

Heart of Aotearoa
INSIDE NZ'S HEART CARE CRISIS
Failures, delays, & inequity laid bare
Letitia's message
Meet our Cardiac Advisory Board
TEER – An open-heart surgery alternative
Robert's journey: a missed opportunity
New course delivers lifesaving heart techniques
Chief Executive
Letitia Harding
Research and Education Manager – Cardiac Health
Dr. Lina Goldstein
Individual Giving Fundraising Executive
Michaela Tahere
PR & Comms Marketing Manager
Chloe Bradwell
Digital Marketing Specialist
Sam Treseder
Digital Content & Marketing Advisor
Jared McOnie
Digital Content Advisor
Cat Mercer
Community Educator Manager
Sharon Pihema
Corporate Sponsorship & Engagement Advisor
Paul Aschenberger
Medical Director
Dr. Sarah Fairley
Chief Cultural Advisor – Māori
Sir John Clarke, KNZM, CNZM
Level



ph: 0800 100 506
.org.nz
LETITIA'S MESSAGE
WELCOME TO THE first edition of the Heart of Aotearoa magazine.
Heart and lung health have a huge overlap across a wide range of diseases, which is why we launched Kia Manawanui Trust – The Heart of Aotearoa.
The Trust’s advocacy efforts focus on raising awareness about cardiac health issues, ensuring that patient voices are heard. We want to promote equitable access to cardiac care, resources and treatments by empowering both healthcare professionals and patients.
Of course, to make a difference in the cardiac space, we also need the right people, which is why we formed the Cardiology Advisory Board (CAB) led by our Medical Director, Dr Sarah Fairley. You can read more about Sarah and the CAB team on page 4.
A key focus of the Trust is to collaborate with experts to ensure that those working in the cardiac space stay informed about emerging research and practices. One such innovation is the Transcatheter Edge-toEdge Repair (TEER) - a medical procedure that can repair a heart valve without the need for openheart surgery. Dr Andrew Chatfield, an interventional cardiologist and a member of our CAB, talks more about this procedure on page 6.
The Trust is committed to providing leadership and expertise in cardiac health, while also raising public awareness about the critical state of New Zealand’s heart health services. This is why we launched the first New Zealand Cardiac Impact Report. This report highlights some of the major issues facing our cardiac services today, and also where we are drastically failing, not only patients, but also our dedicated cardiac
healthcare workers as well. Check out some of the key statistics from the report on page 12.
Heart failure (HF) was one of the key indicators looked at in the Cardiac Impact Report, and, in this edition, Dr Sarah Fairley discusses some of the HF treatments available and funded in New Zealand, and also those that aren't. Best practice treatment guidelines are there for a reason, and if treatments are recommended, then we should be using them. Turn to page 14 to find out more.
This year, I met with the Minister of Health, Hon Simeon Brown - twice - to discuss the myriad of issues facing the cardiac sector. One specific talking point was around the long wait times for patients in the Midland and Central regions needing cardiac catheterisation and echocardiograms.
This year, the Trust, alongside the Transcontinental Coronary Imaging and Physiology Club (TCIP) and Asian Pacific Society of Cardiology (APSC), hosted an Optical Coherence Tomography (OCT) and Intravascular Ultrasound (IVUS) course - the first-ofits-kind in New Zealand. Thirty cardiologists from New Zealand and Australia attended the teaching course that certifies them in OCT and IVUS - lifesaving heart techniques that can halve deaths when used for stent placement. This training was an important moment for education in heart healthcare in New Zealand. This educational course would not have been possible without all our generous supporters. You can read more about it on page 10.
Finally, if you want to donate these holidays, think about donating to the mobile electrocardiogram (ECG) appeal. Many communities don’t have an ECG machine that can detect dangerous heart

ABOVE: Kia Manawanui Trust
CEO Letitia Harding and Minister of Health Hon Simeon Brown
conditions early - before it’s too late - so we are trying to place as many lifesaving mobile ECGs into medical centres across New Zealand as we can. Find out more about delivering a mobile ECG to a community in need on page 17.
Thank you all for travelling on this cardiac journey with us. We are excited to extend our expertise into the cardiac space, and we look forward to another exciting year in 2026!
Noho ora mai,
Letitia Harding
Kia Manawanui Trust – The Heart of Aotearoa NZ Chief Executive
MEET THE EXPERTS GUIDING OUR MISSION

