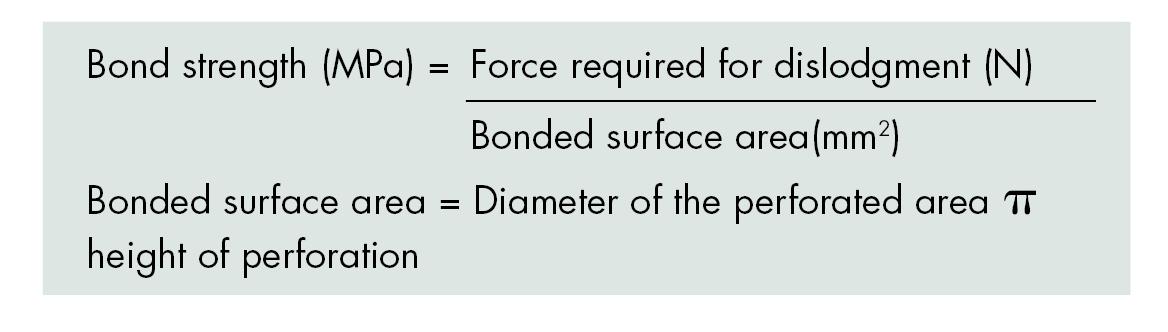
The push-out test was performed using a universal testing machine. The specimens were mounted on the lower platform of the machine (Instron 3366, Inston Corp., USA), and a plunger of 1 mm diameter was allowed to push out the root-repair material under compressive force at a crosshead speed of 1mm/min. Maximum force required for the dislodgment was recorded in newtons. The dislodgement resistance was calculated in megapascals using the following formula:
The data was analysed using One-way ANOVA, and the significant differences were compared using post-hoc Tukey’s tests for intra-group comparisons. Inter-group comparisons were made using independent t –test at a confidence interval of 95%. A p value less that 0.05 was considered significant.
Results
The mean push-out bond strength values, along with standard deviations for both groups after irrigation, are presented in Table 1.
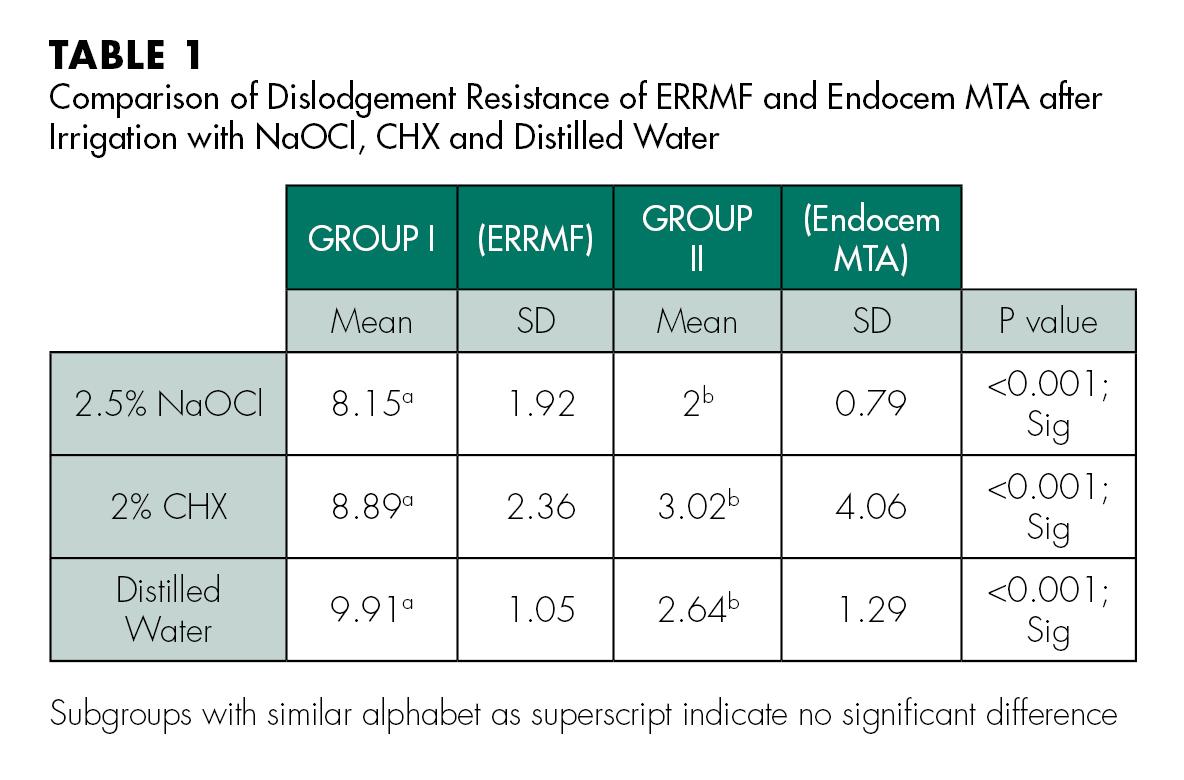
From the results, it was observed that the differences among the push-out bond strengths after irrigating the repaired root canal with ERRMF were not statistically significant, irrespective of the irrigating material used. This suggests that 2.5% NaOCl and 2.0% CHX did not significantly reduce the push-out bond strength (p>0.05). Similar results were observed with the Endocem MTA group as well (p>0.05).
However, a significant difference in the push-out bond strength between the root canal repair materials was observed (p<0.001). Among the materials, ERRMF showed higher pushout bond strength values than Endocem MTA did.
Discussion
The repair process of the root perforations should involve sealing the defect with a biocompatible material. The success of the repair depends on various factors, such as adhesion of the root repair material to the surrounding dentine, adequately sealed coronal restoration and the resistance of the material to dislodgement forces. In addition, the ability of the root repair material to set to a hard and rigid material and resist condensation forces of various restorative materials, such as amalgam, is also an important consideration. It is estimated that a force of approximately 8.9MPa is applied during the condensation of such restorative materials. To withstand these forces, the root repair material should exhibit sufficient elastic modulus without failure. 