
25 minute read
Improvements Driven by BC-Wide Committees

Kidney Care Committee (KCC)
Advertisement
Transplant First moves towards implementing enhanced pre-transplant clinical processes across BC

Featured Accomplishment
Receiving a kidney transplant is the best treatment option for many people facing kidney failure. The Transplant First initiative, a collaboration between BC Renal and BC Transplant, is focused on standardizing pre-transplant processes. This is to ensure every kidney patient who is a potential transplant candidate is identified, assessed and supported along the path toward transplantation, including assistance in finding a living donor.
An important part of the pretransplant process is establishing roles and responsibilities of the various kinds of health professionals involved and supporting better communication across settings and teams as well as with patients. Doing so provides clarity on where patients are at in the process and on who is doing what at each step along the way.
With the launch of the second phase of Transplant First, a
steering committee and various working groups were established, including participation from clinician and administrative groups across kidney care clinics, regional transplant clinics and the provincial transplant centres as well as patient partners.
The dedication and collaborative spirit among these groups to provide input and support this work has been tremendous. In just over a year’s time, the following has been accomplished:
• Pre-transplant processes standardized and agreed upon
• A project evaluation plan created and approved
• PROMIS updates to support new processes developed
• A full education and implementation plan crafted
As the initiative moves towards implementation in 2022, the project team looks forward to the ongoing support from staff at the various clinics and centres involved to ensure a successful launch and sustainment of the standardized processes.
Other Key Initiatives
Implementation of a Home Blood Pressure Monitoring initiative in KCCs
Integration of virtual care into the KCC service delivery model, with an evaluation of the impact on quality of multidisciplinary chronic kidney disease care and patient-provider interactions and relationships (evaluation is in progress)
Evaluation of the provincial ADPKD initiative to assess standardization and delivery of care for patients with ADPKD in the KCC setting, including creation of the first ADPKD annual report “It’s been a great learning experience to work with clinicians and administrative groups from both renal and transplant who are part of the Transplant First initiative. As we worked together, we were able to build greater awareness of each other’s experiences through the pretransplant process and how working together will better support patients through this journey.”
- Sharon Gradin, Project Manager

Drs. Mike Bevilacqua, Olwyn Johnston & Jag Gill, Transplant First Co-Chairs
Web info & resources:
BCRenal.ca Health Professionals Clinical Resources Kidney Care (Non-Dialysis)
Committee background:
Terms of Reference
Glomerulonephritis (GN) Committee
Web info & resources:
BCRenal.ca Health Professionals Clinical Resources Glomerulonephritis
Committee background:
Terms of Reference “A lot has been done to ensure that patients living with chronic kidney disease are properly supported and connected to groups of similar patients. But it is the first time in BC that we have a group of organizations working together to better understand the support and connection needs of patients living with GN – a condition that is relatively rare and often leads to patients feeling isolated and under-supported. Our ultimate goal is to build a BC-centred empowerment network and library of resources that will help such patients feel connected and supported and will inspire them to better advocate for their care.”

-Dr. Sean Barbour, GN Committee Chair
Featured Accomplishment
GN Committee conducts a support needs assessment of people living with GN in BC
People living with rare kidney diseases, such as various types of glomerulonephritis (GN), may lack connection to appropriate community resources and social support, and feel isolated in managing their chronic condition. To better understand these needs of patients and family caregivers living with GN in BC, the GN Committee and BC Renal partnered with the Kidney Foundation of Canada – BC and Yukon Branch and formed a working group with representatives of these organizations, including clinicians, administrators, quality improvement experts and patient partners. The working group designed and conducted two virtual focus groups and several individual virtual interviews with GN patients and their family members. The content from the focus groups and interviews was analyzed for common themes related to perceptions about support needs and what support might look like for patients and families living with GN. Various types of support were highlighted by participants: • informational support • emotional support • appraisal support • support for enabling person- and family-centred GN care When a patient is newly diagnosed or experiencing an abrupt decline in health, they may need more support. All focus group and interview participants recognized that peer support can be helpful as it encompasses informational, emotional and appraisal support, and may help enable a holistic approach to GN care through enhanced connection, reduced uncertainty of what to expect in the kidney journey and better understanding of health information.
Based on the results of the analysis, the working group is currently developing a support strategy for GN patients and family caregivers with a particular focus on establishing a BC-focused support network, patient resources and peer support options and opportunities.
Other Key Initiatives
Developed and implemented pneumocystis jirovecii pneumonia prophylaxis guidelines for patients living with GN who are treated with immunosuppressant medications
Developed and implemented a rituximab funding policy for patients living with membranous nephropathy
Developed a strategy to handle the entry into the Canadian market of rituximab biosimilar drugs