Dr Sarah Fairley – Medical Director of Kia Manawanui Trust
Sarah qualified from Queens University Belfast in 2002 and trained at the Belfast Trust. She completed a PhD in 2011 and finished her higher specialist training in 2014 prior to undertaking an 18-months fellowship in interventional cardiology from 2014–2015. Sarah has worked as an interventional and obstetric cardiologist at Wellington Hospital since then. Sarah’s areas of interest are coronary stenting, coronary artery disease, intravascular imaging, heart disease in pregnancy, rheumatic heart disease and spontaneous coronary dissection. Sarah is the Medical Director of Kia Manawanui Trust and has been Chair of the Cardiac Intervention Group since 2022.
Professor Martin Stiles
Martin Stiles is Director of Electrophysiology at Waikato Hospital and Professor of Medicine at the University of Auckland. He is the Chair of the NZ Division of the Cardiac Society of Australia and New Zealand (CSANZ). Martin chairs the CSANZ Scientific Committee (the first New Zealander to do so) and sits on the Executive Board of the Asia-Pacific Heart Rhythm Society. He has chaired International Expert Consensus Documents on the Investigation of Cardiac Arrest and on ICD Programming.

Dr Adèle Pope
Adèle Pope grew up in small New Zealand towns in the Bay of Plenty and South Auckland before studying medicine at the University of Auckland. Her PhD looking at how high blood pressure changes the heart structure leading to heart failure, which lead her to specialise in cardiology in Auckland before travelling overseas to learn advanced cardiac imaging skills. Adèle has since moved to Hawke’s Bay to help address the inequities in cardiac health care provision in regional New Zealand.

Dr Jennifer Roberts
Jennifer is a registered nurse leader with clinical expertise in cardiology. Jennifer works in clinical practice, in leadership and governance roles and has extensive experience in nursing education. She holds a range of postgraduate qualifications in critical care nursing, tertiary education, is a Master of Nursing and Doctor of Education. Jennifer is an advocate for advanced nursing practice and ensuring nurses in these roles are integral to cardiology service delivery in every region in Aotearoa.

Dr Marcus Lee
Dr Marcus Lee is a senior interventional cardiologist and Clinical Lead for Cardiology in Te Tai Tokerau. He has spent the past decade developing and strengthening cardiac services across Northland, including establishing the Whangārei Cath Lab and driving change that have improved access to timely care for rural and Māori communities. Marcus is an Honorary Senior Lecturer with the University of Auckland and has represented New Zealand on the CSANZ Interventional Working Group.

Dr Andrew Chatfield
Andrew studied medicine at the University of Otago, qualifying in 2010. He completed his cardiology training at Auckland City Hospital, attaining FRACP in 2020. He then undertook a two-year fellowship in Coronary and structural heart disease at the renowned St. Paul’s Hospital in Vancouver, Canada. Andrew returned to New Zealand in 2022 and has since worked full-time as a cardiologist in the Wellington region. He also is an expert in the field of structural heart disease interventions including Transcatheter Aortic Valve Implantation (TAVI), Transcatheter Edge-to Edge Repair (TEER), ASD and PFO closure.

Johanna Lim
Johanna is a Clinical Pharmacist (Cardiology Expert) and Pharmacist Prescriber, currently working in several general practices. In addition to being a member on the Cardiac Society of Australia and New Zealand (CSANZ) AHST executive council, Johanna was also the first pharmacist to be elected as fellow of CSANZ. Johanna also holds other multiple roles, including teaching the cardiovascular module for the University of Auckland Postgraduate Diploma in Clinical Pharmacy and co-lead of the NZHPA Cardiology SIN group.