11 A material with low elastic modulus or weaker adhesive bond with dentine could be displaced from the furcal repair site during the subsequent restoration. 4 Thus, the dislodgement re sistance of the perforation repair materials is an essential parameter to consider in routine clinical practice. The push-out bond test is widely used to measure the displacement resistance, as it is more practical, efficient and reliable for assessing the bond strength. 2
This study evaluated the effect of the irrigants 2.5% NaOCl and 2% CHX on two different root repair materials (ERRMF and Endocem MTA). Both of these materials were selected because the use of MTA for endodontic application is on the rise, especially with the advent of fast-setting versions. The results showed that irrigating with 2.5% NaOCl and 2% CHX had no significant effect on the dislodgement resistance of root-repair materials. This indicates that the setting reaction of the selected root-repair materials progressed sufficiently so that the irrigants did not have any effect on these materials. It is also possible that irrigants did not interfere with the setting of the MTA materials.
Yan P et al. showed that CHX and NaOCl irrigation had no negative effect on the bond strength between MTA and dentin. 6 Similar findings were reported by Adl et al. with the use of 2% CHX. Endocem MTA used in the present study has similar chemical composition as that of the one used in Adl et al., and the observations of the present study are in agreement with their study. 12 Moreover, Jang et al. reported a higher washout resistance when irrigated with NaOCl compared to the saline and CHX-treated groups for Endocem. 9 This could be attributed to the different methodologies used in both studies. In the previous study, the material was placed into an acrylic mold instead of human teeth, which was then immersed in the irrigants for five minutes.
This study also revealed that dislodgement resistance of ERRMF was significantly more than Endocem MTA irrespective of the irrigants used, i.e., 2.5% NaOCl and 2% CHX. This significant difference between the materials can be attributed to the differences in their chemical composition, the setting reaction of the individual material and interaction with the dentine.