Home Hemodialysis (HHD) Committee
Web info & resources:
BCRenal.ca Health Professionals Clinical Resources Home Hemodialysis
Committee background:
Terms of Reference “I am very excited to see the results of the CRASH curriculum. It is a novel way of approaching patients who start dialysis in an unexpected manner. Traditionally, these people remain on facility-based hemodialysis. I am hopeful we can start to optimize home dialysis care for these folks.”

- Dr. Mike Copland, Provincial HHD Medical Director
Featured Accomplishment
CRASH curriculum developed and piloted to support patients with unplanned and suboptimal dialysis starts
The Curriculum to Recruit Acute Starts to Home Dialysis (CRASH) project restarted in April 2021 to better support the needs of unplanned hemodialysis patients with little or no modality selection education. These patients often get missed in the usual education channels of the kidney care clinic, and face increased levels of challenges and anxiety.
This curriculum outlines home dialysis education and transition in three phases using a standardized approach. Nurse navigators applied this approach to guide and support informed, patient-centred modality selection decisions.
Other Key Initiatives
Provincial rollout of AK 98 equipment initiated
Development of the Provincial Key Clinical Quality Indicators report specific to home hemodialysis “Never before have we managed to see the pathways with such detail for these folks who start in a suboptimal manner. This information will help inform leadership regionally and provincially about the true population of patients who could be successful on home therapies.”
- Dr. Mike Copland, Provincial HHD Medical Director
CRASH Patient Journey to Home Dialysis
CRASH
Curriculum to Recruit Acute Starts to Home “I’m not feeling well… I have just found out I have advanced kidney disease and need urgent dialysis."
1. Dialysis Stabilization
May include: medication & dialysis prescription adjustments, blood pressure management, goal setting, introduction to kidney options.
Visit BCRenal.ca to learn more about kidney care and treatment options
Within week 2
Within week 4
5. Home Dialysis Training
May include: peritoneal dialysis or home hemodialysis training, dialysis access support and monitoring, home visits from the kidney team.
Within week 6 2. Home Dialysis Introduction
May include: introduction to self-care, home dialysis options, dialysis access care, peer support, tour of home dialysis training unit.
3. Meet the Home Dialysis Team
May include: consultation with home dialysis nurse, nephrologist and social worker. Work with care team to formalize a treatment plan.
6. Home Dialysis
• Ongoing dialysis treatment at home • Regular clinic follow-up • Dialysis Access Support and Monitoring • Other supports and services
After 6 weeks
4. Monitor
May include: further stabilization on hemodialysis, dialysis access monitoring, waiting for home dialysis training, and home assessment.
Kidney Team and Nurse Navigator
Works closely with you and your family to support you during your kidney journey
BC Renal Resources can be found at:
BCRenal.ca ⊲ Health Info • Learn about Treatment Options • Transitions in Kidney Care • Managing your Care • Mental Health • Home Dialysis Curriculum
If you have any questions, please contact your Nurse Navigator at:
the northern way of caring Nurse Navigator: Contact Info: Aim your cell phone camera at this code
or visit:
BCRenal.ca ⊲ Health Info ⊲ Learn About Treatment Options ⊲ Home Dialysis Curriculum
Peritoneal Dialysis (PD) Committee

Web info & resources:
BCRenal.ca Health Professionals Clinical Resources Peritoneal Dialysis
Committee background:
Terms of Reference
Key Initiatives
Home fellowship with a provincial focus
5-year review of the PD Assist program
Featured Accomplishment
BC rollout of the AMIA with Sharesource cycler machine completed
The provincial rollout of the Baxter AMIA with Sharesource cycler to each regional health authority PD program was completed in 2021. Despite the challenges posed by pandemic restrictions, this project continued strong and added virtual nurse training where possible. In the past year, Island Health, Fraser Health, Northern Health and Providence Health Care PD programs finalized training, and the programs are embracing remote monitoring to support assessment and evaluation of PD treatments.
“Timing of the introduction of the AMIA cycler was fortuitous. The main advantage is its ability to relay important information between patients and the care team without in-person clinic visits or calls. While we never anticipated a scenario where this would be ‘mandatory,’ having it available this year ensured that patients and their families felt well supported. It is another tool to help understand how home dialysis is going and how we can help", says Dr. Suneet Singh, Provincial PD Medical Director.
In 2022, the PD Committee will focus on expanding knowledge about how best to use this technology to support PD care across the province. “Our PD committee has had many important provincial projects over the last few years, but I am especially proud of the PD community for the success of implementation of the new AMIA cycler machine despite the many challenges of the COVID-19 pandemic. Each PD program across the province made the AMIA cycler rollout a priority to complete by the end of 2021 despite having to alter their day-to-day practice to continue to care for patients doing dialysis at home.”
- Dr. Suneet Singh, Provincial PD Medical Director