Samantha Cashell
Samantha is a Cardiac Physiologist with a strong background in heart health and patient care. She completed a Health Science degree and a Postgraduate Diploma in Medical Technology, specialising in Cardiology, at the University of Otago. She later worked at St Thomas' Hospital in London, gaining valuable experience with intravascular imaging such as Intravascular Ultrasound and Optical Coherence Tomography. Samantha now works at Wellington Regional Hospital, where she focuses on using imaging tools more effectively in the cath lab to support the team and improve patient outcomes.
Dai Te Wiata
Dai Te Wiata is a Clinical Nurse Specialist in heart failure at Waikato Hospital, focusing on specialised cardiac care for the Waikato and Midlands area. Dai works mainly in the community, holding nurse-led clinics to eliminate barriers to clinic attendance such as cost, transport difficulties, parking. Being Maaori assists Dai in connecting with whanau who might otherwise have been marginalised to help address ethnic disparities.
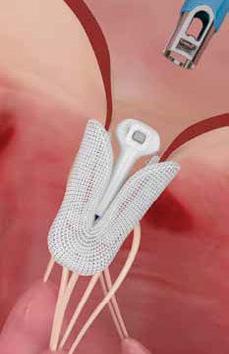
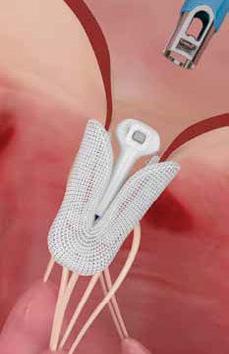
OPEN-HEART SURGERY ALTERNATIVE:
WHAT ONE DEVICE CAN DO FOR HIGH-RISK PATIENTS
OPEN-HEART SURGERY has traditionally been the standard for repairing leaking mitral or tricuspid valves, but it involves considerable risks and a long recovery.
Older adults are often ruled out as candidates due to being considered too high-risk; however, for these patients, Transcatheter Edge-to-Edge Repair (TEER) provides a potential, less invasive alternative with a quicker recovery.
In New Zealand, access to TEER is severely restricted in the public system, leaving many high-risk patients without treatment options.
Dr Andrew Chatfield, a consultant in Coronary and Structural Interventional Cardiology and a member of the Cardiac Advisory Board at Kia Manawanui Trust – The Heart of Aotearoa,
believes TEER is a revolutionary procedure for treating mitral valve regurgitation.
Mitral valve regurgitation is a common but serious condition that if, left untreated, can lead to severe complications, including heart failure and death.
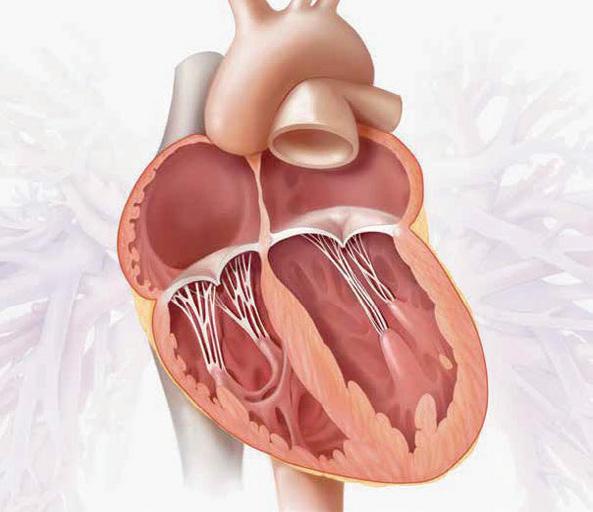
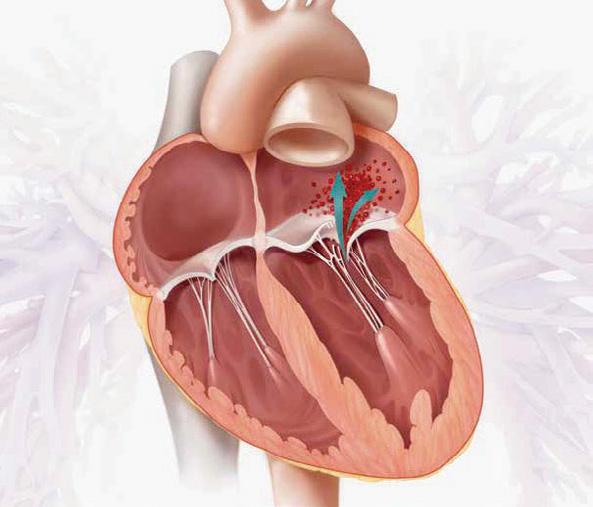
What is mitral valve regurgitation?
Mitral regurgitation (MR) occurs when the mitral valve fails to close properly, causing blood to leak backward and forcing the heart to work harder.
Around 2-5% of the population, and 8% of people over 75, are affected.
The symptoms, shortness of breath, fatigue, and a reduced ability to perform daily tasks, can
progress to pulmonary oedema, heart failure and eventually death if left untreated.
Open-heart surgery is the usual treatment for severe MR, but many high-risk patients cannot undergo it.
In New Zealand, nearly 50% of patients with MR are not offered surgery, particularly those over 75 with additional health issues such as kidney or lung disease. For these patients, the outlook is poor, with worsening quality of life, repeated hospitalisations, and increased risk of stroke.
Without intervention, MR can reduce life expectancy more than many malignant cancers, with half of severe MR patients over 75 dying within five years.