ERRMF consists of dicalcium silicate, tricalcium silicate, zirconium oxide, tantalum pentoxide and calcium sulfate. 13 It is produced as a premixed product to help the clinician with a homogeneous, predictable material. This bioceramic material is manufactured with nanosphere particles (10–3 mm in its greatest diameter), which allows the material to penetrate into the dentinal tubules forming a micromechanical bond to adjacent dentin. 14,15,16 The higher push-out bond strength may also be attributed to its slow hydration process and small size of porosity, which is known to play a crucial role in the association between compressive strength-modulus of elasticity relationship. 17,18
The filler and thickening agents added to make it a putty form may be also be responsible for higher bond strength. 19,20 Moreover, it was seen that zirconium oxide presence can also enhance certain physical properties of the material. 21 Products that require chairside mixing of powder liquid components may have inconsistencies with respect to P:L ratio because of variations in operator mixing, leading to decreased bond strength. 19,20,22 Hence, the higher push-out bond strength obtained for ERRMF might be attributed to the delivery system of this material.
On the other hand, Endocem MTA is chemically related to commercially available MTA. It is based on pozzolan reactions, the free calcium hydroxide that is formed at the time of hydration is used, leading to reduced calcium-releasing ability. Thus, less calcium/phosphorous proportion precipitates are formed, causing the bioactivity to reduce. 23,24 As the bioactivity process has been found to be responsible for strong micromechanical bonding to dentin in case of MTA cements, 25 the reduced push-out bond strength values for Endocem MTA can be attributed to its decreased bioactivity. Thus, ERRMF exhibited better resistance to dislodgement when compared to Endocem MTA after irrigation, owing to its inherent properties.
Conclusion
Within the limitations of this ex-vivo study, it can be concluded that EndoSequence Root Repair Material Fast Set Putty (ERRMF) can be a better alternative to Endocem MTA for repair of furcal perforations, as it exhibited superior bond strength. Further, irrigants (2.5% NaOCl and 2% CHX) had no effect on the bond strength of this material to the tooth.
Queries about this article can be sent to Dr. Purayil, corresponding author, at tina.pp@manipal.edu.
REFERENCES
1. Gorni FG, Andreano A, Ambrogi F, Brambilla E, Gagliani M. Patient and clinical characteristics associated with primary healing of iatrogenic perforations after root canal treatment: results of a long-term Italian study. J Endod 2016;42:211-5.
2. Loxley EC, Liewehr FR, Buxton TB, McPherson JC. The effect of various intracanal oxidizing agents on the push-out strength of various perforation repair materials. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2003;95:490-4.
3. Fuss Z, Trope M. Root perforations: classification and treatment choices based on prognostic factors. Endod Dent Traumatol 1996;12:255-64.
4. Hashem AA, Wanees Amin SA. The effect of acidity on dislodgment resistance of mineral trioxide aggregate and bioaggregate in furcation perforations: an in vitro comparative study. J Endod 2012;38:245-9.
5. Johnson BR. Considerations in the selection of a root-end filling material. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 1999;87:398-404.
6. Yan P, Peng B, Fan B, Fan M, Bian Z. The effects of sodium hypochlorite (5.25%), chlorhexidine (2%) and Glyde File Prep on the bond strength of MTA-dentin. J Endod 2006;32:58-60.
7. Guneser MB, Akbulut MB, Eldeniz AU. Effect of various endodontic irrigants on the pushout bond strength of Biodentine and conventional root perforation repair materials. J Endod 2013;39:380-4.
8. Kogan P, He J, Glickman GN, et al. The effects of various additives on setting properties of MTA. J Endod 2006;32:569-72.
9. Jang GY, Park SJ, Heo SM, Yu MK, Lee KW, Min KS. Washout resistance of fast-setting pozzolan cement under various root canal irrigants. Restor Endod 2013;38:248-52.
10. Alsubait SA. Effect of sodium hypochlorite on push-out bond strength of four calcium silicate-based endodontic materials when used for repairing perforations on human dentin: An in vitro evaluation. J Contemp Dent Pract 2017;18:289-94.
11. Lussi A, Brunner M, Portmann P, Burgin W. Condensation pressure during amalgam placement in patients. Eur J Oral Sci 1995;103:388-93.
12. Adl A, Sadat Shojaee N, Sobhnamayan F, Sadat Shojaee N. The effect of chlorhexidine on push-out bond strength of mineral trioxide aggregate. Avicenna J Dent Res 2014; 6:e21195.
