
3 minute read
CHAPTER 14 DISCECTOMY
Richard A. Gasalberti MD, Isaac J. Kreizman MD, Aziz Abdurakhimov MD, Michael Garbulsky PA
All the percutaneous procedures in intervertebral disc herniation treatment that have been used in the last 35 years are minimally invasive, and the main purpose is to respect as much as possible the anatomy of spine, reducing postoperative complications with a faster return to daily activities. Historically the main goals of percutaneous procedures included sufficient removal of disc material with minimal retraction of the nerve root, adequate hemostasis, the maintenance of spinal stability. There are many percutaneous procedures have been used for spinal disc herniation treatment, for example chemonucleolysis where nucleus pulposus is destroyed using chemical substances, automated percutaneous nucleotomy has been introduced by Onik in 1985, percutaneous manual and endoscopic nucleotomy with posteriolateral approach, intra discal electro thermal therapy (IDET) has been introduced for the treatment of chronic discogenic low back pain due to ruptured annulus and/or small contained disc herniation, nucleoplasty (coblation), percutaneous laser discectomy, and hydrodiscectomy. Nowadays percutaneous procedures in intervertebral disc herniation treatment are safe and minimally traumatic.
Advertisement
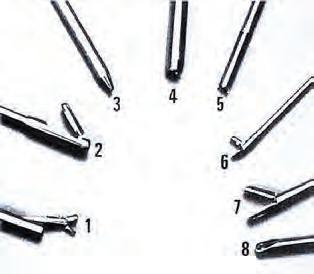
Percutaneous endoscopic discectomy is a least invasive procedure used to reduce a herniated disc. It can be performed on a day care basis under local anesthesia with shorter length of hospitalization thus improving the quality of life earlier. Variable forceps with automated high-power suction shaver and cutter systems are used.
All kinds of lumbar disc herniation, including severely difficult and extremely difficult herniations, are manageable by the percutaneous endoscopic lumbar discectomy (PELD) with transforaminal or interlaminar approache [1] .
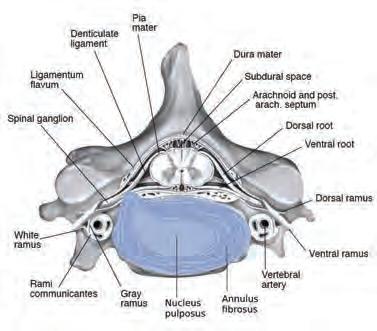
Intervertebral disc is a clinically important structure in human spine. It composed of three regions known as the annulus fibrosus, nucleus pulposus, and cartilaginous end plate. Nucleus pulposus may cause bulging of the outer annular fibers or herniates though annulus fibrosus. Herniation or bulging of the intervertebral disc may compress exiting spinal roots which can lead to radicular pain. Usually intervertebral disc herniates into the central vertebral canal, affecting the inferior nerves. Posterolateral herniation at L4-L5 or L5-S1 is common due to the thin posterior longitudinal ligament and thicker anterior longitudinal ligament. Spinal nerves from C1 to C7 exit though intervertebral foramen above the corresponding vertebra. C8 spinal nerve exit below
C7 vertebra. All other spinal nerves located below the C8 cervical nerve exit intervertebral foramen below the corresponding vertebra. For example, herniation of intervertebral disc at level L3-L4 affects L4 spinal nerve.
The percutaneous lumbar discectomy has proven to be safe, non-destructive, and effective procedure. The success of percutaneous lumbar discectomy depends on proper patient selection, knowledge of spine anatomy, and adherence to the detail of the operative technique.


Indications
The posterolateral approach is preferred for all methods of percutaneous approaches to the disc space, be it for diagnostic or therapeutic purposes. Percutaneous endoscopic discectomy with posterolateral appoach should be strongly considered in patients with extraforaminal far-lateral disc herniation. Other indications for posterolateral approach include lumbar decompression, foraminal herniations, formaminotomy, small non-sequestered extruded disk herniations, central and paracentral disc herniations, synovial cysts, recurrent herniations, decompression of foraminal stenosis, biopsy and debridement of discitis, visualized discectomy and endplate preparation prior to interbody fusion or total disc replacement (TDR) implantation. Also, patients who cannot undergo general anesthesia are excellent candidates for this approach.

Contraindications
Contraindications for percutaneous endoscopic discectomy with posterolateral approach include free or extruded disc fragments within the spinal canal or extruded migrated disc herniations that are out of reach of the foraminal approach, calcified disc herniations, diffuse annular bulge involving the entire circumference of the vertebral body, and ligamentum flavum hypertrophy. Significant migration of disc fragment in an absolute contraindication for endoscopic discectomy.
Complications
Complication of percutaneous endoscopic discectomy are relatively rare. These include infection, nerve root or dorsal root ganglia injury, bleeding, and damage to end plates and disc space collapse.
References
[1] Kim HS, Paudel B, Jang JS, Lee K, Oh SH, Jang IT. Percutaneous Endoscopic Lumbar Discectomy for All Types of Lumbar Disc Herniations (LDH) Including Severely Difficult and Extremely Difficult LDH Cases. Pain Physician. 2018 Jul;21(4):E401-E408. [Pubmed]
[2] Yeung AT, Tsou PM. Posterolateral endoscopic excision for lumbar disc herniation. Spine. 2002;27:722–731.
[3] Ahn Y, Lee S-H, Park WM, Lee HY, Shin SW, Kang HY. Percutaneous endoscopic lumbar discectomy for recurrent disc herniation: surgical technique, outcome, and prognostic factors of 43 consecutive cases. Spine. 2004;29:E326–E332.
[4] Choi G, Lee SH, Raiturker PP, Lee S, Chae YS. Percutaneous endoscopic interlaminar discectomy for intracanalicular disc her- niations at L5-S1 using a rigid working channel endoscope. Oper Neurosurg. 2006;58:59–68.
[5] Knight M, Goswami A. Management of isthmic spondylolisth- esis with posterolateral endoscopic foraminal decompression. Spine. 2003;28:573–581.
[6] Chang MA, Talac R, Kim CW. The endoscopic discectomy learning curve. Submitted for publication.
[7] Tsou PM, Yeung A, Yeing AT. Posterolateral transforaminal selective endoscopic discectomy and thermal annuloplasty for chronic lumbar discogenic pain: a minimal access visualized intradiscal surgical procedure. Spine J. 2004;4(5);10.
[8] Hermantin FU, Peters T, Quartararo L, Kambin PA. Prospec- tive, randomized study comparing the results of open discectomy with those of video-assisted arthroscopic microdiscectomy. J Bone Joint Surg. 1999;81-A:958–965.