ABOVE: Consultant in Coronary and Structural Interventional Cardiology Dr Andrew Chatfield is also a member of the Cardiac Advisory Board at Kia Manawanui Trust – The Heart of Aotearoa.
The benefits of TEER
TEER offers these patients a lifeline.
For those considered “too high risk” for surgery, the only alternative is palliative care.
“For these people, TEER can be lifesaving,” Dr Chatfield says.
Globally, more than 300,000 patients have benefited from TEER.
Research shows that TEER reduces repeat hospital admissions by up to 60 percent, frees up intensivecare beds, and dramatically improves quality of life.
Patients are typically discharged the next day – a stark contrast to the week-long hospital stays and months-long recoveries that follow open-heart surgery.
New Zealand is lagging behind, Dr Chatfield says.
“Internationally, TEER is the standard of care for patients with significant mitral regurgitation who are at high surgical risk.
“It’s publicly funded in places like Canada and Australia,
but here it’s largely confined to the private sector or a few compassionate cases in the public system,” he says.
“We have the technology, we have the expertise, and we have patients who desperately need it. What’s missing is public funding.”
Research
shows that TEER reduces repeat hospital admissions by up to 60 percent, frees up intensive-care beds, and dramatically improves quality of life.
During his fellowship in Vancouver, Dr Chatfield performed structural heart procedures on a weekly basis, including regular TEER cases.
In Wellington, however, he has not been able to perform a single TEER, despite identifying many suitable patients upon his return to New Zealand.
The latest 2025 guidelines from the European Society of Cardiology and the European Association for Cardio-Thoracic Surgery, emphasises early intervention with TEER for patients with mitral regurgitation.
Current funding status
Right now, TEER isn't funded by the Ministry of Health in New Zealand.
Some TEER devices are already available in New Zealand for high-risk patients, yet without government support, access remains limited to those who can pay privately.
"This leaves us in a position of telling some of our most vulnerable patients that they either need to risk open-heart surgery or go without,” Dr Chatfield says.
Patients in New Zealand deserve access to TEER, he says.
“It’s time we brought our standards in line with the rest of the world.”
New Zealand’s failure to fund TEER isn’t just medically outdated – it’s economically irrational, he says.
“The cost of repeated hospital stays, ambulance transfers, and long rehabilitation far outweighs the cost of the procedure itself.
“When you look at the big picture, funding TEER is not just the compassionate choice – it's a financially sensible one.”
BELOW: Dr Andrew Chatfield holding the PASCAL Precision implant system.