About the AMIA cycler
The AMIA cycler machine supports patients in managing their PD therapy at home with features such as voice guidance, a touchscreen control panel and the Sharesource remote patient management platform.
Sharesource allows members of the kidney care team to securely view their patients’ recently completed treatment data, and enables them to remotely adjust their patients’ prescription without requiring them to travel to the clinic.
Hemodialysis (HD) Committee
BC’s hemodialysis units adapt to changing COVID-19 requirements

Featured Accomplishment
The Hemodialysis Committee worked with kidney and infection control practitioners across BC to support HD units in navigating the ever-changing waters of the COVID-19 pandemic. While many health care services could be delayed or offered in another way during the pandemic, HD treatments are life-sustaining and require patients to travel to a hospital or community dialysis unit three times weekly. Services need to continue without interruption throughout the pandemic, regardless of risk factors and/or COVID-19 status. To support the HD units, the committee developed the following:
• A provincial guideline for the screening and management of HD outpatients during the COVID-19 pandemic (with regular updates as the pandemic situation changed)
• A provincial guideline for the use of personal protective
equipment (PPE) for vascular access-related activities during the COVID-19 outbreak
• A provincial guideline for travelling HD patients during the COVID-19 pandemic (with regular updates as the pandemic situation changed)
• A standardized COVID-19 screening questionnaire.
Every patient is screened for COVID-19 symptoms at every HD treatment. This data is used to identify infection control precautions above and beyond the usual precautions for HD patients, as well as whether laboratory testing for
COVID-19 is recommended.
Screening data is entered into the PROMIS information system and trends are analyzed in combination with laboratory results.
• Several provincial resources for HD patients about changes to processes during the
COVID-19 pandemic (e.g., Q&A sheet, use of masks)