13. Hansen S, Marshall G, Sedgley C. Comparison of intracanal Endosequence root repair material and ProRoot MTA to induce pH changes in simulated root resorption defects over 4 weeks in matched pairs of human teeth. J Endod 2011;37:502–6.
14. Damas BA, Wheater MA, Bringas JS, Hoen MM. Cytotoxicity comparison of mineral trioxide aggregates and Endosequence bioceramic root repair materials. J Endod 2011;37:372–5.
15. Jiang Y, Zheng Q, Zhou X, Gao Y, Huang D. A comparative study on root canal repair materials: a cytocompatibility assessment in L929 and MG63 cells. Sci World J 2014;2014:463826.
16. Jeevani E, Jayaprakash T, Bolla N, Vemuri S, Sunil CR, Kalluru RS. Evaluation of sealing ability of MM-MTA, Endosequence, and Biodentine as furcation repair materials: UV spectrophotometric analysis. J Conserv Dent 2014;17:340-3.
17. Barralet JE, Gaunt T, Wright AJ, Gibson IR, Knowles JC. Effect of porosity reduction by compaction on compressive strength and microstructure of calcium phosphate cement. J Biomed Mater Res 2002;63:1-9.
18. Guo YJ, Du TF, Li HB, Shen Y, Mobuchon C, Hieawy A, Wang ZJ, Yang Y, Ma J, Haapasalo M. Physical properties and hydration behavior of a fast-setting bioceramic endodontic material. BMC Oral Health 2016;16:23.
19. Shokouhinejad N, Razmi H, Nekoofar MH, Sajadi S, Dummer PM, Khoshkhounejad M. Push-out bond strength of bioceramic materials in a synthetic tissue fluid. J Dent (Tehran) 2013;10:540-7.
20. Shokouhinejad N, Yazdi KA, Nekoofar MH, Matmir S, Khoshkhounejad M. Effect of acidic environment on dislocation resistance of Endosequence root repair material and mineral trioxide aggregate. J Dent (Tehran) 2014;11:161-6.
21. De Aza AH, Chevalier J, Fantozzi G, Schehl M, Torrecillas R. Crack growth resistance of alumina, zirconia and zirconia toughened alumina ceramics for joint prostheses. Biomaterials 2002;23:937–45.
22. Walsh RM, Woodmansey KF, Glickman GN, He J. Evaluation of compressive strength of hydraulic silicate-based root-end filling materials. J Endod 2014;40:969-72.
23. Askarinejad A, Pourkhorshidi AR, Parhizkar T. Evaluation of the pozzolanic reactivity of sonochemically fabricated nano natural pozzolan. Ultrason Sonochem 2012;19:119-24.
24. Han L, Kodama S, Okiji T. Evaluation of calcium releasing and apatite forming abilities of fast-setting calcium silicate based endodontic materials. Int Endod J 2015;48:124-30.
25. Reyes-Carmona JF, Felippe MS, Felippe WT. The biomineralization ability of mineral trioxide aggregate and Portland cement on dentin enhances the push-out strength. J Endod 2010; 36:286-91.

Dr. Agrawal
Ruchi Agrawal, M.D.S., is a former postgraduate student, Department of Conservative Dentistry & Endodontics, Manipal College of Dental Sciences Manipal. Manipal Academy of Higher Education, Manipal, Karnataka, India.

Dr. Purayil
Tina P. Purayil, M.D.S., is associate professor, Department of Conservative Dentistry & Endodontics, Manipal College of Dental Sciences Manipal. Manipal Academy of Higher Education, Manipal, Karnataka, India.

Dr. Ginjupalli
Kishore Ginjupalli, M.Sc., Ph.D., is associate professor, Department of Dental Materials, Manipal College of Dental Sciences Manipal. Manipal Academy of Higher Education, Manipal, Karnataka, India.

Dr. Ballal
Nidambur V. Ballal, M.D.S., Ph.D., is additional professor, Department of Conservative Dentistry & Endodontics, Manipal College of Dental Sciences, Manipal Academy of Higher Education, Manipal, Karnataka, India.