ROBERT'S JOURNEY
A MISSED OPPORTUNITY
FOR ROBERT HAMLETT, the price of saving his heart has been living with constant pain — and knowing it didn’t have to be this way.
At 83, Robert should have been offered a safe, modern, non-invasive option to fix his failing heart valve.
Instead, he was told the only publicly funded treatment available in New Zealand was open-heart surgery – a risky procedure that literally stops the heart and cracks open the chest.
“I didn’t have a choice,” he says.
“They told me it had to be done and that it was my only option.”
Robert, of Wellington, learnt he had a heart condition when he went into hospital for a hernia operation.
He was told by doctors that they would keep an eye on it, but treatment was not needed at that time.
As the years went on, his condition deteriorated, and he was told he needed to have open heart surgery.
His cardiologist mentioned there was another option available – a minimally invasive procedure called Transcatheter Edge-toEdge Repair (TEER) - but that he would have to fund it himself at a cost of $60,000 - $80,000.
Robert underwent openheart surgery in May 2024.
Rather than feeling stronger and healthier post-surgery, what followed was pain, fear, and months of struggling to reclaim a normal life.
Since his operation, he’s been rushed to hospital eight times – twice by ambulance.
“I’ve been cut across and down my chest, and I’ve had pains in
there – really intense pains – and there is a lump there now too.
“I get nose bleeds, I feel a bit unsteady on my feet, I often forget things and I feel overwhelmed,” he says.
“My family think of me as an invalid now."
For Robert, the frustration is more than physical – it's financial too.
“If TEER had been done through my leg, I don’t think any of this would have happened – I wouldn’t have been rushed off in ambulances because of the pain from that surgical cut.

“But it’s more than that. Each trip costs the system money."
Robert hopes that TEER will become widely available in New Zealand to prevent others having a similar experience to him.






Level One Coronary Intravascular Imaging Certification Course Director, Professor Scott Harding, conducts a lecture.
NEW COURSE DELIVERS LIFE-SAVING HEART TECHNIQUES THAT HALVES DEATHS
IN JULY, Kia Manawanui Trust –The Heart of Aotearoa welcomed 30 cardiologists from across New Zealand and Australia to become certified in advanced cardiac imaging techniques - Optical Coherence Tomography (OCT) and Intravascular Ultrasound (IVUS).
These powerful techniques provide detailed 3D images from inside coronary arteries, enabling more precise stent placement and significantly improving patient outcomes –reducing cardiac deaths by 45%.
This first-of-its-kind course in New Zealand and Australia wouldn’t have been possible without the Transcontinental Coronary Imaging and Physiology Club (TCIP), the Asian Pacific Society of Cardiology (APSC), and the support of our generous
sponsors, Abbott, BioExcel Australia & New Zealand, Boston Scientific, Philips and Terumo.
A huge thank you to all the brilliant cardiologists who joined us.
At Kia Manawanui Trust, we believe every New Zealander deserves access to the highest standard of heart care, and this training is an important step toward making that a reality.
BELOW: (From left) Trust CEO Letitia Harding, Interventional Cardiologist Dr Andrew Chatfield, Trust Medical Director Dr Sarah Fairley, Cardiac Physiologist Samantha Cashell