Dr. John Antonsen, Chair of the Hemodialysis Committee says, “The guidelines and patient resources developed as part of the HD Committee COVID-19 response were utilized by HD units across BC to promote best practices in HD care. In developing these tools, we considered available evidence as well as real life experience to optimize both patient and staff safety during the COVID-19 pandemic. Discussions and decisions were carried out collaboratively, after a review of the evidence and experience of clinicians working on the ‘front line’ with patients.”
Other Key Initiatives
Recruiting up to 3 patient partners to participate on the committee to bring a new and important dimension to the committee’s direction and work
Developed a new guideline on dialyzer selection, with clinical requirements, contractual obligations for provincial dialyzer use and cost all considered in the selection algorithm
Vascular Access Educators Group worked with the PROMIS team to implement an updated Dialysis Access module in PROMIS “It has been very rewarding to have the opportunity to work with a group of kidney and infection control practitioners on such an important and timely initiative that impacts the everyday life of patients on hemodialysis. We have had to evolve our thinking and decisionmaking in ‘real-time’ to stay in sync with the evidence.”
- Dr. John Antonsen, Chair, Hemodialysis Committee
Hemodialysis Patients
Flu & Novel Coronavirus (COVID-19) Important Information for Kidney Patients PD and Home Hemodialysis March 12, 2020 To help keep everyone safe and provide you with the best care during influenza and coronavirus season, we are providing this handout to patients with kidney disease who attend: We ask everyone to wear a mask: When walking through public areas on your way to dialysis When in common areas such as the waiting room or hallway When you are on dialysis and are not eating or drinkingMasks are recommended as a barrier to help prevent respiratory droplets from traveling into the air when the person wearing the mask coughs, sneezes, or talks. They are not recommended for people with difficulty breathing or who cannot remove the mask without help. Key points about masks Wash your hands before putting on a mask Do not touch the mask when you are wearing it Wear masks with two or more layers (preferably 3) Wear the mask over your nose and mouth and secure it under your chin If you wear glasses, use a mask that has a nose wire.
How to wear a mask:
1
PD clinics •
Home hemodialysis clinics We want to reassure you that your care will continue. We’re here to help and support you. Please read this handout carefully. Also please make sure the clinic you visit has your current
contact information. In the weeks ahead, your clinic visit may be changed to a virtual visit rather than in-person – for example, it may be conducted by telephone. This will ensure you are not exposed to crowded waiting rooms and other people who might be sick. Your nephrologist will determine if it’s best to see you in-person. What to do before you come to the clinic If you are scheduled for an in-person visit, please call the clinic if you have any of these symptoms (Clinic phone #: __________________)
•
• Fever Cough (new onset or worsening chronic cough)
• Difficulty breathing / shortness of breath If you have symptoms, you may be: •
Asked additional questions over the phone by a nurse and given instructions on what to do next •
Asked to postpone your appointment or provided the option of a virtual appointment
What to do when you get to the clinic Always clean your hands before entering the clinic. Hand sanitizers are available in the patient waiting area. If you have symptoms of the flu or COVID-19, clinic staff will direct you as to next steps. Web info & resources: BCRenal.ca Health Professionals Clinical Resources Hemodialysis
Committee background:
Terms of Reference
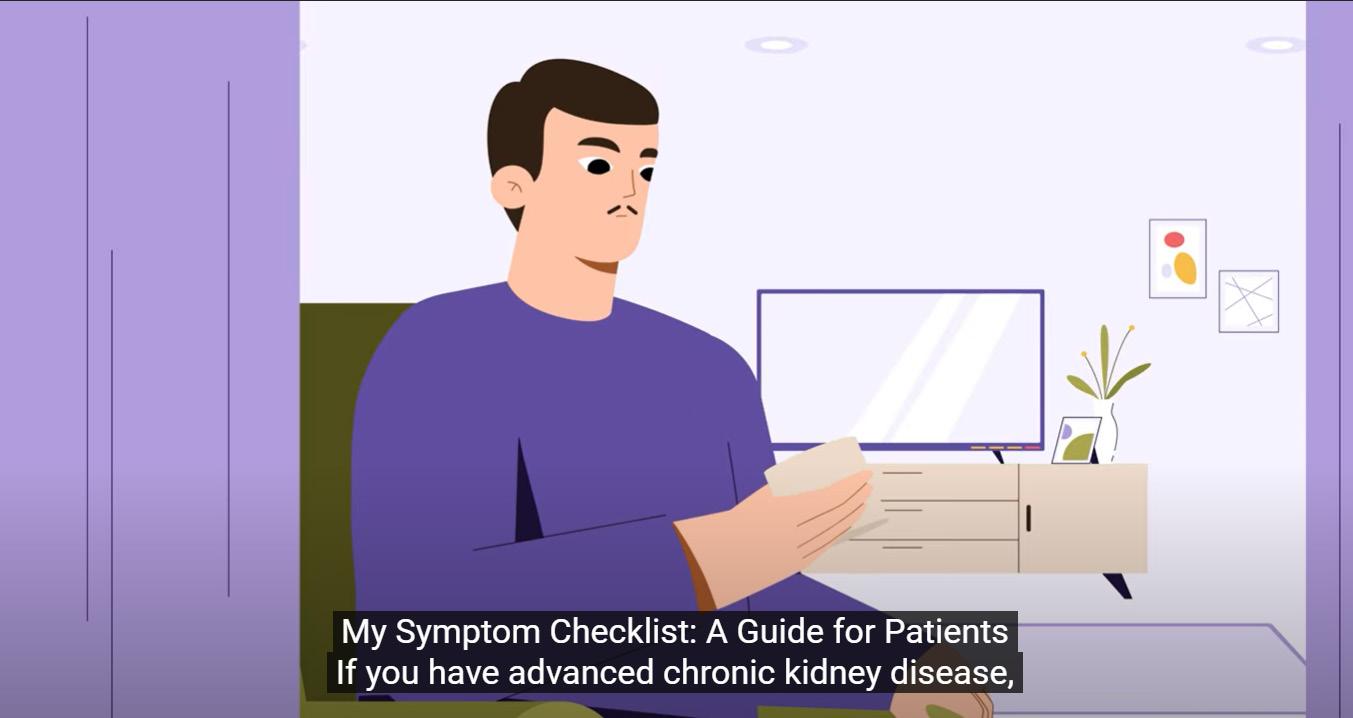
Watch the "My Symptom Checklist: A Guide for Patients" video here
PALLIATIVE CARE Committee
“Just watching the group come together to build this algorithm and this framework was quite remarkable. Everyone was worried, everyone was tired, no one knew where COVID was going – but the dedication this group put into this was really a joy to be a part of.”