NEW REPORT REVEALS GRIM REALITY OF HEART HEALTHCARE IN NZ
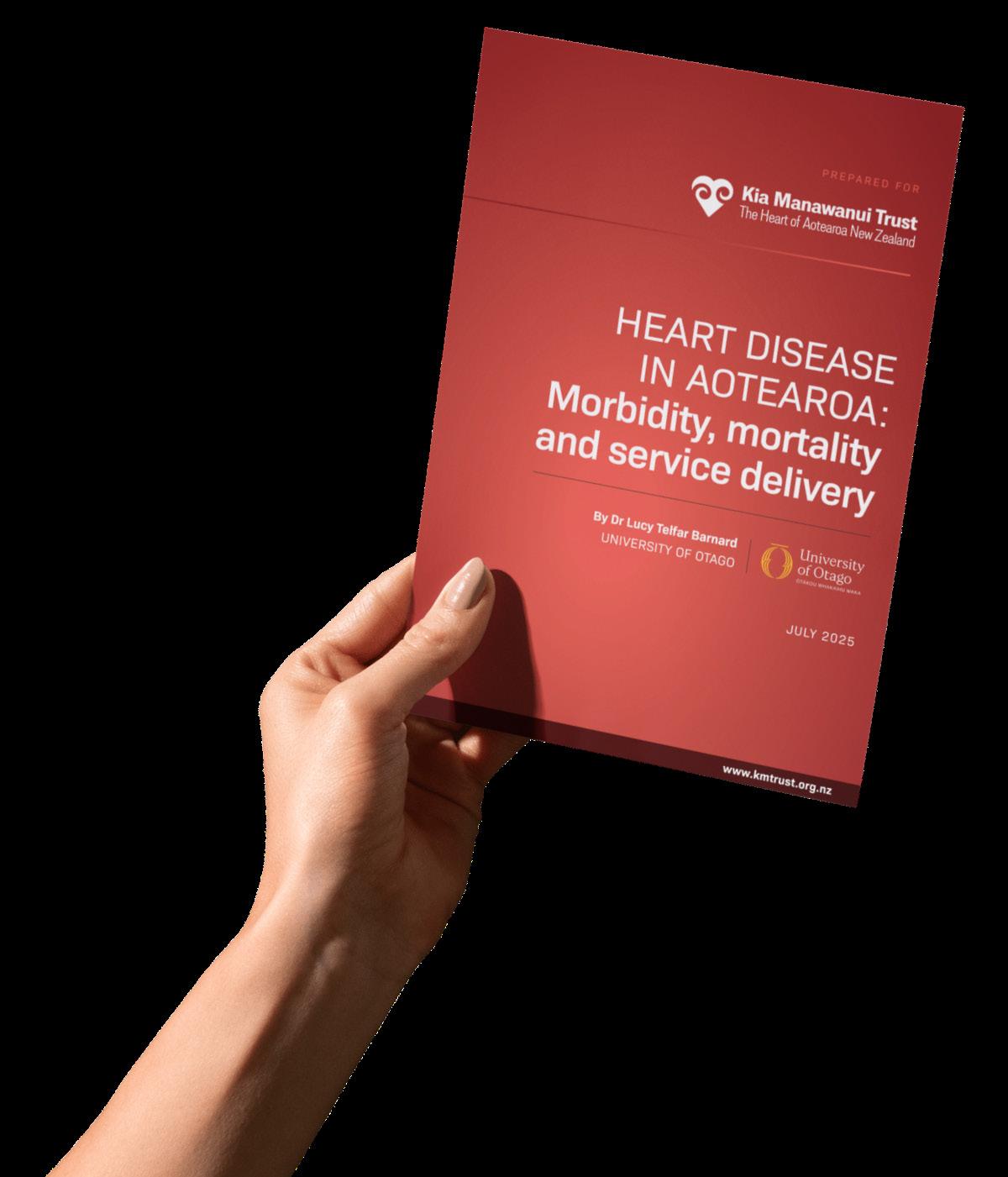
A damning new report has exposed deep flaws in New Zealand’s heart healthcare system, where access to life-saving treatment often depends on luck, postcode, and ethnicity rather than clinical need.
COMMISSIONED BY Kia Manawanui Trust and prepared by the University of Otago, the report reveals a system plagued by chronic under-resourcing, critical workforce shortages, and deadly inequities.
Trust Chief Executive Ms Letitia Harding says the report lays bare a system that is failing at every level.
“Heart care in New Zealand isn’t just stretched – it’s on the verge of collapse.
"We are failing in all aspects, and it's costing New Zealanders their lives.”
Key findings from the Cardiac Impact Report include:
Ǫ Life-threatening delays: Half of all heart attack patients aren't seen within internationally accepted timeframes.
Ǫ Alarming workforce shortage: New Zealand has only a third of the cardiologists it should have.
Ǫ Systemic inequality: Māori and Pacific people are hospitalised or die from heart disease more than a decade earlier, on average, than other New Zealanders.
Ǫ The financial burden: Heart disease costs the country's health system and economy $13.8 billion per year
Ǫ A postcode lottery for care: Regions with the highest death rates - Tairawhiti, Lakes, Whanganui, and Taranaki - have the fewest cardiac specialists.
Ǫ The deadliest conditions: Heart disease accounts for 20% of all deaths in New Zealand. The five heart conditions responsible for the majority are: heart failure, atrial fibrillation and flutter (AFF), acute myocardial infarction (AMI), subsequent myocardial infarction and cardiomyopathy.
Trust Medical Director Dr Sarah Fairley, who is also a Wellingtonbased cardiologist, says the

findings match what frontline clinicians see every day.
“From inside the system, I can tell you that this report reflects what we see every day: a workforce stretched beyond safe limits, patients slipping through the cracks, and no end in sight.”
New Zealand has only one third of the cardiologists needed by international standards.
Ms Harding says this report should be a wake-up call for the Government.
Kia Manawanui Trust is calling for an urgent government response, including immediate investment in public hospital cardiac care infrastructure –beds and equipment – and a national strategy to recruit and retain cardiology staff.
Scan the QR code below or head to kmtrust.org.nz/ cardiac-impact-report
Trust Medical Director Dr Sarah Fairley says patients are slipping through the cracks with no end in sight.
Call to fund much-needed heart failure treatments
Half of the patients diagnosed with heart failure will die within five years if proper medical therapy is not started.
THAT’S THE STARK reality from Interventional Cardiologist Dr Sarah Fairley, who is also the Medical Director of Kia Manawanui Trust.
In New Zealand, heart failure is one of the most common reasons people are admitted to hospital.
Nearly 25% of patients admitted for heart failure also face an unplanned re-admission within just 30 days.
Even more worrying is the high risk of death after a person's first hospitalisation.
“Current statistics show that half of the patients diagnosed with heart failure will be dead in five years, which is truly shocking, and we need to do something about that,” Dr Fairley says.
Heart disease is the leading cause of death in New Zealand. Every 90 minutes, someone dies from heart disease in New Zealand.
Heart disease affects about 2 to 3% of all adults and more than 10% of those over 70, with a growing disparity among Māori and Pacific populations.
Māori experience a roughly 2.3 times higher rate of heart failure compared to non-Māori.
Starting the best treatment for heart failure early, when someone is first diagnosed, can significantly boost their quality of life and extend their lifespan, Dr Fairley says.
However, currently, in New Zealand, the most effective treatment for heart failure isn’t funded for everyone.
What is heart failure?
Heart failure means the heart isn’t pumping as effectively as it should, making it harder for the body to receive the oxygen-rich blood it needs.

Different types of heart failure
Ǫ Heart failure with reduced ejection fraction (HFrEF): The most common type - heart failure with reduced ejection fraction (HFrEF) - involves a weak heart muscle that can’t pump effectively, causing fluid to build up in the lungs, legs, or abdomen. In New Zealand, it's often caused by ischaemic heart disease damaging the heart muscle due to poor blood flow.
Ǫ Heart failure with preserved ejection fraction (HFpEF): The other type - heart failure with preserved ejection fraction (HFpEF) - occurs when the main pumping chamber (the left ventricle) pumps blood properly but cannot relax properly, leading to breathlessness. It’s more common in people with longterm uncontrolled high blood pressure or in older patients.
Managing heart failure: The 'four pillars’ of treatment
The two types of heart failure are managed similarly with GuidelineDirected Medical Therapy (GDMT), also known as the 'four pillars' of heart failure treatment.
The ‘four pillars’ are critical in managing symptoms and slowing the progression of the disease.
While most of the treatments are funded, there are some
with restrictions – and that has cardiologists around the country advocating for full funding.
Dr Fairley says cardiologists know the ‘four pillars’ approach works.
“Life expectancy increases with the 'four pillars' of heart failure treatment.
“For example, in a 55-year old, using all 4 classes of medications provides 8.3 additional years free of cardiovascular death or first hospitalisation for heart failure."
Prevention is crucial, she says.
“The 'four pillars’ medications keep people out of hospital and improve quality of life. If we treat patients early, we can genuinely make a big difference.
“We need access to medications for both treatment and prevention to keep our communities healthier, to save lives, and to reduce hospitalisations.”
Current funding status
Currently, three of the four pillars of heart failure treatment are generally funded, while the other is only funded with special authority restrictions. In Australia and the UK, the drug is available to patients regardless of their heart’s function.
“The 'four pillars’ medications keep people out of hospital and improve quality of life. If we treat patients early, we can genuinely make a big difference."
Guideline-Directed
Medical Therapy (GDMT) or the ‘four pillars’
Ǫ RAAS blockers (ACE inhibitors, ARBs, or ARNIs): These are standard first-line agents in heart failure therapy and are generally funded in New Zealand.
Ǫ Beta blockers: These are also widely used for heart failure in New Zealand. There are currently three funded beta-blockers.
Ǫ Mineralocorticoid Receptor Antagonists (MRAs): Medications are generally funded for heart failure.
Ǫ SGLT2 inhibitors: While previously only funded for type 2 diabetes, they are now also funded for heart failure with reduced ejection fraction (HFrEF) with Special Authority restrictions. This means patients need to meet specific criteria to be eligible for funded access.