Web info & resources:
BCRenal.ca Health Professionals Clinical Resources Palliative Care
Committee background:
Terms of Reference
- Sarah Thomas, Project Manager, speaking about the health professionals and patient partners who made up the working group that quickly mobilized to develop the BC Renal network ethical framework for dialysis allocation during pandemic times
Featured Accomplishment
Improvements made to symptom assessment and management through patient engagement
After key stakeholders identified areas of focus to improve the system assessment and management process, a multidisciplinary working group including patient partners was formed. This working group carried out several initiatives:
• Converted My Symptom Checklist into a fillable PDF (available in multiple languages) • Updated the clinician information sheet • Produced educational videos for clinicians and patients • Developed an original idea for a potential future patient portal that would include symptom assessment and management
Other Key Initiatives
Publication in the Clinical Journal of the American Society of Nephrology highlighting a first-of-kind initiative, Balancing the Needs of Acute and Maintenance Dialysis Patients during the COVID-19 Pandemic - A Proposed Ethical Framework for Dialysis Allocation; related story in BC Kidney Research in Focus, BC Working Group Creates Globally Unique Tool to Balance Acute and Chronic Dialysis Needs During Pandemic

“My favourite highlight of our work in 2021 was the opportunity to collaborate with patient partners. These dedicated individuals were instrumental in providing meaningful input that guided the significant improvements to My Symptom Checklist. This tool is used by kidney clinicians across all treatment options to assess and manage pain and symptoms experienced by patients living with chronic kidney disease. Enhancing symptom treatment will help optimize quality of life for our patients, which is a primary objective of the BC Renal Palliative Care Committee.”
- Dr. Gaylene Hargrove, Chair, Palliative Care Committee
PHARMACY & FORMULARY COMMITTEE

Web info & resources:
BCRenal.ca Health Professionals Clinical Resources Pharmacy & Formulary
Committee background:
Terms of Reference
Key Initiatives
New drugs were evaluated to guide the committee’s decisions around the medications BC Renal funds
Contracts were managed to minimize disruptions and other changes during the pandemic
Oral nutritional supplement funding was extended to kidney transplant patients as a pilot project to support patients in need
Featured Accomplishment
Anemia management protocols updated
Conceived 20 years ago, BC Renal’s anemia management protocols have undergone several changes over the years. These updates have not only reduced drug costs significantly but have also managed to get patients into target ranges sooner and stay within them longer. This avoids either the potential harm from too much drug intake or the drawbacks of a poorer quality of life from too little.
In spring 2021, based on earlier feedback from nurses, basic updates to clarify the protocol algorithms were made available. Later in 2021, more clarity was added and substantive updates were made to reduce workload for nurses and nephrologists by improving processes and streamlining workflow. These latest changes to the protocol algorithms are expected to be available on the BC Renal website by early 2022.
The committee recognizes that introducing changes in these difficult times of the pandemic is not ideal but hopes that ultimately they will make the protocols easier to follow and will consume less of everyone’s valuable time.
Peritoneal Dialysis Anemia Management Protocol
The following protocol, on order of physician, transfers anemia management of hemodialysis patients to non-physician staff (i.e. RNs and renal pharmacists). This protocol is intended to serve as a guide and cannot replace clinical judgment. The recommendations included may be inappropriate for specific clinical situations (e.g. patients with hemochromatosis, thalassemia, PRCA, allergy to IV iron or an erythropoiesis stimulating agent (ESA), history of stroke, active malignancy, history of malignancy, etc.). The lowest ESA dosage to achieve acceptable Hgb range should be used. This algorithm is based on the assumption that the patient is compliant to medication and blood work. Note: ESA refers to both epoetin alfa (Eprex®) and darbepoetin alfa (Aranesp®).
Any change in Hgb greater than or equal to 15 g/L, OR if Hgb is less than 85 g/L OR if Hgb is greater than 139 g/L AND on ESA (or ESA on hold) → Notify nephrologist
Hgb less than 95 g/L Hgb 95 to 115 g/L and stable Hgb greater than 115 g/L
NO Receiving ESA? YES
Check that the previous iron studies have been appropriately monitored and addressed prior to increasing the dose. • Check that the previous iron studies have been appropriately monitored and addressed prior to increasing the dose.
• If TSAT less than 22%, consider iron load instead of increasing ESA dosage.
NO No ESA required. CKD Non-Dialysis Anemia Management Protocol The following protocol, on order of physician, transfers anemia management of CKD non-dialysis patients to non-physician staff (i.e. RNs and renal pharmacists). The following protocol is intended to serve as a guide and cannot replace clinical judgement. The recommendations included may be inappropriate for specific clinical situations (e.g. patients with hemochromatosis, thalassemia, PRCA, allergy to IV iron or an erythropoiesis stimulating agent (ESA), hx of stroke, active malignancy, hx of malignancy, etc.). The lowest ESA dosage to achieve acceptable Hgb range should be used. This algorithm is based on the assumption that the patient is compliant to medication and blood work. Note: ESA refers to both epoetin alfa (Eprex®) and darbepoetin alfa (Aranesp®). Continue to monitor Hgb at the regular Hgb less than 95 g/L blood work cycle.
Hgb 95 to 115 g/L and stable
Hgb greater than 115 g/LAny change in Hgb greater than or equal to 15 g/L, OR if Hgb is less than 85 g/L OR if Hgb is greater than 139 g/L AND on ESA (or ESA on hold) → Notify nephrologist
Receiving ESA?
YES Receiving ESA?
NO YES
• Check that the previous iron studies have been appropriately monitored and addressed prior to increasing the dose. • If TSAT less than 22%, consider increasing PO iron dosage or prescribing IV iron YES
No ESA required. Continue to monitor Hgb at the regular blood work cycle.
ESA on hold or discontinued because Hgb above target
Maintain ESA dose and continue to monitor Hgb at the regular bloodwork cycle.
Consider starting ESA.
Suggested initial dose: epoetin 100 units/kg/wk or darbepoetin 0.9 mcg/kg/ 2 weeks. Obtain an order from MD to start anemia protocol.
BC Renal • BCRenal.ca Reviewed April 2021, Updated Nov 2021
Maintain ESA • Restart ESA at
dose and a reduced dose continue to based on the • • If no dose increase in the past 5 weeks, increase ESA dose as per ESA Dosage Adjustment Tables. If dose was increased in past 5 weeks, maintain that dose until next blood work. monitor Hgb at the regular bloodwork cycle. • dose before hold. Refer to protocol ESA Dosage Adjustment Tables. Continue Hgb monitoring at • Continue to monitor Hgb at the regular blood regular blood work cycle. work cycle.
• Notify MD if Hgb is not in target range after
3 consecutive dose increases. Refer to ESA Hyporesponsiveness Flowchart.
AFTER Hgb STATUS ASSESSMENT ABOVE, ASSESS IRON STATUS. Refer to page 2 for ferrous fumarate or intravenous iron protocol.
Receiving ESA?
NO ESA on hold or discontinued YES because Hgb above target
No ESA required. Continue to monitor Hgb at the regular blood work cycle.