Trust Medical Director
says cardiologists know the ‘four pillars’ approach works, but not all medications are fully funded in New Zealand.
Dr Sarah Fairley

RSV, SHINGLES, & YOUR HEART
LIVING WITH HEART disease, diabetes, or COPD means your body may be more vulnerable when common viruses strike. What might feel like a passing illness for one person can sometimes trigger serious complications for someone with an ongoing condition. The good news is there are practical ways to lower those risks – vaccination, regular check-ups, and being mindful about exposure to illness all help reduce the risk of complications and support your overall health.
RSV: More than just a cold
Respiratory Syncytial Virus (RSV) is widespread in Aotearoa, especially during winter. For most people, it’s unpleasant but manageable – coughs, fever, a runny nose. But older adults or those with weakened immune systems can end up with far more serious outcomes.
Research shows that people admitted to hospital with RSV often face acute cardiac events, and the infection may raise the risk of future heart failure. For anyone already living with heart disease,
RSV can quickly escalate from a nuisance to a medical emergency. Vaccination against RSV is now available and offers a useful safeguard for those most at risk.
Shingles: The virus that never really leaves
If you had chickenpox as a child, the virus didn’t disappear – it stayed in your nerve cells, waiting. Later in life, it can resurface as shingles. Roughly one in three people will experience shingles at some point, with the likelihood climbing as we age or if our immune system is weakened by conditions like heart disease, diabetes, or arthritis.
While some people experience only a mild rash, others face severe pain, eye complications, or postherpetic neuralgia – nerve pain that lingers long after the rash fades. Emerging studies even suggest shingles might increase the risk of cardiovascular events, raising new questions about its wider impact on heart health.
Viruses may seem routine, but if you have a pre-existing heart
condition, they deserve serious attention. If you feel unwell, contacting your healthcare provider early can prevent complications. Pairing that vigilance with regular checkups and recommended vaccines is a simple but powerful way to protect your long-term health.
Breakout box: Current vaccine funding status
In Aotearoa, the Shingrix® vaccination is funded at age 65 and given in two doses. It is recommended (though not funded) from age 50 onwards. Shingrix is funded for certain immunocompromised individuals aged 18 and older who are at increased risk of shingles.
RSV vaccines, including Arexvy®, are available in New Zealand but are not government funded.
This article has been created with financial support from GlaxoSmithKline (NZ) Ltd, and has not had any involvement in the content.
SMALL DEVICE WITH BIG IMPACT FOR COMMUNITIES IN NEED
THOUSANDS OF KIWIS may be living with an undiagnosed heart condition that could put their lives at risk.
Atrial fibrillation (AFib) is a serious heart condition that can lead to stroke and heart failure if undiagnosed. It affects 1 in 35 Kiwis aged between 35 and 74.
Yet, many communitiesparticularly rural areas and among Māori and Pacific people - lack access to heart scan devices (Electrocardiograms, or ECGs) that can detect AFib in about 30 seconds and prevent lifethreatening complications.

work with Pacific patients, have already had some amazing results – identifying AFib in two patients.
Trust Chief Executive Ms Letitia Harding says Māori and Pacific people are disproportionately impacted by AFib, and are diagnosed 10 years younger than other ethnicities.
"Early detection of AFib, which mainly affects our most vulnerable communities, can ultimately save lives. That’s why we want to help."
The campaign is more than just funding a piece of medical equipment, she says.
That’s why Kia Manawanui Trust – The Heart of Aotearoa launched a campaign to get as many portable ECG devices into underserved communities
Another clinic in Hawke’s Bay, who work with Māori patients, has also had success – identifying an irregular heartbeat in one Scan the QR code below or head to kmtrust.org.nz/donate
"It’s about coming up with a practical solution to reduce the potential risks of stroke or heart failure that comes with undiagnosed AFib by speeding up access to diagnosis and treatment."