Hgb 116 to 125 g/L Hgb greater than 125 g/L Hgb 116 to 125 g/L
• If there has been no dosage reduction in the past 5 weeks, reduce
ESA dosage as per protocol ESA Dosage
Adjustment Tables. • If there have been dosage reductions in the past 5 weeks, maintain current dose. • Measure Hgb at the regular blood work cycle.
• Hold ESA
• Measure Hgb in 2 weeks and reassess Hgb status and ESA dosage.
• If Hgb is greater than 125 g/L after 12 weeks of hold, discontinue
ESA - no ESA required.
Home Hemodialysis Anemia Management Protocol The following protocol, on order of physician, transfers anemia management of home hemodialysis patients to non-physician staff (i.e. RNs and renal pharmacists). This protocol is intended to serve as a guide and cannot replace clinical judgment. The recommendations included may be inappropriate for specific clinical situations (e.g. patients with hemochromatosis, thalassemia, PRCA, allergy to IV iron or an erythropoiesis stimulating agent (ESA), history of stroke, active malignancy, history of malignancy, etc.). The lowest ESA dosage to achieve acceptable Hgb range should be used. This algorithm is based on the assumption that the patient is compliant to medication and blood work. Note: ESA refers to both epoetin alfa (Eprex®) and darbepoetin alfa (Aranesp®). Any change in Hgb greater than or equal to 15 g/L, OR if Hgb is less than 85 g/L OR if Hgb is greater than 139 g/L AND on ESA (or ESA on hold) → Notify nephrologistHgb less than 95 g/L
NO Receiving ESA? YES If change is greater than 10 g/L If change is less than or equal to 10 from last g/L from last hemoglobin, hemoglobin, then resume then Check that the previous iron studies have been appropriately monitored and addressed prior to increasing the dose. continue to hold ESA. ESA at reduced dose. Refer to protocol ESA Dosage Adjustment Tables. Continue to monitor Hgb at the regular bloodwork cycle.
Consider starting ESA.
Suggested initial dose: epoetin 100 units/kg/wk or darbepoetin 0.45 mcg/kg/wk. Obtain an order from MD to start anemia protocol.
BC Renal • BCRenal.ca Reviewed April 2021, Updated Nov 2021
Hgb 95 to 115 g/L and stable
Receiving ESA? • Check that the previous iron studies have been appropriately monitored and addressed prior to increasing the dose. • If TSAT less than 22%, consider iron load instead of increasing ESA dosage. NO No ESA required. Continue to monitor Hgb at the regular YES blood work cycle. • If no dose increase in the past 5 weeks, increase ESA dose as per ESA Dosage Adjustment Tables. • If dose was increased in past 5 weeks, maintain that dose until next blood work. • Continue to monitor Hgb at the regular blood work cycle. • Notify MD if Hgb is not in target range after 3 consecutive dose increases. Refer to ESA Hyporesponsiveness Flowchart.
AFTER Hgb STATUS ASSESSMENT ABOVE, ASSESS IRON STATUS. Refer to page 2 for ferrous fumarate or intravenous iron protocol.
Maintain ESA dose and continue to monitor Hgb at the regular bloodwork cycle. • Restart ESA at a reduced dose based on the dose before hold. Refer to protocol ESA Dosage Adjustment Tables. • Continue Hgb monitoring at regular blood work cycle.
ESA on hold or discontinued because Hgb above target
Hgb greater than 115 g/L
Receiving ESA? NO ESA on hold or discontinued
No ESA YES because Hgb above target
required.
Continue to monitor Hgb at the regular blood work cycle.
Hgb 116 to 125 g/L Hgb greater than 125 g/L Hgb 116 to 125 g/L • If there has been no dosage reduction in the past 5 weeks, reduce ESA dosage as per protocol ESA Dosage Adjustment Tables. • If there have been dosage reductions in the past 5 weeks, • maintain current dose. Measure Hgb at the regular blood work cycle.
Restart ESA at a reduced dose based on the dose before hold. Refer to protocol ESA Dosage Adjustment • Tables. Continue Hgb monitoring at regular blood work cycle.
ESA on hold or discontinued because Hgb above target Receiving ESA?
NO YES
ESA on hold or discontinued because Hgb above target No ESA required. Continue to monitor Hgb at the regular blood work cycle.
Hgb 116 to 125 g/L Hgb greater than 125 g/L Hgb 116 to 125 g/L
If change is greater than 10 g/L from last hemoglobin, then resume ESA at reduced dose. If change is less than or equal to 10 g/L from last hemoglobin, then continue to hold ESA.
Refer to protocol ESA Dosage Adjustment Tables.
Continue to monitor Hgb at the regular bloodwork cycle. “As with all the clinical pathways that guide drug usage based on evidence, the anemia management protocol has resulted in very tangible benefits to patients and to BC Renal. It is a great example of putting evidencebased medicine into practice. As with all pathways, it has changed as new evidence becomes available. It also changes based on community feedback and the desire to make it more user-friendly.”
-Dan Martinusen, Chair, Pharmacy & Formulary Committee
What is anemia of chronic kidney disease?
• It is an iron deficiency anemia complicated by a lack of the hormone erythropoietin (EPO) normally produced by the kidneys.
Symptoms develop slowly and more commonly in people with diabetes and those over 60 years old.
• Symptoms can include fatigue, tiredness, shortness of breath, unusually pale skin, weakness, body aches, chest pain, dizziness, fainting, fast or irregular heartbeat, headaches, sleep problems, and trouble concentrating.
• If tests suggest that a person’s kidneys aren’t making enough
EPO hormone, they may need a manufactured form called an erythropoietin-stimulating agent (ESA).








